Abstract
Objective
We validated the Turkish version of the Wisconsin Stone-Quality of Life (WISQoL) questionnaire for male and female patients with kidney stones.
Material and methods
The Turkish version of the WISQoL questionnaire was developed following a well-established multistep process. A total of 84 patients with kidney stones completed the Turkish WISQoL questionnaire, including the other validated questionnaires as The Short Form Health Survey (SF-36 v2) and Beck’s Depression Inventory. Patients completed questionnaires before percutaneous nephrolithotomy (PNL) surgery as well as 2–4 weeks after surgery. Reliability was evaluated by internal consistency (tested by Cronbach’s alfa) and test-retest reliability between week 2 and 4 (tested by Spearman correlation). Domain structures were examined by interdomain correlations using Spearman correlation coefficient. Convergent validity was assessed by correlating the scores of general health domain to the SF-36 v2, and the scores of emotional impact domain to the Beck’s Depression Inventory questionnaire. Sensitivity to change was assessed by comparing scores before and after PNL surgery with the Wilcoxon signed rank test. Discriminant validity was evaluated by comparing the results of patients 2 and 4 weeks after surgery with Wilcoxon-rank sum tests.
Results
The Turkish version of the WISQoL demonstrates good internal consistency (Cronbach’s α=0.72–0.78) and test–retest reliability (p>0.05). Inter-domain associations within the WISQOL showed a substantial correlation between various WISQoL domains, indicating a high conceptual relationship between the domains. Also, the Turkish version of the WISQoL showed convergent validity with the corresponding validated questionnaires (Spearman’s rho correlation coefficient=0.44–0.78). All domains of the WISQoL showed significant sensitivity to change (p≤0.001).
Conclusion
The Turkish version of the WISQoL is a generally reliable instrument that can be self-administered by Turkish patients with kidney stones in clinical and research settings. Further clinical studies in Turkish settings would be useful to provide powerful data on sensitivity to change.
Keywords: Kidney stone, questionnaires, quality of life
Introduction
Clinicians and healthcare providers are recognizing the importance of measuring health-related quality of life (HRQOL) to evaluate differences among patients at a point in time, or longitudinal changes in HRQOL for patients over a longer period of time. In an effort to maximize quality as well as quantity of life, we use general and disease-specific HRQOL, and symptom-related questionnaires to ascertain an individual’s physical and mental well-being. HRQOL questionnaires generally contain multi-domains to yield information about: life expectancy, various symptom states, numerous physiologic states, physical function states, and emotional and cognitive function status. Quality of life data often guide clinical decisions in urology when used in oncologic conditions, such as prostate or bladder cancers.[1,2]
Urolithiasis is a chronic condition that usually causes significant distress for patients. In an acute pain attack, a patient may suffer various problems, which result in missed work as well as visits to the hospital or ER. In recent studies, it was reported that patients with urolithiasis showed decreased HRQOL scores compared to healthy adults.[3] A reliable and valid means to evaluate patients with kidney stones is becoming important for the prediction of clinical outcome, and forms the basis for continued research and development of better treatment methods. Also, disease-specific HRQOL measures performance better than their generic equivalents for assessing effects of specific conditions.[4] To address such needs, in 2016, Penniston et al.[5] developed the Wisconsin Stone-Quality of Life Questionnaire (WISQoL), a self-administered, multidimensional instrument exploring kidney stone-related morbidity in four domains, including social symptoms, emotional symptoms, disease-specific symptoms, and vitality. Its applicability in different cultures, however, has not been reported, and there are limited studies that evaluate clinical outcomes with WISQoL. Finally, the process of translation and psychometric validation of the questionnaire has not been systematically performed.[6]
We developed a Turkish version of the WISQoL and evaluated its psychometric properties to determine if we could evaluate percutaneous nephrolithotomy (PNL) outcomes in Turkish patients.
Material and methods
Translation process and pilot testing
Linguistic validation of the WISQoL in Turkish was performed through a multistep process as recommended by Hutchinson et al.[7]. Initially, the questionnaire was translated from English to Turkish by two professional, independent native Turkish speaking translators (with English as their first foreign language). Then a teleconference consensus meeting was held on the internet with the translators and the urologist authors (HAA and VU). Thereafter, the translated text was further refined to make it understandable by patients from different socio-cultural and educational levels. In the third step, the draft text was sent for back-translation by two professional, independent translators with English as their native language and Turkish as their first foreign language. In the fourth step a second consensus meeting was held with translators and HAA. The back-translations were reviewed, and small modifications were made. This second draft was revised for Turkish grammar and spelling. Finally, HAA performed a pilot test on 5 patients with kidney stones. No additional remarks were noted, and it was deemed that the Turkish version of WISQoL was ready to use. The Turkish WISQoL was also sent to the author of the original English WISQoL (KLP) to compare the back-translation and original version.
Patient selection and data collection
Participants were recruited at two outpatient centers from April 2016 to October 2016. After the local committee of the Okmeydanı Teaching and Research Hospital approved the study, primary total of 90 patients (60 males and 30 females) who underwent PNL surgery were enrolled in the study. Informed consent forms were obtained from all patients. Adult female or male patients, older than 18 years, who underwent unilateral PNL for kidney stones with sufficient Turkish language skills were included in the study. Exclusion criteria were: (1) past or present history of treatment for lower urinary tract symptoms, benign prostatic hyperplasia (BPH), prostate cancer, chronic prostatitis, or pelvic pain syndrome; (2) bilateral kidney stones; (3) stress/urge/mixed type urinary incontinence, overactive bladder syndrome, lower urinary tract dysfunction, neurological and psychiatric diseases, pregnancy; (4) urinary malignancy, bleeding diathesis, recurrent and urinary tract infection; (5) concomitant medication with α-blockers, anticholinergics, analgesics and other drugs which may interfere with the lower urinary tract function; (6) major complications during PNL such as serious bleeding, and (7) ureteral stent insertion. All patients were fully informed about the purpose of the study, which was approved by the Institutional Review Board, and all of them gave their written informed consent. The Turkish WISQoL was administered to patients before PNL (WISQoL-1) and 2 weeks after surgery (WISQoL-2). The questionnaire was completed 4 weeks after PNL surgery (WISQoL-3) to compare patient’s baseline condition with final status. Patients completed other questionnaires within defined measurement time points: The Turkish version of The Short Form 36 Health Survey (SF-36 v2) and Beck’s Depression Inventory. WISQoL scores were computed with established guidelines formulated by the original author (KLP).
PNL surgery
PNL surgery was performed by expert surgeons with the patient under general anesthesia. After ureteral catheterization using a 5 or 6F open-ended ureteral catheter, patients were placed in the prone position, and percutaneous access was achieved under fluoroscopic guidance. Tract dilatation was accomplished using Amplatz or balloon dilators of up to 22F or 30F. Fragmentation and stone removal were accomplished with pneumatic or ultrasonic energy, and using retrieval graspers inserted through rigid 22F–26F nephroscopes. Then, a 16F reentry catheter or an 18F Foley catheter as the nephrostomy tube was inserted. If the patient was comfortable, afebrile, and there was no longer drainage from the nephrostomy site after removal of the nephrostomy tube, the patient was discharged the next day. The patient was seen at 2 and 4weeks after surgery and evaluated with KUB for residual kidney stones.
Statistical analyses
For this analysis, raw WISQoL scores were used. Thus, each of the 28 WISQoL items is scored between 1, and 5 points, and the total score ranged between 28, and 140 points; while the range of subdomain scores varied with the number of items in each subdomain. Statistical analyses were performed with IBM Statistical Package for the Social Sciences Statistics version 22.0 (IBM SPSS Statistics; Armonk, NY, USA) using suitable methods for assessment of multi-steps. The level of significance was set at p<0.05. Internal consistency reliability was tested by Cronbach’s α of WISQoL-1, and test-retest reliability between WISQoL-2 and WISQoL-3 was evaluated by Wilcoxon signed-rank test. Sufficient consistency and reliability were assumed for values >0.70. The power of the study was calculated using the G*Power program (University of Dusseldorf, Dusseldorf, Germany) and the post hoc test with accuracy mode calculation and an effect size convention of 0.6 for the two-tailed t-test, with an alpha error protection of 0.05.
We used Spearman’s rank correlation (r) to assess inter-domain associations of the WISQoL and convergent validity. Convergent validity was assessed by correlating WISQoL-3 subscores and equivalent subdomains of validated questionnaires (Beck’ Depression Inventory, SF-36 v2). Conceptually-related domains (SF-36 v2 vs WISQoL-3) were expected to show a high correlation (r≥0.40). In contrast, questionnaires showing a negative association (Beck’s Depression Inventory vs. WISQoL-3) should correlate inversely (r≤-0.40). Sensitivity to change was analyzed by comparing scores before (WISQoL-1) and after PNL surgery (WISQoL-3) with Wilcoxon’s rank-sum tests.
Results
Six patients were excluded due to refusal to participate in the study. Table 1 shows the demographic and clinical characteristics of 84 patients before PNL surgery. Table 2 shows the internal consistency and test-retest reliability of the Turkish version of WISQoL, which was assessed by Cronbach’s α of WISQoL-2. Internal consistency was high for all WISQoL-2 domains (Cronbach’s α=0.72–0.78). Test-retest reliability was evaluated by comparing subdomains and total scores of WISQoL-2 and WISQoL-3, and no difference was observed between subdomains and total scores (p>0.05).
Table 1.
Demographic and clinical characteristics
| Min–Max | Median | Mean±SD n-% |
|
|---|---|---|---|
| Age (years) | 15.0–63.0 | 39.0 | 38.8±13.1 |
|
| |||
| BMI (kg/m2) | 21.0–32.0 | 25.0 | 25.4±3.1 |
|
| |||
| Sex | |||
| Male | 58 | 69.0% | |
| Female | 26 | 31.0% | |
|
| |||
| Education status | |||
| Primary | 60 | 71.4% | |
| College | 7 | 8.3% | |
| Post Graduate | 17 | 20.2% | |
|
| |||
| Passed a stone(s) ever | |||
| Yes | 39 | 46.4% | |
| No | 45 | 53.6% | |
|
| |||
| Stone disease duration (day) | 0.0–30.0 | 5.0 | 9.0±10.1 |
BMI: body mass index; SD: standard deviation
Table 2.
Internal consistency and test-retest reliability
| Internal consistency Cronbach’s α | Test | Re-Test | p | |||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|||||||
| Mean±SD | Med (Min–Max) | Mean±SD | Med (Min–Max) | |||||
| Domain | ||||||||
|
| ||||||||
| Social impact | 0.74 | 104.5±19.6 | 100 | 70–133 | 105.7±14.9 | 105 | 86–135 | 0.290w |
|
| ||||||||
| Emotional impact | 0.75 | 109.9±18.2 | 114 | 75–131 | 112.9±11.9 | 117 | 87–127 | 0.059w |
|
| ||||||||
| Stone-related impact | 0.77 | 106.1±16.2 | 99 | 79–128 | 105.5±14.2 | 107 | 80–126 | 0.473w |
|
| ||||||||
| Vitality impact | 0.72 | 112.2±14.8 | 120 | 56–138 | 118.2±20.4 | 120 | 56–139 | 0.157w |
|
| ||||||||
| Total score | 0.78 | 107.3±14.7 | 105 | 79–130 | 109.6±9.9 | 110 | 92–124 | 0.202w |
Wilcoxon test.
SD: standard deviation
WISQoL consistently showed a significant correlation between WISQoL subscores, with correlation coefficients between 0.443 and 0.892. Inter-domain correlation for the first three subdomains was acceptable, however, a slightly weaker correlation existed between these domains and the vitality domain (r=0.443–0.549) (Table 3).
Table 3.
Inter-domain associations [Spearman’s rank correlation coefficient (p value)]
| Domain | D1 | D2 | D3 | D4 | |
|---|---|---|---|---|---|
| Social impact D1 | r | - | |||
| p | - | ||||
|
| |||||
| Emotional impact D2 | r | 0.781 | |||
| p | 0.000 | ||||
|
| |||||
| Sone-related impact D3 | r | 0.519 | 0.588 | ||
| p | 0.000 | 0.000 | |||
|
| |||||
| Vitality impact D4 | r | 0.549 | 0.443 | 0.505 | |
| p | 0.000 | 0.000 | 0.000 | ||
|
| |||||
| Total score | r | 0.892 | 0.892 | 0.763 | 0.648 |
| p | 0.000 | 0.000 | 0.000 | 0.000 | |
Spearman Correlation
Convergent validity of WISQoL was evaluated by comparing subdomains of SF-36 v2 and Beck’s depression inventory. Acceptable convergent validity was noticed between WISQoL subdomains and SF-36 v2. Also as expected, a negative correlation was observed between the WISQoL and Beck’s depression inventory (r=−0.654, p<0.001). All other domains correlated significantly with the corresponding items of the validated questionnaires (Table 4).
Table 4.
Convergent validity
| r | p | |
|---|---|---|
| WISQOL social impact vs. SF-36 v2 social functioning | 0.783 | 0.000 |
| WISQOL emotional impact vs. Beck’s depression inventory | −0.654 | 0.000 |
| SF-36 v2 mental health | 0.329 | 0.001 |
| WISQOL stone-related impact vs. SF-36 v2 general health perceptions | 0.737 | 0.000 |
| WISQOL vitality impact vs. SF-36 v2 energy vitality | 0.474 | 0.000 |
Spearman correlation
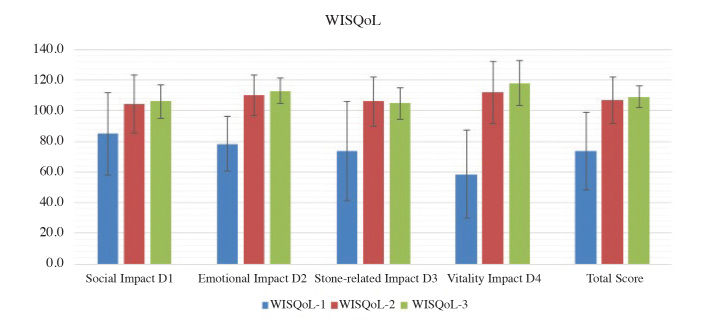
Fifteen of 84 patients (17%) had residual stones and additional surgery was recommended. Fifteen patients were excluded when investigating the sensitivity of WISQoL to change. Sensitivity of WISQoL to change was assessed by comparing subdomains and total scores of 69 kidney stone patients with before PNL with those of patients without any residual stones after PNL surgery. WISQoL scores detected 4 weeks after PNL (WISQoL-3) were significantly higher when compared with those found before PNL (WISQoL-1) (Table 5 and Figure 1).
Table 5.
Sensitivity to change
| Before PNL | After PNL | ||||||
|---|---|---|---|---|---|---|---|
|
|
|
||||||
| Mean±SD | Med (Min–Max) | Mean±SD | Med (Min–Max) | p | |||
| Domain | |||||||
|
| |||||||
| Social impact | 85.0±26.7 | 81 | 42–128 | 104.4±19.0 | 100 | 90–136 | 0.000w |
|
| |||||||
| Emotional impact | 78.4±24.7 | 79 | 63–111 | 110.0±18.2 | 114 | 94–134 | 0.000w |
|
| |||||||
| Stone-related impact | 73.6±32.4 | 82 | 45–125 | 106.1±16.2 | 102 | 97–128 | 0.000w |
|
| |||||||
| Vitality impact | 58.5±28.9 | 54 | 35–101 | 112.2±20.7 | 120 | 90–128 | 0.000w |
|
| |||||||
| Total score | 73.6±25.1 | 76 | 50–103 | 107.3±15.2 | 105 | 97–132 | 0.000w |
Wilcoxon test;
PNL: percutaneous nephrolithotomy
Figure 1.
Comparison of WISQoL total scores before and after PNL
WISQoL: Wisconsin stone-quality of life; PNL: percutaneous nephrolithotomy
Discussion
Urolithiasis is a common urological disease with a >10% lifetime prevalence rate in countries with high standard of living and has increased >37% over the last 20 years.[8,9] Because of the chronic nature of kidney stone disease, patients’ quality of life is decreased, particularly with respect to their physical and mental states.[10] In addition, frequent recurrences and loss of work are other factors that decrease quality of life and, specifically, HRQOL.[11] For all these reasons, HRQOL in kidney stone patients has been evaluated in various publications[12,13] mostly using validated general questionnaires, such as the SF-36 and the Mental Health Inventory. However, disease-specific questionnaires are known to be more appropriate than their general counterparts for patients with a specific diagnosis.[3] In 2017, Penniston et al.[5] made an important step forward in this field by developing and validating the WISQoL questionnaire, which is a 28-item disease-specific regional survey instrument with a 5-point Likert scale for each item. In addition, there are four subdomains that assess the physical impact and emotional impact of kidney stone disease, as well as the impact of health status on social functioning and vitality. In this article, using standardized translation and validation processes, we sought to validate the Turkish version of WISQoL in patients with kidney stones before and after PNL surgery. Our results show that the Turkish version of the WISQoL questionnaire is a reliable instrument for the assessment of kidney stone patients’ problems. Additionally, the Turkish version of the WISQoL shows increased sensitivity to change and convergent validity. These findings suggest that the WISQoL questionnaire has adequate cross-cultural validity potential and might be applicable to other languages. Finally, since only 29% of the patients in our study had an educational status higher than primary school, the readability and generalizability of the Turkish WISQoL appears acceptable.
Internal consistencies were found to be satisfactory for all domains (Table 2), suggesting strong reliability. Test-retest reliability, which was assessed 2 weeks after PNL surgery and compared to preoperative WISQoL scores was high (Table 2). However, it is possible that longer periods between assessments could lower the test-retest reliability correlation coefficient.
A strong inter-domain correlation highlights the ability of each of the 4 subdomains in the Turkish version of the WISQoL to reveal HRQOL effects in patients with similar kidney stone disease (Table 3). The only exception was the presence of a moderate correlation between emotional impact (D2) and vitality impact (D4) (Spearman’s rho correlation coefficient=0.44). A similar finding was observed in the original WISQoL study by Penniston et al.[5] (Spearman’s rho correlation coefficient=0.56). The reason for these findings remains to be clarified. In our study, depression was found in 15% of all patients, and female patients were more prone to depression than males. We observed that contrary to female patients, emotional status of male patients did not affect their vitality.
Convergent validity of the Turkish version of WISQoL was confirmed by a strong correlation with subdomains of the SF-36 v2 measures. In addition, the SF-36 v2 emotional domain and Beck’s Depression Inventory had a high-to-moderate correlation with the emotional impact domain score of the WISQoL questionnaire along with high statistical significance, indicating that the total score of the WISQoL reflects patients’ HRQOL status accurately.
The Turkish version of WISQoL was capable of discriminating among patients with and without kidney stones. The overall scores after surgery increased compared to scores prior to surgery by about 20%, whereas when domains were compared separately, the increase was found to be lower (10–20%). It was observed that the highest increase was in the stone disease impact subdomain, as expected.
Our study has some limitations. Firstly, our institution is an academic stone center; thus, our patients have more complex stone disease and larger stone burden than the general population, which could influence our results. Secondly, we evaluated the effectiveness of the WISQoL questionnaire only in patients with symptomatic kidney stones; its validity in asymptomatic individuals was not investigated and therefore may not be generalizable. Third, we assessed a small number of patients. Studies using the Turkish version of the WISQoL in larger populations are thus warranted.
In conclusion, the Turkish version of the WISQoL is a generally robust instrument that can be self-administered by Turkish patients with kidney stones in the clinical and research settings. Further clinical studies in the Turkish settings would be useful to confirm its sensitivity to change. Copies of the questionnaire can be obtained from the authors.
Acknowledgements
We thank Ms.Gill Mazı for her participation in the translation and back-translation process. We are also grateful to Mr.Ertan Koç, for his excellent assistance in managing the database.
Footnotes
Ethics Committee Approval: Ethics committee approval was received for this study from the ethics committee of Okmeydanı Training and Research Hospital (04.09.2017/660).
Informed Consent: Written informed consent was obtained from patients who participated in this study.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept H.A.A.; Design H.A.A., V.Ü.; Supervision H.A.A., K.L.P.; Resources O.C., M.Ö.; Materials M.Ö.; Data Collection and/or Processing L.C., M.Ö., O.C.; Analysis and/or Interpretation H.A.A., V.Ü., L.C.; Literature Search H.A.A., K.L.P.; Writing Manuscript H.A.A.; Critical Review K.L.P.; Other L.C., V.Ü.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Kim SP, Karnes RJ, Nguyen PL, Ziegenfuss JY, Han LC, Thompson RH, et al. Clinical implementation of quality of life instruments and prediction tools for localized prostate cancer: results from a national survey of radiation oncologists and urologists. J Urol. 2013;189:2092–8. doi: 10.1016/j.juro.2012.11.174. [DOI] [PubMed] [Google Scholar]
- 2.Feuerstein MA, Jacobs M, Piciocchi A, Bochner B, Pusic A, Fayers P, et al. Quality of life and symptom assessment in randomized clinical trials of bladder cancer: A systematic review. Urol Oncol. 2015;33:331–8. doi: 10.1016/j.urolonc.2015.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kartha G, Calle JC, Marchini GS, Monga M. Impact of stone disease: chronic kidney disease and quality of life. Urol Clin North Am. 2013;40:135–47. doi: 10.1016/j.ucl.2012.09.004. [DOI] [PubMed] [Google Scholar]
- 4.Wiebe S, Guyatt G, Weaver B, Matijevic S, Sidwell C. Comparative responsiveness of generic and specific quality-of life instruments. J Clin Epidemiol. 2003;56:52–6. doi: 10.1016/S0895-4356(02)00537-1. [DOI] [PubMed] [Google Scholar]
- 5.Penniston KL, Antonelli JA, Viprakasit DP, Averch TD, Sivalingam S, Sur RL, et al. Validation and Reliability of the Wisconsin Stone Quality of Life Questionnaire. J Urol. 2017;197:1280–8. doi: 10.1016/j.juro.2016.11.097. [DOI] [PubMed] [Google Scholar]
- 6.Zhao PT, Hoenig DM, Smith AD, Okeke Z. A Randomized Controlled Comparison of Nephrostomy Drainage vs Ureteral Stent Following Percutaneous Nephrolithotomy Using the Wisconsin Stone QOL. J Endourol. 2016;30:1275–84. doi: 10.1089/end.2016.0235. [DOI] [PubMed] [Google Scholar]
- 7.Hutchinson A, Bentzen N, König-Zahn C. Cross-cultural health outcome assessment: a user’s guide. European Research Group on Health Outcomes; Ruinen: 1996. pp. 182–98. [Google Scholar]
- 8.Stamatelou KK, Francis ME, Jones CA, Nyberg LM, Curhan GC. Time trends in reported prevalence of kidney stones in the United States: 1976–1994. Kidney Int. 2003;63:1817–23. doi: 10.1046/j.1523-1755.2003.00917.x. [DOI] [PubMed] [Google Scholar]
- 9.Hesse A, Brändle E, Wilbert D, Köhrmann KU, Alken P. Study on the prevalence and incidence of urolithiasis in Germany comparing the years 1979 vs. 2000. Eur Urol. 2003;44:709–13. doi: 10.1016/S0302-2838(03)00415-9. [DOI] [PubMed] [Google Scholar]
- 10.Angell J, Bryant M, Tu H, Goodman M, Pattaras J, Ogan K. Association of depression and urolithiasis. Urology. 2012;79:518–25. doi: 10.1016/j.urology.2011.10.007. [DOI] [PubMed] [Google Scholar]
- 11.Trinchieri ACG, Segura JW, Khoury S, Pak CY, Preminger GM, Tolley D. Stone Disease. Health Publications; Paris: 2003. Epidemiology; pp. 201–29. [Google Scholar]
- 12.Bryant M, Angell J, Tu H, Goodman M, Pattaras J, Ogan K. Health related quality of life for stone formers. J Urol. 2012;188:436–40. doi: 10.1016/j.juro.2012.04.015. [DOI] [PubMed] [Google Scholar]
- 13.Miyaoka R, Ortiz-Alvarado O, Kriedberg C, Alanee S, Chotikawanich E, Monga M. Correlation between stress and kidney stone disease. J Endourol. 2012;26:551–5. doi: 10.1089/end.2010.0536. [DOI] [PubMed] [Google Scholar]