Abstract
Background:
Coronary Computed Tomography Angiography (CTA) has become one of the most important diagnostic imaging modalities for the evaluation of coronary artery diseases. Dur-ing coronary computed CTA, sufficient vascular enhancement is essential for the accurate detection and evaluation of lesions in the coronary arteries. To obtain optimal contrast enhancement and per-form appropriate clinical coronary CTA, physicians, radiologists, and radiology technologists should acquire a basic knowledge of contrast injection protocols.
Conclusion:
This review article summarizes the basic concepts of contrast injection protocols for coronary CTA.
Keywords: CT angiography, computed tomography, ECG, physicians, radiologists, radiology technologists
1. Introduction
With the introduction of 64-row multidetector Computed Tomography (CT), coronary CT Angiography (CTA) has emerged as effective noninvasive modalities for the evaluation of coronary artery diseases [1, 2]. During coronary CTA, sufficient vascular enhancement is crucial for the accurate detection and evaluation of lesions in the coronary arteries [3].
In recent years, there have been several advances in CT hardware and scanning techniques for coronary CTA, which are ongoing. Currently, various CT systems, such as 64-row, 128-row, 256-row, 320-row and dual-source CTs, are clinically used for coronary CTA. Furthermore, there is a wide variety of scan modes, including retrospective electrocardiogram (ECG)-gated helical scan, prospective ECG-triggered axial scan, prospective ECG-triggered volume axial scan with wide detector arrays, and prospective ECG-triggered helical scan with dual-source scanners. However, these mechanical and technical complexities make it difficult to choose an appropriate contrast injection protocol for coronary CTA. Having a complete understanding of contrast injection protocols is important to perform clinically feasible coronary CTA regardless of CT systems and scanning techniques.
This review article summarizes the basic concepts of contrast injection protocols for coronary CTA based on previous reports.
2. Basic knowledge of coronary artery contrast enhancement
Intracoronary contrast attenuation directly affects diagnostic performance and coronary plaque assessment in coronary CTA [4, 5]. Therefore, achieving diagnostically appropriate contrast enhancement is very important for the accurate diagnosis of coronary artery diseases with coronary CTA.
Concepts of an ideal contrast injection protocol for coronary CTA include the following:
Appropriate contrast enhancement.
Homogeneous contrast enhancement in all coronary arteries.
Minimal interpatient variability in contrast enhancement.
High reproducibility in contrast enhancement.
Simple technique.
Low cost.
Patient-friendly procedure.
Unfailing contrast injection protocols are clinically needed, and challenging protocols, such as using an extremely low Contrast Material (CM) dose, should be avoided in routine clinical practice.
Lower intracoronary attenuation of <300 HU on coronary CTA results in a reduced diagnostic accuracy of the detection of coronary artery stenosis, especially in distal coronary segments [3, 5]. Therefore, higher intracoronary attenuation is needed to achieve an appropriate diagnosis. On the other hand, attenuation of >500 HU leads to a significant underestimation of stenosis due to blooming artifacts [6]. In addition, higher attenuation interferes with coronary calcification [7]. Besides, intracoronary attenuation significantly affects coronary plaque attenuation when assessing coronary plaque characterization [4], as coronary plaque attenuation increases with lumen attenuation. Consequently, the target attenuation value of the proximal coronary artery is considered to be 350–400 HU [6, 8, 9].
3. Contrast volume
The Society of Cardiovascular Computed Tomography (SCCT) guidelines for the performance and acquisition of coronary CTA mentions that contrast volume should be adapted to the scan time and patient’s physique [10]. Typical contrast volumes range from 50 to 100 mL with high iodine concentrations (usually 320–400 mgI/mL). A patient weight-tailored CM dose protocol can yield steady vessel enhancement. In fact, previous reports recommend a contrast volume of 245–370 mgI/kg with a short injection duration [11, 12].
In recent years, the incidence of Contrast-induced Nephropathy (CIN) after an intravenous delivery of CM for contrast-enhanced CT has remained controversial [13]. Nevertheless, the risks and benefits of contrast injection in patients at risk of CIN must be carefully considered. Risk factors for CIN include an estimated glomerular filtration rate of <45 mL/min/m2, severe heart disease, dehydration, diabetes mellitus, multiple iodinated CM doses in a short time interval (<24 h), and use of nephrotoxic medications, such as nonsteroidal anti-inflammatory drugs and diuretics [14]. These risk factors should be assessed before examination, after which the lowest diagnostically required contrast volume should be used. The following points should be considered when performing coronary CTA in patients at risk of CIN: alternative imaging (such as stress testing), minimization of contrast volume, and prescan hydration. The SCCT guidelines recommend lower tube voltage acquisition with iterative reconstruction techniques for low CM dose protocols in patients at risk of CIN [10].
Scanning with a low-tube voltage (kilovoltage peak [kVp]) yields higher contrast enhancement than that with the standard 120 kVp because the x-ray output energy at low kVp is closer to the iodine K-edge at 33 keV [15], resulting in CM dose reduction. This method has been widely used in various CT scan protocols [16-21]. In principle, the CM dose can be reduced by 20% using 100 kVp scanning and by 40% using 80 kVp scanning [22-24]. However, 80 kVp scanning is applicable only for slim patients [16]. In obese patients, 80 kVp coronary CTA tends to yield poorer quality images because of the increased image noise attributable to radiation scattering and absorption.
4. Injection duration
The injection duration should be set in consideration of the estimated scan time. Optimal arterial enhancement should be continued for longer than the estimated scan time. Fig. (1) shows a simulated Time–density Curve (TDC) for coronary CTA. A very short contrast injection duration cannot achieve optimal enhancement (350-400 HU). A short injection duration of <10 s may be inadequate to achieve sufficient contrast enhancement of all coronary arteries, especially the distal segments (Fig. 2A). On the other hand, a longer injection duration of >20s results in streak artifacts arising from the right atrium, which can interfere with the coronary arteries [7] (Fig. 2B). Therefore, a contrast injection duration of 10-20s is considered optimal. Handling of patients with abnormal cardiac output requires attention, as cardiac output significantly affects arterial contrast enhancement [25]. It is often difficult to achieve optimal contrast enhancement in patients with the abnormal cardiac output (both high and low cardiac output). Therefore, a longer injection duration is recommended for patients with abnormal cardiac output [10]. Checking on cardiac enlargement on a scout image is helpful to recognize an abnormal cardiac output before contrast injection.
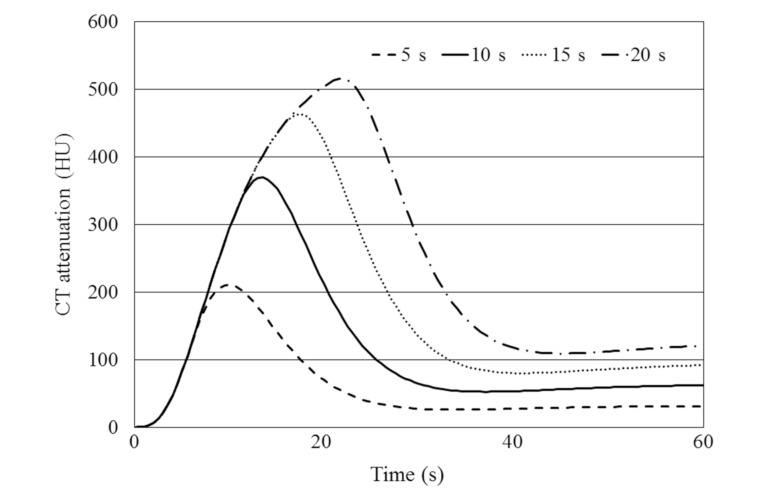
Fig. (1).
Simulated time–density curves of the ascending aorta of a hypothetical adult male (body weight, 60 kg) subjected to varying injection durations (5, 10, 15, and 20 s) of contrast material injected at 5 mL/s. A short injection duration of 5 s was insufficient to achieve optimal contrast enhancement (350-400 HU).
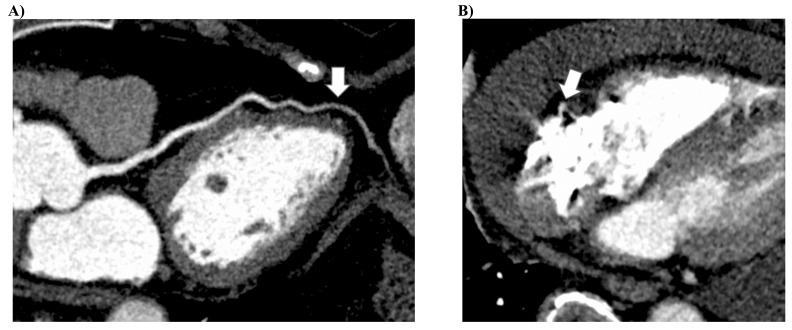
Fig. (2).
(A) A curved multiplanar reconstruction image of the left anterior descending artery acquired under a shorter injection duration of 7 s. Contrast enhancement of the coronary artery is insufficient, especially in the distal segments (arrow). (B) An axial source images acquired with a long injection duration of 30 s. A streak artifact arising from the right atrium interfered with the right coronary artery (arrow).
5. Flow rate
When the contrast injection duration is fixed, a faster flow rate increases, both the delivery rate and total delivered amount of CM, which results in a higher magnitude of arterial enhancement (Fig. 3). On the other hand, when the total amount of CM is fixed, a faster injection increases the delivery rate but shortens the injection duration and time to peak enhancement. For coronary CTA, a flow rate of >4 mL/s is preferred to achieve sufficient arterial contrast enhancement. Actually, the flow rate is determined based on the contrast volume and injection duration. Besides, the risk of contrast extravasation due to a high flow rate should also be considered.
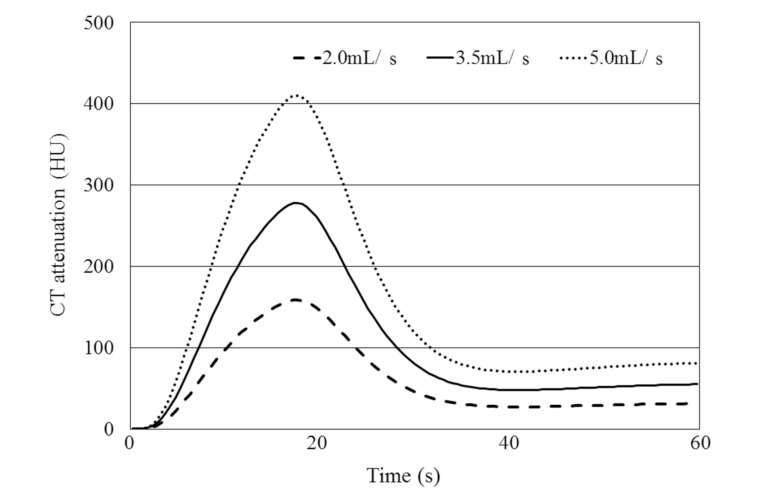
Fig. (3).
Simulated time–density curves of the ascending aorta of a hypothetical adult male (body weight, 60 kg) subjected to a fixed injection duration of 15 s injected at 2.0, 3.5, and 5.0 mL/s. As the flow rate increases, the magnitude of contrast enhancement increases.
6. Saline Flush
A saline flush is helpful when small amounts of CM is used because it pushes the last of the injected CM into the central blood volume, making use of CM that would otherwise remain in the injection tubing and peripheral veins [26]. A saline flush also reduces streak artifacts attributable to dense CM from the superior vena cava and right ventricle that can limit diagnosis of the right coronary artery [27, 28]. Previous studies indicated that a saline flush allowed the use of significantly less CM while maintaining the coronary enhancement obtained with a larger CM volume [28, 29]. An injection rate of 4-5 mL/s as a saline flush is reported to be optimal to achieve maximum enhancement of the coronary arteries using 64-row CT [29]. In practice, contrast injection at 4-5 mL/s is followed by the injection of a saline solution delivered at the same injection rate as the CM. Thirty millimeters of saline may be an appropriate amount for optimal coronary enhancement [30]. Flushing with diluted CM instead of a saline solution is helpful to visualize and assess the right ventricle, as well as the coronary arteries and left ventricle [31].
7. Scan timing methods
The determination of an appropriate scan timing (scan delay) for optimal coronary artery enhancement of each individual is crucial. There are two major scan timing methods, bolus-tracking and test bolus methods [32] (Figs. 4 and 5).
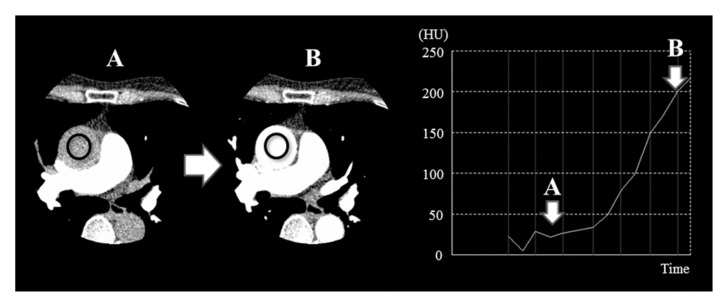
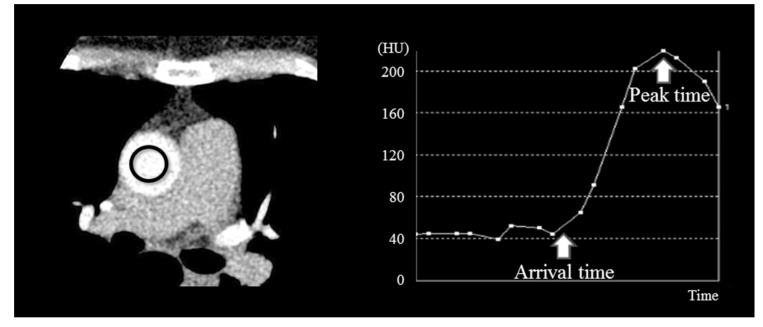
Fig. (4).
Bolus-tracking method. After the start of contrast injection, a region of interest is placed in the ascending aorta and continuous scans are acquired to monitor the CT number of the ascending aorta. A coronary CTA scan is started after the CT number reaches a threshold of 200 HU in the ascending aorta. Scan images A and B correspond to A and B with arrows on the time–density curve.
Fig. (5).
Test bolus method. After intravenous delivery of a small contrast volume (12 mL), a time–density curve (TDC) is acquired via continuous scanning of the ascending aorta. Then, an optimal scan delay is determined from the TDC data.
In the bolus-tracking method, after the start of contrast injection, a region of interest is placed in the artery (usually, in the ascending aorta) and continuous scans are acquired to monitor the CT number of the artery using minimal radiation. Coronary CTA scan is started after the CT number reaches a specific threshold (usually 150-250 HU in the ascending aorta). Disadvantages of this method are 1) Interpatient variability of contrast enhancement due to the post-trigger delay time (approximately 7 s) and 2) Contrast enhancement is subject to the patient’s cardiac output.
With the test bolus method, after intravenous delivery of a small contrast volume (10-20mL of CM), a TDC is acquired via the continuous scanning of the target artery using minimal radiation. Then, the optimal scan delay is determined from the TDC data. A prediction formula for peak enhancement of a targeted artery depending on the duration of injection, as reported by Bae [26], is presented as follows.
When the injection duration is < 15 s,
Arterial peak enhancement = Test_arrival + contrast injection duration/2 [s].
When the injection duration is ≥15 s,
Arterial peak enhancement = Test_arrival + contrast injection duration − 5 [s],
Where Test_arrival is the arrival time of the CM in the target artery in test bolus scanning. The disadvantages of the test bolus method are 1) The need for two contrast injections, 2) Prolonged duration, and 3) Technical complexity.
8. Summary of the basic concepts of contrast injection protocols for coronary CTA
The following is a summary of the key points of the CM injection protocol for coronary CTA.
Unfailing contrast injection protocols are clinically needed.
The target coronary attenuation value is 350–400 HU.
The contrast volume of 245–370 mgI/kg is optimal.
Contrast injection duration of 10-20s is recommended.
A high flow rate of 4–5 mL/s is preferred.
A saline flush should be used at the same injection rate as the CM.
Bolus-tracking or test bolus method should be used.
Conclusion
To perform appropriate clinical coronary CTA, physicians, radiologists, and radiology technologists should acquire a basic knowledge of contrast injection protocols.
Acknowledgements
Declared none.
Consent for Publication
Not applicable.
Conflict of interest
The authors declare no conflict of interest, financial or otherwise.
References
- 1.Budoff M.J., Dowe D., Jollis J.G., et al. Diagnostic performance of 64-multidetector-row coronary computed tomographic angiography for evaluation of coronary artery stenosis in individuals without known coronary artery disease: Results from the prospective multicenter ACCURACY (Assessment by Coronary Computed Tomographic Angiography of Individuals Undergoing Invasive Coronary Angiography) trial. J. Am. Coll. Cardiol. 2008;52(21):1724–1732. doi: 10.1016/j.jacc.2008.07.031. [DOI] [PubMed] [Google Scholar]
- 2.Miller J.M., Rochitte C.E., Dewey M., et al. Diagnostic performance of coronary angiography by 64-row CT. N. Engl. J. Med. 2008;359(22):2324–2336. doi: 10.1056/NEJMoa0806576. [DOI] [PubMed] [Google Scholar]
- 3.Cademartiri F., Mollet N.R., Lemos P.A., et al. Higher intracoronary attenuation improves diagnostic accuracy in MDCT coronary angiography. AJR Am. J. Roentgenol. 2006;187(4):W430-3. doi: 10.2214/AJR.05.1406. [DOI] [PubMed] [Google Scholar]
- 4.Cademartiri F., Mollet N.R., Runza G., et al. Influence of intracoronary attenuation on coronary plaque measurements using multislice computed tomography: Observations in an ex vivo model of coronary computed tomography angiography. Eur. Radiol. 2005;15(7):1426–1431. doi: 10.1007/s00330-005-2697-x. [DOI] [PubMed] [Google Scholar]
- 5.Cademartiri F., Maffei E., Palumbo A.A., et al. Influence of intra-coronary enhancement on diagnostic accuracy with 64-slice CT coronary angiography. Eur. Radiol. 2008;18(3):576–583. doi: 10.1007/s00330-007-0773-0. [DOI] [PubMed] [Google Scholar]
- 6.Fei X., Du X., Yang Q., et al. 64-MDCT coronary angiography: Phantom study of effects of vascular attenuation on detection of coronary stenosis. AJR Am. J. Roentgenol. 2008;191(1):43–49. doi: 10.2214/AJR.07.2653. [DOI] [PubMed] [Google Scholar]
- 7.Becker C.R., Hong C., Knez A., et al. Optimal contrast application for cardiac 4-detector-row computed tomography. Invest. Radiol. 2003;38(11):690–694. doi: 10.1097/01.rli.0000084886.44676.e4. [DOI] [PubMed] [Google Scholar]
- 8.Hausleiter J., Meyer T.S., Martuscelli E., et al. Image quality and radiation exposure with prospectively ECG-triggered axial scanning for coronary CT angiography: The multicenter, multivendor, randomized PROTECTION-III study. JACC Cardiovasc. Imaging. 2012;5(5):484–493. doi: 10.1016/j.jcmg.2011.12.017. [DOI] [PubMed] [Google Scholar]
- 9.Utsunomiya D., Tanaka R., Yoshioka K., et al. Relationship between diverse patient body size- and image acquisition-related factors, and quantitative and qualitative image quality in coronary computed tomography angiography: A multicenter observational study. Jpn. J. Radiol. 2016;34(8):548–555. doi: 10.1007/s11604-016-0556-0. [DOI] [PubMed] [Google Scholar]
- 10.Abbara S., Blanke P., Maroules C.D., et al. SCCT guidelines for the performance and acquisition of coronary computed tomographic angiography: A report of the society of Cardiovascular Computed Tomography Guidelines Committee: Endorsed by the North American Society for Cardiovascular Imaging (NASCI). J. Cardiovasc. Comput. Tomogr. 2016;10(6):435–449. doi: 10.1016/j.jcct.2016.10.002. [DOI] [PubMed] [Google Scholar]
- 11.Tatsugami F., Kanamoto T., Nakai G., et al. Reduction of the total injection volume of contrast material with a short injection duration in 64-detector row CT coronary angiography. Br. J. Radiol. 2010;83(985):35–39. doi: 10.1259/bjr/23203690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nakaura T., Awai K., Yauaga Y., et al. Contrast injection protocols for coronary computed tomography angiography using a 64-detector scanner: Comparison between patient weight-adjusted- and fixed iodine-dose protocols. Invest. Radiol. 2008;43(7):512–519. doi: 10.1097/RLI.0b013e3181727505. [DOI] [PubMed] [Google Scholar]
- 13.McDonald R.J., McDonald J.S., Newhouse J.H., Davenport M.S. Controversies in contrast material-induced acute kidney injury: Closing in on the truth? Radiology. 2015;277(3):627–632. doi: 10.1148/radiol.2015151486. [DOI] [PubMed] [Google Scholar]
- 14.Committee on Drugs and Contrast Media https://www.acr.org/Quality-Safety/Resources/
- 15.Nakayama Y., Awai K., Funama Y., et al. Abdominal CT with low tube voltage: Preliminary observations about radiation dose, contrast enhancement, image quality, and noise. Radiology. 2005;237(3):945–951. doi: 10.1148/radiol.2373041655. [DOI] [PubMed] [Google Scholar]
- 16.Oda S., Utsunomiya D., Funama Y., et al. A hybrid iterative reconstruction algorithm that improves the image quality of low-tube-voltage coronary CT angiography. AJR Am. J. Roentgenol. 2012;198(5):1126–1131. doi: 10.2214/AJR.11.7117. [DOI] [PubMed] [Google Scholar]
- 17.Nakaura T., Nakamura S., Maruyama N., et al. Low contrast agent and radiation dose protocol for hepatic dynamic CT of thin adults at 256-detector row CT: Effect of low tube voltage and hybrid iterative reconstruction algorithm on image quality. Radiology. 2012;264(2):445–454. doi: 10.1148/radiol.12111082. [DOI] [PubMed] [Google Scholar]
- 18.Oda S., Utsunomiya D., Funama Y., et al. Evaluation of deep vein thrombosis with reduced radiation and contrast material dose at computed tomography venography: Clinical application of a combined iterative reconstruction and low-tube-voltage technique. Circ. J. 2012;76(11):2614–2622. doi: 10.1253/circj.cj-12-0032. [DOI] [PubMed] [Google Scholar]
- 19.Utsunomiya D., Oda S., Funama Y., et al. Comparison of standard- and low-tube voltage MDCT angiography in patients with peripheral arterial disease. Eur. Radiol. 2010;20(11):2758–2765. doi: 10.1007/s00330-010-1841-4. [DOI] [PubMed] [Google Scholar]
- 20.Yamamura S., Oda S., Imuta M., et al. Reducing the radiation dose for CT colonography: Effect of low tube voltage and iterative reconstruction. Acad. Radiol. 2016;23(2):155–162. doi: 10.1016/j.acra.2015.03.009. [DOI] [PubMed] [Google Scholar]
- 21.Yamamura S., Oda S., Utsunomiya D., et al. Dynamic computed tomography of locally advanced pancreatic cancer: Effect of low tube voltage and a hybrid iterative reconstruction algorithm on image quality. J. Comput. Assist. Tomogr. 2013;37(5):790–796. doi: 10.1097/RCT.0b013e318296db2b. [DOI] [PubMed] [Google Scholar]
- 22.Itatani R., Oda S., Utsunomiya D., et al. Reduction in radiation and contrast medium dose via optimization of low-kilovoltage CT protocols using a hybrid iterative reconstruction algorithm at 256-slice body CT: Phantom study and clinical correlation. Clin. Radiol. 2013;68(3):e128–e135. doi: 10.1016/j.crad.2012.10.014. [DOI] [PubMed] [Google Scholar]
- 23.Oda S., Weissman G., Vembar M., Weigold W.G. Iterative model reconstruction: Improved image quality of low-tube-voltage prospective ECG-gated coronary CT angiography images at 256-slice CT. Eur. J. Radiol. 2014;83(8):1408–1415. doi: 10.1016/j.ejrad.2014.04.027. [DOI] [PubMed] [Google Scholar]
- 24.Oda S., Utsunomiya D., Yuki H., et al. Low contrast and radiation dose coronary CT angiography using a 320-row system and a refined contrast injection and timing method. J. Cardiovasc. Comput. Tomogr. 2015;9(1):19–27. doi: 10.1016/j.jcct.2014.12.002. [DOI] [PubMed] [Google Scholar]
- 25.Kidoh M., Nakaura T., Funama Y., et al. Paradoxical effect of cardiac output on arterial enhancement at computed tomography: Does cardiac output reduction simply result in an increase in aortic peak enhancement? J. Comput. Assist. Tomogr. 2017;41(3):349–353. doi: 10.1097/RCT.0000000000000541. [DOI] [PubMed] [Google Scholar]
- 26.Bae K.T. Intravenous contrast medium administration and scan timing at CT: Considerations and approaches. Radiology. 2010;256(1):32–61. doi: 10.1148/radiol.10090908. [DOI] [PubMed] [Google Scholar]
- 27.de Monye C., Cademartiri F., de Weert T.T., Siepman D.A., Dippel D.W., van Der Lugt A. Sixteen-detector row CT angiography of carotid arteries: Comparison of different volumes of contrast material with and without a bolus chaser. Radiology. 2005;237(2):555–562. doi: 10.1148/radiol.2372040653. [DOI] [PubMed] [Google Scholar]
- 28.Cademartiri F., Mollet N., van der Lugt A., et al. Non-invasive 16-row multislice CT coronary angiography: Usefulness of saline chaser. Eur. Radiol. 2004;14(2):178–183. doi: 10.1007/s00330-003-2188-x. [DOI] [PubMed] [Google Scholar]
- 29.Kim D.J., Kim T.H., Kim S.J., et al. Saline flush effect for enhancement of aorta and coronary arteries at multidetector CT coronary angiography. Radiology. 2008;246(1):110–115. doi: 10.1148/radiol.2453061953. [DOI] [PubMed] [Google Scholar]
- 30.Behrendt F.F., Bruners P., Keil S., et al. Effect of different saline chaser volumes and flow rates on intravascular contrast enhancement in CT using a circulation phantom. Eur. J. Radiol. 2010;73(3):688–693. doi: 10.1016/j.ejrad.2009.01.008. [DOI] [PubMed] [Google Scholar]
- 31.Utsunomiya D., Awai K., Sakamoto T., et al. Cardiac 16-MDCT for anatomic and functional analysis: Assessment of a biphasic contrast injection protocol. AJR Am. J. Roentgenol. 2006;187(3):638–644. doi: 10.2214/AJR.05.0612. [DOI] [PubMed] [Google Scholar]
- 32.Cademartiri F., Nieman K., van der Lugt A., et al. Intravenous contrast material administration at 16-detector row helical CT coronary angiography: Test bolus versus bolus-tracking technique. Radiology. 2004;233(3):817–823. doi: 10.1148/radiol.2333030668. [DOI] [PubMed] [Google Scholar]