Abstract
Reovirus, which possesses a 10-segmented double-stranded RNA genome, mediates superior antitumor effects via not only virus replication in a tumor cell-specific manner but also other mechanisms distinct from virus replication. Several groups, including ours, reported the reovirus-mediated downregulation of hypoxia inducible factor-1α (HIF-1α) following infection in cultured tumor cells; however, it remained to be clarified whether reovirus downregulates the expression of HIF-1α and its target genes in tumor-bearing hosts. We found that reovirus induced significant downregulation of protein levels of HIF-1α and its target genes in the subcutaneous tumors at 120 h post-systemic administration. Expression of reovirus capsid protein σ3 was found in the pimonidazole-positive hypoxic area in the tumor. Significant levels of tumor cell apoptosis were not found in the tumors of reovirus-treated mice at this time point, suggesting that reovirus-mediated tumor cell killing did not largely contribute to the downregulation of HIF-1α protein levels in the tumors. UV-inactivated reovirus did not induce downregulation of HIF-1α expression in the tumors, indicating that virus replication was indispensable for downregulation of HIF-1α expression in the subcutaneous tumors. This study provides important information for the development of reovirus-mediated virotherapy against various types of tumors.
Keywords: reovirus, HIF-1α, hypoxia, tumor microenvironment, oncolytic virus
Introduction
Solid tumors contain hypoxic areas because tumor blood vessels are structurally and functionally abnormal; i.e., they exhibit high permeability, excessive tortuosity, branching, shunts, and lack of pericytes.1 Hypoxia inducible factor-1α (HIF-1α), which is a principal regulator for the adaptive transcriptional responses to low-oxygen conditions, is stabilized under hypoxic conditions, whereas HIF-1α is subjected to ubiquitination and proteasome-mediated degradation under normoxic conditions.2 HIF-1α translocates to the nucleus, forms heterodimers with HIF-1β, and binds to hypoxia-response elements (HREs) in the promoters of target genes, leading to expression of the target genes.3 HIF-1α target genes include various genes important for the growth, survival, and metastasis of tumor cells, such as solute carrier family 2 member 1 (SLC2A1), ATP binding cassette subfamily B member 1 (ABCB1), and vascular endothelial growth factor (VEGF).4, 5, 6 HIF-1α regulates the tumor microenvironment, which is increasingly recognized as a key factor for cancer therapy, through the regulation of HIF-1α target gene expression.7 Moreover, HIF-1α is involved in the maintenance of cancer stem cells and the immune-suppressive environment in the tumors.8, 9 Thus, HIF-1α is a potential target for cancer therapeutics. A number of HIF-1α inhibitors have been synthesized and have proceeded to clinical trials.10
Recently, much attention has been focused on oncolytic viruses, which show efficient infection in a tumor cell-specific manner, leading to efficient tumor cell lysis. Now more than 10 types of oncolytic viruses, including adenovirus, herpesvirus, and vaccinia virus, have been developed.11 Clinical trials, including phase III trials, using oncolytic viruses are internationally going. In 2015, the US Food and Drug Administration (FDA) approved the first oncolytic virotherapy, talimogene laherparepvec (T-VEC), for the treatment of metastatic melanoma that cannot be removed surgically.12 This virus was subsequently approved in Europe and Australia.13
Among various types of oncolytic viruses, mammalian orthoreovirus type 3 Dearing (hereafter reovirus), which is a non-enveloped, non-pathogenic RNA virus containing a 10-segmented double-stranded RNA genome in the virion, has various unique properties as an oncolytic virus, in addition to efficient tumor cell lysis activity.14 First, because reovirus can be intravenously administered to patients,15 it has the potential to target both primary and metastatic tumor sites. Second, reovirus efficiently activates antitumor immunity via various mechanisms, including activation of innate immunity, release of tumor antigens from dying tumor cells, and inhibition of immune-suppressive cells.16, 17 Combination therapy using reovirus and immune checkpoint inhibitors has shown promising results.18 Third, reovirus shows superior safety profiles. Clinical studies have reported minimal side effects in reovirus-administered patients.19 Due to these unique characteristics, the FDA has granted fast track designation for the reovirus variant Reolysin. In addition to these properties, reovirus has recently been demonstrated to induce downregulation of HIF-1α protein levels in cultured tumor cells.20, 21 HIF-1α is involved in the growth, survival, and malignancy of tumor cells in the hypoxic tumor microenvironment, as described above, suggesting that reovirus-mediated downregulation of HIF-1α contributes to the in vivo antitumor effects of reovirus; however, it remains to be clarified whether reovirus downregulates HIF-1α expression in tumor-bearing hosts following systemic administration.
In this study, we examined whether systemic administration of reovirus induced downregulation of the expression of HIF-1α and its target genes in the subcutaneous tumors. Our results showed that reovirus infected tumor cells not only in the normoxic area but also the pimonidazole-positive hypoxic area, and that HIF-1α protein levels in the tumors were efficiently reduced at 120 h following intravenous administration of reovirus. In addition, HIF-1α target gene expressions in the tumors were also reduced following systemic administration. On the other hand, UV-inactivated reovirus (UV-Reo) failed to mediate downregulation of HIF-1α in the tumors. To the best of our knowledge, this study is the first report showing oncolytic virus-induced downregulation of the expression of HIF-1α and its target genes in solid tumors.
Results
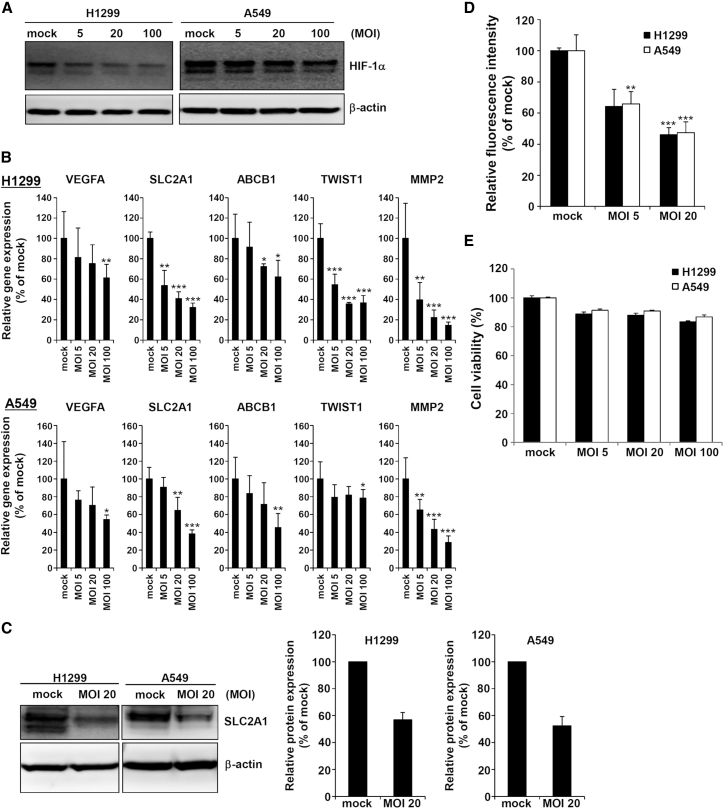
Reovirus Induced Downregulation of HIF-1α Target Genes in Tumor Cells
Several groups, including ours, previously showed that reovirus efficiently reduced the HIF-1α protein levels in cultured tumor cells;20, 21, 22 however, it remained to be fully elucidated whether the expression of HIF-1α target genes was really downregulated following reovirus infection in the cells. In order to examine whether reovirus-mediated downregulation of HIF-1α expression resulted in the transcriptional suppression of HIF-1α target genes, the mRNA levels of several HIF-1α target genes in H1299 and A549 cells were evaluated 24 h following treatment with reovirus. We previously demonstrated that H1299 cells were susceptible to reovirus infection, whereas A549 cells were resistant to reovirus infection.23 Consistent with the previous studies,20, 21, 22 we found that HIF-1α protein levels were downregulated in a dose-dependent manner in the tumor cells following treatment with reovirus, although reovirus-mediated downregulation of HIF-1α in A549 cells was less efficient, compared with that in H1299 cells (Figure 1A). mRNA levels of SLC2A1, ABCB1, matrix metalloproteinase 2 (MMP2), twist family bHLH transcription factor 1 (TWIST1), and VEGFA, which are well-known as HIF-1α target genes, were dose dependently reduced in H1299 and A549 cells following reovirus infection (Figure 1B). Moreover, reovirus infection downregulated the SLC2A1 protein levels and glucose uptake (Figures 1C and 1D). Reduction in the viabilities of these cells at 24 h post-infection was minimal, indicating that reovirus-mediated tumor cell lysis did not significantly contribute to the downregulation of the HIF-1α target genes at this time point (Figure 1E). These results indicated that reovirus-mediated downregulation of HIF-1α expression resulted in transcriptional suppression of HIF-1α target genes in tumor cells.
Figure 1.
Reovirus-Mediated Downregulation of HIF-1α Target Genes in Cultured Tumor Cells
H1299 and A549 cells were treated with reovirus at the indicated MOIs under hypoxic conditions for 24 h. (A) HIF-1α protein levels in the cultured tumor cells following reovirus treatment. (B) mRNA levels of HIF-1α target genes in the cultured tumor cells following reovirus treatment. The data represent the mean ± SD (n = 4). *p < 0.05; **p < 0.01; ***p<0.001, compared with the mock group. (C) Protein levels of SLC2A1 in the cultured tumor cells following reovirus treatment. The band intensities were normalized by those of β-actin. The bars represent the mean ± SD (n = 3). (D) Glucose uptake in the cultured tumor cells following reovirus treatment. Relative fluorescence intensities of 2-NBDG were measured 6 h after the addition of 2-NBDG. (E) Viabilities of cultured tumor cells 24 h after reovirus treatment. The data represent the mean ± SD (n = 4). **p < 0.01; ***p < 0.001, compared with the mock group. The experiments were repeated at least twice.
Reovirus Induced Downregulation of HIF-1α in Subcutaneous Tumors following Systemic Administration
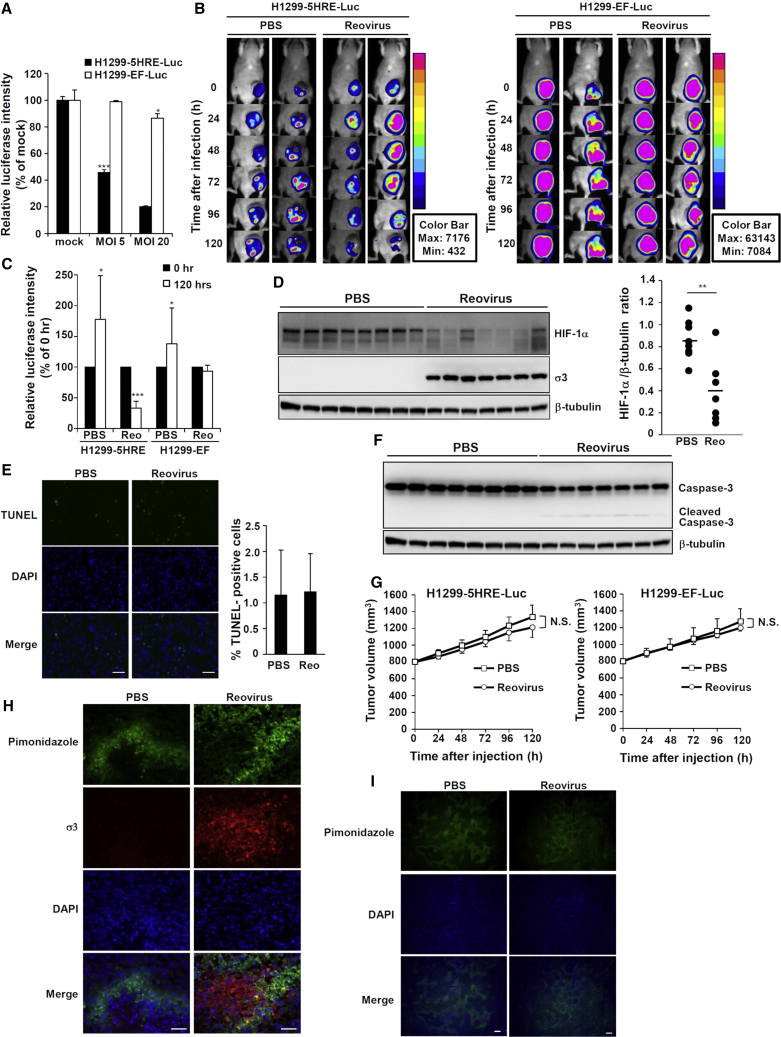
In order to examine whether reovirus downregulated HIF-1α expression levels in subcutaneous tumors following systemic administration, we first generated an H1299 transformant expressing firefly luciferase in a HIF-1α-dependent manner (H1299-5HRE-Luc) by transfection with p5HRE/NLS-ODD-Luc.24 H1299-5HRE-Luc cells expressed much lower levels of luciferase expression under normoxic conditions; on the other hand, they showed approximately 10-fold higher luciferase expression after 24 h of culture under hypoxic conditions (Figure S1). We also generated an H1299 transformant stably expressing firefly luciferase (H1299-EF-Luc) by transfection with pEF-Luc, which constantly mediates firefly luciferase expression under the EF-1α promoter, irrespective of oxygen levels. Reovirus infection induced significant downregulation of luciferase expression in H1299-5HRE-Luc cells in a dose-dependent manner, whereas reovirus-mediated downregulation of luciferase expression was not induced in H1299-EF-Luc cells (Figure 2A).
Figure 2.
Downregulation of HIF-1α in Subcutaneous Tumors following Intravenous Administration of Reovirus
(A) Luciferase expression levels in H1299-5HRE-Luc and H1299-EF-Luc cells following reovirus treatment. Cells were treated with reovirus at the indicated MOIs for 24 h, followed by a luciferase assay. The data represent the mean ± SD (n = 4). *p < 0.05; ***p < 0.001, compared with the mock group. (B) In vivo imaging analysis of luciferase expression in the tumors following intravenous administration of reovirus. Reovirus (1 × 108 PFU/mouse) or PBS was intravenously administered into the tumor-bearing mice via the tail vein. Bioluminescence intensities were then measured at the indicated time points. Data shown are representative images of at least three independent experiments. (C) Quantitative analysis of bioluminescence intensities in the tumors. Bioluminescence intensities in the tumors were measured 120 h after reovirus administration. The data represent the mean ± SD (n = 5–9). *p < 0.05; ***p < 0.001, compared with the PBS group. (D) HIF-1α protein levels in the tumors following reovirus administration. Tumor xenografts were surgically excised 120 h post-systemic administration of reovirus. Total protein lysates were prepared from the whole tumors. Protein levels of HIF-1α target genes were measured by western blotting analysis. The band intensities were normalized by those of β-tubulin. The bars represent the mean (n = 7–8). **p < 0.01, compared with the PBS-administered group. (E) Apoptosis cells in the tumors following reovirus administration. TUNEL assay was carried out using frozen sections of the tumor xenografts collected at 120 h post-systemic administration of reovirus. Scale bars, 50 μm. The quantitative statistical analysis of the percentages of TUNEL-positive cells was carried out by counting the number of TUNEL-positive cells in 10 random microscopic fields. (F) Production of the cleaved form of caspase-3 in the tumor xenografts following reovirus administration. Tumor xenografts were surgically excised at 120 h post-systemic administration of reovirus. (G) Tumor growth following reovirus administration. Tumor volumes were measured following reovirus administration at the indicated time points. The data represent the mean ± SD (n = 6–9). (H and I) Pimonidazole and reovirus capsid protein σ3-positive areas (H) and pimonidazole-positive area (I) in the tumors following reovirus administration. Immunohistochemistry with anti-pimonidazole (green), anti-reovirus capsid protein σ3 (red), and DAPI (blue) was carried out using frozen sections of the tumor xenografts at 120 h following reovirus systemic administration. Scale bars, 50 μm (H); 200 μm (I). The experiments were repeated at least twice.
We next examined luciferase expression in the subcutaneous tumors of nude mice transplanted with H1299-5HRE-Luc and H1299-EF-Luc cells following systemic administration of reovirus by in vivo imaging analysis. Luciferase expression in the H1299-5HRE-Luc tumors gradually declined following systemic administration of reovirus (Figure 2B). A large reduction in luciferase expression in the tumor was observed at 120 h after reovirus injection, whereas no reduction in luciferase expression was apparent in the H1299-EF-Luc tumors (Figures 2B and 2C). In addition to in vivo imaging analysis, we examined HIF-1α protein levels in the tumors by western blotting analysis of the whole tumor lysates at 120 h post-systemic administration of reovirus. HIF-1α protein levels in the tumors of reovirus-treated mice were significantly lower than those in the tumors of PBS-treated mice (Figure 2D). In order to examine whether reovirus-mediated tumor cell killing played a major role in the downregulation of HIF-1α following systemic administration, we examined the percentages of apoptotic tumor cells by TUNEL staining of the tumor sections and activation of caspase-3 by western blotting of the whole tumor lysates following systemic administration of reovirus. The percentages of TUNEL-positive tumor cells were comparable between PBS-treated and reovirus-treated mice 120 h after administration (Figure 2E). Only slight increases in caspase-3 activation in the tumors of reovirus-injected mice were found at this time point (Figure 2F). In addition, there were no statistically significant differences in the tumor volumes between the reovirus-administered and PBS-administered groups, at least at 120 h after administration (Figure 2G), although we found significant regression of the tumor growth after 144 h post-administration in reovirus-treated mice (Figure S2). These data indicated that reovirus-mediated tumor cell killing did not largely contribute to the downregulation of HIF-1α levels in the subcutaneous tumors, at least at this time point, following systemic administration.
Next, we examined whether reovirus infected tumor cells within the hypoxic area of tumors and whether reovirus administration altered the oxygen levels within tumors. Immunohistochemical analysis demonstrated that reovirus outer capsid protein σ3 was detected in not only the normoxic area but also the pimonidazole-positive hypoxic area of tumors (Figures 2H and S3). Areas of the pimonidazole-positive cells were comparable between the tumors of reovirus-treated and PBS-treated mice (Figure 2I). These results indicated that reovirus infected the tumor cells within the hypoxic areas in the tumors following systemic administration, and that reovirus infection did not appear to alter oxygen levels in the tumors, at least not at 120 h after systemic administration. These findings collectively indicate that, following systemic administration, reovirus infected the tumor cells in the hypoxic areas and induced downregulation of HIF-1α in the tumors before apparent induction of tumor cell killing.
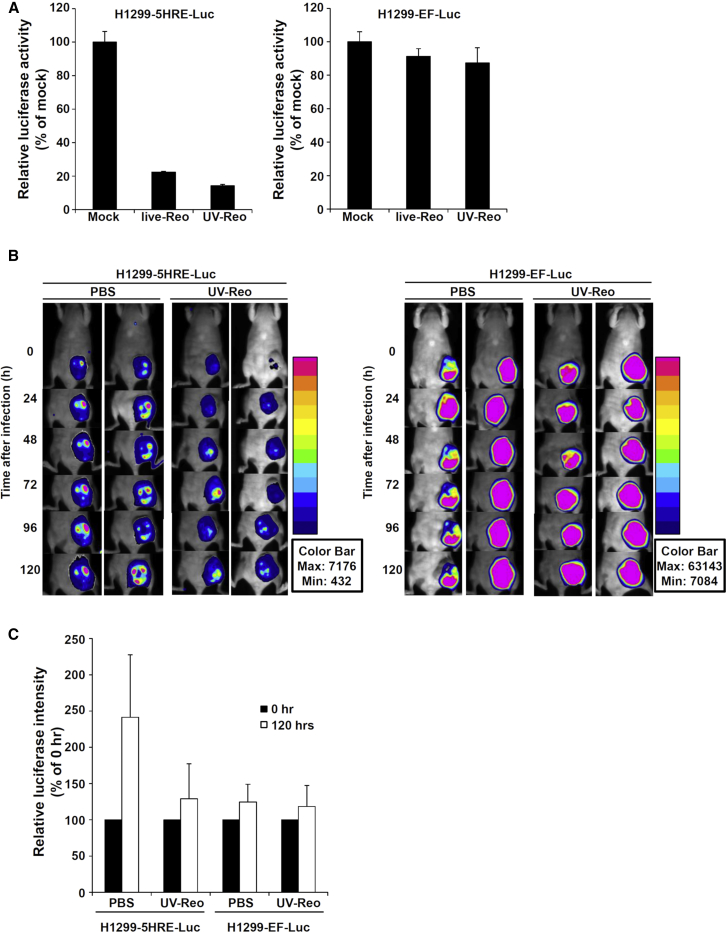
Virus Replication Was Indispensable for Reovirus-Mediated HIF-1α Downregulation in Subcutaneous Tumors following Systemic Administration
We previously demonstrated that UV-Reo efficiently induced downregulation of HIF-1α levels in cultured tumor cells,22 indicating that virus replication was not necessary for reovirus-mediated downregulation of HIF-1α in tumor cells. In the present study, in order to examine whether reovirus replication was necessary for downregulation of HIF-1α in subcutaneous tumors following systemic administration, UV-Reo was intravenously administered to H1299-5HRE-Luc tumor- and H1299-EF-Luc tumor-bearing mice, followed by in vivo imaging analysis. The results showed that UV-Reo mediated downregulation of luciferase expression at a level comparable with that mediated by live reovirus in H1299-5HRE-Luc cells 24 h after treatment, whereas no statistically significant reduction in luciferase expression was found in H1299-EF-Luc cells following treatment with live reovirus and UV-Reo (Figure 3A). These data indicated that virus replication was not indispensable for HIF-1α downregulation in cultured tumor cells. On the other hand, systemic administration of UV-Reo failed to reduce the luciferase expression in not only H1299-EF-Luc subcutaneous tumors but also H1299-5HRE-Luc tumors of the mice (Figures 3B and 3C). These results indicated that, in contrast with reovirus-mediated downregulation of HIF-1α in cultured tumor cells, virus replication was indispensable for the downregulation of HIF-1α expression in the subcutaneous tumors following systemic administration of reovirus.
Figure 3.
The Effects of Intravenous Administration of UV-Reo on HIF-1α Expression in Subcutaneous Tumors
(A) Luciferase expression levels in H1299-5HRE-Luc and H1299-EF-Luc cells following treatment with UV-Reo. Cells were treated with UV-Reo at an MOI of 20 for 24 h, followed by a luciferase assay. The data represent the mean ± SD (n = 4). (B) In vivo imaging analysis of bioluminescence intensities in the tumors following UV-Reo administration. UV-Reo was intravenously administered into the tumor-bearing mice via the tail vein at a dose of 1 × 108 PFU/mouse. Imaging analysis was carried out at the indicated time points. Data shown are representative images of at least two independent experiments. (C) Quantitative analysis of bioluminescence intensities in the tumors. Bioluminescence intensities in the tumors were measured 120 h after reovirus administration. The data represent the mean ± SD (n = 3). The experiments were repeated at least twice.
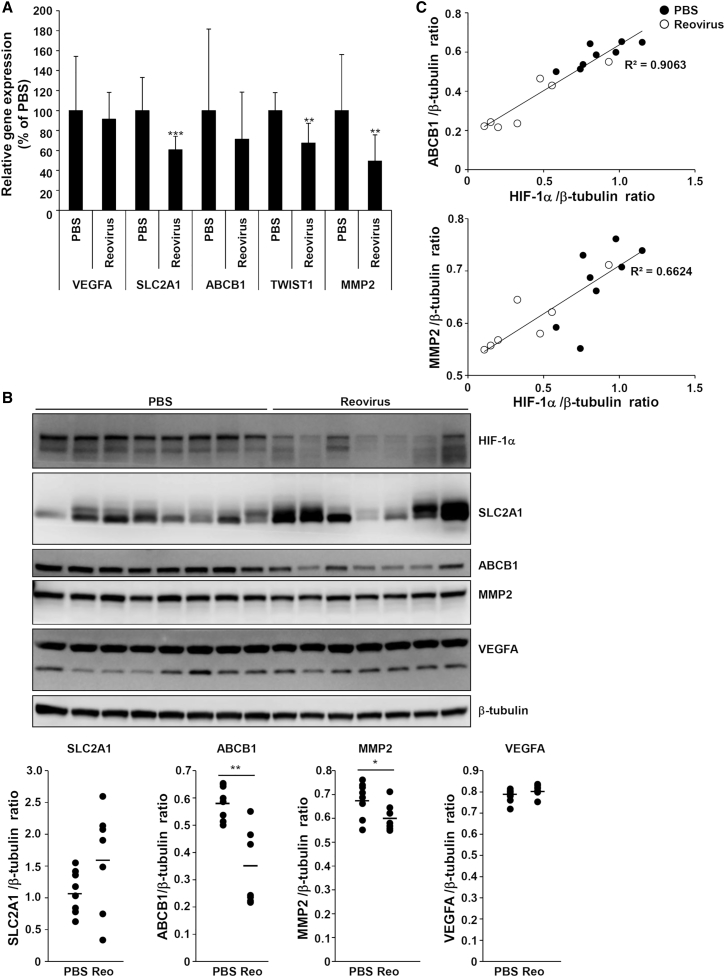
Reovirus-Mediated Downregulation of HIF-1α Led to a Reduction in HIF-1α Target Gene Expression in the Tumors
In order to examine whether reovirus-mediated downregulation of HIF-1α led to a reduction in HIF-1α target gene expression in the tumors, we determined the expression levels of HIF-1α target genes in the tumors. mRNA levels of SLC2A1, TWIST1, and MMP2 in the tumors were significantly reduced following systemic administration of reovirus (Figure 4A). Lower protein levels of the HIF-1α target genes, including ABCB1, in the tumors were demonstrated by western blotting of the whole tumor lysates, although statistically significant differences in the protein levels of SLC2A1 and VEGFA were not found in the tumors of PBS- and reovirus-administered mice (Figure 4B). Protein levels of MMP2 were slightly but statistically significantly reduced in the tumors of reovirus-administered mice. Moreover, relatively strong correlations between the protein levels of HIF-1α and those of ABCB1 (R2 = 0.9063) and MMP2 (R2 = 0.6624) were found in the tumors of PBS- and reovirus-administered mice (Figure 4C). These results indicated that reovirus downregulated the expression levels of not only HIF-1α but also its target genes in the tumors following systemic administration.
Figure 4.
Downregulation of HIF-1α Target Genes in Subcutaneous Tumors following Intravenous Administration of Reovirus
Total RNA and protein were recovered from the whole tumors at 120 h post-intravenous administration of reovirus. (A) mRNA levels of HIF-1α target genes in the tumors at 120 h following reovirus administration. The data represent the mean ± SD (n = 7–8). **p < 0.01; ***p < 0.001, compared with the PBS-administered group. (B) Protein levels of HIF-1α target genes in the tumors at 120 h following reovirus administration. Band intensities were normalized by those of β-tubulin. Note that the images of HIF-1α and β-tubulin are the same as those shown in Figure 2. The bars represent the mean (n = 7–8). *p < 0.05; **p < 0.01, compared with the PBS-administered group. (C) Scatterplot of the protein levels of HIF-1α versus those of HIF-1α target genes (ABCB1 and MMP2) in the tumors at 120 h following reovirus administration. The experiments were repeated at least twice.
Discussion
Hypoxia is a feature of the tumor microenvironment. HIF-1α drives the transcription of many target genes that are important for the growth, survival, and malignant alteration of tumors, indicating that HIF-1α is a crucial target of cancer therapy.7 Previous studies reported that reovirus induced downregulation of HIF-1α in cultured tumor cell lines,20, 21, 22 but it remains to be clarified whether reovirus downregulates the expression of HIF-1α and its target genes in tumor-bearing hosts following systemic administration. In this study, we demonstrated that reovirus induced downregulation of HIF-1α and its target genes in the subcutaneous tumors following intravenous administration before apparent induction of tumor cell apoptosis.
Our major question before beginning this study was whether reovirus infected tumor cells in the hypoxic areas, which are distant from blood vessels, of tumors following systemic administration. Our results showed that reovirus σ3 protein was indeed present in the pimonidazole-positive hypoxic areas at 120 h following systemic administration, indicating that reovirus infected the tumor cells in the hypoxic areas. However, in vivo imaging analysis demonstrated that it took 120 h to mediate downregulation of HIF-1α in the tumors following systemic administration, whereas significant downregulation of HIF-1α was observed at 24 h after addition of reovirus in human cultured tumor cells in vitro.22 In addition, UV-Reo did not appear to induce downregulation of HIF-1α in the subcutaneous tumors, although we previously reported that UV-Reo induced efficient downregulation of HIF-1α at a level comparable with live reovirus in the cultured tumor cells, and that double-stranded RNA virus genome was involved in the induction of reovirus-mediated downregulation of HIF-1α.22 In consideration of all these findings, we conclude that systemically administered reovirus infected the tumor cells in the non-hypoxic areas near the blood vessels, leading to production of progeny virus. Subsequently, progeny virus released from the infected tumor cells in the non-hypoxic areas infected the tumor cells in the hypoxic areas, leading to efficient replication of the virus genome and downregulation of HIF-1α in the tumor cells in the hypoxic areas. Reovirus infection was not disturbed in the cultured tumor cells under a hypoxic condition.25 Alternatively, double-stranded RNA virus genome might be released from the infected cells and taken up by tumor cells in the hypoxic areas, leading to downregulation of HIF-1α. On the other hand, injected UV-Reo was also taken up by tumor cells in the non-hypoxic areas, but progeny virus was not produced. Therefore, UV-Reo did not infect the tumor cells in the hypoxic areas or mediate downregulation of HIF-1α in the tumors. In addition, compared with the in vitro condition, lower amounts of reovirus infected the tumor cells in the subcutaneous tumors following intravenous administration. We previously demonstrated that infection of reovirus at more than MOI 5 was necessary for efficient downregulation of HIF-1α in tumor cells.22 In the case of our present experiments, it probably took 120 h for the production of sufficient amounts of progeny virus, subsequent infection of progeny virus, and virus genome replication in the tumor cells in the hypoxic areas.
This study demonstrated that systemic administration of reovirus resulted in downregulation of HIF-1α and its target genes in the solid tumors before apparent induction of tumor cell apoptosis. HIF-1α plays an important role in maintenance of the tumor microenvironment, including suppression of antitumor immunity and maintenance of cancer stem cells, indicating that inhibition of HIF-1α leads to alteration of the tumor microenvironment.8, 9 Previous studies demonstrated that reovirus induced alterations of the tumor microenvironment following administration.16, 17 For example, reovirus administration in tumor-bearing hosts resulted in the activation of immune cells and induction of lymphocyte infiltration into tumors.16, 26, 27 Reovirus-mediated downregulation of HIF-1α would thus contribute, at least in part, to reovirus-mediated alteration of the tumor microenvironment and subsequent antitumor effects of reovirus.
In this study, systemic administration of reovirus induced the downregulation of ABCB1 and MMP2 protein levels in the tumors, whereas statistically significant differences in the protein levels of SLC2A1 and VEGFA were not found in the tumors of PBS- and reovirus-administered mice. Expression of HIF-1α target genes is regulated by not only HIF-1α but also other transcriptional factors, including NF-κB.28 Reovirus-mediated innate immune responses and/or an inflammatory environment in the tumor would result in activation of NF-κB, leading to upregulation of HIF-1α target genes. Reovirus-mediated suppression of the expression of HIF-1α target genes would be offset by NF-κB-induced upregulation of HIF-1α target gene expression. Several HIF-1α target genes are also expressed on normal cells. For example, SLC2A1 is highly expressed on activated CD4+ lymphocytes.29 In our present study, expression of HIF-1α target genes in blood cells infiltrated into the tumors was detected in the western blotting analysis.
The mechanism of reovirus-induced downregulation of HIF-1α remains to be clarified. We previously demonstrated that reovirus double-stranded RNA genomes were involved in the reovirus-mediated downregulation of HIF-1α.22 In addition to reovirus, oncolytic H-1 parvovirus, which contains a single-stranded DNA genome, and Newcastle disease virus, which has a single-stranded RNA genome, were also demonstrated to downregulate HIF-1α protein levels in cultured tumor cells.30, 31 On the other hand, other viruses, including Epstein-Bar virus (EBV), Kaposi’s sarcoma-associated herpes virus (KSHV), hepatitis B virus (HBV), hepatitis C virus (HCV), and human papillomavirus (HPV), induced upregulation of HIF-1α.32, 33, 34, 35, 36 Thus, the effects of virus infection on the HIF-1α expression levels and mechanism of virus-induced downregulation of HIF-1α differ among the virus types.
In summary, this study demonstrated that reovirus downregulated the expression of HIF-1α and its target genes in solid tumors before its apparent induction of tumor cell apoptosis following systemic administration. Virus replication was indispensable for reovirus-mediated HIF-1α downregulation in the tumors. This study provides important information for the clinical application of reovirus in cancer therapy.
Materials and Methods
Cell Lines and Virus
Human and mouse cultured cells were maintained in an appropriate culture medium containing 5% or 10% fetal bovine serum and antibiotics at 37°C in a 5% CO2 atmosphere. All cell lines were obtained in the years from 2007 to 2013. All experiments were done using cells passaged less than 20 times. The authentication was performed by the vendor, but not by the authors. For hypoxic exposure, cells were incubated in a hypoxic chamber (Veritas, Tokyo, Japan) in the presence of 1% O2, 5% CO2/balance N2 at 37°C. Reovirus was grown in L929 cells (ATCC) and purified by CsCl ultracentrifugation, followed by overnight dialysis. Biological titers of reovirus were determined by a plaque-forming assay using L929 cells. For inactivation treatment, reovirus was irradiated with UV for 1 h. Inactivation of reovirus was confirmed by the cytotoxic effects on L929 cells using a cell counting kit-8 (Dojindo Laboratories, Kumamoto, Japan) according to the manufacturer’s instructions.
Isolation of H1299 Transformants Expressing Firefly Luciferase
H1299 cells (ATCC) were transfected with p5HRE/NLS-ODD-Luc (kindly provided by Dr. H. Harada, Kyoto University, Kyoto, Japan)24 using Lipofectamine 2000 (Thermo Fisher Scientific, San Jose, CA, USA), followed by a 2-week culture in the culture medium containing 500 μg/mL G418 (Nacalai Tesque, Kyoto, Japan). Antibiotic-resistant colonies were isolated, generating H1299-HRE-Luc cells. H1299-EF-Luc cells, which constantly mediate firefly luciferase gene expression under the control of the elongation factor-1α (EF-1α) promoter, were similarly generated as described above using pEF-Luc. pEF-Luc was constructed by insertion of the firefly luciferase gene derived from pGL3-Control (Promega, Madison, WI, USA) into the multicloning site of pEF/myc/nuc (Thermo Fisher Scientific).
Real-Time RT-PCR Analysis
H1299 and A549 cells (ATCC) were seeded on a 24-well plate at 4 × 104 cells/well. On the following day, reovirus was added to the cells at the indicated MOIs. Cells were incubated under hypoxic conditions for 24 h after the addition of reovirus. Total RNA was then recovered using ISOGEN (Nippon Gene, Tokyo, Japan) according to the manufacturer’s instructions. cDNA was synthesized using a Superscript VILO cDNA synthesis kit (Thermo Fisher Scientific). Real-time RT-PCR was performed using THUNDERBIRD SYBR qPCR Mix (TOYOBO, Osaka, Japan) and a StepOnePlus System (Thermo Fisher Scientific). The values were normalized by the mRNA levels of a housekeeping gene, 18S rRNA. The primer sequences used in this study are described in Table S1. For real-time RT-PCR analysis of in vivo gene expression in the subcutaneous tumors, tumor xenografts were surgically excised 120 h post-systemic administration of reovirus, followed by isolation of total RNA using ISOGEN (Nippon Gene). mRNA levels of HIF-1α target genes were then measured as described above.
Western Blotting Analysis
Cell lysates were prepared after a 24-h incubation with reovirus by using radioimmunoprecipitation assay (RIPA) buffer (Thermo Fisher Scientific) containing protease inhibitor cocktail (Sigma, St. Louis, MO, USA). The lysates were analyzed by SDS-PAGE, followed by electro-transfer onto a polyvinylidene fluoride (PVDF) membrane. Western blotting analyses were carried out by using anti-SLC2A1 monoclonal antibody (clone: SPM498, 1:5,000; Abcam, Cambridge, MA, USA) and anti-β-actin monoclonal antibody (clone: AC-15, 1:10,000; Sigma) as primary antibodies and Chemi-Lumi One Super (Nacalai Tesque). Images were captured using an LAS-4000 system (Fujifilm, Tokyo, Japan). For western blotting analysis of the tumor lysates, tumor xenografts were surgically excised 120 h post-systemic administration of reovirus. Total protein lysates were then prepared from whole-tumor xenografts using RIPA buffer (Thermo Fisher Scientific) containing protease inhibitor cocktail (Sigma), followed by western blotting analysis as described above using anti-HIF-1α monoclonal antibody (clone: 54/HIF-1α, 1:1,000; BD Biosciences, San Jose, CA, USA), anti-reovirus σ3 monoclonal antibody (clone: 4F2, 1:2000; Developmental Studies Hybridoma Bank, Iowa City, IA, USA), anti-SLC2A1 monoclonal antibody (clone: SPM498, 1:5,000; Abcam), anti-VEGFA polyclonal antibody (1:1,000; Abcam), anti-ABCB1 polyclonal antibody (1:1,000; Novus Biologicals, Littleton, CO, USA), anti-MMP2 polyclonal antibody (1:1,000; Abcam), anti-caspase-3 polyclonal antibody (1:1,000; Cell Signaling Technology, Danvers, MA, USA), and anti-β-tubulin polyclonal antibody (1:50,000; Abcam) as primary antibodies.
Glucose Uptake Assay
Human tumor cell lines were seeded on a 96-well plate at 1 × 104 cells/well. Cells were incubated under hypoxic conditions for 72 h. Reovirus was then added to the cells at the indicated MOIs. The cells were incubated under hypoxic conditions for 24 h after the addition of reovirus, then cultured for 6 h in glucose-free culture medium containing 100 μg/mL 2-deoxy-2-[(7-nitro-2,1,3-benzoxadiazol-4-yl)amino]- D-glucose (2-NBDG) (Cayman Chemical, Ann Arbor, MI, USA). The amounts of 2-NBDG taken up by cells were measured according to the manufacturer’s instructions.
Luciferase Assay
Human tumor cell lines were seeded on a 96-well plate at 1 × 104 cells/well. On the following day, reovirus was added to the cells at the indicated MOIs. The cells were then incubated under hypoxic conditions for 24 h, followed by a luciferase assay using PicaGene LT2.0 (Toyo Ink, Tokyo, Japan) according to the manufacturer’s instructions.
In Vivo Imaging Analysis of Luciferase Expression in the Tumors
H1299-5HRE-Luc or H1299-EF-Luc cells were subcutaneously injected into the abdomen of 5-week-old female nude mice (BALB/c Slc-nu/nu; SLC, Hamamatsu, Japan). When the tumor volumes reached approximately 800 mm3, reovirus was intravenously administered into the tumor-bearing mice via the tail vein at a dose of 1 × 108 plaque-forming units (PFUs)/mouse. The tumor volume was calculated using the following formula: tumor volume (mm3) = (width)2 × (length) × (1/2). For the in vivo imaging analysis, D-Luciferin solution (4 mg/mouse; FUJIFILM Wako Pure Chemical Corporation, Osaka, Japan) was intravenously administered into the tumor-bearing mice via the tail vein. Luciferase expression was measured using NightOWL LB983 (BERTHOLD Technologies, Tokyo, Japan). All experimental procedures were approved by the Osaka University Institutional Animal Care and Use Committee in accordance with Fundamental Guidelines for Proper Conduct of Animal Experiment and Related Activities in Academic Research Institutions under the jurisdiction of the Ministry of Education, Culture, Sports, Science and Technology of Japan.
Immunohistochemistry of Tumor Tissue Sections
At 120 h after the systemic administration of reovirus, hypoxyprobe-1 (Hypoxyprobe, Burlington, MA, USA) was intravenously administered into the tumor-bearing mice at a dose of 1.2 mg/mouse via the tail vein. The tumor xenografts were surgically excised at 1 h after the administration of hypoxyprobe-1. Frozen sections of the tumor xenografts were prepared with O.C.T. Compound (Sakura Finetech, Tokyo, Japan). Immunostaining was performed using anti-reovirus σ3 monoclonal antibody (clone: 4F2, 1:15; Developmental Studies Hybridoma Bank) and anti-pimonidazole antisera (clone: PAb2627, 1:20; Hypoxyprobe) as primary antibodies. TUNEL assay was carried out using an ApopTag Fluorescein In Situ Apoptosis Detection Kit (Merck Millipore, Darmstadt, Germany) according to the manufacturer’s instructions.
Statistical Analysis
Statistical significance was determined using the Student’s t test. Data are presented as the means ± SD.
Author Contributions
Conceptualization, T.H. and F.S.; Methodology, T.H. and F.S.; Validation, T.H., H.M., and F.S.; Formal Analysis, T.H., H.M., and F.S.; Investigation, T.H. and F.S.; Resources, T.H., H.M., and F.S.; Writing – Original Draft, T.H., H.M., and F.S.; Writing – Review & Editing, T.H., H.M., and F.S.; Supervision, T.H., H.M., and F.S.; Project Administration, T.H., H.M., and F.S.; Funding Acquisition, T.H., H.M., and F.S.
Conflicts of Interest
The authors declare no competing interests.
Acknowledgments
We thank Dr. Hiroshi Harada (Graduate School of Medicine, Kyoto University, Kyoto, Japan) for providing the plasmid. We also thank Dr. Kazuo Takayama, Dr. Eiko Sakai (Graduate School of Pharmaceutical Sciences, Osaka University, Osaka, Japan), Dr. Takeshi Kobayashi, Dr. Yuta Kanai (Research Institute for Microbial Diseases, Osaka University, Osaka, Japan), Dr. Shinae Kizaka-Kondoh (School of Life Science and Technology, Tokyo Institute of Technology, Yokohama, Japan), and Dr. Takahiro Kuchimaru (Center for Molecular Medicine, Jichi Medical University, Tochigi, Japan) for their advice. This work was supported by grants-in-aid for Scientific Research (B) from the Ministry of Education, Culture, Sports, Science and Technology of Japan (MEXT; 17H04101), a grant from the Mochida Memorial Foundation for Medical and Pharmaceutical Research, and the Japanese Agency for Medical Research and Development (AMED) (grant 17am0101084j0001). T. Hotani is a Research Fellow of the Japan Society for the Promotion of Science (grant 16J05703).
Footnotes
Supplemental Information includes three figures and one table and can be found with this article online at https://doi.org/10.1016/j.omto.2018.12.012.
Supplemental Information
References
- 1.Carmeliet P., Jain R.K. Angiogenesis in cancer and other diseases. Nature. 2000;407:249–257. doi: 10.1038/35025220. [DOI] [PubMed] [Google Scholar]
- 2.Salceda S., Caro J. Hypoxia-inducible factor 1α (HIF-1α) protein is rapidly degraded by the ubiquitin-proteasome system under normoxic conditions. Its stabilization by hypoxia depends on redox-induced changes. J. Biol. Chem. 1997;272:22642–22647. doi: 10.1074/jbc.272.36.22642. [DOI] [PubMed] [Google Scholar]
- 3.Wang G.L., Jiang B.H., Rue E.A., Semenza G.L. Hypoxia-inducible factor 1 is a basic-helix-loop-helix-PAS heterodimer regulated by cellular O2 tension. Proc. Natl. Acad. Sci. USA. 1995;92:5510–5514. doi: 10.1073/pnas.92.12.5510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gleadle J.M., Ratcliffe P.J. Induction of hypoxia-inducible factor-1, erythropoietin, vascular endothelial growth factor, and glucose transporter-1 by hypoxia: evidence against a regulatory role for Src kinase. Blood. 1997;89:503–509. [PubMed] [Google Scholar]
- 5.Comerford K.M., Wallace T.J., Karhausen J., Louis N.A., Montalto M.C., Colgan S.P. Hypoxia-inducible factor-1-dependent regulation of the multidrug resistance (MDR1) gene. Cancer Res. 2002;62:3387–3394. [PubMed] [Google Scholar]
- 6.Forsythe J.A., Jiang B.H., Iyer N.V., Agani F., Leung S.W., Koos R.D., Semenza G.L. Activation of vascular endothelial growth factor gene transcription by hypoxia-inducible factor 1. Mol. Cell. Biol. 1996;16:4604–4613. doi: 10.1128/mcb.16.9.4604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Soni S., Padwad Y.S. HIF-1 in cancer therapy: two decade long story of a transcription factor. Acta Oncol. 2017;56:503–515. doi: 10.1080/0284186X.2017.1301680. [DOI] [PubMed] [Google Scholar]
- 8.Wang Y., Liu Y., Malek S.N., Zheng P., Liu Y. Targeting HIF1α eliminates cancer stem cells in hematological malignancies. Cell Stem Cell. 2011;8:399–411. doi: 10.1016/j.stem.2011.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Noman M.Z., Desantis G., Janji B., Hasmim M., Karray S., Dessen P., Bronte V., Chouaib S. PD-L1 is a novel direct target of HIF-1α, and its blockade under hypoxia enhanced MDSC-mediated T cell activation. J. Exp. Med. 2014;211:781–790. doi: 10.1084/jem.20131916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yu T., Tang B., Sun X. Development of inhibitors targeting hypoxia-inducible factor 1 and 2 for cancer therapy. Yonsei Med. J. 2017;58:489–496. doi: 10.3349/ymj.2017.58.3.489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Miest T.S., Cattaneo R. New viruses for cancer therapy: meeting clinical needs. Nat. Rev. Microbiol. 2014;12:23–34. doi: 10.1038/nrmicro3140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pol J., Kroemer G., Galluzzi L. First oncolytic virus approved for melanoma immunotherapy. OncoImmunology. 2015;5:e1115641. doi: 10.1080/2162402X.2015.1115641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fukuhara H., Ino Y., Todo T. Oncolytic virus therapy: a new era of cancer treatment at dawn. Cancer Sci. 2016;107:1373–1379. doi: 10.1111/cas.13027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dermody T.S., Parker J.S., Sherry B. Orthoreviruses. In: Knipe D.M., Howley P., editors. Fields Virol. Sixth Edition. Lippincott Williams & Wilkins; 2013. pp. 1304–1346. [Google Scholar]
- 15.Adair R.A., Roulstone V., Scott K.J., Morgan R., Nuovo G.J., Fuller M., Beirne D., West E.J., Jennings V.A., Rose A. Cell carriage, delivery, and selective replication of an oncolytic virus in tumor in patients. Sci. Transl. Med. 2012;4:138ra77. doi: 10.1126/scitranslmed.3003578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gujar S.A., Marcato P., Pan D., Lee P.W. Reovirus virotherapy overrides tumor antigen presentation evasion and promotes protective antitumor immunity. Mol. Cancer Ther. 2010;9:2924–2933. doi: 10.1158/1535-7163.MCT-10-0590. [DOI] [PubMed] [Google Scholar]
- 17.Katayama Y., Tachibana M., Kurisu N., Oya Y., Terasawa Y., Goda H., Kobiyama K., Ishii K.J., Akira S., Mizuguchi H., Sakurai F. Oncolytic reovirus inhibits immunosuppressive activity of myeloid-derived suppressor cells in a TLR3-dependent manner. J. Immunol. 2018;200:2987–2999. doi: 10.4049/jimmunol.1700435. [DOI] [PubMed] [Google Scholar]
- 18.Rajani K., Parrish C., Kottke T., Thompson J., Zaidi S., Ilett L., Shim K.G., Diaz R.M., Pandha H., Harrington K. Combination therapy with reovirus and anti-PD-1 blockade controls tumor growth through innate and adaptive immune responses. Mol. Ther. 2016;24:166–174. doi: 10.1038/mt.2015.156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Clements D., Helson E., Gujar S.A., Lee P.W. Reovirus in cancer therapy: an evidence-based review. Oncolytic Virother. 2014;3:69–82. doi: 10.2147/OV.S51321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cho I.-R., Koh S.S., Min H.-J., Park E.-H., Ratakorn S., Jhun B.H., Jeong S.H., Yoo Y.H., Youn H.D., Johnston R.N., Chung Y.H. Down-regulation of HIF-1alpha by oncolytic reovirus infection independently of VHL and p53. Cancer Gene Ther. 2010;17:365–372. doi: 10.1038/cgt.2009.84. [DOI] [PubMed] [Google Scholar]
- 21.Gupta-Saraf P., Miller C.L. HIF-1α downregulation and apoptosis in hypoxic prostate tumor cells infected with oncolytic mammalian orthoreovirus. Oncotarget. 2014;5:561–574. doi: 10.18632/oncotarget.1767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hotani T., Tachibana M., Mizuguchi H., Sakurai F. Reovirus double-stranded RNA genomes and polyI:C induce down-regulation of hypoxia-inducible factor 1α. Biochem. Biophys. Res. Commun. 2015;460:1041–1046. doi: 10.1016/j.bbrc.2015.03.147. [DOI] [PubMed] [Google Scholar]
- 23.Terasawa Y., Hotani T., Katayama Y., Tachibana M., Mizuguchi H., Sakurai F. Activity levels of cathepsins B and L in tumor cells are a biomarker for efficacy of reovirus-mediated tumor cell killing. Cancer Gene Ther. 2015;22:188–197. doi: 10.1038/cgt.2015.4. [DOI] [PubMed] [Google Scholar]
- 24.Harada H., Kizaka-Kondoh S., Itasaka S., Shibuya K., Morinibu A., Shinomiya K., Hiraoka M. The combination of hypoxia-response enhancers and an oxygen-dependent proteolytic motif enables real-time imaging of absolute HIF-1 activity in tumor xenografts. Biochem. Biophys. Res. Commun. 2007;360:791–796. doi: 10.1016/j.bbrc.2007.06.149. [DOI] [PubMed] [Google Scholar]
- 25.Figová K., Hraběta J., Eckschlager T. Anticancer efficiency of reovirus in normoxia and hypoxia. Folia Biol. (Praha) 2013;59:68–75. [PubMed] [Google Scholar]
- 26.Errington F., Steele L., Prestwich R., Harrington K.J., Pandha H.S., Vidal L., de Bono J., Selby P., Coffey M., Vile R., Melcher A. Reovirus activates human dendritic cells to promote innate antitumor immunity. J. Immunol. 2008;180:6018–6026. doi: 10.4049/jimmunol.180.9.6018. [DOI] [PubMed] [Google Scholar]
- 27.Prestwich R.J., Errington F., Ilett E.J., Morgan R.S.M., Scott K.J., Kottke T., Thompson J., Morrison E.E., Harrington K.J., Pandha H.S. Tumor infection by oncolytic reovirus primes adaptive antitumor immunity. Clin. Cancer Res. 2008;14:7358–7366. doi: 10.1158/1078-0432.CCR-08-0831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rius J., Guma M., Schachtrup C., Akassoglou K., Zinkernagel A.S., Nizet V., Johnson R.S., Haddad G.G., Karin M. NF-kappaB links innate immunity to the hypoxic response through transcriptional regulation of HIF-1α. Nature. 2008;453:807–811. doi: 10.1038/nature06905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Macintyre A.N., Gerriets V.A., Nichols A.G., Michalek R.D., Rudolph M.C., Deoliveira D., Anderson S.M., Abel E.D., Chen B.J., Hale L.P., Rathmell J.C. The glucose transporter Glut1 is selectively essential for CD4 T cell activation and effector function. Cell Metab. 2014;20:61–72. doi: 10.1016/j.cmet.2014.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cho I.R., Kaowinn S., Moon J., Soh J., Kang H.Y., Jung C.R., Oh S., Song H., Koh S.S., Chung Y.H. Oncotropic H-1 parvovirus infection degrades HIF-1α protein in human pancreatic cancer cells independently of VHL and RACK1. Int. J. Oncol. 2015;46:2076–2082. doi: 10.3892/ijo.2015.2922. [DOI] [PubMed] [Google Scholar]
- 31.Abd-Aziz N., Stanbridge E.J., Shafee N. Newcastle disease virus degrades HIF-1α through proteasomal pathways independent of VHL and p53. J. Gen. Virol. 2016;97:3174–3182. doi: 10.1099/jgv.0.000623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wakisaka N., Kondo S., Yoshizaki T., Murono S., Furukawa M., Pagano J.S. Epstein-Barr virus latent membrane protein 1 induces synthesis of hypoxia-inducible factor 1 α. Mol. Cell. Biol. 2004;24:5223–5234. doi: 10.1128/MCB.24.12.5223-5234.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cai Q., Lan K., Verma S.C., Si H., Lin D., Robertson E.S. Kaposi’s sarcoma-associated herpesvirus latent protein LANA interacts with HIF-1 alpha to upregulate RTA expression during hypoxia: latency control under low oxygen conditions. J. Virol. 2006;80:7965–7975. doi: 10.1128/JVI.00689-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yoo Y.-G., Oh S.H., Park E.S., Cho H., Lee N., Park H., Kim D.K., Yu D.Y., Seong J.K., Lee M.O. Hepatitis B virus X protein enhances transcriptional activity of hypoxia-inducible factor-1alpha through activation of mitogen-activated protein kinase pathway. J. Biol. Chem. 2003;278:39076–39084. doi: 10.1074/jbc.M305101200. [DOI] [PubMed] [Google Scholar]
- 35.Nasimuzzaman M., Waris G., Mikolon D., Stupack D.G., Siddiqui A. Hepatitis C virus stabilizes hypoxia-inducible factor 1alpha and stimulates the synthesis of vascular endothelial growth factor. J. Virol. 2007;81:10249–10257. doi: 10.1128/JVI.00763-07. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 36.Ravi R., Mookerjee B., Bhujwalla Z.M., Sutter C.H., Artemov D., Zeng Q., Dillehay L.E., Madan A., Semenza G.L., Bedi A. Regulation of tumor angiogenesis by p53-induced degradation of hypoxia-inducible factor 1α. Genes Dev. 2000;14:34–44. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.