Abstract
BACKGROUND
Research indicates that the age of onset of first acute myocardial infarction (AMI) is an essential element in the life expectancy that has been decreasing in developing countries. There are various studies performed in Iran reporting a range of ages at time of AMI. Thus, this meta-analysis study is designed to determine the mean age at first AMI in the Iranian population.
METHODS
All studies that met the inclusion and exclusion criteria were reviewed using standard keywords in the databases from 2000 to 2016. Two raters verified a total of 658 articles. Sixteen studies met the inclusion criteria of this study for meta-analysis. Cochran test and I-squared (I2) were used for samples’ homogeneity. Pooled estimates of mean were calculated using the random effects inverse-variance model.
RESULTS
The mean age of AMI varied between 55.9 to 62.9 years among the primary studies. The pooled mean age of first AMI with a 95% confidence interval (CI) for the total sample, men, and women were 59 (58.9, 60.4), 58.7 (58.3, 59.2), and 64.2 (63.5, 64.8), respectively.
CONCLUSION
Our meta-analysis shows that the mean age of first onset of AMI in Iranian people is slightly lower than that reported elsewhere; and it is lower for men than for women.
Keywords: Myocardial Infarction, Meta-Analysis, Iran
Introduction
Coronary artery disease (CAD) is responsible for nearly 46 percent of the mortality in Iran.1 This disease accounts for 80 percent of deaths in the low and middle-income countries.2 A study conducted in Iran indicated that 40 percent of deaths are related to the CAD.3 It is considered the leading cause of death in men and women.4 It should be noted that the age of onset differs by gender.5,6 Based on world statistics in United Kingdom (UK), the prevalence of cardiovascular disease (CVD) in men and women aged 35-44 years is 50% and 18%, respectively. These percentages are 20.5% and 17.1% for men and women over 60 years, respectively.7 A systematic review of the 62 relevant studies among published articles between 1990-2014 reported that the annual incidence of CAD ranged from 27.6% to 57.0% per 100000 people.8 Moreover, some studies conducted in the Gulf States have reported a high incidence of CAD at a younger age. Of those patients, 9.8%-25% were less than 45 years old.9,10 Annually, CAD leads to approximately 6.3 million admissions to the hospitals affiliated to the Iranian Ministry of Health and Medical Education.11 Moreover, death following CAD is estimated to be 205 per 100000 in all age groups and 4156 per 100000 per year in individuals older than 70. Although increasing age is a recognized risk factor for acute myocardial infarction (AMI), a study indicates that an early age of AMI is a serious problem, as it is associated with major morbidity, psychological effects, and financial limitations for the person and the family.12 Awareness of age of AMI is important and useful in the evidence-based decisions, research, prioritization, monitoring and planning in the health system as well as identifying the AMI etiology and risk factors related to that.3 Annually, approximately one percent of men aged 30 to 62 experience at least one symptom of CAD. Of those, about 42 percent evolve into an AMI.13 It should be noted that AMI occurs in men at younger ages than women. For women who are hospitalized for AMI under the age of 50 years, risk of mortality is double that for men.14
The incidence of AMI is increasing and occurring earlier in life in developing countries due to sedentary lifestyle, weight gain, tobacco use as well as the lack of attention to job stress and mental health advice.15,16 However, Okrainec et al. reported that AMI occurred in 38% of patients who were younger than 75 years old.17 It seems that the age of first incidence of AMI is decreasing in Iran.2 Also, the Global Registry of Acute Coronary Events (GRACE) defined age as an independent prognostic factor for AMI. Thus, the mortality risk will increase about 7.1 percent within a decade in all age ranges.18 In other words, aging causes changes in the structure and function of vessels, increasing left ventricular wall thickness, reducing ventricular diastolic compliance, and weakening the sensitivity to changes in the neurohormonal beta receptors in the heart. These factors are just a few that have been postulated.19
The age of onset of AMI and its risk factors among different age and racial groups are influenced by variations in lifestyle and other circumstances.20 Although an increased incidence of AMI is linked with a wide range of individual risk factors, these factors can explain only about 50-60 percent of demographical changes. Thus, there is a need to look beyond of individual factors. Logical and epidemiological context theories suggest that development of disease is influenced by different climates influences. Therefore, describing the demographic, clinical, geographical, and regional factors affecting the incidence of CAD can produce new hypothesis.21
As one of the risk factors of a disease epidemic is younger age,22 a survey of the age at first incidence of AMI can lead to the determination of the epidemiology of AMI22 in the prevention, diagnosis, treatment, and prognosis.23 In Iran, one study reported the mean ± standard deviation (SD) age of AMI as 64.2 ± 10.1 and 57.5 ± 11.4 among men and women, respectively.24 Another study reported the mean age of AMI as 57.2 ± 13.6 for men and 61.6 ± 9.5 for women.23 Neamatipoor et al. also showed that the mean age of AMI has changed over time in the Iranian population. So that, the mean age of women with AMI decreased from 65 years in 1992 to 61 years in 2002. Also, the mean age of first AMI in Iranian men decreased from 59 years in 1992 to 57 years in 2002.20
Considering the opposite findings of previous studies in different countries and time periods, estimation of the mean age of AMI incidence is important to estimate the prevalence of it. This study has the potential to give valuable information to health system policymakers in Iran to use this information for the development of preventive programs. In addition, results of the present survey can provide valuable information for resource allocation. Thus, this study was performed to estimate the average age of AMI onset in Iranian men and women.
Materials and Methods
The present meta-analysis study was based on the sample articles available about the age of AMI in Iran. The databases including PubMed, Web of Knowledge, ScienceDirect, Google Scholar, SID, MedLib, Magiran, and Iranmedex were reviewed. The following key terms were searched: age, onset, incidence, and acute myocardial infarction, with the use of OR and AND operators. Moreover, sources that were not online were searched manually. These sources included MSc or PhD published theses and related books in library, and consultation with researchers. Two independent reviewers screened titles and abstracts for relevance. Articles were obtained and assessed in detail for inclusion. Studies had to meet all three of the following criteria for inclusion: 1) keywords should be mentioned in the title or the abstract section; 2) both mean and SD of the onset age in AMI is needed to be mentioned, and 3) cross-sectional studies. Each of the papers was reviewed for the presence of the selected inclusion and exclusion criteria. Studies were conducted at different times of the year and by different researchers. Studies were excluded if they were or had: 1) incomplete data (mean and SD of the onset age in MI), 2) subjects with diagnosis of acute coronary syndrome (ACS), 3) abstracts only. Some of the authors provided publications of a finding; in this case, only the study with the largest sample size was included in the meta-analysis.
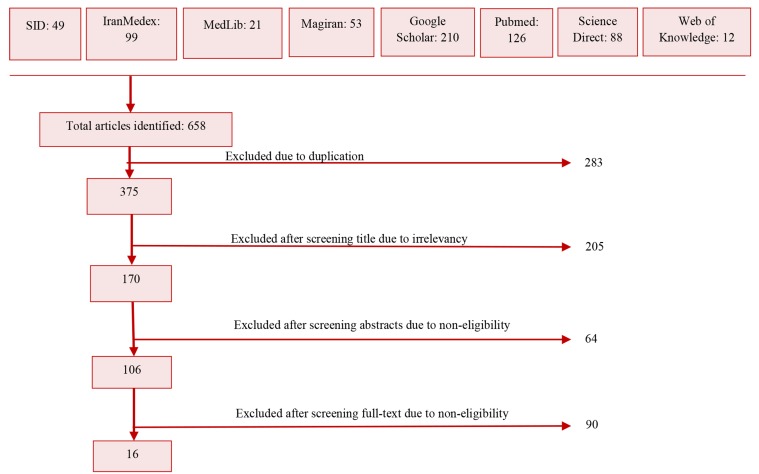
Sixteen papers were found after the thorough search from January1st, 2000 to December 31st, 2016 in Iranian population. Search strategies and the number of articles in each level of study are separately given in figure 1 and table 1, respectively.
Figure 1.
Flow chart of the process and rationale used in selecting studies for inclusion
Table 1.
Characteristics of the studies selected for the meta-analysis
| Authors | Geographic regions | Sample size | Sampling methods | AMI age (year) (mean ± SD) |
||
|---|---|---|---|---|---|---|
| Total | Men | Women | ||||
| Ahmadi et al.25 | Tehran | 20750 | Census | 61.20 ± 13.40 | 59.60 ± 11.80 | 65.40 ± 12.60 |
| Farshidi et al.26 | Bandar Abbas | 227 | Census | 57.93 ± 13.10 | Unknown | Unknown |
| Gholi et al.27 | Karaj | 140 | Convenient | 58.80 ± 11.50 | Unknown | Unknown |
| Hadjian and Jalali28 | Babol | 1233 | Census | 60.60 ± 11.20 | 60.10 ± 11.80 | 61.50 ± 11.00 |
| Hasan pour et al.29 | Shahr-e Kord | 150 | Convenient | 57.70 ± 10.50 | Unknown | Unknown |
| Hojat30 | Jahrom | 150 | Convenient | 55.92 ± 11.00 | Unknown | Unknown |
| Sezavar et al.16 | Tehran | 1829 | Census | 60.63 ± 13.50 | 56.90 ± 12.90 | 66.10 ± 11.60 |
| Kazemy and Sharifzadeh31 | Birjand | 918 | Census | 60.70 ± 12.10 | 58.90 ± 12.20 | 65.30 ± 10.70 |
| Kiani et al.32 | Zahedan | 213 | Convenient | 58.30 ± 12.60 | Unknown | Unknown |
| Taghipour et al.23 | Amol | 366 | Convenient | 58.70 ± 12.20 | 57.44 ± 13.30 | 65.40 ± 12.60 |
| Mohammadian et al.33 | Isfahan | 12815 | Census | 61.85 ± 12.60 | 60.00 ± 12.50 | 66.72 ± 11.30 |
| Beyranvand et al.34 | Tehran | 300 | Convenient | 56.60 ± 9.50 | 55.50 ± 9.50 | 58.20 ± 9.40 |
| Momeni et al.35 | Rasht | 162 | Convenient | 60.29 ± 12.40 | 59.71 ± 12.90 | 60.87 ± 11.90 |
| Sharif Nia et al.1 | Amol | 169 | Convenient | 59.49 ± 11.68 | 57.34 ± 13.60 | 61.64 ± 9.50 |
| Rajaei Behbahani et al.36 | Tehran | 33831 | Census | 62.91 ± 0.50 | 59.70 ± 0.80 | 66.13 ± 0.10 |
| Rostamzadeh et al.37 | Urmia | 81 | Census | 60.00 ± 7.80 | 57.40 ± 13.50 | 67.10 ± 9.00 |
AMI: Acute myocardial infarction; SD: Standard deviation
The following information was extracted for each study: author(s), year of publication, age of AMI, geographical area, sampling methods, mean age of participants, and sample size.
The quality of the extracted studies from the databases was assessed by two raters using checklist of the cross-sectional studies (STROBE), and the disagreements between the two raters were referred to a third rater.
Data were analyzed using Stata software (version 11). Samples’ heterogeneity was determined using Cochran’s Q test and I-squared (I2). The heterogeneity criterion was P < 0.001. Considering the heterogeneity existence, random effects inverse-variance model was used for calculating the mean age of AMI. Egger's test was used to examine publication bias on study outcome. Sensitivity analysis was run for assessing the effect of each study on overall estimate. Also, meta-regression was used in order to estimate the effect of suspicious factors on heterogeneity.
This study was approved by Ethics Committee of Mazandaran University of Medical Sciences, Sari, Iran (Code IR.MAZUMS.REC.95-2179).
Results
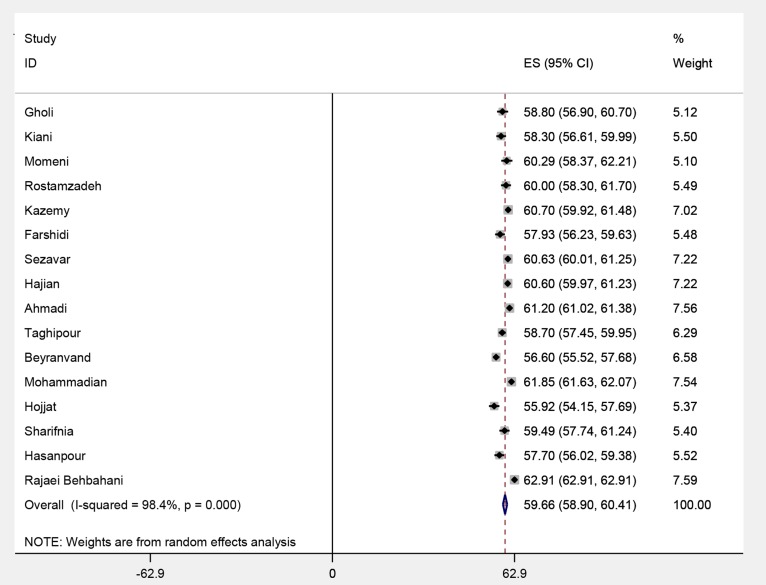
Of 16 eligible studies, 73334 AMI cases were included. The level of heterogeneity among the average age of AMI was highly significant (I2: 98.8%, Q = 948.54, P < 0.001). Hence, we applied the random effects inverse-variance model to aggregate their findings. As shown in figure 2, the mean age of AMI was 59.7 [95% confidence interval (CI): 58.9-60.4).
Figure 2.
The mean age of total patients with acute myocardial infarction (AMI) in each of the first studies entered into meta-analysis and its overall estimate ES: Effect size; CI: Confidence interval
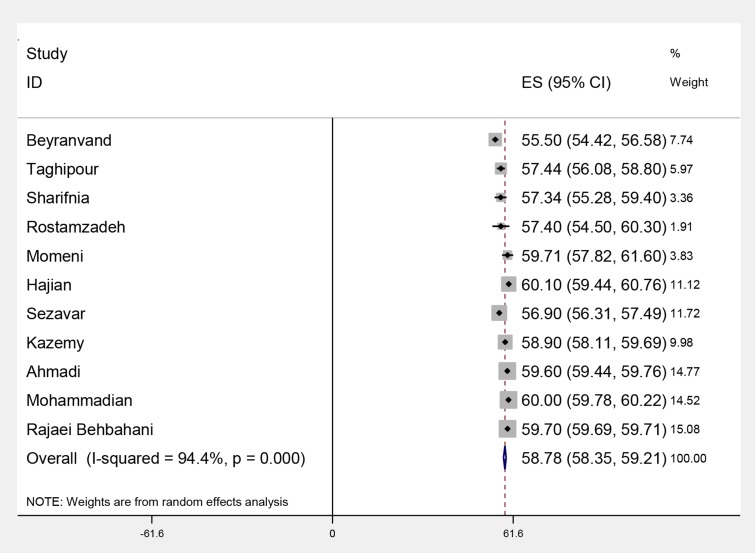
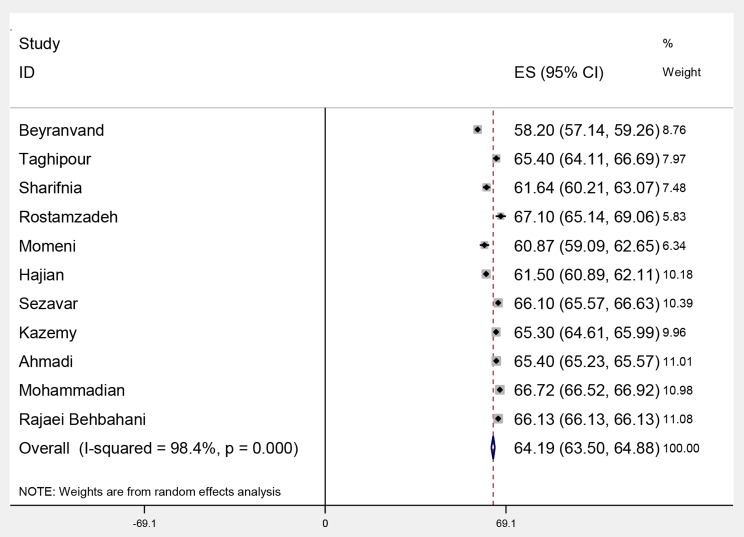
The mean age of AMI (95% CI) for men and women were 58.7 (58.3, 59.2), I2: 94.4%, Q: 176.99, P < 0.001, and 64.2 (63.5, 64.8), I2: 98.4%, Q: 615.30, P < 0.001, respectively. According to figures 3 and 4, the observed difference between the age of AMI among men and women was statistically significant.
Figure 3.
The mean age of acute myocardial infarction (AMI) in men in each of the first studies entered into meta-analysis and its overall estimate ES: Effect size; CI: Confidence interval
Figure 4.
The mean age of acute myocardial infarction (AMI) in women in each of the first studies entered into meta-analysis and its overall estimate ES: Effect size; CI: Confidence interval
A meta-regression model was used and the role of publication year as a potential source of heterogeneity was assessed.
The coefficient of year was -0.07 in this model with a P = 0.370; it should be noted that the incidence of AMI decreased by 0.07 units per year according to the results of meta-regression. However, the publication year did not explain a considerable part of the overall heterogeneity. In addition, the Egger’s test showed that publication bias was evident (β = -7.02, P < 0.001).
Discussion
The present study estimated that the age of onset of first AMI was 59.66 years among 112837 men and women in Iran. The results showed that the mean age of onset of AMI in Iran for men and women were 58.78 and 64.19 years, respectively. A study conducted in Italy reported the mean age of AMI onset 63.1 and 73.1 for men and women, respectively.38 Also, in Netherlands the average age of patients with the first AMI was 66.7 ± 13.2. The mean age of first AMI reported to be 64.2 ± 12.7 for men and 71.6 ± 12.8 for women.39 The average age of 71.8 years in women in comparison with the 65.0 years in men was reported in the USA.40 While in the developed countries, CAD occurs in the mid-sixties and early seventies among men and women, respectively, this happening has been reported to occur a decade earlier in developing countries like Qatar41 and Lebanon.42 Another study showed that the incidence of first AMI in the South Asian countries such as India, Pakistan, Bangladesh, Sri Lanka, and Nepal was occurred at a lower age compared to the rest of the world (i.e., women: 58.6 ± 11.6, and men: 53.0 ± 11.2 years old). The same study examined the risk factors in this population and stated that the lower prevalence of protective risk factors such as leisure time, physical movement, regular alcohol drinking, and everyday intake of fruits and vegetables as well as the higher prevalence of harmful risk factors including elevated apolipoprotein B-100/apolipoprotein A-I (apoB-100/apoA-I) ratio in South Asian countries can be considered as the reason for age difference.43 It should be pointed that the cost of hospitalization, treatment, rehabilitation, and other health care costs are higher in developing countries such as Iran.41 This can lead to late patients' referral and delay in receiving different levels of prevention.
The results of these studies reveal two aspects. First, it reflects the lower mean age of first AMI among Iranian people compared to developed countries. This difference can be explained by higher level of social welfare in developed countries in comparison with Iran and also cultural, lifestyles, and preventive health care differences between developed and developing countries. Possibly the socioeconomic levels are also associated with CAD development;44 areas with lower socioeconomic status have shown a higher risk of AMI.21 It may be due to the fact that in the low-income societies, there are more challenges including less access to health care services, poor quality of health services, limited resources for the policies implementation, and insufficient programs to prevent and manage CAD.45 Moreover, fewer tendencies to engage in the health care behaviors, greater proneness to the stress, and the presence of higher rates of cardiovascular risk factors are other reasons that predispose individuals to be susceptible to AMI.33 Therefore, it is accepted that living in less developed regions places the population at higher risk of cardiovascular events.46
The second important finding is the consistency of the lower age of men compared with women for the onset of the AMI. Higher age of onset in women is due to the protective effect of estrogen on the vascular endothelium. This assumption is greatly formed with the increased rate of AMI approximately 10 years after menopause.47,48 However, it is difficult to separate the effects of aging and menopause. Complex mechanisms that affect the risk of CAD by estrogen is not fully understood. The direct effects of estrogen on the cardiovascular system include increased secretion of nitric oxide that causes vessels dilatations, regulates the production of prostaglandins, and inhibits the smooth muscle proliferation.49 Also, at the time of menopause, estrogen reduction causes endothelial dysfunction and increasing in deposition of fat in the arteries. Therefore, this can accelerate the progression of atherosclerosis.40 However, studies about gender differences in the incidence of CAD have addressed these variations in terms of biological factors.50 Less frequent attention has been given to the social, environmental, and societal factors that have potential effects on the occurrence age of MI.51,52 Although CAD is a major cause of AMI in both men and women, plaque features are varied among different women. Recent data suggest the important role of the microscopic vascular disease in the pathophysiology of coronary events. Naturally, the increased rate of AMI in women is multifactorial, and is influenced by age, race, and ethnicity.40 The study conducted in USA showed that in the age range of 75-84 years, AMI in black men reported to be 12.9 persons per 1000 people, yearly. While black women, white men, and white women were ranked for incidence rate of 10.2, 9.1, and 7.8 persons per 1000 people, respectively.53
Limitations: The meta-analysis was done using studies of hospitalized patients; thus, persons who died of AMI before admission to the hospital were not included. Therefore, there is likely an underestimation. The other limitation of the present study was that Iran is a vast territory with diverse geographical regions. So, failure to include each climatic zone may limit the generalizability of the results.
Conclusion
The results of the current study indicate that the mean age of onset of AMI is 59.3 years and it is lower in men than in women. These findings can be used for planning CAD prevention.
Acknowledgments
Researchers greatly appreciate the Vice Chancellor of Research in Mazandaran University of Medical Sciences for financial support (Code IR.MAZUMS.REC.95-2179).
Footnotes
Conflicts of Interest
Authors have no conflict of interests.
REFERENCES
- 1.Sharif Nia A, Haghdoost A, Nazari R, Bahrami N, Soleimani MA, ormand K. Relationship of risk factors and ST segment changes with symptoms of acute coronary syndrome. Koomesh. 2013;15(1):46–53. [Google Scholar]
- 2.Asareh AR, Cheraghi M, Alasti M. Trend of acute myocardial infarction prevalence toward younger ages in Ahvaz. Iran Heart J. 2012;12(4):43–7. [Google Scholar]
- 3.Ahmadi A, Soori H, Mobasheri M, Etemad K, Khaledifar A. Heart failure, the outcomes, predictive and related factors in Iran. J Mazandaran Univ Med Sci. 2014;24(118):180–8. [Google Scholar]
- 4.Naghavi M, Jafari N. Mortality in the 29 provinces of Iran in 2004. Tehran, Iran: Arvij Publications; 2007. In Persian. [Google Scholar]
- 5.Pilgrim T, Heg D, Tal K, Erne P, Radovanovic D, Windecker S, et al. Age-and gender-related disparities in primary percutaneous coronary interventions for acute ST-segment elevation myocardial infarction. PLoS One. 2015;10(9):e0137047. doi: 10.1371/journal.pone.0137047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zheng X, Dreyer RP, Hu S, Spatz ES, Masoudi FA, Spertus JA, et al. Age-specific gender differences in early mortality following ST-segment elevation myocardial infarction in China. Heart. 2015;101(5):349–55. doi: 10.1136/heartjnl-2014-306456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McCabe JM, Kennedy KF, Eisenhauer AC, Waldman HM, Mort EA, Pomerantsev E, et al. Reporting trends and outcomes in ST-segment-elevation myocardial infarction national hospital quality assessment programs. Circulation. 2014;129(2):194–202. doi: 10.1161/CIRCULATIONAHA.113.006165. [DOI] [PubMed] [Google Scholar]
- 8.Aljefree N, Ahmed F. Prevalence of cardiovascular disease and associated risk factors among adult population in the gulf region: A systematic review. Adv Public Health. 2015;2015:235101. [Google Scholar]
- 9.Akhtar N, Kamran SI, Deleu D, D'Souza A, Miyares F, Elsotouhy A, et al. Ischaemic posterior circulation stroke in State of Qatar. Eur J Neurol. 2009;16(9):1004–9. doi: 10.1111/j.1468-1331.2009.02709.x. [DOI] [PubMed] [Google Scholar]
- 10.Hamad A, Hamad A, Sokrab TE, Momeni S, Mesraoua B, Lingren A. Stroke in Qatar: A one-year, hospital-based study. J Stroke Cerebrovasc Dis. 2001;10(5):236–41. doi: 10.1053/jscd.2001.30382. [DOI] [PubMed] [Google Scholar]
- 11.Ghafari S, Hakim SH, Saghebasl E. The 20 years course of risk factors distribution, treatment modalities, complications and in hospital mortality of acute myocardial infarction in Tabriz Shahid Madani Heart Center. Med J Tabriz Univ Med Sci. 2008;30(3):89–95. [Google Scholar]
- 12.Egred M, Viswanathan G, Davis GK. Myocardial infarction in young adults. Postgrad Med J. 2005;81(962):741–5. doi: 10.1136/pgmj.2004.027532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Glover MU, Kuber MT, Warren SE, Vieweg WV. Myocardial infarction before age 36: Risk factor and arteriographic analysis. Am J Cardiol. 1982;49(7):1600–3. doi: 10.1016/0002-9149(82)90234-x. [DOI] [PubMed] [Google Scholar]
- 14.Vaccarino V, Parsons L, Every NR, Barron HV, Krumholz HM. Sex-based differences in early mortality after myocardial infarction. National Registry of Myocardial Infarction 2 Participants. N Engl J Med. 1999;341(4):217–25. doi: 10.1056/NEJM199907223410401. [DOI] [PubMed] [Google Scholar]
- 15.Daneshmandi M, Sadeghi Sharme M, Ebadi A, Neyse F. The effect of earplugs on sleep quality in patients with acute coronary syndrome. Iran J Crit Care Nurs. 2011;4(3):e7096. [Google Scholar]
- 16.Sezavar S, Valizadeh M, Moradi M, Rahbar M. Trend of changes in Age and Gender of Patients Admitted in Rasul-e-Akram Hospital with First Acute Myocardial Infarction from 1998 to 2007. J Ardabil Univ Med Sci. 2010;10(1):29–37. [Google Scholar]
- 17.Okrainec K, Banerjee DK, Eisenberg MJ. Coronary artery disease in the developing world. Am Heart J. 2004;148(1):7–15. doi: 10.1016/j.ahj.2003.11.027. [DOI] [PubMed] [Google Scholar]
- 18.Al-Saif SM, Alhabib KF, Ullah A, Hersi A, Alfaleh H, Alnemer K, et al. Age and its relationship to acute coronary syndromes in the Saudi project for assessment of coronary events (SPACE) registry: The SPACE age study. J Saudi Heart Assoc. 2012;24(1):9–16. doi: 10.1016/j.jsha.2011.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rich MW, Bosner MS, Chung MK, Shen J, McKenzie JP. Is age an independent predictor of early and late mortality in patients with acute myocardial infarction? Am J Med. 1992;92(1):7–13. doi: 10.1016/0002-9343(92)90008-y. [DOI] [PubMed] [Google Scholar]
- 20.Neamatipoor E, Sabri A, Dahi F, Soltanipoor F. Changing risk and demographic factors of myocardial infarction in a decade (1371-1381) in three university hospital. Tehran Univ Med J. 2006;64(3):88–94. [Google Scholar]
- 21.Kjaerulff TM, Ersboll AK, Gislason G, Schipperijn J. Geographical clustering of incident acute myocardial infarction in Denmark: A spatial analysis approach. Spat Spatiotemporal Epidemiol. 2016;19:46–59. doi: 10.1016/j.sste.2016.05.001. [DOI] [PubMed] [Google Scholar]
- 22. Recommendations of a task force of the European society of cardiology and the European resuscitation council on the pre-hospital management of acute heart attacks. Resuscitation. 1998;38(2):73–98. doi: 10.1016/s0300-9572(98)00064-1. [DOI] [PubMed] [Google Scholar]
- 23.Taghipour B, Sharif Nia H, Soleimani MA, Hekmat Afshar M, Shahidi Far S. Comparison of the clinical symptoms of myocardial infarction in the middle-aged and elderly. J Kermanshah Univ Med Sci. 2014;18(5):e74097. [Google Scholar]
- 24.Sharif Nia SH, Haghdoost AA, Soleymani MA, Taghipour B, Alayi B. Comparison of ferritin level in diabetic and non-diabetic patients with acute myocardial infarction. Horizon Med Sci. 2013;19(3):161–71. [Google Scholar]
- 25.Ahmadi A, Soori H, Mehrabi Y, Etemad K, Samavat T, Khaledifar A. Incidence of acute myocardial infarction in Islamic Republic of Iran: a study using national registry data in 2012. East Mediterr Health J. 2015;21(1):5–12. doi: 10.26719/2015.21.1.5. [DOI] [PubMed] [Google Scholar]
- 26.Farshidi H, Rahimi S, Abdi A, Salehi S, Madani A. Factors associated with pre-hospital delay in patients with acute myocardial infarction. Iran Red Crescent Med J. 2013;15(4):312–6. doi: 10.5812/ircmj.2367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gholi F, Zeighami-Mohamadi S, Imani A, Mahdavi A, Torabi M, Abbasi-Valikandi Z. Anthropometric indices in acute myocardial infarction patients and their relationship with some coronary heart disease risk factors. Iranian Journal of Cardiovascular Nursing. 2013;2(1):14–23. [Google Scholar]
- 28.Hadjian K, Jalali F. Age changing patterns of hospitalized patients with acute myocardial infarction in Babol Shahid Beheshti Hospital (1992-2001). J Birjand Univ Med Sci. 2004;11(4):9–15. [Google Scholar]
- 29.Hasanpour A, Hasanpour M, Foruzandeh N, Ganji F, Asadi Noghani AA, Bakhsha F, et al. A survey on quality of life in patients with myocardial infarction, referred to Shahrekord Hagar hospital in 2005. J Shahrekord Univ Med Sci. 2007;9(3):78–84. [Google Scholar]
- 30.Hojat M. Time period between entrance of severe heart stroke patient to hospital and streptokinase injection by nurses. Iran J Crit Care Nurs. 2009;2(1):35–9. [Google Scholar]
- 31.Kazemy T, Sharifzadeh G. Ten-year changes in mortality and risk factors in acute myocardial infarction in Birjand (1994-2003). Horizon Med Sci. 2004;10(3):38–42. [Google Scholar]
- 32.Kiani F, Hesabi N, Arbabisarjou A. Assessment of risk factors in patients with myocardial infarction. Glob J Health Sci. 2015;8(1):255–62. doi: 10.5539/gjhs.v8n1p255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mohammadian A, Baradaran-AttarMoghaddam H, Sarrafzadegan N, AsadiLari M, Roohani M, Allah-Bakhsi F, et al. Secular trend changes in mean age of morbidity and mortality from an acute myocardial infarction during a 10-year period of time in Isfahan and Najaf Abad. J Shahrekord Univ Med Sci. 2013;14(6):101–14. [Google Scholar]
- 34.Beyranvand MR, Lorvand A, Alipour Parsa S, Motamedi MR, Kolahi AA. The quality of life after first acute myocardial infarction. Pajoohandeh. 2011;15(6):264–72. [Google Scholar]
- 35.Momeni M, Salari A, Ghanbari A, Shakiba M. Sex differences in duration of pre-hospital delay in patients with acute myocardial infarction. Payavard Salamat. 2013;7(2):133–42. [Google Scholar]
- 36.Rajaei Behbahani N, Etemad K, Mehrabi Y, Ahmadi A, Hasani J. Difference in clinical manifestations of myocardial infarction between men and women in Iran in 2014-2015. International Journal of Epidemiologic Research. 2016;3(2):106–11. [Google Scholar]
- 37.Rostamzadeh A, Khadem Vatan K, Yekta Z, Mohammadzadeh H. Evaluation of sex effect on mortality in acute myocardial infarction in Talegani hospital in Urmia. Urmia Med J. 2006;17(1):32–5. [Google Scholar]
- 38.De Luca L, Marini M, Gonzini L, Boccanelli A, Casella G, Chiarella F, et al. Contemporary trends and age-specific sex differences in management and outcome for patients with ST-segment elevation myocardial infarction. J Am Heart Assoc. 2016;5(12) doi: 10.1161/JAHA.116.004202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Koek HL, de Bruin A, Gast A, Gevers E, Kardaun JW, Reitsma JB, et al. Incidence of first acute myocardial infarction in the Netherlands. Neth J Med. 2007;65(11):434–41. [PubMed] [Google Scholar]
- 40.Mehta LS, Beckie TM, DeVon HA, Grines CL, Krumholz HM, Johnson MN, et al. Acute myocardial infarction in women: A scientific statement from the American heart association. Circulation. 2016;133(9):916–47. doi: 10.1161/CIR.0000000000000351. [DOI] [PubMed] [Google Scholar]
- 41.Abed MA, Eshah NF, Moser DK. Risk profile of myocardial infarction in young versus older adults. Heart Lung. 2018;47(3):226–30. doi: 10.1016/j.hrtlng.2018.03.002. [DOI] [PubMed] [Google Scholar]
- 42.Dakik HA, Koubeissi Z, Kleiman NS, Nasrallah A, Sawaya J, Gharzuddine W, et al. Acute myocardial infarction: Clinical characteristics, management and outcome in a university medical centre in a developing Middle Eastern country. Can J Cardiol. 2004;20(8):789–93. [PubMed] [Google Scholar]
- 43.Joshi P, Islam S, Pais P, Reddy S, Dorairaj P, Kazmi K, et al. Risk factors for early myocardial infarction in South Asians compared with individuals in other countries. JAMA. 2007;297(3):286–94. doi: 10.1001/jama.297.3.286. [DOI] [PubMed] [Google Scholar]
- 44.Grimaud O, Lapostolle A, Berr C, Helmer C, Dufouil C, Kihal W, et al. Gender differences in the association between socioeconomic status and subclinical atherosclerosis. PLoS One. 2013;8(11):e80195. doi: 10.1371/journal.pone.0080195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Iloabuchi TC, Mi D, Tu W, Counsell SR. Risk factors for early hospital readmission in low-income elderly adults. J Am Geriatr Soc. 2014;62(3):489–94. doi: 10.1111/jgs.12688. [DOI] [PubMed] [Google Scholar]
- 46.Spatz ES, Beckman AL, Wang Y, Desai NR, Krumholz HM. Geographic variation in trends and disparities in acute myocardial infarction hospitalization and mortality by income levels, 1999-2013. JAMA Cardiol. 2016;1(3):255–65. doi: 10.1001/jamacardio.2016.0382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Iorga A, Cunningham CM, Moazeni S, Ruffenach G, Umar S, Eghbali M. The protective role of estrogen and estrogen receptors in cardiovascular disease and the controversial use of estrogen therapy. Biol Sex Differ. 2017;8(1):33. doi: 10.1186/s13293-017-0152-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Yang XP, Reckelhoff JF. Estrogen, hormonal replacement therapy and cardiovascular disease. Curr Opin Nephrol Hypertens. 2011;20(2):133–8. doi: 10.1097/MNH.0b013e3283431921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Miller VM, Duckles SP. Vascular actions of estrogens: Functional implications. Pharmacol Rev. 2008;60(2):210–41. doi: 10.1124/pr.107.08002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Dreyer RP, Smolderen KG, Strait KM, Beltrame JF, Lichtman JH, Lorenze NP, et al. Gender differences in pre-event health status of young patients with acute myocardial infarction: A VIRGO study analysis. Eur Heart J Acute Cardiovasc Care. 2016;5(1):43–54. doi: 10.1177/2048872615568967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bajaj S, Mahajan V, Grover S, Mahajan A, Mahajan N. Gender based differences in risk factor profile and coronary angiography of patients presenting with acute myocardial infarction in north Indian population. J Clin Diagn Res. 2016;10(5):OC05–OC07. doi: 10.7860/JCDR/2016/16512.7725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kumar A, Kaur H, Devi P. Coronary artery disease in women: How does it differ from men? Indian Association of Clinical Medicine. 2011;13(1):43–7. [Google Scholar]
- 53.Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, et al. Heart disease and stroke statistics--2015 update: A report from the American Heart Association. Circulation. 2015;131(4):e29–322. doi: 10.1161/CIR.0000000000000152. [DOI] [PubMed] [Google Scholar]