Abstract
Purpose: Cardiac rehabilitation is associated with improved clinical outcomes, but the impact of individual cardiac rehabilitation sessions on readmission rates is less studied. Methods: A retrospective evaluation of the relationship between the number of cardiac rehabilitation sessions completed and all-cause and cardiac readmission rates at 1 year was conducted. The 1-year cardiac readmission counts were modeled via Poisson regression. Results: Of the 347 patients included in the primary analysis, 227 (65%) completed all assigned cardiac rehabilitation sessions. At 1 year, 135 patients (39%) had at least 1 cardiac readmission, and 155 patients (45%) had at least 1 all-cause readmission. The primary result was that every additional cardiac rehabilitation session completed was associated with a 1.75% lower incidence rate of 1-year cardiac readmission (P = .01) and a 2% lower incidence rate of all-cause hospital readmission (P = .001). Conclusion: Regardless of the number of cardiac rehabilitation sessions assigned, each additional session attended was associated with reduced cardiac readmission by 1.75% and all-cause readmission by 2%.
Keywords: cardiac rehabilitation, readmission, cardiac readmission, attendance, coronary artery disease
‘Several studies have evaluated the dose-response of cardiac rehabilitation, with additional sessions being associated with better survival, a lower subsequent incidence of myocardial infarction, and reduced hospital readmission rates.’
Introduction
Cardiac rehabilitation is generally associated with improvements in quality of life, risk factor profile, exercise capacity and ability to perform activities of daily living.1-5 In addition, cardiac rehabilitation adherence is associated with improved patient outcomes.6-10 Despite these recognized associations, only 12% of eligible Medicare patients participate in cardiac rehabilitation.7 Moreover, of those patients referred to cardiac rehabilitation, adherence over varied durations is often reported to be in the 50% to 65% range.11-13
Several studies have evaluated the dose-response of cardiac rehabilitation, with additional sessions being associated with better survival, a lower subsequent incidence of myocardial infarction, and reduced hospital readmission rates.6-10,12 The data regarding readmission rates are less than robust. One study found a 25% reduction in long-term readmission risk for cardiac rehabilitation participants compared with nonparticipants.14 A recent meta-analysis found that exercise-based cardiac rehabilitation was associated with reduced hospital admission (30.7% to 26.1%; number needed to treat = 22) compared with no-exercise controls.6
We evaluated our own institutional data to see if each additional cardiac rehabilitation session attended was associated with subsequent reductions in hospital readmission.
Methods
A retrospective review of the relationship between the number of cardiac rehabilitation sessions completed and all-cause hospital readmission rates and cardiac readmission rates 1 year from the index event as well as mortality in HealthPartners members who were referred to cardiac rehabilitation between January 1, 2006, and December 31, 2007, at Regions Hospital was conducted. (HealthPartners is an integrated health care system based in Minnesota. It provides both health care services and health plan financing and administration. The health plan includes more than 1.5 million medical and dental members.) By exclusively using only HealthPartners members referred to cardiac rehabilitation, we were able to capture all events within 30 days and 1 year by review of insurance claims data. Thus, these data provide a comprehensive evaluation of hospital and cardiac readmission rates. Clinical data were collected through queries within the cohorts’ electronic medical record. Mortality information was obtained via the Minnesota death database, which is a public record of deaths occurring in Minnesotans.
The cardiac rehabilitation program included supervised exercise, nutritional counseling, and patient education. Each session lasted approximately 60 to 90 minutes and included 30 to 40 minutes of aerobic exercise, 15 minutes of strength training, and a 30-minute group education session. Patients were instructed to exercise at a rate of perceived exertion of 11 to 14 on the Borg scale, corresponding to “fairly light” to “somewhat hard.”15 Exercise intensity was increased 0.5 to 1 metabolic equivalents every 1 to 3 weeks according to patient exercise training parameters. Cardiac rehabilitation was staffed by exercise physiologists, registered dieticians, and registered nurses under the direction of a cardiologist.
A group of 400 patients attending at least 1 session of cardiac rehabilitation was identified. Patients were assigned to either18, 24, or 36 sessions based on clinical indications, as shown in Table 1. A fourth patient group (sessions unassigned) did not have a specific amount of sessions assigned, with the exception of 2 patients, assigned 12 sessions, 1 patient assigned 5 sessions, and 1 patient assigned 2 sessions. Another 12 patients started cardiac rehabilitation, but only to receive initial exercise instruction, with the intention that they would then exercise on their own. For the remaining 37 patients in this group, the retrospective data collection could not identify the number of sessions assigned. We have included this group in the descriptive statistics but not in the binary or continuous statistical models because perfect attendance and number of sessions missed could not be assessed. The institutional review board approved this study with a waiver of informed consent.
Table 1.
Clinical Guidelines for Determining Number of Cardiac Rehabilitation Sessions Assigned.
| Risk | Criteria | Cardiac Rehabilitation Visits |
|---|---|---|
| Lowa | Uncomplicated event or procedure | 18-24 Visits |
| EF ≥50% | Presence of problems during rehabilitation will move patient into another category and add more sessions | |
| Absence of ectopy, arrhythmia, or block | ||
| Completely revascularized (all areas ≥75% stented or bypassed) | ||
| Moderateb | EF ≥40% | 24-30 Visits |
| Occasional ectopy, arrhythmia, or stable first-degree block | ||
| Microvascular, small vessel disease | ||
| Highc | Complicated event or procedure | 30-36 Visits |
| >2 Stents | ||
| Dissection | ||
| Staged stenting | ||
| Ruptured plaque; thrombectomy | ||
| Groin site hematoma | ||
| CABG and valve surgery | ||
| >1 Valve replaced | ||
| IABP | ||
| Temporary pacemaker | ||
| Hypotension/hypertension | ||
| Hypoxia/pneumonia | ||
| Cardiogenic shock | ||
| Cardiac/respiratory arrest | ||
| CHF | ||
| Postevent or procedural ischemia | ||
| Clinical depression | ||
| EF < 40% | ||
| Frequent arrhythmia, ectopy, or second-degree or higher block | ||
| 1 Or more areas not completely revascularized | ||
| Uncontrolled diabetes (A1C ≥8.0%) | ||
| Dialysis | ||
| Patient requests 36 sessions | ||
| Recent or current substance abuse |
Abbreviations: A1C, glycated hemoglobin; CABG, coronary artery bypass grafting; CHF, congestive heart failure; EF, ejection fraction; IABP, intra-aortic balloon pump.
All characteristics must be present for patients to remain in the low-risk category.
Patients not fitting into either the low- or high-risk will be placed in the moderate-risk category.
Only 1 characteristic must be present to place a patient in the high-risk category.
Statistics
Cardiac rehabilitation attendance was assessed as both binary (perfect vs nonperfect attendance) and as counts (number of sessions attended). Each measure of attendance was used as the primary predictor in 2 iterations of the following model. One-year cardiac readmission counts were modeled via Poisson regression adjusting for age, sex, race, and number of cardiac rehabilitation sessions assigned.
Results
A total of 400 patients were included in the study. The cohort was predominantly male (68%) and Caucasian (84%). Baseline clinical and demographic data are shown in Table 2.
Table 2.
Patient Demographic and Clinical Data.a
| Cohort (400) | 18 Sessions (136) | 24 Sessions (95) | 36 Sessions (116) | Sessions Unassigned (53) | P Value | |
|---|---|---|---|---|---|---|
| Age | 64 ± 12 | 62 ± 11 | 65 ± 11 | 66 ± 12 | 61 ± 12 | .009 |
| Female | 128 (32%) | 43 (32%) | 33 (35%) | 35 (30%) | 17 (32%) | .91 |
| Race | ||||||
| Caucasian | 337 (84%) | 118 (87%) | 89 (94%) | 92 (79%) | 38 (72%) | .001 |
| African American | 27 (7%) | 6 (4%) | 1 (1%) | 13 (11%) | 7 (13%) | .004 |
| Asian | 10 (3%) | 2 (1%) | 1 (1%) | 4 (4%) | 3 (6%) | .26 |
| Hispanic | 5 (1%) | 1 (1%) | 1 (1%) | 1 (1%) | 2 (4%) | .36 |
| American Indian/Alaskan | 2 (<1%) | 0 (0%) | 2 (2%) | 0 (0%) | 0 (0%) | .09 |
| Unavailable | 19 (5%) | 9 (7%) | 1 (1%) | 6 (5%) | 3 (6%) | .25 |
| Referral diagnosis | ||||||
| Angina | 164 (41%) | 76 (56%) | 46 (49%) | 19 (16%) | 23 (43%) | <.00001 |
| S/P cardiac procedures | 111 (28%) | 28 (21%) | 25 (26%) | 45 (39%) | 13 (24%) | .012 |
| Acute MI | 103 (26%) | 29 (21%) | 23 (24%) | 39 (34%) | 12 (23%) | .13 |
| CHF | 12 (3%) | 1 (<1%) | 0 (0%) | 9 (8%) | 2 (4%) | .002 |
| CAD | 3 (1%) | 1 (<1%) | 0 (0%) | 1 (<1%) | 1 (2%) | .64 |
| Arrhythmia | 2 (<1%) | 1 (<1%) | 1 (1%) | 0 (0%) | 0 (0%) | .66 |
| Ischemic cardiomyopathy | 2 (<1%) | 0 (0%) | 0 (0%) | 1 (<1%) | 1 (2%) | .31 |
| Cardiomyopathy | 1 (<1%) | 0 (0%) | 0 (0%) | 1 (<1%) | 0 (0%) | .48 |
| Dissection | 1 (<1%) | 0 (0%) | 0 (0%) | 1 (<1%) | 0 (0%) | .48 |
| Insulin pump status | 1 (<1%) | 0 (0%) | 0 (0%) | 0 (0%) | 1 (2%) | .08 |
| Smoker | ||||||
| Yes | 37 (9%) | 14 (10%) | 4 (4%) | 8 (7%) | 11 (21%) | .006 |
| No | 215 (54%) | 70 (52%) | 49 (52%) | 66 (57%) | 30 (57%) | .77 |
| Unknown | 148 (37%) | 52 (38%) | 42 (44%) | 42 (36%) | 12 (23%) | .07 |
| Body mass index (155) | 30.6 ± 6.4 | 30.1 ± 6 | 33.3 ± 6.9 | 29.9 ± 5.8 | 29.2 ± 6.8 | .04 |
| Systolic blood pressure (161) | 129 ± 20 | 130 ± 19 | 132 ± 19 | 128 ± 21 | 127 ± 18 | .74 |
| Diastolic blood pressure (161) | 71 ± 12 | 74 ± 12 | 73 ± 13 | 69 ± 12 | 72 ± 15 | .22 |
| GFR (288) | 64 ± 14 | 67 ± 11 | 64 ± 13 | 61 ± 17 | 68 ± 12 | .01 |
| LDL (348) | 96 ± 40 | 101 ± 42 | 104 ± 46 | 85 ± 34 | 91 ± 33 | .003 |
| HDL (359) | 42 ± 12 | 43 ± 13 | 43 ± 9 | 42 ± 13 | 39 ± 9 | .2 |
| Triglycerides (357) | 143 ± 80 | 144 ± 78 | 147 ± 87 | 136 ± 85 | 147 ± 61 | .76 |
| HgB A1C (153) | 6.7 ± 1.4 | 6.5 ± 1.1 | 6.3 ± 0.9 | 6.9 ± 1.7 | 7.1 ± 1.4 | .08 |
| 1-Year mortality | 8 (2%) | 1 (0.7%) | 4 (4.2%) | 1 (0.8%) | 2 (3.8%) | .16 |
Abbreviations: CAD, coronary artery disease; CHF, congestive heart failure; GFR, glomerular filtration rate; HDL, high-density lipoprotein; HgB A1C, glycated hemoglobin; LDL, low-density lipoprotein; MI, myocardial infarction.
The data are representative of all 400 patients, unless provided in parentheses. Categorical variables are presented as number (percentage). Continuous variables are presented as mean ± SD.
The primary analysis cohort (Poisson regression) includes 347 patients assigned to either 18, 24, or 36 sessions of cardiac rehabilitation. At 1 year, 135 patients (39%) had at least 1 cardiac readmission and 155 patients (45%) had at least 1 all-cause readmission. These patients were assigned an average of 26 ± 8 cardiac rehabilitation sessions and attended 21 ± 10 sessions. There were 227 (65%) patients who completed all assigned cardiac rehabilitation sessions.
The primary result of our study is that controlling for age, sex, race, and number of cardiac rehabilitation sessions assigned, every additional session completed was associated with a 1.75% lower incidence rate of 1-year cardiac readmission (P = .01) and a 2.0% lower incidence rate of all-cause hospital readmission (P = .0016). Conversely, every missed appointment was associated with a 1.79% higher incidence rate of cardiac readmission (P = .01) and a 2.0% higher incidence rate of all-cause hospital readmission (P = .0016). Patients with nonperfect attendance had a 39% higher incidence rate of cardiac readmission (P = .02) and a 45% higher incidence rate of all-cause hospital readmission at 1 year than patients with perfect cardiac rehabilitation attendance (P = .0061).
Patients assigned to 36 sessions had significantly higher cardiac and all-cause readmission rates at 1 year in comparison to those assigned 18 or 24 sessions. Controlling for adherence, age, sex, and race, those assigned 18 and 24 sessions, respectively, had a 36% and 32% lower 1-year cardiac readmission rate than those assigned 36 sessions (P = .01). As shown in Table 2, patients assigned 36 sessions were older than those assigned 18 sessions. The patients assigned 36 sessions also had a significantly lower glomerular filtration rate (GFR) and low-density lipoprotein (LDL) than those assigned 18 or 24 sessions.
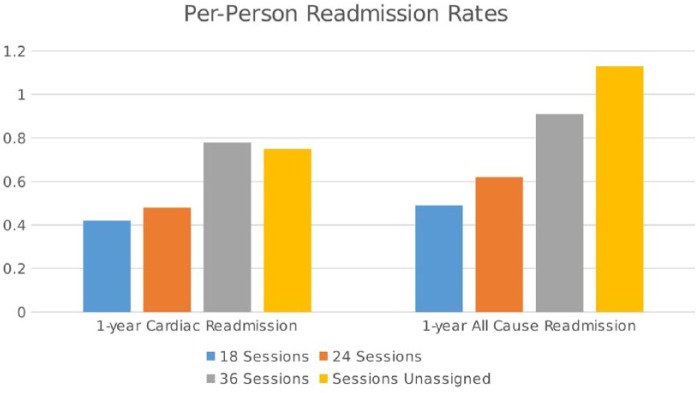
Cardiac and all-cause readmission was significantly lower at 1 year for those with perfect attendance compared with those with at least 1 missed session, regardless of whether they were assigned 18, 24, or 36 sessions (Figure 1). Overall, cardiac and all-cause readmission rates for patients with perfect attendance were 0.47 and 0.56 readmissions per person, whereas for those with nonperfect attendance, the rates were 0.73 and 0.88 readmissions per person. There was no significant difference in the number of cardiac rehabilitation sessions assigned between those with perfect attendance and those with nonperfect attendance.
Figure 1.
One-year, per-person cardiac and all-cause readmission by attendance.
The session’s unassigned group attended an average of 13 ± 9 sessions. This group had a similar cardiac readmission rate as those assigned 36 sessions and had the highest all-cause readmission rate (Figure 1). The all-cause readmission rate exceeded 1 (1.13) readmission per person in a year. This group had a significantly higher smoking rate than the other 3 groups and had the highest glycated hemoglobin (HgB A1C). The mortality rate was 2% at 1 year, with no statistical difference between the groups. There was no statistical relationship between mortality and cardiac rehabilitation attendance.
A secondary finding was that the small African American cohort (n = 20) had an 80% higher incidence rate of cardiac readmission (P = .01) and a 70% higher incidence of all-cause readmission (P = .0153) at 1 year than Caucasians. African Americans also demonstrated a higher smoking rate (P = .05), a lower GFR (P = .004), and a higher HgB A1c (P = .001). In the Poisson regression models, age and sex were not significantly associated with 1 year cardiac readmission.
Discussion
In the present study, we found that each additional session of cardiac rehabilitation attended was associated with significant reductions in both cardiac and all-cause readmission rates, and perfect attendance was associated with significantly less cardiac and all-cause readmissions when compared with nonperfect attendance. Although these findings support those of previous studies, the recognition of the significant impact of each individual cardiac rehabilitation session on readmission rates is novel.
Martin et al12 evaluated 5886 patients referred for cardiac rehabilitation after angiography. Patients were divided into 3 groups: never enrolled in cardiac rehabilitation, did not complete cardiac rehabilitation, and completed cardiac rehabilitation. Those who completed cardiac rehabilitation had significantly better survival as well as significantly lower rates of cardiac hospitalization, all-cause hospitalization, and emergency room visits. In addition, each session of cardiac rehabilitation attended was associated with a 1% decrease in mortality.
Beauchamp et al10 evaluated survival 14 years after cardiac rehabilitation referral. Patients who attended cardiac rehabilitation demonstrated half the risk of death at 14 years as compared with those who did not attend. In addition, the mortality risk for patients who completed <25% of their assigned sessions was double that of those who completed ≥75% of assigned sessions.
Hammill et al9 reviewed Medicare claims data for 30 161 patients referred to cardiac rehabilitation. After the first 36 weeks, they compared survival rates according to the number of cardiac rehabilitation sessions attended. Patients attending ≥36 sessions demonstrated significantly better survival than those attending ≤24. The highest mortality was consistently among those who attended ≤12 sessions.
The above-referenced studies all identified a strong relationship between cardiac rehabilitation adherence and outcomes, demonstrating a 1% decrease in mortality with each session attended.12 Our study finds that a similar relationship exists between each cardiac rehabilitation session attended and readmission. These findings further support the notion that there is a dose response in cardiac rehabilitation, with better attendance being associated with improved patient outcomes.
A common weakness of all these studies, including ours, is the inability to define the impact of selection bias. This bias has been referred to as the healthy-adherer effect.16 The patients who attend cardiac rehabilitation regularly are also those who adhere to their medications, have lower smoking rates, eat healthier diets, exercise more regularly, and have a lower body mass index, and thus, have better clinical outcomes.16 Patients who attend cardiac rehabilitation regularly are also those who may be more likely to adhere to their medications. These behaviors undoubtedly influence an individual’s risk for readmission. This selection bias ultimately makes it difficult to discern the impact of cardiac rehabilitation per se on outcomes versus the impact of healthier patients attending cardiac rehabilitation, thus improving the cardiac rehabilitation outcomes.
Nevertheless, stressing the prognostic importance of cardiac rehabilitation adherence to patients seems warranted. The association between cardiac rehabilitation attendance and readmission provides a compelling argument for practitioners faced with noncompliant patients or those questioning the value of cardiac rehabilitation. Being able to equate each cardiac rehabilitation session attended with a 2% decrease in readmission may be an incentive for some patients to improve their adherence pattern or mitigate their questions regarding the value of cardiac rehabilitation.
Readmission rates for cardiac patients are often some of the highest reported.17 Improving both referral and adherence to cardiac rehabilitation may provide an avenue toward reducing these residually high readmission rates. This may provide a novel perspective because readmission rates are often a metric used in the grading of hospitals. These grades ultimately affect hospital reputation and may even influence reimbursement rates.18
Moreover, patients assigned to 36 sessions in our cohort had significantly higher cardiac and all-cause readmission rates at 1 year than those assigned 18 or 24 sessions. Although this seems counterintuitive to the idea that more cardiac rehabilitation translates to better outcomes, those assigned to 36 sessions appear to have had increased morbidities in comparison to the other 2 groups and demonstrated decreased kidney function. In addition, patients assigned to 36 sessions were older than those assigned to 18 sessions. The patients assigned to 36 sessions had a referral diagnosis of congestive heart failure more often than the other 2 groups. The patients assigned to 36 sessions had significantly lower LDL than the other 2 groups, possibly as a result of more aggressive statin therapy for secondary prevention. Thus, it appears that those assigned to 36 sessions had increased morbidities as compared with the other 2 groups.
The African American population within our cohort (n = 20) had significantly higher readmission rates than our Caucasian population. However, the African American group also demonstrated a significantly higher smoking rate, lower GFR, and higher HgB A1c. Although these may be potential contributors to their increased readmission rates, our African American cohort was small (n = 20), and smoking data were incomplete, representing a potential confounding variable. Nevertheless, this may signify the need for more targeted counseling in African American cardiac rehabilitation participants aimed at smoking cessation, blood pressure management, diabetes management, or combinations thereof.
Limitations
Our report is an observational study of retrospective data. We cannot exclude all potential confounding variables affecting the readmission rates. We also did not include any temporal information in our analysis, and thus, the timing of readmissions relative to cardiac rehabilitation participation may also represent another potential confounder. We are also unable to account for comorbid conditions that could have adversely affected readmission, which includes cardiorespiratory fitness (peak metabolic equivalent) and left ventricular ejection fraction. Smoking data were incomplete in the electronic medical record, which limits our ability to accurately assess statistical relationships.
For the majority of the patients in the sessions unassigned group (n = 37), it was unclear how many cardiac rehabilitation sessions were assigned. This is unfortunately a result of the retrospective data collection. This group had the highest all-cause readmission rate and a cardiac readmission similar to those assigned 36 sessions. The session’s unassigned group attended the fewest cardiac rehabilitation sessions. They also had the poorest diabetes control and highest smoking rate, with the caveat that our smoking data are incomplete. These findings are suggestive that this group was the least compliant in our cohort, which may in part explain their high readmission rates.
Although the association between cardiac rehabilitation attendance and readmission was significant, this does not imply a cause-and-effect relationship. Future studies that closely evaluate the timing of missed cardiac rehabilitation sessions and hospital readmission would provide better insight into the role of cardiac rehabilitation in reducing readmission rates.
Conclusion
Attending individual cardiac rehabilitation sessions was significantly associated with reduced subsequent cardiac and all-cause readmission rates, whereas perfect attendance was associated with the lowest cardiac and all-cause readmission rates. These findings may reflect, at least in part, the salutary effect of exercise-based cardiac rehabilitation, the healthy adherer phenomenon, or both.
Acknowledgments
This study was funded by a Discovery Grant from the HealthPartners Institute for Education and Research, Bloomington, MN.
Footnotes
Authors’ Note: All authors have read and approved the manuscript.
References
- 1. Lavie C, Milani R, Littman A. Benefits of cardiac rehabilitation and exercise training in secondary coronary prevention in the elderly. J Am Coll Cardiol. 1993;22:678-683. [DOI] [PubMed] [Google Scholar]
- 2. Critchley JA, Capewell S. Mortality risk reduction associated with smoking cessation in patients with coronary heart disease: a systematic review. JAMA. 2003;290:86-97. [DOI] [PubMed] [Google Scholar]
- 3. Aldana SG, Whitmer WR, Greenlaw WR, et al. Cardiovascular risk reductions associated with aggressive lifestyle modification and cardiac rehabilitation. Heart Lung. 2003;32:374-382. [DOI] [PubMed] [Google Scholar]
- 4. Lavie CJ, Arena R, Franklin BA. Cardiac rehabilitation and healthy life-style interventions rectifying program deficiencies to improve patient outcomes. J Am Coll Cardiol. 2016;67:13-15. [DOI] [PubMed] [Google Scholar]
- 5. Sandesara PB, Lambert CT, Gordon NF, et al. Cardiac rehabilitation and risk reduction time to “rebrand and reinvigorate”. J Am Coll Cardiol. 2016;65:389-395. [DOI] [PubMed] [Google Scholar]
- 6. Anderson L, Oldridge N, Thompson DR, et al. Exercise-based cardiac rehabilitation for coronary heart disease Cochrane systematic review and meta-analysis. J Am Coll Cardiol. 2016;67:1-12. [DOI] [PubMed] [Google Scholar]
- 7. Suaya JA, Shepard DS, Normand SL, Ades PA, Prottas J, Stason WB. Use of cardiac rehabilitation by Medicare beneficiaries after myocardial infarction or coronary bypass surgery. Circulation. 2007;116:1653-1662. [DOI] [PubMed] [Google Scholar]
- 8. Taylor RS, Brown A, Ebrahim S, et al. Exercise-based rehabilitation for patients with coronary heart disease: systematic review and meta-analysis of randomized controlled trials. Am J Med. 2004;116:682-692. [DOI] [PubMed] [Google Scholar]
- 9. Hammill BG, Curtis LH, Schulman KA, Whellan DJ. Relationship between cardiac rehabilitation and long-term risks of death and myocardial infarction among elderly Medicare beneficiaries. Circulation. 2010;121:63-70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Beauchamp A, Worcester M, Ng A, et al. Attendance at cardiac rehabilitation is associated with lower all-cause mortality after 14 years of follow-up. Heart. 2013;99:620-625. [DOI] [PubMed] [Google Scholar]
- 11. Sanderson BK, Bittner V. Women in cardiac rehabilitation: outcomes and identifying risk for dropout. Am Heart J. 2005;150:1052-1058. [DOI] [PubMed] [Google Scholar]
- 12. Martin B-J, Hauer T, Arena R, et al. Cardiac rehabilitation attendance and outcomes in coronary artery disease patients. Circulation. 2012;126:677-687. [DOI] [PubMed] [Google Scholar]
- 13. Weingarten MN, Salz KA, Thomas RJ, Squires RW. Rates of enrollment for men and women referred to outpatient cardiac rehabilitation. J Cardiopulm Rehabil Prev. 2011;31:217-222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Dunlay SM, Pack QR, Thomas RJ, Killian JM, Roger VL. Participation in cardiac rehabilitation, readmissions, and death after acute myocardial infarction. Am J Med. 2014;127:538-546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Borg G. Borg’s Perceived Exertion and Pain Scales. Leeds, UK: Human Kinetics; 1998. [Google Scholar]
- 16. Alter DA, Zagorski B, Marzolini S, Forhan M, Oh PI. On-site programmatic attendance to cardiac rehabilitation and the healthy-adherer effect. Eur J Prev Cardiol. 2015;22:1232-1246. [DOI] [PubMed] [Google Scholar]
- 17. Hines AL, Barrett ML, Jiang HJ, Steiner CA. Conditions With the Largest Number of Adult Hospital Readmissions by Payer, 2011. Rockville, MD: Agency for Healthcare Research and Quality; 2014. HCUP Statistical Brief #172. [PubMed] [Google Scholar]
- 18. Hospital Readmissions Reduction Program. Affordable Care Act, Subpart 1 of 42 CRT part 412 Sect 1886(q) (2012). [Google Scholar]