While cigarette smoking still remains one of the most pressing global health issues of our time, newer forms of smoking device have been introduced across the globe in the last decade [1]. Electronic nicotine/non-nicotine delivery systems commonly known as electronic cigarettes (eCig) heat a solution (e-liquid) to create vapour [2]; the latest addition to this list is the introduction of heat-not-burn (HNBs) tobacco products branded as IQOS [3]. HNBs are hybrids between eCigs and traditional cigarettes i.e. they are equipped with a device that heats the product, without burning to generate aerosol and the product being heated is not a liquid but real tobacco [4, 5]. eCig vaping is comparatively new but its use is increasing at an alarming rate; it is believed it will surpass the use of traditional cigarettes in next 5 years, with global sales reaching US$10 billion [6]. Since its launch in Italy and Japan in 2014, IQOS has become the leader in the HNB market [4, 7]. To date, IQOS is available in 41 countries, including 22 from the WHO-European region, and its market share has now reached the level of cigars in Italy [4]. Emerging data shows that eCig use, particularly in the young, is associated with future cigarette use [8]. Similarly, over half of the people interested in IQOS are never-smokers [4]. Therefore, both eCigs and IQOS may represent a gateway for nicotine addiction among never-smokers rather than a substitute used for harm-reduction purposes in current smokers [4]. It is now clear that eCig vapour contains high levels of toxic compounds [9], which adversely affect respiratory, gastrointestinal and cardiovascular systems both in vitro and in vivo [10–12]. It is also important to recognise that IQOS products are comparatively new but emerging research suggests that IQOS emits substantially high levels of carbonyls [13]. There is as yet no published comparison between the effect of eCigs, IQOS and tobacco smoke on human lungs. Here, we examine whether exposure to IQOS has the same damaging effect on human airway epithelial and smooth muscle cells as traditional tobacco cigarette and eCigs in vitro.
Short abstract
Heat-not-burn (HNB) devices can alter vital physiological functions in the lung. HNB devices may not be a safer option than cigarette smoking or eCig vaping; this does not support the recommendation of their use over other nicotine delivery products. http://ow.ly/wZ5P30ng8bU
To the Editor:
While cigarette smoking still remains one of the most pressing global health issues of our time, newer forms of smoking device have been introduced across the globe in the last decade [1]. Electronic nicotine/non-nicotine delivery systems commonly known as electronic cigarettes (eCig) heat a solution (e-liquid) to create vapour [2]; the latest addition to this list is the introduction of heat-not-burn (HNBs) tobacco products branded as IQOS [3]. HNBs are hybrids between eCigs and traditional cigarettes i.e. they are equipped with a device that heats the product, without burning to generate aerosol and the product being heated is not a liquid but real tobacco [4, 5]. eCig vaping is comparatively new but its use is increasing at an alarming rate; it is believed it will surpass the use of traditional cigarettes in next 5 years, with global sales reaching US$10 billion [6]. Since its launch in Italy and Japan in 2014, IQOS has become the leader in the HNB market [4, 7]. To date, IQOS is available in 41 countries, including 22 from the WHO-European region, and its market share has now reached the level of cigars in Italy [4]. Emerging data shows that eCig use, particularly in the young, is associated with future cigarette use [8]. Similarly, over half of the people interested in IQOS are never-smokers [4]. Therefore, both eCigs and IQOS may represent a gateway for nicotine addiction among never-smokers rather than a substitute used for harm-reduction purposes in current smokers [4]. It is now clear that eCig vapour contains high levels of toxic compounds [9], which adversely affect respiratory, gastrointestinal and cardiovascular systems both in vitro and in vivo [10–12]. It is also important to recognise that IQOS products are comparatively new but emerging research suggests that IQOS emits substantially high levels of carbonyls [13]. There is as yet no published comparison between the effect of eCigs, IQOS and tobacco smoke on human lungs. Here, we examine whether exposure to IQOS has the same damaging effect on human airway epithelial and smooth muscle cells as traditional tobacco cigarette and eCigs in vitro.
We used human bronchial epithelial cells (Beas-2B, ATCC CRL-9609) and primary human airway smooth muscle (ASM) cells (ATCC PCS-130-010). eCig vapour was generated using an eCig device (KangerTech 3rd Generation; KangerTech, Shenzhen, China) and e-liquid (Blu, Charlotte, NC, USA) (1.2% nicotine); IQOS aerosol was generated using HNB heat-sticks (Philip Morris, Tokyo, Japan) (1.4 mg nicotine); and cigarette-smoke-extract (CSE) was generated using Marlboro Red cigarettes (Philip Morris, Washington, DC, USA) (1.2 mg nicotine). eCig vapour/IQOS aerosol/cigarette smoke was “bubbled” through a T-75 flask containing 25-mL media at a constant rate with modification [14–18]. This freshly generated (100%) eCig vapour, IQOS aerosol and CSE were diluted to the final working concentration and used immediately. Beas-2B or primary human ASM cells were treated with increasing concentrations of CSE, eCig vapour or IQOS aerosol for 72 h, and cell cytotoxicity (Thaizolyl blue tetrazolium bromide (MTT) and lactate dehydrogenase (LDH)), chemokine release (CXCL8), extracellular matrix (ECM) (collagen 1 and fibronectin) release and mitochondrial respiration (glycolysis and proton leak) were measured.
GraphPad (La Jolla, CA, USA) was used for statistical analysis using one-way ANOVA followed by Bonferroni's multiple comparison test.
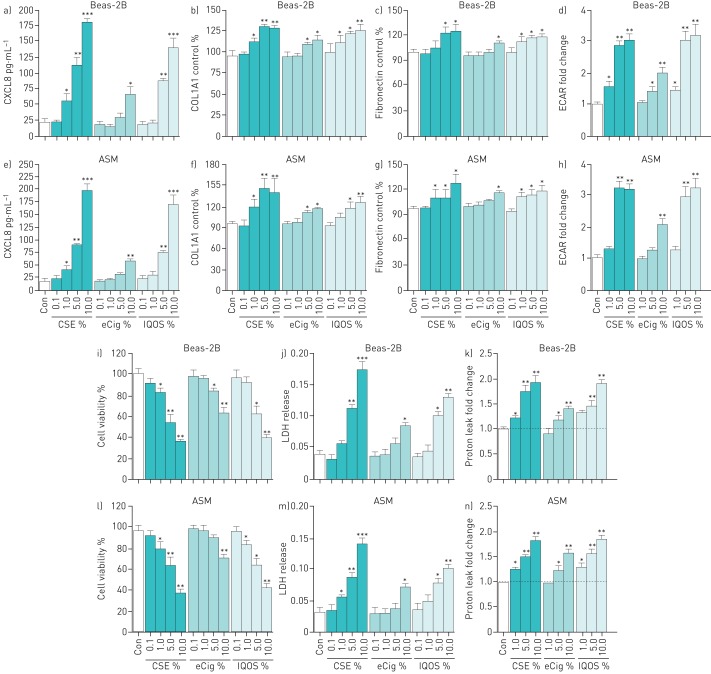
Using two different cytotoxicity assays (MTT and LDH), CSE, eCig or IQOS exposure showed cellular toxicity with increasing concentration (figure 1a–h). A CSE concentration of >10% is highly toxic; therefore, we only used concentrations <10% in our experiments, which is also used widely in many studies [14–18]. In both Beas-2B and ASM cells, we found that CSE exposure significantly reduced cell viability and increased LDH release at 1, 5 and 10% (figure 1i–n). eCig exposure showed similar toxicity at 5 and 10% exposure. Interestingly, IQOS exposure was as toxic as CSE at 1, 5 and 10%. It is evident that both CSE and eCig vapour can induce inflammation in the lung [18, 19], and as shown in figure 1a–h), CSE exposure in a concentration-dependent manner induced the release of CXCL8 in Beas-2B (figure 1a) and ASM cells (figure 1e). eCig exposure induced CXCL8 release at the highest concentration, whereas IQOS exposure showed a similar induction to CSE, suggesting that IQOS is as effective as CSE in inducing chemokine release from both types of airway cells. Next, we measured the induction of ECM proteins with airway cells; CSE, eCig and IQOS exposure in a concentration-dependent manner increased collagen 1 (figure 1b and f) and fibronectin (figure 1c and g) release with both Beas-2B (figure 1b and c) and ASM (figure 1c and g) cells. Finally, we measured mitochondrial respiration using a seahorse analyser, and found that CSE, eCig and IQOS exposure increased the extracellular acidification rate (a measure of glycolysis) (figure 1a–h) and proton leak (a measure of mitochondrial uncoupling) (figure 1i–n) in both Beas-2B (figure 1d) and ASM (figure 1h) cells, respectively.
FIGURE 1.
a–h) Comparison of the effects of cigarette smoke extract (CSE), electronic cigarette (eCig) vapour and IQOS aerosol exposure on a–d) human airway epithelial (Beas-2B) and e–h) human airway smooth muscle (ASM) cells. a and e) show the release of CXCL8 from Beas-2B and ASM cells. The concentration of CXCL8 in supernatant from Beas-2B and ASM cells after 72 h of stimulation with CSE, eCig vapour or IQOS aerosol exposure was measured using ELISA. Deposition of b and f) collagen I alpha 1 (COL1A1) and c and g) fibronectin from Beas-2B and human ASM cells after 72 h of stimulation with CSE, eCig vapour or IQOS aerosol exposure was measured using extracellular matrix (ECM) ELISA at an absorbance of 450 nm and 570 nm, respectively. d and h) The level of glycolysis was determined in Beas-2B and ASM cells using a seahorse analyser, and extracellular acidification rate (ECAR); an index of glycolysis was measured after 72 h of stimulation with CSE, eCig vapour or IQOS aerosol exposure. Data are presented as mean±sem (n=5–7). i–n) The effect of CSE, eCig and IQOS exposure on cellular toxicity and respiration. The cell viability (i and l), the lactate dehydrogenase (LDH) release (j and m) and the mitochondrial respiration (k and n) from Beas-2B and human ASM cells was measured using Thaizolyl blue tetrazolium bromide (MTT) and LDH assays at an absorbance of 570 nm and 490 nm, respectively. k and n) Mitochondrial respiration was measured in Beas-2B and ASM cells using a mito-stress kit on a seahorse analyser (Agilent Technologies Inc., Santa Clara, CA, USA), and proton leak was measured as oxygen consumption rate shown as fold change to control. Cells were stimulated with serial dilution of CSE, eCig vapour or IQOS aerosol for 72 h (n=5). Data are presented as mean±sem. A one-way ANOVA plus Bonferroni post-test was used to determine statistical significance. *: p<0.05 compared with control; **: p<0.01 compared with control; ***: p<0.001 compared with control.
Cigarette smoking has been linked to chronic lung diseases such as chronic obstructive pulmonary disease (COPD), asthma, pulmonary fibrosis, cancer and related comorbidities [1]. It took us nearly five decades to understand the detrimental effects of cigarette smoke on humans. Long-term eCig-exposure studies in humans are currently sparse, limiting our understanding of its direct effect(s) on both disease development and progression. eCig vaping is already at its highest level globally, and many countries are imposing stringent regulations in light of the emerging evidence showing the adverse effects of vaping on human health. IQOS use is comparatively new; it will take years before we start to know its detrimental effect on human health. We demonstrate here for the first time that IQOS exposure is as detrimental as cigarette smoking and vaping to human lung cells. Persistent allergic, smoke or environmental-triggered inflammation leads to airway remodelling/scarring through re-organisation of ECM and airway cell proliferation, and mitochondrial dysfunction plays a pivotal role in this process. These are the principal causes for airflow limitation in asthma and COPD. Here, we have analysed all of these mechanisms: inflammation (CXCL8), ECM release (collagen 1 and fibronectin) and mitochondrial respiration (glycolysis and proton leak). We observed collagen-1 and fibronectin induction by both Beas-2B and ASM cells to CSE, eCig and IQOS exposure. ECM proteins facilitate the conversion of mesenchymal cells to ECM secreting active myofibroblasts and epithelial mesenchymal transition (EMT) in chronic lung disease [20, 21]. Our data suggests that like eCigs and traditional cigarettes, IQOS exposure contributes to altered mitochondrial function which can further exaggerate airway inflammation, airway remodelling and lung cancer through active EMT, as seen in smokers [22]. It is widely understood that mitochondria of airway epithelium and mesenchymal cells play differential roles, consistent with their contributions to disease and essential for cell existence. Mitochondrial dysfunction also underpins many normal physiological processes and in certain pathological conditions, such as obesity or with an oxidant trigger such as smoke, eCigs and IQOS, it may impact lung diseases. Cigarette smoking and eCigs can exaggerate respiratory infections by increasing microbial adherence to the airways [23, 24]; IQOS may increase respiratory infections through similar mechanisms.
Given our current findings and those of previous studies, in a manner very similar to cigarette smoke and eCigs, IQOS has the potential to increase oxidative stress and inflammation, infections, airway remodelling and initiate EMT-related changes in the airways of users of these devices. However, prospective clinical studies must be conducted to verify our in vitro, cell-based but highly important and novel findings on IQOS.
Footnotes
Conflict of interest: S.S. Sohal has nothing to disclose.
Conflict of interest: M.S. Eapen has nothing to disclose.
Conflict of interest: V.G.M. Naidu has nothing to disclose.
Conflict of interest: P. Sharma has nothing to disclose.
Support statement: This study was supported by a Rebecca L. Cooper Foundation Grant to P. Sharma, and S.S. Sohal was supported by the Clifford Craig Foundation. The authors have no links to the tobacco industry. Funding information for this article has been deposited with the Crossref Funder Registry.
References
- 1.Alberg AJ, Shopland DR, Cummings KM. The 2014 Surgeon General's report: commemorating the 50th Anniversary of the 1964 Report of the Advisory Committee to the US Surgeon General and updating the evidence on the health consequences of cigarette smoking. Am J Epidemiol 2014; 179: 403–412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.WHO. Electronic nicotine delivery systems and electronic non-nicotine delivery systems (ENDS/ENNDS). Report. Delhi, India, 2017. https://www.who.int/tobacco/communications/statements/eletronic-cigarettes-january-2017/en/ [Google Scholar]
- 3.Smith MR, Clark B, Ludicke F, et al. Evaluation of the tobacco heating system 2.2. Part 1: description of the system and the scientific assessment program. Regul Toxicol Pharmacol 2016; 81: Suppl. 2, S17–S26. [DOI] [PubMed] [Google Scholar]
- 4.Liu X, Lugo A, Spizzichino L, et al. Heat-not-burn tobacco products: concerns from the Italian experience. Tob Control 2018; 28: 113–114. [DOI] [PubMed] [Google Scholar]
- 5.Auer R, Concha-Lozano N, Jacot-Sadowski I, et al. Heat-not-burn tobacco cigarettes: smoke by any other name. JAMA Intern Med 2017; 177: 1050–1052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dinakar C, O'Connor GT. The health effects of electronic cigarettes. N Engl J Med 2016; 375: 1372–1381. [DOI] [PubMed] [Google Scholar]
- 7.Tabuchi T, Gallus S, Shinozaki T, et al. Heat-not-burn tobacco product use in Japan: its prevalence, predictors and perceived symptoms from exposure to secondhand heat-not-burn tobacco aerosol. Tob Control 2018; 27: e25–e33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bold KW, Kong G, Camenga DR, et al. Trajectories of E-cigarette and conventional cigarette use among youth. Pediatrics 2018; 141: 141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jensen RP, Luo W, Pankow JF, et al. Hidden formaldehyde in e-cigarette aerosols. N Engl J Med 2015; 372: 392–394. [DOI] [PubMed] [Google Scholar]
- 10.Chen H, Li G, Chan YL, et al. Maternal e-cigarette exposure in mice alters DNA methylation and lung cytokine expression in offspring. Am J Respir Cell Mol Biol 2018; 58: 366–377. [DOI] [PubMed] [Google Scholar]
- 11.Crotty Alexander LE, Drummond CA, Hepokoski M, et al. Chronic inhalation of e-cigarette vapor containing nicotine disrupts airway barrier function and induces systemic inflammation and multi-organ fibrosis in mice. Am J Physiol Regul Integr Comp Physiol 2018; 314: R834–R847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lappas AS, Tzortzi AS, Konstantinidi EM, et al. Short-term respiratory effects of e-cigarettes in healthy individuals and smokers with asthma. Respirology 2018; 23: 291–297. [DOI] [PubMed] [Google Scholar]
- 13.Farsalinos KE, Yannovits N, Sarri T, et al. Carbonyl emissions from a novel heated tobacco product (IQOS): comparison with an e-cigarette and a tobacco cigarette. Addiction 2018; 113: 2099–2106. [DOI] [PubMed] [Google Scholar]
- 14.Mercer BA, Kolesnikova N, Sonett J, et al. Extracellular regulated kinase/mitogen activated protein kinase is up-regulated in pulmonary emphysema and mediates matrix metalloproteinase-1 induction by cigarette smoke. J Biol Chem 2004; 279: 17690–17696. [DOI] [PubMed] [Google Scholar]
- 15.Laurent P, Janoff A, Kagan HM. Cigarette smoke blocks cross-linking of elastin in vitro. Am Rev Respir Dis 1983; 127: 189–192. [DOI] [PubMed] [Google Scholar]
- 16.Wylam ME, Sathish V, VanOosten SK, et al. Mechanisms of cigarette smoke effects on human airway smooth muscle. PLoS One 2015; 10: e0128778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Vogel ER, VanOosten SK, Holman MA, et al. Cigarette smoke enhances proliferation and extracellular matrix deposition by human fetal airway smooth muscle. Am J Physiol Lung Cell Mol Physiol 2014; 307: L978–L986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chen L, Ge Q, Tjin G, et al. Effects of cigarette smoke extract on human airway smooth muscle cells in COPD. Eur Respir J 2014; 44: 634–646. [DOI] [PubMed] [Google Scholar]
- 19.Lerner CA, Sundar IK, Yao H, et al. Vapors produced by electronic cigarettes and e-juices with flavorings induce toxicity, oxidative stress, and inflammatory response in lung epithelial cells and in mouse lung. PLoS One 2015; 10: e0116732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jolly MK, Ward C, Eapen MS, et al. Epithelial-mesenchymal transition, a spectrum of states: role in lung development, homeostasis, and disease. Dev Dyn 2018; 247: 346–358. [DOI] [PubMed] [Google Scholar]
- 21.Prakash YS, Pabelick CM, Sieck GC. Mitochondrial dysfunction in airway disease. Chest 2017; 152: 618–626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Guerra F, Guaragnella N, Arbini AA, et al. Mitochondrial dysfunction: a novel potential driver of epithelial-to-mesenchymal transition in cancer. Front Oncol 2017; 7: 295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Grigg J, Walters H, Sohal SS, et al. Cigarette smoke and platelet-activating factor receptor dependent adhesion of Streptococcus pneumoniae to lower airway cells. Thorax 2012; 67: 908–913. [DOI] [PubMed] [Google Scholar]
- 24.Miyashita L, Suri R, Dearing E, et al. E-cigarette vapour enhances pneumococcal adherence to airway epithelial cells. Eur Respir J 2018; 51: 1701592. [DOI] [PMC free article] [PubMed] [Google Scholar]