Abstract
Sentinel macrophages in the lymph node provide a first line of defense against invading viruses. A new study visualizes inflammasome activation in virally infected nodal macrophages in mice and shows that this activation augments both innate and adaptive immunity.
Lymph nodes are specialized battlegrounds in which immune cells encounter a diverse array of pathogens actively conveyed from peripheral tissues. Although the node is a crucial location of the initiation of adaptive immunity, it also functions as a barrier against systemic pathogen dissemination. Just inside the node’s confines, a continuous layer of subcapsular sinus (SCS) macrophages forms the tissue-lymph interface and immediately encounters lymph-borne pathogens that reach the node1,2. SCS macrophages sequester incoming virions, such as those of modified vaccinia Ankara (MVA) virus, a replication-deficient poxvirus that is commonly used as an experimental vaccine vector. The macrophages respond to viral infection in an inflammation-dependent manner3,4.
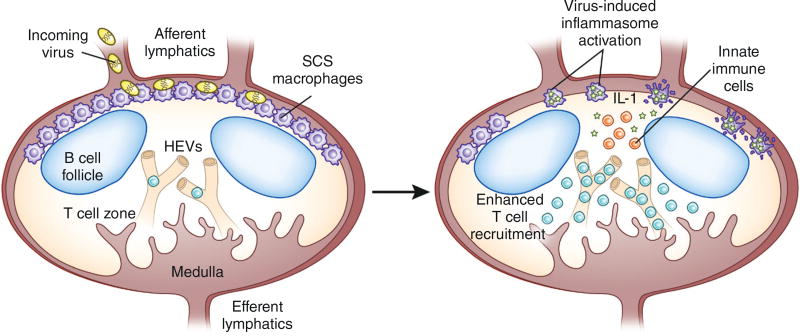
Inflammasomes are large, cytosolic multiprotein complexes that sense intracellular pathogens or danger signals and that initiate inflammatory processes. Poxviruses and other DNA viruses activate inflammasomes after triggering cytoplasmic DNA sensors, such as AIM2 (refs. 5,6), which leads to the rapid polymerization of the common adaptor protein apoptosis-associated speck-like protein containing a caspase-recruitment domain (ASC, also known as PYCARD). ASC forms large (micrometer) filamentous scaffolds, which are referred to as ASC specks, that recruit and activate caspase-1, resulting in the maturation of interleukin (IL)-1β. Although inflammasome activation occurs during infections with many different viruses and is an important aspect of immune control, the precise spatiotemporal kinetics with which this occurs in vivo are unknown. In this issue of Nature Medicine, Sagoo et al.7 visualize this inflammasome activation in MVA-infected SCS macrophages in vivo and describe important downstream effects on both innate and adaptive antiviral immunity (Fig. 1).
Figure 1.
Inflammasome activation in SCS macrophages enhances innate and adaptive immunity. SCS macrophages trap incoming virions and become infected. Sagoo et al.7 develop a method for visualizing inflammasome activation in mice by tagging the inflammasome protein ASC with GFP and analyzing the generation and release of ASC specks (as shown by stars). Macrophages with activated inflammasomes undergo pyroptosis, which liberates specks and mobilizes innate immune effectors (orange). Inflammatory cytokine (such as IL-1) and chemokine production further augments immunity, and increased numbers of CD8+ T cells (teal) are recruited into the lymph node through the high endothelial venules (HEVs).
The authors first visualized inflammasome activation by microscopy in MVA-infected, bone marrow–derived macrophages in vitro. To visualize inflammasome activity, Sagoo et al.7 generated a fusion protein of ASC and GFP in these cells (ASC-GFP), and they analyzed the redistribution of diffuse, cytoplasmic GFP signal to concentrated GFP fluorescence in large perinuclear ASC specks. After this in vitro proof of principle, the authors generated mice with myeloid cells expressing ASC-GFP, including the SCS macrophages that MVA infects in vivo. Within an hour of footpad MVA infection of the mice, specks appeared in the SCS macrophages present in the draining lymph node. Specks peaked within the next few hours and gradually disappeared over the first 12 h after infection. Thus, for the first time, the authors demonstrate a rapid, spatially restricted surge of inflammasome activation upon viral infection in vivo7.
Why was ASC speck formation confined to the period up to 12 h after infection? Lymph node infection with MVA rapidly depletes SCS macrophages; this clearly precludes sustained inflammasome activation4. Sagoo et al.7 thus examined macrophage death via pyroptosis—cell death that is initiated by inflammasome activation and characterized by pore formation, chromatin condensation, cellular swelling and rupture8. MVA-infected, bone marrow–derived macrophages exhibited inflammasome-dependent pyroptotic death in vitro that was not transmitted to neighboring cells, which suggests that direct infection is required for the macrophage death observed in vivo. To characterize macrophage death in vivo, the authors injected a cell-permeant DNA dye to label lymph node cells, and they concurrently imaged nuclear condensation (representing pyroptosis) and ASC speck formation in SCS macrophages. Indeed, macrophages with activated inflammasomes progressed rapidly to cell death through pyroptosis.
Bursting pyroptotic cells release their cytosolic contents, including oligomerized ASC, which the authors found remained visible for hours in vivo. These extracellular ASC specks are known to be catalytically active and capable of propagating inflammation upon reaching the cytoplasm of phagocytosing innate immune cells9. Sagoo et al.7 found that innate immune effector cells in MVA-infected nodes recognized specks within minutes of the specks’ release, clustering in speck-rich areas of the node and even phagocytosing the specks. This led to a rapid, inflammasome-dependent burst of chemokines and the recruitment of neutrophils, monocytes and natural killer cells to the inflamed node. SCS macrophage inflammasome activation also dramatically enhanced the adaptive immune response, with higher recruitment of naïve MVA-specific CD8+ T cells to the lymph, leading to greater numbers of virus-specific effectors and a broadened T cell repertoire.
Although other groups have reported the importance of the inflammasome in SCS macrophages after viral infection3,9, the visualization by Sagoo et al.7 of inflammasome activation in vivo as a spatially defined wave extends our understanding of SCS macrophages in viral infections. SCS macrophages have been dubbed immune ‘flypaper’ on the basis of their efficient acquisition of lymph-borne particulates1. The programmed pyroptosis of macrophages to disseminate ASC specks, however, makes them more similar to a network of land mines positioned at the entrance of lymph nodes, exploding upon infection rather than acting as a simple filter for incoming pathogens. It will be important to determine whether this occurs in other cells that also become infected, such as dendritic cells (DCs)10. As DCs (and not macrophages) prime T cell responses in the node, DC death could be costly to the host, although it may be necessary to prevent intracellular pathogen replication. It will be of great interest to examine both the contribution of inflammasome-driven pyroptosis to the control of viruses that replicate and spread in lymph nodes, and the consequences of programmed macrophage deletion.
The inflammatory amplification of adaptive immunity also raises possibilities for rational vaccine design. Strategies to deliberately trigger nodal macrophage inflammasomes could be used as an adjuvant for many types of vaccines, including simple protein-based vaccines. As a testament to the importance of inflammasome activation for controlling virus infection, MVA (and other large DNA viruses) encode proteins that block inflammasome activation. Indeed, the genomic deletion of just one of these immunomodulatory proteins dramatically reduces virulence in replicating poxviruses, and it enhances T cell responses in an MVA-based vaccine candidate11,12. Shedding light on inflammasomes in vivo could further enhance our ability to manipulate activation at appropriate times during the immune response.
Footnotes
COMPETING FINANCIAL INTERESTS
The author declares no competing financial interests.
References
- 1.Junt T, et al. Nature. 2007;450:110–114. doi: 10.1038/nature06287. [DOI] [PubMed] [Google Scholar]
- 2.Hickman HD, et al. Nat. Immunol. 2008;9:155–165. doi: 10.1038/ni1557. [DOI] [PubMed] [Google Scholar]
- 3.Kastenmüller W, Torabi-Parizi P, Subramanian N, Lämmermann T, Germain RN. Cell. 2012;150:1235–1248. doi: 10.1016/j.cell.2012.07.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gaya M, et al. Science. 2015;347:667–672. doi: 10.1126/science.aaa1300. [DOI] [PubMed] [Google Scholar]
- 5.Hornung V, et al. Nature. 2009;458:514–518. doi: 10.1038/nature07725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rathinam VA, et al. Nat. Immunol. 2010;11:395–402. doi: 10.1038/ni.1864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sagoo PGZ, et al. Nat. Med. 2016;22:64–71. doi: 10.1038/nm.4016. [DOI] [PubMed] [Google Scholar]
- 8.Jorgensen I, Miao EA. Immunol. Rev. 2015;265:130–142. doi: 10.1111/imr.12287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Franklin BS, et al. Nat. Immunol. 2014;15:727–737. doi: 10.1038/ni.2913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gerner MY, Torabi-Parizi P, Germain RN. Immunity. 2015;42:172–185. doi: 10.1016/j.immuni.2014.12.024. [DOI] [PubMed] [Google Scholar]
- 11.Gerlic M, et al. Proc. Natl. Acad. Sci. USA. 2013;110:7808–7813. doi: 10.1073/pnas.1215995110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Perdiguero B, et al. PLoS One. 2012;7:e48524. doi: 10.1371/journal.pone.0048524. [DOI] [PMC free article] [PubMed] [Google Scholar]