Abstract
Objectives
Sexual and physical trauma and substance use are intersecting risks for HIV among young women. This study assesses the feasibility, acceptability and preliminary effects of a novel trauma-informed substance use and sexual risk reduction intervention for young South African women.
Design
A single arm feasibility test and qualitative interviews of participants.
Participants
Sixty women, between 18 and 25 years of age, who reported trauma exposure, substance use and recent condom-less sex were recruited. Twenty participants were randomly selected for qualitative interviews.
Intervention
A six-session group-based intervention.
Main outcome measures
We examined the proportion of women who provided consent, completed counselling and were retained in the study. Qualitative interviews explored intervention acceptability. Preliminary effects of the intervention on substance use, mental health (depression, psychological distress and trauma symptoms) and sexual risk outcomes (STI symptoms, number of partners and condomless sex) were explored.
Results
Of the 66 eligible women, 91% were enrolled. Intervention completion rates were low; 35% attended all sessions. On average, participants attended four sessions (M=3.8, SD=1.3). A 93% follow-up rate was achieved at the 3-month endpoint. In this single group design, reductions in the proportion of participants who tested positive for methamphetamine, cannabis and methaqualone were observed at the 3-month endpoint. Symptoms of depression, psychological distress and trauma; number of STI symptoms; and number of sexual partners also decreased. Outcomes were similar for participants who completed up to four and those who completed five or more sessions. Participants thought the intervention was highly beneficial and proposed modifications to enhance acceptability.
Conclusions
This novel intervention seems acceptable and holds potential benefits for trauma-exposed women who use substances. Truncating the intervention may enhance the likelihood of its implementation. The efficacy of the intervention for improving substance use, sexual risk and mental health outcomes requires testing in a controlled design.
Keywords: gender, substance use, mental health, sexual risk, low-and-middle-income country
Strengths and limitations of this study.
One of the first studies to explore the feasibility and acceptability of a trauma-informed substance use and sexual risk reduction intervention for young women.
The use of mixed methods enables triangulation of findings, increasing confidence in the results.
Qualitative interviews provide a rich description of young women’s experiences of the intervention and recommendation for intervention enhancement.
As this single-arm feasibility test lacked a comparison group, we cannot make inferences about intervention efficacy.
Background
Substance use1 and exposure to physical and sexual trauma2 are highly prevalent, intersecting risks for HIV acquisition among young women in South Africa.3 Substance use is a common coping strategy among trauma-exposed women who use substances to avoid or numb the negative emotions associated with traumatic experiences.4 5 As substance use impairs decision making that leads to inconsistent condom use,6 this coping response may increase young women’s risk for HIV. Substance use also places women in high-risk environments and fuels conflict in interpersonal relationships,7 8 increasing risk of further exposure to physical and sexual trauma9 and directly contributing to HIV risk.10 With a high incidence of HIV among young women in emerging adulthood,11 South Africa needs innovative programmes that address these syndemic risks for HIV acquisition among this vulnerable population.
Although several HIV prevention programmes reach young South African women, these generally do not focus on women who have been trauma exposed and may be using substances. Furthermore, trauma and substance use services in South Africa are provided by separate systems of care.12 13 As substance use services do not provide trauma counselling, women with histories of trauma are often reluctant to use these services and those that do tend to have poorer substance use outcomes than women without a history of physical or sexual abuse.9 14
In high-income countries, trauma-informed substance use interventions have been recommended as a means of overcoming barriers to trauma-exposed women’s use of substance use services.15 Evidence from systematic reviews suggests that this integrated approach leads to significant reductions in substance use and trauma symptoms among women with these multimorbidities.16 17 Despite global HIV prevention guidelines for adolescent girls and young women that recommend the provision of integrated mental health, substance use and HIV prevention services for young women,18 trauma-informed substance use interventions have generally not included HIV prevention components,16 reflecting a missed opportunity to address sexual safety among this highly vulnerable population. To illustrate, none of the 23 studies identified in a recent systematic review of interventions that address alcohol use, violence and sexual risk for HIV directly addressed psychological trauma and substance use coping.19 To meet the intervention needs of this unique population, we developed a trauma-informed substance use and sexual risk reduction intervention for South African women in emerging adulthood.
This study aimed to: (1) assess the feasibility of recruiting and retaining trauma-exposed women who use substances in this intervention, (2) obtain preliminary information on the intervention’s substance use, mental health and sex risk outcomes and (3) explore participants’ perceptions of the acceptability of the intervention. This information is needed to guide decision making about the future of the programme and whether it is worth investing in a randomised controlled trial (RCT) to establish its efficacy.
Methods
This manuscript follows the Consolidated Standards of Reporting Trials guidelines for pilot and feasibility trials20 (see online supplementary file 1). This phase I feasibility study, conducted between July 2016 and February 2017, tested a trauma-informed substance use and sexual risk reduction intervention combined with postprogramme qualitative interviews of participants.
bmjopen-2018-024776supp001.pdf (91.3KB, pdf)
Participants and procedures
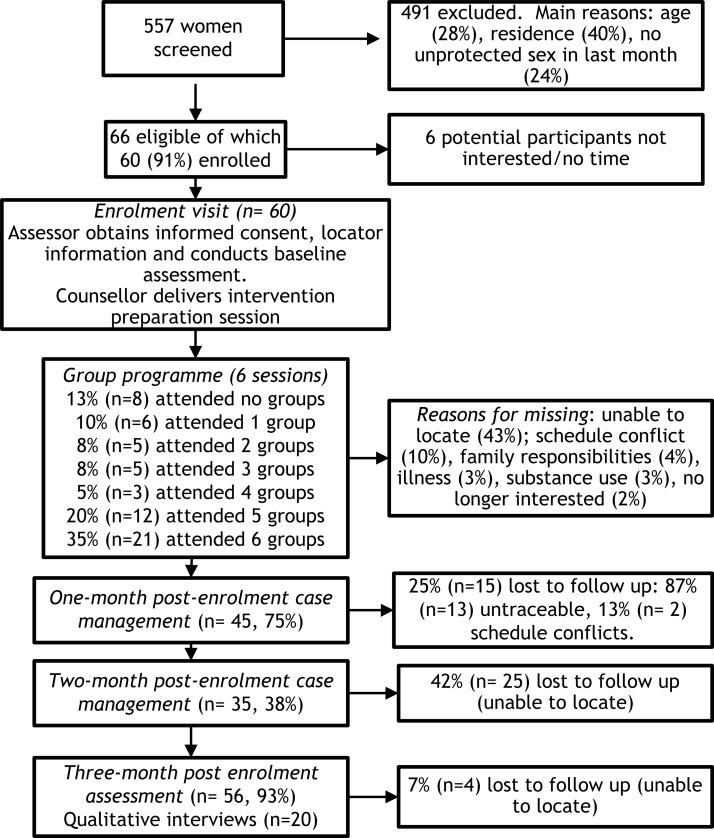
We recruited 60 young women from two low-income, periurban communities in Cape Town, South Africa. The estimated population size of these communities combined is more than 1.5 million people, of which 99% identify as Black African and are isiXhosa speaking, about 40% are unemployed and over half live in informal dwellings or shacks. These communities have high rates of HIV (estimated prevalence is 35%) and have been identified as provincial ‘hotspots’ for substance use and violent crime including violence against women and children.21 22From July 2016 to September 2016, fieldworkers used established community-based street outreach techniques23 to identify potential participants to whom they described the study before requesting verbal consent for eligibility screening. This involved the distribution of marketing flyers and posters in places frequented by women and approaching potential participants in locations frequented by women who use substances. Women were eligible if they were between 18 years and 25 years; lived in the target communities; and reported lifetime experiences of sexual or physical abuse, using at least one illicit drug or heavy episodic drinking (defined as four or more alcoholic drinks on one occasion) weekly for the past 3 months and condomless sex in the past 3 months. Fieldworkers gave eligible women more information about the study and invited those who were eligible and interested to an enrolment appointment (see figure 1).
Figure 1.
Participant flow chart.
At the enrolment appointment, fieldworkers rescreened women to verify study eligibility and obtained their informed consent before collecting contact information, administering the baseline behavioural assessment and conducting rapid biological testing for recent drug use, pregnancy and HIV. All data were collected through interviewer-administered questionnaires. The Medical Diagnostech drug test and NHMed tests were used to test urine samples for methamphetamine, cocaine, opiates, THC (cannabis) and methaqualone use in the past 72 hours. Following standard HIV testing and counselling, two rapid finger-prick tests were used to test for HIV (Unigold and Determine Rapid Tests). If either test was reactive or indeterminate, a confirmatory Tri-line HIV-1/2 Rapid Test was performed. A participant was considered HIV positive when at least two tests were reactive. Participants were also breathalysed to assess recent alcohol use. Immediately after this assessment, participants received information about the intervention programme, they developed a personalised action plan and appointments were scheduled for the first available group session. Participants had 3 weeks to complete the intervention programme. All participants were offered two case management visits (at 1 month and 2 months postenrolment) either at the project site or in the community. The purpose of these visits was to enquire about the participant’s barriers to accessing sexual and reproductive or mental health services, to provide referrals to care and to remain in contact with the participants for retention purposes. Participants were tracked for a 3-month postenrolment follow-up appointment at which time participants were reconsented, the behavioural assessment was readministered and they were retested for recent substance use, HIV and pregnancy. In addition, 20 participants were randomly selected for a qualitative in-depth interview of their perceptions of the acceptability and utility of the programme. These interviews, conducted by an experienced qualitative researcher in isiXhosa (the primary language spoken by participants), occurred after their 3-month assessment and lasted approximately 45 min. Interviews were audio-recorded and transcribed verbatim before being translated into English using standard forward-translation and back-translation techniques. All study-related activities (assessments and the intervention) occurred in private rooms at an established clinical research site located within a nearby local community.
After each contact, participants were given referrals to additional substance use and trauma counselling and appropriate sexual and reproductive health services. Participants received grocery vouchers for completing the baseline and follow-up appointments and the qualitative interviews as well as transport to these appointments. Participants were not incentivised to attend the intervention sessions, although transport and refreshments were provided.
Intervention
We developed a novel trauma-informed substance use and sexual risk reduction intervention for young South African women, known as the trauma-informed Women’s Health Coop (WHC). The process of developing this intervention has been described elsewhere.24 The intervention comprises six open-group sessions delivered over a 2-week period. As such, participants who missed sessions had the opportunity to make up these sessions by attending another group. As trauma-exposed women using substances in our formative work had expressed their preference for an intensive programme of a brief duration, the intervention was delivered over a 2-week period.24 Groups generally consisted of four to eight women.
The intervention is grounded in feminist empowerment theory and cognitive–behavioural therapy, which has strong evidence in support of its effectiveness for treating trauma and substance use disorders.17 25 The intervention provides psychoeducation about substance use, trauma and HIV; cognitive-behavioural strategies for identifying emotional triggers for substance use, emotional regulation, adaptive coping and problem solving, and managing cravings; conflict resolution and sexual safety skills training; and self-care strategies for sustaining recovery and creating a meaningful life. Participants were given opportunities for skills rehearsal and a handout summarising session content and containing exercises for further skills practice. At the end of the programme, participants review their personalised action plan, which was rereviewed during case management activities that occurred 1 month and 2 months after enrolment.
Counsellor training and supervision
A registered psychological counsellor, fluent in isiXhosa, was trained to deliver the programme. She received 2 weeks of training in the intervention that included an assessment of her competence to deliver the intervention. The training curriculum was manualised. We audio-recorded the group sessions and reviewed a random sample for fidelity. During weekly supervision, findings from these fidelity checks were used to provide feedback to the counsellor on how to improve intervention quality.
Measures
Sociodemographic variables
Sociodemographic variables included participants’ employment status (employed vs unemployed), relationship status (single vs in a relationship) and HIV status (positive or negative). Type of trauma exposure was assessed using items from the Trauma History questionnaire.26 A positive response to any of the three items on sexual abuse was classified as sexually abused; any of the three physical abuse questions as physically abused; and at least one physical and one sexual abuse item as both physically and sexually abused.
Substance use outcomes
Change in recent drug use was assessed through results of biological testing (positive vs negative). Questions on the number of days of heavy episodic drinking (defined as four or more drinks on one occasion), methamphetamine, cannabis and methaqualone use in the past 30 days assessed change in frequency of substance use.
Mental health outcomes
The 20-item Centre for Epidemiologic Studies Depression Scale (CES-D) assessed change in depressive symptomatology.27 For this scale, a cut-off score ≥16 indicates probable depression.28 The 10-item Kessler Psychological Distress Scale (K-10) measured change in symptoms of psychological distress. This scale has been shown to have good psychometric properties in South African studies, with a cut-off score ≥20 indicating psychological distress.29 The 10-item Drug Abuse Treatment Outcome Study post-traumatic stress disorder scale,30 adapted for use in South African populations, assessed changes in trauma symptoms. The 19-item Medical Outcomes Study Social Support Survey assessed change in perceived social support. This scale has excellent psychometric properties.31
Sexual risk outcomes
Change in condom use was assessed through a question on condom use at last sexual encounter. Questions on the number of sexual partners and number of symptoms of sexually transmitted infections (STIs) in the past month also assessed change in sexual risk behaviour.
Patient and public involvement
The intervention and the design of the feasibility test were informed by focus group discussions with potential service users and interviews with providers of substance use, HIV and psychological trauma services.23 Our community advisory board that comprises representatives from the Department of Health, Department of Social Development, non-government organisations and service user organisations contributed to the design of the study and the interpretation of findings.
Analyses
We used SPSS V.25.0 to describe the proportion of participants who completed the intervention and retention at 3-month follow-up. We used χ2 tests (or Fisher’s exact tests if cell sizes were small) for categorical and t-tests for continuous variables to explore whether participant attributes were associated with intervention and study completion. χ2 tests explored change from baseline to 3-month follow-up on the categorical outcome variables. Paired sample t-tests were used to examine whether there was change on the outcomes from baseline to follow-up. Results are presented as differences in mean scores with 95% CIs. All testing was two sided, and a significance level of 0.05 was used.
The framework approach32 was used for qualitative data analysis. Two people coded the interview transcripts using NVivo V.11; they met regularly to compare notes and resolved discrepancies through discussion. A third person was not needed to break coding ties. No new codes emerged after coding half the transcripts, implying thematic saturation. Intercoder reliability was high, with a Kappa score of 0.93.
Results
Feasibility of patient recruitment and retention
Field staff screened 557 young women for potential study eligibility of which 66 met the study’s eligibility criteria, the majority were ineligible based on their age (older), residence and because they did not report recent unprotected sex. Almost three-quarters (72.6%) of women screened reported trauma exposure and more than half (56.9%) reported heavy alcohol or drug use. Of the eligible women, 60 (90.7%) were interested in study participation and were enrolled (see figure 1). Table 1 describes the sociodemographic and clinical characteristics of the sample. Most participants (93.3%) had never received substance use or trauma care, and 85.0% reported not knowing where to go for these services. Most (86.7%) participants had K-10 scores of ≥20 indicating psychological distress and 85.0% of participants had CES-D scores of ≥16 indicating probable depression.
Table 1.
Baseline demographic and clinical characteristics of the overall sample (n=60) and by treatment completion status
| Variable | Overall | Treatment completion | ||
| Yes (n=21) | No (n=39) | P value | ||
| Sociodemographic variables | ||||
| In a relationship, N (%) | 55 (91.7) | 20 (95.2) | 35 (89.7) | 0.649 |
| Employment (no), N (%) | 55 (91.7) | 20 (95.2) | 35 (89.7) | 0.649 |
| HIV status (positive), N (%) | 28 (46.7) | 9 (42.9) | 19 (48.7) | 0.788 |
| Newly diagnosed as HIV positive (yes), N (%) | 10 (35.7) | 1 (11.1) | 9 (47.4) | 0.06 |
| Sexual abuse (yes), N (%) | 41 (68.3) | 13 (61.9) | 28 (71.8) | 0.562 |
| Physical abuse (yes), N (%) | 55 (91.7) | 19 (90.5) | 36 (92.3) | 0.602 |
| Sexual and physical abuse (yes), N (%) | 34 (56.7) | 10 (47.6) | 24 (61.5) | 0.414 |
| Substance use outcomes | ||||
| Days of heavy drinking in past month, M (SD) | 8.2 (6.4) | 8.1 (6.0) | 8.3 (6.7) | 0.906 |
| Days of cannabis use in past month, M (SD) | 11.4 (11.9) | 10.4 (11.7) | 11.8 (12.1) | 0.715 |
| Days of methamphetamine in past month, M (SD) | 18.4 (11.6) | 13.5 (13.2) | 20.2 (10.7) | 0.227 |
| Days of methaqualone use in past month, M (SD) | 14.0 (11.9) | 11.1 (13.1) | 15.1 (11.6) | 0.498 |
| Cannabis positive (biological), N (%) | 30 (50.0) | 9 (42.9) | 21 (53.8) | 0.589 |
| Methamphetamine positive (biological), N (%) | 27 (45.0) | 8 (38.1) | 19 (48.7) | 0.587 |
| Methaqualone positive (biological), N (%) | 29 (48.3) | 8 (38.1) | 21 (53.8) | 0.287 |
| Opiate positive (biological), N (%) | 4 (6.7) | 0 (0.0) | 4 (6.7) | 0.287 |
| Mental health outcomes | ||||
| CES-D, M (SD) | 26.1 (9.5) | 27.4 (11.1) | 25.4 (8.6) | 0.489 |
| K-10, M (SD) | 25.7 (6.8) | 25.1 (7.6) | 25.9 (6.5) | 0.693 |
| Trauma symptom, M (SD) | 33.6 (5.6) | 34.9 (7.6) | 31.9 (7.4) | 0.154 |
| MOS-SSS, M (SD) | 60.1 (13.6) | 59.2 (14.4) | 61.3 (13.4) | 0.593 |
| Sexual risk outcomes | ||||
| Number of partners in last month, M (SD) | 1.7 (1.5) | 1.5 (0.7) | 1.9 (1.8) | 0.204 |
| Condom use last sex (yes), N (%) | 10 (16.9) | 2 (10.0) | 8 (20.5) | 0.469 |
| Number of STI symptoms in last month, M (SD) | 1.2 (0.9) | 1.2 (0.6) | 0.9 (1.1) | 0.159 |
CES-D, Centre for Epidemiologic Studies Depression Scale; K-10, 10-item Kessler Psychological Distress Scale; MOS-SSS, Medical Outcomes Study Social Support Survey; STI, sexually transmitted infection.
Of the 60 enrolled participants, 35.0% completed the intervention. On average, participants attended four of the six group sessions (M=3.8; SD=1.3), with 13.3% (n=8) not attending any group sessions. For the case management visits, 45 participants (75%) received a case management visit 1 month after enrolment and 35 (38%) received a case management visit 2 months postenrolment. Figure 1 provides reasons for missed appointments. The association between being newly diagnosed with HIV and not completing treatment approached significance; no other baseline characteristics were associated with treatment completion (table 1). Fifty-six participants (93.3%) completed the 3-month follow-up assessment. Figure 1 provides reasons for attrition. There were no baseline differences on sociodemographic or clinical characteristics between participants who completed the 3-month appointment and those who did not. Although not significant, 97% (n=34) of the 35 participants who received case management completed the 3-month assessment compared with 88% (n=22) of the 25 participants without case management.
Outcomes
Participants reduced the frequency of past month heavy episodic drinking (t=2.9 [df=47], p=0.006), methamphetamine use (t=2.7 [df=25], p=0.012) and cannabis use (t=3.4 [df=43], p=0.001) from the baseline to 3-month assessment (table 2). The proportion of participants who tested positive for methamphetamine (p<0.0001), cannabis (p<0.0001) and methaqualone (p<0.0001) decreased significantly from baseline to 3-month follow-up (table 2).
Table 2.
Change in substance use, mental health and sex risk outcomes for the overall sample (n=56) and by intervention exposure
| Outcomes | Overall sample (n=56) | Intervention dosage of up to and including four sessions (n=23) | Intervention dosage of five or more sessions (n=33) | ||||
| Baseline | 3-month follow-up | Baseline to follow-up Mean difference (95% CI) |
Baseline | 3-month follow-up | Baseline | 3-month follow-up | |
| Substance use outcomes | M (SD) | M (SD) | M (SD) | M (SD) | M (SD) | M (SD) | |
| Days of heavy drinking in past month | 8.4 (6.1) | 5.3 (6.9) | 3.2 (0.9 to 5.4)* | 8.8 (6.7) | 6.7 (8.2) | 8.1 (5.8) | 4.3 (5.8)* |
| Days of cannabis use in past month | 12.3 (12.4) | 6.0 (9.2) | 6.3 (2.6 to 9.9)* | 14.1 (13.5) | 4.7 (7.7)* | 11.1 (11.5) | 6.7 (9.8)* |
| Days of methamphetamine in past month | 19.5 (11.0) | 11.7 (11.3) | 7.8 (1.8 to 13.7)* | 22.0 (9.3) | 9.2 (11.4)* | 17.0 (12.3) | 14.2 (11.0) |
| Days of methaqualone in past month | 14.9 (11.8) | 9.9 (11.4) | 4.9 (−0.7 to 10.5) | 15.3 (10.6) | 7.6 (9.5)* | 14.4 (13.6) | 12.5 (13.2) |
| Cannabis positive (biological), N (%) | 26 (46.4) | 21 (37.5%)* | − | 13 (56.5) | 11 (47.8)* | 13 (39.4) | 10 (30.3)* |
| Methamphetamine positive (biological), N (%) | 25 (44.6) | 20 (35.7%)* | − | 11 (47.8) | 9 (39.1)* | 14 (42.4) | 11 (33.3)* |
| Methaqualone positive (biological), N (%) | 27 (48.2) | 21 (37.5)* | − | 13 (56.5) | 10 (43.5)* | 14 (42.4) | 11 (33.3)* |
| Mental health outcomes | |||||||
| CES-D score | 26.3 (9.6) | 17.7 (7.3) | 8.5 (5.3 to 11.7)* | 24.7 (8.9) | 17.3 (7.5)* | 27.5 (10.1) | 18.1 (7.2)* |
| K-10 score | 25.7 (6.9) | 17.8 (7.3) | 7.9 (5.6 to 10.3)* | 25.4 (7.2) | 17.6 (8.3)* | 25.9 (6.8) | 17.7 (6.5)* |
| Trauma symptom score | 32.9 (7.6) | 21.7 (8.6) | 11.2 (8.8 to 13.6)* | 33.9 (3.5) | 22.2 (7.8)* | 33.4 (6.7) | 21.7 (9.2)* |
| MOS-SSS | 60.6 (14.1) | 63.5 (15.7) | −2.8 (−6.7 to 1.1) | 60.5 (14.5) | 63.8 (16.6) | 60.8 (14.1) | 63.3 (15.3) |
| Sex risk outcome | |||||||
| Number of partners in last month | 1.7 (1.1) | 1.0 (0.4) | 0.6 (0.3 to 1.1)* | 2.1 (2.2) | 1.2 (0.7)* | 1.4 (0.6) | 0.9 (0.4)* |
| Condom use at last sex, N (%) | 8 (14.5) | 25 (45.5) | − | 2 (8.7) | 10 (43.5) | 6 (18.8) | 15 (46.9) |
| STI symptoms in past month | 1.1 (0.9) | 0.2 (0.8) | 0.8 (0.5 to 1.2)* | 0.8 (1.1) | 0.3 (1.0)* | 1.3 (0.8) | 0.2 (0.6)* |
*Significant at p<0.05.
CES-D, Centre for Epidemiologic Studies Depression Scale; K-10, 10-item Kessler Psychological Distress Scale; MOS-SSS, Medical Outcomes Study Social Support Survey; STI, sexually transmitted infection.
Participants significantly reduced their CES-D (t=5.3 [df=55], p<0.0001) and K-10 (t=6.8 [df=55], p<0.0001) scores over time as well as their trauma symptom scores (t=9.4 [df=55], p<0.0001). The proportion of participants with probable depression decreased (85.7% to 53.6% χ2=3.94 [df=1], p=0.047) suggesting clinically significant improvements. Social support did not improve from baseline to 3-month time point (table 2). For sexual risk outcomes, participants reported significant reductions in the number of past month STI symptoms (t=5.7 [df=55], p<0.0001) and the number of past month sexual partners (t=3.5 [df=55], p<0.001; table 2). The proportion of participants who reported condom use at last sexual encounter increased from baseline to 3-month follow-up, although this increase was not statistically significant (p=0.069). As participants generally completed four group sessions, we explored whether there were differences in outcomes among participants who completed up to four sessions and those who completed five or six sessions. Participants who completed up to and including four sessions and participants who completed five or more sessions had similar substance use, mental health and sexual risk outcomes (table 2). We also explored whether there were differences in outcomes among participants who received at least one case management visit and those who did not participate in case management. Only participants who received case management reported reducing the frequency of past month heavy episodic drinking (t=2.1 [df=29], p=0.045) and cannabis use (t=3.4 [df=27], p=0.002) from the baseline to 3-month assessment. No other differences in outcomes were observed between these two groups.
Participants’ perceptions of the intervention
Three broad themes emerged from the qualitative data that reflect participants’ perceptions of the intervention. The first, A moment to pause, describes how the programme offered participants an opportunity to reflect on changes they wished to make. The second theme, Salient programme content, describes the intervention components that participants found most salient and useful for behaviour change. The third theme, Areas for programme strengthening, reflects participants’ recommendations for how to modify the intervention for greater acceptability.
A moment to pause
Almost all participants described how the programme offered them respite from their daily struggles. For many, this was their first opportunity to ‘share their problems with someone’ and reflect on their past experiences, current needs and future goals. Many participants felt that the intervention gave them ‘a different perspective on life’ and helped them regain hope for their future despite their troubled past:
This programme opened my eyes that I am still young, I still have a future ahead of me despite everything that has happened to me. Now I can move on and still achieve big things. (Participant 12)
The intervention also seemed to encourage participants to speak freely about their lives. Several participants described seeking trauma counselling in the past, but not following through because they felt judged and stigmatised. In contrast, participants were ‘thankful for how we were treated’ in this intervention. For many participants, the ‘respectful’ staff made them feel ‘valued’ and ‘not alone with my problems’. Participants described how this made them feel safe enough to engage in the intervention:
I felt free [to talk], there was no-one who was judging me, telling me how wrong I was, or saying, ‘you are doing such bad things,’ and judging my past. (Participant 15)
Salient programme content
Despite some initial concerns that the intervention would be ‘boring’, all participants seemed to gain new ‘knowledge and skills of how to live life positively’. Information about emotion-focused coping responses to trauma (such as substance use and risky sexual behaviour) together with strategies for managing emotion-related triggers for substance use was highly salient for participants:
It’s these triggers that I need to overcome and through the program I’ve learned to overcome them and handle abuse. (Participant 12)
For most participants, anger towards others and self-loathing were common emotional triggers for substance use. Many participants reflected how they were now aware how a build-up of these negative emotions led to ‘explosions’ that created conflict in their intimate and family relationships, social isolation and triggered substance use:
I was an angry person. Sometimes I would look at myself in the mirror and hate myself and end up crying. I was always sitting alone. (Participant 3)
I used to blame others or myself if bad things were happening. Sometimes I would be so angry out of the blue… then you want to use drugs and then end up doing bad things and being hurt. (Participant 6)
Through the intervention, participants became aware of how these negative emotions were a response to unresolved trauma and learnt how to manage these negative emotions (and substance-related cravings) through exercise and mindfulness practice:
That mindfulness exercise we did with breathing. It helps me when I feel sad and lonely… and to stop the cravings. (Participant 7)
Participants also reported that the communication and conflict resolution strategies taught in the programme helped them better manage relationship conflict that triggered substance use and violence:
My boyfriend used to hit me when he is angry. Now he speaks to me. I also know how to speak to him. We get along and do not fight anymore. (Participant 2)
Almost all participants reflected how these new skills and strategies for coping with emotional and other triggers for substance use helped them take steps towards change:
I can see change in my life. Ever since I came here I have become someone else, the person I want to become. It is happening step by step but there is some change. (Participant 17)
I now know who I am and what I want from life. I learned how to control myself as I know what I want. I have learned to put the triggers away. (Participant 14)
Mostly participants described reducing (rather than stopping) their substance use while acknowledging that these reductions led to improvements in the quality of their family and romantic relationships and impacted positively on their sexual risk behaviour:
I was using drugs and it [the program] helped me to reduce. I wasn’t using the condom but now I am using the condom when I am having sex. (Participant 5)
The self-care components of the intervention (including nutrition, budgeting and parenting) were less salient for participants and were rarely mentioned in the interviews.
Areas for programme strengthening
While participants seemed to benefit from the intervention, they highlighted some opportunities for programme strengthening. The first relates to sustainability and duration of counsellor contact, with participants remarking that they ‘felt bad’ when the programme came to an end and ‘wished it to continue’. Instead of proposing additional intervention sessions, they recommended reducing the intensity of the programme by spreading the sessions over 6 weeks rather than 2 weeks. They thought this would enhance support for change and would address some of the barriers that prevent women from fully engaging in intensive programmes:
The two weeks was very short, and I wish we could come back. It must be extended … I wish it could be expanded so we were here for longer. (Participant 13)
A second concern for some participants was the group format. Several participants described feeling ‘uncomfortable’ sharing painful experiences with other women in the group due to concerns about stigma and disclosure. This seemed a particularly salient issue in groups where participants came from the same neighbourhood and ‘all knew each other’:
Like the other day I came with my friend. I noticed that she was not participating, maybe it was because we know each other. I feel like if in the group we can come from different communities so that we don’t judge and share who is in the group outside, then we will be free and share a lot. (Participant 4)
The degree to which participants were able to relate to the experiences of group members also seemed to influence their views of the group. Where participants felt that they shared experiences with others, they were more likely to report feeling satisfied with the group format and tended to describe the groups as ‘supporting each other in the right way’ and that ‘we were one group, we would talk one thing all of us’. In contrast, participants who felt there were major differences between group members were highly concerned about being judged by others:
We did not understand each other into my group. I think we were different because there were those who used drugs and those who drank alcohol. Those drinking alcohol would separate themselves. It’s going to be better if us people using drugs sit alone and have a mutual conversation. (Participant 19)
A further concern was limited postintervention support for change. While there were one or two exceptions, most participants did not develop emotionally supportive relationships with other group members beyond the confines of the programme. Several participants expressed the need for this community-based support but did not feel they could establish these support networks themselves:
We were supporting each other but the support was not like on point … usually when we exit here we separate and never visit each other to see how they are doing. We never saw each other after the sessions. (Participant 3)
Discussion
Despite global HIV prevention guidelines that call for the provision of integrated substance use, psychological trauma and sexual risk reduction services,18 to the best of our knowledge, there are no interventions that address these intersecting risks for HIV among young trauma-exposed South African women. During this phase I study, we found high levels of unmet need for trauma-informed substance use interventions among women from poor communities in the Western Cape. Almost three-quarters of women screened disclosed physical or sexual trauma exposure, and more than half reported heavy alcohol or drug use. Women who were eligible for our intervention demonstrated a strong desire for change, with more than 90% accepting an offer of counselling.
As with other studies,12 13 most of our participants had never initiated trauma or mental health counselling. Along with concerns about stigma and discrimination, limited awareness of services likely contributed to low rates of counselling initiation. Through continuous community-based outreach and a person-centred approach, this study was able to reach and recruit a vulnerable group of trauma-exposed young women with unmet substance use and mental health needs. This confirms the feasibility of recruiting this vulnerable group of young women for a larger study. Nonetheless, as this study’s strict eligibility criteria around age, recent sexual activity and residence limited the number of eligible women we identified, we plan to broaden these inclusion criteria to ensure a future trial can recruit sufficient numbers of trauma-exposed women and to enhance the generalisability of findings to the broad population of trauma-exposed women who use substances.
In addition, findings provide preliminary evidence of the potential benefits of this intervention. Participants reported reducing the frequency of heavy drinking, cannabis and methamphetamine use at the 3-month assessment, with biological evidence of significant reductions in the proportion of participants testing positive for methamphetamine, cannabis and methaqualone supporting self-report data. Depression, psychological distress and trauma severity also diminished significantly, with improvements to depression reaching clinical significance. Significant reductions in sexual risk behaviour were also noted with participants reporting fewer sexual partners and STI symptoms at follow-up. Qualitative findings support these results and suggest possible mechanisms of action. Women reflected how the intervention helped them make positive changes to their substance use and sexual risk behaviour by enhancing their understanding of substance use as a coping response to trauma and providing them with practical tools for regulating negative emotions related to trauma and other stressors.
Participants did however reflect that the programme might have greater success if it provided extended support for change. We had initially hoped that the groups would evolve into peer-support networks; however, these groups dissolved after the programme was completed. As group membership was open rather than closed, this may have contributed to the lack of sustainability. Quantitative findings support these observations: perceptions of social support did not improve because of the intervention. Regardless of whether the intervention remains group based or transitions to an individual format, future studies should consider including community-based peer support groups as part of the intervention. This modification may help support continued development of coping skills and consequently help women sustain any initial behaviour changes. Further qualitative work exploring potential service users’ preferences for the facilitation, structure and content of these peer support groups is needed to guide the development of this intervention component.
Despite these promising outcomes, the poor rate of treatment completion raises concerns about the intervention’s feasibility and highlights the need for additional modifications. Although we collected detailed contact information and actively tracked participants for intervention sessions, just over a third completed the programme. Several factors may have impacted on treatment completion rates. Participants who were newly diagnosed with HIV seemed less likely to complete treatment than those who were already aware of their status. This is not surprising given that other studies have shown that people are more likely to accept the offer of mental health counselling if they have been given time to adjust to their diagnosis.33 To ensure optimal participation, future studies should consider providing this highly vulnerable subgroup with additional supports.
Additionally, given the short window within which participants could complete the intervention, there were limited opportunities to make up missed sessions. Other South African studies using lengthy interventions (≥five sessions) with vulnerable populations have also reported low completion rates, with participants expressing a preference for shorter interventions of up to four sessions.33–35 As participants completed four sessions on average, it may be more efficient to offer four rather than six sessions. As the content that the participants found most helpful (namely, the content on substance use, coping with trauma and sexual risk) was concentrated in four sessions, it seems possible to reduce the number of sessions without affecting programme acceptability. Further support for this suggestion is provided by findings that participants who completed up to four intervention sessions had similar outcomes to those who completed more sessions. Trimming the intervention will allow for better spacing of intervention sessions that would reduce the intensity of the programme. In the qualitative interviews, several participants expressed a preference for a lower intensity programme. Reducing the intensity of the programme could also provide more opportunities for facilitators to reschedule missed sessions. This could improve rates of programme completion. We plan to use these findings to abridge the intervention to four group sessions, each spaced 1 week apart, with an 8-week window within which to complete the programme.
Another plausible explanation for the low uptake of the intervention may lie in the intervention’s group format. Although participants expressed a desire for a group-based intervention during our formative work24 and we took several steps to promote comfort with the group format (such as reinforcing group ground rules around respect and confidentiality at the beginning of each session), several women still expressed discomfort with the group format during the postintervention qualitative interviews. This was largely due to concerns about stigma and privacy, together with difficulties in relating to the diverse experiences of other group members. Concerns about stigma and sexual trauma disclosure, along with the low uptake of group-based intervention components, have been reported in other studies of South African women with histories of sexual trauma.36 37 Given these findings, we plan to adapt the intervention for delivery in an individual format and test whether this improves intervention uptake among this vulnerable population.
Despite the lower than anticipated treatment completion rate, 93% of women completed their 3-month follow-up assessment. This study completion rate corresponds with those obtained in other women-focused intervention studies conducted by our team8 9 14 and demonstrates the effectiveness of our protocols for limiting attrition and the feasibility of retaining this hard-to-reach population in a larger trial. In particular, the addition of case management visits may have contributed to this high retention rate. Although case management activities did not seem to contribute to the outcomes of the programme, we noted a trend towards better retention among those participants who received case management. This is not surprising as these visits provided opportunities to keep participants engaged in the study and allowed staff to explore and address potential barriers to retention. As such, we plan to include case management activities in a future trial.
These are some limitations to this study. The main limitation is that this is a single-arm, uncontrolled feasibility study. Findings are preliminary, and the efficacy of the intervention and whether outcomes of this trauma-informed approach differ from the original WHC still needs to be established in an RCT. Without an RCT of the intervention, we are unable to determine whether the changes observed are attributable to the intervention or other factors. However, our use of mixed methods allowed us to triangulate findings, thereby increasing our confidence in the potential benefits of this intervention. Second, while we used objective measures of recent drug use, we did not include an objective measure of recent alcohol use. In future studies, we plan to include testing for phosphatidylethanol (a biomarker for alcohol use).38 Third, as recruitment was limited to two low-income communities in the Western Cape, findings may not be generalisable to other communities. Nonetheless, this study begins to establish the feasibility, acceptability and preliminary effects of a novel, trauma-informed substance use and sexual risk reduction intervention for young South African women. Findings are being used to modify the intervention for greater efficiency and impact. We plan to assess the acceptability and initial efficacy of this modified trauma-informed substance use and sexual risk intervention in a phase II RCT.
Supplementary Material
Acknowledgments
We would like to thank all study participants, our community advisory board and our field team for their contribution to this study.
Footnotes
Patient consent for publication: Not required.
Contributors: BM and WMW jointly conceived the project, and BM performed the analyses and drafted the manuscript. FAB and TC played major roles in developing and organising the project, data collection and analyses and revised draft versions of the manuscript critically. All authors read and approved the final manuscript.
Funding: Research reported in this publication was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development of the National Institutes of Health under Award Number R21HD082866 and by the South African Medical Research Council.
Competing interests: None declared.
Ethics approval: The South African Medical Research Council (EC 003-2/2015) and RTI International provided ethical approval for this study.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: Quantitative data are available on reasonable request from the corresponding author.
References
- 1. Herman AA, Stein DJ, Seedat S, et al. . The South African Stress and Health (SASH) study: 12-month and lifetime prevalence of common mental disorders. S Afr Med J 2009;99:339–44. [PMC free article] [PubMed] [Google Scholar]
- 2. Kaminer D, Grimsrud A, Myer L, et al. . Risk for post-traumatic stress disorder associated with different forms of interpersonal violence in South Africa. Soc Sci Med 2008;67:1589–95. 10.1016/j.socscimed.2008.07.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Pitpitan EV, Kalichman SC, Eaton LA, et al. . Gender-based violence and HIV sexual risk behavior: alcohol use and mental health problems as mediators among women in drinking venues, Cape Town. Soc Sci Med 2012;75:1417–25. 10.1016/j.socscimed.2012.06.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Berg MK, Hobkirk AL, Joska JA, et al. . The role of substance use coping in the relation between childhood sexual abuse and depression among methamphetamine users in South Africa. Psychol Trauma 2017;9:493–9. 10.1037/tra0000207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Khantzian EJ. The self-medication hypothesis revisited: The dually diagnosed patient. Primary Psychiatry 2003;10:47–54. [Google Scholar]
- 6. Wechsberg WM, Jones HE, Zule WA, et al. . Methamphetamine (“tik”) use and its association with condom use among out-of-school females in Cape Town, South Africa. Am J Drug Alcohol Abuse 2010;36:208–13. 10.3109/00952990.2010.493592 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Abrahams N, Jewkes R, Laubscher R, et al. . Intimate partner violence: prevalence and risk factors for men in Cape Town, South Africa. Violence Vict 2006;21:247–64. 10.1891/vivi.21.2.247 [DOI] [PubMed] [Google Scholar]
- 8. Wechsberg WM, Myers B, Reed E, et al. . Substance use, gender inequity, violence and sexual risk among couples in Cape Town. Cult Health Sex 2013;15:1221–36. 10.1080/13691058.2013.815366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Reed E, Myers B, Novak SP, et al. . Experiences of violence and association with decreased drug abstinence among women in Cape Town, South Africa. AIDS Behav 2015;19:192–8. 10.1007/s10461-014-0820-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Jewkes RK, Dunkle K, Nduna M, et al. . Intimate partner violence, relationship power inequity, and incidence of HIV infection in young women in South Africa: a cohort study. The Lancet 2010;376:41–8. 10.1016/S0140-6736(10)60548-X [DOI] [PubMed] [Google Scholar]
- 11. Shisana O, Rehle T, Simbayi LC, et al. . South African National HIV Prevalence, Incidence, Behaviour and Communication Survey. Cape Town: Human Sciences Research Council, 2011. [Google Scholar]
- 12. Myers B, Carney T, Wechsberg WM. “Not on the agenda”: a qualitative study of influences on health services use among poor young women who use drugs in Cape Town, South Africa. Int J Drug Policy 2016;30:52–8. 10.1016/j.drugpo.2015.12.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Watt MH, Myers B, Towe SL, et al. . The mental health experiences and needs of methamphetamine users in Cape Town: a mixed methods study. S Afr Med J 2015;105:685–8. 10.7196/SAMJnew.7910 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Myers B, Kline TL, Doherty IA, et al. . Perceived need for substance use treatment among young women from disadvantaged communities in Cape Town, South Africa. BMC Psychiatry 2014;14:100 10.1186/1471-244X-14-100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Najavits LM, Hien D. Helping vulnerable populations: a comprehensive review of the treatment outcome literature on substance use disorder and PTSD. J Clin Psychol 2013;69:433–79. 10.1002/jclp.21980 [DOI] [PubMed] [Google Scholar]
- 16. Gilbert L, Raj A, Hien D, et al. . Targeting the SAVA (Substance Abuse, Violence, and AIDS) Syndemic Among Women and Girls: A Global Review of Epidemiology and Integrated Interventions. J Acquir Immune Defic Syndr 2015;69 Suppl 2:S118–27. 10.1097/QAI.0000000000000626 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Roberts NP, Roberts PA, Jones N, et al. . Psychological interventions for post-traumatic stress disorder and comorbid substance use disorder: a systematic review and meta-analysis. Clin Psychol Rev 2015;38:25–38. 10.1016/j.cpr.2015.02.007 [DOI] [PubMed] [Google Scholar]
- 18. UNAIDS. Guidance on HIV prevention among adolescent girls and young women. Putting HIV prevention among adolescent girls and young women on the Fast-Track and engaging men and boys. Vienna, UNAIDS. 2016. Available at http://www.unaids.org/sites/default/files/media_asset/UNAIDS_HIV_prevention_among_adolescent_girls_and_young_women.pdf (Accessed on 8 May 2018).
- 19. Scott-Sheldon LAJ, Senn TE, Keiser TS. Interventions Targeting Alcohol, Violence, and HIV: Current Evidence and Future Directions The Wiley Handbook of Violence and Aggression/The Wiley Handbook of Violence and Aggression, 2017:1–16. [Google Scholar]
- 20. Eldridge SM, Chan CL, Campbell MJ, et al. . CONSORT 2010 statement: extension to randomised pilot and feasibility trials. BMJ 2016;355:i5239 10.1136/bmj.i5239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Western Cape Government. 2016 socio-economic profile: city of Cape Town (p. 36). Cape Town, South Africa. https://www.westerncape.gov.za/assets/departments/treasury/Documents/Socio-economic-profiles/2016/City-of-Cape-Town/city_of_cape_town_2016_socio-economic_profile_sep-lg.pdf (Accessed on 11 Nov 2018).
- 22. Shaikh N, Abdullah F, Lombard CJ, et al. . Masking through averages--intraprovincial heterogeneity in HIV prevalence within the Western Cape. S Afr Med J 2006;96:538–43. [PubMed] [Google Scholar]
- 23. Wechsberg WM, Jewkes R, Novak SP, et al. . A brief intervention for drug use, sexual risk behaviours and violence prevention with vulnerable women in South Africa: a randomised trial of the Women’s Health CoOp. BMJ Open 2013;3:e002622 10.1136/bmjopen-2013-002622 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Myers B, Carney T, Browne FA, et al. . Development of a trauma-informed substance use and sexual risk reduction intervention for young South African women. Patient Prefer Adherence 2018;12:1997–2006. 10.2147/PPA.S175852 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Ponniah K, Hollon SD. Empirically supported psychological treatments for adult acute stress disorder and posttraumatic stress disorder: a review. Depress Anxiety 2009;26:1086–109. 10.1002/da.20635 [DOI] [PubMed] [Google Scholar]
- 26. Green BL. Trauma history questionnaire. measurement of stress, trauma, and adaptation. Lutherville, MD: Sidran Press, 1996. [Google Scholar]
- 27. Radloff LS. A self-report depression scale for research in the general population. Applied Psychological Measurement 1977;1:385–401. [Google Scholar]
- 28. Lewinsohn PM, Seeley JR, Roberts RE, et al. . Center for Epidemiologic Studies Depression Scale (CES-D) as a screening instrument for depression among community-residing older adults. Psychol Aging 1997;12:277–87. 10.1037/0882-7974.12.2.277 [DOI] [PubMed] [Google Scholar]
- 29. Spies G, Kader K, Kidd M, et al. . Validity of the K-10 in detecting DSM-IV-defined depression and anxiety disorders among HIV-infected individuals. AIDS Care 2009;21:1163–8. 10.1080/09540120902729965 [DOI] [PubMed] [Google Scholar]
- 30. Flynn PM, Craddock SG, Hubbard RL, et al. . Methodological overview and Research Design for the Drug Abuse Treatment Outcome Study (DATOS). Psychology of Addictive Behaviors 1997;11:230–43. 10.1037/0893-164X.11.4.230 [DOI] [Google Scholar]
- 31. Sherbourne CD, Stewart AL. The MOS social support survey. Soc Sci Med 1991;32:705–14. 10.1016/0277-9536(91)90150-B [DOI] [PubMed] [Google Scholar]
- 32. Ritchie J, Spencer L. Qualitative data analysis for applied policy research : Bryman A, Burgess RG, Analysing qualitative data. London: Routledge, 1994. [Google Scholar]
- 33. Myers B, Joska JA, Lund C, et al. . Patient preferences for the integration of mental health counseling and chronic disease care in South Africa. Patient Prefer Adherence 2018;12:1797–803. 10.2147/PPA.S176356 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Myers B, Sorsdahl K, Morojele NK, et al. . “In this thing I have everything I need”: perceived acceptability of a brief alcohol-focused intervention for people living with HIV. AIDS Care 2017;29:209–13. 10.1080/09540121.2016.1211242 [DOI] [PubMed] [Google Scholar]
- 35. Sorsdahl K, Stein DJ, Corrigall J, et al. . The efficacy of a blended motivational interviewing and problem solving therapy intervention to reduce substance use among patients presenting for emergency services in South Africa: A randomized controlled trial. Subst Abuse Treat Prev Policy 2015;10:46 10.1186/s13011-015-0042-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Watt MH, Dennis AC, Choi KW, et al. . Impact of Sexual Trauma on HIV Care Engagement: Perspectives of Female Patients with Trauma Histories in Cape Town, South Africa. AIDS Behav 2017;21:3209–18. 10.1007/s10461-016-1617-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Sikkema KJ, Mulawa MI, Robertson C, et al. . Improving AIDS Care After Trauma (ImpACT): Pilot Outcomes of a Coping intervention Among HIV-Infected Women with Sexual Trauma in South Africa. AIDS Behav 2018;22:1039–52. 10.1007/s10461-017-2013-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Nguyen VL, Paull P, Haber PS, et al. . Evaluation of a novel method for the analysis of alcohol biomarkers: Ethyl glucuronide, ethyl sulfate and phosphatidylethanol. Alcohol 2018;67:7–13. 10.1016/j.alcohol.2017.08.009 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2018-024776supp001.pdf (91.3KB, pdf)