Abstract
The phenomenon of homophily first was described in Lazarsfeld and Merton’s classic 1954 friendship analysis as a tendency for friendships to form between those who are alike in some respect. Although theories of decision making address a host of factors that affect the process, the influence of individuals with homophilic ties remains unaccounted for and unexplained. The purpose of this paper is to review theories relevant to decision making and describe what is known about the relationship between homophily and health care decision making. Further, we provide new evidence suggesting the influence of homophily on decision making in results from a randomized, multi-center clinical trial of American men with localized prostate cancer. A diverse sample of 293 men with a new diagnosis of localized prostate cancer reported relevant personal factors influencing the care management decision before randomization to a decision aid or usual care, between 2013 and 2015. Among these personal factors were the level of influence or importance ascribed to various individuals at the time of the treatment decision. One month later, participants reported how prepared they were for decision making. 123 men (42%) reported friends and/or coworkers as information sources, of which 65 (53%) indicated that friends and/or coworkers influenced the care decision. Men who reported friends/coworkers as information sources had significantly higher one-month preparation scores. Our review of decision making theories and practical applicability suggests the influence of homophilic relationships manifests in health care decision making. Faced with a list of options to manage health conditions, decision makers turn to known individuals in their environments, particularly those individuals with whom the decision maker can identify. Clinicians may solicit information from patients about influential others and explain how that support fits into the health decision at hand without dishonoring the importance of the homophilic relationship.
Keywords: Decision theory, social networks, prostate cancer, decision making
INTRODUCTION
Health care providers and researchers have studied health decision making in those at risk for adverse health outcomes and in those with particular diagnoses. Significant, and sometimes unexpected, influence of individuals in the decision maker’s environment has been documented, yet current theories of decision making are inadequate to fully describe, explain or predict this phenomenon. Since the mid-20th century, descriptive decision theory primarily has sought to understand the actions of decision makers through the application of probability theory to the decision-making process. More recent theories of decision making address the influence of individual and contextual factors on the decision-making process, yet the mechanisms by which interpersonal relationships influence health care decision making have not been elucidated.
The sociological phenomenon of homophily, meaning love of the same, underlies the common proverb “birds of a feather flock together.” Homophily first was described in Lazarsfeld and Merton’s classic 1954 analysis of friendship as “a tendency for friendships to form between those who are alike in some respect” (p. 23). The tenets of homophily suggest that higher rates of contact and communication occur between individuals who are similar to each other than between dissimilar individuals. In a seminal review paper, McPherson and colleagues (2001) documented the systematic observation of homophily in studies of group formation beginning in the 1920s. Subsequent studies have described homophily in multiple circumstances such as sales and advertisement, sociology, anthropology and health care.
Improved understanding of the role that homophily may play, mediating the influence of personal contacts on health care decision making, has the potential to inform decision support interventions and expand the theoretical basis for clinical practice. The purpose of this paper is therefore to (a) review existing theories relevant to health decision making; (b) describe what is known about the relationship between homophily and health care decision making; (c) provide new evidence suggesting the influence of homophily on decision making in results from a randomized, multi-center clinical trial of men with localized prostate cancer; and (d) discuss the implications of these findings for patient education and support during health care decision making.
BACKGROUND
The interdisciplinary field of decision science is principally concerned with two questions. First, it seeks to understand how decisions should be made. Second, it seeks to understand how decisions are actually made. Theories that address the question of how decisions should be made typically assume ideal conditions; these theories are known as normative (or prescriptive) decision theories (Yates, 1990). In contrast, theories that address the question of how decisions are actually made are known as descriptive decision theories. Several theories may be used for both normative and descriptive purposes (Kahneman & Tversky, 1979); however, given our focus on treatment decision making in the health care setting, we have limited our discussion of decision theories to those with descriptive purposes.
Classical Decision Theories
Descriptive decision theory can be traced as far back as the 18th century, when the mathematician Daniel Bernoulli published his hypothesis of risk assessment and utility (Busemeyer, 2015). Bernoulli’s hypothesis stated that decision makers evaluate a prospect according to both the risks associated with selecting that prospect and its subjective value (Yates, 1990). Classical decision theory views Bernoulli’s hypothesis as axiomatic (Tversky, 1975) and consequently treats decision making as a rational, analytic process.
Expected Utility Theory (von Neumann & Morgenstern, 1953) is a classical decision theory that posits that when rational decision makers are faced with a choice, they will prefer the option that offers the highest expected utility, which is defined as the value of each outcome weighted by the probability it will occur. The principal critique of this theory has been that individuals often make choices that seem irrational from a purely mathematical standpoint (Kahneman & Tversky, 1979).
Kahneman and Tversky’s (1979) Prospect Theory was an adaptation of Expected Utility Theory that sought to explain irrational decisions. Specifically, in Prospect Theory, the certainty effect states that the response to a loss is more extreme than the response to a gain. According to this theory, the expected utility of each outcome is weighted not by its probability, but by a decision weight based on a normalized scale that excludes impossible events, over-weights low probabilities and under-weights moderate and high probabilities (Tversky & Kahneman, 1981). In 1981, Tversky and Kahneman expanded upon these ideas and described a theory of Behavioral Decision Making that incorporated the potential influence of context into the propositions of Prospect Theory. According to the theorists, the context of a decision—its decision frame-- can mediate a decision maker’s interpretation of the decision and its subsequent outcomes. The decision frame may be influenced by the way in which a decision is portrayed (such as whether each option is described in terms of its potential losses or gains) or by the decision-maker’s personal characteristics and norms.
Yates (1990) further explicated and refined classical decision theory in his seminal text Judgment and Decision Making. In this work, Yates described the importance of coherence to the decision-making process. According to Yates, a coherent likelihood judgment is a human judgment that does not violate the principles of probability theory (p. 118). Yates argued that if a person’s likelihood judgments are incoherent, he or she is likely to make faulty decisions with potentially detrimental consequences. To illustrate this concept, he provided the example of an individual who overestimates the proportion of the population that both has cancer and tests positive for it. The individual in the example has accurate information regarding the proportion of the population that has cancer and the proportion of the population that tests positive for cancer; nevertheless, the individual estimates that the proportion of the population that falls into both categories exceeds the product of the two individual proportions. This is a violation of probability theory, which states that for two independent events A and B, the probability of both A and B occurring is equal to the product of the probabilities of A and B occurring (Pagano & Gauvreau, 2000). An individual who perceives his or her risk for an adverse event to be greater or lower than it is, certainly may make suboptimal decisions based on that perceived risk. However, classical decision theory fails to address the psychological and sociological factors that may contribute to an individual’s incoherent likelihood judgments.
Contemporary Decision Theories
Models of decision making developed later in the 20th century largely account for the influence of personal, psychological and sociological factors on the decision-making process. In these models, concepts such as memory and emotion are viewed as important to decision making; as such, these models offer a tacit acknowledgement of the tendency of individuals to make decisions that may seem irrational from a purely probabilistic perspective.
Janis and Mann’s (1976) Conflict Theory Model of Decision Making is focused on the influence of emotion on decision making and posits that psychological stress imposes limitations on the decision-making process. According to the model, psychological stress during decision making primarily results from the potential for decisions to lead to (a) material and social losses; and (b) the loss of reputation and self-esteem. When faced with psychological stress, the decision maker seeks to cope by resolving the decision as quickly as possible, which may result in errors in decision making. The decision maker is influenced by his or her awareness of the risk associated with making the decision, hope of finding a preferred choice and perception of the amount of time that is available to deliberate.
Building on Janis and Mann’s work, O’Connor developed a measure of decisional conflict (O’Connor, 1995) and then the Ottawa Decision Support Framework (ODSF) (O’Connor et al., 1998). The ODSF has been used widely by health scientists seeking to develop decision aids and other decision support tools (Stacey et al., 2017) and addresses health decisions in which the risks and benefits of each choice are uncertain or sensitive to the decision maker’s values or preferences. According to the ODSF (O’Connor et al., 1998), health decisions are influenced by the patient’s and health care provider’s sociodemographic and clinical characteristics and by the patient’s (a) perception of the decision, including knowledge, expectations, values and decisional conflict; (b) perception of important others, including norms, pressure, support and decision-making role; and (c) resources to make and implement a decision, including personal and external resources. The perception of important others and required resources (e.g., meaningful information) are factors aligned with homophily, notably when important others become reliable, trusted information sources.
In 2006 (Elwyn et al.), and then updated in 2009 (Elwyn et al.), the International Patient Decision Aids Standards (IPDAS) Collaboration put forth criteria for assessing the quality of decision support technologies. High quality decision aids should include some method to help patients personally consider and value key aspects of the decision. Fagerlin et al. (2013) extended this position and described the theoretical foundations upon which value clarification components of decision support should be built. The authors argued that decision making is a process and personal value clarification is relevant to not only the primary decision maker but also to family and providers.
Shortcomings of Existing Theories and Models
Although classical and contemporary theories of decision making address a host of factors that affect the decision-making process, the influence of individuals with homophilic ties remains unaccounted for and unexplained. In the ODSF, the influence of social norms is acknowledged, but social norms may not accurately predict the effect of interpersonal relationships. The ODSF purports that “perceptions of what important others think is the appropriate choice” may influence an individual’s health care decision (O’Connor et al., 1998, p. 270), but does not explore the circumstances under which a personal or social contact is regarded as important to the decision. Likewise, the possession of the personal resources needed to make and implement a decision are identified in the ODSF as a prerequisite to a quality decision. However, the receipt of practical and emotional support from an individual known to the decision maker can be differentiated from the perceived influence of that individual on the decision-making process (Pozzar & Berry, 2017). Health care decisions requiring patients to choose between treatments that have no clear medical evidence for the “best” decision create a scenario in which the patient may rely on known, similar individuals who might make (or have made) a similar decision.
Homophily Origins and Applications
Sociologists Lazarsfeld and Merton (1954) coined the term homophily as “a tendency for friendships to form between those who are alike in some designated respect” (p 23). While studying the friendship process, the investigators distinguished the concept by two mechanisms through which ties among similar people are formed, status and value. Status of selection is forming friendships with those similar to you, or who have similar social influence or social status. Personal linkages are formed based on given characteristics such as age, race, gender and education. Social influence or value homophily happens when individuals modify behaviors to align themselves with behaviors of friends regardless of social status. The authors posited that principle of homophily exists in every type of social network and selection and societal characteristics result in the individual having homogenous social networks.
McPherson et al. (2001), contemporary sociologists, extended earlier work on homophily and discussed evidence of homophily in social networks vis-à-vis demographic variables (one cannot choose) and values variables (one can select). Race/ethnicity was observed as the strongest group affiliation in which homophily was evident. Family networks also were found to be homophilic on most characteristics and strong family bonds were less likely to deteriorate than bonds outside of family. Among the variables reviewed by McPherson and colleagues, occupation networks were one scenario that evidenced homophilic relationships in men, both by structure (in which men were grouped together at the workplace) and nature (the kind of work in which men engaged). Similarity among the members of any homophilic group facilitates information flow, knowledge sharing and understanding. Social networks in which demographic and values variables are shared contain the potential for homophilic relationships, but do not guarantee that degree of affiliation. Contacts within a social network with weak homophilic ties may also provide resource information, however subsequent action may be most influenced by similar others. Homophily takes the nature of the relationships within a social network one step further. McPherson et al. concluded that when demographic similarity suggests shared meaningful knowledge, an expectation would be that individuals associate with similar others for easy, comfortable communication.
Various disciplines have studied and authored extensions of Janis and Mann’s foundational work in difficult decisions. Peer influence and homophilic relationships often have been included as mediating or predictive variables for life choices, ranging from childhood alcohol use (Anderson, Tomlinson, Robinson, & Brown, 2011) to careers (e.g., Gibson & Lawrence, 2010). However, none explains the pivotal decision points and individual behaviors of those facing significant health decisions in adults. Our paper now focuses on health care decision making and blends the sociological, psychological and network influences as we explore the application of homophily.
Homophily in the Health Sciences Literature
Since 2010, researchers have evaluated the extent to which homophilic relationships influence health behavior, with most research focusing on areas of health promotion such as weight management (Meng, 2016; Zhang et al., 2015), vaccination (Llupia, Puig, Mena, Bayas, & Trilla, 2016), HIV risk behaviors (Arnold, Sterrett-Hong, Jonas, & Pollack, 2016; Damacena, Szwarcwald, & de Souza Júnior, 2014; Watson et al., 2014) and smoking (Daw, Margolis, & Verdery, 2015; Flatt, Agimi, & Albert, 2012; Go, Tucker, Green, Pollard, & Kennedy, 2012; Quist, Christensen, Carneiro, Hansen, & Bjorner, 2014). Emerging evidence from these studies suggests that individuals look to similar others when engaging in health behaviors. In a study of HIV risk behaviors among 274 men who have sex with men and transgender women, Arnold and colleagues (2016) determined that participants whose direct social connections had a sexual identity similar to their own were less likely to engage in risky sexual behavior. The authors hypothesized that participants’ contact with similarly-identified peers fostered a healthy sexual identity and provided examples of how to navigate sexual relationships. Likewise, Daw, Margolis, and Verdery (2015) found that in a nationally representative sample of 90,118 American adolescents, siblings engaged in similar health behaviors to a greater extent than friends and classmates. Evidence of the influence of homophilic relationships on the health of older adults was observed by Flatt, Agimi, and Albert (2012), whose study of 118 low-income older adults determined that similarities in health behavior were more pronounced among close social contacts, particularly with regard to smoking and physical inactivity.
Lay health advisor programs for promoting health behaviors in African American (Shelton, Charles, Dunston, Jandorf, & Erwin, 2017) and Latina women (Ayala, Vaz, Earp, Elder, & Cherrington, 2010) are based on an assumption that support, including health information, is best received from an individual from the same ethnic or racial community. The success of such practices suggests the importance of information from individuals with whom a homophilic relationship is established.
Making decisions about health behaviors or treatments for a health condition involves conveyed information, whether actively sought or passively received. Johnson and Meischke’s (1993) Comprehensive Model of Information Seeking (CMIS) was designed to predict health seeking behavior based on antecedent factors (i.e., demographics, experience, needs, beliefs), information carrier factors (i.e., information source, utility of the information) and information seeking behaviors. Information carrier factors can consist of health education websites, discussion/support groups or communication with friends, family and health professionals. Survey researchers have documented health information seeking that has been influenced by Korean mothers’ age and income (Lee & Kim, 2015), US breast cancer survivors’ age, education and race (Han et al., 2010) and attitudinal, normative and control factors in US adults of various cancer diagnoses (Smith-McLallen, Fishbein, & Hornik, 2011). Notably, Smith-McLallen and colleagues reported that the perceived normative pressure of important others predicted seeking information from sources other than the physician. Personal beliefs, experiences and socio-demographic factors were predictive of affecting health-decision making and not all information sources affected health decision making in the same way.
Depending on the type of information one is seeking, technology can provide opportunities to connect with others on a wider range of dimensions. Online support groups allow individuals to know that there are many other people experiencing the same physical and emotional issues. Such social forums also provide space to discuss personal issues, particularly sensitive topics in health care such as private body parts, without any embarrassment (Wang, Walther, Pingree, & Hawkins, 2008). The advent of Internet support groups, whether through social media (e.g., Facebook) or online health communities (e.g., PatientsLikeMe.com), has offered opportunities to investigate information sharing behaviors and relationships with homophily. Nambisan (2011) documented the effect of homophily in moderating information-seeking and promoting perceived empathy among 183 users of online communities sponsored by health institutions serving patients with cancer and diabetes. Using the Perceived Homophily Scale (McCroskey, Richmond, & Daly, 1975), the investigators concluded that homophily is an important variable, interacting with information-seeking to enhance the quality of empathy within an online community and that recommended sponsors of such communities build program features that allow identification of similar others within the user community.
Certainly, not all individuals will embrace electronically-mediated information. Credibility, quality and trustworthiness of the source, individuals’ social connectedness, all influence information seeking behavior, and thus affect decision-making. In Lee & Kim’s 2015 survey, older Korean mothers trusted traditional media sources, whereas younger mothers trusted family, friends and the Internet. Van Stee & Yang (2017) found skepticism of the utility of online cancer information from those of higher socioeconomic status in the Health Information National Trends Survey 4 Cycle 4, suggesting recognition of the range in quality of Internet postings.
The influence of homophilic relationships on patients’ treatment decision making has been described to a lesser extent, yet allusions to similar phenomena are present in the literature. In a seminal grounded theory study of 18 adults with a diagnosis of heart disease, renal failure or cancer, Kelly-Powell (1997) reported that the past experiences of participants’ friends and relatives with a similar condition influenced participants’ attitudes and beliefs about the efficacy of certain treatments. Kelly-Powell determined that personalizing choices represented the core variable that influenced participants’ treatment decisions and wrote that, among other factors, decisions were guided by culture, values, and beliefs “that arose from each individual’s life and his or her relationships with others” (p. 222).
Similarly, several studies of cancer treatment decision making have established that significant or influential others play a role in the decision-making process by both shaping beliefs and providing information. In Berry et al.’s early qualitative work (2003b), that later formed the basis of a decision aid for localized prostate cancer recently diagnosed, men described the importance of hearing from friends and coworkers with whom a homophilic relationship existed both in terms of structure and values. Quotes from participants included “…he’s the type like me, he sees the sex thing as the least of his worries” and “…and that was the first thing my business associate said, at our age, seed implants is what you do” (p. 97). Likewise, in a study of treatment decision making among 21 women with breast cancer, O’Brien and colleagues (2008) found that social networks were important sources of information about treatment options, particularly prior to surgical consultation. The importance of the homophilic relationship as an information source was further illustrated in a study of 1,651 racially and ethnically diverse women with non-metastatic breast cancer, in which less acculturated Latinas placed more importance on friends’ and family members’ opinions than any other racial or ethnic group (Hawley et al., 2009). In a qualitative study of the communication networks of 40 men on a prostate biopsy waiting list, Brown, Oetzel, and Henderson (2016) found that tie strength, medical knowledge, homophily and geographic proximity influenced the extent to which participants disclosed information about their medical condition to social network contacts. Specifically, participants in this study reported quickly developing strong ties with social contacts who were known to have a similar medical condition and sought medical information from social contacts who were either experienced with or knowledgeable about their disease.
In the cancer literature, there is evidence that influential others not only provide information to decision makers, but also may participate in health decisions directly. For example, in a study of 57 women with breast cancer and their husbands, patient participants reported that the involvement of their husbands in the decision-making process was as important to them as that of their physicians (Gilbar & Gilbar, 2009). In a recent population-based survey of women who had decided on a type of breast cancer surgery, the vast majority identified at least two decision support persons who facilitated their deliberations and with whom treatment decisions were discussed (Wallner et al., 2017). The decision support persons were primarily spouses, family members and friends or others, but the investigators did not present data about similarities between these supportive persons and the decision maker.
The explicit role of influential others during the treatment decision-making process has not been fully explicated in the literature. Emerging evidence suggests that the influence of interpersonal relationships on treatment decisions may vary. For instance, in the study of 1,651 women with breast cancer conducted by Hawley and colleagues (2009), participants who had a friend or relative present upon surgical consultation were significantly more likely to receive initial mastectomy than those who did not. In the same study, women who placed a higher value on their spouse’s opinion were less likely to receive initial mastectomy. Conversely, family influences and roles are sometimes unexpected. In a secondary analysis of 60 interviews of patients with bladder cancer conducted as part of an earlier study on bladder cancer treatment decision making (Berry et al., 2015), Pozzar and Berry (2017) found that while men described relying on family for practical and emotional support, it was women that described including family members (assumedly homophilic relationships) in the decision-making process. Variation in the roles of family members perhaps was best described by Shaw, Scott, and Ferrante (2013), who explored the influence of family relationships on the screening, biopsy, and treatment decisions of 64 men with prostate cancer. The authors identified three categories of participants: those who shared decisions with family members, those who opposed the participation of family members in decisions and those who yielded to pressure from family members to make a decision. Importantly, these authors did not examine the role played by social contacts such as friends and coworkers; it may be that men who opposed the influence of family members sought information and support from other sources. Yet, the influence of similar others appears to be significant for a meaningful proportion of decision makers. In a sample of 260 men recently diagnosed with localized prostate cancer (Berry et al., 2006), 80% reported receiving decision-related information from friends and 75% reported that friends had influenced the treatment decision, one way or another. Spouses/partners and other family members were reported as influential and as information sources as well. Finally, a univariate relationship between friends’ stories of prostate cancer experiences was detected as a trending correlate (P=.09) of being prepared for decision making about one month after enrollment in a randomized trial of decision support for men with localized prostate cancer (Berry, Wang, Halpenny, & Hong, 2012).
To date, the majority of studies describing the influence of significant others on cancer treatment decision making have been exploratory in nature. No known study has specifically sought to examine the role of homophilic relationships on cancer treatment decision making, and we do not know what the best outcome might be when exploring the effect of homophily. Nevertheless, findings from the existing literature demonstrate that family members, friends, and other social contacts influence the cancer treatment decision-making process in a variety of ways. In the following exemplar, we provide novel findings from a multi-site randomized trial that highlight the importance of accounting for the potential influence of homophilic relationships on cancer treatment decision making.
EXEMPLAR
We present a secondary analysis of data from a randomized trial that tested a tailored decision aid for men with localized prostate cancer as an exemplar of homophily in health decisions. Details of the multi-site trial have been published elsewhere (Berry et al., 2018). In brief, a diverse sample of men with a new diagnosis of localized prostate cancer were queried prior to randomization as to relevant personal factors influencing the care management decision along with demographics, stage of decision making, disease risk level and information sources. The personal factor list (Berry et al., 2006; Berry et al., 2003b) included items on level of influence or importance ascribed to stories or experiences from friends, coworkers, spouses/partners, other family members and any famous man with prostate cancer. About one month after enrollment, participants reported how prepared they perceived themselves to be for decision making using a validated scale, Preparation for Decision Making (PrepDM) (Bennett et al., 2010).
Of the 293 men with a complete PrepDM score at one month, 123 (42%) reported friends and/or coworkers as information sources, of which 65 (53%) indicated that friends and/or coworkers influenced the care decision (some or a lot). Of the 170 men who did not report friends and/or coworkers as information sources or did not answer the question, 47 (28%) indicated that friends and/or coworkers influenced the care decision. The majority of the sample (88%) had reported a final care decision by one month (Berry et al., 2018).
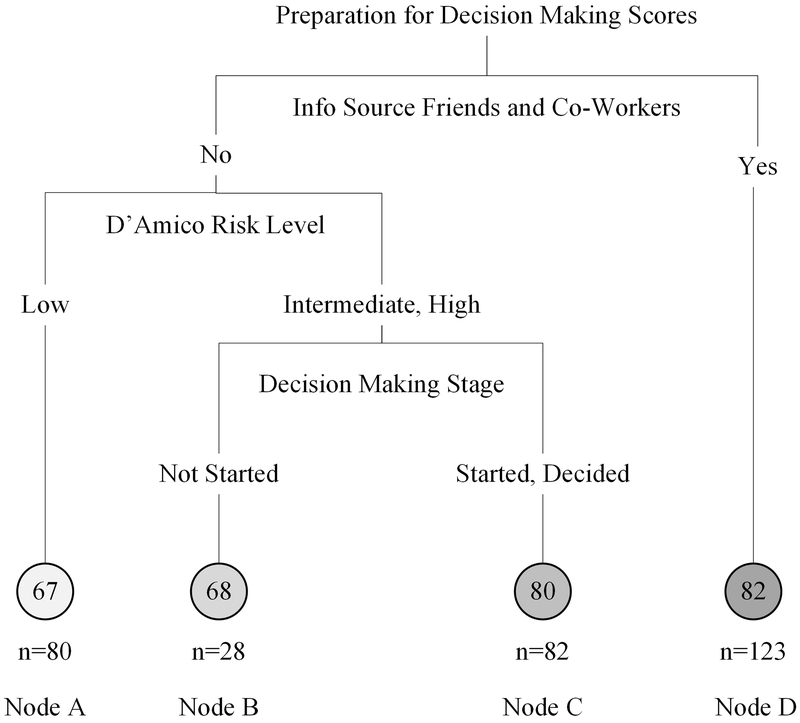
Recursive partitioning was used to build regression trees exploring the most influential factors related to one-month PrepDM total score using the rpart functionality (Therneau, Atkinson, & Ripley, 2017) in R (R Core Team, 2017). The regression tree was built by first identifying the factor that best “splits” the scores of the outcome; the method was applied again to each sub-group recursively until the sample size in a given group was less than 20 men or there was no additional benefit to further dividing the data. In men with a total PrepDM score, and considering baseline demographics, influential factors and information sources, the primary split occurred with whether or not a friend and/or coworker was an information source, followed by the disease risk level. The pruned tree, minimizing the cross-validated error, included friends and/or coworkers as information sources, disease risk level and stage of decision (Figure 1). On average, men who reported friends/coworkers as information sources had higher predicted one-month PrepDM scores (Node D). If friends/coworkers were not reported as information sources, men with low risk disease (Node A) or high/intermediate risk disease prior to the start of the decision-making process (Node B) had lower predicted one-month PrepDM scores. A linear model was then fit with the four groups defined by the end nodes of the pruned regression tree with the group defined by friends/coworkers as an information source (Node D) as the reference level. On average, the PrepDM scores were significantly lower for Nodes A (p<0.001) and B (p<0.001) compared to Node D but not Node C (p=0.40).
Figure 1.
Baseline Predictors for Preparation for Decision Making Scores
DISCUSSION
Classical decision theories have identified processes through which decisions are made but have not addressed the influence of contextual and individual factors in making health care decisions, notably, regarding treatment choices. While contemporary theories take into account the effects of psychological and socioeconomic factors and interpersonal communication in decision making, such theories have overlooked the influence of homophilic relationships in healthcare decision making. The results of this analysis extend the premise of homophily that when faced with a major health care decision, an individual often seeks information from individuals in their social network and that those individuals, and the information shared, play a part in the decision, all resulting in a positive perception of being prepared for the decision at hand. By understanding influencing factors such as income, education and age on health information-seeking behaviors, we are better able to target social networks and improve the trustworthiness and accessibility of information sources.
Our research team also has studied such quantitative variables, documenting in a descriptive study that over half of 260 men with recently diagnosed LPC reported friends as an information source sometimes or always and over half reported some or a lot of influence from friends (Berry et al., 2006). These findings are consistent with Wallner and colleagues’ report (2017) of important and frequent influence of decision-support persons in the networks of women with breast cancer. Taken together, these results may explain some of the relationships proposed in classical and contemporary decision theories. For example, a decision maker’s use of decision frames as described by Tversky and Kahneman (1981) in the context of prospect theory may be influenced in part by homophilic relationships. It may be that when decision makers solicit information from, and are influenced by, the perspectives of similar others, they frame health care decisions not only in terms of each option’s potential medical risks and benefits, but also in terms of the value ascribed to each potential option and outcome by their peers. Similar to Hawley’s study of women with breast cancer (2009), the presence of influential other individual in our analysis actually modified an outcome measure. Consistently, qualitative study results of men with prostate cancer (Berry et al., 2003a) or those considering screening for prostate cancer (Brown et al., 2016) have included rich description of social network ties in which decision makers seek information from men “a lot like me” (Berry et al., 2003a) (p. 97). In this way, the decision frame serves as a heuristic that assists the decision maker in determining the most desirable options and outcomes for someone like them. As suggested by the current study, elimination of all but the most valuable and relevant alternatives may also lead the decision maker to feel better prepared.
As Marin and Wellman (2014) observed, individuals with similar attributes often occupy similar positions in society and have access to similar resources and opportunities. Homophily may also represent one mechanism by which, as proposed in the ODSF (O’Connor et al., 1998), important others influence an individual’s health care decision. The ODSF posits that decision makers are influenced by their perceived resources to make and implement a decision. As such, social contacts who are similar to the decision maker on a given dimension do not merely establish social norms; rather, they may also provide information about resources that in turn affect the decision maker’s perception of the decision.
Accordingly, preparation scores of men without an informative friend or co-worker were predicted by a more complex set of variables. Being diagnosed with lower risk level cancer, in which more options are available, resulted in lower preparation scores at one month after study enrollment and within that group of men, having no family member for an information source further predicted low preparation scores. These sets of relationships between potentially homophilic individuals (family, friends and co-workers) and complicating variables (risk level) confirm the importance of discussing and even including homophilic individuals along with men with prostate cancer in the options review visit. While other research is scant, multiple patient advocate groups and services have based programs on the premise that outside of the clinical setting, patients have a preference for support from another individual with whom at least one characteristic is shared.
Our analysis is limited by the narrow focus on perceived preparation, only one aspect of decision quality. Our survey format embedded in P3P did not provide for open-ended description of details regarding the information gained from others (for example, was it trusted?), nor do we know which direction of influence was documented. A respondent may have ranked a co-worker as highly influential, however it is impossible to know whether the influence was toward or away from a certain care option. We do not know the extent of perceived homophily between the participants and the identified family, friends and co-workers; however, knowing that participants identified the others as influential and a source of information, we have some certainty about the relationships.
What can clinicians do with our exploration of homophily? Consider that consultation appointments made for men newly diagnosed with LPC should include at least one individual from the man’s relationship network, most often a spouse or partner. Consultations with persons who have other types of cancer diagnoses also may benefit from inclusion of such a decision-support partner. Clinicians may solicit information from the patient about influential others. For example, inquiring if someone else known to the patient has been through the same or a similar situation. Clinicians can then explain any differences between the two cases without dishonoring the importance of the homophilic relationship and such communications may help improve the quality of health decision making.
Continued study of the influence of homophilic relationships and patient cancer decision making is warranted. The P3P intervention currently uses communication coaching videos tailored to the user’s race, age and language to enhance patient-clinician visits. A more specifically tailored intervention may have even a greater impact if we were able to tell users that “most men like you were satisfied with the decision you are considering.” We may find that with certain crowd-sourcing methods (Baum, 2016) we can predict additional outcomes based on large data profiles of patient characteristics. Perhaps we can guide patients with particular non-mutable characteristics (e.g., disease risk) to use certain types of information sources, including reliable individuals with homophilic ties, or even to predict decision regret for certain groups of patients.
In future research, it will be worthwhile to measure homophily directly to ascertain its influence relative to other factors thought to affect the involvement of personal and social contacts in health care decision making. As Brown, Oetzel, and Henderson (2016) observed, homophily is one of several variables—including tie strength, medical knowledge, and geographic proximity—that may influence the extent to which decision makers disclose health-related information to social network contacts and in turn receive new information. Current literature and theory support the notion that personal and social contacts play an important role in health care decision making, yet the mechanisms by which these contacts come to be viewed as influential by the decision maker are unclear. By differentiating the effect of homophily from that of other factors, health scientists will contribute to a knowledge base that may eventually dictate an expansion of descriptive decision theory in the health care context.
CONCLUSION
Our review and analysis suggest that homophily is a phenomenon that is manifest in health care decision making. Faced with a list of options to prevent or manage health conditions, decision makers turn to known individuals in their environments, particularly those individuals with whom the decision maker can identify on some level. Decision aid content and clinicians that honor the need for homophilic affirmation may be more effective in supporting shared health decisions.
REFERENCES
- Anderson KG, Tomlinson K, Robinson JM, & Brown SA (2011). Friends or Foes: Social Anxiety, Peer Affiliation, and Drinking in Middle School. Journal of Studies on Alcohol and Drugs, 72(1), 61–69. doi: 10.15288/jsad.2011.72.61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arnold EA, Sterrett-Hong E, Jonas A, & Pollack LM (2016). Social networks and social support among ball-attending African American men who have sex with men and transgender women are associated with HIV-related outcomes. Glob Public Health, 1–15. doi: 10.1080/17441692.2016.1180702 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ayala GX, Vaz L, Earp JA, Elder JP, & Cherrington A (2010). Outcome effectiveness of the lay health advisor model among Latinos in the United States: an examination by role. Health Educ Res, 25(5), 815–840. doi: 10.1093/her/cyq035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baum N (2016). Crowd Sourcing. J Med Pract Manage, 31(4), 238–239. [PubMed] [Google Scholar]
- Bennett C, Graham ID, Kristjansson E, Kearing SA, Clay KF, & O’Connor AM (2010). Validation of a preparation for decision making scale. Patient Educ Couns, 78(1), 130–133. doi:S0738-3991(09)00232-8 [pii] 10.1016/j.pec.2009.05.012 [DOI] [PubMed] [Google Scholar]
- Berry DL, Ellis WJ, Blasko JB, Russell KJ, Bush N, Blumenstein BA, & Lange PH (2006). Factors That Predict Treatment Choice and Satisfaction with the Decision in Men with Localized Prostate Cancer. Clinical Genitourinary Cancer, 5, 219–226. [DOI] [PubMed] [Google Scholar]
- Berry DL, Ellis WJ, Woods NF, Schwien C, Mullen KH, & Yang C (2003a). Treatment decision-making by men with localized prostate cancer: the influence of personal factors. Urol Oncol, 21(2), 93–100. [DOI] [PubMed] [Google Scholar]
- Berry DL, Ellis WJ, Woods NF, Schwien C, Mullen KH, & Yang C (2003b). Treatment decision-making by men with localized prostate cancer: The influence of personal factors. Urologic Oncology: Seminars and Original Investigations, 21(2), 93–100. doi: 10.1016/S1078-1439(02)00209-0 [DOI] [PubMed] [Google Scholar]
- Berry DL, Hong F, Blonquist TM, Halpenny B, Filson CP, Master VA, … Somayaji P. (2018). Decision Support with the Personal Patient Profile-Prostate: A Multi-Center Randomized Trial. J Urol, 199, 89–97. doi: 10.1016/j.juro.2017.07.076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berry DL, Nayak M, Halpenny B, Harrington S, Loughlin KR, Chang P, … Kibel AS. (2015). Treatment Decision Making in Patients with Bladder Cancer. Bladder Cancer, 1, 151–158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berry DL, Wang Q, Halpenny B, & Hong F (2012). Decision preparation, satisfaction and regret in a multi-center sample of men with newly diagnosed localized prostate cancer. Patient Educ Couns, 88(2), 262–267. doi: 10.1016/j.pec.2012.04.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown D, Oetzel J, & Henderson A (2016). Communication networks of men facing a diagnosis of prostate cancer. J Clin Nurs, 25(21-22), 3266–3278. doi: 10.1111/jocn.13369 [DOI] [PubMed] [Google Scholar]
- Busemeyer JR (2015). Cognitive science contributions to decision science. Cognition, 135, 43–46. doi: 10.1016/j.cognition.2014.11.010 [DOI] [PubMed] [Google Scholar]
- Damacena GN, Szwarcwald CL, & de Souza Júnior PRB (2014). HIV risk practices by female sex workers according to workplace. Rev Saúde Pública, 48(2), 428–437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daw J, Margolis R, & Verdery AM (2015). Siblings, friends, course-mates, club-mates: how adolescent health behavior homophily varies by race, class, gender, and health status. Soc Sci Med, 125, 32–39. doi: 10.1016/j.socscimed.2014.02.047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elwyn G, O’Connor A, Stacey D, Volk R, Edwards A, Coulter A, … Whelan T. (2006). Developing a quality criteria framework for patient decision aids: online international Delphi consensus process. Bmj, 333(7565), 417. doi: 10.1136/bmj.38926.629329.AE [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elwyn G, O’Connor AM, Bennett C, Newcombe RG, Politi M, Durand MA, … Edwards A. (2009). Assessing the quality of decision support technologies using the International Patient Decision Aid Standards instrument (IPDASi). PLoS One, 4(3), e4705. doi: 10.1371/journal.pone.0004705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fagerlin A, Pignone M, Abhyankar P, Col N, Feldman-Stewart D, Gavaruzzi T, … Witteman HO. (2013). Clarifying values: an updated review. BMC Med Inform Decis Mak, 13 Suppl 2, S8. doi: 10.1186/1472-6947-13-s2-s8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flatt JD, Agimi Y, & Albert SM (2012). Homophily and health behavior in social networks of older adults. Fam Community Health, 35(4), 312–321. doi: 10.1097/FCH.0b013e3182666650 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibson DE, & Lawrence BS (2010). Women’s and Men’s Career Referents: How Gender Composition and Comparison Level Shape Career Expectations. Organization Science, 21(6), 1159–1175. [Google Scholar]
- Gilbar R, & Gilbar O (2009). The medical decision-making process and the family: The case of breast cancer patients and their husbands. Bioethics, 23(3), 183–192. doi: 10.1111/j.1467-8519.2008.00650.x [DOI] [PubMed] [Google Scholar]
- Go MH, Tucker JS, Green HD Jr., Pollard M, & Kennedy D (2012). Social distance and homophily in adolescent smoking initiation. Drug Alcohol Depend, 124(3), 347–354. doi: 10.1016/j.drugalcdep.2012.02.007 [DOI] [PubMed] [Google Scholar]
- Han JY, Wise M, Kim E, Pingree R, Hawkins RP, Pingree S, … Gustafson DH. (2010). Factors Associated with Use of Interactive Cancer Communication System: An Application of the Comprehensive Model of Information Seeking. J Comput Mediat Commun, 15(3), 367–388. doi: 10.1111/j.1083-6101.2010.01508.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawley ST, Griggs JJ, Hamilton AS, Graff JJ, Janz NK, Morrow M, … Katz SJ. (2009). Decision involvement and receipt of mastectomy among racially and ethnically diverse breast cancer patients. J Natl Cancer Inst, 101(19), 1337–1347. doi: 10.1093/jnci/djp271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janis IL, & Mann L (1976). Coping with decisional conflict: An analysis of how stress affects decision-making suggests interventions to improve the process. American Scientist, 64(6), 657–667. [Google Scholar]
- Johnson J, & Meischke H (1993). A Comprehensive Model of Cancer-Related Information Seeking Applied to Magazines. Human Communication Research, 19(3), 343–367. doi: 10.1111/j.1468-2958.1993.tb00305.x [DOI] [Google Scholar]
- Kahneman D, & Tversky A (1979). Prospect theory: an analysis of decision under risk. Econometrica, 47, 263–291. [Google Scholar]
- Kelly-Powell M (1997). Personalizing choices: patients’ experiences with making treatment decisions. Research in Nursing & Health, 20(3), 219–227. doi: [DOI] [PubMed] [Google Scholar]
- Lazarsfeld PF, & Merton RK (1954). Friendship as a social process: A substantive and methodological analysis. Freedom and control in modern society, 18(1), 18–66. [Google Scholar]
- Lee HO, & Kim S (2015). Linking health information seeking to behavioral outcomes: antecedents and outcomes of childhood vaccination information seeking in South Korea. J Health Commun, 20(3), 285–296. doi: 10.1080/10810730.2014.927035 [DOI] [PubMed] [Google Scholar]
- Llupia A, Puig J, Mena G, Bayas JM, & Trilla A (2016). The social network around influenza vaccination in health care workers: a cross-sectional study. Implement Sci, 11(1), 152. doi: 10.1186/s13012-016-0522-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marin A, & Wellman B (2014). Social Network Analysis: An Introduction. Thousand Oaks, CA: SAGE. [Google Scholar]
- McCroskey JC, Richmond VP, & Daly JA (1975). The development of a measure of perceived homophily in interpersonal communication. Human Communication Research, 1(4), 323–332. [Google Scholar]
- McPherson M, Smith-Lovin L, & Cook JM (2001). Birds of a feather: Homophily in social networks. Annu Rev Sociol, 27, 415–444. [Google Scholar]
- Meng J (2016). Your Health Buddies Matter: Preferential Selection and Social Influence on Weight Management in an Online Health Social Network. Health Commun, 31(12), 1460–1471. doi: 10.1080/10410236.2015.1079760 [DOI] [PubMed] [Google Scholar]
- Nambisan P (2011). Information seeking and social support in online health communities: impact on patients’ perceived empathy. J Am Med Inform Assoc, 18(3), 298–304. doi: 10.1136/amiajnl-2010-000058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Brien MA, Whelan TJ, Charles C, Ellis PM, Gafni A, Lovrics P, … Dimitry S. (2008). Women’s perceptions of their treatment decision-making about breast cancer treatment. Patient Educ Couns, 73(3), 431–436. doi: 10.1016/j.pec.2008.07.015 [DOI] [PubMed] [Google Scholar]
- O’Connor AM (1995). Validation of a decisional conflict scale. Med Decis Making, 15(1), 25–30. [DOI] [PubMed] [Google Scholar]
- O’Connor AM, Tugwell P, Wells GA, Elmslie T, Jolly E, Hollingworth G, … Drake E. (1998). A decision aid for women considering hormone therapy after menopause: decision support framework and evaluation. Patient Educ Couns, 33(3), 267–279. [DOI] [PubMed] [Google Scholar]
- Pagano M, & Gauvreau K (2000). Principles of Biostatistics (2nd ed ed.). Pacific Grove, CA: Duxbury. [Google Scholar]
- Pozzar R, & Berry DL (2017). Gender differences in bladder cancer treatment decision making. Oncol Nurs Forum, 44(2), 204–209. doi: 10.1188/17.ONF.204-209 [DOI] [PubMed] [Google Scholar]
- Quist HG, Christensen U, Carneiro IG, Hansen JV, & Bjorner JB (2014). Do colleagues influence our lifestyle: the matter of smoking, body mass index and leisure-time physical activity? Prev Med, 67, 166–170. doi: 10.1016/j.ypmed.2014.07.032 [DOI] [PubMed] [Google Scholar]
- R Core Team. (2017). R: A language and environment for statistical computing [Computer software]. Vienna, Austria: R Foundation for Statistical Computing; Retrieved from https://www.r-project.org/ [Google Scholar]
- Shaw EK, Scott JG, & Ferrante JM (2013). The influence of family ties on men’s prostate cancer screening, biopsy, and treatment decisions. American Journal of Men’s Health, 7(6), 461–471. doi: 10.1177/1557988313480226 [DOI] [PubMed] [Google Scholar]
- Shelton RC, Charles TA, Dunston SK, Jandorf L, & Erwin DO (2017). Advancing understanding of the sustainability of lay health advisor (LHA) programs for African-American women in community settings. Transl Behav Med, 7(3), 415–426. doi: 10.1007/s13142-017-0491-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith-McLallen A, Fishbein M, & Hornik RC (2011). Psychosocial determinants of cancer-related information seeking among cancer patients. J Health Commun, 16(2), 212–225. doi: 10.1080/10810730.2010.522227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stacey D, Légaré F, Lewis K, Barry MJ, Bennett CL, Eden KB, … Trevena L. (2017). Decision aids for people facing health treatment or screening decisions. Cochrane Database of Systematic Reviews(4). doi: 10.1002/14651858.CD001431.pub5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Therneau T, Atkinson B, & Ripley B (2017). rpart: Recursive Partitioning and Regression Trees. R package version 4.1-11. Retrieved from https://CRAN.R-project.org/package=rpart
- Tversky A (1975). A Critique of Expected Utility Theory: Descriptive and Normative Considerations. Erkenntnis (1975-), 9(2), 163–173. [Google Scholar]
- Tversky A, & Kahneman D (1981). The Framing of Decisions and the Psychology of Choice. Science, 211(4481), 453–458. [DOI] [PubMed] [Google Scholar]
- Van Stee SK, & Yang Q (2017). Online Cancer Information Seeking: Applying and Extending the Comprehensive Model of Information Seeking. Health Commun, 1–10. doi: 10.1080/10410236.2017.1384350 [DOI] [PubMed] [Google Scholar]
- von Neumann J, & Morgenstern O (1953). Theory of Games and Economic Behavior (3 ed.). Princeton, NJ: Princeton University Press. [Google Scholar]
- Wallner LP, Li Y, McLeod MC, Hamilton AS, Ward KC, Veenstra CM, … Hawley ST. (2017). Decision-support networks of women newly diagnosed with breast cancer. Cancer. doi: 10.1002/cncr.30848 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Z, Walther JB, Pingree S, & Hawkins RP (2008). Health information, credibility, homophily, and influence via the Internet: Web sites versus discussion groups. Health communication, 23(4), 358–368. [DOI] [PubMed] [Google Scholar]
- Watson CA, Weng CX, French T, Anderson BJ, Nemeth C, McNutt LA, & Smith LC (2014). Substance abuse treatment utilization, HIV risk behaviors, and recruitment among suburban injection drug users in Long Island, New York. AIDS Behav, 18 Suppl 3, 305–315. doi: 10.1007/s10461-013-0512-2 [DOI] [PubMed] [Google Scholar]
- Yates J (1990). Judgement and Decision-Making. Englewood Cliffs, NJ: Prentice-Hall. [Google Scholar]
- Zhang J, Tong L, Lamberson PJ, Durazo-Arvizu RA, Luke A, & Shoham DA (2015). Leveraging social influence to address overweight and obesity using agent-based models: the role of adolescent social networks. Soc Sci Med, 125, 203–213. doi: 10.1016/j.socscimed.2014.05.049 [DOI] [PMC free article] [PubMed] [Google Scholar]