Summary
Wound care quality and speed of burn healing are important factors that affect the treatment, prognosis and complications of burns. Burn care is challenging, and the ideal method controversial. The aim of this study was to compare the effects of a new dressing (ColActive dressing) in the treatment of superficial second-degree burns versus traditional dressing including Vaseline and Nitrofurazone. This was a randomized clinical trial study involving 25 cases. A superficial second-degree burn area was divided into two parts in each patient; randomly, traditional dressing was used on one area, and ColActive plus Ag dressing on the other. Every 3 days, after removing the dressings and washing the wounds, wound surface area was evaluated by medical photographic records and J image software. Wound surface area in the two groups was compared before dressing and on the 3rd, 6th, 9th and 12th day afterwards. The difference was not significant before dressing, but significant on the 3rd, 6th, 9th and 12th post-operative day. The difference was significant in both groups, but it was more prominent in the ColActive group (p<0.001) than in the traditional group (p<0.05). Considering the results of this study and good results in previous case reports, ColActive may be more effective than traditional dressing. We suggest a more comprehensive study for a longer period with a larger number of cases to compare other important variables such as scar quality, cost, and pain in the two dressings.
Keywords: Nitrofurazone, Vaseline, ColActive Plus Ag, second-degree burn
Abstract
La qualité des soins locaux et la vitesse de cicatrisation sont d’importants paramètres affectant le traitement, le pronostic et les complications des brûlures. La méthode idéale reste encore à trouver. Le but de cet étude est de comparer un nouveau pansement (ColActive ®) au traditionnel nitrofurazone/vaseline sur les brûlures du 2ème superficiel. Il s’agit d’une étude randomisée portant sur 25 patients. Les zones de 2ème superficiel étaient divisées en 2 recevant, après tirage au sort, l’une ColActive® Plus Ag, l’autre nitrofurazone/vaseline. Après nettoyage, les photographies des brûlures étaient évaluées en utilisant Image J, à l’entrée et à J3, 6, 9 et 12. Les différences étaient significatives à J3, 6, 9, 12 avec une valeur de p plus prononcée (<0,001) dans le groupe ColActive® Plus Ag que dans le groupe contrôle (<0,05). Considérant ces résultats en faveur de l’utilisation de ColActive® Plus Ag, nous suggérons une étude plus globale, sur un nombre plus élevé de patients, comparant aussi la qualité cicatricielle, le coût et la douleur.
Introduction
Burn injuries are a major public health problem in the world.1 According to the International Society of Burns, burn is defined as an injury to the skin or other body tissue caused mainly by acute thermal trauma, such as hot liquid, fire, radiation, electricity or friction.2 According to the World Health Organization (WHO), there were 300,000 deaths worldwide due to burns in 2012, with 96% of these deaths occurring in developing countries.3
Boyer classified burns as first- second- and third-degree, according to the tissues affected. Treatment differs according to burn depth. Second-degree burns are those that damage the epidermis and part of the dermis.1 Superficial second-degree burns involve epidermis and superficial layers of dermis. The treatment of these burns is conservative. Burn wound bed preparation is the most important factor affecting the healing of the wound. The care of superficial second-degree burns is controversial, and the ideal method for topical burn care is unknown. The quality of the scar following burns depends on the duration of healing. The aim of care of these burns is to decrease the healing period.
The care principles of burn wounds (wound bed preparation) include the same principles as chronic wound care, which are briefly summed up with T.I.M.E (tissue non-viable or deficient, infection or inflammation, moisture control, epidermal growth), and include early excision, biological control of amount of exudates, prevention of tissue desiccation and adequate moisture in the wound environment. 4
The nature of a chronic wound is similar to the burn wound environment in the amount of MMP levels. T.I.M.E for chronic wound care is equivalent to modern and organized care in burn wounds. Applying the principles of chronic wound care to burn wounds has improved patient survival and prognosis.
An ideal dressing should contain a suitable environment including growth factors and MMPs, at the least create exudates, provide appropriate microbial burden and adequate moisture, lead to less pain and be economical and available.5-8
Different companies have provided several compounds for dressing wounds. One compound that has recently been introduced is ColActive Plus Ag.9 It is claimed that this dressing includes components such as collagen, silver ion, CMC (Carboxy Methyl Cellulose), EDTA (Ethylene Diamine Tetracetic Acid) and Alginate and, therefore, is very effective in the care of wounds, chronic and burn wounds in particular. Some case studies report good results following the application of this dressing to chronic wounds such as diabetic foot ulcer, pressure ulcer, venous ulcers, ulcers caused by blood diseases, partial-thickness burn wounds and acute wounds.10-19
The most important compound within ColActive dressing is collagen. The effectiveness of other dressings including collagen has been reported in numerous clinical trials on several chronic wounds, second-degree burns, acute wounds and location of donor areas.20-27 In our centre, the experience of applying this dressing on second-degree burns has been successful.28
Considering all this evidence, it seems that this compound is effective in the treatment of burn wounds. However, our review of the available literature did not find any reliable study on the use of this dressing, apart from some case reports. Nowadays, therapeutic strategies to restore burned tissue are mostly unsatisfactory from an aesthetic and functional point of view. Thus, new therapeutic strategies to reduce the damage caused by burns are necessary.29
30 Therefore, this study was designed to evaluate the effectiveness of this compound in the treatment of superficial second-degree burns versus traditional dressing including Vaseline and Nitrofurazone.
Materials and methods
This was a randomized clinical trial study to compare two kinds of dressing in patients with superficial second-degree burns, who were referred to the Shahid Motahari Burn Hospital in Tehran, Iran, from August to December 2015. Twentyfive cases were enrolled in the study. The proposal was explained to the patients, and they chose to participate voluntarily. Informed consent was taken from patients, their parents or their legal guardian. The study was approved by the Ethical Committee of Iran University of Medical Science of the Islamic Republic of Iran (IR.IUMS.REC.1349-24669).
Patients of both sexes, aged between 5 to 40 years, who were referred in the first 24 hours after burn trauma, were included. Exclusion criteria included underlying disease, electrical or chemical burn, and inhalation injury.
A superficial second-degree burn area was divided into two parts in every patient. This was clinically performed by an experienced burn surgeon. Randomly, traditional dressing [Nitrofurazone (Iran Najo Company) and Vaseline (Salem Company, Iran)] was used on one area and ColActive plus Ag (composed of collagen, sodium alginate and silver ion and EDTA) on the other. For dressing, each area was washed by the conventional method with normal saline. One area was dressed with Nitrofurazone and Vaseline Gauze and the other area with one sheet of ColActive plus Ag as primary dressing. The Gauze was applied on top of primary dressings in both areas and fixed by bands or Surgifix on the face.
The Vaseline and Nitrofurazone dressing was changed once daily, and the other at least once every 3 days. This was done by an experienced burn nurse. Then every 3 days, after the dressings had been removed and the wounds washed, the patients were evaluated by an experienced burn surgeon, who was blind to the type of dressing used, and photographs of the wounds were taken. Wound surface area was evaluated by medical photographic records and J image software. A burn surgeon evaluated the amount of epithelialization and wound healing every 3 days and the remaining wound surface area was measured by image J software (National Institutes of Health, Bethesda, Maryland, USA). Wound infection was evaluated clinically and by culture. The wounds were assessed by two separate surgeons and infectious disease specialists. Wound culture taken during the dressing change was sent for bacterial wound culture testing. There was no sign of wound infection in our patients.
Statistical analysis was conducted by SPSS-16 and using the t test, and results for the two groups were compared.
Results
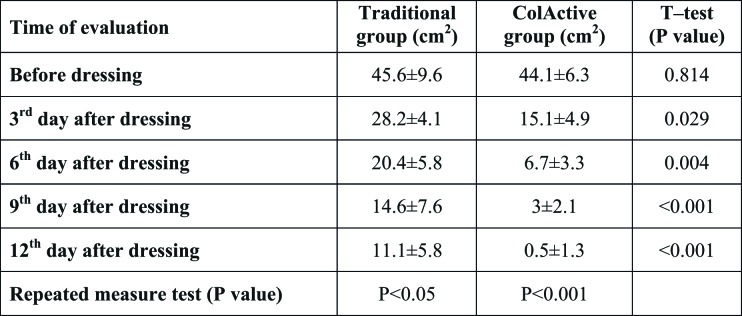
In this study, 25 patients with superficial second-degree burns were evaluated. Nineteen patients (76%) were male and 6 patients (24%) were female. Mean age was 14.2±3.1 years. Clinically, there was no infection in the 2 groups. Wound surface area in the two groups was compared in the days before dressing and on the 3rd, 6th, 9th and 12th day afterwards. The difference was not significant before dressing, but significant on the 3rd, 6th, 9th and 12th post-operative day. The wound surface area was evaluated by Image J software. The difference was significant in both groups, but it was more prominent in the ColActive group (p<0.001) than in the traditional group (p<0.05), as shown in Table I.
Table I. Comparison of wound surface area in traditional and ColActive groups.
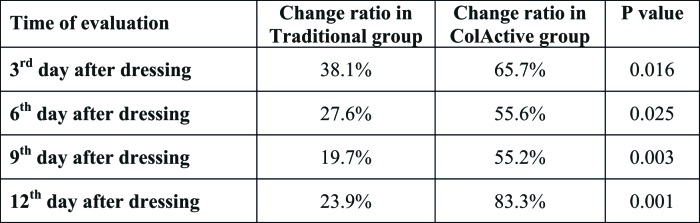
The healing ratio of burn wound area in the 2 groups was also compared. On every day, the difference between the 2 groups was significant. This difference was more prominent from the 9th to the 12th day, which indicates that ColActive dressing is more effective in the final days of dressing, as shown in Table II (Figs. 1, 2 and 3).
Table II. Comparison of ratio change of wound surface area with traditional and ColActive dressing.
Fig. 1. Traditional dressing and ColActive dressing on first day.

Fig. 2. The same wound on the 3rd day.
Fig. 3. The differences between wound surface area on the 9th day.
Discussion
Thermal burn injuries and their consequences are still a major health problem in the world, especially in developing and less developed countries. However, identifying the ideal method to facilitate their healing process is challenging for modern medicine. Many dressings have been introduced by different companies, but the ideal dressing is unknown.
In this study, ColActive plus Ag dressing was compared with traditional dressing including Vaseline and Nitrofurazone. ColActive Plus Ag dressing contains collagen, silver ion, CMC, EDTA and Alginate. All these compounds have been previously applied in different dressings and their effectiveness and safety have been demonstrated. ColActive plus Ag alone includes all these compounds but in different forms, which may increase its effectiveness.
Alginate and carboxymethylcellulose (CMC) have been used in some wound dressings. Alginate and CMC exert an antimicrobial effect due to their gelling properties. Sodium alginate and CMC fibres absorb water and swell, so the spaces between the fibres are closed and bacteria are trapped. Also, the addition of CMC and alginate introduces unique characteristics to the matrix that optimize moisture in the wound bed.31
Some dressings include specific antibacterial agents (e.g. silver ions) in their formulation in order to further protect the wound bed from undesired microbial contaminations.32 Silver-based therapies in the form of silver-impregnated wound dressings and Ag+ salt solutions have been used to treat acute and chronic wounds. Ionized silver (Ag+) is the bioactive form of silver that is capable of reacting with a broad spectrum of biomolecules, including DNA, amino acid residues, and compounds with sulfhydryl groups. Ag+ elicits cytotoxic effects in microorganisms by inducing physical cell wall damage, enhancing membrane permeability, disrupting ATP production and DNA replication, and generating reactive oxygen species (ROS). Silver is unionized in many dressings but is ionized in ColActive dressing, which may make it faster acting and its application less painful.
Collagen is a natural component of the dermal matrix produced by fibroblasts, and functions as protective scaffolding for migrating epithelial cells in the regenerating skin. Collagen gives the skin its tensile strength and is essential for all phases of wound healing. It attracts fibroblasts and keratinocytes to the wound and encourages debridement, angiogenesis and reepithelialization.33
Collagen dressings stimulate new tissue growth and encourage deposition and organization of newly formed collagen fibres and granulation tissue in the wound bed. The matrix metalloproteinases (MMPs) are zinc-dependent endopeptidases. They are capable of degrading all kinds of extracellular matrix proteins. The collagen in the collagen-based dressings bind to the MMPs found in the extracellular fluid of the wounds and is an alternative collagen source, leaving the body’s natural collagen available for normal wound healing.33 Native collagen does not have any exposed receptor, and should be denatured in wound for its effectiveness. Collagen is native in most dressings except in dressings such as ColActive Plus Ag, ColActive plus, Bio Step and Bio Step Ag, where it is denatured.34 Therefore, the collagen is faster-acting in these dressings.
Zinc is a cofactor that is required for MMP activity. Ethylene diamine tetracetic acid (EDTA) is a chelating agent that binds to zinc ion with a very high affinity. EDTA permanently deactivates MMPs by binding to the zinc ions of these proteases. 35,36 Therefore, ColActive inhibits MMPs through two means; collagen and EDTA.
In this study, we found that speed of epithelialization was faster with this dressing than with the conventional dressing during all application durations. For example, on the 6th and 12th day after dressing, 6.7±3.3cm2 and 3±2.1cm2 wound surface area in the ColActive group was not epithelialized, compared with 20.4±5.8cm2 and 11.1±5.8cm2 in the conventional dressing group. The difference was more prominent in the final days of application. In other words, after the 2nd week, this dressing was more effective than the conventional dressing. The greater effectiveness of this dressing in the first days of application may be due to compounds such as CMC and Alginate, but the increased difference in the final days of application compared with the first days of application may be due to compounds such as collagen and EDTA that inhibit proteases such as collagenase. The concentration of MMPs increases as the wound becomes chronic, but the application of dressings that include collagen decreases MMP concentration. On the other hand, it has been proven that in chronic wounds, as the concentration of MMPs decreases, wound healing improves. This finding has been reported in case reports on a number of chronic wounds, such as diabetic, venous and other types of ulcer.10-19 This corresponds with our own findings in the final days of application, when the wound became chronic; ColActive dressing was more effective, which may be due to the effects of collagen and EDTA on some proteases such as collagenase.
Due to many confounding factors, we could not compare the cost of the two dressing methods. ColActive is more expensive than traditional dressing, but considering the lower frequency of dressing and faster healing of wounds, it may generally be more cost effective in the long term. The effects of this dressing on scar quality were not compared because of the short period of study, but they may turn out to be better in the ColActive group because of the shorter healing period.
Conclusion
Considering the findings of this study as well as good results in a number of previous case reports, ColActive may be more effective than traditional dressing. We suggest that a more comprehensive study over a longer period and with a larger number of cases be carried out in order to compare other important variables, such as scar quality, cost, and pain in the two dressings.
Acknowledgments
Conflict of interest.The authors declare that they have no conflict of interest related to this article.
References
- 1.Chiarotto GB, Neves LMG, Esquisatto MAM, do Amaral MEC. Effects of laser irradiation (670-nm InGaP and 830-nm GaAlAs) on burn of second-degree in rats. Lasers Med Sci. 2014;29(5):1685–1693. doi: 10.1007/s10103-014-1573-9. [DOI] [PubMed] [Google Scholar]
- 2.Trajano ETL, da Trajano LA, dos Santos Silva MA, Venter NG. Low-level red laser improves healing of second-degree burn when applied during proliferative phase. Lasers Med Sci. 2015;30(4):1297–1304. doi: 10.1007/s10103-015-1729-2. [DOI] [PubMed] [Google Scholar]
- 3.Ma K, Du M, Liao M, Chen S. Evaluation of wound healing effect of punica granatum L Peel extract on deep second-degree burns in rats. Trop J Pharma Res. 2015;14(1):73–78. [Google Scholar]
- 4.Stanirowski PJ, Wnuk A, Cendrowski K, Sawicki W. Growth factors, silver dressings and negative pressure wound therapy in the management of hard-to-heal postoperative wounds in obstetrics and gynecology: a review. Arch Gynecol Obstet. 2015;2015:1–19. doi: 10.1007/s00404-015-3709-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wen X, Zheng Y, Wu J, Yue L. In vitro and in vivo investigation of bacterial cellulose dressing containing uniform silver sulfadiazine nanoparticles for burn wound healing. Pro Nat Sci-Mater. 2015;25(3):197–203. [Google Scholar]
- 6.Jin SG, Kim KS, Yousaf AM, Kim DW. Mechanical properties and in vivo healing evaluation of a novel Centella asiatica-loaded hydrocolloid wound dressing. Int J Pharma. 2015;490(1-2):240–247. doi: 10.1016/j.ijpharm.2015.05.058. [DOI] [PubMed] [Google Scholar]
- 7.Napavichayanun S, Amornsudthiwat P, Pienpinijtham P, Aramwit P. Interaction and effectiveness of antimicrobials along with healing-promoting agents in a novel biocellulose wound dressing. Mater Sci Eng C. 2015;55:95–104. doi: 10.1016/j.msec.2015.05.026. [DOI] [PubMed] [Google Scholar]
- 8.Huang X-F, Jia J-W. A novel chitosan-based sponge coated with selfassembled thrombin/tannic acid multilayer films as a hemostatic dressing. Chinese J Polym Sci. 2015;33(2):284–290. [Google Scholar]
- 9.Covalon Colactive-Application-Guide.pdf. Retrieved February 1, 2014 http://www.covalon.com/userFiles/Colactive-Application-Guide.pdf . [Google Scholar]
- 10.Brett DW. The evaluation of the matrix metalloproteinase (MMP) inhibition activity of a next generation Collagen based wound care dressing and two traditional Collagen based wound care dressings. Retrieved January 16, 2014 from: http://wwwshefakimiacom/Portals/0/pdf/2pdf.2007 . [Google Scholar]
- 11.Lavinia T. An evaluation of a variety of physical properties key to wound care of collagen based wound dressings. Trademark of Smith & Nephew certain marks reg US Pat & TM Off. 2007 [Google Scholar]
- 12.Cortimi G. A prospective, descriptive, case series to assess the performance of a new collagen matrix dressing as an adjunct therapy in the treatment of partial thickness burns. Retrieved January 18, 2014 from: http://wwwUSCD Regional Burn Centre, 2007. [Google Scholar]
- 13.Hermann K, Niezgoda JA. Collagen carboxy-methyl cellulose for the management of chronic nonhealing wounds. Retrieved January 16, 2014, from: http://wwwsmithnephewcom/global/assets/pdf/hermann_peterson_poster_smithnephew_cs059, 2007. [Google Scholar]
- 14.Davis C, Dalbey C, Hill S. The successful use of a new adjunct therapy in both acute and chronic wounds – a prospective, descriptive case series. Poster presented at The WOCN Society 40th Annual Conference, Orlando, Florida, 2008 [Google Scholar]
- 15.Robert LW. Novel porcine collagen matrix used to stimulate wound closure in arrested wounds. 2007 Retrieved January 18, 2014, from: http://wwwsmithnephewcom . [Google Scholar]
- 16.Madura J. Matrix dressing containing EDTA - a new piece of the wound healing puzzle? Poster presented at The WOCN Society 40th Annual Conference, Largo, FL, 2008. [Google Scholar]
- 17.Reynald CA, Renee P, Barbara AM. A prospective, clinical in-market evaluation to assess the performance of a new collagen matrix dressing on facilitating granulation and epidermal migration, in a variety of wound types. 2007 Retrieved January 16, 2014 from: http://wwwshefakimiacom/Portals/0/pdf/2pdf . [Google Scholar]
- 18.Robert LW. Clinical experience with a novel porcine collagen matrix to facilitate final closure of granulating wounds originally treated with negative pressure wound therapy. 200 Retrieved January18, 2014, from: http://wwwsmithnephewcom/global/assets/pdf/products/wound/r_williams_final_closure-8x4-9_27pdf . [Google Scholar]
- 19.Robert LW. Experience with novel porcine collagen matrix and silver used in long-term dressings. Retrieved January 18, 2014, from: http://wwwsmithnephewcom/global/assets/pdf . [Google Scholar]
- 20.Veves A, Sheehan P, Pham HT. A randomized, controlled trial of Promogran (a collagen/oxidized regenerated cellulose dressing) vs standard treatment in the management of diabetic foot ulcers. Arch Surg. 2002;137(7):822–827. doi: 10.1001/archsurg.137.7.822. [DOI] [PubMed] [Google Scholar]
- 21.Vin F, Teot L, Meaume S. The healing properties of Promogran in venous leg ulcers. J Wound Care. 2002;11(9):335–341. doi: 10.12968/jowc.2002.11.9.26438. [DOI] [PubMed] [Google Scholar]
- 22.Wollina U, Schmidt W-D, Krönert C, Nelskamp C. Some effects of a topical collagen-based matrix on the microcirculation and wound healing in patients with chronic venous leg ulcers: preliminary observations. Int J Low Extrem Wounds. 2005;4(4):214–224. doi: 10.1177/1534734605283001. [DOI] [PubMed] [Google Scholar]
- 23.Letendre S, La Porta G, O’Donnell E, Dempsey J, Leonard K. Pilot trial of biovance collagen-based wound covering for diabetic ulcers. Adv Skin Wound Care. 2009;22(4):161–166. doi: 10.1097/01.ASW.0000305463.32800.32. [DOI] [PubMed] [Google Scholar]
- 24.Kolenik SA, McGovern TW, Leffell DJ. Use of a lyophilized bovine collagen matrix in postoperative wound healing. Dermatol Surg. 1999;25(4):303–307. doi: 10.1046/j.1524-4725.1999.08230.x. [DOI] [PubMed] [Google Scholar]
- 25.Delatte SJ, Evans J, Hebra A, Adamson W. Effectiveness of betaglucan collagen for treatment of partial-thickness burns in children. J Pediatr Surg. 2001;36(1):113–118. doi: 10.1053/jpsu.2001.20024. [DOI] [PubMed] [Google Scholar]
- 26.Mian E, Mian M, Beghe F. Lyophilized type-I collagen and chronic leg ulcers. Int J Tissue React. 1990;113(5):257–269. [PubMed] [Google Scholar]
- 27.Frantz JM, Dupuy BM, Kaufman HE, Beuerman RW. The effect of collagen shields on epithelial wound healing in rabbits. Am J Ophthalmol. 1989;108(5):524–528. doi: 10.1016/0002-9394(89)90428-5. [DOI] [PubMed] [Google Scholar]
- 28.de Carvalho VF, Paggiaro AO, Isaac C, Gringlas J, Ferreira MC. Clinical trial comparing 3 different wound dressings for the management of partial-thickness skin graft donor sites. J Wound Ostomy Continence Nurs. 2011;38(6):643–647. doi: 10.1097/WON.0b013e3182349d2f. [DOI] [PubMed] [Google Scholar]
- 29.Núñez SC, França CM, Silva DFT, Nogueira GEC. The influence of red laser irradiation timeline on burn healing in rats. Lasers Med Sci. 2013;28(2):633–641. doi: 10.1007/s10103-012-1105-4. [DOI] [PubMed] [Google Scholar]
- 30.Zhang X, Liu L, Wei X, Tan YS. Impaired angiogenesis and mobilization of circulating angiogenic cells in HIF-1α heterozygous-null mice after burn wounding. Wound Repair Regen. 2010;18(2):193–201. doi: 10.1111/j.1524-475X.2010.00570.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wiegand C, Abel M, Ruth P, Elsner P, Hipler U-C. In vitro assessment of the antimicrobial activity of wound dressings: influence of the test method selected and impact of the pH. J Mater Sci Mater Med. 2015;26(1):1–13. doi: 10.1007/s10856-014-5343-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Madaghiele M, Demitri C, Sannino A, Ambrosio L. Polymeric hydrogels for burn wound care: advanced skin wound dressings and regenerative templates. Burns Trauma. 2014;2(4):153. doi: 10.4103/2321-3868.143616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mariappan N. Collagen dressing for thermal burns. Sch J App Med Sci. 2015;3(1A):58–61. [Google Scholar]
- 34.Herndon D. Philadelphia: WB Saunders Co, Ltd; 2007. Total burn care. [Google Scholar]
- 35.McCarty SM. The role and control of matrix metalloproteinases (MMPs) in equine cutaneous wounds: a focus on both endogenous and exogenous proteases. Thesis. 2014 [Google Scholar]
- 36.Wooley RE, Ritchie BE, Kemp DT, Capomacchia AC, Burnley VV. Methods and compositions for promoting wound healing. US Patent. 2015;20:150–155. [Google Scholar]