Abstract
Research has shown that tobacco users have an increased risk of collisions compared to nonsmokers. Studies from 1967 through 2013 documented a crude relative risk of collision involvement of about 1.5 among smokers compared to nonsmokers. In January 2009, in response to concerns about the health risks associated with potentially high concentrations of secondhand smoke resulting from smoking in vehicles, the provincial government in Ontario, Canada, introduced legislation restricting smoking in vehicles where children and adolescents are present. We examined the association between reported smoking and involvement in a motor vehicle collision in a large representative sample of adult drivers in Ontario, Canada, from 2002 and 2016, with particular focus on 2002–2008 and 2010–2016, periods before and after the legislation. Data are based on the Centre for Addiction and Mental Health (CAMH) Monitor. Among licensed drivers, prevalence of self-reported collision involvement within the past year for 2002–2008 was 9.39% among those who currently smoked compared to 7.08% of nonsmokers. Following implementation of the legislation, for 2010–2016, the prevalence of collisions for smokers was 7.01% and for nonsmokers was 6.02%. The overall difference for both smokers and nonsmokers between the two time periods was statistically significant; however, the difference between the two groups for the pre-legislation period was significant even after adjusting for potential confounders, while post legislation the difference was not significant. Prior to the legislation, the prevalence of collision was higher among smokers than nonsmokers; following the introduction of the legislation the prevalence was similar for the two groups.
Keywords: Tobacco use, Motor vehicle collision
1. Introduction
Most research on drugs and driving has focused on the use of alcohol and cannabis (Asbridge et al., 2012; Mann et al., 2010; Sayer et al., 2014). However, tobacco smoking in motor vehicles has been shown to be a risk factor for motor vehicle collisions (Begg and Gulliver, 2008; DiFranza et al., 1986; Eby and Kostyniuk, 2004; Lansdown et al., 2015; Lestikow et al., 1998; Lestikow and Petronis, 2009; McGuire, 1972; Prat et al., 2014; Sacks and Nelson, 1994; Sullman et al., 2015: Wen et al., 2005; Young et al., 2003). Lestikow et al. (1998), in an early meta-analysis of ten U. S., Swedish, Norwegian and British studies, reported elevated collision-related death rates among smokers, with a crude relative risk (RR) of 1.61 compared to never smokers. This finding was supported by Wen et al. (2005), who reported that, in Taiwan, the RR among smokers from motor vehicle collisions was 1.88 compared to nonsmokers. A subsequent review on distracted driving by Eby and Kostyniuk (2004) found that cigarette smoking was a contributing factor in between 1 and 5% of distraction-related crashes. They also noted that cigarette smoking was related to faster reaction times in some simulated studies and slower times in others. Whether the basis of this higher prevalence of collisions among tobacco smokers occurs as a result of smoking being a distraction to the driver, or because of the neurological and/or physiological effects of the toxicants in tobacco, or a combination, is not clear (e.g., Brison, 1990; Young et al., 2003).
In Canada over the past half century, various countermeasures have been introduced to reduce smoking because of its health-related harm to both smokers and nonsmokers. Legislation has included restrictions on sales, prohibitions on where smoking is allowed, and campaigns to promote cessation. The prevalence of smoking in Canada has declined from almost 50% among individuals aged 15 years and over in the 1960s to below 15% in 2015 (Reid et al., 2017). Vingilis et al. (2018) found that prevalence of self-reported collision involvement within the past year for 2002–2014 was 8.6% among those who currently smoke compared to 6.5% of nonsmokers. Logistic regression analysis, controlling for the potential confounding effects of sociodemographic, drinking and driving exposure measures, showed that the odds ratio of past-year collision involvement among current smokers was 1.35 times (p = .001) that of nonsmokers.
The purpose of the current paper was to examine the prevalence of motor vehicle collisions among smokers and nonsmokers in Ontario, using data from the Centre for Addiction and Mental Health (CAMH) Monitor survey of the Ontario adult population (aged 18 years and over) from 2002 to 2016. Because of the well-documented evidence that exposure to secondhand smoke has adverse health effects for infants, children and youth (US Department of Health and Human Services, 2006, 2014; American Academy of Pediatrics, 2005; California EPA, 2016; Kirst et al., 2013), the Ontario legislature enacted legislation to protect children and youth under the age of 16 years in vehicles from exposure to secondhand smoke, effective January 21, 2009 (Non Smokers Rights Association, 2017). This legislation designates such behavior by a driver or passenger as an offense with a fine of up to $250 (Highland Shores, 2016). The legislation specifies that individuals “must not light or use a tobacco product in motor vehicles with anyone inside who is under the age of 16 years. The law applies to both moving and parked vehicles -- even if a window, sunroof rooftop, door or other feature of the vehicle is open.” (Smoke Free Ontario, 2016). The introduction of this new legislation provided the opportunity to explore whether there were any changes in the frequency of and the relationship between prevalence of collisions and smoking prior to and following the legislation.
The findings can be used to provide information on this natural experiment and to stimulate additional research on this topic. For example, if other jurisdictions are thinking about similar legislation, the results of out analyses might provider some useful information to support legilsation, in addition to the documented findings of the detrimental health effects resulting from exposure to secondhand smoke.
2. Methods
Data are derived from the CAMH Monitor survey, a continuously-fielded (since 1996) cross-sectional telephone survey of the general adult population (ages 18 years or older) of Ontario, conducted by CAMH and administered by the Institute for Social Research (ISR) at York University (www.camh.ca/camh-monitor).
The main purpose of the survey is to provide epidemiological surveillance of indicators related to alcohol, tobacco, and other drug use, as well as physical and mental health. The survey uses list-assisted random-digit-dialing methods via Computer Assisted Telephone Interviews. The sampling frame is comprised of commercially available lists of telephone numbers as well as telephone numbers between or on either side of listed numbers. In essence, each randomly selected number from a telephone directory serves as a seed for additional random selections that are not restricted to published landline numbers. For example, if the selected number xxx-xxx-8513 is published in a directory then all numbers from xxx-xxx-8510 through xxx-xxx-8519 are included in the sampling frame even if they are cell phone numbers or unlisted numbers. A computer is then used to generate a random sample of telephone numbers from this frame from which each monthly or quarterly sample is drawn. Because unlisted numbers, cell phone numbers and newly activated numbers are potentially interspersed among published numbers in the sampling frame, this strategy provides a superior sample than one restricted to published landline (or equivalently, line phone, fixed line) numbers alone.
For 2002–2010, each annual cycle included monthly samples of between 170 and 215 completions, while for 2011 through 2016, each annual cycle consisted of four independent quarterly samples with approximately 750 completions each. The design employs a two-stage probability selection procedure. Within each regional stratum, a random sample of telephone numbers is selected with equal probability in the first stage of selection (i.e., households). Within households of selected telephone numbers, one respondent aged 18 years or older who could complete the interview in English is usually selected according to the last birthday method. For each calendar year, the monthly or quarterly samples were combined to provide a single annual dataset. Across years, response rates ranged from 58% to 41%, (Ialomiteanu et al., 2017) which is consistent with other surveys of this nature (Fan and Yan, 2010; Wright, 2015). The CAMH Monitor unit response rates are still comparable to more recent Canadian alcohol and drug use Random Digit Dialing (RDD) telephone surveys, including the 2011 and 2012 Canadian Alcohol and Drug Use Monitor Survey (CADUMS) (Health Canada, 2013), which obtained an overall response rate of 44% and 40%, respectively. In the U.S., the Behavioral Risk Factor Surveillance Survey (BRFSS), the largest health risk RDD telephone survey in the U. S., coordinated by the Centers for Disease Control and Prevention, obtained a median survey response rate for all states and territories of 47.2% in 2015 (Centers for Disease Control and Prevention, 2016). The data were weighted to adjust for varying selection probabilities, regional representation and a final post-stratification adjustment to restore the age by gender distribution based on the most recently available census figures. The weighted sample is considered representative of the non-institutionalized Ontario adult population (48% males, mean age 47.7 years (SD = 17.1), 84% urban).
The institutional research ethics committees at CAMH and York University have approved the survey annually. For the purpose of our study, the 13 annual cycles of the survey (2002–2016) were merged, resulting in a data set with N = 21,903 respondents. In order to examine the time periods before and after the implementation of the legislation, two time periods were used: 2002–2008 (N = 10,288) and 2010–2016 (N = 10,099). The data from 2009 was not included because the legislation was implemented in that year and it was not clear how widely the information about the legislation was publicized.
2.1. Definitions
Current cigarette smoking was measured by responses to three items: (tc1) “At the present time, do you smoke cigarettes daily, occasionally or not at all?”; (tc2) “Have you smoked 100 cigarettes in your life?”; and (tc5) “How long ago was it that you last smoked?” Current smoking is defined as someone who: 1) is a daily or occasional smoker, 2) has smoked over 100 cigarettes in lifetime, and 3) has smoked within the past 30 days. Driving exposure was measured by how much respondents report they drive in a typical week (number of kilometers divided by 100 to improve linearity; it is a continuous variable with range 0.01–83.00). Only drivers who reported that they had a valid driver's license and who drove in the past 12 months were included. The collision involvement item asks: “During the past 12 months, how often, if at all, were you involved in an accident or collision involving any kind of damage or injury to you or another person or vehicle while you were driving?” Responses were recoded to a dichotomous outcome (no = 0, yes = 1) (Ialomiteanu et al., 2017). Sociodemographic variables included: gender (female = 0, male = 1), age (as a categorical (18–34, 35–54, 55+ measure), household income (<$30,000, $30,000–49,999, $50,000–79,999, $80,000+, not stated), education (<high school, completed high school, some post-secondary, university degree) and marital status (never married, married/common law partner, previously married). Drinking frequency was measured by the weekly volume of alcohol consumed in standard drinks in the past 12 months (range 0.0–436.5). Hazardous drinking (no = 0–7, yes = 8+) are scores from the Alcohol Use Disorders Identification Test (AUDIT). The AUDIT is a 10-item, 5-point, validated screening instrument developed by the WHO to detect individuals at the less severe end of the spectrum of alcohol problems, with a score greater than seven indicating hazardous alcohol use (Saunders et al., 1993). The AUDIT has been extensively used in both national and Ontario surveys, demonstrating both the validity of the instrument in the Canadian population and the utility of the 8+ cut-off (Ialomiteanu et al., 2016; Kirst et al., 2013; Mann et al., 2010).
3. Analysis
The data used in the analyses were provided by CAMH. The only exception to the use of only valid responses is in the treatment of the income variable, as previous analyses of this dataset have generally shown that respondents who decline to report their income can be systematically different than those who respond to the question (e.g., Mann et al., 2010). These individuals have been combined into one group under “income not stated”. The percentages reported are based on the weighted sample sizes (using weights as provided by CAMH) and are considered representative for the population surveyed.
Most statistical analyses were done as contingency table chi-square tests of the hypothesis that the prevalences are equal, or, equivalently, that the odd ratio is 1. The sociodemographic information was included to describe the samples. The final analysis was the fitting of a logistic regression model for collisions, initially with only smoking, then with the sociodemographic variables, age, gender, education, household income and marital status, and finally, with sociodemographic variables, as well as other possible confounders (driving exposure, drinking frequency and hazardous drinking). The sociodemographic and other possible confounding variables were included in the model in order to test the independent effect of smoking on collisions. The test statistics were Wald chi-squares. SAS software, Version 9.4, for Windows (SAS Institute Inc., 2017) was used for all analyses.
4. Results
Overall, including 2009, 18.2% of the respondents reported being current smokers; there were significant differences by year (Х2(14) = 82.88, p < .001). A total of 22.0% of 18–24 year olds, 20.4% of 35–44 year olds, and 12.3% of 55+ year olds currently smoked (Х2(2) = 241.79, p < .001). Males (20.6%) were more likely to be current smokers than were females (15.4%) (Х2(1) = 998.77, p < .001). There were significantly more current smokers in the period before the enacted law (20.3% in 2002–2008) as compared to the post-2009 (15.9% in 2010–2016) period (Х2(1) = 66.64, p < .001).
Table 1 presents self-reported tobacco and collision involvement for the pre-2009 and post-2009 period, respectively. Both smokers and nonsmokers were involved in fewer collisions in 2010–2016 than in 2000–2008. More smokers than nonsmokers were involved in collision in 2000–2008, while in 2010–2016 the prevalence of collisions among smokers and nonsmokers was equivalent.
Table 1.
Comparisons of prevalences of collisions before and after 2009.
| 2002–2008 | 2010–2016 | Difference | Х2(1) | p-Value | |
|---|---|---|---|---|---|
| Smokers | 9.39% (n = 2103.70) |
7.01% (n = 1608.34) |
2.38% 95% CI (0.62%,4.15%) |
6.77 | 0.009 |
| Nonsmokers | 7.08% (n = 8251.79) |
6.02% (n = 8496.77) |
1.06% 95% CI (0.31%,1.81%) |
7.85 | 0.006 |
| Difference | 2.31% 95%CI (0.95%,3.68%) |
0.99% 95% CI (−0.36%,2.33%) |
|||
| Х2(1) | 12.85 | 2.27 | |||
| p-Value | <0.001 | 0.132 |
For the time period 2000–2008, the odds ratio of collisions for smokers compared to non-smokers decreased from 1.361, 95% CI (1.149, 1.612) to 1.241, 95% CI (1.036, 1.487) when adjusted for sociodemographic variables. It dropped further to 1.209, 95% CI (1.004, 1.455) when adjusted for sociodemographic variables as well as the possible confounders, driving exposure, drinking frequency and hazardous drinking. However, for the time period 2010–2016, the odds ratio only decreased from 1.176, 95% CI (0.952, 1.453) to 1.170, 95% CI (0.932, 1.469), and then to 1.155, 95% CI (0.914, 1.458).
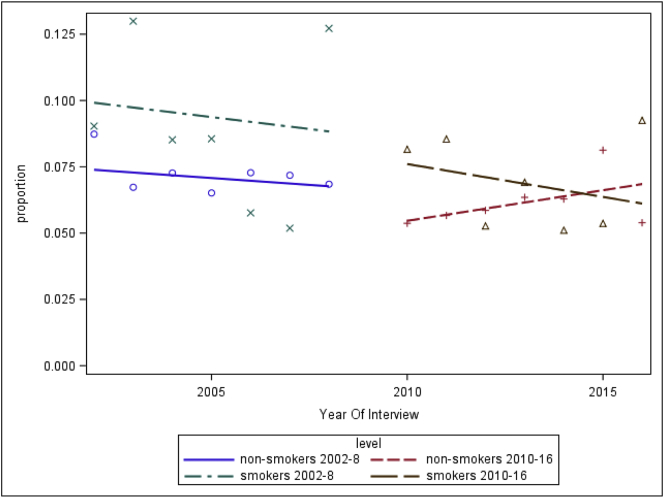
Finally, the proportion of smokers and nonsmokers who reported being in a collision is presented by year from 2002 through 2016 excluding 2009 (Fig. 1). The lines in the Figure are regression lines of percentage over the years of each time period. Although none of the slopes are statistically significant, they show the trend over time, and emphasize the differences in prevalence between smokers and nonsmokers over the two time intervals 2000–2008 and 2010–2016.
Fig. 1.
Trend lines for proportion of smokers and nonsmokers involved in collisions over time periods 2002–2008 and 2010–2016.
5. Discussion/conclusions
Overall, current smokers showed a 33% higher prevalence of collision involvement in the period from 2002 to 2016, compared to nonsmokers. This finding adds to the evidence that smoking is still a road safety risk, despite reductions in prevalence of tobacco use. These findings are consistent with the suggestion that road safety campaigns might benefit from addressing these risks in addition to those posed by drugs like alcohol and cannabis. However, the data do not provide insight into how tobacco use is related to what appears to be higher prevalence of collisions than that among nonsmokers. Research on the possible causal pathways between tobacco use and collision involvement is needed. Two explanations include the possibility that smoking increases distractions to the driver or that there are neurological and/or physiological effects of the toxicants in tobacco that interfere with driving. Recent papers have focused on smoking and driver distraction (Sullman et al., 2015; Young et al., 2003); clearly more research is needed on the topic. Legislation prohibiting smoking while driving may reduce distractions and decrease the potential effects of toxicants.
The findings are an exploration of the percentage of smokers and nonsmokers who reported being involved in at least one collision in the past 12 months before and after introduction of Ontario's Secondhand Smoke legislation. It is of interest to note that the relationships did not change markedly when potential confounders were included in the model. Clearly the results cannot be readily interpreted as they reflect data from an omnibus survey that provides no information on whether the post-legislation reduction in collision rates of smokers were due to smokers no longer smoking in their vehicles, and hence, being at lower risk of collision involvement or to other factors. However, these exploratory findings are intriguing and do warrant more research to determine whether the findings are reliable and if they are, what could be causing these pre-post reductions in collision rates among smokers.
There are some limitations that should be taken into account in considering these findings. All of the information was based on self-report; therefore, there was no validation of smoking status or of involvement in collisions. Given the social unacceptability of smoking and involvement in collisions, it is possible that underreporting may have occurred and, as a result, may have attenuated the relationships. The smokers were not specifically asked about whether they smoked in their vehicles, whether they smoked when children and adolescents were with them in their vehicles and whether they were smoking at the time of a collision. Information about the use of other tobacco products was not included. Moreover, they were not asked about whether they knew about the new regulations. One additional consideration is the fact that current smoking was measured within the past 30 days while occurrence of a collision was within the past 12 months. As a result, it is possible that an individual could have been a current smoker at the time of the survey, but a nonsmoker at the time of the collision. Additionally, although the response rate in recent years is still considered to be good for a telephone survey, and data were weighted to reflect a representative sample of Ontario residents, the sample could potentially be biased.
In-depth qualitative interviews could help to clarify the issues raised above. As well, roadside observational studies similar to those that have been reported by Lansdown et al. (2015) and Sullman et al. (2015) may help to provide information about the extent of smoking while driving, as well as document the presence of children and adolescents in vehicles. Given the nature of the data, the findings do not provide direct support for such legislation. However, the findings may be useful in providing support for similar legislation that can result in protectioning individuals from the detrimental exposure to secondhand smoke and possibly reducing the occurrence of collisions among smokers.
Conflicts of interest
There are no conflicts of interest to report for any of the authors.
Acknowledgments
There are no conflicts of interest to report for any of the authors. No funding was received for the secondary data analysis included in this manuscript.
References
- American Academy of Pediatrics, Task Force on Sudden Infant Death Syndrome The changing concept of sudden infant death syndrome: diagnostic coding shifts; controversies regarding the sleeping environment; and new variables to consider in reducing risk. Pediatrics. 2005;116(5):1245–1255. doi: 10.1542/peds.2005-1499. [DOI] [PubMed] [Google Scholar]
- Asbridge M., Hayden J.A., Cartwright J.L. Acute cannabis consumption and motor vehicle collision risk: systematic review of observational studies and meta-analysis. BMJ. 2012;344:e536. doi: 10.1136/bmj.e536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Begg D.J., Gulliver P. A longitudinal examination of the relationship between adolescent problem behaviors and traffic crash involvement during young adulthood. Traffic Inj. Prev. 2008;9(6):508–514. doi: 10.1080/15389580802335117. [DOI] [PubMed] [Google Scholar]
- Brison R.J. Risk of automobile accidents in cigarette smokers. Can. J. Public Health. 1990;81(2):102–106. [PubMed] [Google Scholar]
- California EPA Air Resources Board. Secondhand smoke in cars fact sheet. 2016. https://www.arb.ca.gov/toxics/ets/documents/ets_cars.pdf
- Centers for Disease Control and Prevention 2016. https://www.cdc.gov/tobacco/data_statistics/fact_sheets/secondhand_smoke/health_effects/index.htm#children
- DiFranza J.R., Winters T.H., Goldberg R.J., Cirillo L., Biliouris T. The relationship of smoking to motor vehicle accidents and traffic violations. N. Y. State J. Med. 1986:464–467. [PubMed] [Google Scholar]
- Eby D.W., Kostyniuk L.P. NASA; Suite 1M32, Washington, DC, 20546-0001, USA: 2004. Driver Distraction and Crashes: an Assessment of Crash Databases and Review of the Literature. (mailto:public-inquiries@hq.nasa.gov, http://www.nasa.gov.12) [Google Scholar]
- Fan W., Yan Z. Factors affecting response rates of the web survey: a systematic review. Comput. Hum. Behav. 2010;26(2):132–139. [Google Scholar]
- Health Canada Canadian Alcohol and Drug Use Monitoring Survey (CADUMS) 2013. https://www.canada.ca/en/health-canada/services/health-concerns/drug-prevention-treatment/canadian-alcohol-drug-use-monitoring-survey.html
- Highland Shores 2016. https://highlandshorescas.com/parenting-help/legislation
- Ialomiteanu A.R., Hamilton H., Adlaf E.M., Mann R.E. Centre for Addiction & Mental Health; Toronto, ON: 2016. CAMH Monitor eReport: Substance Use, Mental Health and Well-being Among Ontario Adults, 1977–2015 (CAMH Research Document Series No. 45)www.camh.ca/camh-monitor [Google Scholar]
- Ialomiteanu A., Adlaf E.M., Mann R.E. Centre for Addiction and Mental Health; Toronto, ON: 2017. CAMH Monitor 2016: Metadata User's eGuide.www.camh.ca/camh-monitor [Google Scholar]
- Kirst M., Mecredy G., Chaiton M. The prevalence of tobacco use co-morbidities in Canada. Can. J. Public Health. 2013;04:e210–e215. doi: 10.17269/cjph.104.3770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lansdown T.C., Stephens A.N., Walker G.H. Multiple driver distractions: a systemic transport problem. Accid. Anal. Prev. 2015;71:360–367. doi: 10.1016/j.aap.2014.07.006. [DOI] [PubMed] [Google Scholar]
- Lestikow B.N., Petronis K. 137 APHA Annual Meeting. 2009. Smoking, crashing and burning: accidental death risks by smoking status in the United States.https://www.researchgate.net/publication/266817956_Smoking_crashing_and_burning_Unintentional_injury_death_risks_by_smoking_status_in_the_US [Google Scholar]
- Lestikow B.N., Martin D.C., Jacobs J., Rocke D.M. Smoking as a risk factor for injury death: a meta-analysis of cohort studies. Prev. Med. 1998;27:871–878. doi: 10.1006/pmed.1998.0374. (Accessed 8/17/18) [DOI] [PubMed] [Google Scholar]
- Mann R.E., Stoduto G., Vingilis E. Alcohol and driving factors in collision risk. Accid. Anal. Prev. 2010;42:1538–1544. doi: 10.1016/j.aap.2010.03.010. [DOI] [PubMed] [Google Scholar]
- McGuire F.L. Smoking driver education and other correlates of accidents among young males. J. Saf. Res. 1972;4:5–11. [Google Scholar]
- Non Smokers Rights Association NSRA's Smoke Free Laws Database. 2017. http://database.nonsmokersrights.ca
- Prat F., Planes M., Gras M.E., Sullman M.J.M. An observational study of driving distractions on urban roads in Spain. Accid. Anal. Prev. 2014;74:8–16. doi: 10.1016/j.aap.2014.10.003. [DOI] [PubMed] [Google Scholar]
- Reid J.L., Hammond D., Rynard V.L., Madill Cl, Burkhalter R. Propel Centre for Population Health Impact, University of Waterloo; Waterloo, Ontario: 2017. Tobacco use in Canada, Patterns and Trends 2017 Edition.https://uwaterloo.ca/tobacco-use-canada/ [Google Scholar]
- Sacks J.J., Nelson D.E. Smoking and injuries: an overview. Prev. Med. 1994;23(4):515–520. doi: 10.1006/pmed.1994.1070. [DOI] [PubMed] [Google Scholar]
- SAS Institute Inc. Seventh edition. SAS Institute Inc; Cary, NC: 2017. Base SAS® 9.4 Procedures Guide. [Google Scholar]
- Saunders J.B., Asland O.G., Babor T.F., De La Fuente J.R., Grant M. Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption--II. Addiction. 1993;88:791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- Sayer G., Ialomiteanu A., Stoduto G. Increased collision risk among drivers who report driving after using alcohol and after using cannabis. Can. J. Public Health. 2014;105(1):e92–e93. doi: 10.17269/cjph.105.4351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smoke Free Ontario 2016. https://www.ontario.ca/page/smoke-free-ontario#section-1
- Sullman M.J.M., Prat F., Tasci D.K. A roadside study of observable driver distractions. Traffic Inj. Prev. 2015;16(6):552–557. doi: 10.1080/15389588.2014.989319. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services . U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; Atlanta: 2006. USDHHS The Health Consequences of Involuntary Exposure to Tobacco Smoke: A Report of the Surgeon General. (Accessed 8/17/18) [Google Scholar]
- U.S. Department of Health and Human Services USDHHS . U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Disease Prevention and Health Promotion, Office on Smoking and Health; Atlanta: 2014. The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General. (Accessed 8/17/18) [Google Scholar]
- Vingilis E., Pederson L.L., Seeley J. Is there a link between motor vehicle collisions and cigarette smoking in Canada: analysis of survey data from Ontario from 2002–2014. Traffic Inj. Prev. 2018;19(4):364–370. doi: 10.1080/15389588.2017.1419342. [DOI] [PubMed] [Google Scholar]
- Wen C.P., Tsai S.P., Cheng T.Y., Chen W.S., Chung W.S.I. Chen. Excess injury mortality among smokers: a neglected tobacco hazard. Tob. Control. 2005;Suppl 1:128–132. doi: 10.1136/tc.2003.005629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright G. An empirical examination of the relationships between response rate and nonresponse bias. Stat. J. IAOS. 2015;31(2):305–315. [Google Scholar]
- Young K., Regan M., Hammer M. Monash University Accident Research Centre; 2003. Driver Distraction: a Review of the Literature. (Report no 206. (Accessed 8/17/18)) [Google Scholar]