Abstract
Transportation type may play a role in the ease with which a person can access healthy food and recreation facilities. Our objective was to determine the relationship between access to a personal vehicle and diet, food insecurity, and physical activity among public housing residents, which are typically low-income, urban populations. We conducted a cross-sectional survey of randomly selected households within two public housing communities in Baltimore, MD (2014–2015). Our independent variable was whether or not the resident had access to a personal vehicle. Our dependent variables were ‘high’ fruit & vegetable intake (≥6.7 servings/day), ‘high’ added sugar intake (≥39.9 tsp/day), food insecurity, and being physically active. We used Poisson regression with robust error variance to estimate relative risk ratios adjusted for demographics and perceived environmental factors. Our sample included 265 adults (response rate of 48%) with mean age of 45 years, 86% women, and 96% African-American. Only 42% had access to a vehicle. No significant associations existed between personal vehicle access with diet or physical activity outcomes. Access to a personal vehicle was associated with significantly lower risk of food insecurity (RR 0.76, 95%CI 0.63–0.92, p < 0.01). We found a significant association between personal vehicle access and lower risk of food insecurity; however, there were no associations with diet or exercise. Based on these results, future research might explore how transportation access influences and might possibly reduce food insecurity.
Keywords: Food supply, Public housing, Transportation, Diet, Exercise
1. Introduction
According to the Centers for Disease Control and Prevention (CDC), chronic diseases including obesity, type 2 diabetes, and cardiovascular disease are the leading causes of death and disability in the United States (Centers for Disease Control and Prevention, n.d.). The U.S. Preventive Services Task Force has recommended counseling individuals at high-risk of disease on lifestyle changes (U.S. Preventive Services Task Force, n.d.), since modifying lifestyle behaviors like diet and exercise can prevent the development or better manage these conditions in individuals with disease. While many Americans are affected by these conditions, disparities exist by socioeconomic status (SES) where low-income groups have a greater burden of disease (Ludwig et al., 2011; Min et al., 2017).
In low-income, urban households, a confluence of factors likely contributes to these disparities. First, many of these low-income households may be located in “food deserts,” which are areas characterized by poor access to healthy, affordable foods (Beaulac et al., 2009) and have been associated with increased risk of overweight/obesity (Morland et al., 2006). Second, food insecurity, which the U.S. Department of Agriculture defines as household-level economic and social conditions that contribute to limited or uncertain access to adequate food (United States Department of Agriculture, n.d.), is estimated to affect nearly a third of households whose annual income is below 185% of the poverty threshold (Coleman-Jensen et al., n.d.). Third, residents of low-income households have greater fear of falling victim to crime (Ross, 2000), which may discourage physical activity outdoors. These factors are particularly relevant to public housing developments, as they are often located in low-income, urban neighborhoods that have limited positive resources that can promote healthy lifestyles (Smith and Kelsey-Harris, 2018).
Transportation type may play a role in the ease with which a person can access healthy food and recreation facilities. In urban environments, particularly those with less reliable public transportation, use of a personal vehicle may be easier or more efficient than other transportation options. For example, Baltimore City residents using a personal vehicle in 2016 spent on average approximately 27 min commuting to work, while it took those using public transportation 49 min (U.S. Census Bureau, n.d.). For individuals living in deprived urban areas or food deserts, where access to food stores and recreation facilities may be limited, having a personal vehicle could improve their ability to travel outside their neighborhood to access healthy food and recreation facilities. A prior evaluation in Baltimore found that it takes approximately 29.1 min to travel to the nearest supermarket for residents in food deserts, but only 1.8 min for those living in high supermarket access communities (Spencer et al., 2011). Taking the bus, the most commonly used public transportation option in Baltimore City (Maryland Department of Transportation, 2018), presents particular challenges for food shopping, as prior research has cited infrequent bus schedules and the burden of heavy grocery bags as disincentives to taking public transportation to desirable supermarkets (Scammell et al., 2015). While previous research has described the challenges with public transportation, we know of no research that has explored whether access to a personal vehicle among residents in deprived areas has beneficial effects on diet, food insecurity, or exercise.
The purpose of this study was to determine the associations between access to a personal vehicle with diet, food insecurity, and physical activity among Baltimore City public housing residents. As compared to individuals without access to a personal vehicle, we hypothesized that residents with access would 1) consume more fruits & vegetables and less added sugars, 2) be less likely to report food insecurity, and 3) be more likely to be physically active.
2. Methods
2.1. Study design & recruitment
We conducted a cross-sectional survey of randomly selected households located within two public housing communities in Baltimore, MD (August 2014 to August 2015). Detailed methods have been previously published (Gudzune et al., 2018). In brief, we randomly selected 600 addresses from the 1272 units within these communities, of which 556 units were occupied and eligible for inclusion. We recruited households by mailing postcards and using up to five door-knocking attempts. Of the 556 eligible households, 266 participated (response rate 47.8%). We used a software program to facilitate data collection (EgoNet, MDLogix). Participants received a $40 gift card as compensation. The Johns Hopkins University School of Medicine Institutional Review Board approved this study.
2.2. Variables
For this analysis, our independent variable was access to a personal vehicle. Residents answered the question, “Do you have direct access to a vehicle you can use (either yours or someone else's)?” to which they responded yes/no.
Our primary dependent variables were measures of diet, food insecurity, and physical activity. For diet, participants answered food frequency questions from the National Health Interview Survey (NHIS) 5-factor dietary screener (National Cancer Institute, n.d.), which enables derivation of rough estimates of usual intake of fruits & vegetables, fiber, calcium, servings of dairy, and added sugar. These estimates are not as accurate as those from other methods such as 24-hour food recalls; however, validation research has suggested that the estimates can discriminate among individuals with regard to intake levels (high versus low) and examine relationships between diet and other variables (National Cancer Institute, n.d.). In this analysis, we estimated daily fruit & vegetable intake (servings/day) and daily added sugar intake (teaspoons/day) using the standard methods recommended by NHIS. We dichotomized these variables to indicate ‘high’ versus ‘not high’ daily intakes using the upper quartile of intakes reported in our sample (high fruit & vegetable intake ≥6.7 servings/day and high added sugar intake ≥39.9 tsp/day).
For food insecurity, we used a previously validated 2-item screener that identifies households that are food insecure (Hager et al., 2010). The screener asks respondents to indicate whether the following statements were true for their household (often true, sometimes true, or never true): “Within the past 12 months we worried whether our food would run out before we got money to buy more” and “Within the past 12 months the food we bought just didn't last and we didn't have money to get more.” We used the recommended approach (often/sometimes true versus never true to either question) to identify participants as food insecure (Hager et al., 2010).
For physical activity, we used a validated exercise screener that 1) asks respondents to think about the things they do outside of work and then rate themselves as to the amount of physical activity they get compared with others their age and sex (much more active, somewhat more active, about the same, somewhat less active, much less active), and 2) whether the respondent regularly engages in strenuous exercise (yes/no) (Ainsworth et al., 1993). We then used the recommended approach to determine whether a participant's leisure time activity level was high (much more active + strenuous activity), moderate (any other activity level + strenuous activity), low (much more active/somewhat more active/about the same + not strenuous activity), or very low (somewhat less/much less active + not strenuous activity) (Ainsworth et al., 1993). We dichotomized responses as ‘active’ if high or moderate and ‘not active’ if low or very low.
We considered a number of covariates. We included age, gender, race (black versus non-black), educational attainment (graduated high school versus not), and unemployment status (unemployed versus not unemployed). We also characterized respondents' comorbid disease burden using a previously validated approach (Seattle Index of Comorbidity) (Fan et al., 2002), which integrates age, smoking status and 7 self-reported medical conditions to calculate a risk score (range 0–14 in our sample). This score has been demonstrated to predict risk of 2-year mortality and hospitalization (Fan et al., 2002), where higher scores predict greater risk of these outcomes. We measured height and weight, using similar methods to those described in the Moving to Opportunities evaluation (Ludwig et al., 2011), which we used to calculate body mass index (BMI). We also captured participants' perceptions of their neighborhood that included daytime and nighttime crime (“The crime rate in my neighborhood makes it unsafe to go on walks DURING THE DAY” and “The crime rate in my neighborhood makes it unsafe to go on walks AT NIGHT,” respectively) using questions from the Neighborhood Environment Walkability Scale (NEWS-A) (Cerin et al., 2006). We also modified questions from this scale to capture the ease of transport to healthy food stores (“It is easy for me to travel in a car or by public transportation to stores that carry healthy foods”) and recreation facilities (“It is easy for me to travel in a car or by public transportation to parks, exercise facilities, or other recreation facilities”). We dichotomized responses to these perceived neighborhood questions as ‘agree’ if strongly agree/somewhat agree versus ‘disagree’ if somewhat disagree/strongly disagree.
2.3. Analyses
We included all head of households that answered whether they had access to a vehicle in our analytic sample (n = 265). We performed descriptive analyses of all variables. To evaluate if clustering by neighborhood occurred, we calculated an interclass correlation coefficient (ρ). Given that there was no substantial clustering (ρ < 0.10), we did not use multilevel models; however, we did elect to adjust all multivariable models for neighborhood to account for potential unmeasured neighborhood effects. We first conducted bivariate analyses examining the associations between vehicle access and our dependent variables. We used two different multivariable regression models for analyses – Poisson regression with robust error variance to estimate relative risk ratios (Zou, 2004) and logistic regression to calculate adjusted predicted probabilities. All regression models were adjusted for age, gender, and neighborhood – “basic models.” We also conducted analyses that used “full models,” which controlled for the following additional covariates. In models examining the diet outcomes, we also adjusted for comorbidity risk score and perceived easy transport to healthy food stores. In models examining the food insecurity outcome, we also adjusted for comorbidity risk score. In models examining the physical activity outcome, we also adjusted for comorbidity risk score and perceived easy transport to recreation. We selected these covariates based upon their statistical significance in bivariate associations and their theoretic potential as confounders. We used STATA 15.0 (College Station, Texas) to conduct all analyses.
3. Results
We included 265 participants that had a mean age of 44.5 years (SD 12.4) and were predominately women (86.0%) and black (95.5%). Mean BMI was 32.7 kg/m2 (SD 10.1). While we do not have access to demographic information of non-responding, eligible households, our sample characteristics are similar to another study of public housing residents in Baltimore City (Ludwig et al., 2011). Overall, the median daily intake of fruits & vegetables was 5.5 servings (IQR 3.0–6.7), median daily added sugar intake was 20.3 tsp (IQR 11.8–39.9), 67.2% were food insecure, and 20.2% were physically active. Interestingly, there was no significant association between food insecurity and either high fruit & vegetable or high added sugar intakes in bivariate analyses (p = 0.32 and p = 0.55, respectively).
Overall, 42.3% had access to a personal vehicle. Table 1 shows the differences in characteristics by vehicle access status. Residents with vehicle access were significantly younger and had lower comorbidity risk scores. They were also significantly more likely to endorse easy transport to healthy food stores and recreation facilities. In bivariate analyses, there was a statistically significant relationship between vehicle access and food insecurity; however, vehicle access had no significant associations with the diet or physical activity variables.
Table 1.
Characteristics of study sample of Baltimore public housing residents by personal vehicle access status.
| Vehicle access (n = 112) | No vehicle access (n = 152) | p-Value⁎ | |
|---|---|---|---|
| Demographics | |||
| Mean age in years (SD) | 42.0 (11.7) | 46.2 (12.7) | 0.01 |
| % women | 88.4 | 84.3 | 0.34 |
| % Black | 97.3 | 94.1 | 0.22 |
| % graduated high school | 69.6 | 64.1 | 0.34 |
| % unemployed | 38.4 | 30.1 | 0.16 |
| Mean comorbidity risk scorea (SD) | 3.8 (2.5) | 4.6 (2.9) | 0.01 |
| Mean body mass index in kg/m2 (SD) | 32.4 (10.2) | 32.8 (10.1) | 0.75 |
| Perceived neighborhood attributes | |||
| % daytime crime affects ability to go out | 63.4 | 61.4 | 0.75 |
| % nighttime crime affects ability to go out | 79.5 | 79.1 | 0.94 |
| % easy transport to healthy food stores | 92.0 | 82.4 | 0.02 |
| % easy transport to recreation facilities | 91.1 | 79.7 | 0.01 |
| Dependent variablesb | |||
| % high fruit & vegetable intake (≥6.7 servings/day) | 28.6 | 23.5 | 0.35 |
| % high added sugar intake (≥39.9 tsp/day) | 26.8 | 24.2 | 0.63 |
| % food insecure | 57.1 | 74.5 | <0.01 |
| % physically active | 24.1 | 17.0 | 0.15 |
p-Values calculated using t-tests and Chi2 tests, as appropriate. Bold text in the table highlights statistically significant results.
Score calculated based on the methods of the Seattle Index of Comorbidity (Fan et al., 2002).
Dietary variables estimated using the National Health Interview Survey (NHIS) 5-factor dietary screener (National Cancer Institute, n.d.), food insecurity assessed with 2-item screener focused on economic food insecurity (Hager et al., 2010), and physical activity assessed using the Lipid Research Clinics questionnaire (Ainsworth et al., 1993) where being ‘physically active’ defined as levels of high or moderate leisure time activity.
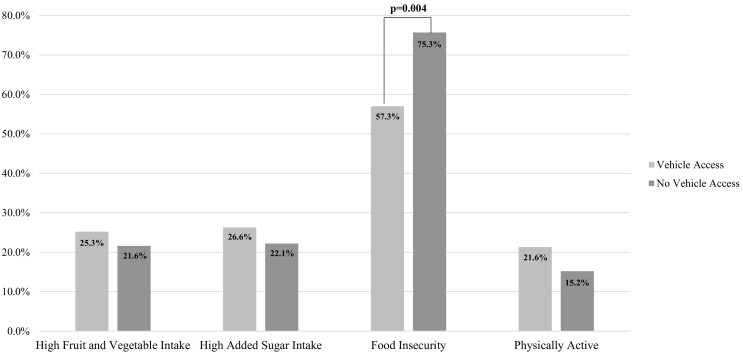
In multivariable models, residents who had access to a vehicle had a significantly lower risk of food insecurity compared with those who did not have vehicle in both basic and full models (Table 2). The adjusted predicted probability of food insecurity was 57.3% for those with vehicle access and 75.3% without vehicle access (Fig. 1) (OR 0.44, 95%CI 0.25–0.76, p < 0.01). Results were similar for the basic model (OR 0.41, 95%CI 0.24–0.71, p < 0.01). There were no significant associations between vehicle access and high fruit & vegetable, high added sugar intake, or physical activity in any of the multivariable models (Table 2, Fig. 1).
Table 2.
Results of basic and full multivariable Poisson regression with robust error variance to estimate relative risk of outcomes by vehicle access status among Baltimore public housing residents.
| RR | 95%CI | p-Value | |
|---|---|---|---|
| Basic modelsa | |||
| High fruit & vegetable intake (≥6.7 servings/day) | 1.17 | 0.78, 1.78 | 0.45 |
| High added sugar intake (≥39.9 tsp/day) | 1.13 | 0.75, 1.69 | 0.57 |
| Food insecure | 0.75 | 0.62. 0.90 | <0.01 |
| Physically active | 1.42 | 0.89, 2.28 | 0.14 |
| Full modelsb | |||
| High fruit & vegetable intake (≥6.7 servings/day) | 1.12 | 0.73, 1.72 | 0.60 |
| High added sugar intake (≥39.9 tsp/day) | 1.18 | 0.78, 1.79 | 0.43 |
| Food insecure | 0.76 | 0.63, 0.92 | <0.01 |
| Physically active | 1.44 | 0.88, 2.33 | 0.14 |
Dietary variables estimated using the National Health Interview Survey (NHIS) 5-factor dietary screener (National Cancer Institute, n.d.), food insecurity assessed with 2-item screener focused on economic food insecurity (Hager et al., 2010), and physical activity assessed using the Lipid Research Clinics questionnaire (Ainsworth et al., 1993) where being ‘physically active’ defined as levels of high or moderate leisure time activity. Bold text in the table indicates statistically significant results.
Basic models are adjusted for age, gender, and neighborhood.
Full models adjusted for all variables in the basic model as well as comorbidity risk score derived from the Seattle Index of Comorbidity (Fan et al., 2002). Models reporting dietary outcomes were also adjusted for perceived easy transport to healthy food stores. Models reporting the physical activity outcome were also adjusted for perceived easy transport to recreation.
Fig. 1.
Adjusted predicted probabilities of diet, food insecurity, and physical activity outcomes among Baltimore public housing residents with and without access to a personal vehicle (full model). Predicted probabilities calculated from results of full logistic regression models, which were adjusted for age, gender, comorbidity risk score, and neighborhood. In models examining the diet outcomes, we also adjusted for food insecurity status and perceived easy transport to healthy food stores. In models examining the physical activity outcome, we also adjusted for perceived easy transport to recreation. Dietary outcomes were estimated from the National Health Interview Survey (NHIS) 5-factor dietary screener (National Cancer Institute, n.d.), where high fruit & vegetable intake was ≥6.7 servings/day and high added sugar intake was ≥39.9 tsp/day, which represent the upper quartile of intakes reported in our sample. For food insecurity, we used the results of a validated 2-item screener (Hager et al., 2010). For physical activity, we used a validated exercise screener (Ainsworth et al., 1993) to determine whether a participant's leisure time activity level dichotomized as ‘active’ if high or moderate and ‘not active’ if low or very low levels. There was a statistically significant difference found in the predicted probabilities of food insecurity (p < 0.01), but no statistically significant difference in the predicted probabilities of high fruit & vegetable intake (p = 0.50), high added sugar intake (p = 0.43), or physical activity (p = 0.19).
4. Discussion
This study is the first examining how access to a personal vehicle affects those living in public housing developments. While less than half of residents had access to a personal vehicle, this access may play a role in conferring benefits to these residents, as food insecurity was less common among this group as compared to those that did not have vehicle access. While all public housing residents are low-income, having access to a personal vehicle may be capturing individuals who have relatively higher socioeconomic status than their neighbors. It is unclear what aspect of socioeconomic status this construct might be measuring, as there was no significant difference in educational attainment or unemployment status between the two groups. We did not collect income data, so we are unable to determine whether vehicle access reflects differences in income. In addition, individuals with vehicle access were significantly younger than participants without vehicle access, and they also had lower comorbid risk scores. Future research on socioeconomic factors in low-income populations should consider correlating access to a personal vehicle along with a full range of other socioeconomic domains (e.g., income, education, employment status, other resources) as well as demographics to better understand who typical vehicle users are in this population.
Food insecurity has been estimated to affect nearly one-third of households whose annual income is below 185% of the poverty threshold (Min et al., 2017); however, approximately two-thirds of households in our sample reported experiencing food insecurity in the past 12 months. The difference in rates may be explained by our use of a food insecurity screener focused on identifying economic conditions that prompted food scarcity. The measure did not evaluate all dimensions of food insecurity, nor is it as robust as more comprehensive assessments of food insecurity. Nonetheless, our result highlights the need for interventions to address this aspect of deprivation in these communities; however, not all households in public housing would necessarily benefit from such services. While all individuals who qualify for public housing must meet certain criteria to be defined as low income, variability exists regarding household financial status (Tucker-Seeley et al., 2013). In addition, income status and material deprivation, such as food insecurity, do not necessarily correlate (Tucker-Seeley et al., 2013), therefore, it is critical to identify characteristics other than income that identify deprivation. Having other ways to identify deprivation may be useful to researchers or local program managers, as residents may be reluctant to provide income information (Couper et al., 2008). Given its association with food insecurity, a question about personal vehicle access could be used to quickly screen and identify individuals at greater risk of deprivation within a low-income group. Such a screening tool may be helpful for lifestyle interventions to better address the needs of the population. For example, a group with vehicle access and less food insecurity may be at a better state to work on improving dietary quality, whereas an intervention to increase food security would be more appropriate for a group struggling to just have food in the house. Future studies are needed to confirm our findings and test the association between vehicle access with income and other aspects of financial hardship and deprivation. If confirmed, screening for personal vehicle access may help lifestyle interventions triage and tailor to the needs of low-income populations. Our results may also suggest that targeting transportation might be an intervention mechanism to reduce food insecurity. However, specifically addressing vehicle access as an intervention to reduce food insecurity has challenges. Social programs, such as the Supplemental Nutrition Assistance Program (SNAP) or the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC), can help people address the economic contributors to food insecurity. The lack of access to personal vehicle has no such equivalent social solutions, and providing access to a vehicle may be economically infeasible for government programs. Therefore, if transportation access is a barrier to food security, then future studies might consider testing whether modifying public transportation (e.g., alter bus routes, provide bus passes) reduces food insecurity.
Individuals with access to a vehicle were more likely to endorse ease in reaching healthy food stores and recreation facilities as compared to those that did not. However, contrary to our hypotheses, we found no statistically significant association between personal vehicle access and diet or physical activity. Our study does not account for how costs might influence the diet and exercise behaviors of these low-income residents, which may explain, in part, the lack of an association between healthy diet and exercise with vehicle access. Less healthful foods have been shown to be less expensive (Drewnowski and Specter, 2004) and higher calorie foods have been perceived as better value for the money in low-income populations (Ledikwe et al., 2005), which may make less healthy foods a more attractive option for public housing residents. Similarly, gyms and recreational facilities may charge for memberships (Statista Survey, n.d.), which may not be economically feasible for a low-income population.
Our study has a number of limitations. Our study population consisted of majority African-American women, and therefore not necessarily applicable to other groups. The response rate to our survey was low (47.8%) and we do not have information about non-responding households, which would provide clarification regarding any selection bias or other study biases in our sample. We do note that the characteristics of our sample are similar to other studies of public housing residents in Baltimore and Maryland (Ludwig et al., 2011; Pollack et al., 2014). We used brief screeners to determine diet, food insecurity, and physical activity variables, which are less detailed than other methods. For example, our 2-item food insecurity screener (Hager et al., 2010) does not capture all of the dimensions of this construct, which could include hunger or quality of food. Our study should be replicated using more comprehensive measures of these domains. In addition, we did not collect information on residents' incomes, so we are unable to examine whether vehicle access was associated with differences in income.
In conclusion, we found a significant association between personal vehicle access and lower risk of food insecurity; however, there were no associations with diet or exercise. Future studies should explore whether vehicle access can be used to identify low-income households at greater risk of deprivation, and whether improving access to efficient transportation, such as a personal vehicle, can be part of reducing food insecurity.
Disclosure
The authors declare no conflicts of interest to report.
Acknowledgements
Research reported in this publication was supported by the National Heart, Lung, And Blood Institute of the National Institutes of Health under Award Number K23HL116601. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The study was also supported by small grants from the Johns Hopkins Osler Center for Clinical Excellence and the Johns Hopkins Urban Health Institute. We would like to thank Jennifer Peyton for her role as study coordinator on this project.
References
- Ainsworth B., Jacobs D., Leon A. Validity and reliability of self-reported physical activity status: the Lipid Research Clinics questionnaire. Med. Sci. Sports Exerc. 1993;25:92–98. doi: 10.1249/00005768-199301000-00013. [DOI] [PubMed] [Google Scholar]
- Beaulac J., Kristjansson E., Cummins S. A systematic review of food deserts, 1966–2007. Prev. Chronic Dis. 2009;6:1. [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention About chronic diseases. https://www.cdc.gov/chronicdisease/about/index.htm Accessed on February 23, 2016 at.
- Cerin E., Saelens B.E., Sallis J.F., Frank L.D. Neighborhood environment walkability scale: validity and development of a short form. Med. Sci. Sports Exerc. 2006;38:1682–1691. doi: 10.1249/01.mss.0000227639.83607.4d. [DOI] [PubMed] [Google Scholar]
- Coleman-Jensen A., Rabbitt M., Gregory C., Singh A. Household food security in the United States in 2015. https://www.ers.usda.gov/webdocs/publications/err215/err-215.pdf?v=42636 Accessed on April 25, 2017 at.
- Couper M.P., Singer E., Conrad F.G., Groves R.M. Risk of disclosure, perceptions of risk, and concerns about privacy and confidentiality as factors in survey participation. J. Off. Stat. 2008;24:255–275. [PMC free article] [PubMed] [Google Scholar]
- Drewnowski A., Specter S. Poverty and obesity: the role of energy density and energy costs. Am. J. Clin. Nutr. 2004;79:6–16. doi: 10.1093/ajcn/79.1.6. [DOI] [PubMed] [Google Scholar]
- Fan V.S., Au D., Heagerty P., Deyo R.A., McDonell M.B., Fihn S.D. Validation of case-mix measures derived from self-reports of diagnoses and health. J. Clin. Epidemiol. 2002;55:371–380. doi: 10.1016/s0895-4356(01)00493-0. [DOI] [PubMed] [Google Scholar]
- Gudzune K., Peyton J., Pollack C.E. Perceived diet and exercise behaviors among social network members with personal lifestyle habits of public housing residents. Health Educ. Behav. 2018;45(5):808–816. doi: 10.1177/1090198118757985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hager E., Quigg A., Black M., Coleman S., Heeren T., Rose-Jacobs R. Development and validity of a 2-item screen to identify families at risk for food insecurity. Pediatrics. 2010;126:e26–e32. doi: 10.1542/peds.2009-3146. [DOI] [PubMed] [Google Scholar]
- Ledikwe J., Ello-Martin J., Rolls B. Portion sizes and the obesity epidemic. J. Nutr. 2005;135:905–909. doi: 10.1093/jn/135.4.905. [DOI] [PubMed] [Google Scholar]
- Ludwig J., Sanbonmatsu L., Gennetian L., Adam E., Duncan G.J., Katz L.F. Neighborhoods, obesity and diabetes – a randomized social experiment. N. Engl. J. Med. 2011;365:1509–1519. doi: 10.1056/NEJMsa1103216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maryland Department of Transportation . Vol. 1. 2018. Maryland Transit Administration Annual Report 2018; p. 10. [Google Scholar]
- Min Y.I., Anugu P., Butler K.R., Hartley T.A., Mwasongwe S., Norweed A.F. Cardiovascular disease burden and socioeconomic correlates: findings from the Jackson Heart Study. J. Am. Heart Assoc. 2017;6 doi: 10.1161/JAHA.116.004416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morland K., Diez Roux A., Wing S. Supermarkets, other food stores, and obesity: the atherosclerosis risk in communities study. Am. J. Prev. Med. 2006;30:333–339. doi: 10.1016/j.amepre.2005.11.003. [DOI] [PubMed] [Google Scholar]
- National Cancer Institute Five-factor screener in the 2005 National Health Interview Survey cancer control supplement: overview. https://epi.grants.cancer.gov/nhis/5factor/ Accessed on March 20, 2017 at.
- Pollack C.E., Green H.D., Kennedy D.P. The impact of public housing on social networks: a natural experiment. Am. J. Public Health. 2014;104:1642–1649. doi: 10.2105/AJPH.2014.301949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross C.E. Walking, exercising, and smoking: does neighborhood matter? Soc. Sci. Med. 2000;51:265–274. doi: 10.1016/s0277-9536(99)00451-7. [DOI] [PubMed] [Google Scholar]
- Scammell M., Torres S., Wayman J., Greenwood N., Thomas G., Kozlowski L. Balancing act: approaches to healthy eating and physical activity among Boston public housing residents. J. Prev. Interv. Community. 2015;43:109–122. doi: 10.1080/10852352.2014.973271. [DOI] [PubMed] [Google Scholar]
- Smith W., Kelsey-Harris R. Tips for facilitating lifestyle changes in low-income communities. Am. Fam. Physician. 2018;98:10. [PubMed] [Google Scholar]
- Spencer M., Petteway R., Bacetti L., Barbot O. 1st ed. Baltimore City Health Department; Baltimore City: 2011. Healthy Baltimore 2015.http://health.baltimorecity.gov/sites/default/files/HealthyBaltimore2015_Final_Web.pdf [Google Scholar]
- Statista Survey How much do you pay for your monthly gym membership? https://www.statista.com/statistics/639067/monthly-price-of-gym-in-us Accessed on December 17, 2018 at.
- Tucker-Seeley R.D., Harley A., Stoddard A., Sorensen G. Financial hardship and self-rated health among low-income housing residents. Health Educ. Behav. 2013;40:442–448. doi: 10.1177/1090198112463021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Census Bureau American Community Survey: means of transportation to work by selected characteristics in 2016. https://factfinder.census.gov/faces/tableservices/jsf/pages/productview.xhtml?pid=ACS_16_1YR_S0802&prodType=table Accessed on April 27, 2018 at.
- U.S. Preventive Services Task Force Healthful diet and physical activity for cardiovascular disease prevention in adults with cardiovascular risk factors: behavioral counseling. https://www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/healthy-diet-and-physical-activity-counseling-adults-with-high-risk-of-cvd Accessed on April 21, 2018 at.
- United States Department of Agriculture Definitions of food security. https://www.ers.usda.gov/topics/food-nutrition-assistance/food-security-in-the-us/definitions-of-food-security/ Accessed on November 29, 2018 at.
- Zou G. A modified Poisson regression approach to prospective studies with binary data. Am. J. Epidemiol. 2004;159:702–706. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]