Abstract
This study investigated the effects of a contoured, prefabricated foot orthosis and a flat insole on plantar pressure and tibial acceleration while walking in defence boots. Twenty-eight adults walked along an 8-metre walkway in a: (i) defence boot (control condition), (ii) defence boot with a flat insole, and (iii) defence boot with a contoured foot orthosis. Plantar pressure data were collected using the pedar-X in-shoe system and tibial accelerations were measured with an accelerometer. In relation to plantar pressure under the rearfoot, the contoured foot orthosis, compared to the defence boot, decreased peak pressure and maximum force, and increased contact area. Under the medial midfoot, the contoured foot orthosis and flat insole increased peak pressure, maximum force and contact area. Under the medial forefoot, the contoured foot orthosis and flat insole increased maximum force. Under the lateral forefoot, the contoured foot orthosis and flat insole increased contact area, with the flat insole also increasing maximum force. In relation to tibial acceleration, the contoured foot orthosis, compared to the defence boot, decreased tibial peak positive acceleration. These findings provide novel biomechanical evidence for the effects of contoured foot orthoses in defence boots.
Introduction
Lower limb overuse injuries are common among physically active defence personnel1–3, with the incidence reported to range from 10 to 47% during initial defence training2,4. Common lower limb overuse injuries include medial tibial stress syndrome, patellofemoral pain, Achilles tendinopathy, plantar fasciitis, and stress fractures1,5–8. Numerous risk factors for lower limb overuse injuries during defence training have been identified, including older age, lower fitness levels, previous injury and some lower limb biomechanical variables2,9–11. Broadly, lower limb overuse injuries are proposed to develop in tissues that are exposed to loads that are greater than what the tissues are prepared for12,13. Accordingly, interventions that decrease tissue loads or increase the body’s tolerance to training loads are of interest to the defence forces.
Defence boots are primarily designed to protect the foot and ankle from direct impact, extreme environmental conditions, and acute musculoskeletal injuries14. However, defence boots have long been considered a potential contributing factor for overuse injury15. Defence boots are often heavy while also having a standard shape and design, which may lead to poor fit and discomfort15. In addition, laboratory-based studies have demonstrated that wearing defence boots can alter lower limb kinematics and also have deleterious effects on lower limb tissue loads and impact forces when compared to athletic footwear14,16.
Making substantial changes to defence boot design or using alternative footwear is not always feasible in the defence context. As such, shock-absorbing insoles or foot orthoses are often used in defence boots to improve comfort17, reduce impact forces18, and to alter lower limb function14,16–18. A recent systematic review concluded that prefabricated foot orthoses, but not shock-absorbing insoles, can decrease the incidence of overall lower limb injuries and lower limb stress fractures during initial defence training19. Although promising, caution is required when interpreting these findings as the clinical trials included in the review were generally of low to moderate methodological quality. Nevertheless, a high quality randomised trial published after the systematic review mentioned above also found that prefabricated foot orthoses can reduce the rate of common lower limb overuse injuries by 34%20. The specific mechanism by which foot orthoses prevent injury is not fully established, although they have been shown to alter plantar pressure distribution, muscle activity and kinematics of the lower limb when used in conventional footwear21. However, at present, there is limited research on whether these same biomechanical effects also occur when foot orthoses are used in defence boots.
The primary aim of this study was to evaluate the effects of a contoured, prefabricated foot orthosis on plantar pressure and tibial acceleration while walking in defence boots. The secondary aim of this study was to evaluate the effects of the foot orthosis on footwear comfort. In doing so, our objective was to provide insights into the possible mechanisms by which contoured foot orthoses may reduce the risk of lower limb overuse injury in defence personnel.
Methods
This study is reported in accordance with The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement22.
Participants
The study was approved by the La Trobe University Human Ethics Committee (S15/202) and written informed consent was obtained from all participants. All experiments were performed in accordance with the World Medical Association’s Declaration of Helsinki. Twenty-eight adult participants from a local university were recruited between February and October 2017. Participants were excluded from the study if they had a history of foot surgery, an existing lower limb injury, or used any form of foot orthosis or shock-absorbing insole. Participant characteristics and anthropometric measures, including the Foot Posture Index (FPI-6)23,24 and navicular drop25, are displayed in Table 1.
Table 1.
Characteristics of participants (N = 28).
| Variable | Mean (SD) | Range |
|---|---|---|
| Age (years) | 24.9 (5.3) | 20.6 to 42.8 |
| Sex, n (%) male | 17 (60.7) | — |
| Height (cm) | 175.0 (8.1) | 162.0 to 190.0 |
| Weight (kg) | 75.6 (11.2) | 50.0 to 100.0 |
| Body mass index (kg/m2) | 24.7 (2.9) | 18.8 to 32.9 |
| Waist circumference (cm) | 83.7 (7.6) | 67.0 to 100.0 |
| Hip circumference (cm) | 100.3 (4.8) | 92.0 to 111.0 |
| Waist to hip circumference ratio | 0.83 (0.05) | 0.73 to 0.94 |
| Foot posture† | 1.96 (1.9) | −1 to 6 |
| Supinated, n (%) | 1 (3.6) | — |
| Normal, n (%) | 24 (85.7) | — |
| Pronated, n (%) | 4 (14.3) | — |
| Navicular drop (mm)25 | 5.14 (3.7) | 0 to 13 |
| Ankle dorsiflexion, knee extended (degrees)56 | 44.6 (10.8) | 31 to 63 |
| Ankle dorsiflexion, knee flexed (degrees)57 | 46.4 (11.6) | 32 to 64 |
Sample size
An a priori sample size calculation estimated that 28 participants were required to provide 80% power to detect a small effect size (0.25) for the three footwear-insole conditions, with statistical significance for hypothesis tests set at p < 0.0526.
Contoured foot orthoses and flat insoles
A contoured, prefabricated foot orthosis and a flat insole were investigated in this study. The contoured foot orthosis and flat insole were manufactured by the same company (Foot Science International, Christchurch, New Zealand), were full-length and were made from the same material (firm single density, 140 kg/m3 closed cell polyethylene foam). The foot orthosis was contoured and varied in thickness, namely it was thicker in the region of the medial arch and around the periphery of the heel, whereas the flat insole had a uniform thickness of 3 mm27.
Procedures
All data were collected at a single session at the same university from which the participants were recruited. Participants were advised that three footwear-insole conditions were being investigated during the study. The following three conditions (Fig. 1) were tested in random order (Research Randomizer, www.randomizer.org):
Figure 1.

The three experimental conditions. Left to right: (i) Oliver defence boot; (ii) flat insole; (iii) contoured foot orthosis.
(i) Defence boot only (control)
(ii) Defence boot with flat insole
(iii) Defence boot with contoured foot orthosis
Each participant had a pair of the shoe insoles fitted to standard-issue Royal Australian Navy defence boots (Oliver Footwear® Style 66–395 230MM (9″) Lace up Structural Firefighter Boot, Ballarat, Australia). The shoe insoles were heat moulded to participants’ feet while wearing the boots. All participants wore standardised thin cotton socks (Bonds®, Kew, Melbourne, Australia) during testing. To maintain participant blinding, the boots were removed from the participants’ sight while the insoles were placed in them. The investigators were not blinded due to the difficulty in concealing the conditions, however this was not considered a limitation as the plantar pressure and accelerometer equipment provides objective data.
Pressures beneath the foot were measured with the pedar®-X in-shoe system, which has been shown to be a valid, reliable and accurate measure of plantar pressure28,29. The pedar®-X insoles are thin, flexible and comprise 99 capacitive sensors. The pedar®-X insoles were calibrated using the trublu® calibration device prior to data collection. Data were recorded at a frequency of 100 Hz. The pedar®-X insoles were placed within the boot, between the foot and the shoe insoles. Tibial accelerations were measured with a lightweight tri-axial accelerometer (measurement range: ± 16 g) (Biometrics Ltd, Newport, United Kingdom). The accelerometer was firmly secured to the anteromedial aspect of the participants’ right distal tibia, which provides an accurate measure of tibial acceleration30,31, and which has been shown to be highly correlated to vertical ground reaction forces experienced during gait32,33. Tibial accelerations were sampled at 1080 Hz (see Fig. 2).
Figure 2.
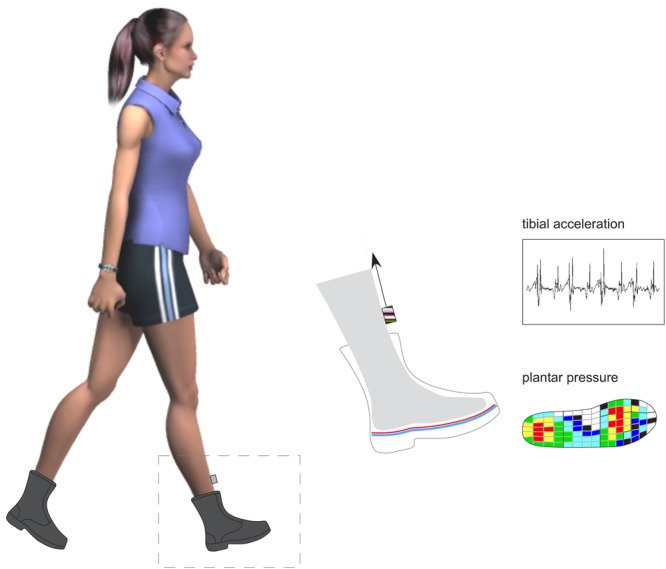
Plantar pressure and tibial acceleration data collection procedure.
After a familiarisation period of approximately 5 minutes in each condition, participants were timed as they completed 4 overground walking trials along an 8-metre walkway. Plantar pressure and tibial acceleration data were collected as participants walked at a comfortable self-determined speed. All trials were within 5% of the recorded walking time of the first trial34.
Following data collection for each condition, and while still blinded, participants rated the shoe comfort on a 100 mm visual analogue scale, with the left end (0 mm) labelled ‘not comfortable at all’ and the right end (100 mm) labelled ‘most comfortable imaginable’.
Data analysis
The primary variables were: (i) plantar pressure (peak pressure, maximum force and contact area) under the rearfoot, midfoot and forefoot, and (ii) tibial peak positive acceleration. The secondary variables were foot contact time and footwear comfort.
For the plantar pressure and tibial acceleration data, only the middle 4 steps from each trial were included in the analysis. For each condition, a total of 16 steps (i.e. 4 steps from 4 trials) per participant were included in the analysis. To meet the independence assumption of statistical analysis, only data from the right limb were used35.
Plantar pressure data were analysed using the Novel-win program (version 20.3.30). Novel percent masks were applied to each individual footprint36,37. The rearfoot mask consisted of the proximal 30% of the foot length, the midfoot mask consisted of the middle 30% of the foot length and the forefoot mask consisted of the distal 40% of the foot length. The midfoot was further divided into lateral and medial halves. The forefoot mask consisted of the medial forefoot (1st metatarsophalangeal joint region), lateral forefoot (including the 2nd through 5th metatarsophalangeal joint regions) and hallux. Acceleration data were initially filtered using a recursive low-pass Butterworth filter38. The acceleration data were then analysed using Python open-source software (Python Software Foundation, https://www.python.org/). An inbuilt function in the software was used to detect the tibial peak positive accelerations, defined as the highest positive acceleration. To achieve this, for each participant, the filtered and non-filtered data were visually inspected and the optimum cut off frequency was determined. This ranged between 100 to 200 Hz across all participants. The minimum distance between peaks was set at 800 frames for all participants.
Statistical analysis was performed using IBM SPSS Statistics 25 (IBM Corporation, Armonk, NY) computer program. The distribution of data were checked for normality. Some variables were positively skewed and therefore required logarithmic transformation prior to inferential analysis. A repeated measures analysis of variance (ANOVA) with Least Significant Difference (LSD) post hoc tests was used for comparison of the means between test conditions. Statistical significance for hypothesis tests was set at the conventional level of p < 0.05. Effect sizes for all significant main effects between the three conditions were calculated using Partial Eta Squared (ηp2), and were interpreted as small (0.00 to <0.06), medium (0.06 to <0.14), and large (>0.14)39. Effect sizes were also reported for all significant pairwise comparisons using Cohen’s d40, and were interpreted as negligible (0 to <0.15), small (0.15 to <0.40), medium (0.40 to <0.75), large (0.75 to <1.10), and very large (>1.10).
Results
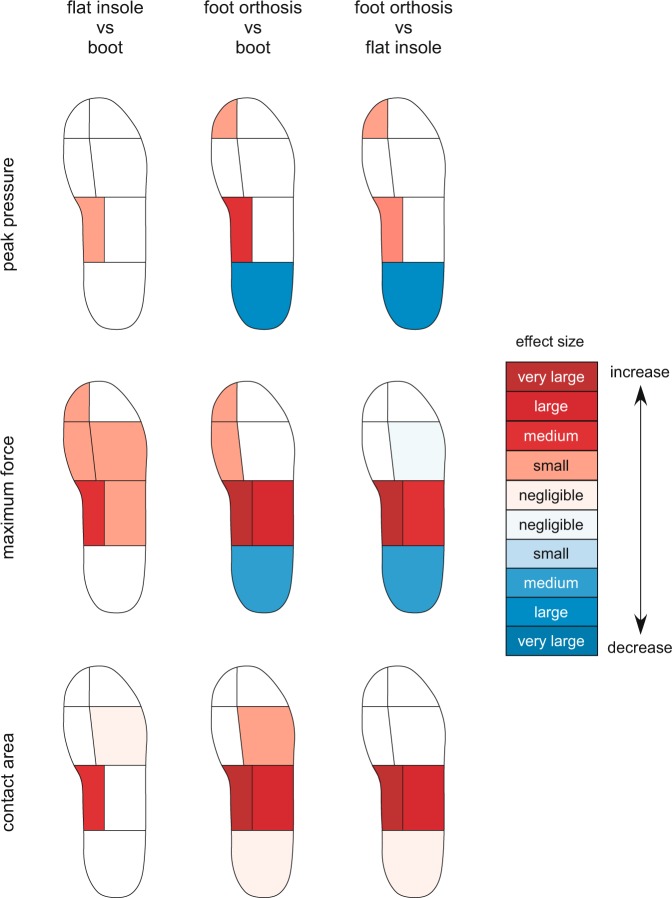
Twenty-eight adult participants (17 men and 11 women) were recruited. The mean walking speed across all trials was 4.49 (±0.56) km/h (range 3.10 to 5.66 km/h). There were no significant differences in total foot contact time between the boot only condition (727.2 ± 61.6 ms), the flat insole (733.2 ± 70.9 ms, p = 0.208) and the foot orthosis (731.2 ± 64.0 ms, p = 0.233). There were a number of significant differences observed in plantar pressures (see Table 2 and Fig. 3) and tibial acceleration (see Table 3) between the three footwear-insole conditions being investigated.
Table 2.
Comparisons of peak pressure, maximum force and contact area for each condition (N = 28).
| Condition | Mean (SD) | Peak pressure (kPa) | Maximum force (N) | Mean (SD) | Contact area (cm2) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| % change | Effect size (d) | P-value | Mean (SD) | % change | Effect size (d) | P-value | % change | Effect size (d) | P-value | |||
| Rearfoot | ||||||||||||
| Boot only (control) | 214.1 (40.0) | n/a | n/a | n/a | 545.3 (117.7) | n/a | n/a | n/a | 43.5 (6.2) | n/a | n/a | n/a |
| Flat insole | 213.9 (38.1) | 0 | −0.01 | 0.953 | 554.9 (126.6) | +2 | 0.08 | 0.193 | 43.5 (6.1) | 0 | 0.00 | 0.971 |
| Foot orthosis | 172.5 (37.9) | −19 | −1.07 | <0.001*# | 497.9 (116.6) | −9 | −0.40 | < 0.001*# | 43.9 (6.2) | + 1 | 0.06 | 0.010*# |
| Medial midfoot | ||||||||||||
| Boot only (control) | 93.3 (42.4) | n/a | n/a | n/a | 14.2 (10.1)† | n/a | n/a | n/a | 4.0 (2.3) | n/a | n/a | n/a |
| Flat insole | 108.4 (49.1) | +16 | 0.33 | 0.016* | 19.6 (11.3)† | +38 | 0.50 | <0.001* | 5.3 (3.1) | +33 | 0.48 | 0.002* |
| Foot orthosis | 128.1 (57.1) | +37 | 0.69 | <0.001*# | 47.4 (15.9)† | +334 | 2.49 | <0.001*# | 14.7 (3.4) | +368 | 3.69 | <0.001*# |
| Lateral midfoot | ||||||||||||
| Boot only (control) | 115.8 (29.0)† | n/a | n/a | n/a | 115.1 (31.5) | n/a | n/a | n/a | 28.3 (3.4) | n/a | n/a | n/a |
| Flat insole | 115.9 (31.6)† | 0 | 0.00 | 0.865 | 125.5 (44.2) | +9 | 0.27 | 0.014* | 27.7 (5.7) | −2 | −0.13 | 0.330 |
| Foot orthosis | 113.9 (32.1)† | −2 | −0.06 | 0.508 | 143.9 (43.2) | +25 | 0.76 | <0.001*# | 31.6 (4.4) | +12 | 0.84 | <0.001*# |
| Medial forefoot | ||||||||||||
| Boot only (control) | 253.9 (58.5) | n/a | n/a | n/a | 218.3 (65.2) | n/a | n/a | n/a | 17.2 (2.6) | n/a | n/a | n/a |
| Flat insole | 271.5 (73.2) | +7 | 0.27 | 0.033 | 237.6 (74.1) | +9 | 0.28 | <0.001* | 17.6 (2.6) | +2 | 0.15 | 0.058 |
| Foot orthosis | 279.6 (88.8) | +10 | 0.34 | 0.042 | 230.7 (72.9) | +6 | 0.18 | 0.017* | 17.6 (2.6) | +2 | 0.15 | 0.038 |
| Lateral forefoot | ||||||||||||
| Boot only (control) | 249.5 (62.8)† | n/a | n/a | n/a | 371.5 (99.5) | n/a | n/a | n/a | 33.9 (4.9) | n/a | n/a | n/a |
| Flat insole | 241.3 (53.4)† | −3 | −0.14 | 0.127 | 392.2 (101.0) | +6 | 0.21 | 0.001* | 34.6 (4.9) | +2 | 0.14 | 0.012* |
| Foot orthosis | 238.8 (63.1)† | −4 | −0.17 | 0.047 | 377.6 (109.6) | +2 | 0.06 | 0.449# | 34.4 (4.8) | +1 | 0.10 | 0.038* |
| Hallux | ||||||||||||
| Boot only (control) | 295.2 (117.4) | n/a | n/a | n/a | 113.6 (49.3) | n/a | n/a | n/a | 7.4 (1.3) | n/a | n/a | n/a |
| Flat insole | 298.4 (90.4) | +1 | 0.03 | 0.774 | 123.9 (46.8) | +9 | 0.21 | 0.004* | 7.6 (1.6) | +3 | 0.14 | 0.438 |
| Foot orthosis | 322.4 (105.8) | +9 | 0.24 | 0.026*# | 121.8 (48.4) | +7 | 0.17 | 0.034* | 7.4 (1.5) | 0 | 0.00 | 0.888 |
Note: % change is relative to the boot only-control condition. †Data transformed prior to determining significance. *Mean differences significant at the 0.05 level compared to the boot only condition. #Mean differences significant at the 0.05 level compared to the flat insole condition.
Figure 3.
Effect size of changes in peak pressure, maximum force and contact area for each experimental condition compared to each other (N = 28).
Table 3.
Peak positive tibial acceleration (g) for each condition (N = 28).
| Condition | Mean (SD) | % change | Effect size (d) | P-value |
|---|---|---|---|---|
| Boot only (control) | 2.22 (0.82)† | n/a | n/a | n/a |
| Flat insole | 2.25 (0.89)† | +1.4 | 0.04 | 0.882 |
| Foot orthosis | 2.07 (0.75)† | −6.8 | −0.19 | 0.018*# |
Note: % change is relative to the boot only-control condition. †Data transformed prior to determining significance. *Mean difference significant at the 0.05 level compared to the boot only condition. #Mean difference significant at the 0.05 level compared to the flat insole condition.
Plantar pressure
Rearfoot
There was a significant effect for peak pressure (Wilk’s Lambda = 0.13, F (2, 26) = 86.10, p < 0.001; effect size large, ηp2 = 0.87, 90% confidence interval [CI] 0.76 to 0.90), maximum force (Wilk’s Lambda = 0.40, F (2, 26) = 19.58, p < 0.001; effect size large, ηp2 = 0.60, 90% CI 0.35 to 0.70) and contact area (Wilk’s Lambda = 0.75, F (2, 26) = 4.29, p = 0.025; effect size large, ηp2 = 0.25, 90% CI 0.02 to 0.42) between the three conditions. Compared to the boot only condition, the contoured foot orthosis provided significant effects on peak pressure (−19%, p < 0.001, effect size large; d = −1.07), maximum force (−9.0%, p < 0.001, effect size medium; d = −0.40) and contact area (+1%, p = 0.010, effect size negligible; d = 0.06), while the flat insole provided no significant effect on these variables. Compared to the flat insole, the contoured foot orthosis provided significant effects on peak pressure (−19%, p < 0.001, effect size large; d = −1.09), maximum force (−10%, p < 0.001, effect size medium; d = −0.47) and contact area (+1%, p = 0.018, effect size negligible; d = 0.06).
Medial midfoot
There was a significant effect for peak pressure (Wilk’s Lambda = 0.55, F (2, 26) = 10.53, p < 0.001; effect size large, ηp2 = 0.45, 90% CI 0.17 to 0.59), maximum force (Wilk’s Lambda = 0.13, F (2, 26) = 85.55, p < 0.001; effect size large, ηp2 = 0.87, 90% CI 0.76 to 0.90) and contact area (Wilk’s Lambda = 0.07, F (2, 26) = 169.87, p = 0.001; effect size large, ηp2 = 0.93, 90% CI 0.87 to 0.95) between the three conditions. Compared to the boot only condition, the contoured foot orthosis provided significant increases on peak pressure (+37%, p < 0.001, effect size medium; d = 0.69), maximum force (+334%, p < 0.001, effect size very large; d = 2.49) and contact area (+368%, p < 0.001, effect size very large; d = 3.69). The flat insole also provided significant increases on peak pressure (+16%, p = 0.016, effect size small; d = 0.33), maximum force (+38%, p < 0.001, effect size medium; d = 0.50) and contact area (+33%, p = 0.002, effect size medium; d = 0.48). Compared to the flat insole, the contoured foot orthosis provided significant increases on peak pressure (+18%, p < 0.001, effect size small; d = 0.37), maximum force (+242%, p < 0.001, effect size very large; d = 2.02) and contact area (+277%, p < 0.001, effect size very large; d = 2.89).
Lateral midfoot
There was a significant effect for maximum force (Wilk’s Lambda = 0.31, F (2, 26) = 28.77, p < 0.001; effect size large, ηp2 = 0.69, 90% CI 0.47 to 0.77) and contact area (Wilk’s Lambda = 0.46, F (2, 26) = 15.04, p = 0.001; effect size large, ηp2 = 0.54, 90% CI 0.27 to 0.66) between the three conditions. Compared to the boot only condition, the contoured foot orthosis provided significant increases on maximum force (+25%, p < 0.001, effect size large; d = 0.76) and contact area (+12%, p < 0.001, effect size large; d = 0.84). The flat insole provided a significant increase on maximum force (+9%, p = 0.014, effect size small; d = 0.27), while having no significant effect on contact area (p = 0.330). Compared to the flat insole, the contoured foot orthosis provided significant increases on maximum force (+15%, p < 0.001, effect size medium; d = 0.42) and contact area (+14%, p < 0.001, effect size large; d = 0.77).
Medial forefoot
There was a significant effect for maximum force (Wilk’s Lambda = 0.61, F (2, 26) = 8.43, p = 0.002; effect size large, ηp2 = 0.39, 90% CI 0.12 to 0.54) between the three conditions. Compared to the boot only condition, the contoured foot orthosis (+6%, p = 0.017, effect size small; d = 0.18) and flat insole provided a significant increase on maximum force (+9%, p < 0.001, effect size small; d = 0.28).
Lateral forefoot
There was a significant effect for maximum force (Wilk’s Lambda = 0.56, F (2, 26) = 10.41, p < 0.001; effect size large, ηp2 = 0.44, 90% CI 0.17 to 0.58) and contact area (Wilk’s Lambda = 0.79, F (2, 26) = 3.48, p = 0.046; effect size large, ηp2 = 0.21, 90% CI 0.02 to 0.38) between the three conditions. Compared to the boot only condition, the contoured foot orthosis provided a significant increase on contact area (+1%, p = 0.038, effect size small; d = 0.10), while having no significant effect on maximum force (p = 0.449). The flat insole provided significant increases on maximum force (+6%, p = 0.001, effect size small; d = 0.21) and contact area (+2%, p = 0.012, effect size negligible; d = 0.14). Compared to the flat insole, the contoured foot orthosis provided a significant decrease on maximum force (−4%, p = 0.011, effect size negligible; d = −0.14).
Hallux
There was a significant effect for peak pressure (Wilk’s Lambda = 0.72, F (2, 26) = 5.19, p = 0.013; effect size large, ηp2 = 0.29, 90% CI 0.04 to 0.45) and maximum force (Wilk’s Lambda = 0.73, F (2, 26) = 4.88, p = 0.016; effect size large, ηp2 = 0.27, 90% CI 0.03 to 0.44) between the three conditions. Compared to the boot only condition, the contoured foot orthosis provided significant increases on peak pressure (+9%, p = 0.026, effect size small; d = 0.24) and maximum force (+7%, p = 0.034, effect size small; d = 0.17). The flat insole provided a significant increase on maximum force (+9%, p = 0.004, effect size small; d = 0.21), while having no significant effect on peak pressure (p = 0.774). Compared to the flat insole, the contoured foot orthosis provided a significant increase on peak pressure (+8%, p < 0.005, effect size small; d = 0.24).
Tibial acceleration
There was a significant effect for tibial peak positive acceleration (Wilk’s Lambda = 0.70, F (2, 26) = 5.67, p = 0.009; effect size large, ηp2 = 0.30, 90% CI 0.05 to 0.47) between the three conditions. Compared to the boot only condition, the contoured foot orthosis provided a significant decrease on tibial peak positive acceleration (−7%, p < 0.018, effect size small; d = −0.19), while the flat insole had no significant effect (p = 0.882). Compared to the flat insole, the contoured foot orthosis significantly decreased peak positive tibial acceleration (−8%, p < 0.016, effect size small; d = −0.22).
Footwear comfort
There were no significant differences in footwear comfort (p = 0.842) between the boot only condition (63.2 ± 17.8 mm), the flat insole (65.8 ± 18.9 mm) and the contoured foot orthosis (64.0 ± 20.3 mm).
Discussion
The aim of this study was to investigate the immediate effects of a contoured, prefabricated foot orthosis and a flat insole on plantar pressure, tibial acceleration and comfort while walking in defence boots. Our findings indicate that, compared to the defence boot only condition, the contoured foot orthosis provided a medium to large reduction on plantar pressure under the rearfoot, medium to very large increases in contact area and plantar pressures under the medial midfoot, and small increases in force under the medial forefoot and hallux. The flat insole also provided increases in contact area and plantar pressure under the medial midfoot, and small increases in force under the lateral forefoot, medial forefoot and hallux. Of note, the increases in contact area and plantar pressures observed with the flat insole under the medial midfoot were significantly less than those provided by the foot orthosis. Compared to the defence boot only condition, the contoured foot orthosis also provided a small reduction on tibial peak positive acceleration while no change was observed with the flat insole. Despite the different plantar pressure and tibial acceleration profiles, there were no differences in comfort on the day of testing between the three footwear-insole conditions.
The contoured shape of the foot orthosis resulted in a very large increase in contact area under the medial midfoot, which was approximately three-fold greater than the boot only condition and flat insole. This enabled the contoured foot orthosis to redistribute force over a greater area of the foot, thus providing large reductions on plantar pressures under the rearfoot. This finding is consistent with previous studies that have found that contoured foot orthoses reduce plantar pressure under the rearfoot41,42. However, another study found that the material from which the orthosis is manufactured, as well as its contour, influence plantar pressures at the midfoot and rearfoot37. Although the flat insole and the contoured foot orthosis used in our current study were made from the same material (140 kg/m3 closed cell polyethylene), the latter was substantially thicker in the region of the medial midfoot and around the periphery of the heel. When considering our findings in the context of the previous research37,42, it is likely that the plantar pressure changes observed in our study can be attributed to both the contour of the foot orthosis, and its thicker material under the midfoot and around the periphery of the heel.
The plantar pressure findings of this study, particularly the medium to large reductions in plantar loading under the rearfoot, may assist in explaining how contoured foot orthoses are effective in the prevention and treatment of some common lower limb overuse injuries19,20,43. For example, a prospective study found that Royal Marine recruits that had greater peak pressure under the rearfoot during barefoot running were at greater risk of developing a tibial stress fracture during initial defence training44. Further, a cross-sectional study found that recreational runners who developed plantar heel pain had greater rearfoot plantar loading compared to uninjured runners45. Regarding the treatment of injuries, a clinical trial has shown that a foot orthosis identical to the device used in this study was effective in the management of plantar heel pain46, while a more recent trial also found this orthosis reduced the incidence of plantar heel pain by 50% in naval recruits undertaking initial defence training20. It must also be noted that our data demonstrates small increases in force under the medial forefoot. This finding suggests caution is required when prescribing foot orthoses in defence boots as the increase in force under the medial forefoot may be of clinical importance and lead to the development of new pathologies in the forefoot, or exacerbate pre-existing pathologies. The greatest concern regarding increases in force under the forefoot is whether it increases the risk of stress fractures of the metatarsals, which have been shown to be a common site for such injuries among military personnel47,48. However, these fractures most commonly affect metatarsals 2–5, where the foot orthosis we tested provided no effect on plantar pressures, so it is unclear whether the changes we observed in forefoot loading are clinically meaningful.
The reduction in tibial peak positive acceleration provided by the contoured foot orthoses is also of interest, as tibial stress injuries, such as medial tibial stress syndrome and tibial stress fractures, are among the most common overuse injuries experienced by physically active defence personnel1. The tibias of individuals with tibial stress injuries have been shown to have less cortical bone (cross sectional area and thickness), which has been proposed to reduce the tibia’s ability to resist tibial loading and bending moments49,50. While bony structure is likely to contribute to the risk of developing tibial stress injury, the magnitude of loading applied to the tibia has also been identified as important. Runners with a history of tibial stress fractures have been shown to experience greater tibial accelerations compared to runners without injury51–53. The reduction in tibial acceleration observed in our study may assist in explaining the findings of a recent systematic review that found that foot orthoses reduced the risk of developing shin pain and tibial stress fractures in defence personnel by 73% and 35%19, respectively. It must be noted, however, that tibial stress injuries are most typically seen in individuals undertaking running-based activities, so it is possible that the effects that foot orthoses have on tibial acceleration are most relevant during running. Nevertheless, as tibial stress injuries are common in defence personnel, the immediate, albeit small, reduction in tibial peak positive acceleration when using contoured foot orthoses during walking in defence boots may be beneficial in the prevention of these injuries.
In addition to altering tissue loading, it has also been proposed that contoured foot orthoses can provide clinical benefits via improvements in comfort54. Of interest, our study found that the contoured foot orthosis, flat insole and defence boots were all perceived as being equally comfortable after a short period of use. From a practical standpoint, this would suggest that contoured foot orthoses may be used for the prevention and treatment of injury without having a detrimental effect on immediate comfort, which is likely to be an important consideration by defence personnel. It must be noted, however, that our study only measured immediate comfort and it is likely that comfort over an extended period of time, such as during prolonged standing or when completing a long march, is of greater importance to defence personnel.
The findings of this study need to be viewed in light of several key limitations. First, the pedar®-X can only record resultant force acting perpendicular to the pressure mapping insole. As the pedar®-X is unable to determine the shear component of forces, it is possible that some inherent measurement error occurs. Despite such limitations, the pedar®-X provides a valid, reliable and accurate measure of plantar pressure and it is considered the best available method for measuring forces acting between the foot and shoe insoles28,29. Second, while the shoe insoles did provide some effect on plantar pressure and tibial acceleration, extrapolating these findings to kinematic changes is inherently speculative, although it has been proposed that the biomechanical effects of foot orthoses result from changes in plantar loading54,55. Third, it remains unknown what effects the shoe insoles have on plantar pressure, tibial acceleration and comfort over the longer term as a result of material compression and acclimatisation. Fourth, although participants were blinded during testing we did not measure how successful this was. As such, some of the differences observed in our study may have resulted, in part, from non-specific effects. Fifth, the participants in this study were healthy (uninjured) and relatively young, and although this is representative of military recruits, it remains unclear if the effects observed in this study may differ among military personnel, who may also be older and / or injured. Sixth, as the participants in our study were only observed during comfortable walking it would be beneficial for future studies to investigate the effects of foot orthoses on biomechanical outcomes during other tasks commonly performed by military personnel, such as marching, during load-carriage, and when in a fatigued state. Finally, we recognise that the association between changes to plantar pressures, tibial accelerations and injury has not been fully established in a military setting. In consideration of the aforementioned limitations, it would be beneficial for future studies to investigate if the changes in biomechanical variables, including plantar pressure and tibial acceleration, have an effect on injury incidence in military personnel.
In summary, the findings of this study indicate that contoured, prefabricated foot orthoses provide significant increases in plantar pressures at the midfoot and force at the medial forefoot, and reductions in plantar pressures at the rearfoot, while also providing small reductions in tibial peak positive acceleration. The flat insole also increased medial midfoot loads, but to a much lesser extent compared to the foot orthosis, while having no effect on tibial peak positive accelerations. These findings provide useful insights into the mechanisms that may be responsible for foot orthoses reducing the rate of lower limb overuse injury in defence personnel.
Acknowledgements
The foot orthoses and flat insoles were donated by Foot Science International Ltd, Christchurch, New Zealand. Foot Science International Ltd had no input into the design or implementation of the trial, and the analysis or interpretation of the data generated from the trial. HBM is currently a National Health and Medical Research Council Senior Research Fellow (ID: 1135995).
Author Contributions
All authors were involved in study concept and design. D.R.B. and K.L. were responsible for acquisition of data and can take responsibility for the integrity of the data. D.R.B. was responsible for statistical analysis and interpretation of data. D.R.B. was responsible for the preparation of the manuscript with all other authors involved in its review prior to submission for publication. The material within has not been and will not be submitted for publication elsewhere. All authors read and approved the final manuscript.
Data Availability
The data generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Competing Interests
The authors declare no competing interests.
Footnotes
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Sharma, J., Greeves, J. P., Byers, M., Bennett, A. N. & Spears, I. R. Musculoskeletal injuries in British Army recruits: a prospective study of diagnosis-specific incidence and rehabilitation times. BMC Musculoskelet Disord16,106 (2015). [DOI] [PMC free article] [PubMed]
- 2.Robinson M, et al. Low fitness, low body mass and prior injury predict injury risk during military recruit training: a prospective cohort study in the British Army. BMJ Open Sport Exerc Med. 2016;2:e000100. doi: 10.1136/bmjsem-2015-000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kaufman KR, Brodine S, Shaffer R. Military training-related injuries: Surveillance, research, and prevention. Am J Prev Med. 2000;18:54–63. doi: 10.1016/S0749-3797(00)00114-8. [DOI] [PubMed] [Google Scholar]
- 4.Nye, N. S., Pawlak, M. T., Webber, B. J., Tchandja, J. N. & Milner, M. R. Description and rate of musculoskeletal injuries in air force basic military trainees, 2012−2014. J Athl Train51, 858-865 (2016). [DOI] [PMC free article] [PubMed]
- 5.Yates B, White S. The Incidence and Risk Factors in the Development of Medial Tibial Stress Syndrome Among Naval Recruits. Am J Sports Med. 2004;32:772–780. doi: 10.1177/0095399703258776. [DOI] [PubMed] [Google Scholar]
- 6.Franklyn-Miller A, Wilson C, Bilzon J, McCrory P. Foot orthoses in the prevention of injury in initial military training: a randomized controlled trial. Am J Sports Med. 2011;39:30–37. doi: 10.1177/0363546510382852. [DOI] [PubMed] [Google Scholar]
- 7.Psaila M, Ranson C. Risk factors for lower leg, ankle and foot injuries during basic military training in the Maltese Armed Forces. Phys Ther Sport. 2017;24:7–12. doi: 10.1016/j.ptsp.2016.09.004. [DOI] [PubMed] [Google Scholar]
- 8.Wills AK, Ramasamy A, Ewins DJ, Etherington J. The incidence and occupational outcome of overuse anterior knee pain during army recruit training. J R Army Med Corps. 2004;150:264–269. doi: 10.1136/jramc-150-04-07. [DOI] [PubMed] [Google Scholar]
- 9.Dowling, G. J. et al. Dynamic foot function as a risk factor for lower limb overuse injury: a systematic review. J Foot Ankle Res7, 53 (2014). [DOI] [PMC free article] [PubMed]
- 10.Neal, B. S. et al. Foot posture as a risk factor for lower limb overuse injury: a systematic review and meta-analysis. J Foot Ankle Res7:55 (2014). [DOI] [PMC free article] [PubMed]
- 11.Bulzacchelli MT, Sulsky SI, Rodriguez-Monguio R, Karlsson LH, Hill MO. Injury during USArmy basic combat training: a systematic review of risk factor studies. Am J Prev Med. 2014;47:813–822. doi: 10.1016/j.amepre.2014.08.008. [DOI] [PubMed] [Google Scholar]
- 12.Gabbett TJ, Hulin BT, Blanch P, Whiteley R. High training workloads alone do not cause sports injuries: how you get there is the real issue. Br J Sports Med. 2016;50:444–445. doi: 10.1136/bjsports-2015-095567. [DOI] [PubMed] [Google Scholar]
- 13.Gabbett TJ. The training—injury prevention paradox: should athletes be training smarter and harder? Br J Sports Med. 2016;50:273–280. doi: 10.1136/bjsports-2015-095788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sinclair J, Taylor PJ. Influence of new military athletic footwear on the kinetics and kinematics of running in relation to army boots. J Strength Cond Res. 2014;28:2900–2908. doi: 10.1519/JSC.0000000000000477. [DOI] [PubMed] [Google Scholar]
- 15.Knapik JJ, Jones BH, Steelman RA. Physical training in boots and running shoes: a historical comparison of injury incidence in basic combat training. Mil Med. 2015;180:321–328. doi: 10.7205/MILMED-D-14-00337. [DOI] [PubMed] [Google Scholar]
- 16.Sinclair J, Taylor PJ, Atkins S. Influence of running shoes and cross-trainers on Achilles tendon forces during running compared with military boots. J R Army Med Corps. 2015;161:140–143. doi: 10.1136/jramc-2014-000308. [DOI] [PubMed] [Google Scholar]
- 17.Mündermann A, Stefanyshyn DJ, Nigg BM. Relationship between footwear comfort of shoe inserts and anthropometric and sensory factors. Med Sci Sports Exerc. 2001;33:1939–1945. doi: 10.1097/00005768-200111000-00021. [DOI] [PubMed] [Google Scholar]
- 18.Windle CM, Gregory SM, Dixon SJ. The shock attenuation characteristics of four different insoles when worn in a military boot during running and marching. Gait Posture. 1999;9:31–37. doi: 10.1016/S0966-6362(99)00002-8. [DOI] [PubMed] [Google Scholar]
- 19.Bonanno DR, Landorf KB, Munteanu SE, Murley GS, Menz HB. Effectiveness of foot orthoses and shock-absorbing insoles for the prevention of injury: a systematic review and meta-analysis. Br J Sports Med. 2017;51:86–96. doi: 10.1136/bjsports-2016-096671. [DOI] [PubMed] [Google Scholar]
- 20.Bonanno DR, Murley GS, Munteanu SE, Landorf KB, Menz HB. Effectiveness of foot orthoses for the prevention of lower limb overuse injuries in naval recruits: a randomised controlled trial. Br J Sports Med. 2018;52:298–302. doi: 10.1136/bjsports-2017-098273. [DOI] [PubMed] [Google Scholar]
- 21.Mills K, Blanch P, Chapman AR, McPoil TG, Vicenzino B. Foot orthoses and gait: a systematic review and meta-analysis of literature pertaining to potential mechanisms. Br J Sports Med. 2010;44:1035–1046. doi: 10.1136/bjsm.2009.066977. [DOI] [PubMed] [Google Scholar]
- 22.von Elm E, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. PLOS Med. 2007;4:e296. doi: 10.1371/journal.pmed.0040296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Redmond AC, Crane YZ, Menz HB. Normative values for the Foot Posture Index. J Foot Ankle Res. 2008;1:6. doi: 10.1186/1757-1146-1-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Redmond AC, Crosbie J, Ouvrier RA. Development and validation of a novel rating system for scoring standing foot posture: the Foot Posture Index. Clin Biomech (Bristol, Avon) 2006;21:89–98. doi: 10.1016/j.clinbiomech.2005.08.002. [DOI] [PubMed] [Google Scholar]
- 25.Brody DM. Techniques in the evaluation and treatment of the injured runner. Orthop Clin North Am. 1982;13:541–558. [PubMed] [Google Scholar]
- 26.Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39:175–191. doi: 10.3758/BF03193146. [DOI] [PubMed] [Google Scholar]
- 27.Bonanno, D. R., Murley, G. S., Munteanu, S. E., Landorf, K. B. & Menz, H. B. Foot orthoses for the prevention of lower limb overuse injuries in naval recruits: study protocol for a randomised controlled trial. J Foot Ankle Res8, 51 (2015). [DOI] [PMC free article] [PubMed]
- 28.Putti AB, Arnold GP, Cochrane L, Abboud RJ. The Pedar in-shoe system: repeatability and normal pressure values. Gait Posture. 2007;25:401–405. doi: 10.1016/j.gaitpost.2006.05.010. [DOI] [PubMed] [Google Scholar]
- 29.Boyd LA, Bontrager EL, Mulroy SJ, Perry J. The reliability and validity of the Novel Pedar system of in-shoe pressure measurement during free ambulation. Gait Posture. 1997;5:165–165. doi: 10.1016/S0966-6362(97)83397-8. [DOI] [Google Scholar]
- 30.Lafortune MA. Three-dimensional acceleration of the tibia during walking and running. J Biomech. 1991;24:877–886. doi: 10.1016/0021-9290(91)90166-K. [DOI] [PubMed] [Google Scholar]
- 31.Lucas-Cuevas, A. G., Encarnacion-Martinez, A., Camacho-Garcia, A., Llana-Belloch, S. & Perez-Soriano, P. The location of the tibial accelerometer does influence impact acceleration parameters during running. J Sports Sci, 1734–1738 (2016). [DOI] [PubMed]
- 32.Laughton CA, McClay Davis I, Hamill J. Effect of strike pattern and orthotic intervention on tibial shock during running. J Appl Biomech. 2003;19:153–168. doi: 10.1123/jab.19.2.153. [DOI] [Google Scholar]
- 33.Hennig EM, Milani TL, Lafortune MA. Use of ground reaction force parameters in predicting peak tibial accelerations in running. J Appl Biomech. 1993;9:306–314. doi: 10.1123/jab.9.4.306. [DOI] [PubMed] [Google Scholar]
- 34.Burnfield JM, Few CD, Mohamed OS, Perry J. The influence of walking speed and footwear on plantar pressures in older adults. Clin Biomech (Bristol, Avon) 2004;19:78–84. doi: 10.1016/j.clinbiomech.2003.09.007. [DOI] [PubMed] [Google Scholar]
- 35.Menz HB. Two feet, or one person? Problems associated with statistical analysis of paired data in foot and ankle medicine. Foot. 2004;14:2–5. doi: 10.1016/S0958-2592(03)00047-6. [DOI] [Google Scholar]
- 36.Gerrard JM, Bonanno DR. Increasing preferred step rate during running reduces plantar pressures. Scand J Med Sci Sports. 2018;28:144–151. doi: 10.1111/sms.12886. [DOI] [PubMed] [Google Scholar]
- 37.McCormick CJ, Bonanno DR, Landorf KB. The effect of customised and sham foot orthoses on plantar pressures. J Foot Ankle Res. 2013;6:19. doi: 10.1186/1757-1146-6-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Shorten MR, Winslow DS. Spectral analysis of impact shock during running. Int J Sports Biomech. 1992;8:288–304. doi: 10.1123/ijsb.8.4.288. [DOI] [Google Scholar]
- 39.Cohen, J. Statistical Power Analysis for the Behavioral Sciences. 2 edn, (L. Erlbaum Associates, 1988).
- 40.Cohen J. A power primer. Psychol Bull. 1992;112:155–159. doi: 10.1037/0033-2909.112.1.155. [DOI] [PubMed] [Google Scholar]
- 41.Goske S, Erdemir A, Petre M, Budhabhatti S, Cavanagh PR. Reduction of plantar heel pressures: insole design using finite element analysis. J Biomech. 2006;39:2363–2370. doi: 10.1016/j.jbiomech.2005.08.006. [DOI] [PubMed] [Google Scholar]
- 42.Bonanno DR, Landorf KB, Menz HB. Pressure-relieving properties of various shoe inserts in older people with plantar heel pain. Gait Posture. 2010;33:385–389. doi: 10.1016/j.gaitpost.2010.12.009. [DOI] [PubMed] [Google Scholar]
- 43.Hawke, F., Burns, J., Radford, J. A. & Du Toit, V. Custom-made foot orthoses for the treatment of foot pain. Cochrane Database Syst Rev, Issue 3. Art. No.: CD006801 (2008). [DOI] [PubMed]
- 44.Nunns M, et al. Four biomechanical and anthropometric measures predict tibial stress fracture: a prospective study of 1065 Royal Marines. Br J Sports Med. 2016;50:1206–1210. doi: 10.1136/bjsports-2015-095394. [DOI] [PubMed] [Google Scholar]
- 45.Ribeiro AP, Joao SM, Dinato RC, Tessutti VD, Sacco IC. Dynamic Patterns of Forces and Loading Rate in Runners with Unilateral Plantar Fasciitis: A Cross-Sectional Study. PLoS One. 2015;10:e0136971. doi: 10.1371/journal.pone.0136971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Landorf KB, Keenan AM, Herbert RD. Effectiveness of foot orthoses to treat plantar fasciitis: a randomized trial. Arch Intern Med. 2006;166:1305–1310. doi: 10.1001/archinte.166.12.1305. [DOI] [PubMed] [Google Scholar]
- 47.Wood AM, et al. Incidence and time to return to training for stress fractures during military basic training. J Sports Med. 2014;2014:1–5. doi: 10.1155/2014/282980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Valimaki VV, et al. Risk factors for clinical stress fractures in male military recruits: a prospective cohort study. Bone. 2005;37:267–273. doi: 10.1016/j.bone.2005.04.016. [DOI] [PubMed] [Google Scholar]
- 49.Franklyn M, Oakes B, Field B, Wells P, Morgan D. Section modulus is the optimum geometric predictor for stress fractures and medial tibial stress syndrome in both male and female athletes. Am J Sports Med. 2008;36:1179–1189. doi: 10.1177/0363546508314408. [DOI] [PubMed] [Google Scholar]
- 50.Milgrom C, et al. The area moment of inertia of the tibia: a risk factor for stress fractures. J Biomech. 1989;22:1243–1248. doi: 10.1016/0021-9290(89)90226-1. [DOI] [PubMed] [Google Scholar]
- 51.Pohl MB, Mullineaux DR, Milner CE, Hamill J, Davis IS. Biomechanical predictors of retrospective tibial stress fractures in runners. J Biomech. 2008;41:1160–1165. doi: 10.1016/j.jbiomech.2008.02.001. [DOI] [PubMed] [Google Scholar]
- 52.Milner CE, Hamill J, Davis I. Are knee mechanics during early stance related to tibial stress fracture in runners? Clin Biomech (Bristol, Avon) 2007;22:697–703. doi: 10.1016/j.clinbiomech.2007.03.003. [DOI] [PubMed] [Google Scholar]
- 53.Milner CE, Ferber R, Pollard CD, Hamill J, Davis IS. Biomechanical factors associated with tibial stress fracture in female runners. Med Sci Sports Exerc. 2006;38:323–328. doi: 10.1249/01.mss.0000183477.75808.92. [DOI] [PubMed] [Google Scholar]
- 54.Nigg BM, Wakeling JM. Impact forces and muscle tuning: a new paradigm. Exerc Sport Sci Rev. 2001;29:37–41. doi: 10.1097/00003677-200101000-00008. [DOI] [PubMed] [Google Scholar]
- 55.Redmond AC, Landorf KB, Keenan AM. Contoured, prefabricated foot orthoses demonstrate comparable mechanical properties to contoured, customised foot orthoses: a plantar pressure study. J Foot Ankle Res. 2009;2:20. doi: 10.1186/1757-1146-2-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Munteanu SE, Strawhorn AB, Landorf KB, Bird AR, Murley GS. A weightbearing technique for the measurement of ankle joint dorsiflexion with the knee extended is reliable. J Sci Med Sport. 2009;12:54–59. doi: 10.1016/j.jsams.2007.06.009. [DOI] [PubMed] [Google Scholar]
- 57.Bennell K, et al. Intra-rater and inter-rater reliability of a weight-bearing lunge measure of ankle dorsiflexion. Aust J Physiother. 1998;44:175–180. doi: 10.1016/S0004-9514(14)60377-9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data generated during and/or analysed during the current study are available from the corresponding author on reasonable request.