Abstract
Introduction
In many sub-Saharan African countries, confronting the dual epidemic of HIV and NCDs is a public health priority especially in high HIV burden countries such as South Africa. Evidence shows that poor health as a consequence of NCDs and HIV among the workforce increases absenteeism and leads to decrease in productivity. However, the prevalence of these co-occurring chronic conditions and associated factors is unknown in the educator workforce. Improved understanding has implications for their management and wellbeing of educators. This paper reports the prevalence of selected NCDs and associated factors among HIV positive educators in South Africa using the 2015/6 survey of Educators in Public Schools in South Africa.
Methods
This was a second-generation surveillance undertaken among educators in selected public schools in all nine provinces in South Africa. A multi-stage stratified cluster design with probability proportional to size sampling was used to draw a random sample of schools. Factors associated with presence of NCDs were determined using a multivariate backward stepwise logistic regression analysis.
Results
A total of 1 365 schools were sampled within which 21 495 (85.5%) educators were interviewed. Out of 2691, HIV Positive educators that responded to the questions on NCDs, 36.9% reported having NCDs. The most commonly reported NCDs were high blood pressure (17.4%), and stomach ulcers (13.5%). The increased odds of reporting the presence of NCDs was significantly associated with being female than male [aOR = 1.5: 95% CI (1.1–1.9), p<0.002], age 45 to 54 years [aOR = 1.8: 95% CI (1.4–2.2), p = p<0.001], and age 55 years and older than those 18 to 24 years [aOR = 2.7: 95% CI (1.8–3.9), p<0.001). The decreased odds of reporting the presence of NCDs was significantly associated with not being absent from school for health reasons [aOR = 0.7: 95% CI (0.6–0.9), p = 0.003].
Conclusion
NCDs care and active screening should be an integral part of HIV programmes including interventions such as prevention, treatment, care and support amongst public school educators in SA. The education department will need to invest in health promotion intervention programmes to prevent and mitigate the negative impact of NCDs and HIV on the sector.
Introduction
In sub-Saharan Africa, non-Communicable Diseases (NCDs) in the context of HIV and antiretroviral provision are an emerging public health challenge especially in high HIV burden populations like South Africa [1–7]. As in many sub-Saharan African countries, confronting the dual epidemic of HIV and NCDs is a public health priority. The country has the highest number of people living with HIV (PLHIV) in the world [8], while concurrently the prevalence of NCDs is high and accounts for high morbidity and mortality [1,6,7,9]
Like HIV, NCDs disproportionately affect poor people. In South Africa, this is intertwined with rapid urbanization and unplanned demographic shift leading to risky and unhealthy life styles in the era of HIV [6,10]. Addressing the comorbid non-communicable disease (NCD) and HIV epidemics is important for improved public health outcomes and better economic growth in the country [11,12]. Commonly reported NCDs among PLHIV include cardiovascular diseases, diabetes, cancers, chronic pulmonary diseases, liver disease, chronic kidney disease, hypertension and depression [6–8].
The determinants of NCD comorbidities in HIV/AIDS vary based on the specific NCD considered. Generally, increased age and increased immune suppression, overweight and obesity, social deprivation, and longer duration of exposure to antiretroviral treatments are some of the most common NCD risk factors in HIV infected individuals [6,8]. Unless urgent action is taken against the rising NCD burden among PLHIV, NCDs will add great pressure to the already existing challenge in the fight against HIV [11,12].
Evidence shows that poor health as a consequence of NCDs and HIV among the workforce increase absenteeism and leads to decrease in productivity [13,14]. However, not much is known about the prevalence and risk factors associated with NCDs among HIV positive workforce in the country. This paper reports the prevalence of NCDs and associated factors among HIV positive educators in South Africa using the 2015/6 survey of Educators in Public Schools in South Africa [15]. Understanding prevalence of these co-occurring chronic conditions and associated factors has implications for their management and the wellbeing of educators, which is a critical factor in the planning and resourcing of the education sector in order to achieve quality outcomes.
Methodology
Study design and sample
This study used data collected as part of the 2015/6 national educator’s survey in South Africa; described in detail elsewhere [15]. The survey followed a cross-sectional approach employing second-generation surveillance methods that combined collection of socio-demographic, behavioural data and a blood specimen using a Dried Blood Spot (DBS) collection. The Education Management Information System (EMIS) Master List of educators from the Department of Basic Education (DBE) for 2012 was used as the sampling frame to identify the schools and number of educators at each school. This comprised 25,179 schools with 389,044 educators. HIV prevalence among educators in South Africa was estimated at 12.7% [16]. Assuming an HIV testing response rate of 73%, a minimum sample size of 27,869 educators was estimated to be sufficient to enable the detection of a minimum of 5% change in HIV prevalence in each reporting domain with 80% power at 5% level of significance and assuming a design effect of two due to potential clustering at school level [15].
A multi-stage stratified cluster design with probability proportional to size sampling was used to draw a random sample of schools and all educators. The sample was stratified by all nine provinces and all the 101 educational districts in the country. In each district a sample of schools were randomly selected with probability proportional to size. This implies that schools with a larger number of educators had a higher chance of being selected [15].
In each selected school, all educators present on the day of the survey were eligible to participate in the study. The sample comprised 1380 randomly selected schools which included primary, secondary, combined, and intermediate schools. The study included educators and school management in public schools who were teaching grades R to 12. Participants were employed full-time or part-time with salaries paid either by the state or by school governing bodies [15].
Out of the 1,380 schools sampled, 1,365 were valid and 96.2% agreed to participate in the study. The proportion of non-response was 3.8%, which included refusals (2.6%) and schools not visited or closed down (1.2%). Of these, 16,391 (65.2%) agreed to provide a blood specimen for HIV testing. The proportions of HIV testing non-response included educators who were interviewed but refused to provide a blood sample (20.3%), educators who refused to be interviewed or to provide a blood sample (5.9%), educators who were present at school but not available to participate (8.0%), and educators who were absent from school on the day of data collection (0.6%) [15].
Study instruments
The study used a questionnaire to collect educators’ socio-demographic and behavioural information. The questionnaire collected information on biographical details, residence and mobility, socio-economic status; information on teaching responsibilities and work load of the educator, impact of HIV on educators; workplace absenteeism, morale and job satisfaction; HIV knowledge and sexual behaviour; health status, and self-reported NCDs.
Dried blood spot (DBS)
Consenting educators were tested for HIV using DBS. A blood specimen was obtained using a finger-prick method, by spotting a maximum of five circles onto a Whatman grade 903 Guthrie card and sent to the laboratory for HIV testing. The VironostiKa HIV Uniform II Ag/Ab assay (EIA 1) and Roche Elecys HIV 1 Ag/Ab assay (EIA 2), was used to test for HIV antibodies. All specimens were tested using EIA 1 and those that tested positive using EIA 1 were re-tested using EIA 2. For quality assurance purposes 10 percent of the samples that tested HIV-negative using EIA 1 were re-tested using EIA 2. Any samples producing discordant results with the first two EIAs were submitted to a nucleic acid amplification testing (NAAT) (EIA 3) for final interpretation of discordant samples [15].
Outcome variable
The outcome variable was based on the question “Within the past five years, did a health practitioner (doctor, nurse, etc.) ever tell you that you have any of the following conditions or treated you for such conditions?” diabetes (Yes/No), cancer (Yes/No), high blood pressure (Yes/No), heart disease (Yes/No), stomach ulcers (Yes/No), and lung problems (Yes/No). The responses were then categorized and dichotomised into presence (Yes = 1) and absence (No = 0) of at least one or more NCDs.
Explanatory variables
This included background characteristics such as sex (male and female), age (18 to 24 years, 25 to 34 years, 35 to 44 years, 45 to 54 years and 55 years and older), race (Black African and other race groups), marital status (married and not married), locality type (urban formal-. planned, urban informal-unplanned, rural formal-commercial farms, and rural informal-tribal areas), position in the school (teacher/educator, senior teacher, head of department, education specialist, deputy principal/principal), Educators absent and unhealthy, number of days absent in 2014 (0–4 days, 5–19 days, 20 days and more).
Ethical considerations
Ethical approval for the research protocol was provided by the Human Sciences Research Council Research Ethics Committee (REC: 6/21/05/14). Written informed consent was provided by all educators who agreed to participate. All data were collected anonymously. Data were not linked to any individual or school in the reporting and the discussion of the results.
Statistical analysis
Frequency distribution and percentages were used to summarize the distribution of each NCD and the presence of one or all NCDs was reported by background characteristics of study participants. Pearson chi-square test was used to compare proportional differences in the presence of NCDs by background characteristics. A multivariate logistic regression model using backward stepwise selection method was fitted to determine factors associated with the presence of selected NCDs among HIV positive educators. Probability for removal of variables in the model was set at a p-value of 0.20. Adjusted Odds ratios (aORs) with 95% confidence intervals (CIs) are reported, and p-values ≤ 0.05 were considered statistically significant. Coefficient plots were used to display the results of the final model. All data were analysed using STATA 13.0 (StataCorp, College Station, TX, USA).
Results
Prevalence of individual NCDs
The overall prevalence of self-reported NCDs was 36.9% (95% CI: 34.2–39.6%) out of 2691 HIV positive participants who responded to the NCD questions. Fig 1 shows that of these 64.7% reported no NCD, 26% reported two NCDs and only 2.2% reported three or more NCDs.
Fig 1. The distribution of non-communicable diseases (NCDs) comorbidities among HIV positive educators in South Africa.
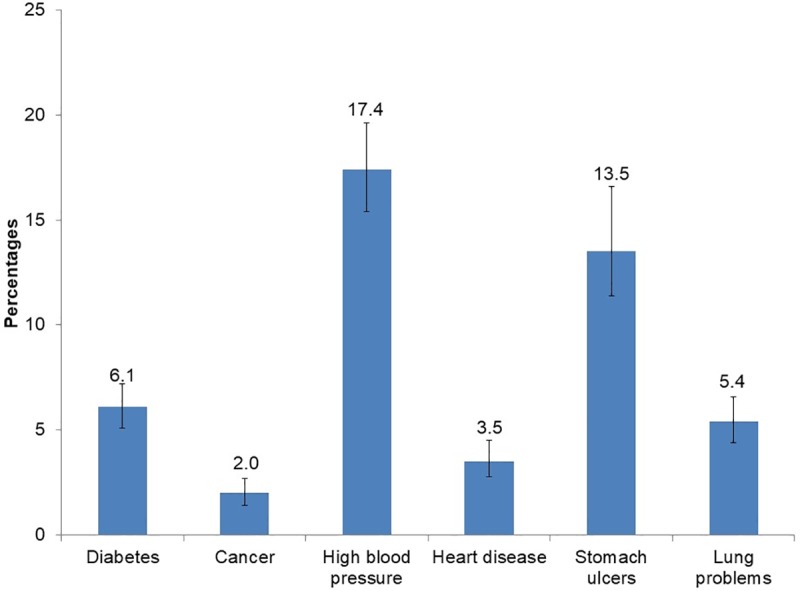
Fig 2 shows that the commonly reported NCDs were high blood pressure (17.4%) and stomach ulcers (13.5%).
Fig 2. Prevalence of reported non-communicable diseases (NCDs) among HIV positive educators in South Africa.
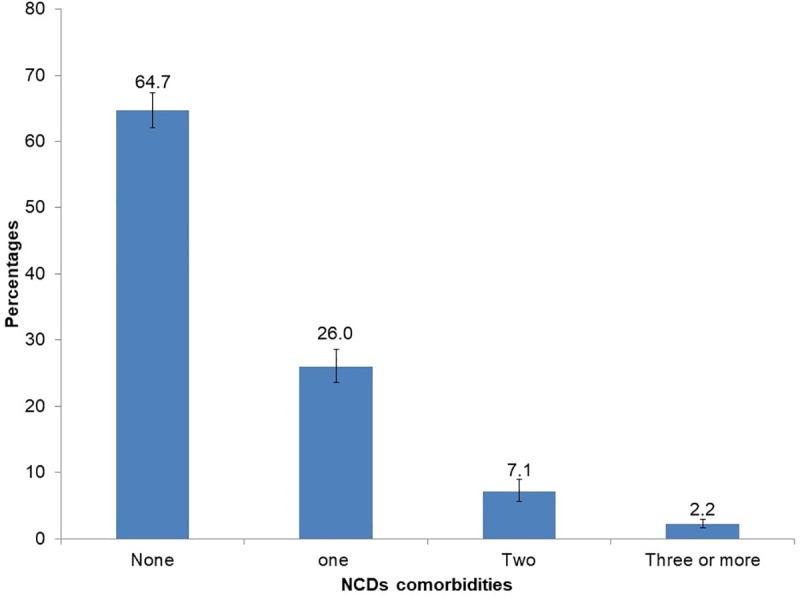
Table 1 shows that the prevalence of diabetes was slightly higher among those 50 years and older (13.1%). The prevalence of high blood pressure was higher among teachers of other race groups (35.2%), those 50 years and older (33.3%) and among teachers in senior positions (26.4%). The prevalence of stomach ulcers were slightly higher among teachers 18–24 years age (22.9%), and those in urban informal schools (21.1%). The prevalence of self-reported Lung / breathing problems, cancers and heart diseases was low.
Table 1. Prevalence of self-reported NCDs by background characteristics among HIV positive educators in South Africa.
| Diabetes | Cancer | High blood pressure | Heart disease | Stomach ulcers | Lung problems | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | N | % | N | % | n | % | n | % | N | % | |
| Sex | ||||||||||||
| Male | 598 | 6.3 | 598 | 1.6 | 598 | 11.5 | 598 | 4.5 | 598 | 7.9 | 599 | 6.3 |
| Female | 2050 | 6 | 2054 | 2.1 | 2052 | 19.3 | 2052 | 3.2 | 2053 | 15.8 | 2052 | 5.1 |
| Age in years | ||||||||||||
| 18 to 24 | 29 | 0 | 29 | 0 | 29 | 0 | 29 | 1.5 | 29 | 22.9 | 29 | 0 |
| 25 to 34 | 422 | 1.5 | 423 | 1.9 | 423 | 7.3 | 422 | 2.9 | 423 | 10.4 | 425 | 3.5 |
| 35 to 44 | 961 | 3.5 | 962 | 2.4 | 963 | 15.1 | 962 | 2.3 | 963 | 17.1 | 961 | 5.7 |
| 45 to 54 | 1053 | 9.1 | 1055 | 1.8 | 1053 | 21 | 1054 | 4.2 | 1053 | 12.4 | 1053 | 5.9 |
| 55+ | 183 | 13.1 | 183 | 1.4 | 182 | 33.3 | 183 | 7.8 | 183 | 10.8 | 183 | 6.9 |
| Race | ||||||||||||
| Black African | 2624 | 6 | 2628 | 2 | 2626 | 17.2 | 2626 | 3.6 | 2627 | 13.9 | 2627 | 5.4 |
| Other | 23 | 9 | 23 | 0 | 23 | 35.2 | 23 | 0 | 23 | 4.6 | 23 | 8.9 |
| Marital status | ||||||||||||
| Married | 956 | 7.5 | 957 | 2.6 | 957 | 18.7 | 956 | 4.6 | 956 | 12.7 | 957 | 6.3 |
| Not Married | 1294 | 4.5 | 1298 | 1.6 | 1297 | 15.7 | 1297 | 2.1 | 1296 | 14.5 | 1296 | 4 |
| Divorced/Separated | 146 | 7.8 | 146 | 3.3 | 146 | 22.2 | 146 | 8.8 | 147 | 15.2 | 147 | 7.1 |
| Widower/Widow | 249 | 7.3 | 248 | 0.6 | 247 | 17.7 | 248 | 3.5 | 249 | 14.1 | 248 | 8.8 |
| Locality type | ||||||||||||
| Urban formal | 581 | 7.2 | 582 | 2.7 | 580 | 16.5 | 582 | 4.4 | 581 | 9.4 | 582 | 5.9 |
| Urban informal | 313 | 7.2 | 314 | 1.9 | 313 | 19.8 | 314 | 4.4 | 313 | 21.1 | 313 | 5.5 |
| Rural formal | 661 | 4.6 | 662 | 1.1 | 663 | 15.8 | 661 | 3 | 661 | 9.9 | 661 | 5.8 |
| Rural informal | 989 | 5.8 | 990 | 2.1 | 990 | 17.8 | 990 | 2.9 | 993 | 16.7 | 992 | 5.1 |
| Position in the school | ||||||||||||
| Teacher/educator | 2191 | 5.7 | 2196 | 2.1 | 2194 | 17.2 | 2194 | 3.6 | 2193 | 14.4 | 2194 | 5.3 |
| Senior teacher | 75 | 5.9 | 76 | 0.8 | 76 | 26.4 | 76 | 6.3 | 76 | 16.3 | 76 | 11.7 |
| Head of department | 232 | 7.9 | 230 | 1.6 | 230 | 15.5 | 230 | 2 | 232 | 8.5 | 231 | 4.7 |
| Education specialist | 9 | 0 | 9 | 0 | 9 | 14.6 | 9 | 3.5 | 9 | 14.8 | 9 | 0 |
| Deputy principal/Principal | 134 | 8.8 | 134 | 1.2 | 134 | 18.6 | 134 | 2.8 | 134 | 11.3 | 134 | 6 |
| Educators absent and unhealthy | ||||||||||||
| Absent | 744 | 6.5 | 745 | 2.8 | 745 | 16.2 | 745 | 4 | 746 | 16.1 | 746 | 7.2 |
| Present | 1882 | 6 | 1884 | 1.7 | 1882 | 17.9 | 1882 | 3.3 | 1882 | 13 | 1882 | 4.8 |
| Number of day absent in 2014 | ||||||||||||
| 0–4 days | 535 | 8.3 | 535 | 2.6 | 536 | 17.4 | 535 | 3.3 | 536 | 8.9 | 534 | 2.5 |
| 5–19 days | 1151 | 5.6 | 1154 | 1.6 | 1154 | 16.5 | 1153 | 3.7 | 1153 | 16.1 | 1152 | 5.4 |
| 20 days and more | 167 | 4.1 | 168 | 7.3 | 167 | 15.9 | 168 | 6.3 | 168 | 14.9 | 169 | 8.7 |
Presence of selected NCDs by background characteristics
Out of a sample of 2691 educators, 26.0% (95% CI: 23.6–28.6) reported one NCD, 7.1% (95% CI: 5.6–9.0) reported two and 2.2% (95% CI: 1.6–2.9) reported more than three NCDs. Table 2 shows that the presence of NCDs was significantly higher among females (40.0%), educators aged 45–54 years (41.1%), those teaching in school located in urban informal areas (48.2%), and those absent 20 days and more (48.8%), respectively.
Table 2. The presence of selected non-communicable diseases (NCDs) by background characteristics among HIV positive educators in South Africa.
| Variables | N | % | 95% CI | p-value |
|---|---|---|---|---|
| Sex | ||||
| Male | 604 | 27.4 | 23.3–31.8 | <0.001 |
| Female | 2087 | 40.0 | 36.8–43.3 | |
| Age in years | ||||
| 18 to 24 | 30 | 25.4 | 10.7–49.1 | 0.001 |
| 25 to 34 | 434 | 27.6 | 22.6–33.2 | |
| 35 to 44 | 973 | 34.4 | 29.0–40.3 | |
| 45 to 54 | 1071 | 41.1 | 37.4–44.9 | |
| 55+ | 183 | 47.8 | 38.9–56.8 | |
| Race | ||||
| Black African | 2666 | 36.8 | 34.1–39.6 | 0.334 |
| Other | 23 | 46.9 | 27.7–67.1 | |
| Marital status | ||||
| Married | 960 | 36.8 | 32.4–41.3 | 0.790 |
| Widower/Widow | 593 | 36.0 | 32.6–39.5 | |
| Locality type | ||||
| Urban formal | 586 | 31.6 | 27.3–36.4 | 0.010 |
| Urban informal | 316 | 48.2 | 37.6–59.0 | |
| Rural formal | 666 | 33.0 | 29.0–37.3 | |
| Rural informal | 999 | 37.0 | 33.0–41.3 | |
| Position in the school | ||||
| Teacher/educator | 2208 | 35.8 | 32.8–39.0 | 0.242 |
| Senior teacher | 77 | 51.8 | 37.7–65.7 | |
| Head of department | 235 | 34.3 | 27.6–41.7 | |
| Education specialist | 9 | 25.9 | 5.8–66.2 | |
| Deputy principal/Principal | 135 | 39.1 | 29.1–50.0 | |
| Educators absent and unhealthy | ||||
| Yes | 750 | 37.9 | 33.8–42.1 | 0.461 |
| No | 1897 | 35.8 | 32.5–39.3 | |
| Number of day absent in 2014 | ||||
| 0–4 days | 541 | 34.5 | 29.5–39.8 | 0.021 |
| 5–19 days | 1159 | 35.1 | 31.2–39.2 | |
| 20 days and more | 191 | 48.8 | 39.8–57.9 |
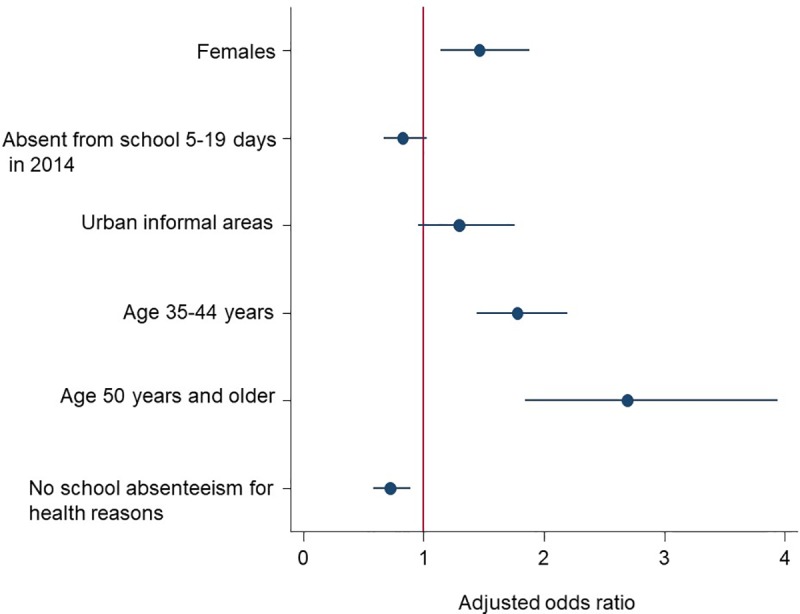
Multivariate model
Fig 3 shows the results of the multivariate stepwise backward logistic regression model between the presence of selected NCDs and explanatory variables. The increased odds of reporting the presence of NCDs was significantly associated with being female than male [aOR = 1.5: 95% CI (1.1–1.9), p<0.002], age 45 to 54 years [aOR = 1.8: 95% CI (1.4–2.2), p<0.001], and 55 years and older than those 18 to 24 years old [aOR = 2.7: 95% CI (1.8–3.9), p<0.001). While the decreased odds of reporting the presence of NCDs was significantly associated with not being absent from school for health reasons [aOR = 0.7: 95% CI (0.6–0.9), p = 0.003].
Fig 3. Coefficient plots of multivariate stepwise backward logistic regression model of factors associated with reported non-communicable diseases (NCDs) among HIV positive educators in South Africa.
Discussion
The study revealed that more than a third of HIV positive educators had NCDs. The more prevalent NCDs were high blood pressure and stomach ulcers. These were also the most commonly reported NCDs in the 2004/5 South African Public Schools Survey [16]. This suggests the intersection of NCDs with HIV has remained unchanged in the past ten years in this population. This linkage highlights the need to integrate responses for HIV and NCDs among educators in this sector.
The findings showed that women were more likely to report NCDs than men. This may be a reflection of the different health seeking behaviour by women when compared to men. Nevertheless, studies have advanced that women's susceptibility to NCDs is linked to physical inactivity and obesity, which are reported to be higher among women than the men [6,7,17,18]. This suggests that successful management of both HIV and NCDs should involve strategic screening for NCDs and promotion of healthy behaviours for all educators in the sector.
The presence of selected NCDs was associated with rise in age. Generally, advanced age is associated with low physical activity and poor health [6,17–20]. Increased access to anti-retroviral treatment has turned HIV in to a chronic disorder. HIV positive people live longer. The increasing age comes with an increased risk of NCD comorbidity [6, 20]. There is therefore a need to control and prevent NCDs and their common risk factors among educators living with HIV.
Similar to current findings in the 2004/5 South African Public Schools Survey HIV and NCDs were observed to contribute to poor health and absenteeism [16]. Given the fact that NCDs in the same way as HIV affects health directly and indirectly [3], both can hinder the ability of educators to perform their duties. Since the joint burden may have major adverse effects on the educator wellbeing and performance. Prevention and management of HIV infection and NCDs through health promotion, treatment and regular monitoring of treatment outcomes is vital for the education sectors.
Limitations
The prevalence NCDs may be underestimated by self-reporting and not considering other NCDs. Furthermore, it have would have been better to consider each NCD as a single outcome and not combined them. However, we were also limited by the small numbers hence the pooled analysis. There may also be other potential unmeasured risk factors and / or confounders that were not taken into account in this analysis. Furthermore, the cross-sectional nature of the survey does not allow for proper inference of the causality between NCDs and explanatory variables in the context of HIV among educators. Nevertheless, this study provides the evidence base on the prevalence of NCDs and their associated risk factors among HIV positive educators using a nationally representative sample. This is useful in planning and rolling out the NCDs active screening as an integral part of the HIV programmes including interventions such as prevention, treatment and care amongst public school educators in SA.
Conclusion
The study revealed that the presence of NCDs was relatively high. The commonly reported NCDs were high blood pressure and stomach ulcers. The analysis also identified specific background characteristics as predisposing to NCDs. Furthermore, the findings suggest a connection between absenteeism and presence of NCDs among HIV positive educators. Therefore, regular monitoring of NCD and associated risk factors is of paramount importance among HIV positive educators. There is a need for more research to address the complex interaction between HIV and NCDs in the workforce in order to inform policy and interventions.
Supporting information
(DTA)
Data Availability
All relevant data are available within the paper and its Supporting Information files.
Funding Statement
This work received support from The Global Fund to Fight AIDS, Tuberculosis and Malaria through Networking HIV and AIDS Community of Southern Africa (NACOSA) on behalf of The South African National AIDS Council (SANAC) and Department of Basic Education (DBE), and the Human Sciences Research Council (HSRC). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Hofman K. Non-communicable diseases in South Africa: A challenge to economic development. SAMJ. 2014; 104(10):01. [DOI] [PubMed] [Google Scholar]
- 2.UNAIDS. Chronic care of HIV and non-communicable diseases: How to leverage the HIV experience. Joint United Nations Programme on HIV/AIDS, Geneva; 2011. [Google Scholar]
- 3.Sogarwal R, Mehra S. Approaches to Address NCD among PLHIV in Low and Middle Income Counties. J AIDS Clin Res. 2015; 6(472):2. [Google Scholar]
- 4.Narayan KM, Miotti PG, Anand NP, Kline LM, Harmston C, Gulakowski R, et al. HIV and non-communicable disease comorbidities in the era of antiretroviral therapy: a vital agenda for research in low- and middle-income country settings. J Acquir Immune Defic Syndr. 2014; 67:S2–S7. 10.1097/QAI.0000000000000267 [DOI] [PubMed] [Google Scholar]
- 5.Chhoun P, Tuot S, Harries AD, Kyaw NT, Pal K, Mun P, et al. High prevalence of non-communicable diseases and associated risk factors amongst adults living with HIV in Cambodia. PloS one. 2017; 12(11):e0187591 10.1371/journal.pone.0187591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Oni T, Youngblood E, Boulle A, McGrath N, Wilkinson RJ, Levitt NS. Patterns of HIV, TB, and non-communicable disease multi-morbidity in peri-urban South Africa-a cross sectional study. BMC infectious diseases. 2015; 15(1):20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.van Heerden A, Barnabas RV, Norris SA, Micklesfield LK, van Rooyen H, Celum C. High prevalence of HIV and non‐communicable disease (NCD) risk factors in rural KwaZulu‐Natal, South Africa. JIAS. 2017; 20(2):e25012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Simbayi LC, Zuma K, Zungu N, Moyo S, Marinda E, Jooste S, et al. South African National HIV Prevalence, Incidence, Behaviour and Communication Survey; 2017. Cape Town: HSRC Pres; in press. [Google Scholar]
- 9.Levitt NS, Steyn K, Dave J, Bradshaw D. Chronic non-communicable diseases and HIV-AIDS on a collision course: relevance for health care delivery, particularly in low-resource settings—insights from South Africa. Am J Clin Nutr. 2019; 94(6):1690S–6S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.WHO. Commission on the Social Determinants of Health. Geneva: World Health Organization, 2008. [Google Scholar]
- 11.Deeks SG, Lewin SR, Havlir DV. The end of AIDS: HIV infection as a chronic disease. Lancet. 2013; 382 (9903): 1525–33. 10.1016/S0140-6736(13)61809-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Smit M, Olney J, Ford NP, Vitoria M, Gregson S, Vassall A, et al. The growing burden of non-communicable disease among persons living with HIV in Zimbabwe. AIDS. 2018. 27; 32(6):773 10.1097/QAD.0000000000001754 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kolbe-Alexander T, Greyling M, Da Silva R, Milner K, Patel D, et al. The relationship between workplace environment and employee health behaviours in a South African workforce. J Occup Environ Med. 2014; 56(10):1094–9. 10.1097/JOM.0000000000000236 [DOI] [PubMed] [Google Scholar]
- 14.Guariguata L, de Beer I, Hough R, Mulongeni P, Feeley FG, de Wit TF. Prevalence and knowledge assessment of HIV and non-communicable disease risk factors among formal sector employees in Namibia. PloS one. 2015; 10(7):e0131737 10.1371/journal.pone.0131737 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zuma K, Simbayi LC, Rehle T, Mbelle N, Zungu NP, Mthembu J et al. The Health of Educators in Public Schools in South Africa. Cape Town: Human Sciences; 2016. [Google Scholar]
- 16.Shisana O, Peltzer K, Zungu-Dirwayi N, Louw J. The health of our educators: a focus on HIV/AIDS in South African public schools, 2004/5 survey. Cape Town: Human Sciences; 2005. [Google Scholar]
- 17.Phaswana-Mafuya N, Peltzer K, Chirinda W, Musekiwa A, Kose Z. Socio-demographic predictors of multiple non-communicable disease risk factors among older adults in South Africa. Glob Health Action. 2013; 6(1):20680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Minicuci N, Biritwum RB, Mensah G, Yawson AE, Naidoo N, Chatterji S, Kowal P. Socio-demographic and socio-economic patterns of chronic non-communicable disease among the older adult population in Ghana. Glob Health Action. 2014; 7(1):21292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wandera SO, Ntozi J, Kwagala B. Prevalence and correlates of disability among older Ugandans: evidence from the Uganda National Household Survey. Glob Health Action. 2014; 7(1):25686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Negin J, Martiniuk A, Cumming RG, Naidoo N, Phaswana-Mafuya N, Madurai L, Williams S, Kowal P. Prevalence of HIV and chronic comorbidities among older adults. AIDS. 2012; 26(01):S55. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DTA)
Data Availability Statement
All relevant data are available within the paper and its Supporting Information files.


