Abstract
Meningitis is defined as an inflammation of the protective covering of brain and spinal cord collectively called as meninges. Meningeal infection can be complicated by intraventricular empyema. There are 9 cases of intraventricular empyema described in the literature out of which only three are described to be caused by Neisseria meningitidis. We report the fourth rare case.
A 61-year-old female with past medical history of diabetes and hypertension presented with the chief complaint of fever with chills and headache of 1-day duration. CT head did not reveal any acute abnormalities. Lumbar puncture was obtained and empiric IV antimicrobial agents were started. CSF analysis showed gram negative diplococci with culture growing Neisseria meningitidis suggesting meningococcal meningitis. Due to persistent headache and lethargy after complicated meningitis was suspected and MRI of brain was obtained which reflected a diagnosis of intraventricular empyema.
Pyogenic ventriculitis also known as intraventricular empyema or ependymitis, is a defined as an inflammation of the ependymal lining of the cerebral ventricular system and is characterized by the presence of suppurative fluid in the ventricles. It is a health care associated complication and is often confused with meningitis due to the similar presentation. Therefore, persistent symptoms despite optimal antimicrobial therapy (therapeutic failure) should alarm the presence of pyogenic ventriculitis.
This is the fourth case of intraventricular empyema reported secondary to Neisseria meningitidis. Our case reiterates that clinicians should maintain an index of suspicion for complicated meningitis in patients not responding to standard antimicrobial therapy.
Keywords: Ventriculitis, Neisseria meningitidis, Intraventricular empyema
Introduction
Meningitis is defined as an inflammation of the protective covering of brain and spinal cord collectively called as meninges. Etiology can be bacterial, viral or fungal. Pathogenesis of meningitis involves microbial adherence and colonization of the nasopharynx, mucosal invasion followed by blood stream infection and subsequent seeding in the subarachnoid space. Meningeal infection can be complicated by intraventricular empyema or pyogenic ventriculitis. It is a rare, debilitating and a severe intracranial infection characterized by inflammation of ventricular ependymal lining. It carries a diagnostic challenge as it has nonspecific overlap of symptoms with meningitis. If not managed early, it can lead to hydrocephalus and death. MRI is the most sensitive tool used in the diagnosis of pyogenic ventriculitis. There are a total of 9 cases of intraventricular empyema described in the literature out of which only three are described to be caused by Neisseria meningitidis. We report the fourth case which elaborates this extremely rare condition of intraventricular empyema caused by Neisseria meningitidis and resonates the significance of looking into subtle findings for early management which in turn improves patient mortality.
Case report
A 61-year-old female with past medical history of diabetes and hypertension presented with the chief complaint of fever with chills and headache of 1 day duration. Headache was severe and prominently in the frontal region, associated with nausea but no vomiting. There was no photophobia or phonophobia. Blood pressure on admission was 129/60 mm Hg, heart rate of 122/minute, respiratory rate of 16/minute, saturation 98% on room air and temperature of 103.1 F. The patient was lethargic during the interview but his orientation was not clouded. Comprehensive physical examination revealed diffuse macular rash across the arms, legs and chest. No focal neurological deficit was identified. Laboratory values revealed a white blood cell count of 20.1 × 103/μL, hemoglobin 14.1 g/dL, hematocrit 41.8% and platelet count of 168 × 103 /μL. Basic metabolic panel was within the normal limits. CT head did not reveal any acute intracranial pathologic process. Lumbar puncture was obtained and patient was empirically started on IV vancomycin and IV ceftriaxone. Dexamethasone was administered prior to the initiation of antimicrobials.
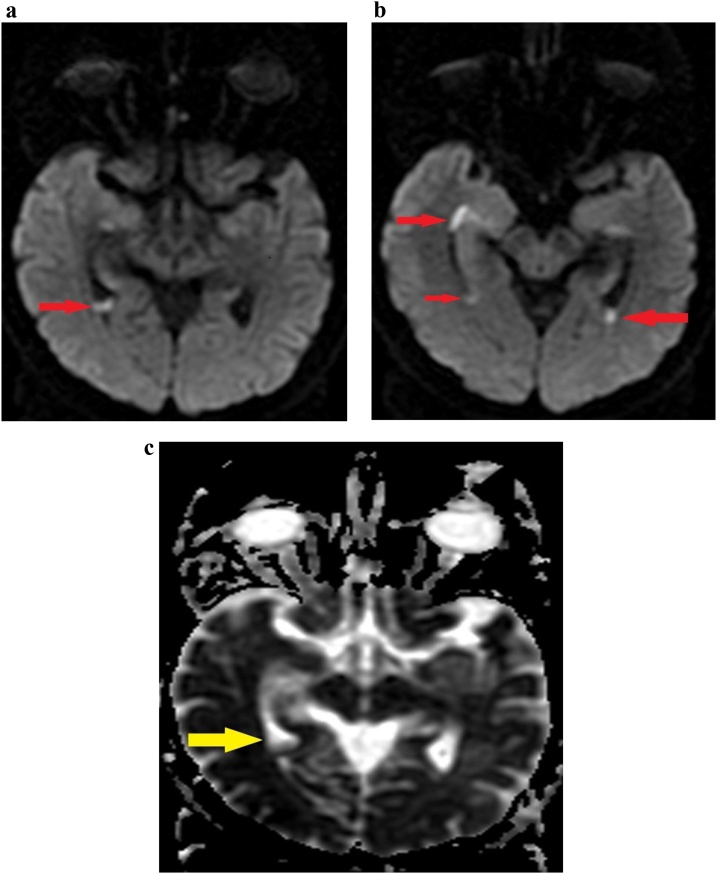
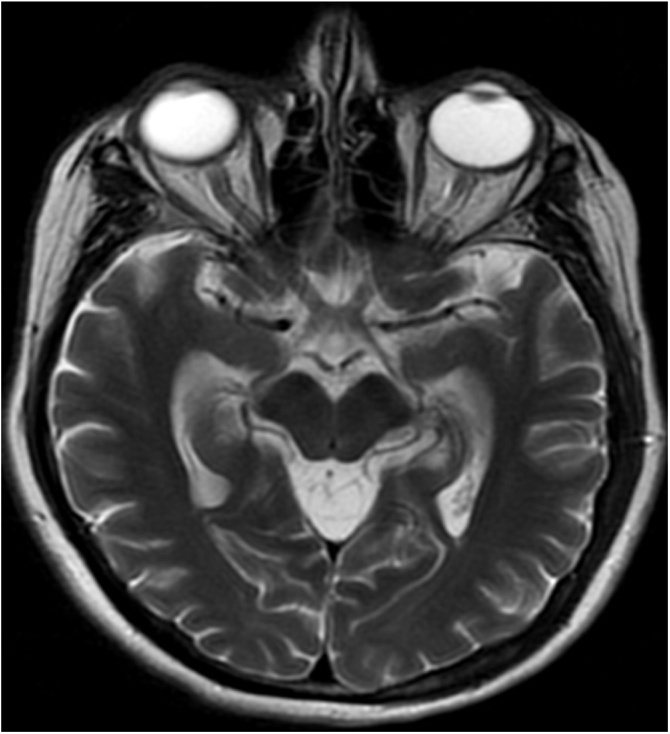
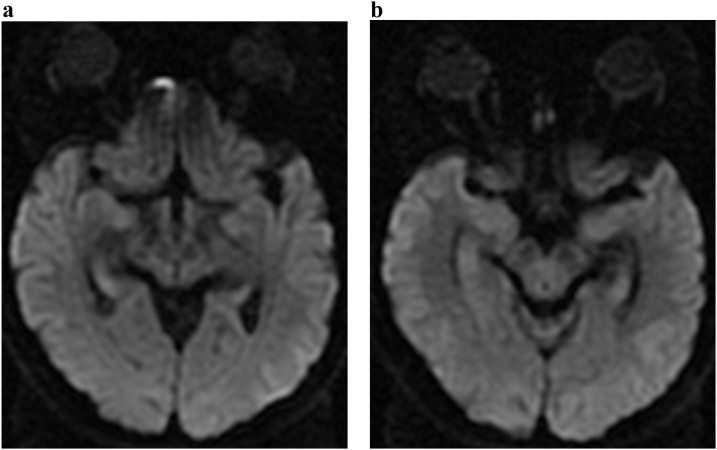
A bedside lumbar puncture was obtained which revealed a white blood cell count 475/μL (neutrophils: 87%), RBC count 270/μL, glucose 92 mg/dL and protein 149 mg/dL. Gram stain revealed gram negative diplococci raising the concern of meningococcal meningitis. CSF culture grew Neisseria meningitidis. Antimicrobial therapy was narrowed to IV ceftriaxone after culture results were available. With the continuation of IV ceftriaxone, patient became afebrile. However, the patient continued to have persistent headache and lethargy. Suspecting complicated meningitis after MRI of brain (Fig. 1a–c) was obtained which revealed foci of bright signal involving both nondependent portions of both lateral ventricles as well as dependent portions of both lateral ventricles reflecting a diagnosis of intraventricular empyema. No signal abnormalities were visualized on T2 weighted axial brain imaging (Fig. 2). At this juncture, neurosurgical consultation was obtained for possible drainage of empyema, however, continuation of medical management was recommended. IV ceftriaxone was continued for a total of 6 weeks (1 week inpatient and 5 weeks outpatient). MRI brain (Fig. 3a and b) was repeated at four weeks post discharge that revealed complete resolution of intraventricular empyema. Patient remained symptom free at 3 months follow up and continues to follow up in our Neurology clinic.
Fig. 1.
MRI Brain Diffusion weighted images (Fig. 1a and b) demonstrating foci of bright signal (red arrows) involving non-dependent as well as the dependent portions of both lateral ventricles which shows dark signal (yellow arrow) on ADC (apparent diffusion coefficient) mapping (Fig. 1c) reflecting ventriculitis.
Fig. 2.
Corresponding T2 weighted axial brain image showing no signal abnormalities.
Fig. 3.
(a) and (b): MRI Brain (Diffusion weighted images) showing post therapy non-visualization of foci of bright signal in non- dependent as well as dependent portions of both lateral ventricles suggesting good response to therapy.
Discussion
Pyogenic ventriculitis, also known as intraventricular empyema or ependymitis, is defined as an inflammation of the ependymal lining of the cerebral ventricular system and is characterized by the presence of suppurative fluid in the ventricles. It is mostly a health care associated infection and is a recognized complication of bacterial meningitis, ruptured brain abscesses, neurosurgical procedures or intraventricular drains or trauma. The process commonly affects neonates but can also be rarely seen in adults. Clinical presentation can vary from indolent course to fever, headache, focal neurological deficits, neck stiffness or seizure and is often confused with meningitis due to the similar presentation. Positive CSF culture and CSF pleocytosis are other features which are shared among both meningitis and intraventricular suppuration. Therefore, persistent symptoms despite optimal antibiotic therapy (therapeutic failure) should alarm the presence of pyogenic ventriculitis.
The pathogenesis behind this life-threatening condition is described as the entry of the causative organism into choroid plexus which creates an inflammatory response [1]. This prevents the CSF absorption acting as a blockage to the normal flow resulting in ventriculomegaly. Most common organisms involved in the pathogenesis are Streptococcus pneumoniae, Neisseria meningitidis and Staphylococcus aureus. Other organisms like E. faecalis, E.coli and Peptostreptococcus species have also been identified. The infection has also been described as a rare complication of infective endocarditis [2]. The first case of Neisseria meningitidis induced pyogenic ventriculitis was reported in 2016 by Nakahara et al. [3], second case was reported by Gronthoud et al. [4] in 2017 and the third case was described by Lesourd et al. [5] in 2018. These cases are summarized in Table 1. To our knowledge, our case is the fourth reported case of Neisseria meningitidis induced intraventricular empyema.
Table 1.
Summary of case reports of intraventricular empyema caused by Neisseria meningitidis.
| Authors | Age | Gender | Presentation | Causative agent | Antibiotic regimen | Outcome | Outcome |
|---|---|---|---|---|---|---|---|
| Gronthoud et al. [4] | 55 | Male | Fever, occipital headache and right ankle swelling |
N.meningitidis Serogroup B |
Piperacillin-Tazobactamfollowed by ceftriaxone and rifampin | Full recovery with no neurological sequelae | survived |
| Lesourd et al. [5] | 85 | Male | Fever |
N.meningitidis Serogroup B |
Cefotaxime and dexamethasone (for 4 days) followed by oral levofloxacin | Full recovery with no neurological sequelae | survived |
| Nakahara et al. [3] | 64 | Male | Fever and altered mental status | N.meningitidis | Ceftriaxone followed by moxifloxacin | Full recovery with no neurological sequelae | survived |
| Our case | 61 | Female | Fever, headache and chills |
N.meningitidis Serogroup B |
Ceftriaxone | Full recovery with no neurological sequelae | survived |
Diagnosis is confirmed by brain imaging. MRI is more reliable than CT scan in identification of pus in the cerebral ventricular system and ependymal inflammation as CT scan lacks the sensitivity. MRI can differentiate between blood and pus unlike CT scan. Diffusion weighted MRI imaging, being the best imaging technique, shows irregular ventricular debris which is also the most characteristic finding as per the study done by Fukui et al. [6]. It was detected in 16 out of 17 cases (94%) of healthcare associated ventriculitis. Other imaging findings like periventricular enhancement was noted in 7 out of 9 cases (78%), ependymal enhancement was detected in 7 out of 11 cases (64%) and pial enhancement was present in 13 out of 17 cases (76%).
Due to the rarity of this described case, no well defined antimicrobial regimen or protocol has been established yet. The case by Nakahara et al. [3] was managed with 17 days of ceftriaxone followed by 12 weeks of oral moxifloxacin. The other case by Gronthoud et al. [4] was treated with ceftriaxone for 6 weeks and 1 week of rifampin and treatment regimen of 2 weeks of cefotaxime followed by 2 weeks of oral levofloxacin was initiated in the case by Lesourd et al. [5]. All of these cases showed full recovery without any neurological sequelae. Our case was managed by IV ceftriaxone for 6 weeks.
Conclusion
This is the fourth case of intraventricular empyema reported secondary to Neisseria meningitidis. Our case reiterates that clinicians should maintain an index of suspicion for complicated meningitis in patients not responding to standard antibiotic therapy.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of interest statement
No conflicts of interest among authors.
References
- 1.Agrawal A., Cincu R., Timothy J. Current concepts and approach to ventriculitis. Infect Dis Clin Pract. 2008;16(2):100–104. [Google Scholar]
- 2.Jung G.W., Parkins M.D., Church D. Pyogenic ventriculitis complicating Aggregatibacter aphrophilus infective endocarditis: a case report and literature review. Can J Infect Dis Med Microbiol. 2009;20(3) doi: 10.1155/2009/971735. e107-e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nakahara H., Oda T., Fukao E., Horiuchi I., Honma Y., Uchigata M. A case of meningococcal meningitis that was difficult to treat owing to concurrent ventriculitis. Rinsho Shinkeigaku. 2016;56(5):344–347. doi: 10.5692/clinicalneurol.cn-000831. [DOI] [PubMed] [Google Scholar]
- 4.Gronthoud F., Hassan I., Newton P. Primary pyogenic ventriculitis caused by Neisseria meningitidis: case report and review of the literature. JMM Case Rep. 2017;4(1) doi: 10.1099/jmmcr.0.005078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lesourd A., Magne N., Soares A., Lemaitre C., Taha M.K., Gueit I. Primary bacterial ventriculitis in adults, an emergent diagnosis challenge: report of a meningoccal case and review of the literature. BMC Infect Dis. 2018;18(1):226. doi: 10.1186/s12879-018-3119-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fukui M.B., Williams R.L., Mudigonda S. CT and MR imaging features of pyogenic ventriculitis. AJNR Am J Neuroradiol. 2001;22(8):1510–1516. [PMC free article] [PubMed] [Google Scholar]