Abstract
Background: Colostomy formation can solve complications of bowel management following spinal cord injury (SCI). Newly injured patients at this spinal unit have chosen colostomy as a preferred option for bowel management. Objectives: To discover the reasons patients choose colostomy formation early following SCI and make comparison with those choosing it later, and to establish whether early colostomy is safe and advisable. Methods: Medical and nursing records of patients with SCI who chose to have a colostomy during the period 2005–2016 were examined retrospectively. Data were gathered concerning reasons for choosing a colostomy, early and later complications, the need for further surgery, and independence with bowel care before and after surgery. Patients were divided into two groups: those who chose a colostomy “early” during inpatient rehabilitation and those who chose it “later” as is traditional. Results: Reasons for choosing colostomy differed. Reducing reliance on caregiver and independence were of more importance to the early group; the later group chose colostomy to solve bowel care problems. Early complication rates in both groups were low. Longer term complications were higher in the early group, with the most common complication being rectal discharge. Parastomal hernia rates were low in both groups, as was the need for further surgery. Colostomy formation led to 20.8% of all patients gaining independence with bowel care. Conclusion: This study found colostomy to be a safe and effective option when performed early after SCI and demonstrates colostomy can be a means of gaining independence and making bowel care easier and more acceptable to the newly injured patient.
Keywords: bowel management, colostomy, independence, spinal cord injury
Spinal cord injury (SCI) has a profound impact on bowel function and continence and commonly results in neurogenic bowel dysfunction, that is, delayed transit of stool through the colon, lack of awareness of having a full rectum, and impaired or absent ability to expel stool from the body.1 To achieve regular bowel emptying and maintain continence, usual practice is to teach patients or caregivers to utilize noninvasive methods such as diet adaption and use of pharmaceuticals to achieve desirable stool consistency and techniques of straining, digital stimulation, or manual evacuation to empty the bowel.1–3
Neurogenic bowel dysfunction together with straining and digital rectal interventions frequently lead to further bowel-related complications. Coggrave et al4 found 39% experienced constipation and 36% hemorrhoids, and they found that bowel dysfunction impacts life significantly more than other impairments. Krogh et al5 found 75% of participants had incontinence of varying frequency and 39% said bowel dysfunction restricted their social activities and quality of life (QOL). Other complications include autonomic dysreflexia (AD), fecal impaction, anal fissure, prolapse, lack of independence, and feelings of degradation.4,6–9 Several studies have found that bowel care can be lengthy, taking over an hour in many cases.10,11 Longitudinal studies have found that bowel function and complications tend to worsen over time.12,13 Research has shown that for those living with SCI, improving bowel function is an area of great importance. In Anderson's14 study, this was ranked as being highly important to both those with quadriplegia and tetraplegia. Simpson et al's15 systematic review confirmed improvement in bowel function as an important priority for individuals.
When dietary manipulation, use of pharmaceuticals, and digital rectal interventions fail to achieve satisfactory bowel management, professional advice advocates the use of more invasive techniques, such as rectally inserted colonic irrigation (eg, Peristeen), sacral root stimulation, and antegrade continence enema (ACE),1 which is a surgical technique using the appendix to create an abdominal stoma through which fluid can be flushed to promote bowel evacuation. Both of these procedures have been found to improve bowel function and QOL in some individuals with SCI.16,17
A final suggested method of bowel management is colostomy.1 Studies have found it to be a safe and well-accepted intervention,18 which can improve bowel management, reduce complications, and improve QOL.19 Colostomy may be performed to alleviate chronic problems of abdominal distension, megacolon, and difficulty evacuating the bowels,18 and it is also indicated in the management of pressure ulcers to alleviate fecal contamination.10,20 Patients are highly satisfied with colostomy, find it greatly reduces time taken to perform bowel care, and frequently wish they had it performed much earlier.6,18,21–23 An additional benefit of colostomy is that it can enable some patients to achieve independence in bowel care, which more complex interventions of rectal irrigation and ACE procedures may not. Colostomy formation is still referred to, however, as a later resort in bowel management interventions,1 and it is often not considered until all other interventions have failed. Coggrave et al22 state it is unclear whether the reason for delaying colostomy is the readiness of patients or the reluctance of health care professionals to suggest stoma formation.
It has therefore been of interest to observe a shift in practice in our hospital (Salisbury District Hospital) over the last 5 years, as increasing numbers of patients with SCI have requested colostomy in the first few months following their spinal injury, while still receiving inpatient rehabilitation. The reasons why patients are seeking colostomy at such an early stage are being investigated, as well as the safety and efficacy of this shift in practice. We report on early findings of our research.
Methods
This is a retrospective study of patients with SCI who chose to have a colostomy for bowel management at Salisbury District Hospital during the period 2005–2016. Health Research Authority, ethical, university, and hospital trust permission were obtained to carry out the research. Patients were identified by electronic and physical database and stoma nurse record searches. Once patients had been identified, information was gathered from hospital medical notes and stoma nurse records; for those patients whose stoma care was transferred to another area after discharge from hospital, local stoma nurses were contacted for further information. Patients were divided into two groups: those who chose a colostomy “early” in the first few months after spinal injury and during inpatient rehabilitation, and those who chose it “later” usually more than a year after injury and after being discharged home (see Figure 1 for more detailed definition). Patients were excluded who had a colostomy formed for a reason other than choice (eg, cancer, fistula, or injuries sustained at the time of their SCI).
Figure 1.
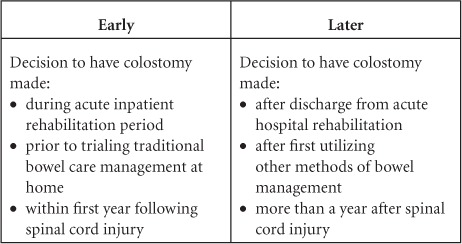
Operational definitions of early and later colostomy.
Data gathered included reasons for choosing to have a colostomy, bowel management methods and complications prior to colostomy, early surgical complications, and longer term complications related to stoma formation. Independence with bowel care pre and post colostomy was also documented. Early surgical complications were graded according to Clavien-Dindo classification.24
It has been noted that a lack of uniformity in agreed colostomy complications hinders comparison of research findings.25 Later complication categories used by others were assessed before deciding criteria for this research.11,18,21,22 It was decided to record incidence of the following: hernia, prolapse, rectal discharge, defunctioning colitis (termed diversion colitis by some),26 retraction, and stenosis. Data on incidence and type of further stoma-related surgery were also gathered.
Exact tests of independence/association were obtained using StatXact v.11 software package, and comparisons were made using the chi-square or Fisher's exact test. Statistical significance was defined as p < .05.
Results
Eighty-three patients were identified as having had a colostomy at varying time intervals following SCI between 2005 and 2016. Of these, six were excluded due to having a colostomy for cancer or bowel fistula and five because their hospital records were unobtainable due to patients passing away prior to a change in the hospital record-keeping system. Of the remaining 72 patients, 20 had chosen to have an early colostomy and 52 had chosen it later. Fifty-seven were male and 15 were female. Complexity of data in terms of whether injuries were complete or incomplete and gaps in recording of American Spinal Cord Injury Association Impairment Scales (AIS) meant no meaningful comparisons could be made at this time between neurological deficit level and the decision to have a colostomy. Records did show that for both early and later groups approximately half of those choosing a colostomy had cervical spine injuries, a little less than half had thoracic spine injuries, and a small number had either lumbar or sacral level injuries. Sixty-nine of the 72 patients studied lived outside the local catchment area and so were transferred to the care of another stoma care nurse on discharge home. No patients were under the age of 18 at the time of colostomy.
The first patients to choose an early colostomy did so in 2013, and additional data about the total numbers of patients admitted to the authors' spinal unit in the period from 2013 to 2016 when data collection ended were sought. It was found that in this time period 215 patients were admitted with a new SCI, with a mean age of 49 years (range, 15–90). Mean age at injury of those choosing an early colostomy in this same period was 58 years (range, 36–72). Forty-two elective colostomies were performed in this time: 22 were later colostomies, and 20 were early ones. The 20 patients who chose to have an early colostomy meant that 9.3% of all newly injured patients undergoing rehabilitation in this UK hospital chose to have a colostomy as their preferred method of bowel management in this time period. This is almost four times as many choosing an early colostomy as the 2.4% of individuals with SCI that Coggrave et al4 found to have colostomy overall in the UK. Mean time from SCI to having a colostomy was 6.5 months for the early group and 214.6 months for the later group. Most frequently given reasons by those in the later group for having a colostomy were localized bowel care complications (eg, anal fissure, hemorrhoids, pain) and lengthy bowel care (Table 1). The early group differed in that whilst incontinence was the most commonly cited reason, other important reasons were to reduce reliance on caregiver and increase independence and to improve QOL. They also found bowel care degrading/embarrassing. (QOL was a general term documented in medical notes rather than a specific measure we used and reflects a qualitative rather than quantitative assessment.) These reasons were of less importance to the later group. The differences in reasons given between the two groups are statistically significant (p < .0001).
Table 1.
Reasons for choosing colostomy
| Reasons for colostomy | Early group (n=20) | Later group (n=52) | Total (N=72) | Probabilitya |
|---|---|---|---|---|
| Localized complication (eg hemorrhoids, anal fissure, pain/bleeding) | 2 (10%) | 29 (55.8%) | 31 | 0.0004 |
| Incontinence | 10 (50%) | 21 (40.4%) | 31 | 0.5962 |
| Gain control | 1 (5%) | 0 | 1 | 0.2778 |
| Increase QOL | 5 (25%) | 10 (19.2%) | 15 | 0.7467 |
| Reduce carer reliance/independence | 7 (35%) | 5 (9.6%) | 12 | 0.0156 |
| Time | 0 | 25 (48.1%) | 25 | 0.0001 |
| Dissatisfaction with present management | 2 (10%) | 11 (21.2%) | 13 | 0.3297 |
| Embarrassing/degrading | 5 (25%) | 2 (3.8%) | 6 | 0.0154 |
| Neurogenic pain | 0 | 3 (5.8%) | 3 | 0.5553 |
| Constipation | 0 | 5 (9.6%) | 5 | 0.3129 |
| Own knowledge/research | 4 (20%) | 2 (3.8%) | 6 | 0.0465 |
| Make bowel care easier | 2 (10%) | 0 | 2 | 0.0743 |
| Anxiety/depression/distress of bowel care | 3 (15%) | 2 (3.8%) | 5 | 0.1272 |
| Planning for future | 1 (5%) | 1 (1.9%) | 2 | 0.4812 |
| AD | 4 (20%) | 7 (13.5%) | 11 | 0.4849 |
Note: AD = autonomic dysreflexia; QOL = quality of life.
aProbability of differences between the groups being due to chance, p < .0001.
Early surgical complication rates were acceptable, with no significant difference between the two groups (Table 2; p = .29). Several patients experienced parastomal cellulitis following surgery, five of which required treatment with antibiotics. Two patients (one from the early and one from the later group) developed bowel ischemia and required further surgery and resection; one of these also required negative pressure wound therapy to achieve wound closure. Another patient from the early colostomy group developed a deep vein thrombosis and pressure sore postoperatively, which led to a delay in discharge from hospital.
Table 2.
Early complications by Clavien-Dindo classification
| Clavien-Dindo classification | Early | Later | Total |
|---|---|---|---|
| Grade 0 | 15 (75%) | 47 (90.4%) | 62 (86.1%) |
| Grade I | 2 (10%) | 2 (3.8%) | 4 (5.6%) |
| Grade II | 2 (10%) | 2 (3.8%) | 4 (5.6%) |
| Grade III | 0 | 1 (1.9%) | 1 (1.4%) |
| Grade IV | 1 (5%) | 0 | 1 (1.4%) |
| Total | 20 | 52 | 72 |
Note: Probability of differences between the groups being due to chance, p = .29.
Patients had between zero and three longer term complications (Table 3). Forty percent of the early group experienced no later complications, compared with 69.2% of the later group (exact p = .0005). The most common longer term complication in both groups was rectal discharge.22 In one of the patients in the later colostomy group, it led to them undergoing a proctectomy. Rectal discharge accounted for nearly half of the complications reported by the early group, but only 11.5% of the later group. Of those in the later colostomy group, 11.5% were known to have developed a parastomal hernia and none of those in the early group, giving an overall known hernia rate of 8.3% for the whole patient group.
Table 3.
Later complications
| Complication | Early | Later | Total |
|---|---|---|---|
| None | 8 (40%) | 36 (69.2%) | 44 (61.1%) |
| Rectal discharge | 8 (40%) | 6 (11.5%) | 14 (19.4%) |
| Hernia | 0 | 6 (11.5%) | 6 (8.3%) |
| Prolapse | 2 (10%) | 5 (9.6%) | 7 (9.7%) |
| Retraction | 4 (20%) | 1 (1.9%) | 5 (6.9%) |
| Stenosis | 3 (15%) | 1(1.9%) | 4 (5.6%) |
| Defunctioning (diversion) colitis | 1 (5%) | 0 | 1 (1.4%) |
| Total no. of complications | 26 | 55 | 83 |
Note: Probability of differences between the groups being due to chance, p = .0005.
There was no significant difference between the groups requiring further surgery related to their stoma (p = .28). Two patients from the early group (10%) and 11 of the later group (21.2%) underwent further surgery related to their stoma (Table 4). Nearly all of these had one further operation; one of the later group required two operations. In both early patients, this was a refashion for stenosis. In the later group, hernia repair was the most common reason for surgery. Only one patient was dissatisfied with their stoma and underwent colostomy reversal. This patient was in the later group. Following colostomy formation, nine of the early group and six of the later group achieved independence with bowel care, having been reliant on caregivers previously. This is a total 20.8% of patients gaining independence with bowel management.
Table 4.
Further surgery
| Further ops | Early | Later | Total |
|---|---|---|---|
| Hernia repair | 0 | 5 (9.6%) | 5 (6.9%) |
| Refashion | 2 (10%) | 2 (3.8%) | 4 (5.6%) |
| Proctectomy | 0 | 1 (1.9%) | 1 (1.4%) |
| Prolapse repair | 0 | 3 (5.8%) | 3 (4.2%) |
| Total | 2 (10%) | 11 (21.2%) | 13 (18.1%) |
Note: Probability of differences between the groups being due to chance, p = .0028.
Discussion
Patients who chose an early colostomy were an average 9 years older than the general spinal unit inpatient population at that time. Patient numbers are small for making statistical inference, but it may be that older patients are more likely to choose colostomy earlier than younger ones. Body image and relationship status were not investigated as part of this study; it may merit further investigation to ascertain if this impacts on their decision to undergo colostomy formation and to discover whether age impacts decision making in patients who are not spinally injured.
Reasons given for choosing colostomy concur with previous findings.11,22 The statistically significant differing reasons for choosing colostomy cited by the two groups here are of interest. The most frequently given reason for the later group was complications related to bowel care. This was an infrequent reason for the early group, who have not had time to develop some of the bowel care–related complications experienced by the later group. Length of time taken to perform bowel care was frequently mentioned by the later group but by none of the early group, suggesting increasing time needed for bowel care may be something that worsens over time. The desire to reduce reliance on caregivers and gain independence was a frequently expressed reason given by the early group, none of whom were independent in bowel care prior to colostomy. The early group were more likely to cite finding bowel care degrading and embarrassing than the later group, and incontinence was this group's most commonly given reason.
Offering colostomy as an alternative to traditional bowel care may be appropriate at this early stage to help counter these feelings and aid adaptation in the early stages of adjustment to life following SCI. It could be argued that as the later group are less likely to find bowel care degrading and embarrassing, it is something the earlier group would have adjusted to in time without having had the colostomy. Becoming used to something, however, may not mean it is the best option; none of the early group have so far expressed dissatisfaction with their colostomy or a desire to have it reversed. This is an area in which traditional thinking is being challenged.
Findings here challenge the base assumption that colostomy is solely about solving bowel care difficulties. It is being chosen by this early group of patients as a way to achieve independence before complications and difficulties have yet been fully encountered. This signifies a fundamental paradigm shift in thinking about the role of colostomy in patients with a spinal injury. It is demonstrated here to be of particular importance to the early group. Perhaps all patients should be made more aware of the option of colostomy during their inpatient period.
Achieving independence can be an important factor in psychological adaption to SCI, and it is an area that is measured when assessing QOL in those with chronic illness.27 Gains in independence and control achieved by colostomy may aid adaption to injury and improve QOL. Control over bowel function and reduction in the time it takes may also lead to increased numbers of patients returning to work. Kennedy and Hasson28 found only one third of patients were able to do so following SCI. Returning to work, involvement in sport and social activities, and being able to go on holiday are benefits that other research has found to be positive outcomes of colostomy formation.6 The increase in independence, which this research has demonstrated, is of great importance to those with SCI.14 In our study, a fifth of patients gained independence in an area of life where they were previously dependent on others. Having a colostomy enabled one of the early group patients to live independently once discharged home; without it he would have needed assistance for bowel care, and he felt his QOL and freedom to partake in social activities would have been greatly reduced. It could be suggested that enabling independence in an important personal domain through colostomy formation at an early stage may help adaption to SCI.
No significant harm was demonstrated in our research by having colostomy performed at an early stage during rehabilitation following SCI. Early surgical complication rates were low with no Grade V complications. Later complications were significantly higher in the early colostomy group, with 60% experiencing at least one complication compared to only 30.8% of the later group. Similar to the research findings of others, rectal leakage was a common complication; more of the early group cited this as a complication than did the later group. The reasons for this are not known. It may be a symptom that settles after a period of time (the early group had their stomas for 1–4 years); it may be perceived as less of a problem and so not reported as often by those in the later group who have suffered more significant bowel care complications over a number of years; or there may be a physical reason why individuals undergoing early colostomy are more likely to experience rectal discharge. This merits further investigation.
In many cases where patients did report complications, the accompanying remark was that despite the complication they were still glad they had the colostomy. The colostomy was described as having “transformed my life,” “made bowel care easier,” enabled individuals to go on holiday for the first time since injury, and have significantly improved QOL. The fact that only one patient had their colostomy reversed adds weight to these statements and suggests individuals view complications of their colostomy as less significant than complications they experienced with traditional bowel care.
The number of patients requiring further surgery was low. The early group had less surgery, but they have had their colostomies for a shorter length of time (between 1 and 4 years) compared to the later group (between 1 and 12 years). There is no evidence that having a colostomy early leads to a greater risk of needing further surgery.
Parastomal hernia rate in the general population with end colostomy is between 4% and 48.1%.29 Our data found a low hernia rate of 8.3% in our spinally injured population. This is comparable to previous findings of 13%22 and 9.4%18 rates of parastomal hernia in those with a spinal injury.
It may be of value to reconsider whether a pyramid model1 is still the most appropriate way to approach bowel care in the newly spinally injured patient. Colostomy sits at the apex of the pyramid, historically the last resort, but our early patient group is choosing this much earlier and for reasons other than simply to regulate bowel function.
Bowel care interventions may need to be tailored more individually and holistically. Consideration should be made of psychological and social needs, including the patients' likelihood of returning to work and their physical need to achieve regular bowel evacuation. We suggest bowel care methods that most suit individual needs, including colostomy, should be discussed without reference to a progressive hierarchy of interventions.
Conclusion
Evidence so far supports early colostomy during rehabilitation following SCI to be safe and beneficial to patients who request it. It can increase patient independence and reduce the need for caregiver support on discharge from hospital. The shift toward early colostomy may require health care professionals to reconsider the role of colostomy. It is no longer being used solely to relieve intractable bowel complications; it is being adopted early by patients to facilitate independence following SCI and make bowel care more acceptable to them. It is an option that all patients should be made aware of during early rehabilitation.
Future work
The research into our patient group is ongoing. Further work is needed to find out why early colostomates experience more rectal discharge than those who have it done at a later stage post SCI. The significance of age, body image, and relationship status on the decision to choose early colostomy formation merits investigation. The benefit of colostomy early in SCI rehabilitation in adaptation and increasing independence needs further research.
Limitations of the study
Stoma department patient records were more extensive for those operated on since 2013 when records became electronic, and less complete information was available for those patients whose stoma care was transferred to another area when the patients left hospital. The method of gathering data from medical and nursing notes gives only the recorded professional understanding of patient experiences. The use of a questionnaire to allow patients to self-report complications may give a different and more complete picture.
The true extent of stoma-related complications may not be known, if patients are self-managing problems without seeking help from medical staff or stoma care nurses.
The first recorded early colostomies were recorded in 2013. It is not yet known whether more bowel-related complications will arise over the longer term.
Invitation for correspondence
The authors welcome comment on what is observed and practiced here. It would be of benefit to hear of the current practices and trends in other spinal units. Correspondence should be directed to the corresponding author.
Funding Support
Mr. Branagan, Mrs. Boucher, Mrs. Bryan, and Mrs. Dukes report grants from the Association of Stoma Care Nurses during the conduct of the study.
REFERENCES
- 1.Multidisciplinary Association of Spinal Cord Injury Professionals Guidelines for management of neurogenic bowel dysfunction in individuals with central neurological conditions. 2012 http://wwwmascipcouk/Homeaspx Accessed July 23, 2018.
- 2.Coggrave M, McCreath A. Bowel management following spinal cordinjury. Bucking hamshire Hospitals NHS Trust. 2007 http://www.buckshealthcare.nhs.uk/Downloads/Patient-leaflets-NSIC/Bowel%20management%20following%20spinal%20cord%20injury.pdf Accessed July 23, 2018.
- 3.Pryor J, Fisher M, Middleton J. Management of the neurogenic bowel for adults with spinal cord injuries. Agency for Clinical Innovation; Chatswood, NSW, Australia: 2014. https://www.aci.health.nsw.gov.au/__data/assets/pdf_file/0019/155215/Management-Neurogenic-Bowel.pdf Accessed July 23, 2018. [Google Scholar]
- 4.Coggrave M, Norton C, Wilson-Barnett J. Management of neurogenic bowel dysfunction in the community after spinal cord injury: A postal survey in the United Kingdom. Spinal Cord. 2009;47(4):323–330. doi: 10.1038/sc.2008.137. [DOI] [PubMed] [Google Scholar]
- 5.Krogh K, Nielsen J, Djurhuus JC, Mosdal C, Sabroe S, Laurberg S. Colorectal function in patients with spinal cord lesions. Dis Colon Rectum. 1997;40(10):1233–1239. doi: 10.1007/BF02055170. [DOI] [PubMed] [Google Scholar]
- 6.Craven ML, Etchells J. A review of the outcome of stoma surgery on spinal cord injured patients. J Adv Nurs. 1998;27(5):922–926. doi: 10.1046/j.1365-2648.1998.00582.x. [DOI] [PubMed] [Google Scholar]
- 7.Williams LM, Shem K, Patel A. Persistent autonomic dysreflexia due to bowel care in spinal cord injured men: A case series. Am J Phys Med Rehabil. 2014:a84-a. [Google Scholar]
- 8.Kirk PM, King RB, Temple R, Bourjaily J, Thomas P. Long-term follow-up of bowel management after spinal cord injury. SCI Nurs. 1997;14(2):56–63. [PubMed] [Google Scholar]
- 9.Menter R, Weitzenkamp D, Cooper D, Bingley J, Charlifue S, Whiteneck G. Bowel management outcomes in individuals with long-term spinal cord injuries. Spinal Cord. 1997;35:608–612. doi: 10.1038/sj.sc.3100461. [DOI] [PubMed] [Google Scholar]
- 10.Stone JM, Wolfe VA, Nino-Murcia M, Perkash I. Colostomy as treatment for complications of spinal cord injury. Arch Phys Med Rehabil. 1990;71(7):514–518. [PubMed] [Google Scholar]
- 11.Bølling Hansen R, Staun M, Kalhauge A, Langholz E, Biering-Sørensen F. Bowel function and quality of life after colostomy in individuals with spinal cord injury. J Spinal Cord Med. 2016;39(3):281–289. doi: 10.1179/2045772315Y.0000000006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nielsen SD, Faaborg PM, Finnerup NB, Christensen P, Krogh K. Ageing with neurogenic bowel dysfunction. Spinal Cord. 2017 doi: 10.1038/sc.2017.22. [DOI] [PubMed] [Google Scholar]
- 13.Savic G, Charlifue S, Glass C, Soni BM, Gerhart KA, Jamous MA. British ageing with SCI study: Changes in physical and psychosocial outcomes over time. Top Spinal Cord Inj Rehabil. 2010;15(3):41–53. [Google Scholar]
- 14.Anderson KD. Targeting recovery: Priorities of the spinal cord-injured population. J Neurotrauma. 2004;21(10):1371–1383. doi: 10.1089/neu.2004.21.1371. [DOI] [PubMed] [Google Scholar]
- 15.Simpson LA, Eng JJ, Hsieh JTC, Wolfe DL. The health and life priorities of individuals with spinal cord injury: A systematic review. J Neurotrauma. 2012;29(8):1548–1555. doi: 10.1089/neu.2011.2226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Smith PH, Decter RM. Antegrade continence enema procedure: Impact on quality of life in patients with spinal cord injury. Spinal Cord. 2015;53(3):213–215. doi: 10.1038/sc.2014.223. [DOI] [PubMed] [Google Scholar]
- 17.Christensen P, Kvitzau B, Krogh K, Buntzen S, Laurberg S. Neurogenic colorectal dysfunction - use of new antegrade and retrograde colonic wash-out methods. Spinal Cord. 2000;38(4):255–261. doi: 10.1038/sj.sc.3100991. [DOI] [PubMed] [Google Scholar]
- 18.Branagan G, Tromans A, Finnis D. Effect of stoma formation on bowel care and quality of life in patients with spinal cord injury. Spinal Cord. 2003;41(12):680–683. doi: 10.1038/sj.sc.3101529. [DOI] [PubMed] [Google Scholar]
- 19.Hocevar B, Gray M. Intestinal diversion (colostomy or ileostomy) in patients with severe bowel dysfunction following spinal cord injury. J Wound Ostomy Continence Nurs. 2008;35(2):159–166. doi: 10.1097/01.WON.0000313638.29623.40. [DOI] [PubMed] [Google Scholar]
- 20.Saltzstein RJ, Romano J. The efficacy of colostomy as a bowel management alternative in selected spinal cord injury patients. J Am Paraplegia Soc. 1990;13(2):9–13. doi: 10.1080/01952307.1990.11735808. [DOI] [PubMed] [Google Scholar]
- 21.Rosito O, Nino-Murcia M, Wolfe VA, Kiratli BJ, Perkash I. The effects of colostomy on the quality of life in patients with spinal cord injury: A retrospective analysis. J Spinal Cord Med. 2002;25(3):174. doi: 10.1080/10790268.2002.11753619. [DOI] [PubMed] [Google Scholar]
- 22.Coggrave MJ, Ingram RM, Gardner BP, Norton CS. The impact of stoma for bowel management after spinal cord injury. Spinal Cord. 2012;50(11):848–852. doi: 10.1038/sc.2012.66. [DOI] [PubMed] [Google Scholar]
- 23.Munck J, Simoens C, Thill V et al. Intestinal stoma in patients with spinal cord injury: A retrospective study of 23 patients. Hepato-Gastroenterology. 2008;55(88):2125–2129. [PubMed] [Google Scholar]
- 24.Clavien P, Barkun J, de Oliveira M et al. The Clavien-Dindo classification of surgical complications: Five-year experience. Ann Surg. 2009;250(2):187–196. doi: 10.1097/SLA.0b013e3181b13ca2. [DOI] [PubMed] [Google Scholar]
- 25.Boucher M. Early elective colostomy following spinal cord injury. Br J Nurs. 2016;25(5):S4–S10. doi: 10.12968/bjon.2016.25.5.S4. [DOI] [PubMed] [Google Scholar]
- 26.Lai JM, Chuang TY, Francisco GE, Strayer JR. Diversion colitis: A cause of abdominal discomfort in spinal cord injury patients with colostomy. Arch Phys Med Rehabil; Presented as a poster at the 57th Annual Assembly of the American Academy of Physical Medicine and Rehabilitation; Orlando, FL. November 16–20, 1995; 1997. pp. 670–671. [DOI] [PubMed] [Google Scholar]
- 27.Burckhardt C, Anderson K. The Quality of Life Scale (QOLS): Reliability, validity, and utilization. Health Qual Life Outcomes. 2003;1:60–7. doi: 10.1186/1477-7525-1-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kennedy P, Hasson L. Return-to-work intentions during spinal cord injury rehabilitation: An audit of employment outcomes. Spinal Cord. 2016;54(2):141. doi: 10.1038/sc.2015.122. [DOI] [PubMed] [Google Scholar]
- 29.Carne P, Robertson G, Frizelle F. Parastomal hernia. Br J Surg. 2003;90(7):784–793. doi: 10.1002/bjs.4220. [DOI] [PubMed] [Google Scholar]


