Abstract
Dystrophinopathies are caused by mutations in DMD resulting in progressive muscle weakness. They are historically divided into the more severe Duchenne (DMD) and milder Becker (BMD) muscular dystrophy phenotypes. Classification is important for research and clinical care. The purpose of this study was to describe a multi-variable approach to classifying cases from the Muscular Dystrophy Surveillance, Tracking, and Research Network (MD STARnet) and to assess the accuracy of the diagnostic classification scheme. We used age at loss of mobility, molecular testing results, and age at symptom onset to classify cases as having DMD or BMD and to assess sensitivity and specificity. Mobility status showed low sensitivity and high specificity for predicting DMD (65.5% and 99.3%, respectively) and BMD (62.8% and 97.7%, respectively) phenotypes. Molecular testing showed 90.9% sensitivity and 66.4% specificity for DMD; 76.3% sensitivity and 90.0% specificity for BMD. Age of onset predicted DMD with sensitivity of 73.9% and specificity of 69.0%; BMD had 99.7% specificity and 36.7% sensitivity. Mobility status, molecular test results, and age at symptom onset are important but inconsistent measures for accurately classifying individuals into DMD or BMD phenotypes. These results have implications for prognosis in newly diagnosed individuals and for classifying phenotype in clinical trials.
Keywords: Muscular dystrophies, Duchenne, Becker, phenotype, diagnostic accuracy, dystrophinopathy
INTRODUCTION
Dystrophinopathies are X-linked disorders characterized by progressive muscle weakness primarily affecting males. They are caused by mutations in the DMD gene that affect production of the dystrophin protein. Duchenne muscular dystrophy (DMD) is at the severe end of the spectrum with early loss of ambulation and compromised skeletal, respiratory, cardiac, and sometimes cognitive function [1]. Becker muscular dystrophy (BMD) has a milder presentation with slower disease progression, later age at loss of ambulation, and variable involvement of the cardiac and respiratory systems [1].
Although attempts at classifying affected individuals into DMD and BMD phenotypes are important for research and clinical care, there is a clinical spectrum of severity in individuals with dystrophinopathies that does not always segregate them into distinct categories [2]. This variability in clinical severity makes classification of some cases difficult, and complicates issues such as determining patient eligibility for clinical trials where phenotype is an eligibility requirement [3, 4]. To differentiate cases that do not fit the typical DMD or BMD phenotypes, numerous boundary-spanning terms, including classifications from mild to severe or intermediate muscular dystrophy, have been reported in the literature [4–8]. Some research has identified potential severity sub-groups within phenotypes, which further exacerbates the classification dilemma [6, 7, 9].
Classification can be even more difficult when using data from retrospective research studies such as the Muscular Dystrophy Surveillance, Tracking, and Research Network (MD STARnet), a population-based surveillance system for muscular dystrophy funded by the Centers for Disease Control and Prevention. However, compared to prospective studies, retrospective studies might provide a more complete clinical course for determining phenotype because they include entire populations of affected individuals at various stages in their disease progression. MD STARnet investigators have used a variety of approaches to exclude DMD or BMD cases from specific analyses in which just one phenotype was the focus of study. While numerous approaches to classify phenotype and severity exist, no single variable has been found to be sufficient and a multivariable approach is required [2].
Therefore, the purposes of this study are to: evaluate the multivariable approach to phenotype classification with selected clinical measures available in the MD STARnet dataset, 2) estimate the diagnostic accuracy of each selected clinical measure independently, and 3) compare the multivariable approach of assigning phenotype to other classification schemes found in the literature.
METHODS
Case population
MD STARnet contains longitudinal clinical outcomes data gathered from clinic sources for individuals diagnosed with a childhood-onset dystrophinopathy, born on or after January 1, 1982, and residing in an MD STARnet site (Arizona, Colorado, Georgia, Hawaii, Iowa, and 12 counties in western New York State). MD STARnet collects medical record data from inpatient and outpatient records from multiple sources, with a focus on neuromuscular clinics. Data collection occurred retrospectively from the time of case identification through death or 2012. Trained abstractors reviewed records annually for additional information until death, movement out of the surveillance area, or the end of the surveillance program. Data collected included demographics, diagnostics, medical history, treatment and management, and family history information. This project used Version 8 data. A full description of MD STARnet methodology has been published [10, 11].
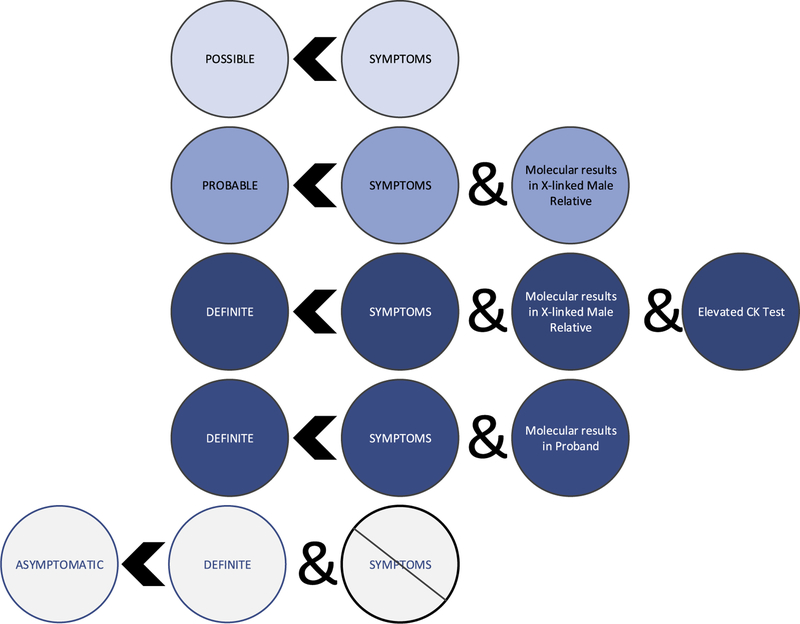
All cases abstracted in MD STARnet undergo review by a committee of neuromuscular clinical experts who assess the clinical signs and symptoms, family history information, and laboratory data to assign a case status (definite, probable, possible, asymptomatic, affected female, or not affected). The MD STARnet case status assignments included in this analysis are described in detail in previous publications and are shown in Fig. 1 [10, 11]. Affected females and confirmed DMD pregnancy terminations were excluded from this phenotype classification project. There is no differentiation between DMD and BMD cases within the MD STARnet case assignment status; therefore, a systematic method for assigning phenotype was needed.
Fig. 1.
Muscular Dystrophy Surveillance Tracking and Research Network case classification criteria.
Multivariable approach to phenotype classification
For this study, we searched for publications in PubMed and Embase. We reviewed key publications to identify clinical measures for phenotype classification. Evidence from the reviewed publications was consolidated to create index variables (hereinafter referred to as index) to classify reference standards (hereinafter referred to as phenotype) as described in Table 1. We used mobility, symptom onset, and molecular test results as indices to classify cases into DMD or BMD phenotypes. The mobility index included a combination of steroid use and ambulation status and the molecular index was based on genetics frameshift or western blot dystrophin quantities. This scheme is described in more detail in the Indices section below and in Table 1.
Table 1.
Clinical variables grouped into three indices to define phenotypes in the MD STARnet dataset
| Variables for Mobility Index | Variables for Molecular Index | Variable for Onset Index | |||||
|---|---|---|---|---|---|---|---|
| Phenotype | Ambulation Ceased† | Steroid Use | Genetics | Western Blot | Symptom Onset | ||
| DMD | <12 years [2,5,6, 16] |
and | Any level of use, non-use, or unknown use |
Reading Frame shift (Del/Dup) or stop/nonsense PM [2, 8.9, 18–21,23,24] |
or | <5% noted or absent [2, 9, 12, 18–20, 23] |
<5 years [2, 16, 19] |
| < 16 years [17–24] |
and | >24 m continuous use before ambulation ceased or age 12 years; gap < 1 m [17, 19^ 22] |
Reading Frame shift (Del/Dup) or stop/nonsense PM [2, 8.9. 18–21,23,24] |
or | <5% noted or absent [2, 9, 12, 18–20, 23] |
<5 years [2, 16, 19] |
|
| BMD | (or ambulating) > 16 years [2,5,6,16,21] |
and | Any level of use, non-use, or unknown use |
No reading Frame shift (Del/Dup) or missense PM [2. 8.21] |
or | >20% noted or decreased [2, 12] |
>10 years [2, 16] |
Various sources show 12/13 years < Duchenne muscular dystrophy; 12/13 years ≤ intermediate muscular dystrophy ≤15/16 years; Becker muscular dystrophy ≥15/16 years.
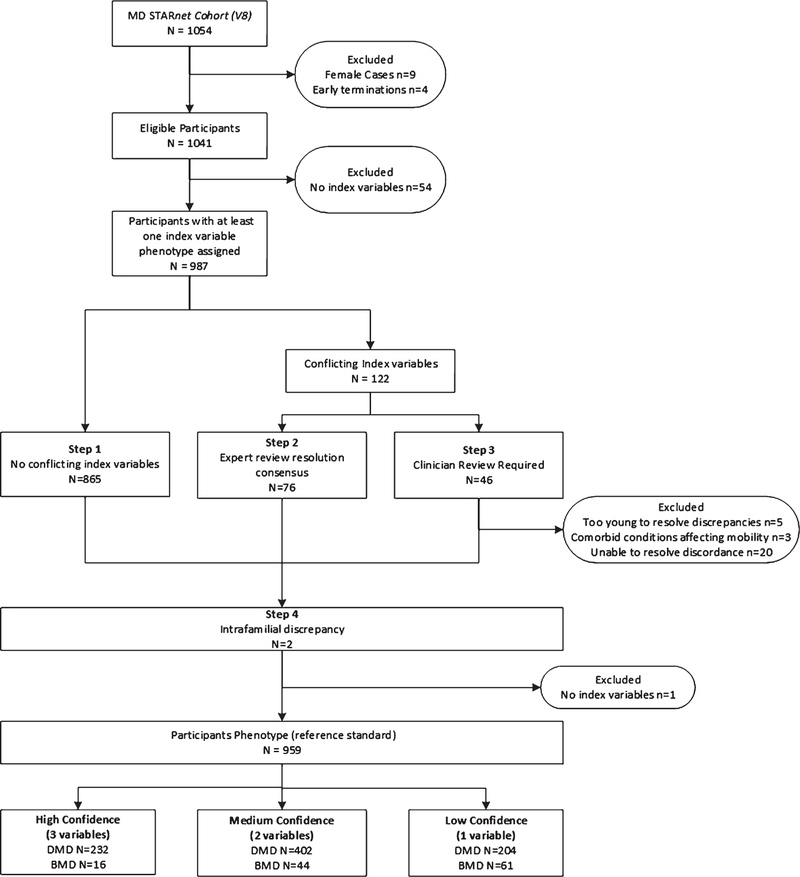
Using a four-step process shown in Fig. 2, we assigned the phenotypes (DMD, BMD, or Inconclusive) for all cases in MD STARnet with available data. If the three indices indicated the same phenotype for a given case, that case was assigned a DMD or BMD phenotype. Assignment of an inconclusive phenotype resulted from indices that contained valid data, but for which the values fell outside the range specified for either DMD or BMD (Table 1). Phenotypes were set to missing if there were no data available to define them.
Fig. 2.
Inclusion and exclusion of Muscular Dystrophy Surveillance Tracking and Research Network (MD STARnet) cases in classifying phenotypes. DMD: Duchenne muscular dystrophy; BMD: Becker muscular dystrophy.
Given the multivariable approach to assigning phenotypes, we also classified the level of certainty for an assigned phenotype based on the number of indices available. Low certainty indicated only one index was available to assign the phenotype; high certainty indicated that all three indices were available to assign the phenotype. In the majority of cases (n = 865, 88%) there were no discrepancies in the assignment of a phenotype (Fig. 2, Step 1).
Processing of cases with discrepancies in the phenotype assigned by the indices included up to two additional steps. Each case was reviewed independently by two MD STARnet researchers (CW, JA), who were very familiar with the dataset and who were able to locate additional data to clarify conflicts or declare them unresolvable. Data fields reviewed for additional information were those with descriptive free text from diagnosis notes, muscle biopsy and genetic testing results, and text documenting mobility limitations, signs and symptoms, and any general information not commonly associated with index variables. For every case for which there was a discrepancy in phenotype assignment across indices, reviewers created an annotated database with all factors in favor or against the assignment of a phenotype and proposed a resolution of the discrepancy. Resolution occurred by 1) dropping an index with a variable of questionable value, 2) revising a variable for an index based on evidence not considered during the initial classification, or 3) clinician review (Fig. 3, Step 3). Resolution of discrepancies involving the molecular index relied on predictions of phenotypic variability for genetic mutations reported in the Leiden, Edystrophin, and UMD databases, as well as reversal hotspots reported in the literature [2, 5, 6, 12–15]. Resolution involving the mobility and onset index values was typically achieved by dropping the index due to insufficient evidence supporting the value of a variable to classify the phenotype. Data were also reviewed when siblings were classified as having different phenotypes through the process described above. Resolved cases were then assigned a final phenotype (Fig. 2, Steps 2 and 4).
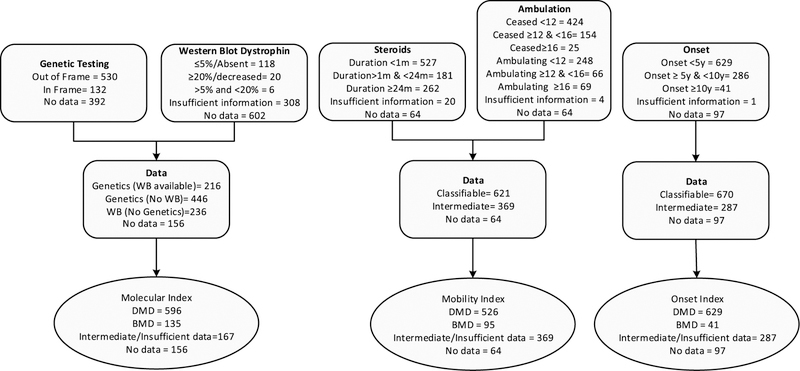
Fig. 3.
Flow chart of data availability for classification of each index variable in the entire cohort (N = 1054). Insufficient information demonstrates an indication that testing, steroid use or onset documentation exists in the record but not enough information is provided to allow for phenotype prediction for the index variable. Intermediate classifies all cases whose values fall in between the designated cut-offs for BMD and DMD (e.g. Western Blot Dystrophin between 5% and 20%). Intermediate categories for the remaining index variables can be determined using Table 1. WB – Western Blot, DMD – Duchenne muscular dystrophy, BMD – Becker muscular dystrophy.
Cases delegated to the clinician review team (EC, DM, KM) were those for which resolution was not directly attributable to evidence in the record, were more complicated, or for which the expert reviewers (JA, CW) requested consensus review (Fig. 2, Step 3). Members of this team independently coded each case as DMD, BMD or undetermined based on their clinical judgement of the information presented before the final phenotype assignment was made on a consensus conference call. All discordant cases with similar criteria were treated the same to ensure any decisions made were systematically applied. This most notably included those cases classified as having the DMD phenotype according to symptom onset and molecular results, but not according to the mobility index, and were ambulating well beyond the BMD reference standard. The discordant case resolutions applied only to the phenotypes assigned through the three indices. The original values of the variables in question were unchanged to allow for an unbiased analysis of the diagnostic accuracy of the phenotypes.
Indices
Mobility index
The mobility index was derived from the documented age at which independent ambulation ceased. It includes two conditions: age regardless of steroid use, and the total duration of steroid treatment prior to the age at which ambulation ceased. The DMD phenotype was defined according to the mobility index as documentation of ceased ambulation or full-time wheelchair use before the individual’s 12th birthday, regardless of steroid use, or 2) documentation of ceased ambulation or full-time wheelchair use prior to the individual’s 16th birthday, if steroid treatment was received continuously for at least two years before ceasing ambulation [2, 5, 6, 16–24]. The continuous use requirement allowed for gaps in use of steroids shorter than 30 days. The BMD phenotype, according to the mobility index, was defined as documentation of independent ambulation on or after the individual’s 16th birthday regardless of steroid use [2, 5, 6, 16, 21].
Molecular index
The molecular index combined results from genetic mutation analysis and western-blot dystrophin levels obtained from a muscle biopsy. The DMD phenotype, according to the molecular index, was defined as the presence of a mutation predicting a shift in the mRNA reading frame (out-of-frame) or a western blot test documenting dystrophin levels of 5% or less [2, 5, 7, 8, 12]. When both values were present, the genetic mutation information prevailed over the western blot data. The BMD phenotype, according to the molecular index, was defined as evidence of an in-frame mutation or western blot test documenting dystrophin levels of 20% or higher [2, 8, 12, 21]. Frameshift information was obtained from the Leiden neuromuscular reading frame checker [15].
Onset index
The onset index variable refers to the earliest documented age of first symptom, which included any of the following: gross motor delays, positive Gowers sign, trouble walking or running, trouble climbing, frequent falls, abnormal gait, and inability to keep up with peers. According to the onset index, the DMD phenotype was defined as age of first symptom that occurred before the 5th birthday. The BMD phenotype was defined as age of first symptom that occurred on or after the 10th birthday [2, 9, 12, 17]. Cases with symptom onset ages that did not meet these criteria were assigned an inconclusive phenotype.
Statistical analysis
We used chi-square tests to evaluate the association between demographic variables and MD STARnet cases classified with a DMD or BMD phenotype. Additionally, we tested the accuracy of the three indices (mobility, molecular, onset) in identifying DMD and BMD phenotypes by measuring sensitivity, specificity, positive predictive value, and negative predictive value in Microsoft Excel using the gold standard generated from the criteria reported in the literature (See Table 1). We also used receiver operating characteristic (ROC) curves to evaluate the ability of each index to discriminate muscular dystrophy phenotypes by estimating areas under the curve (AUC) and the corresponding 95% confidence intervals and standard errors. Cases with missing values for a given index were not included in the diagnostic accuracy analyses for that index.
Finally, we classified MD STARnet cases using criteria from several studies to demonstrate the value of including multiple variables to assign phenotype. The criteria in the literature included different combinations and cut-off values for the same criteria included in our multivariable approach.
RESULTS
Use of indices to assign phenotypes
The MD STARnet database contains 1,054 individual cases. After initial exclusions, 987 cases were available for phenotypic classification. Out of 987 cases, 85% (n = 838) were classified as DMD, 12% (n = 121) as BMD, and 3% (n = 28) were unclassifiable. Of the 838 DMD cases, the certainty of the assigned phenotype was considered high for 28% of cases, medium for 48%, and low for 24% of cases. Regarding the certainty of the BMD phenotypes, 13%, 36%, and 50% were considered high, medium, and low, respectively. Non-classifiable cases were either too young to determine ambulation status (last known ambulation age <13 years) (n = 5), had a comorbid condition affecting ambulation (n = 3), or had conflicting index variable phenotypes that could not be resolved (n = 20). Of these 20 unresolvable discrepant cases, 11 had values indicating the DMD phenotype according to onset and molecular indices, but were assigned the BMD phenotype according to the mobility index, due to evidence of walking beyond their 16th birthday. The remaining nine cases had varying combinations of BMD, DMD, and inconclusive phenotype assignments, making resolution difficult.
For classification with the mobility index, 95% (n = 942) of eligible cases had either ambulation or steroid data. Among this group, 62% (n = 615) had values assigned as DMD or BMD, and 33% (n = 327) were inconclusive (Table 2). Two cases were excluded from sensitivity analysis for the mobility index as they contained only steroid data and no ambulation information. For the molecular index, there were 724 eligible cases. Of these, 723 had phenotypes assigned as DMD or BMD and one was assigned an inconclusive phenotype. For the onset index, data were available for 922 eligible cases, with 668 assigned a DMD or BMD phenotype and 254 assigned an inconclusive phenotype.
Table 2.
Selected demographics for MD STARnet case classifications and phenotype assignments
| All Cases |
No phenotype assigned |
DMD |
BMD |
P* | |||||
|---|---|---|---|---|---|---|---|---|---|
| Total | N | % | N | % | N | % | N | % | |
| 987 | 100% | 28 | 100% | 838 | 100% | 121 | 100% | ||
| State | 0.40 | ||||||||
| Arizona | 229 | 23% | 6 | 22% | 199 | 24% | 24 | 20% | |
| Colorado | 214 | 22% | 7 | 25% | 184 | 22% | 23 | 19% | |
| Georgia | 272 | 28% | 3 | 11% | 233 | 28% | 36 | 30% | |
| Hawaii | 23 | 3% | - | – | 22 | 3% | 1 | 1% | |
| Iowa | 124 | 12% | 3 | 11% | 104 | 12% | 17 | 14% | |
| New York | 125 | 12% | 9 | 32% | 96 | 12% | 20 | 17% | |
| Race/Ethnicity | 0.02 | ||||||||
| Non-Hispanic White | 576 | 58% | 18 | 64% | 482 | 58% | 76 | 635 | |
| Hispanic, Any Race | 200 | 20% | 4 | 14% | 182 | 22% | 14† | 12% | |
| Non-Hispanic Black | 68 | 8% | 3 | 10% | 57 | 7% | 8 | 7% | |
| Other | 61 | 6% | 1 | 4% | 54 | 6% | 6 | 5% | |
| Unknown | 82 | 8% | 2 | 8% | 63 | 8% | 17† | 14% | |
| MD STARnet Classification | 0.01 | ||||||||
| Definite | 820 | 83% | 26 | 93% | 693 | 83% | 101 | 83% | |
| Probable | 65 | 7% | 2 | 7% | 57 | 7% | 6 | 5% | |
| Possible | 94 | 10% | - | – | 84 | 10% | 10 | 8% | |
| Asymptomatic | 8 | 1% | - | – | 4 | 0% | 4† | 3% | |
| Level of Certainty | 0.01 | ||||||||
| High (3 variables) | 248 | 25% | - | – | 232 | 28% | 16 | 13% | |
| Med (2 variables) | 446 | 45% | - | – | 402 | 48% | 44 | 37% | |
| Low (1 variable) | 265 | 27% | - | – | 204 | 24% | 61† | 50% | |
| Molecular Index Variable | |||||||||
| DMD | 589 | 60% | 18 | 65% | 549 | 66% | 22 | 18% | 0.00 |
| BMD | 134 | 13% | 8 | 28% | 55 | 7% | 71† | 59% | |
| Inconclusive | 1 | 0% | - | – | 1 | 0% | 0 | 0% | |
| Missing | 263 | 27% | - | – | - | – | - | – | |
| Mobility Index Variable | |||||||||
| DMD | 525 | 53% | 1 | 0% | 524 | 63% | 01 | 0% | 0.37 |
| BMD | 90 | 9% | 18 | 64% | 1 | 0% | 71 | 59% | |
| Inconclusive | 327 | 33% | 8 | 29% | 277 | 33% | 42 | 35% | |
| Missing | 45 | 5% | - | – | - | – | - | ||
| Onset Index Variable | |||||||||
| DMD | 627 | 63% | 22 | 79% | 588 | 70% | 17† | 14% | 0.00 |
| BMD | 41 | 4% | 1 | 3% | 4† | 0% | 36† | 30% | |
| Inconclusive | 254 | 26% | 5 | 18% | 204 | 24% | 45 | 37% | |
| Missing | 65 | 7% | - | – | - | – | - | – | |
MD STARnet: Muscular Dystrophy Surveillance Tracking and Research Network; BMD: Becker muscular dystrophy; DMD: Duchenne muscular dystrophy.
Only predictive and non-predictive for BMD vs DMD were included in chi-square analyses. Non-predictive included wrong phenotype and inconclusive.
Cells contributing to chi-square differences with a standardized residual ≥|2.0|
Figure 3 demonstrates the data availability across all cases for each index variable. An overview of genetic mutations are included in Table 5. 874/1054 (83%) of all cases had some genetic testing performed, but only 662/1054 63% of cases had classifiable genetic mutation data available, 1% of which showed exceptions to the reading frame rule when compared with muscle biopsy data. We had familial DNA results available that were not used in an individual’s phenotype classification. Of the 392 cases who could not be classified using genetics, 55 had classifiable familial DNA. Upon further review, none of those 55 cases would have resulted in a change in the phenotype reported. Eleven cases demonstrated conflicting predictions between western blot and genetics. Classification was deferred to biopsy results in seven cases due to actual phenotype prediction reported by the lab and in two cases due to mutation occurring in a well-known reversal hotspot. The last two cases were deferred to genetics, as there was conflicting data in the biopsy report.
Table 5.
Final phenotype case classification by specific known predictive mutation locations and general mutation effect information
| Reading Frame Effect and Mutation Type | Affected Exon(s) | Phenotype Prediction | N | Actual Mutation | MD STARnet Phenotype |
Reference | ||
|---|---|---|---|---|---|---|---|---|
| DMD | BMD | NC | ||||||
| Frameshift | ||||||||
| Deletion | <8 | BMD | 6 | Multiexon | 100% | 0% | 0% | [2, 5, 6, 56] |
| Deletion | 3–7 | Variable | 13 | 3–7 | 69% | 31% | 0% | [43] |
| Duplication | 2 | DMD Only | 8 | 2 | 88% | 0% | 12% | [5] |
| Deletion/Duplication | Flanking 44 | BMD | 85 | Single Exon | 84% | 4% | 12% | [41, 42, 56] |
| Multiexon | 88% | 8% | 3% | |||||
| Deletion | 52 | DMD | 9 | 52 | 100% | 0% | 0% | |
| Remaining Deletions/ | All other | DMD | 59 | Single Exon | 93% | 2% | 5% | |
| Duplications | 237 | Multiexon | 97% | 0% | 3% | |||
| In-Frame | ||||||||
| Deletion/Duplication | Inclusive of | DMD | 9 | Multiexon | 100% | 0% | 0% | [56] |
| exons 64–70 | ||||||||
| or exons | ||||||||
| 2–10 & 32–45 | ||||||||
| Deletion | <11 | BMD | Single Exon | |||||
| 1 | 3 | 100% | 0% | 0% | [56] | |||
| Multiexon | ||||||||
| 2 | 2–7 | 0% | 100% | 0% | ||||
| 4 | 3–4 | 0% | 100% | 0% | ||||
| 1 | 3–5 | 100% | 0% | 0% | ||||
| 1 | 3–8 | 0% | 100% | 0% | ||||
| Deletion | 45–55 | BMD | 5 | 45–55 | 0% | 80% | 20% | [56] |
| Deletion | 45–47 | BMD | 16 | 45–47 | 0% | 100% | 0% | [58] |
| Deletion | 48 | BMD | 1 | 48 | 0% | 100% | 0% | |
| Deletion | 10–40 | BMD | 1 | 10–42 | 100% | 0% | 0% | [56] |
| Remaining Deletions/ | All other | BMD | 3 | 42; 47; 64 | 100% | 0% | 0% | |
| Duplications | 13 | 3–13; 3–20; 3–30; | 100% | 0% | 0% | |||
| 4–16; 4–48; 10–16; | ||||||||
| 13–44; 20–21; 21–29; | ||||||||
| 30–44; 45–46; 50–51; | ||||||||
| 52–57 | ||||||||
| 2 | 3–15 | 100% | 0% | 0% | ||||
| 2 | 3–24; 56–60 | 0% | 0% | 100% | ||||
| 6 | 3–29; 6–18; 8–21; | 0% | 100% | 0% | ||||
| 38–48; 43–51; 52–55 | ||||||||
| 8–19 | ||||||||
| 3 | 17–44 | 100% | 0% | 0% | ||||
| 2 | 19–20 | 50% | 50% | 0% | ||||
| 3 | 45–48 | 100% | 0% | 0% | ||||
| 15 | 45–49 | 7% | 73% | 20% | ||||
| 9 | 45–53 | 0% | 89% | 11% | ||||
| 7 | 45–55 | 29% | 71% | 0% | ||||
| 2 | 47–51 | 0% | 50% | 50% | ||||
| 2 | 48–51 | 100% | 0% | 0% | ||||
| 5 | 50–55 | 60% | 40% | 0% | ||||
| 4 | 51–52 | 100% | 0% | 0% | ||||
| 4 | 52–53 | 75% | 0% | 25% | ||||
| 2 | 100% | 0% | 0% | |||||
| All Other mutations in database | ||||||||
| Remaining Deletions/ | Includes 1 & 79 | UNK | 5 | Single Exon | 80% | 20% | 0% | |
| Duplications | 9 | Multiexon | 67% | 11% | 22% | |||
| Point Mutations | Any | DMD | 100 | Nonsense | 94% | 3% | 3% | |
| BMD | 5 | Missense | 60% | 20% | 20% | |||
| UNK | 3 | Unknown | 67% | 33% | 0% | |||
| Unknown mutation type & effect | UNK | UNK | 6 | 83% | 0% | 17% | ||
BMD – Becker muscular dystrophy, DMD – Duchenne muscular dystrophy; NC – Not classifiable; UNK – Unknown.
Demographic distributions
DMD and BMD phenotypes showed similar distributions of demographic characteristics across the MD STARnet sites (Table 2). The BMD phenotype was less frequent among Hispanics. Cases with a BMD phenotype were more likely to be missing race/ethnicity information. The BMD phenotype was also more likely to have an asymptomatic MD STARnet classification, to have a phenotype assigned with a low level of certainty, and to have an inconclusive phenotype based on the onset index. Finally, there was a significant difference in the proportion of deceased cases for each group (21% for DMD vs. 5% for BMD, p < 0.01).
Diagnostic accuracy
Diagnostic accuracy was assessed for each phenotype assigned through each index separately (Table 3A). The mobility index had the highest specificity for DMD (99.3%) and the molecular index had the highest sensitivity for DMD (90.7%). The overall accuracy in assigning a phenotype was less than 87% for the indices. The AUCs for distinguishing “DMD” from “not DMD” phenotypes from each index ranged from 0.627 (0.465–0.789) to 0.836 (0.746–0.927).
Table 3A.
Diagnostic accuracy for each index to identify the DMD phenotype determined with the MD STARnet algorithm.
| Index† | MD STARnet Phenotype‡ |
Sensitivity | Specificity | AUC | Standard Error | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| DMD | Not DMD | (95%CI) | (95%CI) | PPV | NPV | Accuracy | (95%CI) | |||
| Mobility | DMD Not DMD |
524 276 |
1 139 |
65.5% (62.09−68.79) |
99.3% (96.08−99.98) |
99.8% | 33.5% | 70.5% | 0.836 (0.746–0.927) |
4.6% |
| Onset | DMD Not DMD |
588 208 |
39 87 |
73.9% (70.67−76.98) |
69.0% (60.20−76.98) |
93.8% | 29.5% | 73.2% | 0.627 (0.465−0.789) |
8.3% |
| Molecular | DMD Not DMD |
549 56 |
40 79 |
90.7% (88.31−93.07) |
66.4% (57.15−74.78) |
93.2% | 58.5% | 86.7% | 0.786 (0.733−0.838) |
2.7% |
MD STARnet: Muscular Dystrophy Surveillance Tracking and Research Network; DMD: Duchenne muscular dystrophy; BMD: Becker muscular dystrophy; CI: confidence interval; PPV: positive predictive value; NPV: negative predictive value; AUC: area under the curve.
Case classifications for DMD are included for each index. Not DMD represents all cases assigned as BMD or Inconclusive by index variables. Not all cases have all indices available.
Not DMD represents all phenotypes assigned as BMD or not assigned to any phenotype.
For the BMD phenotype (Table 3B), the onset index had the highest specificity (99.4%), and the molecular index had the highest sensitivity (76.3%). The overall accuracy across all indices ranged from 88.3% to 93.5%, and the AUCs ranged from 0.669 (0.591–0.748) to 0.832 (0.779–0.884).
Table 3B.
Diagnostic accuracy for each index to identify the BMD phenotype determined with the MD STARnet algorithm
| MD STARnet phenotype‡ |
Sensitivity | Specificity | AUC | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Index† | BMD | Not BMD | (95%CI) | (95%CI) | PPV | NPV | Accuracy | (95%CI) | Standard Error | |
| Mobility | BMD | 71 | 19 | 62.8% | 97.7% | 78.9% | 95.1% | 93.5% | 0.777 | 3.7% |
| Not BMD | 42 | 808 | (53.24–71.74) | (96.44–98.61) | (0.805–0.848) | |||||
| Onset | BMD | 36 | 5 | 36.7% | 99.4% | 87.8% | 93.0% | 92.7% | 0.669 | 4.0% |
| Not BMD | 62 | 819 | (27.22–47.07) | (98.59–99.80) | (0.591–0.748) | |||||
| Molecular | BMD | 71 | 63 | 76.3% | 90.0% | 53.0% | 96.3% | 88.3% | 0.832 | 2.7% |
| Not BMD | 22 | 568 | (66.40–84.54) | (87.39–92.23) | (0.779–0.884) | |||||
MD STARnet: Muscular Dystrophy Surveillance Tracking and Research Network; BMD: Becker muscular dystrophy; DMD: Duchenne muscular dystrophy; CI: confidence interval; PPV: positive predictive value; NPV: negative predictive value; AUC: area under the curve.
Case classifications for BMD are included for each index variable. Not BMD represents all cases assigned as DMD or Inconclusive by index variables. Not all cases have all indices available.
Not BMD represents all phenotypes assigned as DMD or not assigned to any phenotype.
Phenotype classifications
Table 4 shows how MD STARnet cases would be classified using the criteria described in studies from the literature. Using a combination of available data and multiple variables, we were able to classify 92% (n = 959) of all cases. Seventy percent (n = 694) of the cases had at least two variables. In contrast, we were able to classify up to 78% of cases using criteria from the King et al. (2007) study that combined mutation data and age at loss of ambulation. Studies that restricted classification to age at loss of ambulation enabled classification of 48% to 66% of cases. Reports using results from the western blot test on muscle tissue and genetic testing yielded 13% and 63%, respectively. No studies used age of onset alone to classify individuals as having DMD or BMD.
Table 4.
Applying various diagnostic criteria in the literature to the MD STARnet population of 1041 eligible participants
| Article | Criteria† | BMD | DMD | Intermediate | Unclassified |
|---|---|---|---|---|---|
| MD STARnet | BMD: Loss of ambulation≥16 years OR | 121 | 838 | NA | 82 |
| In-frame mutation OR | |||||
| Decreased (≥20%) dystrophin WB OR | |||||
| Onset of symptoms≥10 years OR | |||||
| Multiple concordant combination of the above | |||||
| DMD: Loss of ambulation <12 years (<16 years with ≥24 months continuous steroid use before loss of ambulation or 12years) OR | |||||
| Out-of-frame mutation OR | |||||
| Absent (<5%) dystrophin WB OR | |||||
| Onset of symptoms <5 years OR | |||||
| Multiple concordant combination of the above | |||||
| Ambulation only | |||||
| Tuffery-Giraud et al. 2009 | BMD: Loss of ambulation >16 years | 73 | 484 | 99 | 385 |
| Humbertclaude et al. 2012 | DMD: Loss of ambulation <13 years | ||||
| Elhawary et al. 2004[5, 6, 26] | IMD: Loss of ambulation ≥13 years≤16 years | ||||
| Humbertclaude et al. 2013 [7] | BMD: Loss of ambulation >16 years | 73 | 333 | 250 | 385 |
| DMD: Loss of ambulation <11 years | |||||
| IMD: Loss of ambulation ≥11 years ≥ 16 years | |||||
| Juan Mateu et al. 2013, 2015 | Clinical presentation, age at onset (not defined) | 154 | 534 | NA | 353 |
| [27, 28] | |||||
| BMD: Loss of ambulation >13 years | |||||
| DMD: Loss of ambulation≤13 years | |||||
| Dastur et al. 2008 [29] | BMD: Loss of ambulation ≤ 16 years | 89 | 484 | NA | 468 |
| DMD: Loss of ambulation <13 years | |||||
| Bushby et al. 1993 [51] | BMD: Loss of ambulation >16 years | 73 | 423 | NA | 545 |
| DMD: Loss of ambulation < 12 years | |||||
| Molecular only | |||||
| Anthony et al. 2011 | BMD: In-Frame mutation | 131 | 523 | NA | 387 |
| Gangopadhyay et al. 1992 | DMD: Out-of-Frame mutation | ||||
| Straathof et al. 2009‡ | |||||
| Bello 2012‡ [3, 24, 33, 47] | |||||
| Desguerre et al. 2009 | BMD: Deficiency of dystrophin,IHC or WB | ||||
| Magri et al. 2011 | DMD: Absence of dystrophin,IHC or WB | 20 | 118 | NA | 903 |
| Houde et al. 2008 | |||||
| Barp et al. 2015 [12, 20, 45, | |||||
| 52] | |||||
| Ricotti et al. 2013 [23] | DMD: Out-of-frame mutation OR | NA | 589 | NA | 452 |
| Absence (<5%) of dystrophin IHC | |||||
| Hoffman et al. 1989 | BMD: Dystrophin quantity >3% | 40 | 107 | 0 | 894 |
| Carsana et al. 2005 [53, 54] | DMD: Absence of dystrophin on muscle biospy | ||||
| Multiple | |||||
| Biggar et al. 2006 | DMD: Symptom onset <5 years AND | NA | 378 | NA | 663 |
| Balaban et al. 2005 [17, 19] | Muscle biopsy OR DNA mutation‡ | ||||
| King et al. 2007 [21] | DMD: Out-of-frame mutation OR | NA | 814 | NA | 227 |
| Loss of ambulation≤15 years | |||||
| McDonald et al. 2013 [55] | DMD: Symptom onset <9y AND | NA | 74 | NA | 967 |
| Nonsense mutations AND | |||||
| Ambulatory >=5y w ith no steroids or minimum 6 | |||||
| months stable steroid use |
MD STARnet: Muscular Dystrophy Surveillance Tracking and Research Network; BMD: Becker muscular dystrophy; DMD: Duchenne musculardystrophy;IMD:intermediatemusculardystrophyIHC:immunohistochemistry;WB:westernblot.
BMDalsoincludeindividuals still ambulating beyond cut off age.
Assumption that original criteria of reading frame rule and dystrophin absence used when “confirmed DMD” listed.
DISCUSSION
Determining phenotypes for individuals diagnosed with a dystrophinopathy is important in both clinical and research settings. Clinically, phenotype assignment can assist clinicians in providing anticipatory guidance and estimating timing of therapeutic interventions. In research, examining data by phenotype is key to describing the clinical course of disease, evaluating the success of existing interventions in minimizing disease impact, and assessing the potential for new interventions. In this study, we conducted a multivariable analysis of common clinical indicators of disease severity to assess their validity for distinguishing among dystrophinopathy phenotypes. Using empirically derived indices, we independently classified each case as consistent with a DMD or BMD phenotype. Inconclusive phenotype assignments were a minority. Finally, we assessed the diagnostic accuracy of these assignments by calculating sensitivity, specificity, and diagnostic accuracy for these indices.
Age at loss of ambulation is arguably the most reliable symptom of disease progression for distinguishing DMD from BMD among those diagnosed with a dystrophinopathy. A large proportion of retrospective studies use loss of ambulation as the sole phenotype classification criterion [5, 6, 21, 25–30]. However, the predictive value of this symptom is imperfect, due in part to prolonged ambulation among steroid users [16–22]. Exceptions to the rule do exist and numerous studies identify an intermediate phenotype often qualified as severe Becker or mild Duchenne. This nomenclature captures those individuals who continue to ambulate independently beyond the DMD upper-bound age, but cease ambulation before the BMD lower-bound age [5, 26–28, 31–33]. Given the variability in reported age at ceased ambulation for both DMD and BMD [2, 5–7, 9, 12, 16–24], our algorithm for assigning phenotypes took into account both the age at which independent ambulation ceased and the duration of steroid use, where appropriate. In our study, the mobility index was poor at ruling in both phenotypes (low sensitivity) but performed well at ruling them out (high specificity), whereas diagnostic accuracy for DMD was 70.5% and for BMD was 93.5%.
The emergence of molecular testing, which includes DNA testing and muscle biopsy, has become standard practice in the diagnostic process. Phenotypic assignments from DNA test results are based on interpretations of the effect of the mutation on the translational reading frame, which affects quality and length of the dystrophin protein created [3]. The majority of genetic mutations (92%–96%) follow the “reading frame rule” proposed by Monaco et al (1988) [34]. As with ambulation status, there are exceptions to the reading-frame rule in predicting phenotype. Many of the mutations occurring at the 5’ end of the gene that predict a frameshift mutation have been confirmed to produce a phenotype exception (i.e., BMD phenotype) [27, 29, 32, 33, 35–39]. Additionally, mutations at the 3’ end of the gene are thought to rescue the DMD phenotype if the N-terminus and C-terminus functionality is maintained [35, 36]. Several frameshift reversal hotspots have also been identified in the literature [2, 5, 6, 8, 40–43], and modifier genes have been reported that can alter phenotype presentation [44–47]. In addition to the above exceptions, approximately 5–7% of all cases will not have a mutation that is detectable under the genetic testing technology standards used during the eras reported in this dataset. This variability in mutation prediction supports our proposal of using additional molecular tests to predict phenotype and review of discrepancies in genetic results for individual cases [48, 49]. Muscle biopsies are invasive, no longer considered a first-line diagnostic test in DMD and BMD, and dependent on the pathologist’s skill and experience for valid interpretation but were more frequently performed during the eras reported in this dataset [2, 3, 12]. Overall, phenotype assignments from our molecular (combining genetic and western blot) index showed contrasting results for assigning the BMD and DMD phenotypes. The index was good at ruling in but poor at ruling out the DMD phenotype, whereas the opposite was found for predicting the BMD phenotype.
Lastly, the age at onset of symptoms is used clinically to predict phenotypic severity [2, 9, 12, 17]. The symptom onset age has limitations as it is often subject to parent recall and can be affected by previous knowledge of family history wherein parents may either notice symptoms sooner or have their child evaluated earlier. Symptoms typically related to ambulation limitations (trouble running, abnormal gait, trouble with stairs), signs such as muscle weakness that is apparent on rising/standing (Gowers maneuver), and other general signs (calf hypertrophy, proximal muscle weakness, loss of skills, lordosis) were used for the index. Determining age at onset depends on the thoroughness of provider documentation of early history and symptom onset and thus is more susceptible to bias than prospectively documented age at loss of ambulation [2, 9, 12, 17]. The onset index performed poorly for ruling in and ruling out DMD. For BMD, the onset index performed well for ruling out BMD but poorly for ruling in the phenotype.
The challenge of classifying individuals into distinct DMD and BMD phenotypes results from the documented variability in presentation even after diagnostic test results (DNA and muscle biopsy) [2, 5–7, 9, 12, 16–24]. Overall, the diagnostic accuracy for determining a phenotype using a single clinical measure is reduced with some exceptions. For example, the determination of clinical trial eligibility can utilize DNA evidence of frameshift mutations or quantification of dystrophin in muscle biopsy to include DMD cases and exclude BMD cases. Genetic mutation data acquired using current standards would be greater than 90% effective in identifying phenotype, as intronic breakpoints, double mutations, alternative splice sites, and modifier genes continue to be identified that contribute to phenotype rescue [26–28, 32, 35, 45, 46, 50]. By incorporating additional clinical criteria, it may be possible to maximize the selection of patients with ‘true’ DMD. In retrospective studies, age at loss of independent ambulation in conjunction with quantification of steroid use is effective for ruling out both DMD and BMD based on the cutoffs used in this study and could provide added value to phenotype classification.
Strengths of this study include a comprehensive population-based surveillance system and availability of longitudinal data collection, allowing the use of clinical data across multiple stages of disease progression. Multiple levels of review were conducted to increase the reliability of the multivariable phenotype assignments based on multiple clinical endpoints, a large number of available cases, and expert clinical review. Limitations of this approach include the use of data collected from medical records, which may not contain complete data, since documentation is not standardized across providers as it would be in a prospective trial. There is also the potential for recall bias by parents when reporting the timing of symptom onset as their child ages. Our data span multiple decades of genetic testing and we do not have sufficient data to demonstrate the validity of the testing performed across all cases. We also intentionally avoided the use of an IMD classification as this variable was intended to provide us with the required data to respond to reviewers regarding BMD vs DMD in manuscripts as opposed to a spectrum.
CONCLUSION
Our study demonstrates the feasibility of distinguishing among dystrophinopathy phenotypes by using three empirically defined indices amid variability in clinical presentation. When the phenotypes assigned according to each of the three indices–mobility status, molecular test results, and onset of symptoms–are concordant, confidence in the phenotype assignment is higher. This approach could be used in clinical trials and other research where distinguishing between dystrophinopathy phenotypes is paramount, and may provide additional clinical information for disease management.
ACKNOWLEDGMENTS INCLUDING SOURCES OF SUPPORT
This publication was supported by the grant numbers, DD000830, DD000831, DD000832, DD000834, DD000835, DD000836, DD000837 funded by the Centers for Disease Control and Prevention. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the Centers for Diseases Control and Prevention or the Department of Health and Human Services. Research was performed in compliance with guidelines on human subjects research either through local Institutional Review Board approvals or exemptions as public health related activities.
Footnotes
The findings and conclusions in this report are those of the author(s) and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
CONFLICT OF INTEREST
The authors have no conflicts of interest to report
REFERENCES
- [1].Dubowitz V The Muscular Dystrophies. In: Dubowitz V, editor. Muscle Disorders in Childhood 2nd ed. Philadelphia: W.B. Suanders Company, Ltd; 1995, pp. 34–133. [Google Scholar]
- [2].Flanigan KM. Duchenne and becker muscular dystrophies. Neurol Clin [Internet] 2014;32(3):671–88. doi: 10.1016/j.ncl.2014.05.002 . Available from: 10.1016/j.ncl.2014.05.002 10.1016/j.ncl.2014.05.002. Available from: http://dx.doi.org/10.1016/j.ncl.2014.05.002 [DOI] [PubMed] [Google Scholar]
- [3].Anthony K, Cirak S, Torelli S, Tasca G, Feng L, Arechavala-Gomeza V, et al. Dystrophin quantification and clinical correlations in Becker muscular dystrophy: Implications for clinical trials. Brain 2011;134(12):3544–56. 10.1093/brain/awr291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Santos R, Gonc¸alves A, Oliveira J. New variants, challenges and pitfalls in DMD genotyping: Implications in diagnosis, prognosis and therapy. J Hum Genet 2014;1–11. 10.1038/jhg.2014.54 [DOI] [PubMed]
- [5].Tuffery-Giraud S, Be´roud C, Leturcq F, Yaou R Ben, Hamroun D, Michel-Calemard L, et al. Genotype-phenotype analysis in 2,405 patients with a dystrophinopathy using the UMD-DMD database: A model of nation-wide knowledgebase. Hum Mutat 2009;30(6):934–45. 10.1002/humu.20976 [DOI] [PubMed] [Google Scholar]
- [6].Humbertclaude V, Hamroun D, Bezzou K, Be´rard C, Boespflug-Tanguy O, Bommelaer C, et al. Motor and respiratory heterogeneity in Duchenne patients: Implication for clinical trials. Eur J Paediatr Neurol 2012;16(2):149–60. 10.1016/j.ejpn.2011.07.001 [DOI] [PubMed] [Google Scholar]
- [7].Humbertclaude V, Hamroun D, Picot M-C, Bezzou K, Be´rard C, Boespflug-Tanguy O, et al. Phenotypic heterogeneity and phenotype-genotype correlations in dystrophinopathies: Contribution of genetic and clinical databases. Rev Neurol (Paris) 2013;169(8–9):583–94. 10.1016/j.neurol.2013.04.004 [DOI] [PubMed] [Google Scholar]
- [8].Aartsma-Rus A, Van Deutekom JCT, Fokkema IF, Van Ommen GJB, Den Dunnen JT. Entries in the Leiden Duchenne muscular dystrophy mutation database: An overview of mutation types and paradoxical cases that confirm the reading-frame rule. Muscle and Nerve 2006/06/14. 2006;34(2):135–44. 10.1002/mus.20586 [DOI] [PubMed] [Google Scholar]
- [9].Desguerre I, Christov C, Mayer M, Zeller R, Becane H-M, Bastuji-Garin S, et al. Clinical heterogeneity of duchenne muscular dystrophy (DMD): Definition of sub-phenotypes and predictive criteria by long-term follow-up. PLoS One 2009;4(2):e4347 10.1371/journal.pone.0004347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Miller LA, Romitti PA, Cunniff C, Druschel C, Mathews KD, Meaney FJ, et al. The muscular dystrophy surveillance tracking and research network (MD STARnet): Surveillance methodology. Birth Defects Res Part A - Clin Mol Teratol 2006;76(11):793–7. 10.1002/bdra.20279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Mathews KD, Cunniff C, Kantamneni JR, Ciafaloni E, Miller T, Matthews D, et al. Muscular dystrophy surveillance tracking and research network (MD STARnet): Case definition in surveillance for childhood-onset Duchenne/Becker muscular dystrophy. J Child Neurol 2010;25(9):1098–102. 10.1177/0883073810371001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Magri F, Govoni A, D’Angelo MG, Del Bo R, Ghezzi S, Sandra G, et al. Genotype and phenotype characterization in a large dystrophinopathic cohort with extended follow-up. J Neurol 2011;258(9):1610–23. 10.1007/s00415-011-5979 [DOI] [PubMed] [Google Scholar]
- [13]. UMD-DMD France. The DMD mutations database.
- [14]. EDystrophin. eDystrophin.
- [15].den Dunnen JT. DMD exonic deletions/duplications reading-frame checker 1.9 and sequence variant database. Leiden Muscular Dystrophy pages
- [16].Emery A, Skinner R. Clinical studies in benign (Becker type) X-linked muscular dystrophy. Clin Genet 1976;10:189–201. [DOI] [PubMed] [Google Scholar]
- [17].Biggar WD, Harris VA, Eliasoph L, Alman B. Long-term benefits of deflazacort treatment for boys with Duchenne muscular dystrophy in their second decade. Neuromuscul Disord 2006;16:249–55. 10.1016/j.nmd.2006.01.010 [DOI] [PubMed] [Google Scholar]
- [18].Angelini C, Pegoraro E, Turella E, Intino MT, Pini A, Costa C. Deflazacort in Duchenne dystrophy: Study of long-term effect. Muscle Nerve 1994;17:386–91. 10.1002/mus.880170405 [DOI] [PubMed] [Google Scholar]
- [19].Balaban B, Matthews DJ, Clayton GH, Carry T. Corticosteroid treatment and functional improvement in duchenne muscular dystrophy. Am J Phys Med Rehabil 2005;84(11):843–50. 10.1097/01.phm.0000184156.98671.d0 [DOI] [PubMed] [Google Scholar]
- [20].Houde S, Filiatrault M, Fournier A, Dube J, D’Arcy S, Be´rube´ D, et al. Deflazacort use in Duchenne muscular dystrophy: An 8-year follow-up. Pediatr Neurol 2008;38(3):200–6. 10.1016/j.pediatrneurol.2007.11.001 [DOI] [PubMed] [Google Scholar]
- [21].King WM, Ruttencutter R, Nagaraja HN, Matkovic V, Landoll J, Hoyle C, et al. Orthopedic outcomes of long-term daily corticosteroid treatment in Duchenne muscular dystrophy. Neurology 2007;68(19):1607–13. 10.1212/01.wnl.0000260974.41514.83 [DOI] [PubMed] [Google Scholar]
- [22].Yilmaz O, Karaduman A, Topalog˘lu H. Prednisolone therapy in Duchenne muscular dystrophy prolongs ambulation and prevents scoliosis. Eur J Neurol 2004;11(8):541–4. 10.1111/j.1468-1331.2004.00866.x [DOI] [PubMed] [Google Scholar]
- [23].Ricotti V, Ridout DA, Scott E, Quinlivan R, Robb SA, Manzur AY, et al. Long-term benefits and adverse effects of intermittent versus daily glucocorticoids in boys with Duchenne muscular dystrophy. J Neurol Neurosurg Psychiatry 2013;84(6):698–705. 10.1136/jnnp-2012-303902 [DOI] [PubMed] [Google Scholar]
- [24].Straathof CSM, Overweg-Plandsoen WCGT, van den Burg GJ, van der Kooi AJ, Verschuuren JJGM, de Groot IJM. Prednisone 10 days on/10 days off in patients with Duchenne muscular dystrophy. J Neurol 2009;256(5):768–73. 10.1007/s00415-009-5012-y [DOI] [PubMed] [Google Scholar]
- [25].Humbertclaude V, Hamroun D, Picot MC, Bezzou K, Be´rard C, Boespflug-Tanguy O, et al. Variabilite´ phe´notypique et corre´lations ge´notype-phe´notype des dystrophinopathies: Contribution des banques de donne´es. Rev Neurol (Paris) 2013;169(8–9):583–94. 10.1016/j.neurol.2013.04.004 [DOI] [PubMed] [Google Scholar]
- [26].Elhawary NA, Nasser AE, Shawky RM, Hashem N. Frameshift deletion mechanisms in Egyptian Duchenne and Becker muscular dystrophy families. Mol Cells 2004;18(2):141–9. [PubMed] [Google Scholar]
- [27].Juan-Mateu J, Gonza´lez-Quereda L, Rodr´ıguez MJ, Verdura E, La´zaro K, Jou C, et al. Interplay between DMD point mutations and splicing signals in dystrophinopathy phenotypes. PLoS One 2013;8(3). 10.1371/journal.pone.0059916 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Juan-Mateu J, Gonzalez-Quereda L, Rodriguez MJ, Baena M, Verdura E, Nascimento A, et al. DMD mutations in 576 dystrophinopathy families: A step forward in genotype- phenotype correlations. PLoS One 2015;10(8):1–21. 10.1371/journal.pone.0135189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Dastur R, Gaitonde P, Khadilkar S, Nadkarni J, Khadikar S, Nadkarni J. Becker muscular dystrophy in Indian patients: Analysis of dystrophin gene deletion patterns. Neurol India 2008;56(3):374 doi: GALE: A350308622 [DOI] [PubMed] [Google Scholar]
- [30].Bushby K The clinical, genetic, and dystophin characteristics of Becker MD. I Natural history. J Neurol 1993;240(2):98–104. [DOI] [PubMed] [Google Scholar]
- [31].Nicolas A, Raguenes-Nicol C, Yaou R Ben, Hir SA Le, Cheron A, Veronique V, et al. Becker muscular dystrophy severity is linked to the structure of dystrophin. Hum Mol Genet 2015;24(5):1267–79. 10.1093/hmg/ddu537 [DOI] [PubMed] [Google Scholar]
- [32].Gualandi F, Rimessi P, Trabanelli C, Spitali P, Neri M, Patarnello T, et al. Intronic breakpoint definition and transcription analysis in DMD/BMD patients with deletion/duplication at the 5??? mutation hot spot of the dystrophin gene. Gene 2006;370(1–2):26–33. 10.1016/j.gene.2005.11.002 [DOI] [PubMed] [Google Scholar]
- [33].Gangopadhyay SB, Sherratt TG, Heckmatt JZ, Dubowitz V, Miller G, Shokeir M, et al. Dystrophin in frameshift deletion patients with Becker muscular dystrophy. Am J Hum Genet 1992;51(3):562–70. [PMC free article] [PubMed] [Google Scholar]
- [34].Monaco AP, Bertelson CJ, Liechti-Gallati S, Moser H, Kunkel LM. An explanation for the phenotypic differences between patients bearing partial deletions of the DMD locus. Genomics 1988;2(1):90–5. 10.1016/0888-7543(88)90113-9 [DOI] [PubMed] [Google Scholar]
- [35].Ferlini A, Neri M, Gualandi F. The medical genetics of dystrophinopathies: Molecular genetic diagnosis and its impact on clinical practice. Neuromuscul Disord 2013;23(1):4–14. 10.1016/j.nmd.2012.09.002 [DOI] [PubMed] [Google Scholar]
- [36].Muntoni F, Torelli S, Ferlini A. Dystrophin and mutations: One gene, several proteins, multiple phenotypes. Lancet Neurol 2003;2(12):731–40. 10.1016/S1474-4422(03)00585-4 [DOI] [PubMed] [Google Scholar]
- [37].Sironi M, Pozzoli U, Cagliani R, Comi GP, Bardoni A, Bresolin N. Analysis of splicing parameters in the dystrophin gene: Relevance for physiological and pathogenetic splicing mechanisms. Hum Genet 2001;109(1):73–84. 10.1007/s004390100547 [DOI] [PubMed] [Google Scholar]
- [38].Magri F, Del Bo R, D’Angelo MG, Govoni A, Ghezzi S, Gandossini S, et al. Clinical and molecular characterization of a cohort of patients with novel nucleotide alterations of the Dystrophin gene detected by direct sequencing. BMC Med Genet 2011;12(1):37 10.1186/1471-2350-12-37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Beggs a H, Hoffman EP, Snyder JR, Arahata K, Specht L, Shapiro F, et al. Exploring the molecular basis for variability among patients with Becker muscular dystrophy: Dystrophin gene and protein studies. Am J Hum Genet 1991;49:54–67. [PMC free article] [PubMed] [Google Scholar]
- [40].van den Bergen JC, Wokke BH, Janson AA, van Duinen SG, Hulsker MA, Ginjaar HB, et al. Dystrophin levels and clinical severity in Becker muscular dystrophy patients. J Neurol Neurosurg Psychiatry [Internet] 2013/12/03. 2014;85(7):747–53. doi: 10.1136/jnnp-2013-306350 . Available from: 10.1136/jnnp-2013-306350http://jnnp.bmj.com/cgi/doi/10.1136/jnnp-2013-306350. Available from: http://jnnp.bmj.com/cgi/doi/10.1136/jnnp-2013-306350 [DOI] [PubMed] [Google Scholar]
- [41].Pane M, Mazzone ES, Sivo S, Sormani MP, Messina S, D’Amico A, et al. Long term natural history data in ambulant boys with Duchenne muscular dystrophy: 36-month changes. PLoS One [Internet] 2014/10/02. 2014;9(10):e108205 doi: 10.1371/journal.pone.0108205 . Available from: 10.1371/journal.pone.0108205http://www.embase.com/search/results?subaction=viewrecord&from=export&id=L600087044. Available from: http://www.embase.com/search/results?subaction=viewrecord&from=export&id=L600087044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Bello L, Morgenroth LP, Gordish-Dressman H, Hoffman EP, McDonald CM, Cirak S. DMD genotypes and loss of ambulation in the CINRG Duchenne Natural History Study. Neurology 2016;87(4):401–9. 10.1212/WNL.0000000000002891 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Winnard a V, Mendell JR, Prior TW, Florence J, Burghes AH. Frameshift deletions of exons 3–7 and revertant fibers in Duchenne muscular dystrophy: Mechanisms of dystrophin production. Am J Hum Genet 1995;56(1):158–66. [PMC free article] [PubMed] [Google Scholar]
- [44].Vo AH, Mcnally EM. Modifier genes and their effect on Duchenne muscular dystrophy. Curr Opin Neurol 2015;28(5):528–34. 10.1097/WCO.0000000000000240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Barp A, Bello L, Politano L, Melacini P, Calore C, Polo A, et al. Genetic modifiers of duchenne muscular dystrophy and dilated cardiomyopathy. PLoS One 2015;10(10):1–14. 10.1371/journal.pone.0141240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Barnard A, Romero de Mello Sa S, Willcocks R, Senesac C, Finkel R, Forbes S, et al. Genetic polymorphisms modify intramuscular fat infiltration in Duchenne muscular dystrophy. Neuromuscul Disord [Internet] 2015;25(2015):S254–5. doi: 10.1016/j.nmd.2015.06.252 . Available from: 10.1016/j.nmd.2015.06.252http://linkinghub.elsevier.com/retrieve/pii/S0960896615004332. Available from: http://linkinghub.elsevier.com/retrieve/pii/S0960896615004332 [DOI] [Google Scholar]
- [47].Bello L, Piva L, Barp A, Taglia A, Picillo E, Vasco G, et al. Importance of SPP1 genotype as a covariate in clinical trials in Duchenne muscular dystrophy. Neurology 2012;79(2):159–62. 10.1212/WNL.0b013e31825f04ea [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].Dent K, Dunn D, von Niederhausern A, Aoyagu A, Kerr L, Bromberg M, et al. Improved molecular diagnosis of dystrophinopathies in an unselected clinical cohort. Am J Med Genet A 2005;134(3):295–8. [DOI] [PubMed] [Google Scholar]
- [49].National Human Genome Research Institute, National Institutes of Health. Learning About Duchenne Muscular Dystrophy 2013.
- [50].Kesari A, Pirra LN, Bremadesam L, McIntyre O, Gordon E, Dubrovsky AL, et al. Integrated DNA, cDNA, and protein studies in Becker muscular dystrophy show high exception to the reading frame rule. Hum Mutat 2008/03/19. 2008;29(5):728–37. 10.1002/humu.20722 [DOI] [PubMed] [Google Scholar]
- [51].Bushby KMD, Gardner-Medwin D. The clinical, genetic and dystrophin characteristics of Becker muscular dystrophy - I. Natural history. J Neurol 1993;240(2):98–104. 10.1007/BF00858725 [DOI] [PubMed] [Google Scholar]
- [52].Desguerre I, Mayer M, Christov C, Leturcq F, Chelly J, Gherardi RK. Phenotypic heterogeneity of Duchenne myopathy and prognosis criteria. Arch Pediatr 2009/06/23. 2009;16(6):681–3. 10.1016/s0929-693x(09)74110-7 [DOI] [PubMed] [Google Scholar]
- [53].Carsana A, Frisso G, Tremolaterra MR, Lanzillo R, Vitale DF, Santoro L, et al. Analysis of dystrophin gene deletions indicates that the hinge III region of the protein correlates with disease severity. Ann Hum Genet 2005/04/23. 2005;69(Pt 3):253–9. 10.1046/j.1529-8817.2005.00160.x [DOI] [PubMed] [Google Scholar]
- [54].Hoffman EP, Kunkel LM. Dystrophin abnormalities in duchenne/becker muscular dystrophy. Neuron 1989;2:1019–29. [DOI] [PubMed] [Google Scholar]
- [55].Mcdonald CM, Henricson EK, Abresch RT, Florence J, Eagle M, Gappmaier E, et al. The 6-minute walk test and other clinical endpoints in duchenne muscular dystrophy: Reliability, concurrent validity, and minimal clinically important differences from a multicenter study. Muscle and Nerve 2013;48(3):357–68. 10.1002/mus.23905 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [56].Aartsma-Rus A, Ginjaar IB, Bushby K. The importance of genetic diagnosis for Duchenne muscular dystrophy. J Med Genet 2016;53(3):145–51. 10.1136/jmedgenet-2015-103387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [57].Flanigan KM, Dunn DM, Von Niederhausern A, Soltanzadeh P, Howard MT, Sampson JB, et al. Nonsense mutation-associated Becker muscular dystrophy: Interplay between exon definition and splicing regulatory elements within the DMD gene. Hum Mutat 2011;32(3):299–308. 10.1002/humu.21426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [58].van den Bergen JC, Wokke BH, Hulsker MA, Verschuuren JJ, Aartsma-Rus AM, Sewry CA, et al. Studying the role of dystrophin-associated proteins in influencing Becker muscular dystrophy disease severity. Neuromuscul Disord 2015/01/31. 2015;25(6):530 10.1016/j.nmd.2015.04.010 [DOI] [PubMed] [Google Scholar]