Abstract
Objectives: To identify and classify tools for assessing the influence of neurogenic bowel dysfunction (NBD) on quality of life (QoL) after spinal cord injury (SCI). Methods: In this systematic review, MEDLINE/PubMed, CINAHL, and PsycInfo were searched to identify studies assessing the influence of NBD on QoL (or related construct) after SCI. Two independent reviewers screened titles and abstracts, and both reviewers classified tools as subjective or objective according to Dijkers' theoretical QoL framework. Results: Seventy-two studies were identified, and 35 studies met the inclusion criteria. Five objective measures assessed the influence of NBD on QoL, which were validated for use in SCI, but no measure was condition-specific to NBD. Eight measures were classified as subjective tools; two had an established reliability and validity for SCI while six had some psychometric evidence for use in the SCI population. Five subjective measures (NBD score, Burwood QoL Questionnaire, Impediments to Community Integration [ICI] Scale, SCI-QoL Bowel Management Difficulties, and Survey of Neurogenic Bowel Characteristics) were developed specifically for SCI. The NBD score showed sensitivity to the influence of NBD on QoL in experimental trials. Conclusion: Thirteen tools assessed the influence of NBD on QoL in SCI. Although not developed specifically for SCI, the Health Utility Index (HUI-III) was the only tool identified that provided data on “QoL as utility” on the impact of NBD. The validated NBD score was the only condition-specific tool to assess QoL as “subjective well-being.” Further validation of existing tools could help to inform practice and policy related to resource allocation for bowel care post SCI.
Keywords: neurogenic bowel dysfunction, outcome measurement, quality of life, spinal cord injury, systematic review
Timely and complete bowel evacuation without complication and/or continence are issues of central importance to persons with neurogenic bowel dysfunction (NBD) following spinal cord injury (SCI), their families, community supports, and health care providers.1,2 In fact, bowel incontinence was reported to be the greatest source of social discomfort following SCI.3 Further, recovery of bowel function was perceived to be more important than walking by individuals with SCI.1 NBD has been reported to adversely influence the daily activities and lifestyle of 40% to 60% of individuals living with SCI.4,5
Symptoms of NBD vary depending on whether the individual has an upper motor neuron bowel (persistent constipation) or a lower motor neuron bowel (persistent incontinence).2 Therefore, the complications associated with NBD are quite diverse and include (but are not limited to) abdominal distension, autonomic dysreflexia, hemorrhoids, anal fissure, and rectal prolapse.6 In severe cases, approximately 25% of individuals with long-term SCI require hospitalization for gastrointestinal complications.4,7
Dissatisfaction with bowel management is associated with lower perceived QoL, with issues of time, pain or discomfort, and poor results (ineffective evacuation) being the most commonly reported.8 While most individuals with SCI achieve adequate bowel management strategies,9 the time to complete their bowel movements, dependence on others, and unpredictability continue to impact social participation and QoL.8–13 For example, in a survey of 1,200 individuals with SCI, incontinence negatively affected the QoL in 62% of respondents.10 Individuals with higher level injuries were more likely to require assistance with bowel management, which could also adversely impact QoL.10 Moreover, if assistance was provided by family members, there may be associated emotional distress and negative impacts on relationships.11 Consequently, NBD can impede a person with SCI from participating in recreational and other social activities, resuming employment following injury, or returning to school.14
Advancing treatments for bowel management after SCI have the potential to improve participation and QoL.14–18 However, accurately measuring individual progress and treatment effects on QoL requires the use of condition-specific (ie, QoL specific to NBD) validated outcome tools. Part of the challenge when selecting QoL outcomes is that a concrete definition of QoL is lacking, and there is little agreement regarding how to best measure it.19 Few QoL tools are developed for a specific population or health condition; thus, many outcomes do not capture all important constructs. Specific to NBD after SCI, there are a number of issues not accounted for in existing outcome tools.14,18 For example, existing outcome tools do not distinguish between upper motor neuron versus lower motor neuron NBD. Moreover, most tools focus predominantly on the body structures and function domains of the International Classification of Functioning, Disability and Health (ICF) framework and exclude or fail to consider personal and environmental factors and participation in community activities.14,17
In response to an identified need, for the appropriate selection of outcome tools to assess the influence of SCI-related secondary health conditions on QoL, the application of Dijkers's theoretical QoL framework has been useful.20 In particular, this framework classifies outcome measures as either assessing QoL from an objective perspective (ie, societal viewpoint) or a subjective one (ie, personal viewpoint).21,22 As a result of this classification approach, clinicians and researchers canmakeinformedchoicesaboutthebestQoLtools to use.20 QoL outcomes related to the influence of spasticity, pressure ulcers, and neurogenic bladder have been classified and documented using the aforementioned framework.23–25
Objective measures are based on the assumption that there is widespread consensus on the constituents of QoL,19,22 meaning that objective measures focus on external conditions and contain items that can be defined and quantified to reflect societal standards. Conversely, subjective measures follow a more individualistic approach and the assumption that QoL can only be judged by the individual or individual's experiencing it.26 Each perspective has inherent advantages and disadvantages in their measurement approach.21 Objective measures can be used to inform decision-makers on how to allocate funds and resources for various interventions, whereas subjective measures can provide patients with a means of describing to health professionals how their condition influences their QoL in terms of both their physical health and overall well-being. To date, there has been one systematic review on the influence of NBD post SCI, however it was not exclusively focused on QoL or selection of QoL measures.17
Given the substantial influence that NBD can have on QoL post SCI, and the need to advance measurement science to ensure that new treatments capture clinically meaningful changes, the purpose of this review was to (1) identify outcome measures that assess the influence of NBD on QoL and related constructs (eg, social participation) after SCI; (2) classify each outcome according to Dijkers's framework; and (3) summarize the psychometric properties of each tool.
Methods
A systematic review of the literature published between January 1975 and June 2016 was conducted using multiple online databases (MEDLINE/PubMed, CINAHL, and PsycInfo). No limit was set on publication date to ensure that all relevant articles on the topic could be identified. To identify relevant articles presenting QoL tools for assessing NBD in adults with SCI, we used the key words “spinal cord injuries” and its variants, along with the following terms: neurogenic bowel dysfunction, quality of life, participation, personal or life satisfaction, and activities of daily living. The reference lists of identified articles were also reviewed. Studies eligible for inclusion were written in English, included adult participants of whom at least 50% of the sample were persons with SCI, and contained one or more tools assessing the influence of NBD on QoL (or a related construct, such as social participation). Studies that examined global constructs of QoL post SCI, did not link QoL with NBD, contained pediatric populations or pediatric-onset SCI, or were primary qualitative studies were excluded.
Two raters independently conducted searches and then rated the titles and abstracts. Consensus on the selected abstracts was attained, and then relevant full-text articles were abstracted. If consensus could not be reached regarding article inclusion, a third rater was available for consultation. Descriptive information related to study design, participants, outcomes, and related findings were abstracted into a summary table (see Table 1). QoL outcomes were then classified according to Dijkers' theoretical framework by one rater and verified by a second rater.19,22
Table 1.
Identified studies
|
DESIGN Author (year) Research design |
METHODS (Objective, Population, Bowel Dysfunction Assessment, QoL Outcome Measures) |
QoL RESULTS |
|---|---|---|
| Adriaansen et al (2015)55 Cross-sectional multicenter study |
Objective: Describe bowel management & its outcomes in individuals living with an SCI for at least 10 yrs. Population: Individuals (N=258; age range, 28–65 yrs) who acquired their SCI between 18 & 35 yrs of age, who were at least 10 yr post-SCI, & who used a wheelchair for their daily mobility. NBD Assessment: International SCI Bowel Function Basic Data Set. QoL Outcome Measures: NBD score, a simple rating scale. |
1. Severe NBD was present in 36% of all participants & in 40% of those using a conservative method. However, only 14% were (very) dissatisfied with their current bowel management. 2. Dissatisfaction with bowel management was significantly associated with constipation & severe NBD. 3. With increasing time since injury, there was a nonsignificant trend observed toward a decline in dissatisfaction with bowel management & a significant decline in severe NBD. |
| Anson et al (1993)44 Cross-sectional & longitudinal survey |
Objective: Explore relationships among social support, adjustment, & secondary complications in persons with SCI. Population: 125 persons with SCI, 18 yrs + YPI > 1 yr. NBD Assessment: SCI QLI QoL Outcome Measures: SCI QLI; RSS scale. |
4. Social adjustment was associated with the number of diarrhea events. 5. Getting advice was negatively (r = −.029) associated with number of diarrhea events (p < .05). 6. No differences in diarrhea or constipation between high- & low-level support groups. |
| Branagan et al (2003)43 Cross-sectional survey |
Objective: Evaluate the effect of intestinal stoma formation in SCI patients. Population: 32 (27 men) patients with SCI (tetraplegia, paraplegia), mean age at onset 28.9 (range, 6–62 yrs), mean time of injury to stoma formation 17.1 mos (0–36.25). NBD Assessment: Presence of stoma QoL Outcome Measures: Nonstandardized study-specific questionnaire. |
1 18 patients reported that a stoma gave them ↑ independence, 12 reported no difference, & 1 felt his independence ↓ despite a significant ↓ time spent in bowel care. 2. QoL after stoma formation was described as much better by 25 patients, as better by 5, & QoL as worse by 1. |
| Christensen et al (2000)31 Cross-sectional survey |
Objective: Evaluate an ECC & MACE in patients with SCI. Population: 21 patients (10 men) with SCI offered ECC, mean age 39.9 (range, 7±72 yrs). 8 patients with SCI (3 men) + MACE, mean age 32.8 (range, 15–66 yrs). NBD Assessment: Single capsule with 24 or 10 radiopaque markers followed by abdominal X-ray; bowel management techniques. QoL Outcome Measures: Nonstandardized study-specific questionnaire. |
1. Before treatment with the ECC, 7 out of 11 patients available for follow-up felt that colorectal dysfunction imposed a major restriction on their QoL & social activities. 2. Before treatment with the ECC, 2 patients reported some restrictions, 1 reported a minor restriction, & 1 failed to answer the question. 3. At follow-up, 2 patients reported that colorectal dysfunction caused only some or little restriction & 3 patients reported no restriction. 4. At follow-up, 2 felt some restriction, 6 reported a minor restriction, & 6 reported no restriction. 5. Before MACE, 3 out of 5 patients were available at follow-up. |
| Christensen et al (2006)29 Prospective, randomized controlled multicenter trial |
Objective: Compare outcomes of transanal irrigation vs conservative bowel management in patients with SCI. Population: 87 patients (18 men) with SCI, median age 31.6 ± 13.3 yrs. NBD Assessment: St. Mark's Fecal Incontinence; CCCSS; Modified American Society of Colorectal Surgeon fecal incontinence scores. QoL Outcome Measures: NBD score |
1. Compared with conservative bowel management, transanal irrigation improves constipation, fecal incontinence, & symptom-related QoL. |
| Christensen et al (2008)28 Prospective, randomizedcontrolled multicenter trial |
Objective: Compare the symptoms of NBD in patients with SCI at baseline & after 10 weeks of treatment with transanal irrigation & identify possible factors that could predict treatment outcome. Population: 62 patients (45 men) with SCI (supraconal conal/cauda equina, complete, incomplete), mean age 47.5 ±15.5. NBD Assessment: Transanal irrigation, CCCSS; St. Mark's Fecal Incontinence. QoL Outcome Measures: NBD score |
1. Scores on the NBD improved from baseline to termination (p < .0001). 2. Regression analyses revealed that there was a reduction in the impact of bowel dysfunction on QoL but depended significantly on complete injury, being male, & ability to walk & varied significantly between study centres. |
| Coggrave et al (2009)45 Cross-sectional survey |
Objective: Describe bowel management in community dwelling persons with SCI & explore associations between age, injury, dependency problems, interventions, & satisfaction. Population: 1,334 persons (73.4% men) with SCI, median age 52 (19–91 yrs), median YPI 18 (1–65 yrs). NBD Assessment: Self-report (survey). QoL Outcome Measures: Nonstandardized study-specific questionnaire. |
1. Bowel dysfunction impacted on life activities to varying degrees & impact of bowel dysfunction was rated as significantly ↑ (p .001) than other aspects of SCI. 2. 20% of respondents were dissatisfied or very dissatisfied with bowel management & low satisfaction was associated with more frequent incontinence (p < .001), more problems (p < .001), longer duration of care (p< .001), more management (p = .008), & more interventions used (p < .001). |
| Coggrave et al (2013)15 Multicentre, retrospective self-report postal survey |
Objective: Characterize SCI individuals with a stoma, their stoma management & outcomes, identify sources of information & support for decision making & explore the impact of a stoma on life satisfaction. Population: 92 individuals, mean age 56 yrs, mean duration of injury 26 yrs, 91% with colostomy, 9% ileostomy. NBD Assessment: Self-report (survey). QoL Outcome Measures: Nonstandardized study-specific questionnaire (accompanied by TSCS, SWLS, & HADS) & 3-item nonstandardized questionnaire. |
1. Satisfaction with stoma was high; provision of sufficient information preoperatively was important, those with ileostomy were more dependent & less satisfied. 2. Life satisfaction & physical self-concept were both lower in this sample than in previously reported samples of SCI individuals without reported bowel difficulties or stoma. |
| Craven et al (2012)46 Cross-sectional survey |
Objective: Describe the relationships between secondary health conditions & health preference post SCI. Population: 357 persons (218 men) with SCI (AIS A-D), mean age 54.0 (range, 24–89), mean YPI 19.3 (range, 2–65). NBD Assessment: Bowel dysfunction item from the SCS. QoL Outcome Measures: HUI-III. |
1. Persons in no/mild bowel dysfunction group had ↑ (p < .0001) HUI-III scores than those in the moderate/severe bowel dysfunction group. |
| Del Popolo et al (2008)37 Pre-post intervention |
Objective: Evaluate the effects of Peristeen Anal Irrigation on NBD & QoL. Population: 36 patients (18 men) with SCI, median age 31.6 ± 13.3 yrs. NBD Assessment: Function, duration of the evacuation disorder, method of defecation, dietary supplements, the need for assistance for evacuation & the predominant intestinal symptom during/after defecation, NBD. QoL Outcome Measures: Nonstandardized study-specific questionnaire. |
1. Patient's opinions of their QoL score & degree of satisfaction ↑ from pre- to post-intervention (p = .001). 2. A high percentage of patients reported a change in their level of dependency after the treatment period. |
| Faaborg et al (2008)56 Longitudinal |
Objective: Describe long-term colorectal function in SCI patients. Population: 72 patients (48 men) with SCI, mean age 38.0 ± 11.9 yrs, YPI 37.5 ± 45.2 mos. NBD Assessment: Self-reported constipation, obstructed defecation, & fecal incontinence (survey). QoL Outcome Measures: Non-standardized study specific questionnaire; NBD score. |
1. The impact of colorectal dysfunction causing some or major restrictions on QoL or social activities ↑ from 25% to 38% from 1996 to 2006 (p < .005). 2. The impact of constipation influencing QoL ↑ from 15% to 23% from 1996 to 2006 (p < .15). |
| Glickman & Kamm (1996)4 Cross-sectional survey |
Objective: Determine the prevalence, nature, & effects – both physical & psychological – of SCI on bowel function. Population: 115 outpatients (77% men) with SCI, median age 38 (18–75 yrs), median YPI 62 (9–491 mos). NBD Assessment: Self-report (survey). QoL Outcome Measures: HADS; non-standardized questionnaire. |
1. Bowel dysfunction was a source of psychological distress in 54% of patients & was associated with time required for bowel management (p = .005) & frequency of incontinence (p = .001). 2. HADS scores correlated significantly with time taken for bowel management. 3. Bowel management problems were rated above urinary problems & not far below loss of mobility, impaired sexual function, & dependence. |
| Han et al (1998)47 Cross-sectional survey |
Objective: Investigate the characteristics of chronic GI problems & bowel dysfunction in patients with SCI. Population: 72 patients (48 men) with SCI, mean age 38.0 ± 11.9 yrs, YPI 37.5 ± 45.2 mos. NBD Assessment: Self-report (survey). QoL Outcome Measures: MBI Score. |
1. Bowel dysfunction was unrelated to age, duration, & neurological level of SCI, ASIA score, or level of activity. 2. Post-SCI GI problems were mainly bowel problems such as defecation difficulty (40.3%) & this affected ADL. |
| Hicken et al (2001)39 Case-control |
Objective: Examined the QoL among individuals with SCI requiring assistance for bowel & bladder management compared to those with independent control of their bladders & bowels. Population: 53 matched pairs (49% men): (1) bladder/bowel dependent individuals & (2) bladder/bowel independent individuals, mean age 37.02 yrs, YPI divided into 4 groups (1, 2–5, 6–15, >16 yrs). Groups matched on age, sex, education, race, & lesion level. NBD Assessment: FIM. QoL Outcome Measures: CHART; SWLS; SF-12. |
1. The bladder/bowel-dependent individuals reported ↓ life satisfaction & greater overall handicap (p < .001). In particular, persons who were bladder dependent had lower CHART subscale scores than bladder independent group on the following: physical independence (p < .001), mobility (p < .001), & occupational functioning (p < .05). 2. The bladder/bowel independent group initiated more social contact with strangers compared to bladder/bowel-dependent individuals (p = .056). 3. Although there were no group differences concerning social integration, the bladder/bowel-dependent group may have more difficulties initiating new social relationships. |
| Kachourbos & Creasey (2000)32 Post-intervention cross-sectional survey |
Objective: Assess recollections of health & QoL preoperatively in relation to bladder & bowel care & rate changes in QoL post-implant of an implantable stimulator. Population: 16 persons with SCI, 6 mos post surgery. NBD Assessment: Presence of implantable stimulator. QoL Outcome Measures: Non-standardized study specific questionnaire. |
1. Bowel program times were reduced from a mean of 5.4 hr per week preoperatively to 2.0 hr per week postoperatively. 2. Respondents reported a greater sense of independence, ↑ socialization, greater control over their lives, improved interpersonal relationships, improved self-image, ↓ feelings of depression, & an overall improvement in QoL. |
| Kelly et al (1999)30 Retrospective chart review & cross-sectional survey |
Objective: Evaluate the long-term outcomes of intestinal stomas post-SCI. Population: 14 patients (16 men) with SCI, mean age 54.8 yrs at time of stoma, mean time from SCI to stoma 15 yrs. NBD Assessment: Presence of stoma. QoL Outcome Measures: Nonstandardized study specific questionnaire. Similar to Dijker's typical QoL measure of ADL. |
1. Ten patients reported that colostomy was beneficial to their QoL. One person whose QoL remained unchanged post colostomy reported worse QoL at 10-yr follow-up. |
| Kim (2012)48 Cross-sectional survey |
Objective: Describe defecation stimulation methods & their outcomes & investigate the impact of bowel dysfunction on QoL in SCI. Population: 388 persons with SCI (295 men), mean age 44.5±10.8 yrs, mean YPI 14.2±9.5 yrs. NBD Assessment: Bowel stimulation method, frequency of bowel movements, defecation time, symptoms of AD, frequency of fecal incontinence, & flatus. QoL Outcome Measures: Nonstandardized study-specific questionnaire. |
1. Frequency of fecal incontinence had the greatest effects on QoL. 2. When patients had fecal incontinence every day, they had 67.4 times greater chance to obtain severely lowered general QoL. 3. Time taken in defecation >60 min, presence of perianal skin problem, & flatus incontinence also significantly influenced QoL. 4. QoL deterioration differs between each stimulation user. Decline in general QoL was greater in large-volume enemas users than in DRS users. 5. Social QoL deterioration was much more profound in large-volume enemas users than in DRS or finger evacuations users. 6. QoL at home was lower in patients using large-volume enemas than in those using other methods. 7. Mini-enema users had worse QoL at home than digital rectal stim users |
| Kirk et al (1997)5 Cross-sectional survey |
Objective: Describe impact of NBD on life activities. Population: 171 adults (128 men) with SCI, mean age 39.5 ± 14.5 yrs, mean YPI 8.9 ± 8.9. NBD Assessment: Self-report (survey). QoL Outcome Measures: Nonstandardized study-specific questionnaire (Bowel Program Outcome Questionnaire). |
1. 61% indicated NBD interfered with their life. 2. 47 of 105 respondents described a loss of freedom to go places, missing work, school or social events, or having to plan their lives around their bowels. |
| Krogh et al (1997)50 Cross-sectional survey |
Objective: Describe the frequency & severity of colorectal problems among patients with spinal cord lesions & determine whether these problems are associated with age, gender, time since lesion, level & severity of lesion. Population: 424 persons with SCI (300 men), mean age 41 (range 8–88 yrs), YPI 41 (range 0–59 yrs). NBD Assessment: Self-report (survey). QoL Outcome Measures: Nonstandardized study-specific questionnaire. |
1. 39% reported colorectal dysfunction caused some/major restrictions on social activities or QoL. 2. 29% reported disturbed defecation caused some/major restriction on social activities & 32% reported it caused some/major restriction on QoL. 3. 19% reported fecal incontinence caused some/major restriction on social activities & 20% reported it caused some/major restriction on QoL. 4. 30% reported bowel dysfunction was ↑ than bladder or sexual dysfunction. |
| Krogh et al (2006)49 Cross-sectional survey |
Objective: Develop & validate a symptom-based score for the NBD score. Population: 424 persons (72% men) with SCI, mean age 41 (8–88 yrs), mean YPI 14 (0–88 yrs). NBD Assessment: NBD score. QoL Outcome Measures: NBD score. |
1. Several items on the NBD found the impact on QoL ↑ with the severity of symptoms. Frequency of bowel movements was associated with QoL (p < .0001), as was frequency of fecal incontinence. 2. Difference in NBD scores among patients reporting no, little, some, or major impacts on QoL were significant (p < .001). 3. There may be an association between self-reported QoL & restriction of social activities due to bowel dysfunction. |
| Liu et al (2009)51 Cross-sectional survey |
Objective: Assess the relationship between the severity of NBD & HrQoL in persons with various degrees of SCI. Population: 128 (95 men) respondents with SCI, 36 with tetraplegia, 58 with paraplegia, 34 with paresis, mean age 48.3 (range 13–84 yrs), YPI divided into 4 groups (1–2 yrs, 3–5 yrs, 6–10 yrs, & over 10 yrs). NBD Assessment: NBD score. QoL Outcome Measures: SF-36; NBD score. |
1. Persons with very minor NBD had the ↑ scores on the SF-36 in contrast to persons with severe NBD, who had the ↓scores. 2. Significant differences were found on the SF-36 physical functioning (p < .001) & the physical component summary (p < .001) subscales. 3. Participants with worse NBD were likely to have ↓physical QoL (p < .001). |
| Lombardi (2010)33 Retrospective non-blinded design without controls. |
Objective: Evaluate the efficacy & safety of sacral neuromodulation in incomplete SCI affected by chronic NBD. Population: 23 patients with SCI (13 men), mean age 36±9 yrs. NBD Assessment: Wexner Score; episodes of fecal incontinence, no. of evacuations/week. QoL Outcome Measures: SF-36. |
1. Patients in both groups (constipation & fecal incontienence) had significant ↓ (p < .05) in Wexner scores. 2. QoL in both groups consistently showed statistical improvement (p < .05). |
| Lombardi et al (2011)34 Retrospective cross-sectional survey |
Objective: Assess the concomitant clinical improvement in incomplete SCI with NBD using sacral neuromodulation. Population: 75 patients with incomplete SCI. NBD Assessment: Incontinence & constipation. QoL Outcome Measures: SF-36. |
1. Bladder function & incontinence improved. 2. In the general & mental health domains of the SF-36, all patients improved their scores by at least 20% compared with baseline after sacral neuromodulation. |
| Luther et al (2005)40 Case-control |
Objective: Compare QoL for people with NBD & SCI using either a standard care program or colostomy. Population: 74 veterans (73 men) with SCI + colostomy, 296 SCI controls without colostomy, age range < 20–89, YPI within past 20 yr. NBD Assessment: Presence of colostomy. QoL Outcome Measures: IBDQ. |
1. No significant differences were detected on IBDQ between persons with SCI + colostomy & those with SCI only. |
| Lynch et al (2000)10 Controlled, descriptive & comparative questionnaire study |
Objective: Describe the bowel function of SCI patients & compare it to a general community control group. Population: 467 SCI patients & 467 control subjects were age & gender matched. Mean age for the SCI patients 43.5 (range, 15–89 yrs), mean YPI 14 (range, 0.7–42.1 yrs). Mean age for the controls 45.3 (range, 17–78 yr). NBD Assessment: General bowel function, incidence of incontinence, & defecation methods. QoL Outcome Measures: Nonstandardized questionnaire. |
1. Incontinence affected the QoL for 62% SCI patients compared to 8% of the controls. 2. Incontinence did not affect the majority of the controls (92.3%) in terms of everyday activities compared to 43.9% of SCI patients (p < .0001). |
| Noonan et al (2008)52 Cross-sectional survey |
Objective: Determine the effect of associated SCI conditions on health status & QoL. Population: 70 persons (57 men) with central cord syndrome, mean age at injury 45±18 yrs (range, 13–91), mean age at follow-up 51 ±18 yrs (range, 19–95). NBD Assessment: Self-report (survey). QoL Outcome Measures: SF-36; numeric QoL rating. |
1. Bowel, bladder & sexual dysfunction on the physical component score of the SF-36 were significant, but the effect ↓ when controlling for personal & confounding factors. 2. Bowel, bladder & sexual dysfunction were not related to the mental component scores of the SF-36. 3. Problems with bowel, bladder, & sexual dysfunction were significantly (p< .01) associated with QoL when personal & confounding factors were NOT controlled for. |
| Pardee et al (2012)8 Exploratory, descriptive correlational design |
Objective: Investigate the association between characteristics of individuals with SCI & neurogenic bowel & their perceived QoL. Population: 241 surveys; from adults over age 18, diagnosed with SCI & neurogenic bowel more than 2 yrs post injury, AIS of A, B, C, or D & residing in the community. NBD Assessment: Survey of neurogenic bowel characteristics. QoL Outcome Measures: QoL survey. |
1. Regardless of the bowel management program 54% (n = 127) were satisfied with current methods. Although time reported to complete bowel programs ranged from 1 to 120 min, there was no difference in rating of satisfaction with time. 2. There was a statistically significant difference between those satisfied & dissatisfied with current bowel management & QoL; those satisfied demonstrated a higher QoL on 3 subscales, work function (p = .021), bowel problems (p < .001), & social function (p < .001). Those dissatisfied with their bowel program perceived a lower QoL & indicated problem of time (p = .001), pain or discomfort (p = .033), & poor results (p < .001). |
| Randell et al (2001)41 Prospective controlled comparative analysis |
Objective: Determine whether a colostomy changes QoL in patients with SCI. Population: 26 (15 men) patients with SCI (tetraplegia, paraplegia) + colostomy, age range 22–87, range of injury to stoma formation 7 mos – 20 yrs. 26 SCI controls (age, gender, injury, & YPI matched) without colostomy. NBD Assessment: Presence of colostomy. QoL Outcome Measures: Burwood QoL Questionnaire. |
1. No significant differences were detected on QoL between persons with SCI + colostomy & those with SCI only. |
| Roach et al (2000)53 Cross-sectional survey |
Objective: Examine the relationship between bowel dysfunction, impediment to community integration & QoL in persons with SCI. Population: 103 SCI consumers (76.7% men), mean age 39 yrs, YPI 14 yr. NBD Assessment: Self-report (survey). QoL Outcome Measures: Andrews & Withey (1976) Life Satisfaction Survey; nonstandardized study specific questionnaire on community integration (ICI). |
1. Significant negative relationship between subjective severity & 3 ICI measures; the higher the perceived severity of bowel dysfunction, the more it affected (1) personal relationships (p < .01); (2) feelings about themselves (p < .01); (3) their home environment (p < .05). 2. The number of days each month a person stayed at home because of lack of bowel control was associated with all 3 ICI scales (p < .01). The ↑ bowel accidents per month, the ↑ negative a respondent felt about him/herself (p < .05). 3. None of the bowel dysfunction characteristics were significantly related to the satisfaction of life items, but non-parametric analyses revealed that 2 of the ICI items were associated with satisfaction with free time & family life. |
| Rosito et al (2002)35 Pre-post intervention |
Objective: Evaluate the effects of colostomy on the QoL in patients with SCI. Population: 27 patients (26 men) with SCI, mean age of 62.9 (range 44–79 yrs), YPI 25.8 (range 8–48 yrs), mean time since stoma formation 8 (range 1.5–28 yrs), mean time with severe bowel dysfunction 5.5 (range 0.5–18 yr). NBD Assessment: Presence of colostomy. QoL Outcome Measures: Nonstandardized study specific questionnaire. Similar to Dijker's typical QoL measure of ADL. |
1. Colostomy improved (p ≤ .0001) total QoL. 2. Significant improvements after colostomy observed in physical health, self-efficacy, psychosocial status, & recreation/leisure but not in body image. 3. 85% of patients reported an ↑ in total QoL after colostomy; 70% of patients were satisfied with their personal lives before colostomy compared to 89% of patients after colostomy. 4. 67% of patients felt more independent after colostomy compared to 30% of patients that felt the same level of independence. |
| Safadi et al (2003)36 Retrospective chart review & cross-sectional survey |
Objective: Evaluate the long-term outcomes of colostomies & ileostomies post SCI. Population: 45 patients (44 men) with SCI, mean age 55.9 yrs, mean time from SCI to stoma 20.3 yrs. NBD Assessment: Presence of stoma. QoL Outcome Measures: Nonstandardized study specific questionnaire. |
1. In the right-sided colostomy group (n=20), QoL & health status scores improved (p < .05). 2. In the left-sided colostomy group (n=20), QoL & health status scores improved (p < .05). 3. In the ileostomy group (n=7), QoL & health status scores improved (p < .05). |
| Teichman et al (2003)79 Retrospective review |
Objective: To determine the long-term outcomes from the Malone antegrade continence enema (ACE) procedure in adult neurogenic patients. Population: 6 patients (mean age = 35 yrs), mean follow-up of 4.5 yrs. NBD Assessment: Pre-ACE & post-ACE toileting times, bowel continence status, & complications. QoL Outcome Measures: Nonstandardized questionnaire. |
1. Five patients (83%) were satisfied with their outcome & rated their QoL higher after the ACE procedure compared with pre-ACE. |
| Westgren & Levi (1998)54 Cross-sectional survey |
Objective: Determine associations between major outcome variables after SCI & QoL. Population: 320 persons (261 men) with SCI, mean age 42 (17–78 yr), YPI ≤4 yrs & ≥4 yrs. NBD Assessment: Medical records via clinical database. QoL Outcome Measures: SF-36. |
1. Bowel dysfunction was associated with ↓ QoL. 2. Bowel dysfunction yielded a medium effect sizes in the general physical functioning (p = .001), bodily pain (p = .003), general health (p = .001), vitality (p = .001), social function (p = .004), & mental health (p = .001) subscales. |
| Worsøe et al (2008)42 Retrospective chart review & cross-sectional survey |
Objective: Evaluate the long-term outcomes of ACE & ACE + colostomy in patients with SCI. Population: 80 patients (12 men) with SCI, mean age 51 yrs at time of stoma, mean follow-up time was 75 mos (range, 3–183). NBD Assessment: Continued ACE or ACE+colostomy at follow-up; Wexner score. QoL Outcome Measures: Nonstandardized study-specific questionnaire. |
1. 34 of 43 patients still using ACE were satisfied or very satisfied with the result, 8 patients were neither satisfied nor dissatisfied, & none were dissatisfied or very dissatisfied. One person did not provide a response. 2. On an arbitrary scale (0–100) mean values for bowel function before & after were 12 & 81 respectively (p < .01). For social function, the corresponding values were 30 & 81 (p < .01) & for QoL they were 28 & 81 (p < .01). |
| Tulsky et al (2015)57 Mixed-methods design |
Objective: To describe the development & psychometric properties of the SCI-QoL Bladder Management Difficulties & Bowel Management Difficulties item banks & Bladder Complications scale. Population: 757 adults with traumatic SCI of traumatic etiology, 18 yrs of age & older. NBD Assessment: N/A QoL Outcome Measures: In development. |
1. The SCI-QoL Bladder Management Difficulties & Bowel Management Difficulties item banks are psychometrically robust & are available as computer adaptive tests or short forms. |
Note: Studies are listed in alphabetical order according to the last name of the first author. ACE = antegrade colonic enema; AD = autonomic dysreflexia; ADL = activities of daily living; AIS = American Spinal Injury Association Impairment Scale; CHART = Criag Handicap and Assessment Reporting Technique; CCCSS = Cleveland Clinic Constipation Scoring System; DRS = digital rectal stimulation; ECC = enema continence catheter; FIM = Functional Independence Measure; GI = gastrointestinal; HADS = Hospital Anxiety & Depression Scale; HrQoL = health-related quality of life; HUI = Health Utilities Index; ICI = impediments to community integration; MBI = Modified Barthel Index; mos = months; NBD = neurogenic bowel dysfunction; N/A = not available; QLI = Quality of Life Index; QoL = quality of life; RSS = Reciprocal Support Scale; SCI = spinal cord injury(ies); SCS = Secondary Condition Scale; SF-12 = Short-Form 12; SF-36 = Short-Form 36; SWLS = Satisfaction with Life Scale; YPI = years post injury; yr(s) = years.
Table 1.
Identified studies (CONT.)
|
DESIGN Author (year) Research design |
METHODS (Objective, Population, Bowel Dysfunction Assessment, QoL Outcome Measures) |
QoL RESULTS |
|---|---|---|
| Adriaansen et al (2015)55 Cross-sectional multicenter study |
Objective: Describe bowel management & its outcomes in individuals living with an SCI for at least 10 yrs. Population: Individuals (N=258; age range, 28–65 yrs) who acquired their SCI between 18 & 35 yrs of age, who were at least 10 yr post-SCI, & who used a wheelchair for their daily mobility. NBD Assessment: International SCI Bowel Function Basic Data Set. QoL Outcome Measures: NBD score, a simple rating scale. |
1. Severe NBD was present in 36% of all participants & in 40% of those using a conservative method. However, only 14% were (very) dissatisfied with their current bowel management. 2. Dissatisfaction with bowel management was significantly associated with constipation & severe NBD. 3. With increasing time since injury, there was a nonsignificant trend observed toward a decline in dissatisfaction with bowel management & a significant decline in severe NBD. |
| Anson et al (1993)44 Cross-sectional & longitudinal survey |
Objective: Explore relationships among social support, adjustment, & secondary complications in persons with SCI. Population: 125 persons with SCI, 18 yrs + YPI > 1 yr. NBD Assessment: SCI QLI QoL Outcome Measures: SCI QLI; RSS scale. |
4. Social adjustment was associated with the number of diarrhea events. 5. Getting advice was negatively (r = −.029) associated with number of diarrhea events (p < .05). 6. No differences in diarrhea or constipation between high- & low-level support groups. |
| Branagan et al (2003)43 Cross-sectional survey |
Objective: Evaluate the effect of intestinal stoma formation in SCI patients. Population: 32 (27 men) patients with SCI (tetraplegia, paraplegia), mean age at onset 28.9 (range, 6–62 yrs), mean time of injury to stoma formation 17.1 mos (0–36.25). NBD Assessment: Presence of stoma QoL Outcome Measures: Nonstandardized study-specific questionnaire. |
1 18 patients reported that a stoma gave them ↑ independence, 12 reported no difference, & 1 felt his independence ↓ despite a significant ↓ time spent in bowel care. 2. QoL after stoma formation was described as much better by 25 patients, as better by 5, & QoL as worse by 1. |
| Christensen et al (2000)31 Cross-sectional survey |
Objective: Evaluate an ECC & MACE in patients with SCI. Population: 21 patients (10 men) with SCI offered ECC, mean age 39.9 (range, 7±72 yrs). 8 patients with SCI (3 men) + MACE, mean age 32.8 (range, 15–66 yrs). NBD Assessment: Single capsule with 24 or 10 radiopaque markers followed by abdominal X-ray; bowel management techniques. QoL Outcome Measures: Nonstandardized study-specific questionnaire. |
1. Before treatment with the ECC, 7 out of 11 patients available for follow-up felt that colorectal dysfunction imposed a major restriction on their QoL & social activities. 2. Before treatment with the ECC, 2 patients reported some restrictions, 1 reported a minor restriction, & 1 failed to answer the question. 3. At follow-up, 2 patients reported that colorectal dysfunction caused only some or little restriction & 3 patients reported no restriction. 4. At follow-up, 2 felt some restriction, 6 reported a minor restriction, & 6 reported no restriction. 5. Before MACE, 3 out of 5 patients were available at follow-up. |
| Christensen et al (2006)29 Prospective, randomized controlled multicenter trial |
Objective: Compare outcomes of transanal irrigation vs conservative bowel management in patients with SCI. Population: 87 patients (18 men) with SCI, median age 31.6 ± 13.3 yrs. NBD Assessment: St. Mark's Fecal Incontinence; CCCSS; Modified American Society of Colorectal Surgeon fecal incontinence scores. QoL Outcome Measures: NBD score |
1. Compared with conservative bowel management, transanal irrigation improves constipation, fecal incontinence, & symptom-related QoL. |
| Christensen et al (2008)28 Prospective, randomizedcontrolled multicenter trial |
Objective: Compare the symptoms of NBD in patients with SCI at baseline & after 10 weeks of treatment with transanal irrigation & identify possible factors that could predict treatment outcome. Population: 62 patients (45 men) with SCI (supraconal conal/cauda equina, complete, incomplete), mean age 47.5 ±15.5. NBD Assessment: Transanal irrigation, CCCSS; St. Mark's Fecal Incontinence. QoL Outcome Measures: NBD score |
1. Scores on the NBD improved from baseline to termination (p < .0001). 2. Regression analyses revealed that there was a reduction in the impact of bowel dysfunction on QoL but depended significantly on complete injury, being male, & ability to walk & varied significantly between study centres. |
| Coggrave et al (2009)45 Cross-sectional survey |
Objective: Describe bowel management in community dwelling persons with SCI & explore associations between age, injury, dependency problems, interventions, & satisfaction. Population: 1,334 persons (73.4% men) with SCI, median age 52 (19–91 yrs), median YPI 18 (1–65 yrs). NBD Assessment: Self-report (survey). QoL Outcome Measures: Nonstandardized study-specific questionnaire. |
1. Bowel dysfunction impacted on life activities to varying degrees & impact of bowel dysfunction was rated as significantly ↑ (p .001) than other aspects of SCI. 2. 20% of respondents were dissatisfied or very dissatisfied with bowel management & low satisfaction was associated with more frequent incontinence (p < .001), more problems (p < .001), longer duration of care (p< .001), more management (p = .008), & more interventions used (p < .001). |
| Coggrave et al (2013)15 Multicentre, retrospective self-report postal survey |
Objective: Characterize SCI individuals with a stoma, their stoma management & outcomes, identify sources of information & support for decision making & explore the impact of a stoma on life satisfaction. Population: 92 individuals, mean age 56 yrs, mean duration of injury 26 yrs, 91% with colostomy, 9% ileostomy. NBD Assessment: Self-report (survey). QoL Outcome Measures: Nonstandardized study-specific questionnaire (accompanied by TSCS, SWLS, & HADS) & 3-item nonstandardized questionnaire. |
1. Satisfaction with stoma was high; provision of sufficient information preoperatively was important, those with ileostomy were more dependent & less satisfied. 2. Life satisfaction & physical self-concept were both lower in this sample than in previously reported samples of SCI individuals without reported bowel difficulties or stoma. |
| Craven et al (2012)46 Cross-sectional survey |
Objective: Describe the relationships between secondary health conditions & health preference post SCI. Population: 357 persons (218 men) with SCI (AIS A-D), mean age 54.0 (range, 24–89), mean YPI 19.3 (range, 2–65). NBD Assessment: Bowel dysfunction item from the SCS. QoL Outcome Measures: HUI-III. |
1. Persons in no/mild bowel dysfunction group had ↑ (p < .0001) HUI-III scores than those in the moderate/severe bowel dysfunction group. |
| Del Popolo et al (2008)37 Pre-post intervention |
Objective: Evaluate the effects of Peristeen Anal Irrigation on NBD & QoL. Population: 36 patients (18 men) with SCI, median age 31.6 ± 13.3 yrs. NBD Assessment: Function, duration of the evacuation disorder, method of defecation, dietary supplements, the need for assistance for evacuation & the predominant intestinal symptom during/after defecation, NBD. QoL Outcome Measures: Nonstandardized study-specific questionnaire. |
1. Patient's opinions of their QoL score & degree of satisfaction ↑ from pre- to post-intervention (p = .001). 2. A high percentage of patients reported a change in their level of dependency after the treatment period. |
| Faaborg et al (2008)56 Longitudinal |
Objective: Describe long-term colorectal function in SCI patients. Population: 72 patients (48 men) with SCI, mean age 38.0 ± 11.9 yrs, YPI 37.5 ± 45.2 mos. NBD Assessment: Self-reported constipation, obstructed defecation, & fecal incontinence (survey). QoL Outcome Measures: Non-standardized study specific questionnaire; NBD score. |
1. The impact of colorectal dysfunction causing some or major restrictions on QoL or social activities ↑ from 25% to 38% from 1996 to 2006 (p < .005). 2. The impact of constipation influencing QoL ↑ from 15% to 23% from 1996 to 2006 (p < .15). |
| Glickman & Kamm (1996)4 Cross-sectional survey |
Objective: Determine the prevalence, nature, & effects – both physical & psychological – of SCI on bowel function. Population: 115 outpatients (77% men) with SCI, median age 38 (18–75 yrs), median YPI 62 (9–491 mos). NBD Assessment: Self-report (survey). QoL Outcome Measures: HADS; non-standardized questionnaire. |
1. Bowel dysfunction was a source of psychological distress in 54% of patients & was associated with time required for bowel management (p = .005) & frequency of incontinence (p = .001). 2. HADS scores correlated significantly with time taken for bowel management. 3. Bowel management problems were rated above urinary problems & not far below loss of mobility, impaired sexual function, & dependence. |
| Han et al (1998)47 Cross-sectional survey |
Objective: Investigate the characteristics of chronic GI problems & bowel dysfunction in patients with SCI. Population: 72 patients (48 men) with SCI, mean age 38.0 ± 11.9 yrs, YPI 37.5 ± 45.2 mos. NBD Assessment: Self-report (survey). QoL Outcome Measures: MBI Score. |
1. Bowel dysfunction was unrelated to age, duration, & neurological level of SCI, ASIA score, or level of activity. 2. Post-SCI GI problems were mainly bowel problems such as defecation difficulty (40.3%) & this affected ADL. |
| Hicken et al (2001)39 Case-control |
Objective: Examined the QoL among individuals with SCI requiring assistance for bowel & bladder management compared to those with independent control of their bladders & bowels. Population: 53 matched pairs (49% men): (1) bladder/bowel dependent individuals & (2) bladder/bowel independent individuals, mean age 37.02 yrs, YPI divided into 4 groups (1, 2–5, 6–15, >16 yrs). Groups matched on age, sex, education, race, & lesion level. NBD Assessment: FIM. QoL Outcome Measures: CHART; SWLS; SF-12. |
1. The bladder/bowel-dependent individuals reported ↓ life satisfaction & greater overall handicap (p < .001). In particular, persons who were bladder dependent had lower CHART subscale scores than bladder independent group on the following: physical independence (p < .001), mobility (p < .001), & occupational functioning (p < .05). 2. The bladder/bowel independent group initiated more social contact with strangers compared to bladder/bowel-dependent individuals (p = .056). 3. Although there were no group differences concerning social integration, the bladder/bowel-dependent group may have more difficulties initiating new social relationships. |
| Kachourbos & Creasey (2000)32 Post-intervention cross-sectional survey |
Objective: Assess recollections of health & QoL preoperatively in relation to bladder & bowel care & rate changes in QoL post-implant of an implantable stimulator. Population: 16 persons with SCI, 6 mos post surgery. NBD Assessment: Presence of implantable stimulator. QoL Outcome Measures: Non-standardized study specific questionnaire. |
1. Bowel program times were reduced from a mean of 5.4 hr per week preoperatively to 2.0 hr per week postoperatively. 2. Respondents reported a greater sense of independence, ↑ socialization, greater control over their lives, improved interpersonal relationships, improved self-image, ↓ feelings of depression, & an overall improvement in QoL. |
| Kelly et al (1999)30 Retrospective chart review & cross-sectional survey |
Objective: Evaluate the long-term outcomes of intestinal stomas post-SCI. Population: 14 patients (16 men) with SCI, mean age 54.8 yrs at time of stoma, mean time from SCI to stoma 15 yrs. NBD Assessment: Presence of stoma. QoL Outcome Measures: Nonstandardized study specific questionnaire. Similar to Dijker's typical QoL measure of ADL. |
1. Ten patients reported that colostomy was beneficial to their QoL. One person whose QoL remained unchanged post colostomy reported worse QoL at 10-yr follow-up. |
| Kim (2012)48 Cross-sectional survey |
Objective: Describe defecation stimulation methods & their outcomes & investigate the impact of bowel dysfunction on QoL in SCI. Population: 388 persons with SCI (295 men), mean age 44.5±10.8 yrs, mean YPI 14.2±9.5 yrs. NBD Assessment: Bowel stimulation method, frequency of bowel movements, defecation time, symptoms of AD, frequency of fecal incontinence, & flatus. QoL Outcome Measures: Nonstandardized study-specific questionnaire. |
1. Frequency of fecal incontinence had the greatest effects on QoL. 2. When patients had fecal incontinence every day, they had 67.4 times greater chance to obtain severely lowered general QoL. 3. Time taken in defecation >60 min, presence of perianal skin problem, & flatus incontinence also significantly influenced QoL. 4. QoL deterioration differs between each stimulation user. Decline in general QoL was greater in large-volume enemas users than in DRS users. 5. Social QoL deterioration was much more profound in large-volume enemas users than in DRS or finger evacuations users. 6. QoL at home was lower in patients using large-volume enemas than in those using other methods. 7. Mini-enema users had worse QoL at home than digital rectal stim users |
| Kirk et al (1997)5 Cross-sectional survey |
Objective: Describe impact of NBD on life activities. Population: 171 adults (128 men) with SCI, mean age 39.5 ± 14.5 yrs, mean YPI 8.9 ± 8.9. NBD Assessment: Self-report (survey). QoL Outcome Measures: Nonstandardized study-specific questionnaire (Bowel Program Outcome Questionnaire). |
1. 61% indicated NBD interfered with their life. 2. 47 of 105 respondents described a loss of freedom to go places, missing work, school or social events, or having to plan their lives around their bowels. |
| Krogh et al (1997)50 Cross-sectional survey |
Objective: Describe the frequency & severity of colorectal problems among patients with spinal cord lesions & determine whether these problems are associated with age, gender, time since lesion, level & severity of lesion. Population: 424 persons with SCI (300 men), mean age 41 (range 8–88 yrs), YPI 41 (range 0–59 yrs). NBD Assessment: Self-report (survey). QoL Outcome Measures: Nonstandardized study-specific questionnaire. |
1. 39% reported colorectal dysfunction caused some/major restrictions on social activities or QoL. 2. 29% reported disturbed defecation caused some/major restriction on social activities & 32% reported it caused some/major restriction on QoL. 3. 19% reported fecal incontinence caused some/major restriction on social activities & 20% reported it caused some/major restriction on QoL. 4. 30% reported bowel dysfunction was ↑ than bladder or sexual dysfunction. |
| Krogh et al (2006)49 Cross-sectional survey |
Objective: Develop & validate a symptom-based score for the NBD score. Population: 424 persons (72% men) with SCI, mean age 41 (8–88 yrs), mean YPI 14 (0–88 yrs). NBD Assessment: NBD score. QoL Outcome Measures: NBD score. |
1. Several items on the NBD found the impact on QoL ↑ with the severity of symptoms. Frequency of bowel movements was associated with QoL (p < .0001), as was frequency of fecal incontinence. 2. Difference in NBD scores among patients reporting no, little, some, or major impacts on QoL were significant (p < .001). 3. There may be an association between self-reported QoL & restriction of social activities due to bowel dysfunction. |
| Liu et al (2009)51 Cross-sectional survey |
Objective: Assess the relationship between the severity of NBD & HrQoL in persons with various degrees of SCI. Population: 128 (95 men) respondents with SCI, 36 with tetraplegia, 58 with paraplegia, 34 with paresis, mean age 48.3 (range 13–84 yrs), YPI divided into 4 groups (1–2 yrs, 3–5 yrs, 6–10 yrs, & over 10 yrs). NBD Assessment: NBD score. QoL Outcome Measures: SF-36; NBD score. |
1. Persons with very minor NBD had the ↑ scores on the SF-36 in contrast to persons with severe NBD, who had the ↓scores. 2. Significant differences were found on the SF-36 physical functioning (p < .001) & the physical component summary (p < .001) subscales. 3. Participants with worse NBD were likely to have ↓physical QoL (p < .001). |
| Lombardi (2010)33 Retrospective non-blinded design without controls. |
Objective: Evaluate the efficacy & safety of sacral neuromodulation in incomplete SCI affected by chronic NBD. Population: 23 patients with SCI (13 men), mean age 36±9 yrs. NBD Assessment: Wexner Score; episodes of fecal incontinence, no. of evacuations/week. QoL Outcome Measures: SF-36. |
1. Patients in both groups (constipation & fecal incontienence) had significant ↓ (p < .05) in Wexner scores. 2. QoL in both groups consistently showed statistical improvement (p < .05). |
| Lombardi et al (2011)34 Retrospective cross-sectional survey |
Objective: Assess the concomitant clinical improvement in incomplete SCI with NBD using sacral neuromodulation. Population: 75 patients with incomplete SCI. NBD Assessment: Incontinence & constipation. QoL Outcome Measures: SF-36. |
1. Bladder function & incontinence improved. 2. In the general & mental health domains of the SF-36, all patients improved their scores by at least 20% compared with baseline after sacral neuromodulation. |
| Luther et al (2005)40 Case-control |
Objective: Compare QoL for people with NBD & SCI using either a standard care program or colostomy. Population: 74 veterans (73 men) with SCI + colostomy, 296 SCI controls without colostomy, age range < 20–89, YPI within past 20 yr. NBD Assessment: Presence of colostomy. QoL Outcome Measures: IBDQ. |
1. No significant differences were detected on IBDQ between persons with SCI + colostomy & those with SCI only. |
| Lynch et al (2000)10 Controlled, descriptive & comparative questionnaire study |
Objective: Describe the bowel function of SCI patients & compare it to a general community control group. Population: 467 SCI patients & 467 control subjects were age & gender matched. Mean age for the SCI patients 43.5 (range, 15–89 yrs), mean YPI 14 (range, 0.7–42.1 yrs). Mean age for the controls 45.3 (range, 17–78 yr). NBD Assessment: General bowel function, incidence of incontinence, & defecation methods. QoL Outcome Measures: Nonstandardized questionnaire. |
1. Incontinence affected the QoL for 62% SCI patients compared to 8% of the controls. 2. Incontinence did not affect the majority of the controls (92.3%) in terms of everyday activities compared to 43.9% of SCI patients (p < .0001). |
| Noonan et al (2008)52 Cross-sectional survey |
Objective: Determine the effect of associated SCI conditions on health status & QoL. Population: 70 persons (57 men) with central cord syndrome, mean age at injury 45±18 yrs (range, 13–91), mean age at follow-up 51 ±18 yrs (range, 19–95). NBD Assessment: Self-report (survey). QoL Outcome Measures: SF-36; numeric QoL rating. |
1. Bowel, bladder & sexual dysfunction on the physical component score of the SF-36 were significant, but the effect ↓ when controlling for personal & confounding factors. 2. Bowel, bladder & sexual dysfunction were not related to the mental component scores of the SF-36. 3. Problems with bowel, bladder, & sexual dysfunction were significantly (p< .01) associated with QoL when personal & confounding factors were NOT controlled for. |
| Pardee et al (2012)8 Exploratory, descriptive correlational design |
Objective: Investigate the association between characteristics of individuals with SCI & neurogenic bowel & their perceived QoL. Population: 241 surveys; from adults over age 18, diagnosed with SCI & neurogenic bowel more than 2 yrs post injury, AIS of A, B, C, or D & residing in the community. NBD Assessment: Survey of neurogenic bowel characteristics. QoL Outcome Measures: QoL survey. |
1. Regardless of the bowel management program 54% (n = 127) were satisfied with current methods. Although time reported to complete bowel programs ranged from 1 to 120 min, there was no difference in rating of satisfaction with time. 2. There was a statistically significant difference between those satisfied & dissatisfied with current bowel management & QoL; those satisfied demonstrated a higher QoL on 3 subscales, work function (p = .021), bowel problems (p < .001), & social function (p < .001). Those dissatisfied with their bowel program perceived a lower QoL & indicated problem of time (p = .001), pain or discomfort (p = .033), & poor results (p < .001). |
| Randell et al (2001)41 Prospective controlled comparative analysis |
Objective: Determine whether a colostomy changes QoL in patients with SCI. Population: 26 (15 men) patients with SCI (tetraplegia, paraplegia) + colostomy, age range 22–87, range of injury to stoma formation 7 mos – 20 yrs. 26 SCI controls (age, gender, injury, & YPI matched) without colostomy. NBD Assessment: Presence of colostomy. QoL Outcome Measures: Burwood QoL Questionnaire. |
1. No significant differences were detected on QoL between persons with SCI + colostomy & those with SCI only. |
| Roach et al (2000)53 Cross-sectional survey |
Objective: Examine the relationship between bowel dysfunction, impediment to community integration & QoL in persons with SCI. Population: 103 SCI consumers (76.7% men), mean age 39 yrs, YPI 14 yr. NBD Assessment: Self-report (survey). QoL Outcome Measures: Andrews & Withey (1976) Life Satisfaction Survey; nonstandardized study specific questionnaire on community integration (ICI). |
1. Significant negative relationship between subjective severity & 3 ICI measures; the higher the perceived severity of bowel dysfunction, the more it affected (1) personal relationships (p < .01); (2) feelings about themselves (p < .01); (3) their home environment (p < .05). 2. The number of days each month a person stayed at home because of lack of bowel control was associated with all 3 ICI scales (p < .01). The ↑ bowel accidents per month, the ↑ negative a respondent felt about him/herself (p < .05). 3. None of the bowel dysfunction characteristics were significantly related to the satisfaction of life items, but non-parametric analyses revealed that 2 of the ICI items were associated with satisfaction with free time & family life. |
| Rosito et al (2002)35 Pre-post intervention |
Objective: Evaluate the effects of colostomy on the QoL in patients with SCI. Population: 27 patients (26 men) with SCI, mean age of 62.9 (range 44–79 yrs), YPI 25.8 (range 8–48 yrs), mean time since stoma formation 8 (range 1.5–28 yrs), mean time with severe bowel dysfunction 5.5 (range 0.5–18 yr). NBD Assessment: Presence of colostomy. QoL Outcome Measures: Nonstandardized study specific questionnaire. Similar to Dijker's typical QoL measure of ADL. |
1. Colostomy improved (p ≤ .0001) total QoL. 2. Significant improvements after colostomy observed in physical health, self-efficacy, psychosocial status, & recreation/leisure but not in body image. 3. 85% of patients reported an ↑ in total QoL after colostomy; 70% of patients were satisfied with their personal lives before colostomy compared to 89% of patients after colostomy. 4. 67% of patients felt more independent after colostomy compared to 30% of patients that felt the same level of independence. |
| Safadi et al (2003)36 Retrospective chart review & cross-sectional survey |
Objective: Evaluate the long-term outcomes of colostomies & ileostomies post SCI. Population: 45 patients (44 men) with SCI, mean age 55.9 yrs, mean time from SCI to stoma 20.3 yrs. NBD Assessment: Presence of stoma. QoL Outcome Measures: Nonstandardized study specific questionnaire. |
1. In the right-sided colostomy group (n=20), QoL & health status scores improved (p < .05). 2. In the left-sided colostomy group (n=20), QoL & health status scores improved (p < .05). 3. In the ileostomy group (n=7), QoL & health status scores improved (p < .05). |
| Teichman et al (2003)79 Retrospective review |
Objective: To determine the long-term outcomes from the Malone antegrade continence enema (ACE) procedure in adult neurogenic patients. Population: 6 patients (mean age = 35 yrs), mean follow-up of 4.5 yrs. NBD Assessment: Pre-ACE & post-ACE toileting times, bowel continence status, & complications. QoL Outcome Measures: Nonstandardized questionnaire. |
1. Five patients (83%) were satisfied with their outcome & rated their QoL higher after the ACE procedure compared with pre-ACE. |
| Westgren & Levi (1998)54 Cross-sectional survey |
Objective: Determine associations between major outcome variables after SCI & QoL. Population: 320 persons (261 men) with SCI, mean age 42 (17–78 yr), YPI ≤4 yrs & ≥4 yrs. NBD Assessment: Medical records via clinical database. QoL Outcome Measures: SF-36. |
1. Bowel dysfunction was associated with ↓ QoL. 2. Bowel dysfunction yielded a medium effect sizes in the general physical functioning (p = .001), bodily pain (p = .003), general health (p = .001), vitality (p = .001), social function (p = .004), & mental health (p = .001) subscales. |
| Worsøe et al (2008)42 Retrospective chart review & cross-sectional survey |
Objective: Evaluate the long-term outcomes of ACE & ACE + colostomy in patients with SCI. Population: 80 patients (12 men) with SCI, mean age 51 yrs at time of stoma, mean follow-up time was 75 mos (range, 3–183). NBD Assessment: Continued ACE or ACE+colostomy at follow-up; Wexner score. QoL Outcome Measures: Nonstandardized study-specific questionnaire. |
1. 34 of 43 patients still using ACE were satisfied or very satisfied with the result, 8 patients were neither satisfied nor dissatisfied, & none were dissatisfied or very dissatisfied. One person did not provide a response. 2. On an arbitrary scale (0–100) mean values for bowel function before & after were 12 & 81 respectively (p < .01). For social function, the corresponding values were 30 & 81 (p < .01) & for QoL they were 28 & 81 (p < .01). |
| Tulsky et al (2015)57 Mixed-methods design |
Objective: To describe the development & psychometric properties of the SCI-QoL Bladder Management Difficulties & Bowel Management Difficulties item banks & Bladder Complications scale. Population: 757 adults with traumatic SCI of traumatic etiology, 18 yrs of age & older. NBD Assessment: N/A QoL Outcome Measures: In development. |
1. The SCI-QoL Bladder Management Difficulties & Bowel Management Difficulties item banks are psychometrically robust & are available as computer adaptive tests or short forms. |
Note: Studies are listed in alphabetical order according to the last name of the first author. ACE = antegrade colonic enema; AD = autonomic dysreflexia; ADL = activities of daily living; AIS = American Spinal Injury Association Impairment Scale; CHART = Criag Handicap and Assessment Reporting Technique; CCCSS = Cleveland Clinic Constipation Scoring System; DRS = digital rectal stimulation; ECC = enema continence catheter; FIM = Functional Independence Measure; GI = gastrointestinal; HADS = Hospital Anxiety & Depression Scale; HrQoL = health-related quality of life; HUI = Health Utilities Index; ICI = impediments to community integration; MBI = Modified Barthel Index; mos = months; NBD = neurogenic bowel dysfunction; N/A = not available; QLI = Quality of Life Index; QoL = quality of life; RSS = Reciprocal Support Scale; SCI = spinal cord injury(ies); SCS = Secondary Condition Scale; SF-12 = Short-Form 12; SF-36 = Short-Form 36; SWLS = Satisfaction with Life Scale; YPI = years post injury; yr(s) = years.
Table 1.
Identified studies (CONT.)
|
DESIGN Author (year) Research design |
METHODS (Objective, Population, Bowel Dysfunction Assessment, QoL Outcome Measures) |
QoL RESULTS |
|---|---|---|
| Adriaansen et al (2015)55 Cross-sectional multicenter study |
Objective: Describe bowel management & its outcomes in individuals living with an SCI for at least 10 yrs. Population: Individuals (N=258; age range, 28–65 yrs) who acquired their SCI between 18 & 35 yrs of age, who were at least 10 yr post-SCI, & who used a wheelchair for their daily mobility. NBD Assessment: International SCI Bowel Function Basic Data Set. QoL Outcome Measures: NBD score, a simple rating scale. |
1. Severe NBD was present in 36% of all participants & in 40% of those using a conservative method. However, only 14% were (very) dissatisfied with their current bowel management. 2. Dissatisfaction with bowel management was significantly associated with constipation & severe NBD. 3. With increasing time since injury, there was a nonsignificant trend observed toward a decline in dissatisfaction with bowel management & a significant decline in severe NBD. |
| Anson et al (1993)44 Cross-sectional & longitudinal survey |
Objective: Explore relationships among social support, adjustment, & secondary complications in persons with SCI. Population: 125 persons with SCI, 18 yrs + YPI > 1 yr. NBD Assessment: SCI QLI QoL Outcome Measures: SCI QLI; RSS scale. |
4. Social adjustment was associated with the number of diarrhea events. 5. Getting advice was negatively (r = −.029) associated with number of diarrhea events (p < .05). 6. No differences in diarrhea or constipation between high- & low-level support groups. |
| Branagan et al (2003)43 Cross-sectional survey |
Objective: Evaluate the effect of intestinal stoma formation in SCI patients. Population: 32 (27 men) patients with SCI (tetraplegia, paraplegia), mean age at onset 28.9 (range, 6–62 yrs), mean time of injury to stoma formation 17.1 mos (0–36.25). NBD Assessment: Presence of stoma QoL Outcome Measures: Nonstandardized study-specific questionnaire. |
1 18 patients reported that a stoma gave them ↑ independence, 12 reported no difference, & 1 felt his independence ↓ despite a significant ↓ time spent in bowel care. 2. QoL after stoma formation was described as much better by 25 patients, as better by 5, & QoL as worse by 1. |
| Christensen et al (2000)31 Cross-sectional survey |
Objective: Evaluate an ECC & MACE in patients with SCI. Population: 21 patients (10 men) with SCI offered ECC, mean age 39.9 (range, 7±72 yrs). 8 patients with SCI (3 men) + MACE, mean age 32.8 (range, 15–66 yrs). NBD Assessment: Single capsule with 24 or 10 radiopaque markers followed by abdominal X-ray; bowel management techniques. QoL Outcome Measures: Nonstandardized study-specific questionnaire. |
1. Before treatment with the ECC, 7 out of 11 patients available for follow-up felt that colorectal dysfunction imposed a major restriction on their QoL & social activities. 2. Before treatment with the ECC, 2 patients reported some restrictions, 1 reported a minor restriction, & 1 failed to answer the question. 3. At follow-up, 2 patients reported that colorectal dysfunction caused only some or little restriction & 3 patients reported no restriction. 4. At follow-up, 2 felt some restriction, 6 reported a minor restriction, & 6 reported no restriction. 5. Before MACE, 3 out of 5 patients were available at follow-up. |
| Christensen et al (2006)29 Prospective, randomized controlled multicenter trial |
Objective: Compare outcomes of transanal irrigation vs conservative bowel management in patients with SCI. Population: 87 patients (18 men) with SCI, median age 31.6 ± 13.3 yrs. NBD Assessment: St. Mark's Fecal Incontinence; CCCSS; Modified American Society of Colorectal Surgeon fecal incontinence scores. QoL Outcome Measures: NBD score |
1. Compared with conservative bowel management, transanal irrigation improves constipation, fecal incontinence, & symptom-related QoL. |
| Christensen et al (2008)28 Prospective, randomizedcontrolled multicenter trial |
Objective: Compare the symptoms of NBD in patients with SCI at baseline & after 10 weeks of treatment with transanal irrigation & identify possible factors that could predict treatment outcome. Population: 62 patients (45 men) with SCI (supraconal conal/cauda equina, complete, incomplete), mean age 47.5 ±15.5. NBD Assessment: Transanal irrigation, CCCSS; St. Mark's Fecal Incontinence. QoL Outcome Measures: NBD score |
1. Scores on the NBD improved from baseline to termination (p < .0001). 2. Regression analyses revealed that there was a reduction in the impact of bowel dysfunction on QoL but depended significantly on complete injury, being male, & ability to walk & varied significantly between study centres. |
| Coggrave et al (2009)45 Cross-sectional survey |
Objective: Describe bowel management in community dwelling persons with SCI & explore associations between age, injury, dependency problems, interventions, & satisfaction. Population: 1,334 persons (73.4% men) with SCI, median age 52 (19–91 yrs), median YPI 18 (1–65 yrs). NBD Assessment: Self-report (survey). QoL Outcome Measures: Nonstandardized study-specific questionnaire. |
1. Bowel dysfunction impacted on life activities to varying degrees & impact of bowel dysfunction was rated as significantly ↑ (p .001) than other aspects of SCI. 2. 20% of respondents were dissatisfied or very dissatisfied with bowel management & low satisfaction was associated with more frequent incontinence (p < .001), more problems (p < .001), longer duration of care (p< .001), more management (p = .008), & more interventions used (p < .001). |
| Coggrave et al (2013)15 Multicentre, retrospective self-report postal survey |
Objective: Characterize SCI individuals with a stoma, their stoma management & outcomes, identify sources of information & support for decision making & explore the impact of a stoma on life satisfaction. Population: 92 individuals, mean age 56 yrs, mean duration of injury 26 yrs, 91% with colostomy, 9% ileostomy. NBD Assessment: Self-report (survey). QoL Outcome Measures: Nonstandardized study-specific questionnaire (accompanied by TSCS, SWLS, & HADS) & 3-item nonstandardized questionnaire. |
1. Satisfaction with stoma was high; provision of sufficient information preoperatively was important, those with ileostomy were more dependent & less satisfied. 2. Life satisfaction & physical self-concept were both lower in this sample than in previously reported samples of SCI individuals without reported bowel difficulties or stoma. |
| Craven et al (2012)46 Cross-sectional survey |
Objective: Describe the relationships between secondary health conditions & health preference post SCI. Population: 357 persons (218 men) with SCI (AIS A-D), mean age 54.0 (range, 24–89), mean YPI 19.3 (range, 2–65). NBD Assessment: Bowel dysfunction item from the SCS. QoL Outcome Measures: HUI-III. |
1. Persons in no/mild bowel dysfunction group had ↑ (p < .0001) HUI-III scores than those in the moderate/severe bowel dysfunction group. |
| Del Popolo et al (2008)37 Pre-post intervention |
Objective: Evaluate the effects of Peristeen Anal Irrigation on NBD & QoL. Population: 36 patients (18 men) with SCI, median age 31.6 ± 13.3 yrs. NBD Assessment: Function, duration of the evacuation disorder, method of defecation, dietary supplements, the need for assistance for evacuation & the predominant intestinal symptom during/after defecation, NBD. QoL Outcome Measures: Nonstandardized study-specific questionnaire. |
1. Patient's opinions of their QoL score & degree of satisfaction ↑ from pre- to post-intervention (p = .001). 2. A high percentage of patients reported a change in their level of dependency after the treatment period. |
| Faaborg et al (2008)56 Longitudinal |
Objective: Describe long-term colorectal function in SCI patients. Population: 72 patients (48 men) with SCI, mean age 38.0 ± 11.9 yrs, YPI 37.5 ± 45.2 mos. NBD Assessment: Self-reported constipation, obstructed defecation, & fecal incontinence (survey). QoL Outcome Measures: Non-standardized study specific questionnaire; NBD score. |
1. The impact of colorectal dysfunction causing some or major restrictions on QoL or social activities ↑ from 25% to 38% from 1996 to 2006 (p < .005). 2. The impact of constipation influencing QoL ↑ from 15% to 23% from 1996 to 2006 (p < .15). |
| Glickman & Kamm (1996)4 Cross-sectional survey |
Objective: Determine the prevalence, nature, & effects – both physical & psychological – of SCI on bowel function. Population: 115 outpatients (77% men) with SCI, median age 38 (18–75 yrs), median YPI 62 (9–491 mos). NBD Assessment: Self-report (survey). QoL Outcome Measures: HADS; non-standardized questionnaire. |
1. Bowel dysfunction was a source of psychological distress in 54% of patients & was associated with time required for bowel management (p = .005) & frequency of incontinence (p = .001). 2. HADS scores correlated significantly with time taken for bowel management. 3. Bowel management problems were rated above urinary problems & not far below loss of mobility, impaired sexual function, & dependence. |
| Han et al (1998)47 Cross-sectional survey |
Objective: Investigate the characteristics of chronic GI problems & bowel dysfunction in patients with SCI. Population: 72 patients (48 men) with SCI, mean age 38.0 ± 11.9 yrs, YPI 37.5 ± 45.2 mos. NBD Assessment: Self-report (survey). QoL Outcome Measures: MBI Score. |
1. Bowel dysfunction was unrelated to age, duration, & neurological level of SCI, ASIA score, or level of activity. 2. Post-SCI GI problems were mainly bowel problems such as defecation difficulty (40.3%) & this affected ADL. |
| Hicken et al (2001)39 Case-control |
Objective: Examined the QoL among individuals with SCI requiring assistance for bowel & bladder management compared to those with independent control of their bladders & bowels. Population: 53 matched pairs (49% men): (1) bladder/bowel dependent individuals & (2) bladder/bowel independent individuals, mean age 37.02 yrs, YPI divided into 4 groups (1, 2–5, 6–15, >16 yrs). Groups matched on age, sex, education, race, & lesion level. NBD Assessment: FIM. QoL Outcome Measures: CHART; SWLS; SF-12. |
1. The bladder/bowel-dependent individuals reported ↓ life satisfaction & greater overall handicap (p < .001). In particular, persons who were bladder dependent had lower CHART subscale scores than bladder independent group on the following: physical independence (p < .001), mobility (p < .001), & occupational functioning (p < .05). 2. The bladder/bowel independent group initiated more social contact with strangers compared to bladder/bowel-dependent individuals (p = .056). 3. Although there were no group differences concerning social integration, the bladder/bowel-dependent group may have more difficulties initiating new social relationships. |
| Kachourbos & Creasey (2000)32 Post-intervention cross-sectional survey |
Objective: Assess recollections of health & QoL preoperatively in relation to bladder & bowel care & rate changes in QoL post-implant of an implantable stimulator. Population: 16 persons with SCI, 6 mos post surgery. NBD Assessment: Presence of implantable stimulator. QoL Outcome Measures: Non-standardized study specific questionnaire. |
1. Bowel program times were reduced from a mean of 5.4 hr per week preoperatively to 2.0 hr per week postoperatively. 2. Respondents reported a greater sense of independence, ↑ socialization, greater control over their lives, improved interpersonal relationships, improved self-image, ↓ feelings of depression, & an overall improvement in QoL. |
| Kelly et al (1999)30 Retrospective chart review & cross-sectional survey |
Objective: Evaluate the long-term outcomes of intestinal stomas post-SCI. Population: 14 patients (16 men) with SCI, mean age 54.8 yrs at time of stoma, mean time from SCI to stoma 15 yrs. NBD Assessment: Presence of stoma. QoL Outcome Measures: Nonstandardized study specific questionnaire. Similar to Dijker's typical QoL measure of ADL. |
1. Ten patients reported that colostomy was beneficial to their QoL. One person whose QoL remained unchanged post colostomy reported worse QoL at 10-yr follow-up. |
| Kim (2012)48 Cross-sectional survey |
Objective: Describe defecation stimulation methods & their outcomes & investigate the impact of bowel dysfunction on QoL in SCI. Population: 388 persons with SCI (295 men), mean age 44.5±10.8 yrs, mean YPI 14.2±9.5 yrs. NBD Assessment: Bowel stimulation method, frequency of bowel movements, defecation time, symptoms of AD, frequency of fecal incontinence, & flatus. QoL Outcome Measures: Nonstandardized study-specific questionnaire. |
1. Frequency of fecal incontinence had the greatest effects on QoL. 2. When patients had fecal incontinence every day, they had 67.4 times greater chance to obtain severely lowered general QoL. 3. Time taken in defecation >60 min, presence of perianal skin problem, & flatus incontinence also significantly influenced QoL. 4. QoL deterioration differs between each stimulation user. Decline in general QoL was greater in large-volume enemas users than in DRS users. 5. Social QoL deterioration was much more profound in large-volume enemas users than in DRS or finger evacuations users. 6. QoL at home was lower in patients using large-volume enemas than in those using other methods. 7. Mini-enema users had worse QoL at home than digital rectal stim users |
| Kirk et al (1997)5 Cross-sectional survey |
Objective: Describe impact of NBD on life activities. Population: 171 adults (128 men) with SCI, mean age 39.5 ± 14.5 yrs, mean YPI 8.9 ± 8.9. NBD Assessment: Self-report (survey). QoL Outcome Measures: Nonstandardized study-specific questionnaire (Bowel Program Outcome Questionnaire). |
1. 61% indicated NBD interfered with their life. 2. 47 of 105 respondents described a loss of freedom to go places, missing work, school or social events, or having to plan their lives around their bowels. |
| Krogh et al (1997)50 Cross-sectional survey |
Objective: Describe the frequency & severity of colorectal problems among patients with spinal cord lesions & determine whether these problems are associated with age, gender, time since lesion, level & severity of lesion. Population: 424 persons with SCI (300 men), mean age 41 (range 8–88 yrs), YPI 41 (range 0–59 yrs). NBD Assessment: Self-report (survey). QoL Outcome Measures: Nonstandardized study-specific questionnaire. |
1. 39% reported colorectal dysfunction caused some/major restrictions on social activities or QoL. 2. 29% reported disturbed defecation caused some/major restriction on social activities & 32% reported it caused some/major restriction on QoL. 3. 19% reported fecal incontinence caused some/major restriction on social activities & 20% reported it caused some/major restriction on QoL. 4. 30% reported bowel dysfunction was ↑ than bladder or sexual dysfunction. |
| Krogh et al (2006)49 Cross-sectional survey |
Objective: Develop & validate a symptom-based score for the NBD score. Population: 424 persons (72% men) with SCI, mean age 41 (8–88 yrs), mean YPI 14 (0–88 yrs). NBD Assessment: NBD score. QoL Outcome Measures: NBD score. |
1. Several items on the NBD found the impact on QoL ↑ with the severity of symptoms. Frequency of bowel movements was associated with QoL (p < .0001), as was frequency of fecal incontinence. 2. Difference in NBD scores among patients reporting no, little, some, or major impacts on QoL were significant (p < .001). 3. There may be an association between self-reported QoL & restriction of social activities due to bowel dysfunction. |
| Liu et al (2009)51 Cross-sectional survey |
Objective: Assess the relationship between the severity of NBD & HrQoL in persons with various degrees of SCI. Population: 128 (95 men) respondents with SCI, 36 with tetraplegia, 58 with paraplegia, 34 with paresis, mean age 48.3 (range 13–84 yrs), YPI divided into 4 groups (1–2 yrs, 3–5 yrs, 6–10 yrs, & over 10 yrs). NBD Assessment: NBD score. QoL Outcome Measures: SF-36; NBD score. |
1. Persons with very minor NBD had the ↑ scores on the SF-36 in contrast to persons with severe NBD, who had the ↓scores. 2. Significant differences were found on the SF-36 physical functioning (p < .001) & the physical component summary (p < .001) subscales. 3. Participants with worse NBD were likely to have ↓physical QoL (p < .001). |
| Lombardi (2010)33 Retrospective non-blinded design without controls. |
Objective: Evaluate the efficacy & safety of sacral neuromodulation in incomplete SCI affected by chronic NBD. Population: 23 patients with SCI (13 men), mean age 36±9 yrs. NBD Assessment: Wexner Score; episodes of fecal incontinence, no. of evacuations/week. QoL Outcome Measures: SF-36. |
1. Patients in both groups (constipation & fecal incontienence) had significant ↓ (p < .05) in Wexner scores. 2. QoL in both groups consistently showed statistical improvement (p < .05). |
| Lombardi et al (2011)34 Retrospective cross-sectional survey |
Objective: Assess the concomitant clinical improvement in incomplete SCI with NBD using sacral neuromodulation. Population: 75 patients with incomplete SCI. NBD Assessment: Incontinence & constipation. QoL Outcome Measures: SF-36. |
1. Bladder function & incontinence improved. 2. In the general & mental health domains of the SF-36, all patients improved their scores by at least 20% compared with baseline after sacral neuromodulation. |
| Luther et al (2005)40 Case-control |
Objective: Compare QoL for people with NBD & SCI using either a standard care program or colostomy. Population: 74 veterans (73 men) with SCI + colostomy, 296 SCI controls without colostomy, age range < 20–89, YPI within past 20 yr. NBD Assessment: Presence of colostomy. QoL Outcome Measures: IBDQ. |
1. No significant differences were detected on IBDQ between persons with SCI + colostomy & those with SCI only. |
| Lynch et al (2000)10 Controlled, descriptive & comparative questionnaire study |
Objective: Describe the bowel function of SCI patients & compare it to a general community control group. Population: 467 SCI patients & 467 control subjects were age & gender matched. Mean age for the SCI patients 43.5 (range, 15–89 yrs), mean YPI 14 (range, 0.7–42.1 yrs). Mean age for the controls 45.3 (range, 17–78 yr). NBD Assessment: General bowel function, incidence of incontinence, & defecation methods. QoL Outcome Measures: Nonstandardized questionnaire. |
1. Incontinence affected the QoL for 62% SCI patients compared to 8% of the controls. 2. Incontinence did not affect the majority of the controls (92.3%) in terms of everyday activities compared to 43.9% of SCI patients (p < .0001). |
| Noonan et al (2008)52 Cross-sectional survey |
Objective: Determine the effect of associated SCI conditions on health status & QoL. Population: 70 persons (57 men) with central cord syndrome, mean age at injury 45±18 yrs (range, 13–91), mean age at follow-up 51 ±18 yrs (range, 19–95). NBD Assessment: Self-report (survey). QoL Outcome Measures: SF-36; numeric QoL rating. |
1. Bowel, bladder & sexual dysfunction on the physical component score of the SF-36 were significant, but the effect ↓ when controlling for personal & confounding factors. 2. Bowel, bladder & sexual dysfunction were not related to the mental component scores of the SF-36. 3. Problems with bowel, bladder, & sexual dysfunction were significantly (p< .01) associated with QoL when personal & confounding factors were NOT controlled for. |
| Pardee et al (2012)8 Exploratory, descriptive correlational design |
Objective: Investigate the association between characteristics of individuals with SCI & neurogenic bowel & their perceived QoL. Population: 241 surveys; from adults over age 18, diagnosed with SCI & neurogenic bowel more than 2 yrs post injury, AIS of A, B, C, or D & residing in the community. NBD Assessment: Survey of neurogenic bowel characteristics. QoL Outcome Measures: QoL survey. |
1. Regardless of the bowel management program 54% (n = 127) were satisfied with current methods. Although time reported to complete bowel programs ranged from 1 to 120 min, there was no difference in rating of satisfaction with time. 2. There was a statistically significant difference between those satisfied & dissatisfied with current bowel management & QoL; those satisfied demonstrated a higher QoL on 3 subscales, work function (p = .021), bowel problems (p < .001), & social function (p < .001). Those dissatisfied with their bowel program perceived a lower QoL & indicated problem of time (p = .001), pain or discomfort (p = .033), & poor results (p < .001). |
| Randell et al (2001)41 Prospective controlled comparative analysis |
Objective: Determine whether a colostomy changes QoL in patients with SCI. Population: 26 (15 men) patients with SCI (tetraplegia, paraplegia) + colostomy, age range 22–87, range of injury to stoma formation 7 mos – 20 yrs. 26 SCI controls (age, gender, injury, & YPI matched) without colostomy. NBD Assessment: Presence of colostomy. QoL Outcome Measures: Burwood QoL Questionnaire. |
1. No significant differences were detected on QoL between persons with SCI + colostomy & those with SCI only. |
| Roach et al (2000)53 Cross-sectional survey |
Objective: Examine the relationship between bowel dysfunction, impediment to community integration & QoL in persons with SCI. Population: 103 SCI consumers (76.7% men), mean age 39 yrs, YPI 14 yr. NBD Assessment: Self-report (survey). QoL Outcome Measures: Andrews & Withey (1976) Life Satisfaction Survey; nonstandardized study specific questionnaire on community integration (ICI). |
1. Significant negative relationship between subjective severity & 3 ICI measures; the higher the perceived severity of bowel dysfunction, the more it affected (1) personal relationships (p < .01); (2) feelings about themselves (p < .01); (3) their home environment (p < .05). 2. The number of days each month a person stayed at home because of lack of bowel control was associated with all 3 ICI scales (p < .01). The ↑ bowel accidents per month, the ↑ negative a respondent felt about him/herself (p < .05). 3. None of the bowel dysfunction characteristics were significantly related to the satisfaction of life items, but non-parametric analyses revealed that 2 of the ICI items were associated with satisfaction with free time & family life. |
| Rosito et al (2002)35 Pre-post intervention |
Objective: Evaluate the effects of colostomy on the QoL in patients with SCI. Population: 27 patients (26 men) with SCI, mean age of 62.9 (range 44–79 yrs), YPI 25.8 (range 8–48 yrs), mean time since stoma formation 8 (range 1.5–28 yrs), mean time with severe bowel dysfunction 5.5 (range 0.5–18 yr). NBD Assessment: Presence of colostomy. QoL Outcome Measures: Nonstandardized study specific questionnaire. Similar to Dijker's typical QoL measure of ADL. |
1. Colostomy improved (p ≤ .0001) total QoL. 2. Significant improvements after colostomy observed in physical health, self-efficacy, psychosocial status, & recreation/leisure but not in body image. 3. 85% of patients reported an ↑ in total QoL after colostomy; 70% of patients were satisfied with their personal lives before colostomy compared to 89% of patients after colostomy. 4. 67% of patients felt more independent after colostomy compared to 30% of patients that felt the same level of independence. |
| Safadi et al (2003)36 Retrospective chart review & cross-sectional survey |
Objective: Evaluate the long-term outcomes of colostomies & ileostomies post SCI. Population: 45 patients (44 men) with SCI, mean age 55.9 yrs, mean time from SCI to stoma 20.3 yrs. NBD Assessment: Presence of stoma. QoL Outcome Measures: Nonstandardized study specific questionnaire. |
1. In the right-sided colostomy group (n=20), QoL & health status scores improved (p < .05). 2. In the left-sided colostomy group (n=20), QoL & health status scores improved (p < .05). 3. In the ileostomy group (n=7), QoL & health status scores improved (p < .05). |
| Teichman et al (2003)79 Retrospective review |
Objective: To determine the long-term outcomes from the Malone antegrade continence enema (ACE) procedure in adult neurogenic patients. Population: 6 patients (mean age = 35 yrs), mean follow-up of 4.5 yrs. NBD Assessment: Pre-ACE & post-ACE toileting times, bowel continence status, & complications. QoL Outcome Measures: Nonstandardized questionnaire. |
1. Five patients (83%) were satisfied with their outcome & rated their QoL higher after the ACE procedure compared with pre-ACE. |
| Westgren & Levi (1998)54 Cross-sectional survey |
Objective: Determine associations between major outcome variables after SCI & QoL. Population: 320 persons (261 men) with SCI, mean age 42 (17–78 yr), YPI ≤4 yrs & ≥4 yrs. NBD Assessment: Medical records via clinical database. QoL Outcome Measures: SF-36. |
1. Bowel dysfunction was associated with ↓ QoL. 2. Bowel dysfunction yielded a medium effect sizes in the general physical functioning (p = .001), bodily pain (p = .003), general health (p = .001), vitality (p = .001), social function (p = .004), & mental health (p = .001) subscales. |
| Worsøe et al (2008)42 Retrospective chart review & cross-sectional survey |
Objective: Evaluate the long-term outcomes of ACE & ACE + colostomy in patients with SCI. Population: 80 patients (12 men) with SCI, mean age 51 yrs at time of stoma, mean follow-up time was 75 mos (range, 3–183). NBD Assessment: Continued ACE or ACE+colostomy at follow-up; Wexner score. QoL Outcome Measures: Nonstandardized study-specific questionnaire. |
1. 34 of 43 patients still using ACE were satisfied or very satisfied with the result, 8 patients were neither satisfied nor dissatisfied, & none were dissatisfied or very dissatisfied. One person did not provide a response. 2. On an arbitrary scale (0–100) mean values for bowel function before & after were 12 & 81 respectively (p < .01). For social function, the corresponding values were 30 & 81 (p < .01) & for QoL they were 28 & 81 (p < .01). |
| Tulsky et al (2015)57 Mixed-methods design |
Objective: To describe the development & psychometric properties of the SCI-QoL Bladder Management Difficulties & Bowel Management Difficulties item banks & Bladder Complications scale. Population: 757 adults with traumatic SCI of traumatic etiology, 18 yrs of age & older. NBD Assessment: N/A QoL Outcome Measures: In development. |
1. The SCI-QoL Bladder Management Difficulties & Bowel Management Difficulties item banks are psychometrically robust & are available as computer adaptive tests or short forms. |
Note: Studies are listed in alphabetical order according to the last name of the first author. ACE = antegrade colonic enema; AD = autonomic dysreflexia; ADL = activities of daily living; AIS = American Spinal Injury Association Impairment Scale; CHART = Criag Handicap and Assessment Reporting Technique; CCCSS = Cleveland Clinic Constipation Scoring System; DRS = digital rectal stimulation; ECC = enema continence catheter; FIM = Functional Independence Measure; GI = gastrointestinal; HADS = Hospital Anxiety & Depression Scale; HrQoL = health-related quality of life; HUI = Health Utilities Index; ICI = impediments to community integration; MBI = Modified Barthel Index; mos = months; NBD = neurogenic bowel dysfunction; N/A = not available; QLI = Quality of Life Index; QoL = quality of life; RSS = Reciprocal Support Scale; SCI = spinal cord injury(ies); SCS = Secondary Condition Scale; SF-12 = Short-Form 12; SF-36 = Short-Form 36; SWLS = Satisfaction with Life Scale; YPI = years post injury; yr(s) = years.
Table 1.
Identified studies (CONT.)
|
DESIGN Author (year) Research design |
METHODS (Objective, Population, Bowel Dysfunction Assessment, QoL Outcome Measures) |
QoL RESULTS |
|---|---|---|
| Adriaansen et al (2015)55 Cross-sectional multicenter study |
Objective: Describe bowel management & its outcomes in individuals living with an SCI for at least 10 yrs. Population: Individuals (N=258; age range, 28–65 yrs) who acquired their SCI between 18 & 35 yrs of age, who were at least 10 yr post-SCI, & who used a wheelchair for their daily mobility. NBD Assessment: International SCI Bowel Function Basic Data Set. QoL Outcome Measures: NBD score, a simple rating scale. |
1. Severe NBD was present in 36% of all participants & in 40% of those using a conservative method. However, only 14% were (very) dissatisfied with their current bowel management. 2. Dissatisfaction with bowel management was significantly associated with constipation & severe NBD. 3. With increasing time since injury, there was a nonsignificant trend observed toward a decline in dissatisfaction with bowel management & a significant decline in severe NBD. |
| Anson et al (1993)44 Cross-sectional & longitudinal survey |
Objective: Explore relationships among social support, adjustment, & secondary complications in persons with SCI. Population: 125 persons with SCI, 18 yrs + YPI > 1 yr. NBD Assessment: SCI QLI QoL Outcome Measures: SCI QLI; RSS scale. |
4. Social adjustment was associated with the number of diarrhea events. 5. Getting advice was negatively (r = −.029) associated with number of diarrhea events (p < .05). 6. No differences in diarrhea or constipation between high- & low-level support groups. |
| Branagan et al (2003)43 Cross-sectional survey |
Objective: Evaluate the effect of intestinal stoma formation in SCI patients. Population: 32 (27 men) patients with SCI (tetraplegia, paraplegia), mean age at onset 28.9 (range, 6–62 yrs), mean time of injury to stoma formation 17.1 mos (0–36.25). NBD Assessment: Presence of stoma QoL Outcome Measures: Nonstandardized study-specific questionnaire. |
1 18 patients reported that a stoma gave them ↑ independence, 12 reported no difference, & 1 felt his independence ↓ despite a significant ↓ time spent in bowel care. 2. QoL after stoma formation was described as much better by 25 patients, as better by 5, & QoL as worse by 1. |
| Christensen et al (2000)31 Cross-sectional survey |
Objective: Evaluate an ECC & MACE in patients with SCI. Population: 21 patients (10 men) with SCI offered ECC, mean age 39.9 (range, 7±72 yrs). 8 patients with SCI (3 men) + MACE, mean age 32.8 (range, 15–66 yrs). NBD Assessment: Single capsule with 24 or 10 radiopaque markers followed by abdominal X-ray; bowel management techniques. QoL Outcome Measures: Nonstandardized study-specific questionnaire. |
1. Before treatment with the ECC, 7 out of 11 patients available for follow-up felt that colorectal dysfunction imposed a major restriction on their QoL & social activities. 2. Before treatment with the ECC, 2 patients reported some restrictions, 1 reported a minor restriction, & 1 failed to answer the question. 3. At follow-up, 2 patients reported that colorectal dysfunction caused only some or little restriction & 3 patients reported no restriction. 4. At follow-up, 2 felt some restriction, 6 reported a minor restriction, & 6 reported no restriction. 5. Before MACE, 3 out of 5 patients were available at follow-up. |
| Christensen et al (2006)29 Prospective, randomized controlled multicenter trial |
Objective: Compare outcomes of transanal irrigation vs conservative bowel management in patients with SCI. Population: 87 patients (18 men) with SCI, median age 31.6 ± 13.3 yrs. NBD Assessment: St. Mark's Fecal Incontinence; CCCSS; Modified American Society of Colorectal Surgeon fecal incontinence scores. QoL Outcome Measures: NBD score |
1. Compared with conservative bowel management, transanal irrigation improves constipation, fecal incontinence, & symptom-related QoL. |
| Christensen et al (2008)28 Prospective, randomizedcontrolled multicenter trial |
Objective: Compare the symptoms of NBD in patients with SCI at baseline & after 10 weeks of treatment with transanal irrigation & identify possible factors that could predict treatment outcome. Population: 62 patients (45 men) with SCI (supraconal conal/cauda equina, complete, incomplete), mean age 47.5 ±15.5. NBD Assessment: Transanal irrigation, CCCSS; St. Mark's Fecal Incontinence. QoL Outcome Measures: NBD score |
1. Scores on the NBD improved from baseline to termination (p < .0001). 2. Regression analyses revealed that there was a reduction in the impact of bowel dysfunction on QoL but depended significantly on complete injury, being male, & ability to walk & varied significantly between study centres. |
| Coggrave et al (2009)45 Cross-sectional survey |
Objective: Describe bowel management in community dwelling persons with SCI & explore associations between age, injury, dependency problems, interventions, & satisfaction. Population: 1,334 persons (73.4% men) with SCI, median age 52 (19–91 yrs), median YPI 18 (1–65 yrs). NBD Assessment: Self-report (survey). QoL Outcome Measures: Nonstandardized study-specific questionnaire. |
1. Bowel dysfunction impacted on life activities to varying degrees & impact of bowel dysfunction was rated as significantly ↑ (p .001) than other aspects of SCI. 2. 20% of respondents were dissatisfied or very dissatisfied with bowel management & low satisfaction was associated with more frequent incontinence (p < .001), more problems (p < .001), longer duration of care (p< .001), more management (p = .008), & more interventions used (p < .001). |
| Coggrave et al (2013)15 Multicentre, retrospective self-report postal survey |
Objective: Characterize SCI individuals with a stoma, their stoma management & outcomes, identify sources of information & support for decision making & explore the impact of a stoma on life satisfaction. Population: 92 individuals, mean age 56 yrs, mean duration of injury 26 yrs, 91% with colostomy, 9% ileostomy. NBD Assessment: Self-report (survey). QoL Outcome Measures: Nonstandardized study-specific questionnaire (accompanied by TSCS, SWLS, & HADS) & 3-item nonstandardized questionnaire. |
1. Satisfaction with stoma was high; provision of sufficient information preoperatively was important, those with ileostomy were more dependent & less satisfied. 2. Life satisfaction & physical self-concept were both lower in this sample than in previously reported samples of SCI individuals without reported bowel difficulties or stoma. |
| Craven et al (2012)46 Cross-sectional survey |
Objective: Describe the relationships between secondary health conditions & health preference post SCI. Population: 357 persons (218 men) with SCI (AIS A-D), mean age 54.0 (range, 24–89), mean YPI 19.3 (range, 2–65). NBD Assessment: Bowel dysfunction item from the SCS. QoL Outcome Measures: HUI-III. |
1. Persons in no/mild bowel dysfunction group had ↑ (p < .0001) HUI-III scores than those in the moderate/severe bowel dysfunction group. |
| Del Popolo et al (2008)37 Pre-post intervention |
Objective: Evaluate the effects of Peristeen Anal Irrigation on NBD & QoL. Population: 36 patients (18 men) with SCI, median age 31.6 ± 13.3 yrs. NBD Assessment: Function, duration of the evacuation disorder, method of defecation, dietary supplements, the need for assistance for evacuation & the predominant intestinal symptom during/after defecation, NBD. QoL Outcome Measures: Nonstandardized study-specific questionnaire. |
1. Patient's opinions of their QoL score & degree of satisfaction ↑ from pre- to post-intervention (p = .001). 2. A high percentage of patients reported a change in their level of dependency after the treatment period. |
| Faaborg et al (2008)56 Longitudinal |
Objective: Describe long-term colorectal function in SCI patients. Population: 72 patients (48 men) with SCI, mean age 38.0 ± 11.9 yrs, YPI 37.5 ± 45.2 mos. NBD Assessment: Self-reported constipation, obstructed defecation, & fecal incontinence (survey). QoL Outcome Measures: Non-standardized study specific questionnaire; NBD score. |
1. The impact of colorectal dysfunction causing some or major restrictions on QoL or social activities ↑ from 25% to 38% from 1996 to 2006 (p < .005). 2. The impact of constipation influencing QoL ↑ from 15% to 23% from 1996 to 2006 (p < .15). |
| Glickman & Kamm (1996)4 Cross-sectional survey |
Objective: Determine the prevalence, nature, & effects – both physical & psychological – of SCI on bowel function. Population: 115 outpatients (77% men) with SCI, median age 38 (18–75 yrs), median YPI 62 (9–491 mos). NBD Assessment: Self-report (survey). QoL Outcome Measures: HADS; non-standardized questionnaire. |
1. Bowel dysfunction was a source of psychological distress in 54% of patients & was associated with time required for bowel management (p = .005) & frequency of incontinence (p = .001). 2. HADS scores correlated significantly with time taken for bowel management. 3. Bowel management problems were rated above urinary problems & not far below loss of mobility, impaired sexual function, & dependence. |
| Han et al (1998)47 Cross-sectional survey |
Objective: Investigate the characteristics of chronic GI problems & bowel dysfunction in patients with SCI. Population: 72 patients (48 men) with SCI, mean age 38.0 ± 11.9 yrs, YPI 37.5 ± 45.2 mos. NBD Assessment: Self-report (survey). QoL Outcome Measures: MBI Score. |
1. Bowel dysfunction was unrelated to age, duration, & neurological level of SCI, ASIA score, or level of activity. 2. Post-SCI GI problems were mainly bowel problems such as defecation difficulty (40.3%) & this affected ADL. |
| Hicken et al (2001)39 Case-control |
Objective: Examined the QoL among individuals with SCI requiring assistance for bowel & bladder management compared to those with independent control of their bladders & bowels. Population: 53 matched pairs (49% men): (1) bladder/bowel dependent individuals & (2) bladder/bowel independent individuals, mean age 37.02 yrs, YPI divided into 4 groups (1, 2–5, 6–15, >16 yrs). Groups matched on age, sex, education, race, & lesion level. NBD Assessment: FIM. QoL Outcome Measures: CHART; SWLS; SF-12. |
1. The bladder/bowel-dependent individuals reported ↓ life satisfaction & greater overall handicap (p < .001). In particular, persons who were bladder dependent had lower CHART subscale scores than bladder independent group on the following: physical independence (p < .001), mobility (p < .001), & occupational functioning (p < .05). 2. The bladder/bowel independent group initiated more social contact with strangers compared to bladder/bowel-dependent individuals (p = .056). 3. Although there were no group differences concerning social integration, the bladder/bowel-dependent group may have more difficulties initiating new social relationships. |
| Kachourbos & Creasey (2000)32 Post-intervention cross-sectional survey |
Objective: Assess recollections of health & QoL preoperatively in relation to bladder & bowel care & rate changes in QoL post-implant of an implantable stimulator. Population: 16 persons with SCI, 6 mos post surgery. NBD Assessment: Presence of implantable stimulator. QoL Outcome Measures: Non-standardized study specific questionnaire. |
1. Bowel program times were reduced from a mean of 5.4 hr per week preoperatively to 2.0 hr per week postoperatively. 2. Respondents reported a greater sense of independence, ↑ socialization, greater control over their lives, improved interpersonal relationships, improved self-image, ↓ feelings of depression, & an overall improvement in QoL. |
| Kelly et al (1999)30 Retrospective chart review & cross-sectional survey |
Objective: Evaluate the long-term outcomes of intestinal stomas post-SCI. Population: 14 patients (16 men) with SCI, mean age 54.8 yrs at time of stoma, mean time from SCI to stoma 15 yrs. NBD Assessment: Presence of stoma. QoL Outcome Measures: Nonstandardized study specific questionnaire. Similar to Dijker's typical QoL measure of ADL. |
1. Ten patients reported that colostomy was beneficial to their QoL. One person whose QoL remained unchanged post colostomy reported worse QoL at 10-yr follow-up. |
| Kim (2012)48 Cross-sectional survey |
Objective: Describe defecation stimulation methods & their outcomes & investigate the impact of bowel dysfunction on QoL in SCI. Population: 388 persons with SCI (295 men), mean age 44.5±10.8 yrs, mean YPI 14.2±9.5 yrs. NBD Assessment: Bowel stimulation method, frequency of bowel movements, defecation time, symptoms of AD, frequency of fecal incontinence, & flatus. QoL Outcome Measures: Nonstandardized study-specific questionnaire. |
1. Frequency of fecal incontinence had the greatest effects on QoL. 2. When patients had fecal incontinence every day, they had 67.4 times greater chance to obtain severely lowered general QoL. 3. Time taken in defecation >60 min, presence of perianal skin problem, & flatus incontinence also significantly influenced QoL. 4. QoL deterioration differs between each stimulation user. Decline in general QoL was greater in large-volume enemas users than in DRS users. 5. Social QoL deterioration was much more profound in large-volume enemas users than in DRS or finger evacuations users. 6. QoL at home was lower in patients using large-volume enemas than in those using other methods. 7. Mini-enema users had worse QoL at home than digital rectal stim users |
| Kirk et al (1997)5 Cross-sectional survey |
Objective: Describe impact of NBD on life activities. Population: 171 adults (128 men) with SCI, mean age 39.5 ± 14.5 yrs, mean YPI 8.9 ± 8.9. NBD Assessment: Self-report (survey). QoL Outcome Measures: Nonstandardized study-specific questionnaire (Bowel Program Outcome Questionnaire). |
1. 61% indicated NBD interfered with their life. 2. 47 of 105 respondents described a loss of freedom to go places, missing work, school or social events, or having to plan their lives around their bowels. |
| Krogh et al (1997)50 Cross-sectional survey |
Objective: Describe the frequency & severity of colorectal problems among patients with spinal cord lesions & determine whether these problems are associated with age, gender, time since lesion, level & severity of lesion. Population: 424 persons with SCI (300 men), mean age 41 (range 8–88 yrs), YPI 41 (range 0–59 yrs). NBD Assessment: Self-report (survey). QoL Outcome Measures: Nonstandardized study-specific questionnaire. |
1. 39% reported colorectal dysfunction caused some/major restrictions on social activities or QoL. 2. 29% reported disturbed defecation caused some/major restriction on social activities & 32% reported it caused some/major restriction on QoL. 3. 19% reported fecal incontinence caused some/major restriction on social activities & 20% reported it caused some/major restriction on QoL. 4. 30% reported bowel dysfunction was ↑ than bladder or sexual dysfunction. |
| Krogh et al (2006)49 Cross-sectional survey |
Objective: Develop & validate a symptom-based score for the NBD score. Population: 424 persons (72% men) with SCI, mean age 41 (8–88 yrs), mean YPI 14 (0–88 yrs). NBD Assessment: NBD score. QoL Outcome Measures: NBD score. |
1. Several items on the NBD found the impact on QoL ↑ with the severity of symptoms. Frequency of bowel movements was associated with QoL (p < .0001), as was frequency of fecal incontinence. 2. Difference in NBD scores among patients reporting no, little, some, or major impacts on QoL were significant (p < .001). 3. There may be an association between self-reported QoL & restriction of social activities due to bowel dysfunction. |
| Liu et al (2009)51 Cross-sectional survey |
Objective: Assess the relationship between the severity of NBD & HrQoL in persons with various degrees of SCI. Population: 128 (95 men) respondents with SCI, 36 with tetraplegia, 58 with paraplegia, 34 with paresis, mean age 48.3 (range 13–84 yrs), YPI divided into 4 groups (1–2 yrs, 3–5 yrs, 6–10 yrs, & over 10 yrs). NBD Assessment: NBD score. QoL Outcome Measures: SF-36; NBD score. |
1. Persons with very minor NBD had the ↑ scores on the SF-36 in contrast to persons with severe NBD, who had the ↓scores. 2. Significant differences were found on the SF-36 physical functioning (p < .001) & the physical component summary (p < .001) subscales. 3. Participants with worse NBD were likely to have ↓physical QoL (p < .001). |
| Lombardi (2010)33 Retrospective non-blinded design without controls. |
Objective: Evaluate the efficacy & safety of sacral neuromodulation in incomplete SCI affected by chronic NBD. Population: 23 patients with SCI (13 men), mean age 36±9 yrs. NBD Assessment: Wexner Score; episodes of fecal incontinence, no. of evacuations/week. QoL Outcome Measures: SF-36. |
1. Patients in both groups (constipation & fecal incontienence) had significant ↓ (p < .05) in Wexner scores. 2. QoL in both groups consistently showed statistical improvement (p < .05). |
| Lombardi et al (2011)34 Retrospective cross-sectional survey |
Objective: Assess the concomitant clinical improvement in incomplete SCI with NBD using sacral neuromodulation. Population: 75 patients with incomplete SCI. NBD Assessment: Incontinence & constipation. QoL Outcome Measures: SF-36. |
1. Bladder function & incontinence improved. 2. In the general & mental health domains of the SF-36, all patients improved their scores by at least 20% compared with baseline after sacral neuromodulation. |
| Luther et al (2005)40 Case-control |
Objective: Compare QoL for people with NBD & SCI using either a standard care program or colostomy. Population: 74 veterans (73 men) with SCI + colostomy, 296 SCI controls without colostomy, age range < 20–89, YPI within past 20 yr. NBD Assessment: Presence of colostomy. QoL Outcome Measures: IBDQ. |
1. No significant differences were detected on IBDQ between persons with SCI + colostomy & those with SCI only. |
| Lynch et al (2000)10 Controlled, descriptive & comparative questionnaire study |
Objective: Describe the bowel function of SCI patients & compare it to a general community control group. Population: 467 SCI patients & 467 control subjects were age & gender matched. Mean age for the SCI patients 43.5 (range, 15–89 yrs), mean YPI 14 (range, 0.7–42.1 yrs). Mean age for the controls 45.3 (range, 17–78 yr). NBD Assessment: General bowel function, incidence of incontinence, & defecation methods. QoL Outcome Measures: Nonstandardized questionnaire. |
1. Incontinence affected the QoL for 62% SCI patients compared to 8% of the controls. 2. Incontinence did not affect the majority of the controls (92.3%) in terms of everyday activities compared to 43.9% of SCI patients (p < .0001). |
| Noonan et al (2008)52 Cross-sectional survey |
Objective: Determine the effect of associated SCI conditions on health status & QoL. Population: 70 persons (57 men) with central cord syndrome, mean age at injury 45±18 yrs (range, 13–91), mean age at follow-up 51 ±18 yrs (range, 19–95). NBD Assessment: Self-report (survey). QoL Outcome Measures: SF-36; numeric QoL rating. |
1. Bowel, bladder & sexual dysfunction on the physical component score of the SF-36 were significant, but the effect ↓ when controlling for personal & confounding factors. 2. Bowel, bladder & sexual dysfunction were not related to the mental component scores of the SF-36. 3. Problems with bowel, bladder, & sexual dysfunction were significantly (p< .01) associated with QoL when personal & confounding factors were NOT controlled for. |
| Pardee et al (2012)8 Exploratory, descriptive correlational design |
Objective: Investigate the association between characteristics of individuals with SCI & neurogenic bowel & their perceived QoL. Population: 241 surveys; from adults over age 18, diagnosed with SCI & neurogenic bowel more than 2 yrs post injury, AIS of A, B, C, or D & residing in the community. NBD Assessment: Survey of neurogenic bowel characteristics. QoL Outcome Measures: QoL survey. |
1. Regardless of the bowel management program 54% (n = 127) were satisfied with current methods. Although time reported to complete bowel programs ranged from 1 to 120 min, there was no difference in rating of satisfaction with time. 2. There was a statistically significant difference between those satisfied & dissatisfied with current bowel management & QoL; those satisfied demonstrated a higher QoL on 3 subscales, work function (p = .021), bowel problems (p < .001), & social function (p < .001). Those dissatisfied with their bowel program perceived a lower QoL & indicated problem of time (p = .001), pain or discomfort (p = .033), & poor results (p < .001). |
| Randell et al (2001)41 Prospective controlled comparative analysis |
Objective: Determine whether a colostomy changes QoL in patients with SCI. Population: 26 (15 men) patients with SCI (tetraplegia, paraplegia) + colostomy, age range 22–87, range of injury to stoma formation 7 mos – 20 yrs. 26 SCI controls (age, gender, injury, & YPI matched) without colostomy. NBD Assessment: Presence of colostomy. QoL Outcome Measures: Burwood QoL Questionnaire. |
1. No significant differences were detected on QoL between persons with SCI + colostomy & those with SCI only. |
| Roach et al (2000)53 Cross-sectional survey |
Objective: Examine the relationship between bowel dysfunction, impediment to community integration & QoL in persons with SCI. Population: 103 SCI consumers (76.7% men), mean age 39 yrs, YPI 14 yr. NBD Assessment: Self-report (survey). QoL Outcome Measures: Andrews & Withey (1976) Life Satisfaction Survey; nonstandardized study specific questionnaire on community integration (ICI). |
1. Significant negative relationship between subjective severity & 3 ICI measures; the higher the perceived severity of bowel dysfunction, the more it affected (1) personal relationships (p < .01); (2) feelings about themselves (p < .01); (3) their home environment (p < .05). 2. The number of days each month a person stayed at home because of lack of bowel control was associated with all 3 ICI scales (p < .01). The ↑ bowel accidents per month, the ↑ negative a respondent felt about him/herself (p < .05). 3. None of the bowel dysfunction characteristics were significantly related to the satisfaction of life items, but non-parametric analyses revealed that 2 of the ICI items were associated with satisfaction with free time & family life. |
| Rosito et al (2002)35 Pre-post intervention |
Objective: Evaluate the effects of colostomy on the QoL in patients with SCI. Population: 27 patients (26 men) with SCI, mean age of 62.9 (range 44–79 yrs), YPI 25.8 (range 8–48 yrs), mean time since stoma formation 8 (range 1.5–28 yrs), mean time with severe bowel dysfunction 5.5 (range 0.5–18 yr). NBD Assessment: Presence of colostomy. QoL Outcome Measures: Nonstandardized study specific questionnaire. Similar to Dijker's typical QoL measure of ADL. |
1. Colostomy improved (p ≤ .0001) total QoL. 2. Significant improvements after colostomy observed in physical health, self-efficacy, psychosocial status, & recreation/leisure but not in body image. 3. 85% of patients reported an ↑ in total QoL after colostomy; 70% of patients were satisfied with their personal lives before colostomy compared to 89% of patients after colostomy. 4. 67% of patients felt more independent after colostomy compared to 30% of patients that felt the same level of independence. |
| Safadi et al (2003)36 Retrospective chart review & cross-sectional survey |
Objective: Evaluate the long-term outcomes of colostomies & ileostomies post SCI. Population: 45 patients (44 men) with SCI, mean age 55.9 yrs, mean time from SCI to stoma 20.3 yrs. NBD Assessment: Presence of stoma. QoL Outcome Measures: Nonstandardized study specific questionnaire. |
1. In the right-sided colostomy group (n=20), QoL & health status scores improved (p < .05). 2. In the left-sided colostomy group (n=20), QoL & health status scores improved (p < .05). 3. In the ileostomy group (n=7), QoL & health status scores improved (p < .05). |
| Teichman et al (2003)79 Retrospective review |
Objective: To determine the long-term outcomes from the Malone antegrade continence enema (ACE) procedure in adult neurogenic patients. Population: 6 patients (mean age = 35 yrs), mean follow-up of 4.5 yrs. NBD Assessment: Pre-ACE & post-ACE toileting times, bowel continence status, & complications. QoL Outcome Measures: Nonstandardized questionnaire. |
1. Five patients (83%) were satisfied with their outcome & rated their QoL higher after the ACE procedure compared with pre-ACE. |
| Westgren & Levi (1998)54 Cross-sectional survey |
Objective: Determine associations between major outcome variables after SCI & QoL. Population: 320 persons (261 men) with SCI, mean age 42 (17–78 yr), YPI ≤4 yrs & ≥4 yrs. NBD Assessment: Medical records via clinical database. QoL Outcome Measures: SF-36. |
1. Bowel dysfunction was associated with ↓ QoL. 2. Bowel dysfunction yielded a medium effect sizes in the general physical functioning (p = .001), bodily pain (p = .003), general health (p = .001), vitality (p = .001), social function (p = .004), & mental health (p = .001) subscales. |
| Worsøe et al (2008)42 Retrospective chart review & cross-sectional survey |
Objective: Evaluate the long-term outcomes of ACE & ACE + colostomy in patients with SCI. Population: 80 patients (12 men) with SCI, mean age 51 yrs at time of stoma, mean follow-up time was 75 mos (range, 3–183). NBD Assessment: Continued ACE or ACE+colostomy at follow-up; Wexner score. QoL Outcome Measures: Nonstandardized study-specific questionnaire. |
1. 34 of 43 patients still using ACE were satisfied or very satisfied with the result, 8 patients were neither satisfied nor dissatisfied, & none were dissatisfied or very dissatisfied. One person did not provide a response. 2. On an arbitrary scale (0–100) mean values for bowel function before & after were 12 & 81 respectively (p < .01). For social function, the corresponding values were 30 & 81 (p < .01) & for QoL they were 28 & 81 (p < .01). |
| Tulsky et al (2015)57 Mixed-methods design |
Objective: To describe the development & psychometric properties of the SCI-QoL Bladder Management Difficulties & Bowel Management Difficulties item banks & Bladder Complications scale. Population: 757 adults with traumatic SCI of traumatic etiology, 18 yrs of age & older. NBD Assessment: N/A QoL Outcome Measures: In development. |
1. The SCI-QoL Bladder Management Difficulties & Bowel Management Difficulties item banks are psychometrically robust & are available as computer adaptive tests or short forms. |
Note: Studies are listed in alphabetical order according to the last name of the first author. ACE = antegrade colonic enema; AD = autonomic dysreflexia; ADL = activities of daily living; AIS = American Spinal Injury Association Impairment Scale; CHART = Criag Handicap and Assessment Reporting Technique; CCCSS = Cleveland Clinic Constipation Scoring System; DRS = digital rectal stimulation; ECC = enema continence catheter; FIM = Functional Independence Measure; GI = gastrointestinal; HADS = Hospital Anxiety & Depression Scale; HrQoL = health-related quality of life; HUI = Health Utilities Index; ICI = impediments to community integration; MBI = Modified Barthel Index; mos = months; NBD = neurogenic bowel dysfunction; N/A = not available; QLI = Quality of Life Index; QoL = quality of life; RSS = Reciprocal Support Scale; SCI = spinal cord injury(ies); SCS = Secondary Condition Scale; SF-12 = Short-Form 12; SF-36 = Short-Form 36; SWLS = Satisfaction with Life Scale; YPI = years post injury; yr(s) = years.
Table 1.
Identified studies (CONT.)
|
DESIGN Author (year) Research design |
METHODS (Objective, Population, Bowel Dysfunction Assessment, QoL Outcome Measures) |
QoL RESULTS |
|---|---|---|
| Adriaansen et al (2015)55 Cross-sectional multicenter study |
Objective: Describe bowel management & its outcomes in individuals living with an SCI for at least 10 yrs. Population: Individuals (N=258; age range, 28–65 yrs) who acquired their SCI between 18 & 35 yrs of age, who were at least 10 yr post-SCI, & who used a wheelchair for their daily mobility. NBD Assessment: International SCI Bowel Function Basic Data Set. QoL Outcome Measures: NBD score, a simple rating scale. |
1. Severe NBD was present in 36% of all participants & in 40% of those using a conservative method. However, only 14% were (very) dissatisfied with their current bowel management. 2. Dissatisfaction with bowel management was significantly associated with constipation & severe NBD. 3. With increasing time since injury, there was a nonsignificant trend observed toward a decline in dissatisfaction with bowel management & a significant decline in severe NBD. |
| Anson et al (1993)44 Cross-sectional & longitudinal survey |
Objective: Explore relationships among social support, adjustment, & secondary complications in persons with SCI. Population: 125 persons with SCI, 18 yrs + YPI > 1 yr. NBD Assessment: SCI QLI QoL Outcome Measures: SCI QLI; RSS scale. |
4. Social adjustment was associated with the number of diarrhea events. 5. Getting advice was negatively (r = −.029) associated with number of diarrhea events (p < .05). 6. No differences in diarrhea or constipation between high- & low-level support groups. |
| Branagan et al (2003)43 Cross-sectional survey |
Objective: Evaluate the effect of intestinal stoma formation in SCI patients. Population: 32 (27 men) patients with SCI (tetraplegia, paraplegia), mean age at onset 28.9 (range, 6–62 yrs), mean time of injury to stoma formation 17.1 mos (0–36.25). NBD Assessment: Presence of stoma QoL Outcome Measures: Nonstandardized study-specific questionnaire. |
1 18 patients reported that a stoma gave them ↑ independence, 12 reported no difference, & 1 felt his independence ↓ despite a significant ↓ time spent in bowel care. 2. QoL after stoma formation was described as much better by 25 patients, as better by 5, & QoL as worse by 1. |
| Christensen et al (2000)31 Cross-sectional survey |
Objective: Evaluate an ECC & MACE in patients with SCI. Population: 21 patients (10 men) with SCI offered ECC, mean age 39.9 (range, 7±72 yrs). 8 patients with SCI (3 men) + MACE, mean age 32.8 (range, 15–66 yrs). NBD Assessment: Single capsule with 24 or 10 radiopaque markers followed by abdominal X-ray; bowel management techniques. QoL Outcome Measures: Nonstandardized study-specific questionnaire. |
1. Before treatment with the ECC, 7 out of 11 patients available for follow-up felt that colorectal dysfunction imposed a major restriction on their QoL & social activities. 2. Before treatment with the ECC, 2 patients reported some restrictions, 1 reported a minor restriction, & 1 failed to answer the question. 3. At follow-up, 2 patients reported that colorectal dysfunction caused only some or little restriction & 3 patients reported no restriction. 4. At follow-up, 2 felt some restriction, 6 reported a minor restriction, & 6 reported no restriction. 5. Before MACE, 3 out of 5 patients were available at follow-up. |
| Christensen et al (2006)29 Prospective, randomized controlled multicenter trial |
Objective: Compare outcomes of transanal irrigation vs conservative bowel management in patients with SCI. Population: 87 patients (18 men) with SCI, median age 31.6 ± 13.3 yrs. NBD Assessment: St. Mark's Fecal Incontinence; CCCSS; Modified American Society of Colorectal Surgeon fecal incontinence scores. QoL Outcome Measures: NBD score |
1. Compared with conservative bowel management, transanal irrigation improves constipation, fecal incontinence, & symptom-related QoL. |
| Christensen et al (2008)28 Prospective, randomizedcontrolled multicenter trial |
Objective: Compare the symptoms of NBD in patients with SCI at baseline & after 10 weeks of treatment with transanal irrigation & identify possible factors that could predict treatment outcome. Population: 62 patients (45 men) with SCI (supraconal conal/cauda equina, complete, incomplete), mean age 47.5 ±15.5. NBD Assessment: Transanal irrigation, CCCSS; St. Mark's Fecal Incontinence. QoL Outcome Measures: NBD score |
1. Scores on the NBD improved from baseline to termination (p < .0001). 2. Regression analyses revealed that there was a reduction in the impact of bowel dysfunction on QoL but depended significantly on complete injury, being male, & ability to walk & varied significantly between study centres. |
| Coggrave et al (2009)45 Cross-sectional survey |
Objective: Describe bowel management in community dwelling persons with SCI & explore associations between age, injury, dependency problems, interventions, & satisfaction. Population: 1,334 persons (73.4% men) with SCI, median age 52 (19–91 yrs), median YPI 18 (1–65 yrs). NBD Assessment: Self-report (survey). QoL Outcome Measures: Nonstandardized study-specific questionnaire. |
1. Bowel dysfunction impacted on life activities to varying degrees & impact of bowel dysfunction was rated as significantly ↑ (p .001) than other aspects of SCI. 2. 20% of respondents were dissatisfied or very dissatisfied with bowel management & low satisfaction was associated with more frequent incontinence (p < .001), more problems (p < .001), longer duration of care (p< .001), more management (p = .008), & more interventions used (p < .001). |
| Coggrave et al (2013)15 Multicentre, retrospective self-report postal survey |
Objective: Characterize SCI individuals with a stoma, their stoma management & outcomes, identify sources of information & support for decision making & explore the impact of a stoma on life satisfaction. Population: 92 individuals, mean age 56 yrs, mean duration of injury 26 yrs, 91% with colostomy, 9% ileostomy. NBD Assessment: Self-report (survey). QoL Outcome Measures: Nonstandardized study-specific questionnaire (accompanied by TSCS, SWLS, & HADS) & 3-item nonstandardized questionnaire. |
1. Satisfaction with stoma was high; provision of sufficient information preoperatively was important, those with ileostomy were more dependent & less satisfied. 2. Life satisfaction & physical self-concept were both lower in this sample than in previously reported samples of SCI individuals without reported bowel difficulties or stoma. |
| Craven et al (2012)46 Cross-sectional survey |
Objective: Describe the relationships between secondary health conditions & health preference post SCI. Population: 357 persons (218 men) with SCI (AIS A-D), mean age 54.0 (range, 24–89), mean YPI 19.3 (range, 2–65). NBD Assessment: Bowel dysfunction item from the SCS. QoL Outcome Measures: HUI-III. |
1. Persons in no/mild bowel dysfunction group had ↑ (p < .0001) HUI-III scores than those in the moderate/severe bowel dysfunction group. |
| Del Popolo et al (2008)37 Pre-post intervention |
Objective: Evaluate the effects of Peristeen Anal Irrigation on NBD & QoL. Population: 36 patients (18 men) with SCI, median age 31.6 ± 13.3 yrs. NBD Assessment: Function, duration of the evacuation disorder, method of defecation, dietary supplements, the need for assistance for evacuation & the predominant intestinal symptom during/after defecation, NBD. QoL Outcome Measures: Nonstandardized study-specific questionnaire. |
1. Patient's opinions of their QoL score & degree of satisfaction ↑ from pre- to post-intervention (p = .001). 2. A high percentage of patients reported a change in their level of dependency after the treatment period. |
| Faaborg et al (2008)56 Longitudinal |
Objective: Describe long-term colorectal function in SCI patients. Population: 72 patients (48 men) with SCI, mean age 38.0 ± 11.9 yrs, YPI 37.5 ± 45.2 mos. NBD Assessment: Self-reported constipation, obstructed defecation, & fecal incontinence (survey). QoL Outcome Measures: Non-standardized study specific questionnaire; NBD score. |
1. The impact of colorectal dysfunction causing some or major restrictions on QoL or social activities ↑ from 25% to 38% from 1996 to 2006 (p < .005). 2. The impact of constipation influencing QoL ↑ from 15% to 23% from 1996 to 2006 (p < .15). |
| Glickman & Kamm (1996)4 Cross-sectional survey |
Objective: Determine the prevalence, nature, & effects – both physical & psychological – of SCI on bowel function. Population: 115 outpatients (77% men) with SCI, median age 38 (18–75 yrs), median YPI 62 (9–491 mos). NBD Assessment: Self-report (survey). QoL Outcome Measures: HADS; non-standardized questionnaire. |
1. Bowel dysfunction was a source of psychological distress in 54% of patients & was associated with time required for bowel management (p = .005) & frequency of incontinence (p = .001). 2. HADS scores correlated significantly with time taken for bowel management. 3. Bowel management problems were rated above urinary problems & not far below loss of mobility, impaired sexual function, & dependence. |
| Han et al (1998)47 Cross-sectional survey |
Objective: Investigate the characteristics of chronic GI problems & bowel dysfunction in patients with SCI. Population: 72 patients (48 men) with SCI, mean age 38.0 ± 11.9 yrs, YPI 37.5 ± 45.2 mos. NBD Assessment: Self-report (survey). QoL Outcome Measures: MBI Score. |
1. Bowel dysfunction was unrelated to age, duration, & neurological level of SCI, ASIA score, or level of activity. 2. Post-SCI GI problems were mainly bowel problems such as defecation difficulty (40.3%) & this affected ADL. |
| Hicken et al (2001)39 Case-control |
Objective: Examined the QoL among individuals with SCI requiring assistance for bowel & bladder management compared to those with independent control of their bladders & bowels. Population: 53 matched pairs (49% men): (1) bladder/bowel dependent individuals & (2) bladder/bowel independent individuals, mean age 37.02 yrs, YPI divided into 4 groups (1, 2–5, 6–15, >16 yrs). Groups matched on age, sex, education, race, & lesion level. NBD Assessment: FIM. QoL Outcome Measures: CHART; SWLS; SF-12. |
1. The bladder/bowel-dependent individuals reported ↓ life satisfaction & greater overall handicap (p < .001). In particular, persons who were bladder dependent had lower CHART subscale scores than bladder independent group on the following: physical independence (p < .001), mobility (p < .001), & occupational functioning (p < .05). 2. The bladder/bowel independent group initiated more social contact with strangers compared to bladder/bowel-dependent individuals (p = .056). 3. Although there were no group differences concerning social integration, the bladder/bowel-dependent group may have more difficulties initiating new social relationships. |
| Kachourbos & Creasey (2000)32 Post-intervention cross-sectional survey |
Objective: Assess recollections of health & QoL preoperatively in relation to bladder & bowel care & rate changes in QoL post-implant of an implantable stimulator. Population: 16 persons with SCI, 6 mos post surgery. NBD Assessment: Presence of implantable stimulator. QoL Outcome Measures: Non-standardized study specific questionnaire. |
1. Bowel program times were reduced from a mean of 5.4 hr per week preoperatively to 2.0 hr per week postoperatively. 2. Respondents reported a greater sense of independence, ↑ socialization, greater control over their lives, improved interpersonal relationships, improved self-image, ↓ feelings of depression, & an overall improvement in QoL. |
| Kelly et al (1999)30 Retrospective chart review & cross-sectional survey |
Objective: Evaluate the long-term outcomes of intestinal stomas post-SCI. Population: 14 patients (16 men) with SCI, mean age 54.8 yrs at time of stoma, mean time from SCI to stoma 15 yrs. NBD Assessment: Presence of stoma. QoL Outcome Measures: Nonstandardized study specific questionnaire. Similar to Dijker's typical QoL measure of ADL. |
1. Ten patients reported that colostomy was beneficial to their QoL. One person whose QoL remained unchanged post colostomy reported worse QoL at 10-yr follow-up. |
| Kim (2012)48 Cross-sectional survey |
Objective: Describe defecation stimulation methods & their outcomes & investigate the impact of bowel dysfunction on QoL in SCI. Population: 388 persons with SCI (295 men), mean age 44.5±10.8 yrs, mean YPI 14.2±9.5 yrs. NBD Assessment: Bowel stimulation method, frequency of bowel movements, defecation time, symptoms of AD, frequency of fecal incontinence, & flatus. QoL Outcome Measures: Nonstandardized study-specific questionnaire. |
1. Frequency of fecal incontinence had the greatest effects on QoL. 2. When patients had fecal incontinence every day, they had 67.4 times greater chance to obtain severely lowered general QoL. 3. Time taken in defecation >60 min, presence of perianal skin problem, & flatus incontinence also significantly influenced QoL. 4. QoL deterioration differs between each stimulation user. Decline in general QoL was greater in large-volume enemas users than in DRS users. 5. Social QoL deterioration was much more profound in large-volume enemas users than in DRS or finger evacuations users. 6. QoL at home was lower in patients using large-volume enemas than in those using other methods. 7. Mini-enema users had worse QoL at home than digital rectal stim users |
| Kirk et al (1997)5 Cross-sectional survey |
Objective: Describe impact of NBD on life activities. Population: 171 adults (128 men) with SCI, mean age 39.5 ± 14.5 yrs, mean YPI 8.9 ± 8.9. NBD Assessment: Self-report (survey). QoL Outcome Measures: Nonstandardized study-specific questionnaire (Bowel Program Outcome Questionnaire). |
1. 61% indicated NBD interfered with their life. 2. 47 of 105 respondents described a loss of freedom to go places, missing work, school or social events, or having to plan their lives around their bowels. |
| Krogh et al (1997)50 Cross-sectional survey |
Objective: Describe the frequency & severity of colorectal problems among patients with spinal cord lesions & determine whether these problems are associated with age, gender, time since lesion, level & severity of lesion. Population: 424 persons with SCI (300 men), mean age 41 (range 8–88 yrs), YPI 41 (range 0–59 yrs). NBD Assessment: Self-report (survey). QoL Outcome Measures: Nonstandardized study-specific questionnaire. |
1. 39% reported colorectal dysfunction caused some/major restrictions on social activities or QoL. 2. 29% reported disturbed defecation caused some/major restriction on social activities & 32% reported it caused some/major restriction on QoL. 3. 19% reported fecal incontinence caused some/major restriction on social activities & 20% reported it caused some/major restriction on QoL. 4. 30% reported bowel dysfunction was ↑ than bladder or sexual dysfunction. |
| Krogh et al (2006)49 Cross-sectional survey |
Objective: Develop & validate a symptom-based score for the NBD score. Population: 424 persons (72% men) with SCI, mean age 41 (8–88 yrs), mean YPI 14 (0–88 yrs). NBD Assessment: NBD score. QoL Outcome Measures: NBD score. |
1. Several items on the NBD found the impact on QoL ↑ with the severity of symptoms. Frequency of bowel movements was associated with QoL (p < .0001), as was frequency of fecal incontinence. 2. Difference in NBD scores among patients reporting no, little, some, or major impacts on QoL were significant (p < .001). 3. There may be an association between self-reported QoL & restriction of social activities due to bowel dysfunction. |
| Liu et al (2009)51 Cross-sectional survey |
Objective: Assess the relationship between the severity of NBD & HrQoL in persons with various degrees of SCI. Population: 128 (95 men) respondents with SCI, 36 with tetraplegia, 58 with paraplegia, 34 with paresis, mean age 48.3 (range 13–84 yrs), YPI divided into 4 groups (1–2 yrs, 3–5 yrs, 6–10 yrs, & over 10 yrs). NBD Assessment: NBD score. QoL Outcome Measures: SF-36; NBD score. |
1. Persons with very minor NBD had the ↑ scores on the SF-36 in contrast to persons with severe NBD, who had the ↓scores. 2. Significant differences were found on the SF-36 physical functioning (p < .001) & the physical component summary (p < .001) subscales. 3. Participants with worse NBD were likely to have ↓physical QoL (p < .001). |
| Lombardi (2010)33 Retrospective non-blinded design without controls. |
Objective: Evaluate the efficacy & safety of sacral neuromodulation in incomplete SCI affected by chronic NBD. Population: 23 patients with SCI (13 men), mean age 36±9 yrs. NBD Assessment: Wexner Score; episodes of fecal incontinence, no. of evacuations/week. QoL Outcome Measures: SF-36. |
1. Patients in both groups (constipation & fecal incontienence) had significant ↓ (p < .05) in Wexner scores. 2. QoL in both groups consistently showed statistical improvement (p < .05). |
| Lombardi et al (2011)34 Retrospective cross-sectional survey |
Objective: Assess the concomitant clinical improvement in incomplete SCI with NBD using sacral neuromodulation. Population: 75 patients with incomplete SCI. NBD Assessment: Incontinence & constipation. QoL Outcome Measures: SF-36. |
1. Bladder function & incontinence improved. 2. In the general & mental health domains of the SF-36, all patients improved their scores by at least 20% compared with baseline after sacral neuromodulation. |
| Luther et al (2005)40 Case-control |
Objective: Compare QoL for people with NBD & SCI using either a standard care program or colostomy. Population: 74 veterans (73 men) with SCI + colostomy, 296 SCI controls without colostomy, age range < 20–89, YPI within past 20 yr. NBD Assessment: Presence of colostomy. QoL Outcome Measures: IBDQ. |
1. No significant differences were detected on IBDQ between persons with SCI + colostomy & those with SCI only. |
| Lynch et al (2000)10 Controlled, descriptive & comparative questionnaire study |
Objective: Describe the bowel function of SCI patients & compare it to a general community control group. Population: 467 SCI patients & 467 control subjects were age & gender matched. Mean age for the SCI patients 43.5 (range, 15–89 yrs), mean YPI 14 (range, 0.7–42.1 yrs). Mean age for the controls 45.3 (range, 17–78 yr). NBD Assessment: General bowel function, incidence of incontinence, & defecation methods. QoL Outcome Measures: Nonstandardized questionnaire. |
1. Incontinence affected the QoL for 62% SCI patients compared to 8% of the controls. 2. Incontinence did not affect the majority of the controls (92.3%) in terms of everyday activities compared to 43.9% of SCI patients (p < .0001). |
| Noonan et al (2008)52 Cross-sectional survey |
Objective: Determine the effect of associated SCI conditions on health status & QoL. Population: 70 persons (57 men) with central cord syndrome, mean age at injury 45±18 yrs (range, 13–91), mean age at follow-up 51 ±18 yrs (range, 19–95). NBD Assessment: Self-report (survey). QoL Outcome Measures: SF-36; numeric QoL rating. |
1. Bowel, bladder & sexual dysfunction on the physical component score of the SF-36 were significant, but the effect ↓ when controlling for personal & confounding factors. 2. Bowel, bladder & sexual dysfunction were not related to the mental component scores of the SF-36. 3. Problems with bowel, bladder, & sexual dysfunction were significantly (p< .01) associated with QoL when personal & confounding factors were NOT controlled for. |
| Pardee et al (2012)8 Exploratory, descriptive correlational design |
Objective: Investigate the association between characteristics of individuals with SCI & neurogenic bowel & their perceived QoL. Population: 241 surveys; from adults over age 18, diagnosed with SCI & neurogenic bowel more than 2 yrs post injury, AIS of A, B, C, or D & residing in the community. NBD Assessment: Survey of neurogenic bowel characteristics. QoL Outcome Measures: QoL survey. |
1. Regardless of the bowel management program 54% (n = 127) were satisfied with current methods. Although time reported to complete bowel programs ranged from 1 to 120 min, there was no difference in rating of satisfaction with time. 2. There was a statistically significant difference between those satisfied & dissatisfied with current bowel management & QoL; those satisfied demonstrated a higher QoL on 3 subscales, work function (p = .021), bowel problems (p < .001), & social function (p < .001). Those dissatisfied with their bowel program perceived a lower QoL & indicated problem of time (p = .001), pain or discomfort (p = .033), & poor results (p < .001). |
| Randell et al (2001)41 Prospective controlled comparative analysis |
Objective: Determine whether a colostomy changes QoL in patients with SCI. Population: 26 (15 men) patients with SCI (tetraplegia, paraplegia) + colostomy, age range 22–87, range of injury to stoma formation 7 mos – 20 yrs. 26 SCI controls (age, gender, injury, & YPI matched) without colostomy. NBD Assessment: Presence of colostomy. QoL Outcome Measures: Burwood QoL Questionnaire. |
1. No significant differences were detected on QoL between persons with SCI + colostomy & those with SCI only. |
| Roach et al (2000)53 Cross-sectional survey |
Objective: Examine the relationship between bowel dysfunction, impediment to community integration & QoL in persons with SCI. Population: 103 SCI consumers (76.7% men), mean age 39 yrs, YPI 14 yr. NBD Assessment: Self-report (survey). QoL Outcome Measures: Andrews & Withey (1976) Life Satisfaction Survey; nonstandardized study specific questionnaire on community integration (ICI). |
1. Significant negative relationship between subjective severity & 3 ICI measures; the higher the perceived severity of bowel dysfunction, the more it affected (1) personal relationships (p < .01); (2) feelings about themselves (p < .01); (3) their home environment (p < .05). 2. The number of days each month a person stayed at home because of lack of bowel control was associated with all 3 ICI scales (p < .01). The ↑ bowel accidents per month, the ↑ negative a respondent felt about him/herself (p < .05). 3. None of the bowel dysfunction characteristics were significantly related to the satisfaction of life items, but non-parametric analyses revealed that 2 of the ICI items were associated with satisfaction with free time & family life. |
| Rosito et al (2002)35 Pre-post intervention |
Objective: Evaluate the effects of colostomy on the QoL in patients with SCI. Population: 27 patients (26 men) with SCI, mean age of 62.9 (range 44–79 yrs), YPI 25.8 (range 8–48 yrs), mean time since stoma formation 8 (range 1.5–28 yrs), mean time with severe bowel dysfunction 5.5 (range 0.5–18 yr). NBD Assessment: Presence of colostomy. QoL Outcome Measures: Nonstandardized study specific questionnaire. Similar to Dijker's typical QoL measure of ADL. |
1. Colostomy improved (p ≤ .0001) total QoL. 2. Significant improvements after colostomy observed in physical health, self-efficacy, psychosocial status, & recreation/leisure but not in body image. 3. 85% of patients reported an ↑ in total QoL after colostomy; 70% of patients were satisfied with their personal lives before colostomy compared to 89% of patients after colostomy. 4. 67% of patients felt more independent after colostomy compared to 30% of patients that felt the same level of independence. |
| Safadi et al (2003)36 Retrospective chart review & cross-sectional survey |
Objective: Evaluate the long-term outcomes of colostomies & ileostomies post SCI. Population: 45 patients (44 men) with SCI, mean age 55.9 yrs, mean time from SCI to stoma 20.3 yrs. NBD Assessment: Presence of stoma. QoL Outcome Measures: Nonstandardized study specific questionnaire. |
1. In the right-sided colostomy group (n=20), QoL & health status scores improved (p < .05). 2. In the left-sided colostomy group (n=20), QoL & health status scores improved (p < .05). 3. In the ileostomy group (n=7), QoL & health status scores improved (p < .05). |
| Teichman et al (2003)79 Retrospective review |
Objective: To determine the long-term outcomes from the Malone antegrade continence enema (ACE) procedure in adult neurogenic patients. Population: 6 patients (mean age = 35 yrs), mean follow-up of 4.5 yrs. NBD Assessment: Pre-ACE & post-ACE toileting times, bowel continence status, & complications. QoL Outcome Measures: Nonstandardized questionnaire. |
1. Five patients (83%) were satisfied with their outcome & rated their QoL higher after the ACE procedure compared with pre-ACE. |
| Westgren & Levi (1998)54 Cross-sectional survey |
Objective: Determine associations between major outcome variables after SCI & QoL. Population: 320 persons (261 men) with SCI, mean age 42 (17–78 yr), YPI ≤4 yrs & ≥4 yrs. NBD Assessment: Medical records via clinical database. QoL Outcome Measures: SF-36. |
1. Bowel dysfunction was associated with ↓ QoL. 2. Bowel dysfunction yielded a medium effect sizes in the general physical functioning (p = .001), bodily pain (p = .003), general health (p = .001), vitality (p = .001), social function (p = .004), & mental health (p = .001) subscales. |
| Worsøe et al (2008)42 Retrospective chart review & cross-sectional survey |
Objective: Evaluate the long-term outcomes of ACE & ACE + colostomy in patients with SCI. Population: 80 patients (12 men) with SCI, mean age 51 yrs at time of stoma, mean follow-up time was 75 mos (range, 3–183). NBD Assessment: Continued ACE or ACE+colostomy at follow-up; Wexner score. QoL Outcome Measures: Nonstandardized study-specific questionnaire. |
1. 34 of 43 patients still using ACE were satisfied or very satisfied with the result, 8 patients were neither satisfied nor dissatisfied, & none were dissatisfied or very dissatisfied. One person did not provide a response. 2. On an arbitrary scale (0–100) mean values for bowel function before & after were 12 & 81 respectively (p < .01). For social function, the corresponding values were 30 & 81 (p < .01) & for QoL they were 28 & 81 (p < .01). |
| Tulsky et al (2015)57 Mixed-methods design |
Objective: To describe the development & psychometric properties of the SCI-QoL Bladder Management Difficulties & Bowel Management Difficulties item banks & Bladder Complications scale. Population: 757 adults with traumatic SCI of traumatic etiology, 18 yrs of age & older. NBD Assessment: N/A QoL Outcome Measures: In development. |
1. The SCI-QoL Bladder Management Difficulties & Bowel Management Difficulties item banks are psychometrically robust & are available as computer adaptive tests or short forms. |
Note: Studies are listed in alphabetical order according to the last name of the first author. ACE = antegrade colonic enema; AD = autonomic dysreflexia; ADL = activities of daily living; AIS = American Spinal Injury Association Impairment Scale; CHART = Criag Handicap and Assessment Reporting Technique; CCCSS = Cleveland Clinic Constipation Scoring System; DRS = digital rectal stimulation; ECC = enema continence catheter; FIM = Functional Independence Measure; GI = gastrointestinal; HADS = Hospital Anxiety & Depression Scale; HrQoL = health-related quality of life; HUI = Health Utilities Index; ICI = impediments to community integration; MBI = Modified Barthel Index; mos = months; NBD = neurogenic bowel dysfunction; N/A = not available; QLI = Quality of Life Index; QoL = quality of life; RSS = Reciprocal Support Scale; SCI = spinal cord injury(ies); SCS = Secondary Condition Scale; SF-12 = Short-Form 12; SF-36 = Short-Form 36; SWLS = Satisfaction with Life Scale; YPI = years post injury; yr(s) = years.
Table 1.
Identified studies (CONT.)
|
DESIGN Author (year) Research design |
METHODS (Objective, Population, Bowel Dysfunction Assessment, QoL Outcome Measures) |
QoL RESULTS |
|---|---|---|
| Adriaansen et al (2015)55 Cross-sectional multicenter study |
Objective: Describe bowel management & its outcomes in individuals living with an SCI for at least 10 yrs. Population: Individuals (N=258; age range, 28–65 yrs) who acquired their SCI between 18 & 35 yrs of age, who were at least 10 yr post-SCI, & who used a wheelchair for their daily mobility. NBD Assessment: International SCI Bowel Function Basic Data Set. QoL Outcome Measures: NBD score, a simple rating scale. |
1. Severe NBD was present in 36% of all participants & in 40% of those using a conservative method. However, only 14% were (very) dissatisfied with their current bowel management. 2. Dissatisfaction with bowel management was significantly associated with constipation & severe NBD. 3. With increasing time since injury, there was a nonsignificant trend observed toward a decline in dissatisfaction with bowel management & a significant decline in severe NBD. |
| Anson et al (1993)44 Cross-sectional & longitudinal survey |
Objective: Explore relationships among social support, adjustment, & secondary complications in persons with SCI. Population: 125 persons with SCI, 18 yrs + YPI > 1 yr. NBD Assessment: SCI QLI QoL Outcome Measures: SCI QLI; RSS scale. |
4. Social adjustment was associated with the number of diarrhea events. 5. Getting advice was negatively (r = −.029) associated with number of diarrhea events (p < .05). 6. No differences in diarrhea or constipation between high- & low-level support groups. |
| Branagan et al (2003)43 Cross-sectional survey |
Objective: Evaluate the effect of intestinal stoma formation in SCI patients. Population: 32 (27 men) patients with SCI (tetraplegia, paraplegia), mean age at onset 28.9 (range, 6–62 yrs), mean time of injury to stoma formation 17.1 mos (0–36.25). NBD Assessment: Presence of stoma QoL Outcome Measures: Nonstandardized study-specific questionnaire. |
1 18 patients reported that a stoma gave them ↑ independence, 12 reported no difference, & 1 felt his independence ↓ despite a significant ↓ time spent in bowel care. 2. QoL after stoma formation was described as much better by 25 patients, as better by 5, & QoL as worse by 1. |
| Christensen et al (2000)31 Cross-sectional survey |
Objective: Evaluate an ECC & MACE in patients with SCI. Population: 21 patients (10 men) with SCI offered ECC, mean age 39.9 (range, 7±72 yrs). 8 patients with SCI (3 men) + MACE, mean age 32.8 (range, 15–66 yrs). NBD Assessment: Single capsule with 24 or 10 radiopaque markers followed by abdominal X-ray; bowel management techniques. QoL Outcome Measures: Nonstandardized study-specific questionnaire. |
1. Before treatment with the ECC, 7 out of 11 patients available for follow-up felt that colorectal dysfunction imposed a major restriction on their QoL & social activities. 2. Before treatment with the ECC, 2 patients reported some restrictions, 1 reported a minor restriction, & 1 failed to answer the question. 3. At follow-up, 2 patients reported that colorectal dysfunction caused only some or little restriction & 3 patients reported no restriction. 4. At follow-up, 2 felt some restriction, 6 reported a minor restriction, & 6 reported no restriction. 5. Before MACE, 3 out of 5 patients were available at follow-up. |
| Christensen et al (2006)29 Prospective, randomized controlled multicenter trial |
Objective: Compare outcomes of transanal irrigation vs conservative bowel management in patients with SCI. Population: 87 patients (18 men) with SCI, median age 31.6 ± 13.3 yrs. NBD Assessment: St. Mark's Fecal Incontinence; CCCSS; Modified American Society of Colorectal Surgeon fecal incontinence scores. QoL Outcome Measures: NBD score |
1. Compared with conservative bowel management, transanal irrigation improves constipation, fecal incontinence, & symptom-related QoL. |
| Christensen et al (2008)28 Prospective, randomizedcontrolled multicenter trial |
Objective: Compare the symptoms of NBD in patients with SCI at baseline & after 10 weeks of treatment with transanal irrigation & identify possible factors that could predict treatment outcome. Population: 62 patients (45 men) with SCI (supraconal conal/cauda equina, complete, incomplete), mean age 47.5 ±15.5. NBD Assessment: Transanal irrigation, CCCSS; St. Mark's Fecal Incontinence. QoL Outcome Measures: NBD score |
1. Scores on the NBD improved from baseline to termination (p < .0001). 2. Regression analyses revealed that there was a reduction in the impact of bowel dysfunction on QoL but depended significantly on complete injury, being male, & ability to walk & varied significantly between study centres. |
| Coggrave et al (2009)45 Cross-sectional survey |
Objective: Describe bowel management in community dwelling persons with SCI & explore associations between age, injury, dependency problems, interventions, & satisfaction. Population: 1,334 persons (73.4% men) with SCI, median age 52 (19–91 yrs), median YPI 18 (1–65 yrs). NBD Assessment: Self-report (survey). QoL Outcome Measures: Nonstandardized study-specific questionnaire. |
1. Bowel dysfunction impacted on life activities to varying degrees & impact of bowel dysfunction was rated as significantly ↑ (p .001) than other aspects of SCI. 2. 20% of respondents were dissatisfied or very dissatisfied with bowel management & low satisfaction was associated with more frequent incontinence (p < .001), more problems (p < .001), longer duration of care (p< .001), more management (p = .008), & more interventions used (p < .001). |
| Coggrave et al (2013)15 Multicentre, retrospective self-report postal survey |
Objective: Characterize SCI individuals with a stoma, their stoma management & outcomes, identify sources of information & support for decision making & explore the impact of a stoma on life satisfaction. Population: 92 individuals, mean age 56 yrs, mean duration of injury 26 yrs, 91% with colostomy, 9% ileostomy. NBD Assessment: Self-report (survey). QoL Outcome Measures: Nonstandardized study-specific questionnaire (accompanied by TSCS, SWLS, & HADS) & 3-item nonstandardized questionnaire. |
1. Satisfaction with stoma was high; provision of sufficient information preoperatively was important, those with ileostomy were more dependent & less satisfied. 2. Life satisfaction & physical self-concept were both lower in this sample than in previously reported samples of SCI individuals without reported bowel difficulties or stoma. |
| Craven et al (2012)46 Cross-sectional survey |
Objective: Describe the relationships between secondary health conditions & health preference post SCI. Population: 357 persons (218 men) with SCI (AIS A-D), mean age 54.0 (range, 24–89), mean YPI 19.3 (range, 2–65). NBD Assessment: Bowel dysfunction item from the SCS. QoL Outcome Measures: HUI-III. |
1. Persons in no/mild bowel dysfunction group had ↑ (p < .0001) HUI-III scores than those in the moderate/severe bowel dysfunction group. |
| Del Popolo et al (2008)37 Pre-post intervention |
Objective: Evaluate the effects of Peristeen Anal Irrigation on NBD & QoL. Population: 36 patients (18 men) with SCI, median age 31.6 ± 13.3 yrs. NBD Assessment: Function, duration of the evacuation disorder, method of defecation, dietary supplements, the need for assistance for evacuation & the predominant intestinal symptom during/after defecation, NBD. QoL Outcome Measures: Nonstandardized study-specific questionnaire. |
1. Patient's opinions of their QoL score & degree of satisfaction ↑ from pre- to post-intervention (p = .001). 2. A high percentage of patients reported a change in their level of dependency after the treatment period. |
| Faaborg et al (2008)56 Longitudinal |
Objective: Describe long-term colorectal function in SCI patients. Population: 72 patients (48 men) with SCI, mean age 38.0 ± 11.9 yrs, YPI 37.5 ± 45.2 mos. NBD Assessment: Self-reported constipation, obstructed defecation, & fecal incontinence (survey). QoL Outcome Measures: Non-standardized study specific questionnaire; NBD score. |
1. The impact of colorectal dysfunction causing some or major restrictions on QoL or social activities ↑ from 25% to 38% from 1996 to 2006 (p < .005). 2. The impact of constipation influencing QoL ↑ from 15% to 23% from 1996 to 2006 (p < .15). |
| Glickman & Kamm (1996)4 Cross-sectional survey |
Objective: Determine the prevalence, nature, & effects – both physical & psychological – of SCI on bowel function. Population: 115 outpatients (77% men) with SCI, median age 38 (18–75 yrs), median YPI 62 (9–491 mos). NBD Assessment: Self-report (survey). QoL Outcome Measures: HADS; non-standardized questionnaire. |
1. Bowel dysfunction was a source of psychological distress in 54% of patients & was associated with time required for bowel management (p = .005) & frequency of incontinence (p = .001). 2. HADS scores correlated significantly with time taken for bowel management. 3. Bowel management problems were rated above urinary problems & not far below loss of mobility, impaired sexual function, & dependence. |
| Han et al (1998)47 Cross-sectional survey |
Objective: Investigate the characteristics of chronic GI problems & bowel dysfunction in patients with SCI. Population: 72 patients (48 men) with SCI, mean age 38.0 ± 11.9 yrs, YPI 37.5 ± 45.2 mos. NBD Assessment: Self-report (survey). QoL Outcome Measures: MBI Score. |
1. Bowel dysfunction was unrelated to age, duration, & neurological level of SCI, ASIA score, or level of activity. 2. Post-SCI GI problems were mainly bowel problems such as defecation difficulty (40.3%) & this affected ADL. |
| Hicken et al (2001)39 Case-control |
Objective: Examined the QoL among individuals with SCI requiring assistance for bowel & bladder management compared to those with independent control of their bladders & bowels. Population: 53 matched pairs (49% men): (1) bladder/bowel dependent individuals & (2) bladder/bowel independent individuals, mean age 37.02 yrs, YPI divided into 4 groups (1, 2–5, 6–15, >16 yrs). Groups matched on age, sex, education, race, & lesion level. NBD Assessment: FIM. QoL Outcome Measures: CHART; SWLS; SF-12. |
1. The bladder/bowel-dependent individuals reported ↓ life satisfaction & greater overall handicap (p < .001). In particular, persons who were bladder dependent had lower CHART subscale scores than bladder independent group on the following: physical independence (p < .001), mobility (p < .001), & occupational functioning (p < .05). 2. The bladder/bowel independent group initiated more social contact with strangers compared to bladder/bowel-dependent individuals (p = .056). 3. Although there were no group differences concerning social integration, the bladder/bowel-dependent group may have more difficulties initiating new social relationships. |
| Kachourbos & Creasey (2000)32 Post-intervention cross-sectional survey |
Objective: Assess recollections of health & QoL preoperatively in relation to bladder & bowel care & rate changes in QoL post-implant of an implantable stimulator. Population: 16 persons with SCI, 6 mos post surgery. NBD Assessment: Presence of implantable stimulator. QoL Outcome Measures: Non-standardized study specific questionnaire. |
1. Bowel program times were reduced from a mean of 5.4 hr per week preoperatively to 2.0 hr per week postoperatively. 2. Respondents reported a greater sense of independence, ↑ socialization, greater control over their lives, improved interpersonal relationships, improved self-image, ↓ feelings of depression, & an overall improvement in QoL. |
| Kelly et al (1999)30 Retrospective chart review & cross-sectional survey |
Objective: Evaluate the long-term outcomes of intestinal stomas post-SCI. Population: 14 patients (16 men) with SCI, mean age 54.8 yrs at time of stoma, mean time from SCI to stoma 15 yrs. NBD Assessment: Presence of stoma. QoL Outcome Measures: Nonstandardized study specific questionnaire. Similar to Dijker's typical QoL measure of ADL. |
1. Ten patients reported that colostomy was beneficial to their QoL. One person whose QoL remained unchanged post colostomy reported worse QoL at 10-yr follow-up. |
| Kim (2012)48 Cross-sectional survey |
Objective: Describe defecation stimulation methods & their outcomes & investigate the impact of bowel dysfunction on QoL in SCI. Population: 388 persons with SCI (295 men), mean age 44.5±10.8 yrs, mean YPI 14.2±9.5 yrs. NBD Assessment: Bowel stimulation method, frequency of bowel movements, defecation time, symptoms of AD, frequency of fecal incontinence, & flatus. QoL Outcome Measures: Nonstandardized study-specific questionnaire. |
1. Frequency of fecal incontinence had the greatest effects on QoL. 2. When patients had fecal incontinence every day, they had 67.4 times greater chance to obtain severely lowered general QoL. 3. Time taken in defecation >60 min, presence of perianal skin problem, & flatus incontinence also significantly influenced QoL. 4. QoL deterioration differs between each stimulation user. Decline in general QoL was greater in large-volume enemas users than in DRS users. 5. Social QoL deterioration was much more profound in large-volume enemas users than in DRS or finger evacuations users. 6. QoL at home was lower in patients using large-volume enemas than in those using other methods. 7. Mini-enema users had worse QoL at home than digital rectal stim users |
| Kirk et al (1997)5 Cross-sectional survey |
Objective: Describe impact of NBD on life activities. Population: 171 adults (128 men) with SCI, mean age 39.5 ± 14.5 yrs, mean YPI 8.9 ± 8.9. NBD Assessment: Self-report (survey). QoL Outcome Measures: Nonstandardized study-specific questionnaire (Bowel Program Outcome Questionnaire). |
1. 61% indicated NBD interfered with their life. 2. 47 of 105 respondents described a loss of freedom to go places, missing work, school or social events, or having to plan their lives around their bowels. |
| Krogh et al (1997)50 Cross-sectional survey |
Objective: Describe the frequency & severity of colorectal problems among patients with spinal cord lesions & determine whether these problems are associated with age, gender, time since lesion, level & severity of lesion. Population: 424 persons with SCI (300 men), mean age 41 (range 8–88 yrs), YPI 41 (range 0–59 yrs). NBD Assessment: Self-report (survey). QoL Outcome Measures: Nonstandardized study-specific questionnaire. |
1. 39% reported colorectal dysfunction caused some/major restrictions on social activities or QoL. 2. 29% reported disturbed defecation caused some/major restriction on social activities & 32% reported it caused some/major restriction on QoL. 3. 19% reported fecal incontinence caused some/major restriction on social activities & 20% reported it caused some/major restriction on QoL. 4. 30% reported bowel dysfunction was ↑ than bladder or sexual dysfunction. |
| Krogh et al (2006)49 Cross-sectional survey |
Objective: Develop & validate a symptom-based score for the NBD score. Population: 424 persons (72% men) with SCI, mean age 41 (8–88 yrs), mean YPI 14 (0–88 yrs). NBD Assessment: NBD score. QoL Outcome Measures: NBD score. |
1. Several items on the NBD found the impact on QoL ↑ with the severity of symptoms. Frequency of bowel movements was associated with QoL (p < .0001), as was frequency of fecal incontinence. 2. Difference in NBD scores among patients reporting no, little, some, or major impacts on QoL were significant (p < .001). 3. There may be an association between self-reported QoL & restriction of social activities due to bowel dysfunction. |
| Liu et al (2009)51 Cross-sectional survey |
Objective: Assess the relationship between the severity of NBD & HrQoL in persons with various degrees of SCI. Population: 128 (95 men) respondents with SCI, 36 with tetraplegia, 58 with paraplegia, 34 with paresis, mean age 48.3 (range 13–84 yrs), YPI divided into 4 groups (1–2 yrs, 3–5 yrs, 6–10 yrs, & over 10 yrs). NBD Assessment: NBD score. QoL Outcome Measures: SF-36; NBD score. |
1. Persons with very minor NBD had the ↑ scores on the SF-36 in contrast to persons with severe NBD, who had the ↓scores. 2. Significant differences were found on the SF-36 physical functioning (p < .001) & the physical component summary (p < .001) subscales. 3. Participants with worse NBD were likely to have ↓physical QoL (p < .001). |
| Lombardi (2010)33 Retrospective non-blinded design without controls. |
Objective: Evaluate the efficacy & safety of sacral neuromodulation in incomplete SCI affected by chronic NBD. Population: 23 patients with SCI (13 men), mean age 36±9 yrs. NBD Assessment: Wexner Score; episodes of fecal incontinence, no. of evacuations/week. QoL Outcome Measures: SF-36. |
1. Patients in both groups (constipation & fecal incontienence) had significant ↓ (p < .05) in Wexner scores. 2. QoL in both groups consistently showed statistical improvement (p < .05). |
| Lombardi et al (2011)34 Retrospective cross-sectional survey |
Objective: Assess the concomitant clinical improvement in incomplete SCI with NBD using sacral neuromodulation. Population: 75 patients with incomplete SCI. NBD Assessment: Incontinence & constipation. QoL Outcome Measures: SF-36. |
1. Bladder function & incontinence improved. 2. In the general & mental health domains of the SF-36, all patients improved their scores by at least 20% compared with baseline after sacral neuromodulation. |
| Luther et al (2005)40 Case-control |
Objective: Compare QoL for people with NBD & SCI using either a standard care program or colostomy. Population: 74 veterans (73 men) with SCI + colostomy, 296 SCI controls without colostomy, age range < 20–89, YPI within past 20 yr. NBD Assessment: Presence of colostomy. QoL Outcome Measures: IBDQ. |
1. No significant differences were detected on IBDQ between persons with SCI + colostomy & those with SCI only. |
| Lynch et al (2000)10 Controlled, descriptive & comparative questionnaire study |
Objective: Describe the bowel function of SCI patients & compare it to a general community control group. Population: 467 SCI patients & 467 control subjects were age & gender matched. Mean age for the SCI patients 43.5 (range, 15–89 yrs), mean YPI 14 (range, 0.7–42.1 yrs). Mean age for the controls 45.3 (range, 17–78 yr). NBD Assessment: General bowel function, incidence of incontinence, & defecation methods. QoL Outcome Measures: Nonstandardized questionnaire. |
1. Incontinence affected the QoL for 62% SCI patients compared to 8% of the controls. 2. Incontinence did not affect the majority of the controls (92.3%) in terms of everyday activities compared to 43.9% of SCI patients (p < .0001). |
| Noonan et al (2008)52 Cross-sectional survey |
Objective: Determine the effect of associated SCI conditions on health status & QoL. Population: 70 persons (57 men) with central cord syndrome, mean age at injury 45±18 yrs (range, 13–91), mean age at follow-up 51 ±18 yrs (range, 19–95). NBD Assessment: Self-report (survey). QoL Outcome Measures: SF-36; numeric QoL rating. |
1. Bowel, bladder & sexual dysfunction on the physical component score of the SF-36 were significant, but the effect ↓ when controlling for personal & confounding factors. 2. Bowel, bladder & sexual dysfunction were not related to the mental component scores of the SF-36. 3. Problems with bowel, bladder, & sexual dysfunction were significantly (p< .01) associated with QoL when personal & confounding factors were NOT controlled for. |
| Pardee et al (2012)8 Exploratory, descriptive correlational design |
Objective: Investigate the association between characteristics of individuals with SCI & neurogenic bowel & their perceived QoL. Population: 241 surveys; from adults over age 18, diagnosed with SCI & neurogenic bowel more than 2 yrs post injury, AIS of A, B, C, or D & residing in the community. NBD Assessment: Survey of neurogenic bowel characteristics. QoL Outcome Measures: QoL survey. |
1. Regardless of the bowel management program 54% (n = 127) were satisfied with current methods. Although time reported to complete bowel programs ranged from 1 to 120 min, there was no difference in rating of satisfaction with time. 2. There was a statistically significant difference between those satisfied & dissatisfied with current bowel management & QoL; those satisfied demonstrated a higher QoL on 3 subscales, work function (p = .021), bowel problems (p < .001), & social function (p < .001). Those dissatisfied with their bowel program perceived a lower QoL & indicated problem of time (p = .001), pain or discomfort (p = .033), & poor results (p < .001). |
| Randell et al (2001)41 Prospective controlled comparative analysis |
Objective: Determine whether a colostomy changes QoL in patients with SCI. Population: 26 (15 men) patients with SCI (tetraplegia, paraplegia) + colostomy, age range 22–87, range of injury to stoma formation 7 mos – 20 yrs. 26 SCI controls (age, gender, injury, & YPI matched) without colostomy. NBD Assessment: Presence of colostomy. QoL Outcome Measures: Burwood QoL Questionnaire. |
1. No significant differences were detected on QoL between persons with SCI + colostomy & those with SCI only. |
| Roach et al (2000)53 Cross-sectional survey |
Objective: Examine the relationship between bowel dysfunction, impediment to community integration & QoL in persons with SCI. Population: 103 SCI consumers (76.7% men), mean age 39 yrs, YPI 14 yr. NBD Assessment: Self-report (survey). QoL Outcome Measures: Andrews & Withey (1976) Life Satisfaction Survey; nonstandardized study specific questionnaire on community integration (ICI). |
1. Significant negative relationship between subjective severity & 3 ICI measures; the higher the perceived severity of bowel dysfunction, the more it affected (1) personal relationships (p < .01); (2) feelings about themselves (p < .01); (3) their home environment (p < .05). 2. The number of days each month a person stayed at home because of lack of bowel control was associated with all 3 ICI scales (p < .01). The ↑ bowel accidents per month, the ↑ negative a respondent felt about him/herself (p < .05). 3. None of the bowel dysfunction characteristics were significantly related to the satisfaction of life items, but non-parametric analyses revealed that 2 of the ICI items were associated with satisfaction with free time & family life. |
| Rosito et al (2002)35 Pre-post intervention |
Objective: Evaluate the effects of colostomy on the QoL in patients with SCI. Population: 27 patients (26 men) with SCI, mean age of 62.9 (range 44–79 yrs), YPI 25.8 (range 8–48 yrs), mean time since stoma formation 8 (range 1.5–28 yrs), mean time with severe bowel dysfunction 5.5 (range 0.5–18 yr). NBD Assessment: Presence of colostomy. QoL Outcome Measures: Nonstandardized study specific questionnaire. Similar to Dijker's typical QoL measure of ADL. |
1. Colostomy improved (p ≤ .0001) total QoL. 2. Significant improvements after colostomy observed in physical health, self-efficacy, psychosocial status, & recreation/leisure but not in body image. 3. 85% of patients reported an ↑ in total QoL after colostomy; 70% of patients were satisfied with their personal lives before colostomy compared to 89% of patients after colostomy. 4. 67% of patients felt more independent after colostomy compared to 30% of patients that felt the same level of independence. |
| Safadi et al (2003)36 Retrospective chart review & cross-sectional survey |
Objective: Evaluate the long-term outcomes of colostomies & ileostomies post SCI. Population: 45 patients (44 men) with SCI, mean age 55.9 yrs, mean time from SCI to stoma 20.3 yrs. NBD Assessment: Presence of stoma. QoL Outcome Measures: Nonstandardized study specific questionnaire. |
1. In the right-sided colostomy group (n=20), QoL & health status scores improved (p < .05). 2. In the left-sided colostomy group (n=20), QoL & health status scores improved (p < .05). 3. In the ileostomy group (n=7), QoL & health status scores improved (p < .05). |
| Teichman et al (2003)79 Retrospective review |
Objective: To determine the long-term outcomes from the Malone antegrade continence enema (ACE) procedure in adult neurogenic patients. Population: 6 patients (mean age = 35 yrs), mean follow-up of 4.5 yrs. NBD Assessment: Pre-ACE & post-ACE toileting times, bowel continence status, & complications. QoL Outcome Measures: Nonstandardized questionnaire. |
1. Five patients (83%) were satisfied with their outcome & rated their QoL higher after the ACE procedure compared with pre-ACE. |
| Westgren & Levi (1998)54 Cross-sectional survey |
Objective: Determine associations between major outcome variables after SCI & QoL. Population: 320 persons (261 men) with SCI, mean age 42 (17–78 yr), YPI ≤4 yrs & ≥4 yrs. NBD Assessment: Medical records via clinical database. QoL Outcome Measures: SF-36. |
1. Bowel dysfunction was associated with ↓ QoL. 2. Bowel dysfunction yielded a medium effect sizes in the general physical functioning (p = .001), bodily pain (p = .003), general health (p = .001), vitality (p = .001), social function (p = .004), & mental health (p = .001) subscales. |
| Worsøe et al (2008)42 Retrospective chart review & cross-sectional survey |
Objective: Evaluate the long-term outcomes of ACE & ACE + colostomy in patients with SCI. Population: 80 patients (12 men) with SCI, mean age 51 yrs at time of stoma, mean follow-up time was 75 mos (range, 3–183). NBD Assessment: Continued ACE or ACE+colostomy at follow-up; Wexner score. QoL Outcome Measures: Nonstandardized study-specific questionnaire. |
1. 34 of 43 patients still using ACE were satisfied or very satisfied with the result, 8 patients were neither satisfied nor dissatisfied, & none were dissatisfied or very dissatisfied. One person did not provide a response. 2. On an arbitrary scale (0–100) mean values for bowel function before & after were 12 & 81 respectively (p < .01). For social function, the corresponding values were 30 & 81 (p < .01) & for QoL they were 28 & 81 (p < .01). |
| Tulsky et al (2015)57 Mixed-methods design |
Objective: To describe the development & psychometric properties of the SCI-QoL Bladder Management Difficulties & Bowel Management Difficulties item banks & Bladder Complications scale. Population: 757 adults with traumatic SCI of traumatic etiology, 18 yrs of age & older. NBD Assessment: N/A QoL Outcome Measures: In development. |
1. The SCI-QoL Bladder Management Difficulties & Bowel Management Difficulties item banks are psychometrically robust & are available as computer adaptive tests or short forms. |
Note: Studies are listed in alphabetical order according to the last name of the first author. ACE = antegrade colonic enema; AD = autonomic dysreflexia; ADL = activities of daily living; AIS = American Spinal Injury Association Impairment Scale; CHART = Criag Handicap and Assessment Reporting Technique; CCCSS = Cleveland Clinic Constipation Scoring System; DRS = digital rectal stimulation; ECC = enema continence catheter; FIM = Functional Independence Measure; GI = gastrointestinal; HADS = Hospital Anxiety & Depression Scale; HrQoL = health-related quality of life; HUI = Health Utilities Index; ICI = impediments to community integration; MBI = Modified Barthel Index; mos = months; NBD = neurogenic bowel dysfunction; N/A = not available; QLI = Quality of Life Index; QoL = quality of life; RSS = Reciprocal Support Scale; SCI = spinal cord injury(ies); SCS = Secondary Condition Scale; SF-12 = Short-Form 12; SF-36 = Short-Form 36; SWLS = Satisfaction with Life Scale; YPI = years post injury; yr(s) = years.
Table 1.
Identified studies (CONT.)
|
DESIGN Author (year) Research design |
METHODS (Objective, Population, Bowel Dysfunction Assessment, QoL Outcome Measures) |
QoL RESULTS |
|---|---|---|
| Adriaansen et al (2015)55 Cross-sectional multicenter study |
Objective: Describe bowel management & its outcomes in individuals living with an SCI for at least 10 yrs. Population: Individuals (N=258; age range, 28–65 yrs) who acquired their SCI between 18 & 35 yrs of age, who were at least 10 yr post-SCI, & who used a wheelchair for their daily mobility. NBD Assessment: International SCI Bowel Function Basic Data Set. QoL Outcome Measures: NBD score, a simple rating scale. |
1. Severe NBD was present in 36% of all participants & in 40% of those using a conservative method. However, only 14% were (very) dissatisfied with their current bowel management. 2. Dissatisfaction with bowel management was significantly associated with constipation & severe NBD. 3. With increasing time since injury, there was a nonsignificant trend observed toward a decline in dissatisfaction with bowel management & a significant decline in severe NBD. |
| Anson et al (1993)44 Cross-sectional & longitudinal survey |
Objective: Explore relationships among social support, adjustment, & secondary complications in persons with SCI. Population: 125 persons with SCI, 18 yrs + YPI > 1 yr. NBD Assessment: SCI QLI QoL Outcome Measures: SCI QLI; RSS scale. |
4. Social adjustment was associated with the number of diarrhea events. 5. Getting advice was negatively (r = −.029) associated with number of diarrhea events (p < .05). 6. No differences in diarrhea or constipation between high- & low-level support groups. |
| Branagan et al (2003)43 Cross-sectional survey |
Objective: Evaluate the effect of intestinal stoma formation in SCI patients. Population: 32 (27 men) patients with SCI (tetraplegia, paraplegia), mean age at onset 28.9 (range, 6–62 yrs), mean time of injury to stoma formation 17.1 mos (0–36.25). NBD Assessment: Presence of stoma QoL Outcome Measures: Nonstandardized study-specific questionnaire. |
1 18 patients reported that a stoma gave them ↑ independence, 12 reported no difference, & 1 felt his independence ↓ despite a significant ↓ time spent in bowel care. 2. QoL after stoma formation was described as much better by 25 patients, as better by 5, & QoL as worse by 1. |
| Christensen et al (2000)31 Cross-sectional survey |
Objective: Evaluate an ECC & MACE in patients with SCI. Population: 21 patients (10 men) with SCI offered ECC, mean age 39.9 (range, 7±72 yrs). 8 patients with SCI (3 men) + MACE, mean age 32.8 (range, 15–66 yrs). NBD Assessment: Single capsule with 24 or 10 radiopaque markers followed by abdominal X-ray; bowel management techniques. QoL Outcome Measures: Nonstandardized study-specific questionnaire. |
1. Before treatment with the ECC, 7 out of 11 patients available for follow-up felt that colorectal dysfunction imposed a major restriction on their QoL & social activities. 2. Before treatment with the ECC, 2 patients reported some restrictions, 1 reported a minor restriction, & 1 failed to answer the question. 3. At follow-up, 2 patients reported that colorectal dysfunction caused only some or little restriction & 3 patients reported no restriction. 4. At follow-up, 2 felt some restriction, 6 reported a minor restriction, & 6 reported no restriction. 5. Before MACE, 3 out of 5 patients were available at follow-up. |
| Christensen et al (2006)29 Prospective, randomized controlled multicenter trial |
Objective: Compare outcomes of transanal irrigation vs conservative bowel management in patients with SCI. Population: 87 patients (18 men) with SCI, median age 31.6 ± 13.3 yrs. NBD Assessment: St. Mark's Fecal Incontinence; CCCSS; Modified American Society of Colorectal Surgeon fecal incontinence scores. QoL Outcome Measures: NBD score |
1. Compared with conservative bowel management, transanal irrigation improves constipation, fecal incontinence, & symptom-related QoL. |
| Christensen et al (2008)28 Prospective, randomizedcontrolled multicenter trial |
Objective: Compare the symptoms of NBD in patients with SCI at baseline & after 10 weeks of treatment with transanal irrigation & identify possible factors that could predict treatment outcome. Population: 62 patients (45 men) with SCI (supraconal conal/cauda equina, complete, incomplete), mean age 47.5 ±15.5. NBD Assessment: Transanal irrigation, CCCSS; St. Mark's Fecal Incontinence. QoL Outcome Measures: NBD score |
1. Scores on the NBD improved from baseline to termination (p < .0001). 2. Regression analyses revealed that there was a reduction in the impact of bowel dysfunction on QoL but depended significantly on complete injury, being male, & ability to walk & varied significantly between study centres. |
| Coggrave et al (2009)45 Cross-sectional survey |
Objective: Describe bowel management in community dwelling persons with SCI & explore associations between age, injury, dependency problems, interventions, & satisfaction. Population: 1,334 persons (73.4% men) with SCI, median age 52 (19–91 yrs), median YPI 18 (1–65 yrs). NBD Assessment: Self-report (survey). QoL Outcome Measures: Nonstandardized study-specific questionnaire. |
1. Bowel dysfunction impacted on life activities to varying degrees & impact of bowel dysfunction was rated as significantly ↑ (p .001) than other aspects of SCI. 2. 20% of respondents were dissatisfied or very dissatisfied with bowel management & low satisfaction was associated with more frequent incontinence (p < .001), more problems (p < .001), longer duration of care (p< .001), more management (p = .008), & more interventions used (p < .001). |
| Coggrave et al (2013)15 Multicentre, retrospective self-report postal survey |
Objective: Characterize SCI individuals with a stoma, their stoma management & outcomes, identify sources of information & support for decision making & explore the impact of a stoma on life satisfaction. Population: 92 individuals, mean age 56 yrs, mean duration of injury 26 yrs, 91% with colostomy, 9% ileostomy. NBD Assessment: Self-report (survey). QoL Outcome Measures: Nonstandardized study-specific questionnaire (accompanied by TSCS, SWLS, & HADS) & 3-item nonstandardized questionnaire. |
1. Satisfaction with stoma was high; provision of sufficient information preoperatively was important, those with ileostomy were more dependent & less satisfied. 2. Life satisfaction & physical self-concept were both lower in this sample than in previously reported samples of SCI individuals without reported bowel difficulties or stoma. |
| Craven et al (2012)46 Cross-sectional survey |
Objective: Describe the relationships between secondary health conditions & health preference post SCI. Population: 357 persons (218 men) with SCI (AIS A-D), mean age 54.0 (range, 24–89), mean YPI 19.3 (range, 2–65). NBD Assessment: Bowel dysfunction item from the SCS. QoL Outcome Measures: HUI-III. |
1. Persons in no/mild bowel dysfunction group had ↑ (p < .0001) HUI-III scores than those in the moderate/severe bowel dysfunction group. |
| Del Popolo et al (2008)37 Pre-post intervention |
Objective: Evaluate the effects of Peristeen Anal Irrigation on NBD & QoL. Population: 36 patients (18 men) with SCI, median age 31.6 ± 13.3 yrs. NBD Assessment: Function, duration of the evacuation disorder, method of defecation, dietary supplements, the need for assistance for evacuation & the predominant intestinal symptom during/after defecation, NBD. QoL Outcome Measures: Nonstandardized study-specific questionnaire. |
1. Patient's opinions of their QoL score & degree of satisfaction ↑ from pre- to post-intervention (p = .001). 2. A high percentage of patients reported a change in their level of dependency after the treatment period. |
| Faaborg et al (2008)56 Longitudinal |
Objective: Describe long-term colorectal function in SCI patients. Population: 72 patients (48 men) with SCI, mean age 38.0 ± 11.9 yrs, YPI 37.5 ± 45.2 mos. NBD Assessment: Self-reported constipation, obstructed defecation, & fecal incontinence (survey). QoL Outcome Measures: Non-standardized study specific questionnaire; NBD score. |
1. The impact of colorectal dysfunction causing some or major restrictions on QoL or social activities ↑ from 25% to 38% from 1996 to 2006 (p < .005). 2. The impact of constipation influencing QoL ↑ from 15% to 23% from 1996 to 2006 (p < .15). |
| Glickman & Kamm (1996)4 Cross-sectional survey |
Objective: Determine the prevalence, nature, & effects – both physical & psychological – of SCI on bowel function. Population: 115 outpatients (77% men) with SCI, median age 38 (18–75 yrs), median YPI 62 (9–491 mos). NBD Assessment: Self-report (survey). QoL Outcome Measures: HADS; non-standardized questionnaire. |
1. Bowel dysfunction was a source of psychological distress in 54% of patients & was associated with time required for bowel management (p = .005) & frequency of incontinence (p = .001). 2. HADS scores correlated significantly with time taken for bowel management. 3. Bowel management problems were rated above urinary problems & not far below loss of mobility, impaired sexual function, & dependence. |
| Han et al (1998)47 Cross-sectional survey |
Objective: Investigate the characteristics of chronic GI problems & bowel dysfunction in patients with SCI. Population: 72 patients (48 men) with SCI, mean age 38.0 ± 11.9 yrs, YPI 37.5 ± 45.2 mos. NBD Assessment: Self-report (survey). QoL Outcome Measures: MBI Score. |
1. Bowel dysfunction was unrelated to age, duration, & neurological level of SCI, ASIA score, or level of activity. 2. Post-SCI GI problems were mainly bowel problems such as defecation difficulty (40.3%) & this affected ADL. |
| Hicken et al (2001)39 Case-control |
Objective: Examined the QoL among individuals with SCI requiring assistance for bowel & bladder management compared to those with independent control of their bladders & bowels. Population: 53 matched pairs (49% men): (1) bladder/bowel dependent individuals & (2) bladder/bowel independent individuals, mean age 37.02 yrs, YPI divided into 4 groups (1, 2–5, 6–15, >16 yrs). Groups matched on age, sex, education, race, & lesion level. NBD Assessment: FIM. QoL Outcome Measures: CHART; SWLS; SF-12. |
1. The bladder/bowel-dependent individuals reported ↓ life satisfaction & greater overall handicap (p < .001). In particular, persons who were bladder dependent had lower CHART subscale scores than bladder independent group on the following: physical independence (p < .001), mobility (p < .001), & occupational functioning (p < .05). 2. The bladder/bowel independent group initiated more social contact with strangers compared to bladder/bowel-dependent individuals (p = .056). 3. Although there were no group differences concerning social integration, the bladder/bowel-dependent group may have more difficulties initiating new social relationships. |
| Kachourbos & Creasey (2000)32 Post-intervention cross-sectional survey |
Objective: Assess recollections of health & QoL preoperatively in relation to bladder & bowel care & rate changes in QoL post-implant of an implantable stimulator. Population: 16 persons with SCI, 6 mos post surgery. NBD Assessment: Presence of implantable stimulator. QoL Outcome Measures: Non-standardized study specific questionnaire. |
1. Bowel program times were reduced from a mean of 5.4 hr per week preoperatively to 2.0 hr per week postoperatively. 2. Respondents reported a greater sense of independence, ↑ socialization, greater control over their lives, improved interpersonal relationships, improved self-image, ↓ feelings of depression, & an overall improvement in QoL. |
| Kelly et al (1999)30 Retrospective chart review & cross-sectional survey |
Objective: Evaluate the long-term outcomes of intestinal stomas post-SCI. Population: 14 patients (16 men) with SCI, mean age 54.8 yrs at time of stoma, mean time from SCI to stoma 15 yrs. NBD Assessment: Presence of stoma. QoL Outcome Measures: Nonstandardized study specific questionnaire. Similar to Dijker's typical QoL measure of ADL. |
1. Ten patients reported that colostomy was beneficial to their QoL. One person whose QoL remained unchanged post colostomy reported worse QoL at 10-yr follow-up. |
| Kim (2012)48 Cross-sectional survey |
Objective: Describe defecation stimulation methods & their outcomes & investigate the impact of bowel dysfunction on QoL in SCI. Population: 388 persons with SCI (295 men), mean age 44.5±10.8 yrs, mean YPI 14.2±9.5 yrs. NBD Assessment: Bowel stimulation method, frequency of bowel movements, defecation time, symptoms of AD, frequency of fecal incontinence, & flatus. QoL Outcome Measures: Nonstandardized study-specific questionnaire. |
1. Frequency of fecal incontinence had the greatest effects on QoL. 2. When patients had fecal incontinence every day, they had 67.4 times greater chance to obtain severely lowered general QoL. 3. Time taken in defecation >60 min, presence of perianal skin problem, & flatus incontinence also significantly influenced QoL. 4. QoL deterioration differs between each stimulation user. Decline in general QoL was greater in large-volume enemas users than in DRS users. 5. Social QoL deterioration was much more profound in large-volume enemas users than in DRS or finger evacuations users. 6. QoL at home was lower in patients using large-volume enemas than in those using other methods. 7. Mini-enema users had worse QoL at home than digital rectal stim users |
| Kirk et al (1997)5 Cross-sectional survey |
Objective: Describe impact of NBD on life activities. Population: 171 adults (128 men) with SCI, mean age 39.5 ± 14.5 yrs, mean YPI 8.9 ± 8.9. NBD Assessment: Self-report (survey). QoL Outcome Measures: Nonstandardized study-specific questionnaire (Bowel Program Outcome Questionnaire). |
1. 61% indicated NBD interfered with their life. 2. 47 of 105 respondents described a loss of freedom to go places, missing work, school or social events, or having to plan their lives around their bowels. |
| Krogh et al (1997)50 Cross-sectional survey |
Objective: Describe the frequency & severity of colorectal problems among patients with spinal cord lesions & determine whether these problems are associated with age, gender, time since lesion, level & severity of lesion. Population: 424 persons with SCI (300 men), mean age 41 (range 8–88 yrs), YPI 41 (range 0–59 yrs). NBD Assessment: Self-report (survey). QoL Outcome Measures: Nonstandardized study-specific questionnaire. |
1. 39% reported colorectal dysfunction caused some/major restrictions on social activities or QoL. 2. 29% reported disturbed defecation caused some/major restriction on social activities & 32% reported it caused some/major restriction on QoL. 3. 19% reported fecal incontinence caused some/major restriction on social activities & 20% reported it caused some/major restriction on QoL. 4. 30% reported bowel dysfunction was ↑ than bladder or sexual dysfunction. |
| Krogh et al (2006)49 Cross-sectional survey |
Objective: Develop & validate a symptom-based score for the NBD score. Population: 424 persons (72% men) with SCI, mean age 41 (8–88 yrs), mean YPI 14 (0–88 yrs). NBD Assessment: NBD score. QoL Outcome Measures: NBD score. |
1. Several items on the NBD found the impact on QoL ↑ with the severity of symptoms. Frequency of bowel movements was associated with QoL (p < .0001), as was frequency of fecal incontinence. 2. Difference in NBD scores among patients reporting no, little, some, or major impacts on QoL were significant (p < .001). 3. There may be an association between self-reported QoL & restriction of social activities due to bowel dysfunction. |
| Liu et al (2009)51 Cross-sectional survey |
Objective: Assess the relationship between the severity of NBD & HrQoL in persons with various degrees of SCI. Population: 128 (95 men) respondents with SCI, 36 with tetraplegia, 58 with paraplegia, 34 with paresis, mean age 48.3 (range 13–84 yrs), YPI divided into 4 groups (1–2 yrs, 3–5 yrs, 6–10 yrs, & over 10 yrs). NBD Assessment: NBD score. QoL Outcome Measures: SF-36; NBD score. |
1. Persons with very minor NBD had the ↑ scores on the SF-36 in contrast to persons with severe NBD, who had the ↓scores. 2. Significant differences were found on the SF-36 physical functioning (p < .001) & the physical component summary (p < .001) subscales. 3. Participants with worse NBD were likely to have ↓physical QoL (p < .001). |
| Lombardi (2010)33 Retrospective non-blinded design without controls. |
Objective: Evaluate the efficacy & safety of sacral neuromodulation in incomplete SCI affected by chronic NBD. Population: 23 patients with SCI (13 men), mean age 36±9 yrs. NBD Assessment: Wexner Score; episodes of fecal incontinence, no. of evacuations/week. QoL Outcome Measures: SF-36. |
1. Patients in both groups (constipation & fecal incontienence) had significant ↓ (p < .05) in Wexner scores. 2. QoL in both groups consistently showed statistical improvement (p < .05). |
| Lombardi et al (2011)34 Retrospective cross-sectional survey |
Objective: Assess the concomitant clinical improvement in incomplete SCI with NBD using sacral neuromodulation. Population: 75 patients with incomplete SCI. NBD Assessment: Incontinence & constipation. QoL Outcome Measures: SF-36. |
1. Bladder function & incontinence improved. 2. In the general & mental health domains of the SF-36, all patients improved their scores by at least 20% compared with baseline after sacral neuromodulation. |
| Luther et al (2005)40 Case-control |
Objective: Compare QoL for people with NBD & SCI using either a standard care program or colostomy. Population: 74 veterans (73 men) with SCI + colostomy, 296 SCI controls without colostomy, age range < 20–89, YPI within past 20 yr. NBD Assessment: Presence of colostomy. QoL Outcome Measures: IBDQ. |
1. No significant differences were detected on IBDQ between persons with SCI + colostomy & those with SCI only. |
| Lynch et al (2000)10 Controlled, descriptive & comparative questionnaire study |
Objective: Describe the bowel function of SCI patients & compare it to a general community control group. Population: 467 SCI patients & 467 control subjects were age & gender matched. Mean age for the SCI patients 43.5 (range, 15–89 yrs), mean YPI 14 (range, 0.7–42.1 yrs). Mean age for the controls 45.3 (range, 17–78 yr). NBD Assessment: General bowel function, incidence of incontinence, & defecation methods. QoL Outcome Measures: Nonstandardized questionnaire. |
1. Incontinence affected the QoL for 62% SCI patients compared to 8% of the controls. 2. Incontinence did not affect the majority of the controls (92.3%) in terms of everyday activities compared to 43.9% of SCI patients (p < .0001). |
| Noonan et al (2008)52 Cross-sectional survey |
Objective: Determine the effect of associated SCI conditions on health status & QoL. Population: 70 persons (57 men) with central cord syndrome, mean age at injury 45±18 yrs (range, 13–91), mean age at follow-up 51 ±18 yrs (range, 19–95). NBD Assessment: Self-report (survey). QoL Outcome Measures: SF-36; numeric QoL rating. |
1. Bowel, bladder & sexual dysfunction on the physical component score of the SF-36 were significant, but the effect ↓ when controlling for personal & confounding factors. 2. Bowel, bladder & sexual dysfunction were not related to the mental component scores of the SF-36. 3. Problems with bowel, bladder, & sexual dysfunction were significantly (p< .01) associated with QoL when personal & confounding factors were NOT controlled for. |
| Pardee et al (2012)8 Exploratory, descriptive correlational design |
Objective: Investigate the association between characteristics of individuals with SCI & neurogenic bowel & their perceived QoL. Population: 241 surveys; from adults over age 18, diagnosed with SCI & neurogenic bowel more than 2 yrs post injury, AIS of A, B, C, or D & residing in the community. NBD Assessment: Survey of neurogenic bowel characteristics. QoL Outcome Measures: QoL survey. |
1. Regardless of the bowel management program 54% (n = 127) were satisfied with current methods. Although time reported to complete bowel programs ranged from 1 to 120 min, there was no difference in rating of satisfaction with time. 2. There was a statistically significant difference between those satisfied & dissatisfied with current bowel management & QoL; those satisfied demonstrated a higher QoL on 3 subscales, work function (p = .021), bowel problems (p < .001), & social function (p < .001). Those dissatisfied with their bowel program perceived a lower QoL & indicated problem of time (p = .001), pain or discomfort (p = .033), & poor results (p < .001). |
| Randell et al (2001)41 Prospective controlled comparative analysis |
Objective: Determine whether a colostomy changes QoL in patients with SCI. Population: 26 (15 men) patients with SCI (tetraplegia, paraplegia) + colostomy, age range 22–87, range of injury to stoma formation 7 mos – 20 yrs. 26 SCI controls (age, gender, injury, & YPI matched) without colostomy. NBD Assessment: Presence of colostomy. QoL Outcome Measures: Burwood QoL Questionnaire. |
1. No significant differences were detected on QoL between persons with SCI + colostomy & those with SCI only. |
| Roach et al (2000)53 Cross-sectional survey |
Objective: Examine the relationship between bowel dysfunction, impediment to community integration & QoL in persons with SCI. Population: 103 SCI consumers (76.7% men), mean age 39 yrs, YPI 14 yr. NBD Assessment: Self-report (survey). QoL Outcome Measures: Andrews & Withey (1976) Life Satisfaction Survey; nonstandardized study specific questionnaire on community integration (ICI). |
1. Significant negative relationship between subjective severity & 3 ICI measures; the higher the perceived severity of bowel dysfunction, the more it affected (1) personal relationships (p < .01); (2) feelings about themselves (p < .01); (3) their home environment (p < .05). 2. The number of days each month a person stayed at home because of lack of bowel control was associated with all 3 ICI scales (p < .01). The ↑ bowel accidents per month, the ↑ negative a respondent felt about him/herself (p < .05). 3. None of the bowel dysfunction characteristics were significantly related to the satisfaction of life items, but non-parametric analyses revealed that 2 of the ICI items were associated with satisfaction with free time & family life. |
| Rosito et al (2002)35 Pre-post intervention |
Objective: Evaluate the effects of colostomy on the QoL in patients with SCI. Population: 27 patients (26 men) with SCI, mean age of 62.9 (range 44–79 yrs), YPI 25.8 (range 8–48 yrs), mean time since stoma formation 8 (range 1.5–28 yrs), mean time with severe bowel dysfunction 5.5 (range 0.5–18 yr). NBD Assessment: Presence of colostomy. QoL Outcome Measures: Nonstandardized study specific questionnaire. Similar to Dijker's typical QoL measure of ADL. |
1. Colostomy improved (p ≤ .0001) total QoL. 2. Significant improvements after colostomy observed in physical health, self-efficacy, psychosocial status, & recreation/leisure but not in body image. 3. 85% of patients reported an ↑ in total QoL after colostomy; 70% of patients were satisfied with their personal lives before colostomy compared to 89% of patients after colostomy. 4. 67% of patients felt more independent after colostomy compared to 30% of patients that felt the same level of independence. |
| Safadi et al (2003)36 Retrospective chart review & cross-sectional survey |
Objective: Evaluate the long-term outcomes of colostomies & ileostomies post SCI. Population: 45 patients (44 men) with SCI, mean age 55.9 yrs, mean time from SCI to stoma 20.3 yrs. NBD Assessment: Presence of stoma. QoL Outcome Measures: Nonstandardized study specific questionnaire. |
1. In the right-sided colostomy group (n=20), QoL & health status scores improved (p < .05). 2. In the left-sided colostomy group (n=20), QoL & health status scores improved (p < .05). 3. In the ileostomy group (n=7), QoL & health status scores improved (p < .05). |
| Teichman et al (2003)79 Retrospective review |
Objective: To determine the long-term outcomes from the Malone antegrade continence enema (ACE) procedure in adult neurogenic patients. Population: 6 patients (mean age = 35 yrs), mean follow-up of 4.5 yrs. NBD Assessment: Pre-ACE & post-ACE toileting times, bowel continence status, & complications. QoL Outcome Measures: Nonstandardized questionnaire. |
1. Five patients (83%) were satisfied with their outcome & rated their QoL higher after the ACE procedure compared with pre-ACE. |
| Westgren & Levi (1998)54 Cross-sectional survey |
Objective: Determine associations between major outcome variables after SCI & QoL. Population: 320 persons (261 men) with SCI, mean age 42 (17–78 yr), YPI ≤4 yrs & ≥4 yrs. NBD Assessment: Medical records via clinical database. QoL Outcome Measures: SF-36. |
1. Bowel dysfunction was associated with ↓ QoL. 2. Bowel dysfunction yielded a medium effect sizes in the general physical functioning (p = .001), bodily pain (p = .003), general health (p = .001), vitality (p = .001), social function (p = .004), & mental health (p = .001) subscales. |
| Worsøe et al (2008)42 Retrospective chart review & cross-sectional survey |
Objective: Evaluate the long-term outcomes of ACE & ACE + colostomy in patients with SCI. Population: 80 patients (12 men) with SCI, mean age 51 yrs at time of stoma, mean follow-up time was 75 mos (range, 3–183). NBD Assessment: Continued ACE or ACE+colostomy at follow-up; Wexner score. QoL Outcome Measures: Nonstandardized study-specific questionnaire. |
1. 34 of 43 patients still using ACE were satisfied or very satisfied with the result, 8 patients were neither satisfied nor dissatisfied, & none were dissatisfied or very dissatisfied. One person did not provide a response. 2. On an arbitrary scale (0–100) mean values for bowel function before & after were 12 & 81 respectively (p < .01). For social function, the corresponding values were 30 & 81 (p < .01) & for QoL they were 28 & 81 (p < .01). |
| Tulsky et al (2015)57 Mixed-methods design |
Objective: To describe the development & psychometric properties of the SCI-QoL Bladder Management Difficulties & Bowel Management Difficulties item banks & Bladder Complications scale. Population: 757 adults with traumatic SCI of traumatic etiology, 18 yrs of age & older. NBD Assessment: N/A QoL Outcome Measures: In development. |
1. The SCI-QoL Bladder Management Difficulties & Bowel Management Difficulties item banks are psychometrically robust & are available as computer adaptive tests or short forms. |
Note: Studies are listed in alphabetical order according to the last name of the first author. ACE = antegrade colonic enema; AD = autonomic dysreflexia; ADL = activities of daily living; AIS = American Spinal Injury Association Impairment Scale; CHART = Criag Handicap and Assessment Reporting Technique; CCCSS = Cleveland Clinic Constipation Scoring System; DRS = digital rectal stimulation; ECC = enema continence catheter; FIM = Functional Independence Measure; GI = gastrointestinal; HADS = Hospital Anxiety & Depression Scale; HrQoL = health-related quality of life; HUI = Health Utilities Index; ICI = impediments to community integration; MBI = Modified Barthel Index; mos = months; NBD = neurogenic bowel dysfunction; N/A = not available; QLI = Quality of Life Index; QoL = quality of life; RSS = Reciprocal Support Scale; SCI = spinal cord injury(ies); SCS = Secondary Condition Scale; SF-12 = Short-Form 12; SF-36 = Short-Form 36; SWLS = Satisfaction with Life Scale; YPI = years post injury; yr(s) = years.
Table 1.
Identified studies (CONT.)
|
DESIGN Author (year) Research design |
METHODS (Objective, Population, Bowel Dysfunction Assessment, QoL Outcome Measures) |
QoL RESULTS |
|---|---|---|
| Adriaansen et al (2015)55 Cross-sectional multicenter study |
Objective: Describe bowel management & its outcomes in individuals living with an SCI for at least 10 yrs. Population: Individuals (N=258; age range, 28–65 yrs) who acquired their SCI between 18 & 35 yrs of age, who were at least 10 yr post-SCI, & who used a wheelchair for their daily mobility. NBD Assessment: International SCI Bowel Function Basic Data Set. QoL Outcome Measures: NBD score, a simple rating scale. |
1. Severe NBD was present in 36% of all participants & in 40% of those using a conservative method. However, only 14% were (very) dissatisfied with their current bowel management. 2. Dissatisfaction with bowel management was significantly associated with constipation & severe NBD. 3. With increasing time since injury, there was a nonsignificant trend observed toward a decline in dissatisfaction with bowel management & a significant decline in severe NBD. |
| Anson et al (1993)44 Cross-sectional & longitudinal survey |
Objective: Explore relationships among social support, adjustment, & secondary complications in persons with SCI. Population: 125 persons with SCI, 18 yrs + YPI > 1 yr. NBD Assessment: SCI QLI QoL Outcome Measures: SCI QLI; RSS scale. |
4. Social adjustment was associated with the number of diarrhea events. 5. Getting advice was negatively (r = −.029) associated with number of diarrhea events (p < .05). 6. No differences in diarrhea or constipation between high- & low-level support groups. |
| Branagan et al (2003)43 Cross-sectional survey |
Objective: Evaluate the effect of intestinal stoma formation in SCI patients. Population: 32 (27 men) patients with SCI (tetraplegia, paraplegia), mean age at onset 28.9 (range, 6–62 yrs), mean time of injury to stoma formation 17.1 mos (0–36.25). NBD Assessment: Presence of stoma QoL Outcome Measures: Nonstandardized study-specific questionnaire. |
1 18 patients reported that a stoma gave them ↑ independence, 12 reported no difference, & 1 felt his independence ↓ despite a significant ↓ time spent in bowel care. 2. QoL after stoma formation was described as much better by 25 patients, as better by 5, & QoL as worse by 1. |
| Christensen et al (2000)31 Cross-sectional survey |
Objective: Evaluate an ECC & MACE in patients with SCI. Population: 21 patients (10 men) with SCI offered ECC, mean age 39.9 (range, 7±72 yrs). 8 patients with SCI (3 men) + MACE, mean age 32.8 (range, 15–66 yrs). NBD Assessment: Single capsule with 24 or 10 radiopaque markers followed by abdominal X-ray; bowel management techniques. QoL Outcome Measures: Nonstandardized study-specific questionnaire. |
1. Before treatment with the ECC, 7 out of 11 patients available for follow-up felt that colorectal dysfunction imposed a major restriction on their QoL & social activities. 2. Before treatment with the ECC, 2 patients reported some restrictions, 1 reported a minor restriction, & 1 failed to answer the question. 3. At follow-up, 2 patients reported that colorectal dysfunction caused only some or little restriction & 3 patients reported no restriction. 4. At follow-up, 2 felt some restriction, 6 reported a minor restriction, & 6 reported no restriction. 5. Before MACE, 3 out of 5 patients were available at follow-up. |
| Christensen et al (2006)29 Prospective, randomized controlled multicenter trial |
Objective: Compare outcomes of transanal irrigation vs conservative bowel management in patients with SCI. Population: 87 patients (18 men) with SCI, median age 31.6 ± 13.3 yrs. NBD Assessment: St. Mark's Fecal Incontinence; CCCSS; Modified American Society of Colorectal Surgeon fecal incontinence scores. QoL Outcome Measures: NBD score |
1. Compared with conservative bowel management, transanal irrigation improves constipation, fecal incontinence, & symptom-related QoL. |
| Christensen et al (2008)28 Prospective, randomizedcontrolled multicenter trial |
Objective: Compare the symptoms of NBD in patients with SCI at baseline & after 10 weeks of treatment with transanal irrigation & identify possible factors that could predict treatment outcome. Population: 62 patients (45 men) with SCI (supraconal conal/cauda equina, complete, incomplete), mean age 47.5 ±15.5. NBD Assessment: Transanal irrigation, CCCSS; St. Mark's Fecal Incontinence. QoL Outcome Measures: NBD score |
1. Scores on the NBD improved from baseline to termination (p < .0001). 2. Regression analyses revealed that there was a reduction in the impact of bowel dysfunction on QoL but depended significantly on complete injury, being male, & ability to walk & varied significantly between study centres. |
| Coggrave et al (2009)45 Cross-sectional survey |
Objective: Describe bowel management in community dwelling persons with SCI & explore associations between age, injury, dependency problems, interventions, & satisfaction. Population: 1,334 persons (73.4% men) with SCI, median age 52 (19–91 yrs), median YPI 18 (1–65 yrs). NBD Assessment: Self-report (survey). QoL Outcome Measures: Nonstandardized study-specific questionnaire. |
1. Bowel dysfunction impacted on life activities to varying degrees & impact of bowel dysfunction was rated as significantly ↑ (p .001) than other aspects of SCI. 2. 20% of respondents were dissatisfied or very dissatisfied with bowel management & low satisfaction was associated with more frequent incontinence (p < .001), more problems (p < .001), longer duration of care (p< .001), more management (p = .008), & more interventions used (p < .001). |
| Coggrave et al (2013)15 Multicentre, retrospective self-report postal survey |
Objective: Characterize SCI individuals with a stoma, their stoma management & outcomes, identify sources of information & support for decision making & explore the impact of a stoma on life satisfaction. Population: 92 individuals, mean age 56 yrs, mean duration of injury 26 yrs, 91% with colostomy, 9% ileostomy. NBD Assessment: Self-report (survey). QoL Outcome Measures: Nonstandardized study-specific questionnaire (accompanied by TSCS, SWLS, & HADS) & 3-item nonstandardized questionnaire. |
1. Satisfaction with stoma was high; provision of sufficient information preoperatively was important, those with ileostomy were more dependent & less satisfied. 2. Life satisfaction & physical self-concept were both lower in this sample than in previously reported samples of SCI individuals without reported bowel difficulties or stoma. |
| Craven et al (2012)46 Cross-sectional survey |
Objective: Describe the relationships between secondary health conditions & health preference post SCI. Population: 357 persons (218 men) with SCI (AIS A-D), mean age 54.0 (range, 24–89), mean YPI 19.3 (range, 2–65). NBD Assessment: Bowel dysfunction item from the SCS. QoL Outcome Measures: HUI-III. |
1. Persons in no/mild bowel dysfunction group had ↑ (p < .0001) HUI-III scores than those in the moderate/severe bowel dysfunction group. |
| Del Popolo et al (2008)37 Pre-post intervention |
Objective: Evaluate the effects of Peristeen Anal Irrigation on NBD & QoL. Population: 36 patients (18 men) with SCI, median age 31.6 ± 13.3 yrs. NBD Assessment: Function, duration of the evacuation disorder, method of defecation, dietary supplements, the need for assistance for evacuation & the predominant intestinal symptom during/after defecation, NBD. QoL Outcome Measures: Nonstandardized study-specific questionnaire. |
1. Patient's opinions of their QoL score & degree of satisfaction ↑ from pre- to post-intervention (p = .001). 2. A high percentage of patients reported a change in their level of dependency after the treatment period. |
| Faaborg et al (2008)56 Longitudinal |
Objective: Describe long-term colorectal function in SCI patients. Population: 72 patients (48 men) with SCI, mean age 38.0 ± 11.9 yrs, YPI 37.5 ± 45.2 mos. NBD Assessment: Self-reported constipation, obstructed defecation, & fecal incontinence (survey). QoL Outcome Measures: Non-standardized study specific questionnaire; NBD score. |
1. The impact of colorectal dysfunction causing some or major restrictions on QoL or social activities ↑ from 25% to 38% from 1996 to 2006 (p < .005). 2. The impact of constipation influencing QoL ↑ from 15% to 23% from 1996 to 2006 (p < .15). |
| Glickman & Kamm (1996)4 Cross-sectional survey |
Objective: Determine the prevalence, nature, & effects – both physical & psychological – of SCI on bowel function. Population: 115 outpatients (77% men) with SCI, median age 38 (18–75 yrs), median YPI 62 (9–491 mos). NBD Assessment: Self-report (survey). QoL Outcome Measures: HADS; non-standardized questionnaire. |
1. Bowel dysfunction was a source of psychological distress in 54% of patients & was associated with time required for bowel management (p = .005) & frequency of incontinence (p = .001). 2. HADS scores correlated significantly with time taken for bowel management. 3. Bowel management problems were rated above urinary problems & not far below loss of mobility, impaired sexual function, & dependence. |
| Han et al (1998)47 Cross-sectional survey |
Objective: Investigate the characteristics of chronic GI problems & bowel dysfunction in patients with SCI. Population: 72 patients (48 men) with SCI, mean age 38.0 ± 11.9 yrs, YPI 37.5 ± 45.2 mos. NBD Assessment: Self-report (survey). QoL Outcome Measures: MBI Score. |
1. Bowel dysfunction was unrelated to age, duration, & neurological level of SCI, ASIA score, or level of activity. 2. Post-SCI GI problems were mainly bowel problems such as defecation difficulty (40.3%) & this affected ADL. |
| Hicken et al (2001)39 Case-control |
Objective: Examined the QoL among individuals with SCI requiring assistance for bowel & bladder management compared to those with independent control of their bladders & bowels. Population: 53 matched pairs (49% men): (1) bladder/bowel dependent individuals & (2) bladder/bowel independent individuals, mean age 37.02 yrs, YPI divided into 4 groups (1, 2–5, 6–15, >16 yrs). Groups matched on age, sex, education, race, & lesion level. NBD Assessment: FIM. QoL Outcome Measures: CHART; SWLS; SF-12. |
1. The bladder/bowel-dependent individuals reported ↓ life satisfaction & greater overall handicap (p < .001). In particular, persons who were bladder dependent had lower CHART subscale scores than bladder independent group on the following: physical independence (p < .001), mobility (p < .001), & occupational functioning (p < .05). 2. The bladder/bowel independent group initiated more social contact with strangers compared to bladder/bowel-dependent individuals (p = .056). 3. Although there were no group differences concerning social integration, the bladder/bowel-dependent group may have more difficulties initiating new social relationships. |
| Kachourbos & Creasey (2000)32 Post-intervention cross-sectional survey |
Objective: Assess recollections of health & QoL preoperatively in relation to bladder & bowel care & rate changes in QoL post-implant of an implantable stimulator. Population: 16 persons with SCI, 6 mos post surgery. NBD Assessment: Presence of implantable stimulator. QoL Outcome Measures: Non-standardized study specific questionnaire. |
1. Bowel program times were reduced from a mean of 5.4 hr per week preoperatively to 2.0 hr per week postoperatively. 2. Respondents reported a greater sense of independence, ↑ socialization, greater control over their lives, improved interpersonal relationships, improved self-image, ↓ feelings of depression, & an overall improvement in QoL. |
| Kelly et al (1999)30 Retrospective chart review & cross-sectional survey |
Objective: Evaluate the long-term outcomes of intestinal stomas post-SCI. Population: 14 patients (16 men) with SCI, mean age 54.8 yrs at time of stoma, mean time from SCI to stoma 15 yrs. NBD Assessment: Presence of stoma. QoL Outcome Measures: Nonstandardized study specific questionnaire. Similar to Dijker's typical QoL measure of ADL. |
1. Ten patients reported that colostomy was beneficial to their QoL. One person whose QoL remained unchanged post colostomy reported worse QoL at 10-yr follow-up. |
| Kim (2012)48 Cross-sectional survey |
Objective: Describe defecation stimulation methods & their outcomes & investigate the impact of bowel dysfunction on QoL in SCI. Population: 388 persons with SCI (295 men), mean age 44.5±10.8 yrs, mean YPI 14.2±9.5 yrs. NBD Assessment: Bowel stimulation method, frequency of bowel movements, defecation time, symptoms of AD, frequency of fecal incontinence, & flatus. QoL Outcome Measures: Nonstandardized study-specific questionnaire. |
1. Frequency of fecal incontinence had the greatest effects on QoL. 2. When patients had fecal incontinence every day, they had 67.4 times greater chance to obtain severely lowered general QoL. 3. Time taken in defecation >60 min, presence of perianal skin problem, & flatus incontinence also significantly influenced QoL. 4. QoL deterioration differs between each stimulation user. Decline in general QoL was greater in large-volume enemas users than in DRS users. 5. Social QoL deterioration was much more profound in large-volume enemas users than in DRS or finger evacuations users. 6. QoL at home was lower in patients using large-volume enemas than in those using other methods. 7. Mini-enema users had worse QoL at home than digital rectal stim users |
| Kirk et al (1997)5 Cross-sectional survey |
Objective: Describe impact of NBD on life activities. Population: 171 adults (128 men) with SCI, mean age 39.5 ± 14.5 yrs, mean YPI 8.9 ± 8.9. NBD Assessment: Self-report (survey). QoL Outcome Measures: Nonstandardized study-specific questionnaire (Bowel Program Outcome Questionnaire). |
1. 61% indicated NBD interfered with their life. 2. 47 of 105 respondents described a loss of freedom to go places, missing work, school or social events, or having to plan their lives around their bowels. |
| Krogh et al (1997)50 Cross-sectional survey |
Objective: Describe the frequency & severity of colorectal problems among patients with spinal cord lesions & determine whether these problems are associated with age, gender, time since lesion, level & severity of lesion. Population: 424 persons with SCI (300 men), mean age 41 (range 8–88 yrs), YPI 41 (range 0–59 yrs). NBD Assessment: Self-report (survey). QoL Outcome Measures: Nonstandardized study-specific questionnaire. |
1. 39% reported colorectal dysfunction caused some/major restrictions on social activities or QoL. 2. 29% reported disturbed defecation caused some/major restriction on social activities & 32% reported it caused some/major restriction on QoL. 3. 19% reported fecal incontinence caused some/major restriction on social activities & 20% reported it caused some/major restriction on QoL. 4. 30% reported bowel dysfunction was ↑ than bladder or sexual dysfunction. |
| Krogh et al (2006)49 Cross-sectional survey |
Objective: Develop & validate a symptom-based score for the NBD score. Population: 424 persons (72% men) with SCI, mean age 41 (8–88 yrs), mean YPI 14 (0–88 yrs). NBD Assessment: NBD score. QoL Outcome Measures: NBD score. |
1. Several items on the NBD found the impact on QoL ↑ with the severity of symptoms. Frequency of bowel movements was associated with QoL (p < .0001), as was frequency of fecal incontinence. 2. Difference in NBD scores among patients reporting no, little, some, or major impacts on QoL were significant (p < .001). 3. There may be an association between self-reported QoL & restriction of social activities due to bowel dysfunction. |
| Liu et al (2009)51 Cross-sectional survey |
Objective: Assess the relationship between the severity of NBD & HrQoL in persons with various degrees of SCI. Population: 128 (95 men) respondents with SCI, 36 with tetraplegia, 58 with paraplegia, 34 with paresis, mean age 48.3 (range 13–84 yrs), YPI divided into 4 groups (1–2 yrs, 3–5 yrs, 6–10 yrs, & over 10 yrs). NBD Assessment: NBD score. QoL Outcome Measures: SF-36; NBD score. |
1. Persons with very minor NBD had the ↑ scores on the SF-36 in contrast to persons with severe NBD, who had the ↓scores. 2. Significant differences were found on the SF-36 physical functioning (p < .001) & the physical component summary (p < .001) subscales. 3. Participants with worse NBD were likely to have ↓physical QoL (p < .001). |
| Lombardi (2010)33 Retrospective non-blinded design without controls. |
Objective: Evaluate the efficacy & safety of sacral neuromodulation in incomplete SCI affected by chronic NBD. Population: 23 patients with SCI (13 men), mean age 36±9 yrs. NBD Assessment: Wexner Score; episodes of fecal incontinence, no. of evacuations/week. QoL Outcome Measures: SF-36. |
1. Patients in both groups (constipation & fecal incontienence) had significant ↓ (p < .05) in Wexner scores. 2. QoL in both groups consistently showed statistical improvement (p < .05). |
| Lombardi et al (2011)34 Retrospective cross-sectional survey |
Objective: Assess the concomitant clinical improvement in incomplete SCI with NBD using sacral neuromodulation. Population: 75 patients with incomplete SCI. NBD Assessment: Incontinence & constipation. QoL Outcome Measures: SF-36. |
1. Bladder function & incontinence improved. 2. In the general & mental health domains of the SF-36, all patients improved their scores by at least 20% compared with baseline after sacral neuromodulation. |
| Luther et al (2005)40 Case-control |
Objective: Compare QoL for people with NBD & SCI using either a standard care program or colostomy. Population: 74 veterans (73 men) with SCI + colostomy, 296 SCI controls without colostomy, age range < 20–89, YPI within past 20 yr. NBD Assessment: Presence of colostomy. QoL Outcome Measures: IBDQ. |
1. No significant differences were detected on IBDQ between persons with SCI + colostomy & those with SCI only. |
| Lynch et al (2000)10 Controlled, descriptive & comparative questionnaire study |
Objective: Describe the bowel function of SCI patients & compare it to a general community control group. Population: 467 SCI patients & 467 control subjects were age & gender matched. Mean age for the SCI patients 43.5 (range, 15–89 yrs), mean YPI 14 (range, 0.7–42.1 yrs). Mean age for the controls 45.3 (range, 17–78 yr). NBD Assessment: General bowel function, incidence of incontinence, & defecation methods. QoL Outcome Measures: Nonstandardized questionnaire. |
1. Incontinence affected the QoL for 62% SCI patients compared to 8% of the controls. 2. Incontinence did not affect the majority of the controls (92.3%) in terms of everyday activities compared to 43.9% of SCI patients (p < .0001). |
| Noonan et al (2008)52 Cross-sectional survey |
Objective: Determine the effect of associated SCI conditions on health status & QoL. Population: 70 persons (57 men) with central cord syndrome, mean age at injury 45±18 yrs (range, 13–91), mean age at follow-up 51 ±18 yrs (range, 19–95). NBD Assessment: Self-report (survey). QoL Outcome Measures: SF-36; numeric QoL rating. |
1. Bowel, bladder & sexual dysfunction on the physical component score of the SF-36 were significant, but the effect ↓ when controlling for personal & confounding factors. 2. Bowel, bladder & sexual dysfunction were not related to the mental component scores of the SF-36. 3. Problems with bowel, bladder, & sexual dysfunction were significantly (p< .01) associated with QoL when personal & confounding factors were NOT controlled for. |
| Pardee et al (2012)8 Exploratory, descriptive correlational design |
Objective: Investigate the association between characteristics of individuals with SCI & neurogenic bowel & their perceived QoL. Population: 241 surveys; from adults over age 18, diagnosed with SCI & neurogenic bowel more than 2 yrs post injury, AIS of A, B, C, or D & residing in the community. NBD Assessment: Survey of neurogenic bowel characteristics. QoL Outcome Measures: QoL survey. |
1. Regardless of the bowel management program 54% (n = 127) were satisfied with current methods. Although time reported to complete bowel programs ranged from 1 to 120 min, there was no difference in rating of satisfaction with time. 2. There was a statistically significant difference between those satisfied & dissatisfied with current bowel management & QoL; those satisfied demonstrated a higher QoL on 3 subscales, work function (p = .021), bowel problems (p < .001), & social function (p < .001). Those dissatisfied with their bowel program perceived a lower QoL & indicated problem of time (p = .001), pain or discomfort (p = .033), & poor results (p < .001). |
| Randell et al (2001)41 Prospective controlled comparative analysis |
Objective: Determine whether a colostomy changes QoL in patients with SCI. Population: 26 (15 men) patients with SCI (tetraplegia, paraplegia) + colostomy, age range 22–87, range of injury to stoma formation 7 mos – 20 yrs. 26 SCI controls (age, gender, injury, & YPI matched) without colostomy. NBD Assessment: Presence of colostomy. QoL Outcome Measures: Burwood QoL Questionnaire. |
1. No significant differences were detected on QoL between persons with SCI + colostomy & those with SCI only. |
| Roach et al (2000)53 Cross-sectional survey |
Objective: Examine the relationship between bowel dysfunction, impediment to community integration & QoL in persons with SCI. Population: 103 SCI consumers (76.7% men), mean age 39 yrs, YPI 14 yr. NBD Assessment: Self-report (survey). QoL Outcome Measures: Andrews & Withey (1976) Life Satisfaction Survey; nonstandardized study specific questionnaire on community integration (ICI). |
1. Significant negative relationship between subjective severity & 3 ICI measures; the higher the perceived severity of bowel dysfunction, the more it affected (1) personal relationships (p < .01); (2) feelings about themselves (p < .01); (3) their home environment (p < .05). 2. The number of days each month a person stayed at home because of lack of bowel control was associated with all 3 ICI scales (p < .01). The ↑ bowel accidents per month, the ↑ negative a respondent felt about him/herself (p < .05). 3. None of the bowel dysfunction characteristics were significantly related to the satisfaction of life items, but non-parametric analyses revealed that 2 of the ICI items were associated with satisfaction with free time & family life. |
| Rosito et al (2002)35 Pre-post intervention |
Objective: Evaluate the effects of colostomy on the QoL in patients with SCI. Population: 27 patients (26 men) with SCI, mean age of 62.9 (range 44–79 yrs), YPI 25.8 (range 8–48 yrs), mean time since stoma formation 8 (range 1.5–28 yrs), mean time with severe bowel dysfunction 5.5 (range 0.5–18 yr). NBD Assessment: Presence of colostomy. QoL Outcome Measures: Nonstandardized study specific questionnaire. Similar to Dijker's typical QoL measure of ADL. |
1. Colostomy improved (p ≤ .0001) total QoL. 2. Significant improvements after colostomy observed in physical health, self-efficacy, psychosocial status, & recreation/leisure but not in body image. 3. 85% of patients reported an ↑ in total QoL after colostomy; 70% of patients were satisfied with their personal lives before colostomy compared to 89% of patients after colostomy. 4. 67% of patients felt more independent after colostomy compared to 30% of patients that felt the same level of independence. |
| Safadi et al (2003)36 Retrospective chart review & cross-sectional survey |
Objective: Evaluate the long-term outcomes of colostomies & ileostomies post SCI. Population: 45 patients (44 men) with SCI, mean age 55.9 yrs, mean time from SCI to stoma 20.3 yrs. NBD Assessment: Presence of stoma. QoL Outcome Measures: Nonstandardized study specific questionnaire. |
1. In the right-sided colostomy group (n=20), QoL & health status scores improved (p < .05). 2. In the left-sided colostomy group (n=20), QoL & health status scores improved (p < .05). 3. In the ileostomy group (n=7), QoL & health status scores improved (p < .05). |
| Teichman et al (2003)79 Retrospective review |
Objective: To determine the long-term outcomes from the Malone antegrade continence enema (ACE) procedure in adult neurogenic patients. Population: 6 patients (mean age = 35 yrs), mean follow-up of 4.5 yrs. NBD Assessment: Pre-ACE & post-ACE toileting times, bowel continence status, & complications. QoL Outcome Measures: Nonstandardized questionnaire. |
1. Five patients (83%) were satisfied with their outcome & rated their QoL higher after the ACE procedure compared with pre-ACE. |
| Westgren & Levi (1998)54 Cross-sectional survey |
Objective: Determine associations between major outcome variables after SCI & QoL. Population: 320 persons (261 men) with SCI, mean age 42 (17–78 yr), YPI ≤4 yrs & ≥4 yrs. NBD Assessment: Medical records via clinical database. QoL Outcome Measures: SF-36. |
1. Bowel dysfunction was associated with ↓ QoL. 2. Bowel dysfunction yielded a medium effect sizes in the general physical functioning (p = .001), bodily pain (p = .003), general health (p = .001), vitality (p = .001), social function (p = .004), & mental health (p = .001) subscales. |
| Worsøe et al (2008)42 Retrospective chart review & cross-sectional survey |
Objective: Evaluate the long-term outcomes of ACE & ACE + colostomy in patients with SCI. Population: 80 patients (12 men) with SCI, mean age 51 yrs at time of stoma, mean follow-up time was 75 mos (range, 3–183). NBD Assessment: Continued ACE or ACE+colostomy at follow-up; Wexner score. QoL Outcome Measures: Nonstandardized study-specific questionnaire. |
1. 34 of 43 patients still using ACE were satisfied or very satisfied with the result, 8 patients were neither satisfied nor dissatisfied, & none were dissatisfied or very dissatisfied. One person did not provide a response. 2. On an arbitrary scale (0–100) mean values for bowel function before & after were 12 & 81 respectively (p < .01). For social function, the corresponding values were 30 & 81 (p < .01) & for QoL they were 28 & 81 (p < .01). |
| Tulsky et al (2015)57 Mixed-methods design |
Objective: To describe the development & psychometric properties of the SCI-QoL Bladder Management Difficulties & Bowel Management Difficulties item banks & Bladder Complications scale. Population: 757 adults with traumatic SCI of traumatic etiology, 18 yrs of age & older. NBD Assessment: N/A QoL Outcome Measures: In development. |
1. The SCI-QoL Bladder Management Difficulties & Bowel Management Difficulties item banks are psychometrically robust & are available as computer adaptive tests or short forms. |
Note: Studies are listed in alphabetical order according to the last name of the first author. ACE = antegrade colonic enema; AD = autonomic dysreflexia; ADL = activities of daily living; AIS = American Spinal Injury Association Impairment Scale; CHART = Criag Handicap and Assessment Reporting Technique; CCCSS = Cleveland Clinic Constipation Scoring System; DRS = digital rectal stimulation; ECC = enema continence catheter; FIM = Functional Independence Measure; GI = gastrointestinal; HADS = Hospital Anxiety & Depression Scale; HrQoL = health-related quality of life; HUI = Health Utilities Index; ICI = impediments to community integration; MBI = Modified Barthel Index; mos = months; NBD = neurogenic bowel dysfunction; N/A = not available; QLI = Quality of Life Index; QoL = quality of life; RSS = Reciprocal Support Scale; SCI = spinal cord injury(ies); SCS = Secondary Condition Scale; SF-12 = Short-Form 12; SF-36 = Short-Form 36; SWLS = Satisfaction with Life Scale; YPI = years post injury; yr(s) = years.
Similar to previous studies that classified QoL tools used to assess the influence of different SCI-related secondary conditions,23–25 Dijkers' QoL framework was used to categorize outcome measures as being either objective or subjective and was used to provide a deeper understanding of the QoL constructs underlying each measure (see Figure 1).19,22 Briefly described, the model categorizes measures into three categories: QoL as “utility,” “achievements,” and “subjective well-being.”
Figure 1.
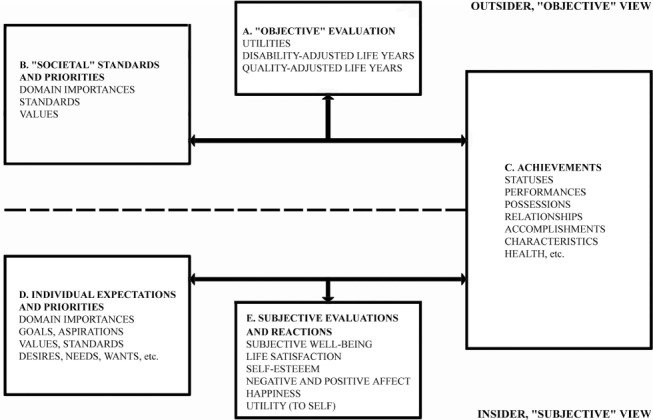
Dijkers' theoretical framework for the classification of quality of life outcome tools. Adapted from Dijkers MP. Individualization in quality of life measurement: Instruments and approaches. Arch Phys Med Rehabil. 2003;84(4 suppl 2): S3-14. Copyright © 2003, with permission from Elsevier (Elsevier License Number: 4106821509985).
QoL as utility reflects the desirability and preferences of life valuations (box A, Figure 1) and is obtained by judging one's tradition, achievements, and status in terms of societal norms and standards (box B). Hence, QoL as utility is expressed as an outsider's viewpoint (objective) and provides a metric framing QoL, typically used to support health economic analyses.22 Similarly, QoL as achievements is an objective perspective that takes into account the individual's possessions, accomplishments, status, and so on (box C), while excluding the subjective reactions to these qualities.22 Therefore, QoL is predicted by what a person has obtained in his or her life (ie, good health, marriage, etc; box C), which society generally views as indicative of what one needs to have a “good life” (box B). QoL as subjective well-being recognizes that humans develop individual priorities/wants (box E), which may range in relative importance (box D). When these needs/wants are compared to reality (box C), the resulting reactions by respondents might range from positive to negative and are likely to affect morale, life satisfaction, and other expectations (box E).22 QoL as “subjective well-being” can therefore be explained as “feelings of well-being as influenced by the good things in life.”27(p1)
This methodology was used to classify QoL outcomes specific to NBD as objective or subjective, and the relevant constructs of QoL that comprised each tool were identified (ie, A, B, C, D, E) (Figure 1). Each QoL measure was mapped to one or more QoL constructs (Figure 1) by a first reviewer and verified by a second reviewer. The psychometric properties and sensitivity of each tool to capture the impact on QoL were also summarized (Table 2).
Table 2.
Summary of outcome measures
| Outcome toola | QoL construct | SCI psychometrics | Format/Scoring | Administrative burden | Sensitive to NBD impact | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| A | B | C | D | E | ||||||
| Craig Handicap Assessment & Reporting Technique (CHART) | O | X | Reliability & validityestablished for SCI (see Hall et al67 for details). | 32-item scale that assesses the degree of handicap experienced by persons with SCI across 6 domains: orientation, physical independence, mobility, occupational functioning, social integration, and economic self-sufficiency. | ~ 15 min | +Hicken et al (2001)39 | ||||
| Health Utilities Index-III (HUI-III) | O | X | X | X | Preliminary evidenceof validity in SCI (see Mittmann et al66 for details). | Evaluates 8 attributes (vision, hearing, speech, ambulation, dexterity, emotion, cognition, & pain) in respondents over the 4 weeks prior to the administration date. Each attribute is assigned to one of the 5 or 6 levels of ability/disability. Scores for each attribute are combined using a multiplicative utility function & reported as a single metric ranging from 0 (death) to 1 (perfect health). | ~3–10 min | +Craven et al (2012)46 | ||
| Medical Outcomes Study Short-Form (SF-36) | O | X | X | Reliability & validity established for SCI (see Hill et al58 for details). | 36 items covering 8 domains related to functioning & health. Scoring is norm-based, with a general population mean score of 50 and an SD of 10. ↑ scores indicate ↑ levels of health. | ~ 5–10 min | −Noonan et al (2008)52 + Lombardi et al (2010)33 +Lombardi et al (2011)34 +Liu et al (2009)51 +Westgren & Levi (1998)54 |
|||
| Medical Outcomes Study Short-Form (SF-12) | O | X | X | Construct validity established for SCI (see Andresen et al59 for details). | 12 items, derived from the physical and mental domains of the SF-36. | ~ 5 min | +Hicken et al (2001)39 | |||
| Modified Barthel Index (MBI) | O | X | X | Reliability & validity established for SCI (see Anderson et al60 for details). | 10-item scale where each activity is given 1 of 5 levels of dependency ranging from 0 (unable to perform task) to a maximum of 5, 10, or 15 (fully independent). | ~ 10 min | −Han et al (1998)47 | |||
| Burwood QoL Questionnaire | S | X | X | Preliminary face validity (see Randell et al41 for details). | 26 items covering 5 domains: systemic symptoms, and emotional, social, work, and bowel function | NR | +Lynch et al (2000)10 −Randell et al (2001)41 |
|||
| Hospital Anxiety & Depression Scale (HADS) | S | X | Reliability and validity established for SCI (see Woolrich et al69 for details). | Self-assessment mood scale developed for medical outpatients containing 14 questions graded on a 4-point Likert scale with subscales of anxiety and depression, with a sum score ranging from 0 to 21 for each and a cutoff value of >7 on either of the 2 subscales. | ~ 20 min | +Glickman & Kamm (1996)4 | ||||
| Impediments to Community Integration (ICI) Scale | S | X | X | Preliminary reliability established for SCI. Further evaluation needed (see Roach et al53 for details). | 16 statements reflecting different domains of a person's life derived from literature on QoL and through 3 SCI consumer focus group discussions. Respondents have to rate how much a specific activity was affected by their current bowel dysfunction on a scale of 1 to 10 with 1 meaning not at all and 10 meaning very much. | NR | +Roach et al (2000)53 | |||
| Inflammatory Bowel Disease Questionnaire (IBDQ) | S | X | X | Preliminary reliability established for SCI; further evaluation needed (see Luther et al40 for details). | Contains 32 questions evaluating general activities of daily living, intestinal function such as bowel habit and abdominal pain as well as social performance, personal interactions, and emotional status. Responses are graded on a 7-point Likert scale, from 7 (not a problem at all) to 1 (a very severe problem). | ~ 20 min | −Luther et al (2005)40 | |||
| Neurogenic bowel dysfunction (NBD) score | S | X | X | X | Reliability and validity established for SCI (see Krogh et al49,50 for details). | 10-item scale assessing background parameters, fecal incontinence, constipation, obstructed defecation, & impact on QoL. | ~ 5 min | +Christensen et al (2008)28 +Christensen et al (2006)29 +Liu et al (2009)51 +Krogh et al (2006)49 + Adriaansen et al (2015)55 |
||
| Reciprocal Social Support (RSS) Scale | S | X | X | Some evidence of reliability for SCI; further evaluation needed (see Krause et al68 for further details). | 8 questions rating types of support received from families, friends, & the community. Responses are ranked on a 7-point scale ranging from 1 (never) to 7 (always). ↑scores indicate ↑levels of support. | ~ 10–15 min | +Anson et al (1993)44 | |||
| Spinal cord injury – quality of life (SCI-QOL) bowel management difficulties | S | X | X | Reliability and validity established for SCI (see Tulsky et al57 for further details). | 26 items on bowel management difficulty. Complications experienced recently are rated on a scale ranging from 1(never/not at all) to 5 (always/very much). 1 item is reverse scored between 1 (always) & 5 (never). Items are summed then converted to a standardized T-metric score. Higher scores indicate higher degree of difficulty. Available as a computer adaptive tool or as a short form. | NR | + Tulsky et al (2015)57 | |||
| Survey of neurogenic bowel characteristics (SNBC) | S | X | X | Face and content validity (see Pardee et al8 for further details). | 9 demographic questions related to education, employment, living situation, & satisfaction with bowel management. A second section addresses questions specific to either a colostomy or a bowel program that may affect QoL. | NR | + Pardee et al (2012)8 | |||
Note: A = achievement; HrQoL = health-related quality of life; NR = not reported; SCI = spinal cord injury; SWB = subjective well-being; (+) = sensitive to bowel dysfunction impact; (−) = not sensitive to bowel dysfunction impact; ↑ = increase.
aO = objective; S = subjective.
Table 2.
Summary of outcome measures (CONT.)
| Outcome toola | QoL construct | SCI psychometrics | Format/Scoring | Administrative burden | Sensitive to NBD impact | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| A | B | C | D | E | ||||||
| Craig Handicap Assessment & Reporting Technique (CHART) | O | X | Reliability & validityestablished for SCI (see Hall et al67 for details). | 32-item scale that assesses the degree of handicap experienced by persons with SCI across 6 domains: orientation, physical independence, mobility, occupational functioning, social integration, and economic self-sufficiency. | ~ 15 min | +Hicken et al (2001)39 | ||||
| Health Utilities Index-III (HUI-III) | O | X | X | X | Preliminary evidenceof validity in SCI (see Mittmann et al66 for details). | Evaluates 8 attributes (vision, hearing, speech, ambulation, dexterity, emotion, cognition, & pain) in respondents over the 4 weeks prior to the administration date. Each attribute is assigned to one of the 5 or 6 levels of ability/disability. Scores for each attribute are combined using a multiplicative utility function & reported as a single metric ranging from 0 (death) to 1 (perfect health). | ~3–10 min | +Craven et al (2012)46 | ||
| Medical Outcomes Study Short-Form (SF-36) | O | X | X | Reliability & validity established for SCI (see Hill et al58 for details). | 36 items covering 8 domains related to functioning & health. Scoring is norm-based, with a general population mean score of 50 and an SD of 10. ↑ scores indicate ↑ levels of health. | ~ 5–10 min | −Noonan et al (2008)52 + Lombardi et al (2010)33 +Lombardi et al (2011)34 +Liu et al (2009)51 +Westgren & Levi (1998)54 |
|||
| Medical Outcomes Study Short-Form (SF-12) | O | X | X | Construct validity established for SCI (see Andresen et al59 for details). | 12 items, derived from the physical and mental domains of the SF-36. | ~ 5 min | +Hicken et al (2001)39 | |||
| Modified Barthel Index (MBI) | O | X | X | Reliability & validity established for SCI (see Anderson et al60 for details). | 10-item scale where each activity is given 1 of 5 levels of dependency ranging from 0 (unable to perform task) to a maximum of 5, 10, or 15 (fully independent). | ~ 10 min | −Han et al (1998)47 | |||
| Burwood QoL Questionnaire | S | X | X | Preliminary face validity (see Randell et al41 for details). | 26 items covering 5 domains: systemic symptoms, and emotional, social, work, and bowel function | NR | +Lynch et al (2000)10 −Randell et al (2001)41 |
|||
| Hospital Anxiety & Depression Scale (HADS) | S | X | Reliability and validity established for SCI (see Woolrich et al69 for details). | Self-assessment mood scale developed for medical outpatients containing 14 questions graded on a 4-point Likert scale with subscales of anxiety and depression, with a sum score ranging from 0 to 21 for each and a cutoff value of >7 on either of the 2 subscales. | ~ 20 min | +Glickman & Kamm (1996)4 | ||||
| Impediments to Community Integration (ICI) Scale | S | X | X | Preliminary reliability established for SCI. Further evaluation needed (see Roach et al53 for details). | 16 statements reflecting different domains of a person's life derived from literature on QoL and through 3 SCI consumer focus group discussions. Respondents have to rate how much a specific activity was affected by their current bowel dysfunction on a scale of 1 to 10 with 1 meaning not at all and 10 meaning very much. | NR | +Roach et al (2000)53 | |||
| Inflammatory Bowel Disease Questionnaire (IBDQ) | S | X | X | Preliminary reliability established for SCI; further evaluation needed (see Luther et al40 for details). | Contains 32 questions evaluating general activities of daily living, intestinal function such as bowel habit and abdominal pain as well as social performance, personal interactions, and emotional status. Responses are graded on a 7-point Likert scale, from 7 (not a problem at all) to 1 (a very severe problem). | ~ 20 min | −Luther et al (2005)40 | |||
| Neurogenic bowel dysfunction (NBD) score | S | X | X | X | Reliability and validity established for SCI (see Krogh et al49,50 for details). | 10-item scale assessing background parameters, fecal incontinence, constipation, obstructed defecation, & impact on QoL. | ~ 5 min | +Christensen et al (2008)28 +Christensen et al (2006)29 +Liu et al (2009)51 +Krogh et al (2006)49 + Adriaansen et al (2015)55 |
||
| Reciprocal Social Support (RSS) Scale | S | X | X | Some evidence of reliability for SCI; further evaluation needed (see Krause et al68 for further details). | 8 questions rating types of support received from families, friends, & the community. Responses are ranked on a 7-point scale ranging from 1 (never) to 7 (always). ↑scores indicate ↑levels of support. | ~ 10–15 min | +Anson et al (1993)44 | |||
| Spinal cord injury – quality of life (SCI-QOL) bowel management difficulties | S | X | X | Reliability and validity established for SCI (see Tulsky et al57 for further details). | 26 items on bowel management difficulty. Complications experienced recently are rated on a scale ranging from 1(never/not at all) to 5 (always/very much). 1 item is reverse scored between 1 (always) & 5 (never). Items are summed then converted to a standardized T-metric score. Higher scores indicate higher degree of difficulty. Available as a computer adaptive tool or as a short form. | NR | + Tulsky et al (2015)57 | |||
| Survey of neurogenic bowel characteristics (SNBC) | S | X | X | Face and content validity (see Pardee et al8 for further details). | 9 demographic questions related to education, employment, living situation, & satisfaction with bowel management. A second section addresses questions specific to either a colostomy or a bowel program that may affect QoL. | NR | + Pardee et al (2012)8 | |||
Note: A = achievement; HrQoL = health-related quality of life; NR = not reported; SCI = spinal cord injury; SWB = subjective well-being; (+) = sensitive to bowel dysfunction impact; (−) = not sensitive to bowel dysfunction impact; ↑ = increase.
aO = objective; S = subjective.
Results
Following duplicate removal and screening of titles and abstracts, 82 full-text articles were assessed for eligibility and 35 met the inclusion criteria. Figure 2 provides a flow diagram illustrating the search and selection of studies. The details of two randomized controlled trials,28,29 11 pre-post interventions studies,6,8,30–38 4 comparison studies,10,39–41 16 cross-sectional observational and comparative studies,4,5,42–55 1 longitudinal study,56 and 1 mixed-methods study57 are presented in Table 1.
Figure 2.
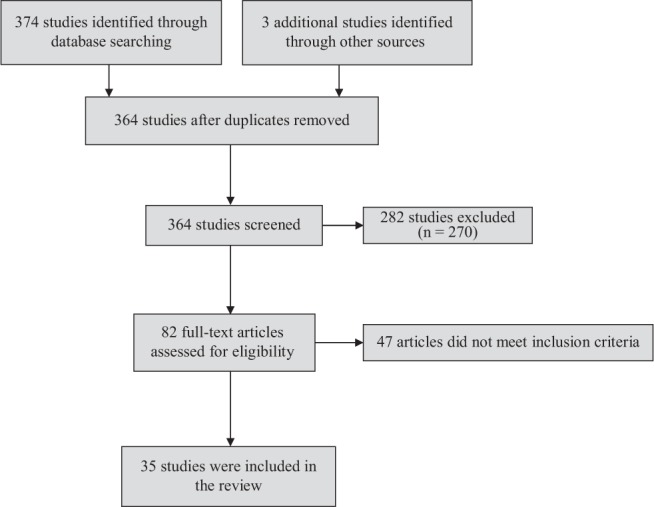
PRISMA flow diagram of studies reviewed and selected for inclusion.
A total of 13 QoL outcome tools were identified (5 objective, 8 subjective). Table 2 presents each QoL tool with details about the underlying QoL constructs,19,22 psychometric properties, format and scoring, administrative burden, and sensitivity of the tool to NBD.
Objective QoL outcomes specific to NBD
The Medical Outcomes Survey Short Form (SF-36) was the most commonly used objective measure of health-related QoL33,34,51,52,54 (used in 5 of 35 studies). The SF-12, a shortened version of the SF-36 measuring the same QoL constructs, was also used in one study.39 Both the SF-36 and the SF-12 provide a generic assessment of physical and mental health status, derived across eight domains of health and functioning (boxes B and C, Figure 1). Specific to individuals with SCI, the SF-36 has documented reliability and validity,58 and the SF-12 has construct validity.59 Although both the SF-36 and SF-12 were sensitive to changes in QoL that were related to NBD (Table 2), neither tool has items specific to SCI or NBD. As measured by the SF-36 or SF-12, studies identified in this review showed that NBD was associated with decreased health-related QoL,54,59 with more severe cases of NBD associated with lower QoL and more mild case of NBD associated with higher QoL.51 Improvements in bowel function after sacral neuromodulation were also associated with improved health-related QoL in two studies.33,34
The Modified Barthel Index (MBI), a measure of functional status, was used in one study.47 The MBI is an objective tool comprised of 10 items of activities of daily living that are scored for level of dependency on a scale ranging from 0 (unable to perform task) to 15 (fully independent) (boxes B and C, Figure 1). The MBI is not a measure of QoL per se but does assess key activities of daily living that have implications for QoL, and it might be a useful tool to help further validate other measures of QoL since it has been found to be a reliable tool for SCI,60 with a good internal consistency (alpha 0.88–0.90) and sufficient interrater agreement (intraclass correlation coefficient [ICC] = 0.77).61,62 The correlations between the MBI and the American Spinal Injury Association Impairment Scale (AIS) motor and sensory scales were moderate to high as expected, providing evidence of convergent validity.61 There has been limited evidence of construct validity for the bowel and bladder items in SCI.61 MBI scores have been documented to be responsive to environmental changes.61,62 However, bowel function was not associated with functional status as measured by the MBI.47
The Health Utility Index Mark III (HUI-III) was used in one study to ascribe the burden of various secondary health conditions, including NBD, following SCI.46 The HUI-III is a comprehensive system for describing the health status of individuals and for assigning a preference (or utility) score.63 A preference score is a societal representation of well-being, which is typically reported as a single metric anchored at 0 (death) with 1 (perfect health) at the end of the ranking, thus representing a preference for a health state.64 These health state morbidities are measured across a group of individuals and combined into a utility score, which can then be used as a quality metric for calculating the number of quality adjusted life-years gained in cost-utility analyses65 (boxes A, B, and C, Figure 1). Although Craven et al46 provided some evidence with regard to QoL as utility for NBD, only preliminary evidence of concurrent validity has been established to date.66 Individuals without NBD or with mild NBD reported higher HUI-III scores than those who had moderate or severe NBD, suggesting the HUI-III is sensitive to the influence of NBD on QoL.46 An important limitation of this study was that bowel dysfunction was assessed via self-report using the Secondary Conditions Scale, which asked participants if they had bowel problems and, if so, to rate its severity (mild, moderate, or severe). Further work on the sensitivity of the HUI-III to this secondary condition is required to determine if it is sensitive to other self-reported measures or objective assessments of bowel problems.
The Craig Handicap Assessment and Reporting Technique (CHART) was used in one study to assess the degree of handicap experienced by individuals with SCI due to NBD.39 The CHART is a 32-item scale assessing the degree of handicap experienced across six areas, including orientation, physical independence, mobility, occupational functioning, social integration, and economic self-sufficiency (boxes B and C, Figure 1). The CHART is reliable and valid for use in SCI52,67 and is sensitive to the impact of NBD on QoL. Individuals who were dependent on others for bowel management reported lower satisfaction and higher perceived handicap, specifically in the physical independence, mobility, and occupational functioning domains.39
Subjective QoL measures specific to NBD
The NBD score, the most commonly used subjective QoL tool in 5 of 35 studies,28,29,49,51,55 was developed to assess the influence of NBD on QoL in persons with SCI.49 Ten items related to symptoms of constipation and fecal incontinence and their impact on QoL are evaluated, with scores ranging from 0 (very minor bowel dysfunction) to 47 (very severe bowel dysfunction)49 (boxes C, D, and E, Figure 1). Although the questionnaire is primarily comprised of items that assess NBD symptoms from an objective standpoint, the development of this tool was based on subjective perceptions of the impact of NBD on QoL in people with SCI, and the scale has a subjective QoL item. The developers of the scale acknowledge that that their tool is vague with regard to which aspects of QoL are impacted but believe that it is likely social activities.49 Based on the tool development process, along with the inclusion of the single subjective QoL item, we have classified it as a subjective measure of QoL.
The reliability and validity of the NBD score have been established for SCI.49 The results of two experimental trials using the NBD score showed that transanal irrigation lead to improved bowel function and improved QoL (NBD score decreased by 4.5; p < .0001).28,29 More severe symptoms of constipation or fecal incontinence were associated with lower QoL in other cross-sectional studies.49,51,55
The Burwood QoL Questionnaire was developed as a study-specific measure to assess the QoL related to bowel function after SCI and was used in two studies.10,41 The questionnaire comprises 26 items, covering five domains of functioning, including systemic symptoms and emotional, social, work, and bowel function (boxes C and E, Figure 1).41 Only preliminary face validity has been established for use in SCI populations.4,10 According to the Burwood QoL Questionnaire, incontinence influenced QoL in 62% of individuals with SCI.10 However, when used to detect the impact of colostomy on QoL, there were no differences observed between those who received a colostomy and those who did not.41
The Survey of Neurogenic Bowel Characteristics (SNBC) contains questions about health-related (bowel program management) and non-health-related (demographic status) factors that may affect QoL (boxes C and E, Figure 1). This self-administered survey focuses on demographic aspects surrounding QoL after SCI. The SNBC seems to be sensitive to the influence of NBD on QOL, as satisfaction with bowel management was associated with higher QoL and dissatisfaction with bowel management was associated with lower QoL.8 Only face and content validity have been established for the SNBC to date.8
The SCI-QoL Bowel Management Difficulties assesses the impact of bowel management difficulties on QoL (box E, Figure 1).57 This tool evaluates how often 26 various bowel management difficulties are experienced on a scale ranging from 1 (never) to 5 (always). Reliability and validity assessment of the final item banks have been documented.57 Furthermore, the tool can be easily administered using computer adaptive testing or short forms. The sensitivity of the SCI-QoL Bowel Management Difficulties is unknown, as the tool has not yet been used outside of this validation study.57
The Impediments to Community Integration (ICI) Scale evaluates the impact of NBD on community participation after SCI (box E, Figure 1) through 16 statements that reflect three general areas of life (leisure activity, socializing, and feeling bad about oneself). Preliminary reliability has been established for SCI, but further evaluation is required.53 The findings of the study assessing bowel dysfunction in 103 persons with SCI suggest the ICI Scale is sensitive to the influence of NBD on QoL, as severity of bowel dysfunction significantly influenced personal relationships and feelings about oneself.53
The Inflammatory Bowel Disease Questionnaire (IBDQ) comprises 32 questions covering the activities of daily living, intestinal function, social performance, personal interactions, and emotional status (box E, Figure 1).40 Similar to the ICI, preliminary reliability has been established for the IBDQ in SCI, but the tool was not found to be sensitive to differences in bowel function between individuals with SCI who had a colostomy and those who did not.40
Related constructs used to assess the influence of NBD on QoL included social support (Reciprocal Social Support [RSS] Scale) and affect (Hospital Anxiety and Depression Scale). The RSS scale evaluates levels of reciprocal social support from families, friends, and the community in four areas (ie, social interaction, material assistance, emotional support, and non-paid personal assistance) (boxes C and E, Figure 1). Frequency of incontinence and material support given and received were shown to be significantly correlated in one study, but there is no evidence of the impact of bowel function and emotional support given or received.44 The RSS has acceptable internal consistency for use in SCI, but further validation is needed.68
The HADS was developed with a focus on the patient and their mood state to screen for anxiety (7 items) and depression (7 items) (box E, Figure 1). The frequency that each of the 14 items is experienced is rated on a 4-point scale from 0 (not at all) to 3 (very often). Although not a measure of QoL per se, it is arguable that the HADS taps into the construct of affect, which would qualify it as a QoL measure of subjective well-being. Psychometric properties of the HADS in SCI have been documented,69 and HADS scores were significantly correlated with time required for bowel management.4
Discussion
The purpose of this systematic review was to identify, classify, and summarize existing tools for assessing the influence of NBD on QoL (and related constructs) after SCI. The findings of this review support efforts toward an improved conceptual understanding of QoL to ensure that investigators employ appropriate research designs and suitable outcome measures to assess this prevalent secondary health condition. The summary of QoL outcome tools may also aid clinicians in the selection of appropriate tools for assessing the impact of NBD on QoL in patients with SCI, which may guide practice.
Findings from this review show that existing tools are representative of Dijkers's three QoL domains of utility, achievements, and subjective well-being.19,22 Although no objective tool was developed specifically for SCI, all tools have been validated for use in the SCI population. Likewise, no objective tools have specific items related to NBD in SCI, but four of five tools have shown sensitivity to the impact of NBD (CHART, HUI-III, SF-36, SF-12). Five of the eight subjective tools were developed specifically to assess the influence of NBD on QoL in SCI (Burwood QoL Questionnaire, ICI Scale, NBD score, SCI-QoL Bowel Management Difficulties, and SNBC). At least some psychometric evidence has been generated for all five of these tools, and all five tools have shown sensitivity to impact of NBD. The goal of classification in this review is to assist researchers and clinicians in the outcome tool selection process, not to endorse the use of one tool over another.
Constantly evolving conceptualizations and definitions of QoL and related constructs (eg, social participation, life satisfaction) make measurement difficult and confusing for both researchers and clinicians.70 In addition to providing clear definitions and conceptualizations of QoL (eg, QoL specific to a secondary health condition in SCI),70 the inclusion of both objective and subjective tools has been suggested.28 Objective tools provide insight on what society agrees is important to health, but does not consider what is important to the individual. Conversely, subjective measures expose individuals' feelings and perceptions about their health-related issues but may overlook societal norms.71 Recommendations moving forward are that QoL assessments include a combination of psychometrically sound, objective and subjective QoL tools that cover the three QoL domains described in Dijkers' model (utility, achievement, subjective well-being) and that have shown sensitivity to NBD in SCI.
The SF-36 is among the most widely used measures of health-related QoL in the field of medicine72,73 and was the most commonly used objective measure of NBD-specific QoL in this review. The strengths of the SF-36 include that it can be administered in 10 minutes or less to provide a relatively valid and responsive tool for assessing health-related QoL according to society. Although the SF-36 has documented reliability and validity specific to SCI, there is limited evidence of its sensitivity to the impact of NBD on QoL. This limitation could potentially be minimized by pairing the SF-36 with a condition-specific tool,74 such as the NBD.
Like the SF-36, the HUI-III contains no items specific to NBD or SCI and psychometric evidence for SCI is preliminary. However, the HUI-III represents a comprehensive and potentially promising objective tool for assessing preference-based health state (ie, utility; boxes A, B, and C, Figure 1).19 Objective measurement of health utility is becoming of increasing interest in medicine and rehabilitation science, as evidence of cost utility and cost-effectiveness is most likely to inform decisions regarding resource allocation.75 Use of validated utility tools, such as the HUI-III, may help to promote evidence-based practice specific to NBD treatment in SCI.
With regard to subjective measures, the NBD score was the most comprehensive tool, incorporating both subjective domains of QoL (subjective well-being, achievements) (boxes C, D, and E, Figure 1).19 The NBD score takes 5 minutes or less to administer, has strong psychometric properties,49 and has shown sensitivity to impact of NBD on QoL in five studies (including two RCTs).28,29,49,51,55 In fact, the NBD score is the only QoL outcome tool identified in this review that showed responsiveness to change in QoL due to changes in bowel function.28,29 As noted, the majority of items on the scale reflect those typically seen in objective measures, but the underlying design of the scale, along with the inclusion of the subjective QoL items, suggests that its resulting score is reflective of subjective perceptions of the impact of NBD on QoL after SCI. Further work to determine its subjective properties should be explored by using it with other subjective measures of QoL (general and condition-specific) to confirm this assumption.
The Burwood QoL Questionnaire, ICI Scale, and SNBC captured QoL constructs related to achievements and subjective evaluations (boxes C and E, Figure 1),19 which are important for understanding whether patients' expectations are met and whether individuals are satisfied with their life, happy, and have overall perceived well-being. The SCI-QoL Bowel Management Difficulty was developed using a patient-centered approach to develop three subjective QoL outcome tools that include items about neurogenic bowel in SCI.57 From a clinical and statistical perspective, the SCI-QOL Bowel Management Difficulties items bank shows promise for measuring overall well-being and life satisfaction (Subjective Evaluations and Reactions, box E, Figure 1).19
Three other subjective tools were identified to assess the impact of NBD on QoL (HADS, IBDQ, RSS) in this review. While the IBDQ was developed specifically to measure QoL related to bowel dysfunction, it was developed for use in individuals with inflammatory bowel diseases such as Crohn's and colitis.76 Although the IBDQ has been validated for use in SCI, the tool was not sensitive to the impact of NBD. It is likely that the items touch on condition-specific issues of NBD, but lack a comprehensive assessment of SCI-related impairments (eg, paralysis). Both the HADS and RSS are validated for use in SCI and showed sensitivity to the impact of NDB but are not QoL measures per se nor do they have condition-specific items (NBD and/or SCI).
The recent development of NBD-specific tools for SCI is timely in the advancement of SCI treatments for NBD and for revolutionizing QoL measurement. This review identified both objective and subjective tools and provided recommendations for their use based on existing psychometric properties and evidence of responsiveness to NBD impact. However, the quality of evidence to date is quite low, as most studies were cross-sectional designs. Moreover, the variability in QoL between individuals with upper motor neuron versus lower motor neuron bowel dysfunction may have important implications on QoL that have not yet been addressed.77,78 For example, individuals with upper motor NBD have a hyperreflexive bowel and experience normal or increased sphincter tone, constipation and fecal retention, with reflexive defecation. Bowel care is recommended every 1 to 3 days, and rectal suppositories or digital stimulation can be used to assist in evacuation. Conversely, individuals with lower motor NBD experience constipation and incontinence, reduced anal sphincter tone, and the defecation reflex is absent. Daily bowel care is recommended, and neither suppositories nor digital stimulate are effective. Therefore, it seems that upper motor NBD symptoms may impact less on QoL; however, current tools are not able to detect the discussed differences.
Future studies should continue to validate existing tools and provide evidence of responsiveness and clinical significance in experimental trials. More research that examines the associations between QoL and changes in NBD over time would also help to clarify whether QoL changes in persons with SCI as bowel function improves. A broader understanding of how NBD impacts QoL of individuals with SCI would facilitate better planning of services, treatment, and rehabilitation.14 In the current practice, clinicians largely direct their efforts toward addressing the health condition (ie, NBD) and its associated impact on body functions and structures (eg, loss of volitional control, bowel transit times). Better measurement of QoL and related constructs will address the expressed need for consideration of activities, participation, and contextual factors (personal, environmental) that reflect the whole lived experiences of individuals living with NBD after SCI.14
Limitations
A limitation of this review is that samples with <50% of individuals with SCI were excluded, which may introduce bias in the results. Further, information on cross-cultural applications were not available. It is also possible that we did not identify all relevant articles for inclusion.
Conclusion
Accurate assessment of NBD impact on QoL should be an important consideration in rehabilitation practice, as it influences the extent and nature of the treatments applied. Based on this review, promising objective (HUI-III) and subjective (NBD score, ICI Scale, Survey of Neurogenic Bowel Characteristics, and SCI-QoL Bowel Management Difficulties) outcome tools were identified for assessing the impact of NBD on QoL in SCI. Further work is recommended to increase evidence of their validity, reliability, and clinical utility. A combination of objective and subjective QoL tools are recommended to best understand the impact of NBD over time, treatments effects, clinical practice, and resource allocation issues within the health care system.
Footnotes
Conflicts of Interest
The authors declare no conflicts of interest.
REFERENCES
- 1.Anderson KD. Targeting recovery: Priorities of the spinal cord-injured population. J Neurotrauma. 2004;21:1371–1383. doi: 10.1089/neu.2004.21.1371. [DOI] [PubMed] [Google Scholar]
- 2.Smith K, Balioussis C, Craven BC, E-Scan Investigative Team Craven BC, Verrier M, Balioussis C, editors. et al. Rehabilitation Environmental Scan Atlas: Capturing Capacity in Canadian SCI Rehabilitation. 2012:61–68. In. eds. NATLAS2012WEB_2014.pdf. http://www.rickhanseninstitute.org/images/stories/ESCAN/RHESCA Accessed April 14, 2017.
- 3.Dunn M. Social discomfort in the patient with spinal cord injury. Arch Phys Med Rehabil. 1977;58:257–260. [PubMed] [Google Scholar]
- 4.Glickman S, Kamm MA. Bowel dysfunction in spinal-cord-injury patients. Lancet. 1996;347:1651–1653. doi: 10.1016/s0140-6736(96)91487-7. [DOI] [PubMed] [Google Scholar]
- 5.Kirk PM, King RB, Temple R, Bourjaily J, Thomas P. Long-term follow-up of bowel management after spinal cord injury. SCI Nurse. 1997;14:56–63. [PubMed] [Google Scholar]
- 6.Coggrave MJ, Ingram RM, Gardner BP, Norton CS. The impact of stoma for bowel management after spinal cord injury. Spinal Cord. 2012;50:848–852. doi: 10.1038/sc.2012.66. [DOI] [PubMed] [Google Scholar]
- 7.Stone JM, Nino-Murcia M, Wolfe VA, Perkash I. Chronic gastrointestinal problems in spinal cord injury patients: A prospective analysis. Am J Gastroenterol. 1990;85:1114–1119. [PubMed] [Google Scholar]
- 8.Pardee C, Bricker D, Rundquist J, MacRae C, Tebben C. Characteristics of neurogenic bowel in spinal cord injury and perceived quality of life. Rehabil Nurse. 2012;37:128–135. doi: 10.1002/RNJ.00024. [DOI] [PubMed] [Google Scholar]
- 9.Lynch AC, Antony A, Dobbs BR, Frizelle FA. Bowel dysfunction following spinal cord injury. Spinal Cord. 2001;39:193–203. doi: 10.1038/sj.sc.3101119. [DOI] [PubMed] [Google Scholar]
- 10.Lynch AC, Wong C, Anthony A, Dobbs BR, Frizelle FA. Bowel dysfunction following spinal cord injury: A description of bowel function in a spinal cord-injured population and comparison with age and gender matched controls. Spinal Cord. 2000;38:717–723. doi: 10.1038/sj.sc.3101058. [DOI] [PubMed] [Google Scholar]
- 11.Steins SA, Bergman SB, Goetz LL. Neurogenic bowel dysfunction after spinal cord injury: Clinical evaluation and rehabilitative management. Arch Phys Med Rehabil. 1997;78:S86–S102. doi: 10.1016/s0003-9993(97)90416-0. [DOI] [PubMed] [Google Scholar]
- 12.Correa GI, Rotter KP. Clinical evaluation and management of neurogenic bowel after spinal cord injury. Spinal Cord. 2000;38:301–308. doi: 10.1038/sj.sc.3100851. [DOI] [PubMed] [Google Scholar]
- 13.Longo WE, Woolsey RM, Vernava AM, Virgo KS, McKirgan L, Johnson FE. Cisapride for constipation in spinal cord injured patients: A preliminary report. J Spinal Cord Med. 1995;18:240–244. doi: 10.1080/10790268.1995.11719403. [DOI] [PubMed] [Google Scholar]
- 14.Burns AS, St-Germain D, Connolly M et al. Phenomenological study of eurogenic bowel from the perspective of individuals living with spinal cord injury. Arch Phys Med Rehabil. 2015;96:49–55. doi: 10.1016/j.apmr.2014.07.417. [DOI] [PubMed] [Google Scholar]
- 15.Coggrave M, Norton C. Management of faecal incontinence and constipation in adults with central neurological diseases. Cochrane Database Syst Rev. 2013;12:Cd002115. doi: 10.1002/14651858.CD002115.pub4. [DOI] [PubMed] [Google Scholar]
- 16.Consortium for Spinal Cord Medicine Clinical Practice Guidelines: Neurogenic Bowel Management in Adults with Spinal Cord Injury. Washington, DC: Paralyzed Veterans of America; 1998. [DOI] [PubMed] [Google Scholar]
- 17.Krassioukov A, Eng JJ, Claxton G, Sakakibara BM, Shum S. Neurogenic bowel management after spinal cord injury: A systematic review of the evidence. Spinal Cord. 2010;48:718–733. doi: 10.1038/sc.2010.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Burns AS, St-Germain D, Connolly M et al. Neurogenic bowel after spinal cord injury from the perspective of support providers: A phenomenological study. Phys Med Rehabil. 2015;7:407–416. doi: 10.1016/j.pmrj.2014.09.020. [DOI] [PubMed] [Google Scholar]
- 19.Dijkers M. “What's in a name?” The indiscriminate use of the “quality of life” label, and the need to bring about clarity in conceptualizations. Int J Nursing Stud. 2007;44:153–155. doi: 10.1016/j.ijnurstu.2006.07.016. [DOI] [PubMed] [Google Scholar]
- 20.Hitzig SL, Noreau L, Balioussis C, Routhier F, Kairy D, Craven BC. The development of the spinal cord injury participation and quality of life (PAR-QoL) tool-kit. Disabil Rehabil. 2013;35:1408–1414. doi: 10.3109/09638288.2012.735340. [DOI] [PubMed] [Google Scholar]
- 21.Dijkers MP. Individualization in quality of life measurement: Instruments and approaches. Arch Phys Med Rehabil. 2003;84:S3–14. doi: 10.1053/apmr.2003.50241. [DOI] [PubMed] [Google Scholar]
- 22.Dijkers MP. Quality of life of individuals with spinal cord injury: A review of conceptualization, measurement, and research findings. J Rehabil Res Dev. 2005;42:87–110. doi: 10.1682/jrrd.2004.08.0100. [DOI] [PubMed] [Google Scholar]
- 23.Hitzig SL, Balioussis C, Nussbaum E, McGillivray CF, Catharine Craven B, Noreau L. Identifying and classifying quality-of-life tools for assessing pressure ulcers after spinal cord injury. J Spinal Cord Med. 2013;36:600–615. doi: 10.1179/2045772313Y.0000000129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Best KL, Ethans K, Craven BC, Noreau L, Hitzig S. Identifying and classifying quality of life tools for assessing neurogenic bladder after spinal cord injury. J Spinal Cord Med. 2017;40(5):501–517. doi: 10.1080/10790268.2016.1226700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Balioussis C, Hitzig SL, Flett H, Noreau L, Craven BC. Identifying and classifying quality of life tools for assessing spasticity after spinal cord injury. Top Spinal Cord Inj Rehabil. 2014;20:208–224. doi: 10.1310/sci2003-208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Young RR, Shahani BT. Spasticity in spinal cord injured patients. In: Bloch RE, Basbaum M, editors. Management of Spinal Cord Injuries. Baltimore: Williams and Wilkins; 1986. pp. 241–283. [Google Scholar]
- 27.Dijkers MP. Quality of life after traumatic brain injury: A review of research approaches and findings. Arch Phys Med Rehabil. 2004;85:S21–35. doi: 10.1016/j.apmr.2003.08.119. [DOI] [PubMed] [Google Scholar]
- 28.Christensen P, Bazzocchi G, Coggrave M et al. Outcome of transanal irrigation for bowel dysfunction in patients with spinal cord injury. J Spinal Cord Med. 2008;31:560–567. doi: 10.1080/10790268.2008.11754571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Christensen P, Bazzocchi G, Coggrave M et al. A randomized, controlled trial of transanal irrigation versus conservative bowel management in spinal cord-injured patients. Gastroenterology. 2006;131:738–747. doi: 10.1053/j.gastro.2006.06.004. [DOI] [PubMed] [Google Scholar]
- 30.Kelly SR, Shashidharan M, Borwell B, Tromans AM, Finnis D, Grundy DJ. The role of intestinal stoma in patients with spinal cord injury. Spinal Cord. 1999;37:211–214. doi: 10.1038/sj.sc.3100764. [DOI] [PubMed] [Google Scholar]
- 31.Christensen P, Kvitzau B, Krogh K, Buntzen S, Laurberg S. Neurogenic colorectal dysfunction - use of new antegrade and retrograde colonic wash-out methods. Spinal Cord. 2000;38:255–261. doi: 10.1038/sj.sc.3100991. [DOI] [PubMed] [Google Scholar]
- 32.Kachourbos MJ, Creasey GH. Health promotion in motion: Improving quality of life for persons with neurogenic bladder and bowel using assistive technology. SCI Nurs. 2000;17:125–129. [PubMed] [Google Scholar]
- 33.Lombardi G, Del Popolo G, Cecconi F, Surrenti E, Macchiarella A. Clinical outcome of sacral neuromodulation in incomplete spinal cord-injured patients suffering from neurogenic bowel dysfunctions. Spinal Cord. 2010;48:154–159. doi: 10.1038/sc.2009.101. [DOI] [PubMed] [Google Scholar]
- 34.Lombardi G, Nelli F, Mencarini M, Del Popolo G. Clinical concomitant benefits on pelvic floor dysfunctions after sacral neuromodulation in patients with incomplete spinal cord injury. Spinal Cord. 2011;49:629–636. doi: 10.1038/sc.2010.176. [DOI] [PubMed] [Google Scholar]
- 35.Rosito O, Nino-Murcia M, Wolfe VA, Kiratli BJ, Perkash I. The effects of colostomy on the quality of life in patients with spinal cord injury: A retrospective analysis. J Spinal Cord Med. 2002;25:174–183. doi: 10.1080/10790268.2002.11753619. [DOI] [PubMed] [Google Scholar]
- 36.Safadi BY, Rosito O, Nino-Murcia M, Wolfe VA, Perkash I. Which stoma works better for colonic dysmotility in the spinal cord injured patient? Am J Surg. 2003;186:437–442. doi: 10.1016/j.amjsurg.2003.07.007. [DOI] [PubMed] [Google Scholar]
- 37.Del Popolo G, Mosiello G, Pilati C et al. Treatment of neurogenic bowel dysfunction using transanal irrigation: A multicenter Italian study. Spinal Cord. 2008;46:517–522. doi: 10.1038/sj.sc.3102167. [DOI] [PubMed] [Google Scholar]
- 38.Teichman JM, Zabihi N, Kraus SR, Harris JM, Barber DB. Long-term results for Malone antegrade continence enema for adults with neurogenic bowel disease. Urology. 2003;61:502–506. doi: 10.1016/s0090-4295(02)02282-3. [DOI] [PubMed] [Google Scholar]
- 39.Hicken BL, Putzke JD, Richards JS. Bladder management and quality of life after spinal cord injury. Am J Phys Med Rehabil. 2001;80:916–922. doi: 10.1097/00002060-200112000-00008. [DOI] [PubMed] [Google Scholar]
- 40.Luther SL, Nelson AL, Harrow JJ, Chen F, Goetz LL. A comparison of patient outcomes and quality of life in persons with neurogenic bowel: Standard bowel care program vs colostomy. J Spinal Cord Med. 2005;28:387–393. doi: 10.1080/10790268.2005.11753838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Randell N, Lynch AC, Anthony A, Dobbs BR, Roake JA, Frizelle FA. Does a colostomy alter quality of life in patients with spinal cord injury? A controlled study. Spinal Cord. 2001;39:279–282. doi: 10.1038/sj.sc.3101156. [DOI] [PubMed] [Google Scholar]
- 42.Worsoe J, Christensen P, Krogh K, Buntzen S, Laurberg S. Long-term results of antegrade colonic enema in adult patients: Assessment of functional results. Dis Colon Rectum. 2008;51:1523–1528. doi: 10.1007/s10350-008-9401-6. [DOI] [PubMed] [Google Scholar]
- 43.Branagan G, Tromans A, Finnis D. Effect of stoma formation on bowel care and quality of life in patients with spinal cord injury. Spinal Cord. 2003;41:680–683. doi: 10.1038/sj.sc.3101529. [DOI] [PubMed] [Google Scholar]
- 44.Anson CA, Stanwyck DJ, Krause JS. Social support and health status in spinal cord injury. Paraplegia. 1993;31:632–638. doi: 10.1038/sc.1993.102. [DOI] [PubMed] [Google Scholar]
- 45.Coggrave M, Norton C, Wilson-Barnett J. Management of neurogenic bowel dysfunction in the community after spinal cord injury: A postal survey in the United Kingdom. Spinal Cord. 2009;47:323–330. doi: 10.1038/sc.2008.137. [DOI] [PubMed] [Google Scholar]
- 46.Craven C, Hitzig SL, Mittmann N. Impact of impairment and secondary health conditions on health preference among Canadians with chronic spinal cord injury. J Spinal Cord Med. 2012;35:361–370. doi: 10.1179/2045772312Y.0000000046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Han TR, Kim JH, Kwon BS. Chronic gastrointestinal problems and bowel dysfunction in patients with spinal cord injury. Spinal Cord. 1998;36:485–490. doi: 10.1038/sj.sc.3100616. [DOI] [PubMed] [Google Scholar]
- 48.Kim JY, Koh ES, Leigh J, Shin HI. Management of bowel dysfunction in the community after spinal cord injury: A postal survey in the Republic of Korea. Spinal Cord. 2012;50:303–308. doi: 10.1038/sc.2011.124. [DOI] [PubMed] [Google Scholar]
- 49.Krogh K, Christensen P, Sabroe S, Laurberg S. Neurogenic bowel dysfunction score. Spinal Cord. 2006;44:625–631. doi: 10.1038/sj.sc.3101887. [DOI] [PubMed] [Google Scholar]
- 50.Krogh K, Nielsen J, Djurhuus JC, Mosdal C, Sabroe S, Laurberg S. Colorectal function in patients with spinal cord lesions. Dis Colon Rectum. 1997;40:1233–1239. doi: 10.1007/BF02055170. [DOI] [PubMed] [Google Scholar]
- 51.Liu CW, Huang CC, Yang YH, Chen SC, Weng MC, Huang MH. Relationship between neurogenic bowel dysfunction and health-related quality of life in persons with spinal cord injury. J Rehabil Med. 2009;41:35–40. doi: 10.2340/16501977-0277. [DOI] [PubMed] [Google Scholar]
- 52.Noonan VK, Kopec JA, Zhang H, Dvorak MF. Impact of associated conditions resulting from spinal cord injury on health status and quality of life in people with traumatic central cord syndrome. Arch Phys Med Rehabil. 2008;89:1074–1082. doi: 10.1016/j.apmr.2007.10.041. [DOI] [PubMed] [Google Scholar]
- 53.Roach MJ, Frost FS, Creasey G. Social and personal consequences of acquired bowel dysfunction for persons with spinal cord injury. J Spinal Cord Med. 2000;23:263–269. doi: 10.1080/10790268.2000.11753535. [DOI] [PubMed] [Google Scholar]
- 54.Westgren N, Levi R. Quality of life and traumatic spinal cord injury. Arch Phys Med Rehabil. 1998;79:1433–1439. doi: 10.1016/s0003-9993(98)90240-4. [DOI] [PubMed] [Google Scholar]
- 55.Adriaansen JJ, van Asbeck FW, van Kuppevelt D, Snoek GJ, Post MW. Outcomes of neurogenic bowel management in individuals living with a spinal cord injury for at least 10 years. Arch Phys Med Rehabil. 2015;96:905–912. doi: 10.1016/j.apmr.2015.01.011. [DOI] [PubMed] [Google Scholar]
- 56.Faaborg PM, Christensen P, Finnerup N, Laurberg S, Krogh K. The pattern of colorectal dysfunction changes with time since spinal cord injury. Spinal Cord. 2008;46:234–238. doi: 10.1038/sj.sc.3102121. [DOI] [PubMed] [Google Scholar]
- 57.Tulsky DS, Kisala PA, Tate DG, Spungen AM, Kirshblum SC. Development and psychometric characteristics of the SCI-QOL Bladder Management Difficulties and Bowel Management Difficulties item banks and short forms and the SCI-QOL Bladder Complications scale. J Spinal Cord Med. 2015;38:288–302. doi: 10.1179/2045772315Y.0000000030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Hill MR, Noonan VK, Sakakibara BM, Miller WC. Quality of life instruments and definitions in individuals with spinal cord injury: A systematic review. Spinal Cord. 2010;48:438–450. doi: 10.1038/sc.2009.164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Andresen EM, Fouts BS, Romeis JC, Brownson CA. Performance of health-related quality-of-life instruments in a spinal cord injured population. Arch Phys Med Rehabil. 1999;80:877–884. doi: 10.1016/s0003-9993(99)90077-1. [DOI] [PubMed] [Google Scholar]
- 60.Anderson K, Aito S, Atkins M et al. Functional recovery measures for spinal cord injury: An evidence-based review for clinical practice and research. J Spinal Cord Med. 2008;31:133–144. doi: 10.1080/10790268.2008.11760704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kucukdeveci AA, Yavuzer G, Tennant A, Suldur N, Sonel B, Arasil T. Adaptation of the modified Barthel Index for use in physical medicine and rehabilitation in Turkey. Scand J Rehabil Med. 2000;32:87–92. [PubMed] [Google Scholar]
- 62.Shah S, Vanclay F, Cooper B. Improving the sensitivity of the Barthel Index for stroke rehabilitation. J Clin Epidemiol. 1989;42:703–709. doi: 10.1016/0895-4356(89)90065-6. [DOI] [PubMed] [Google Scholar]
- 63.Feeny D, Furlong W, Torrance GW et al. Multiattribute and single-attribute utility functions for the health utilities index mark 3 system. Med Care. 2002;40:113–128. doi: 10.1097/00005650-200202000-00006. [DOI] [PubMed] [Google Scholar]
- 64.Robinson R. Cost-utility analysis. Brit Med J. 1993;307:859–862. doi: 10.1136/bmj.307.6908.859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Boyle MH, Furlong W, Feeny D, Torrance GW, Hatcher J. Reliability of the Health Utilities Index-Mark III used in the 1991 cycle 6 Canadian General Social Survey Health Questionnaire. Qual Life Res. 1995;4:249–257. doi: 10.1007/BF02260864. [DOI] [PubMed] [Google Scholar]
- 66.Mittmann N, Trakas K, Risebrough N, Liu BA. Utility scores for chronic conditions in a community-dwelling population. Pharmaco Econom. 1999;15:369–376. doi: 10.2165/00019053-199915040-00004. [DOI] [PubMed] [Google Scholar]
- 67.Hall K, Dijkers M, Whiteneck G, Brooks CA, Krause JS. The Craig Handicap Assessment and Reporting Technique (CHART): Metric properties and scoring. Top Spinal Cord Inj Rehabil. 1998;4:16–30. [Google Scholar]
- 68.Krause JS, Coker JL, Charlifue S, Whiteneck GG. Health outcomes among American Indians with spinal cord injury. Arch Phys Med Rehabil. 2000;81(7):924–931. doi: 10.1053/apmr.2000.5618. [DOI] [PubMed] [Google Scholar]
- 69.Woolrich RA, Kennedy P, Tasiemski T. A preliminary psychometric evaluation of the Hospital Anxiety and Depression Scale (HADS) in 963 people living with a spinal cord injury. Psychol Health Med. 2006;11:80–90. doi: 10.1080/13548500500294211. [DOI] [PubMed] [Google Scholar]
- 70.Post MWM. Definitions of quality of life: What has happened and how to move on. Top Spinal Cord Injury Rehabil. 2014;20(3):167–180. doi: 10.1310/sci2003-167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Angur MG, Widgery R, Angur SG. Congruence among objective and subjective quality-of-life (QOL) indicators. AJBR. http://ajbr.org/Archives/Congruence%20among%20Objective%20and%20Subjective%20Quality-of-Life%20(QOL)%20indicators.pdf Accessed October 23, 2017.
- 72.McHorney CA, Ware JE, Jr, Lu JF, Sherbourne CD. The MOS 36-item Short-Form Health Survey (SF-36): III. Tests of data quality, scaling assumptions, and reliability across diverse patient groups. Med Care. 1994;32:40–66. doi: 10.1097/00005650-199401000-00004. [DOI] [PubMed] [Google Scholar]
- 73.Whitehurst DG, Engel L, Bryan S. Short Form health surveys and related variants in spinal cord injury research: A systematic review. J Spinal Cord Med. 2014;37:128–138. doi: 10.1179/2045772313Y.0000000159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Andresen EM, Meyers AR. Health-related quality of life outcomes measures. Arch Phys Med Rehabil. 2000;81:S30–45. doi: 10.1053/apmr.2000.20621. [DOI] [PubMed] [Google Scholar]
- 75.Sanders GD, Neumann PJ, Basu A et al. Recommendations for conduct, methodological practices, and reporting of cost-effectiveness analyses: Second panel on cost-effectiveness in health and medicine. JAMA. 2016;316(10):1093–1103. doi: 10.1001/jama.2016.12195. [DOI] [PubMed] [Google Scholar]
- 76.Irvine EJ, Feagan BG, Wong CJ. Does self-administration of a quality of life index for inflammatory bowel disease change the results? J Clin Epidemiol. 1996;49:1177–85. doi: 10.1016/0895-4356(96)00136-9. 78. [DOI] [PubMed] [Google Scholar]
- 77.Consortium for Spinal Cord Medicine Clinical practice guidelines: Neurogenic bowel management in adults with spinal cord injury. J Spinal Cord Med. 1998;21:248–293. doi: 10.1080/10790268.1998.11719536. [DOI] [PubMed] [Google Scholar]
- 78.Linsenmeyer TA, Stone JM, Steins SA. Neurogenic bowel. In: Delisa J, editor. Physical Medicine and Rehabilitation: Principles and Practice, Volume 2. 4th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2005. 1641 pp. [Google Scholar]
- 79.Teichman JM, Zabihi N, Kraus SR, Harris JM, Barber DB. Long-term results for Malone antegrade continence enema for adults with neurogenic bowel disease. Urology. 2003;61(3):502–506. doi: 10.1016/s0090-4295(02)02282-3. [DOI] [PubMed] [Google Scholar]


