Abstract
While it is recognized that acculturation influences adiposity risk, the direction and magnitude of this relationship remain unclear. Previous studies' use of proxy acculturation measures and exclusively cross-sectional study designs have limited understanding of this research question. The aim of this study was to examine associations between acculturation and adiposity among Puerto Ricans (45–75 years) living on the mainland United States. We analyzed data from the longitudinal (baseline, 2-year, 5-year) Boston Puerto Rican Health Study (n = 1114). Language-based and psychological-based acculturations were assessed at baseline using questionnaires. Acculturation scores were divided into tertile categories; higher tertiles indicate greater English- and U.S.-based acculturation. Adiposity was assessed using BMI and waist circumference at baseline and each follow-up. Linear mixed effects regression models were fit with baseline acculturation tertile as the predictor and baseline or change in adiposity as the outcome. When examining baseline associations with language acculturation tertiles, participants in the middle acculturation tertile (bilingual) had 2.48 cm (95%CI: −4.64, −0.31) lower waist circumference compared to the more Spanish-based acculturation tertile. When examining the associations between baseline language acculturation tertiles and change in adiposity, those in the more English-based acculturation tertile had higher annual gains in BMI (0.13 kg/m2 (95%CI: 0.01, 0.25)) and waist circumference (0.44 cm (95%CI: 0.01, 0.88)) over 5-years compared to those in the more Spanish-based acculturation tertile. No significant differences in adiposity were found across psychological-based acculturation tertiles. In conclusion, English language-based acculturation at baseline influences long-term adiposity. Psychological-based acculturation may capture distinct acculturation processes from the language-based construct.
Keywords: Acculturation, Obesity, Minority health, Puerto Ricans, Hispanics/Latinos
Highlights
-
•
We tested associations between baseline acculturation constructs and change in adiposity over time.
-
•
Higher English language acculturation was associated with greater adiposity over 5-years.
-
•
Neither U.S. nor Puerto Rican psychological acculturation was associated with adiposity over 5-years.
-
•
Language- and psychological-based acculturation may capture distinct processes.
1. Introduction
Hispanics/Latinos comprise the largest ethnic minority group in the United States (U.S.), with a rapidly growing population that is estimated to double by 2060 (Colby and Ortman, 2017). Compared to non-Hispanic whites, Hispanic/Latino adults experience a disproportionately high burden of poor health outcomes, with the prevalence of obesity nearly 10% higher among Hispanic/Latino adults (47%) compared to their non-Hispanic white counterparts (38%) (Hales et al., 2017). Interest in reducing obesity among Hispanics/Latinos is underscored by a robust body of literature linking excess adiposity to many negative health consequences including chronic disease, cardiovascular risk factors, and endocrine and metabolic conditions (Reilly et al., 2003).
Reasons for greater obesity among racial/ethnic minorities such as Hispanics/Latinos are complex (The State of Obesity, 2017). One factor posited to influence weight gain among racial/ethnic minorities is acculturation, defined as the ways in which individuals or groups engage with a new culture via shifts in behaviors, attitudes, values, and identities (Berry, 2003). Acculturation depends on societal factors (e.g., society of origin and society of settlement) and personal factors (e.g., life events and coping mechanisms) that exist prior to, and arise during, the course of acculturation (Berry, 1997). As part of the acculturation process, individuals must make decisions regarding heritage cultural maintenance and dominant culture participation. During its course, acculturation permeates many aspects of an individual's life (including dietary patterns, physical activity, socioeconomic status, employment, social support systems, and neighborhood environment) in various ways, and these lifestyle factors in turn affect obesity risk (Pérez-Escamilla, 2011). Thus, differences in obesity risk are to be expected across ranges of acculturation.
While several studies have suggested that greater acculturation to the dominant culture is associated with more overweight and obesity (Delavari et al., 2013; Abraído-Lanza et al., 2005; Bates et al., 2008; Garcia et al., 2012; Goel et al., 2004), other studies have found null results and a few have reported a protective effect of acculturation against obesity risk (Hazuda et al., 1991; Khan et al., 1997; Miller et al., 2004). For example, Isasi et al. found no relationship between U.S. acculturation (measured using the Short Acculturation Scale for Hispanics) and likelihood of obesity among a large cohort of Hispanic/Latino adults aged 18 to 74 years (Isasi et al., 2015). The majority of previous research has relied on convenient proxy measures of acculturation, such as place of birth, age at arrival, or length of residence (Pérez-Escamilla, 2011; Matsudaira, 2006), but these measures do not adequately capture the complex acculturation process, as they capture a limited domain and assume that an individual follows a linear trajectory of acculturation (Matsudaira, 2006). Moreover, few studies have compared the extent to which different measures of acculturation, such as language use or psychological orientation, may be associated with obesity (Khan et al., 1997; Gordon-Larsen et al., 2003). Knowing how these associations contrast may inform which aspects of the acculturation experience are potentially protective or detrimental for obesity risk. Finally, almost all studies examining acculturation and obesity have been exclusively cross-sectional, limiting the strength of causal inferences that can be made.
The present study aims to address existing gaps in the literature by examining the association between two acculturation scales (language- and psychological-based) at baseline and changes in adiposity over 5-year follow-up among a cohort of middle-aged and older Puerto Rican adults living in Boston, Massachusetts. There are several demographic, socioeconomic, and behavioral characteristics that may confound the relationship between acculturation and obesity risk. For example, lower socioeconomic status is associated with lower acculturation and higher obesity in developed countries (McLaren, 2007; Van Rompay et al., 2012), while smoking is generally associated with higher acculturation (among women) and lower obesity (Bethel and Schenker, 2005; Wack and Rodin, 1982). Hence, all analyses are adjusted for potential confounders. Given that Puerto Ricans are the second largest Hispanic/Latino heritage and experience disproportionately high levels of obesity (Isasi et al., 2015; Collazo et al., 2010), critically examining acculturation as a potential risk factor for adiposity is necessary within this population.
2. Methods
2.1. Study population
We analyzed data from the Boston Puerto Rican Health Study (BPRHS), a longitudinal cohort of Puerto Rican adults recruited in 2004–2009 (n = 1500) and followed-up at 2-years (n = 1258) and 5-years (n = 961). A complete description of the study protocol has been published previously (Tucker et al., 2010). Participants were recruited from the Greater Boston area using door-to-door enumeration in neighborhoods of high Hispanic-density, identified using the year 2000 census tracks, and through community approaches (e.g., recruitment at community festivals/fairs) (Tucker et al., 2010). Eligible participants were self-identified Puerto Ricans aged 45–75 years, who were able to answer questions in English or Spanish, had no serious health conditions or cognitive impairment, and were living in the Boston metro area (Tucker et al., 2010). Sociodemographics, health status, and lifestyle behaviors were collected through questionnaires at home-based interviews conducted by bilingual interviewers. Interviewers received thorough training on best practices to administer questionnaires and perform measurements, in line with procedures from the National Health and Nutrition Examination Survey II and the MacArthur Studies of Successful Aging (Chumlea et al., 1998; Seeman et al., 1994). Questionnaires and measurement procedures were consistent across each follow-up.
All participants provided written informed consent. The study was approved by the institutional review boards at Tufts Medical Center, Tufts University, and Northeastern University.
2.2. Measures
2.2.1. Acculturation
Acculturation was assessed at baseline by trained, bilingual interviewers using the Psychological Acculturation Scale (Tropp et al., 1999) and a modified version of the language-based Bidimensional Acculturation Scale for Hispanics (Marin and Gamba, 1996). The Psychological Acculturation Scale assessed orientation to Puerto Rican and mainland U.S. cultures by asking to which cultural group(s) individuals most identified for 10 questions related to attachment and belonging (e.g., culture for which individual shares most beliefs and values). Responses were recorded on a 5-point Likert scale, with 1 being “Only with Puerto Ricans,” 3 being “Same among Puerto Ricans and Americans” (i.e. bicultural), and 5 being “Only with Americans.” A summary psychological-acculturation score (ranging from 0 to 50) was calculated, with lower scores indicative of more Puerto Rican psychological-based acculturation and higher scores indicative of more U.S. psychological-based acculturation.
The modified version of the language-based Bidimensional Acculturation Scale for Hispanics measured acculturation by asking which language(s) individuals used for seven usual activities (watching T.V., reading newspapers/books, speaking with neighbors, at work, listening to the radio, with friends, and with family). Responses were recorded on a 5-point Likert scale, with 1 being “Only Spanish,” 3 being “Both equally” (i.e., bilingual), and 5 being “Only English”. A summary language-based acculturation score (ranging from 0 to 100) was calculated, with lower scores indicative of more Spanish-based acculturation and higher scores indicative of more English language-based acculturation.
Baseline psychological- and language-based acculturation scores were categorized into tertile categories (psychological-based acculturation = more Puerto Rican, 0–14.9; middle, 15–20.9; more U.S., 21–50; language-based acculturation = more Spanish-speaking, 0–8.3; middle, 8.3–34.9; more English-speaking, 35–100). Consistent with other studies (Zhang et al., 2015; Mattei et al., 2018), acculturation scores were classified into tertiles to capture the non-linear associations between acculturation status and obesity risk and to maintain sample size in each group. As a bicultural and bilingual orientation would be represented by each score's midpoint, we consider the middle tertile of psychological acculturation score to include bicultural individuals and the middle tertile of the language-acculturation score to include bilingual individuals in the context of this cohort.
Although acculturation was measured at each follow-up, only baseline acculturation measures were used in this analysis due to minimal change in acculturation experienced by participants in our study sample. For example, the mean psychological-based acculturation score only changed by 0.4 points over the 2-year follow-up and 1.5 points over the 5-year follow-up, while the language-based acculturation score only changed by 1.3 points over the 2-year follow-up and 2.5 points over the 5-year follow-up. Limited change is expected, given that this is a population of older adults who have already spent considerable time on the mainland U.S. (e.g., average of >30 years in mainland U.S. at baseline) and who we may be capturing at a later stage in their acculturation process.
2.2.2. BMI and waist circumference
Body mass index (BMI) and waist circumference were measured in the same way at baseline, 2-year, and 5-year follow-up. Using standard protocols (Tucker et al., 2010), standing height, weight, and waist circumference were measured in duplicate by trained technicians, using a SECA 214 Portable Stadiometer, a Toledo Weight Plate (Model I5S, Bay State and Systems Inc. Burlington, MA), and a measuring tape to the nearest 0.1 cm for waist circumference at the umbilicus, respectively. The average of the measures was used. BMI was calculated as weight (in kilograms) divided by the square of height (in meters).
2.2.3. Covariates
A sociodemographic questionnaire at baseline was used to collect information on age (continuous), sex (male, female), marital status (married, divorced/separated, widowed, never married), educational attainment (<8th grade, 9th–12th grade, some college or higher), household income (<$10,000, $10,000–$24,999, >$24,999), current employment (yes, no), food insufficiency (yes, no), health insurance (yes, no), smoking status (never, former, current), and age at migration (continuous).
Food insufficiency was assessed using a question adapted from the USDA Food Security/Hunger Scale (Bickel et al., 2000), wherein participants were asked to describe the food eaten in their household in the last 12-months, with responses “sometimes not enough to eat” and “often not enough to eat” classified as food insufficient and responses “enough of the kinds of foods we want to eat” and “enough but not always the kinds of food we want” classified as food sufficient. Smoking status was defined as “never” if the respondent smoked <100 cigarettes in their entire life, “former” if they reported smoking in the past but not currently, and “current” if they reported smoking currently.
2.3. Statistical analysis
From a total of 1500 individuals recruited at baseline, the study population for this analysis was limited to 1114 participants (74%) who had complete data on language- and psychological-based acculturation (exclusion n = 14), BMI and waist circumference (exclusion n = 16), and all covariates (exclusion n = 356) at baseline. We assessed differences in baseline characteristics across acculturation tertiles using analysis of variance (ANOVA) for continuous variables and chi-square analysis for categorical variables.
To examine cross-sectional associations at baseline, separate linear regression models were fit with baseline psychological- or language-based acculturation tertiles as the predictor and baseline BMI or waist circumference as the outcome. This created 4 cross-sectional models: 1) baseline psychological-based acculturation tertiles predicting baseline BMI, 2) baseline psychological-based acculturation tertiles predicting baseline waist circumference, 3) baseline language-based acculturation tertiles predicting baseline BMI, and 4) baseline language-based acculturation tertiles predicting baseline waist circumference. All models were adjusted for the following baseline variables: age, sex, marital status, education status, household income, current employment, food insufficiency, health insurance, age at migration, and smoking status.
To examine associations between baseline acculturation tertile and change in adiposity over follow-up, linear mixed effects regression models with robust standard error estimators were fit to examine baseline psychological- or language-based acculturation tertiles as the predictor and change in BMI or waist circumference over 5-year follow-up as the outcome. This created 4 models: 1) baseline psychological-based acculturation tertiles predicting change in BMI over 5-years, 2) baseline psychological-based acculturation tertiles predicting change in waist circumference over 5-years, 3) baseline language-based acculturation tertiles predicting change in BMI over 5-years and 4) baseline language-based acculturation tertiles predicting change in waist circumference over 5-years. These models adjusted for the same baseline demographic covariates as the cross-sectional models. To determine annual change in BMI or waist circumference for each acculturation tertile, the models additionally included time of interview (measured as a continuous variable in years) as a separate covariate and as part of an interaction term with acculturation tertile (acculturation × time). As a sensitivity analysis, we also fitted linear mixed effects regression models using average acculturation tertile over follow-up (i.e., tertile based on average of baseline, 2-year, and 5-year acculturation scores) as the predictor, instead of baseline only.
Analyses were conducted using SAS version 9.3 (SAS Institute, Inc., Cary, NC). Significance was set at p < 0.05.
3. Results
Participants in the more English-based language acculturation tertile were younger, more likely to be male, married or widowed, employed, and current smokers, as well as to have higher educational attainment, higher household income, and to have migrated to the mainland U.S. at an earlier age than those in the more Spanish-based language acculturation tertile (Table 1). Participants in the more U.S.-based psychological acculturation tertile were younger, had higher educational attainment, higher household income, were more likely to be employed, and to have migrated to the mainland U.S. at an earlier age, compared to those in the more Puerto Rican-based psychological acculturation tertile.
Table 1.
Baseline characteristics by language-based and psychological-based acculturation tertile among adults in the Boston Puerto Rican Health Study.
| Characteristic | Language-based acculturation scale |
Psychological-based acculturation scale |
||||||
|---|---|---|---|---|---|---|---|---|
| More Spanish (n = 331) |
Middle (bilingual) (n = 413) |
More English (n = 370) |
p | More Puerto Rican (n = 378) |
Middle (bicultural) (n = 343) |
More U.S. (n = 393) |
p | |
| Age, mean (SE) | 59.7 (0.40) | 57.4 (0.36) | 55.1 (0.38) | <0.0001 | 58.6 (0.38) | 57.3 (0.40) | 56.1 (0.37) | <0.0001 |
| Age at migration, mean (SE) | 28.3 (0.61) | 23.3 (0.54) | 18.0 (0.58) | <0.0001 | 26.1 (0.59) | 23.9 (0.62) | 19.2 (0.58) | <0.0001 |
| Female (%) | 72.5 | 69.5 | 58.4 | 0.0001 | 66.1 | 68.5 | 65.7 | 0.68 |
| Marital status (%) | 0.003 | 0.29 | ||||||
| Married | 27.0 | 36.1 | 36.0 | 32.5 | 32.9 | 34.4 | ||
| Single | 43.8 | 37.8 | 41.1 | 40.2 | 39.4 | 42.2 | ||
| Divorced | 15.7 | 11.9 | 7.0 | 13.2 | 13.4 | 7.9 | ||
| Widowed | 13.6 | 14.3 | 16.0 | 14.0 | 14.3 | 15.5 | ||
| Education status (%) | <0.0001 | <0.0001 | ||||||
| ≤8th grade | 69.2 | 44.6 | 21.4 | 57.1 | 41.4 | 34.1 | ||
| Some high school | 26.9 | 45.3 | 45.1 | 36.8 | 41.1 | 41.5 | ||
| ≥high school | 3.9 | 10.2 | 33.5 | 6.1 | 17.5 | 24.4 | ||
| Household income (%) | <0.0001 | <0.0001 | ||||||
| <$10,000 | 57.7 | 42.9 | 28.7 | 49.7 | 43.2 | 34.9 | ||
| $10,000–$24,999 | 35.4 | 41.7 | 37.8 | 38.1 | 36.2 | 41.0 | ||
| >$24,999 | 7.3 | 15.5 | 33.5 | 12.2 | 20.7 | 24.2 | ||
| Currently employed (%) | 6.7 | 14.8 | 39.5 | <0.0001 | 12.2 | 19.0 | 30.0 | <0.0001 |
| Food insufficiency (%) | 12.4 | 9.4 | 10.3 | 0.42 | 10.3 | 10.2 | 11.2 | 0.89 |
| Health insurance (%) | 96.4 | 95.2 | 92.7 | 0.08 | 95.2 | 94.8 | 94.2 | 0.79 |
| Smoking status (%) | 0.005 | 0.49 | ||||||
| Never | 49.9 | 47.0 | 37.8 | 48.4 | 44.0 | 42.0 | ||
| Former | 29.3 | 32.0 | 32.4 | 28.8 | 31.8 | 33.3 | ||
| Current | 20.9 | 21.1 | 29.7 | 22.8 | 24.2 | 24.7 | ||
Notes: Psychological-based acculturation was assessed by asking to which cultural group(s) individuals most identified for questions related to attachment and belonging. Language-based acculturation was assessed by asking which language(s) individuals used for usual daily activities. Baseline psychological- and language-based acculturation scores were categorized into tertiles (psychological-based acculturation = low, 0–14.9; middle, 15–20.9; high, 21–50; language-based acculturation = low, 0–8.3; middle, 8.3–34.9; high, 35–100).
Food insufficiency was assessed using a question adapted from the USDA Food Security/Hunger Scale, wherein participants were asked to describe the food eaten in their household in the last 12-months, with responses “sometimes not enough to eat” and “often not enough to eat” classified as food insufficient and responses “enough of the kinds of foods we want to eat” and “enough but not always the kinds of food we want” classified as food sufficient. Smoking status was defined as “never” if the respondent smoked <100 cigarettes in their entire life, “former” if they reported smoking in the past but not currently, and “current” if they reported currently smoking.
Compared to those in the more Spanish-based acculturation tertile at baseline, those in the middle language-based acculturation tertile (i.e., bilingual) had a 2.48 cm (95%CI: −4.64, −0.31) lower waist circumference at baseline (Table 2). No significant differences in BMI or waist circumference at baseline were found across baseline psychological-based acculturation tertiles.
Table 2.
Differences (95%CI) in baseline BMI and waist circumference across baseline psychological- or language-based acculturation tertiles.
| BMI (kg/m2) beta coefficient (95%CI) |
Waist circumference (cm) beta coefficient (95%CI) |
|
|---|---|---|
| Language-based acculturation | ||
| More Spanish | Ref. | Ref. |
| Middle (bilingual) | −0.80 (−1.74, 0.15) | −2.48 (−4.64, −0.31)⁎ |
| More English | −0.98 (−2.10, 0.14) | −1.84 (−4.42, 0.74) |
| Psychological-based acculturation | ||
| More Puerto Rican | Ref. | Ref. |
| Middle (bicultural) | 0.32 (−0.61, 1.24) | 0.64 (−1.49, 2.77) |
| More U.S. | −0.59 (−1.53, 0.34) | −1.55 (−3.71, 0.60) |
BMI = body mass index; CI = confidence interval.
Notes: Psychological-based acculturation was assessed by asking to which cultural group(s) individuals most identified for questions related to attachment and belonging. Language-based acculturation was assessed by asking which language(s) individuals used for usual daily activities. Baseline psychological- and language-based acculturation scores were categorized into tertiles (psychological-based acculturation = more Puerto Rican, 0–14.9; middle, 15–20.9; more U.S., 21–50; language-based acculturation = more Spanish-speaking, 0–8.3; middle, 8.3–34.9; more English-speaking, 35–100). Linear mixed effects regression models were fit to examine baseline psychological- or language-based acculturation tertiles as the predictor and baseline BMI or waist circumference as the outcome, and were adjusted for age, sex, marital status, education status, household income, current employment, food insufficiency, health insurance, age at migration, and smoking status.
p-Value < 0.05.
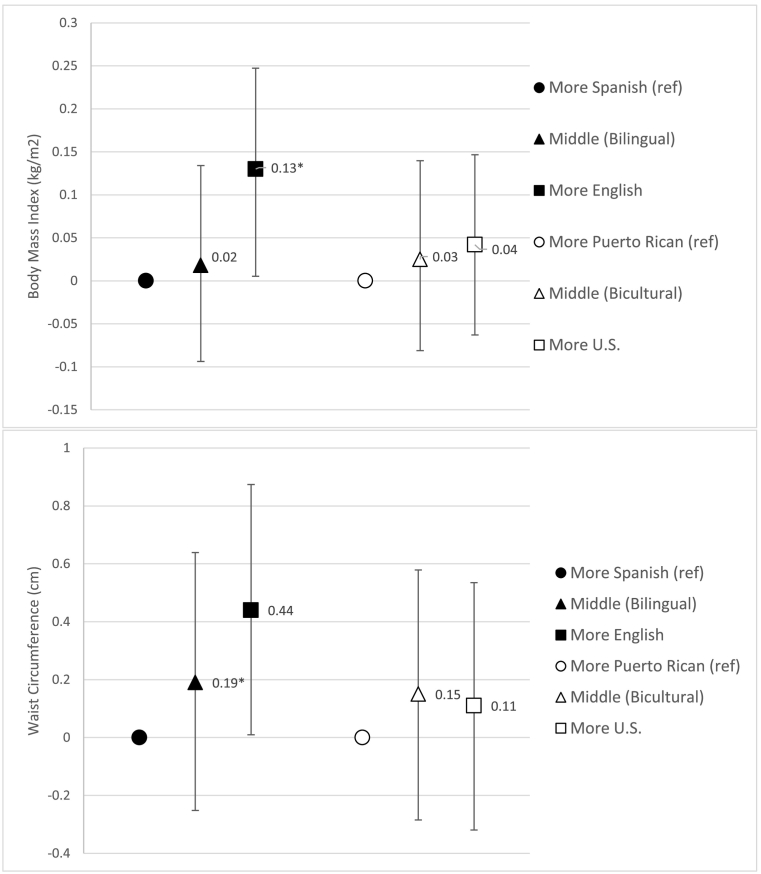
Compared to those in the more Spanish-based language acculturation tertile at baseline, those in the more English-based language acculturation tertile had a 0.13 kg/m2 (95%CI: 0.01, 0.25) higher annual change in BMI and a 0.44 cm (95%CI: 0.01, 0.88) higher annual change in waist circumference over 5-year follow-up (Fig. 1). No significant differences in annual BMI or waist circumference change over 5-years were found across baseline psychological-based acculturation tertiles.
Fig. 1.
Difference (95%CI) in annual BMI and waist circumference change over 5-year follow-up across baseline psychological- or language-based acculturation tertiles.
Figure legend: Psychological-based acculturation was assessed by asking to which cultural group(s) individuals most identified for questions related to attachment and belonging. Language-based acculturation was assessed by asking which language(s) individuals used for usual daily activities. Baseline psychological- and language-based acculturation scores were categorized into tertiles (psychological-based acculturation = more Puerto Rican, 0–14.9; middle, 15–20.9; more U.S., 21–50; language-based acculturation = more Spanish-speaking, 0–8.3; middle, 8.3–34.9; more English-speaking, 35–100). Linear mixed effects regression models with robust standard error estimators were fit to examine baseline psychological- or language-based acculturation tertiles as the predictor and change in BMI or waist circumference over 5-year follow-up as the outcome, and were adjusted for age, sex, marital status, education status, household income, current employment, food insufficiency, health insurance, age at migration, and smoking status.
Sensitivity analysis using average acculturation tertile over follow-up as the predictor produced similar point estimates as those obtained when modeling baseline tertile acculturation as predictor. Compared to those who were in the more Spanish-based acculturation tertile over follow-up, those in the more English-based acculturation tertile had a 0.51 cm (95%CI: 0.01, 1.02) higher annual change in waist circumference over 5-years. The association for English-based acculturation and BMI was marginally significant (beta-coefficient (95%CI): 0.13 kg/m2 (0.0, 0.26)). No significant differences in changes in outcomes were found for averaged psychological-based acculturation tertiles.
4. Discussion
Our study is one of the first evaluations of the association between baseline acculturation status and change in adiposity conducted among Puerto Rican adults living in the U.S. mainland. Our findings suggest that Puerto Ricans who have more English-based language acculturation at baseline experience greater increases in adiposity over 5-years compared to those with more Spanish-based language acculturation. We did not find any associations between psychological-based acculturation and adiposity, suggesting that language- and psychological-based measures capture distinct constructs of the acculturation process. Models using baseline adiposity versus change in adiposity as the outcome were inconsistent, underscoring the importance of utilizing prospective studies, which may provide stronger inferences on acculturation-adiposity dynamics.
Our finding of an association between language-based acculturation at baseline and change in adiposity contributes to a growing body of evidence suggesting that more English-based acculturation is associated with overweight and obesity risk among Hispanics/Latinos living in the U.S. (Abraído-Lanza et al., 2005; Bates et al., 2008; Garcia et al., 2012; Goel et al., 2004). There are several possible mechanisms by which language-based acculturation could contribute to increased adiposity. First, highly acculturated individuals often conform the most to a dominant culture's dietary patterns (Pérez-Escamilla, 2011; Satia-Abouta et al., 2002). In particular, researchers have found that Hispanics/Latinos with higher English language acculturation consume more fast foods and cook fewer homemade meals (akin to the typical U.S. diet) than their less-acculturated counterparts (Zhang et al., 2015; Langellier et al., 2015; Park et al., 2011). This intake of energy-dense and nutritionally-poor foods is hypothesized to generate metabolic disturbances which can in turn lead to fat accumulation (Laraia, 2013). Second, individuals with higher English language acculturation experience greater exposure to U.S. food advertising and marketing through engagement with English-language TV, radio, and social media (Larsen et al., 2003; Clayman et al., 2010). Additionally, research among adult women has demonstrated that Spanish-language food advertisements provide substantially more health and nutrition information than English-language advertisements, suggesting that as individuals acculturate they may lose contact with positive health messaging in Spanish that may be protective against obesity (Abbatangelo-Gray et al., 2008). However, a cross-sectional analysis in this same cohort of Puerto Rican adults found that higher English language-based acculturation was associated with mixed dietary behaviors (i.e. lower intake of legumes but higher intake of cereal fiber) (Van Rompay et al., 2012), suggesting that diet quality may not be the primary pathway mediating associations between language-based acculturation and adiposity. In addition to diet, acculturation may lead to adiposity through other pathways including increased stress, reduced physical activity, and substance abuse (Pérez-Escamilla, 2011). Research examining the role that non-dietary factors may play in mediating the relationship between language-based acculturation and adiposity is limited, presenting a high-need area for future research.
Associations between baseline acculturation and change in adiposity were not consistent across language and psychological measures of acculturation. While we found that more English-based acculturation at baseline was associated with higher increases in BMI and waist circumference over 5-years, no significant associations were found for psychological-based acculturation. These inconsistencies reflect the notion that the two measures are tapping into distinct constructs of the acculturation process (Matsudaira, 2006; Marino et al., 2000). The psychological acculturation scale assesses subjective internal changes represented by values, identity, beliefs, and cultural attachment, while the language-based scale assesses overt behavioral (i.e. language-related) dimensions of acculturation, which are arguably easier for an individual to alter than one's psychological positions (Matsudaira, 2006; Marino et al., 2000). Although we found a moderate correlation between the two constructs of acculturation (r = 0.53, p < 0.0001), their differing associations with adiposity suggest that the two measures are not interchangeable and indeed assess two distinct concepts. Future research is needed to understand why psychological acculturation does not appear to be associated with adiposity.
Models using baseline adiposity versus change in adiposity as the outcome were inconsistent. One reason for this inconsistency could be the presence of reverse causation, as it is plausible that pre-existing adiposity may affect one's acculturation status. For example, individuals with overweight or obesity may be less likely to identify with and acculturate towards U.S.-American culture given their perceptions of weight stigma and discrimination in the country (Puhl and Heuer, 2009). The potential for reverse causation suggests that previous cross-sectional studies should be interpreted with caution as they may not reflect the true directional effect that acculturation has on adiposity. Another possible explanation for the discrepancy in findings is that the relationship between acculturation and adiposity may not be constant over time. For example, being bilingual may be initially protective against weight gain, but as time goes on and individuals spend more time in the U.S., becoming more acculturated may turn detrimental (Himmelgreen et al., 2004). This is particularly relevant for our study population of older adults who have already spent considerable time in the U.S. and who we may be capturing at a later stage in their acculturation process. In general, longitudinal studies are more appropriate for establishing temporality and producing robust causal inferences for studies on acculturation and obesity. Hence, future studies should move away from the existing reliance on cross-sectional data and towards greater use of prospective study designs. Moreover, researchers should examine this research question among study populations that experience substantial change in acculturation over time, such that both the exposure (acculturation) and outcome (adiposity) can be analyzed in a longitudinal manner.
Our study found that the middle language-based acculturation tertile (i.e. bilingual) was associated with lower waist circumference at baseline, similar to a cross-sectional analysis in this same cohort that observed that higher English language-based acculturation was associated with lower central obesity (Van Rompay et al., 2012). However, we did not find evidence that either biculturalism or bilingualism was protective against increases in adiposity over time. Bilingualism is characterized by a simultaneous retention of one's heritage language and engagement with English. Being bilingual in the U.S. may lead to better employment, higher earnings, and greater access to healthcare (Becerra et al., 2015; DuBard and Gizlice, 2008), all of which may contribute to healthier lifestyles and lower adiposity. Similarly, bicultural individuals are hypothesized to have more successful adaptation because they possess a number of protective factors including engaging with two cultural communities (providing two social support systems), decreased experience of prejudice and discrimination (since one appears to “fit in” with dominant culture), and a flexible personality (required to maintain connection with both cultures) (Berry, 1997). Emerging evidence from other studies has suggested a lower risk of obesity for bilingual and bicultural individuals (Hazuda et al., 1991; Wang et al., 2011). A possible reason that our study did not detect a protective effect of bilingualism or biculturalism against gains in adiposity over time is that individuals in our study sample had a predominantly low distribution of acculturation. Hence, the individuals categorized in the middle tertiles of acculturation in our study may not possess the true characteristics of biculturalism or bilingualism needed to confer protective effects against adiposity over time seen in other studies.
Although the differences in BMI and waist circumference between language-based acculturation tertiles observed in our study were modest, these risks may compound over time to substantially increase obesity risk at the population level. This is of particular importance given the disproportionately high burden of obesity experienced by Hispanics/Latinos in the U.S. (Ogden and Carroll, 2010). At baseline, nearly 90% of study participants were classified as having either overweight or obesity using BMI and 70% were classified as having abdominal obesity using waist circumference. Moreover, further chronic disease risk may be gained by these small increases in adiposity; it has been estimated that each centimeter of waist circumference increases the risk of a cardiovascular event by 2% (De Koning et al., 2007), while each unit decrease in BMI may result in 26 and 28 fewer cases of chronic disease per 1000 men and women, respectively (Kearns et al., 2014). Hence, findings from this study should be used to tailor the delivery and content of health messages as part of obesity and chronic diseases prevention efforts among Hispanics/Latinos. For example, as individuals become more acculturated to mainland U.S. culture, interventions could emphasize maintaining heritage-specific cultural dietary practices that are healthy (e.g., beans and rice in healthy ratios, traditional fruits and vegetables, ethnic spices and herbs), while incorporating dominant culture dietary foods and practices that are healthy given their wider availability and simultaneously discouraging unhealthy ones (e.g., fast food, sugar-sweetened beverages). Additionally, interventions should be tailored to the distinct channels that Hispanic/Latinos with varying levels of linguistic acculturation to access health and obesity-related information (Livingston et al., 2008).
4.1. Study limitations and strengths
Our study has some limitations. First, the missing values for certain baseline covariates (e.g., income) reduced our sample size and therefore our statistical power. Additionally, if this missingness was related to both acculturation and BMI/waist circumference, then this may have introduced selection bias into our results. For example, if individuals with low acculturation were more likely to be missing data (and thus be excluded from our study sample) and these individuals were also more likely to have higher BMI/waist circumference, then our reported results are an underestimate of the true association between low acculturation and adiposity risk. Additionally, the loss to follow-up incurred over 5-year follow-up may also have introduced bias into our results, wherein participants who dropped out of the study may be different than those who remained in the study. For example, individuals with low levels of acculturation may have been more likely to leave Boston to return to Puerto Rico than their counterparts with high levels of acculturation. Next, the relatively small sample size in each acculturation tertile limited our ability to test effect modification by other variables of interest (e.g., circular migration, age at arrival). Additionally, the BPRHS also consists of a very specific population (middle-aged and older Puerto Rican adults living in Boston) and thus the results may not be generalizable to other Puerto Ricans or other Hispanics/Latinos living in the U.S. mainland. In particular, most participants had lived on the mainland U.S. for many years (mean duration = 34 years) and may be at a later stage of acculturation than individuals newly arrived in the U.S. mainland. However, studies of Puerto Ricans in other U.S. mainland cities have shown similar levels of adiposity and acculturation to our study population (Isasi et al., 2015), suggesting that results may still be generalizable. Finally, the high baseline prevalence of overweight and obesity limited the statistical power to test the association between acculturation and risk of overweight or obesity over follow-up.
Our study includes a number of strengths. The use of change in adiposity as an outcome measure enhances our ability to establish temporality and strengthens causal inferences. Additionally, we conducted a sensitivity analysis using average acculturation tertile over follow-up as the predictor variable, demonstrating that our results were robust to an alternate analytic approach. We also compared two measures of acculturation (language- and psychological-based) in order to ascertain their relative associations with BMI and waist circumference. Our models were adjusted for several important confounders assessed with validated tools; future studies should consider potential mediators in the acculturation and adiposity association, such as physical activity or diet.
5. Conclusions
Puerto Ricans are one of the largest ethnic minority groups in the U.S. and experience disproportionately high prevalence of obesity (Isasi et al., 2015; Collazo et al., 2010), highlighting the need to identify and address risk factors for obesity. Future studies using longitudinal measures of both acculturation and adiposity are needed to expand the findings of this study and examine the extent to which different variables (e.g., dietary quality, physical activity) mediate the relationship between acculturation and adiposity. Researchers should move away from a reliance on proxy measures of acculturation (e.g., length of stay in the U.S.) and future research should incorporate bidimensional measurements of acculturation into their analyses. Future research is also needed to examine whether the relationship between acculturation and adiposity is modified by other variables such as sex, age, and migration-related factors (e.g., circular migration, age at arrival).
Funding
This study was funded by the National Heart, Lung, and Blood Institute grant P50-HL105185; National Institute on Aging grants P01-AG023394 and R01-AG055948, and a Mentored Career Development Award to Promote Faculty Diversity in Biomedical Research (K01-HL120951) from the NIH/National Heart, Lung, and Blood Institute. Dr. McClain received support for this study from a NIH Ruth L. Kirschstein Institutional Training Grant Postdoctoral Fellowship (T32 DK 7703-23).
References
- Abbatangelo-Gray J., Byrd-Bredbenner C., Austin S.B. Health and nutrient content claims in food advertisements on Hispanic and mainstream prime-time television. J. Nutr. Educ. Behav. 2008;40(6):348–354. doi: 10.1016/j.jneb.2008.01.003. [DOI] [PubMed] [Google Scholar]
- Abraído-Lanza A.F., Chao M.T., Florez K.R. Do healthy behaviors decline with greater acculturation?: implications for the Latino mortality paradox. Soc. Sci. Med. 2005;61(6):1243–1255. doi: 10.1016/j.socscimed.2005.01.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bates L.M., Acevedo-Garcia D., Alegría M., Krieger N. Immigration and generational trends in body mass index and obesity in the United States: results of the National Latino and Asian American Survey, 2002–2003. Am. J. Public Health. 2008;98(1):70–77. doi: 10.2105/AJPH.2006.102814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becerra D., Androff D., Messing J.T., Castillo J., Cimino A. Linguistic acculturation and perceptions of quality, access, and discrimination in health care among Latinos in the United States. Soc. Work Health Care. 2015;54(2):134–157. doi: 10.1080/00981389.2014.982267. [DOI] [PubMed] [Google Scholar]
- Berry J.W. Immigration, acculturation, and adaptation. Appl. Psychol. 1997;46(1):5–34. [Google Scholar]
- Berry J.W. American Psychological Association; 2003. Conceptual Approaches to Acculturation. [Google Scholar]
- Bethel J.W., Schenker M.B. Acculturation and smoking patterns among Hispanics: a review. Am. J. Prev. Med. 2005;29(2):143–148. doi: 10.1016/j.amepre.2005.04.014. [DOI] [PubMed] [Google Scholar]
- Bickel G., Nord M., Price C., Hamilton W., Cook J. 2000. Guide to Measuring Household Food Security. Revised. [Google Scholar]
- Chumlea W.C., Guo S.S., Wholihan K., Cockram D., Kuczmarski R.J., Johnson C.L. Stature prediction equations for elderly non-Hispanic white, non-Hispanic black, and Mexican-American persons developed from NHANES III data. J. Am. Diet. Assoc. 1998;98(2):137–142. doi: 10.1016/S0002-8223(98)00036-4. [DOI] [PubMed] [Google Scholar]
- Clayman M.L., Manganello J.A., Viswanath K., Hesse B.W., Arora N.K. Providing health messages to Hispanics/Latinos: understanding the importance of language, trust in health information sources, and media use. J. Health Commun. 2010;15(sup3):252–263. doi: 10.1080/10810730.2010.522697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colby S.L., Ortman J.M. 2017. Projections of the Size and Composition of the US Population: 2014 to 2060: Population Estimates and Projections. [Google Scholar]
- Collazo S.G., Ryan C.L., Bauman K.J. 2010. Profile of the Puerto Rican Population in United States and Puerto Rico: 2008. Paper presented at: Annual Meeting of the Population Association of America. [Google Scholar]
- De Koning L., Merchant A.T., Pogue J., Anand S.S. Waist circumference and waist-to-hip ratio as predictors of cardiovascular events: meta-regression analysis of prospective studies. Eur. Heart J. 2007;28(7):850–856. doi: 10.1093/eurheartj/ehm026. [DOI] [PubMed] [Google Scholar]
- Delavari M., Sønderlund A.L., Swinburn B., Mellor D., Renzaho A. Acculturation and obesity among migrant populations in high income countries–a systematic review. BMC Public Health. 2013;13(1):458. doi: 10.1186/1471-2458-13-458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DuBard C.A., Gizlice Z. Language spoken and differences in health status, access to care, and receipt of preventive services among US Hispanics. Am. J. Public Health. 2008;98(11):2021–2028. doi: 10.2105/AJPH.2007.119008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia L., Gold E.B., Wang L., Yang X., Mao M., Schwartz A.V. The relation of acculturation to overweight, obesity, pre-diabetes and diabetes among US Mexican-American women and men. Ethn. Dis. 2012;22(1):58. [PMC free article] [PubMed] [Google Scholar]
- Goel M.S., McCarthy E.P., Phillips R.S., Wee C.C. Obesity among US immigrant subgroups by duration of residence. JAMA. 2004;292(23):2860–2867. doi: 10.1001/jama.292.23.2860. [DOI] [PubMed] [Google Scholar]
- Gordon-Larsen P., Harris K.M., Ward D.S., Popkin B.M. Acculturation and overweight-related behaviors among Hispanic immigrants to the US: the National Longitudinal Study of Adolescent Health. Soc. Sci. Med. 2003;57(11):2023–2034. doi: 10.1016/s0277-9536(03)00072-8. [DOI] [PubMed] [Google Scholar]
- Hales C., Carroll M., Fryar C., Ogden C. NCHS Data Brief. Number 288. National Center for Health Statistics; 2017. Prevalence of obesity among adults and youth: United States, 2015–2016. [PubMed] [Google Scholar]
- Hazuda H.P., Mitchell B.D., Haffner S.M., Stern M.P. Obesity in Mexican American subgroups: findings from the San Antonio Heart Study. Am. J. Clin. Nutr. 1991;53(6):1529S–1534S. doi: 10.1093/ajcn/53.6.1529S. [DOI] [PubMed] [Google Scholar]
- Himmelgreen D.A., Pérez-Escamilla R., Martinez D. The longer you stay, the bigger you get: length of time and language use in the US are associated with obesity in Puerto Rican women. Am. J. Phys. Anthropol. 2004;125(1):90–96. doi: 10.1002/ajpa.10367. [DOI] [PubMed] [Google Scholar]
- Isasi C.R., Ayala G.X., Sotres-Alvarez D. Is acculturation related to obesity in Hispanic/Latino adults? Results from the Hispanic community health study/study of Latinos. J. Obes. 2015;2015 doi: 10.1155/2015/186276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kearns K., Dee A., Fitzgerald A.P., Doherty E., Perry I.J. Chronic disease burden associated with overweight and obesity in Ireland: the effects of a small BMI reduction at population level. BMC Public Health. 2014;14(1):143. doi: 10.1186/1471-2458-14-143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khan L., Sobal J., Martorell R. Acculturation, socioeconomic status, and obesity in Mexican Americans, Cuban Americans, and Puerto Ricans. Int. J. Obes. Relat. Metab. Disord. 1997;21(2) doi: 10.1038/sj.ijo.0800367. [DOI] [PubMed] [Google Scholar]
- Langellier B.A., Brookmeyer R., Wang M.C., Glik D. Language use affects food behaviours and food values among Mexican-origin adults in the USA. Public Health Nutr. 2015;18(2):264–274. doi: 10.1017/S1368980014000287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laraia B.A. Food insecurity and chronic disease. Adv. Nutr. 2013;4(2):203–212. doi: 10.3945/an.112.003277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larsen P., Harris K., Ward D., Popkin B. Acculturation on overweight behaviors among Hispanic immigrants to the United States: the national longitudinal study of adolescent health. Soc. Sci. Med. 2003;57:2023–2034. doi: 10.1016/s0277-9536(03)00072-8. [DOI] [PubMed] [Google Scholar]
- Livingston G., Minushkin S., Cohn D.V. Pew Hispanic Center; 2008. Hispanics and the Health Care in the United States: Access, Information and Knowledge: A Joint Pew Hispanic Center and Robert Wood Johnson Foundation Research Report. [Google Scholar]
- Marin G., Gamba R.J. A new measurement of acculturation for Hispanics: the Bidimensional Acculturation Scale for Hispanics (BAS) Hisp. J. Behav. Sci. 1996;18(3):297–316. [Google Scholar]
- Marino R., Stuart G.W., Minas I.H. Acculturation of values and behavior: a study of Vietnamese immigrants. Meas. Eval. Couns. Dev. 2000;33(1):21. [Google Scholar]
- Matsudaira T. Measures of psychological acculturation: a review. Transcult. Psychiatry. 2006;43(3):462–487. doi: 10.1177/1363461506066989. [DOI] [PubMed] [Google Scholar]
- Mattei J., McClain A., Falcón L., Noel S., Tucker K. Dietary acculturation among Puerto Rican adults varies by acculturation construct and dietary measure. J. Nutr. 2018;148(11):1804–1813. doi: 10.1093/jn/nxy174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaren L. Socioeconomic status and obesity. Epidemiol. Rev. 2007;29(1):29–48. doi: 10.1093/epirev/mxm001. [DOI] [PubMed] [Google Scholar]
- Miller A.M., Chandler P.J., Wilbur J., Sorokin O. Acculturation and cardiovascular disease risk in midlife immigrant women from the former Soviet Union. Prog. Cardiovasc. Nurs. 2004;19(2):47–55. doi: 10.1111/j.0889-7204.2004.02267.x. [DOI] [PubMed] [Google Scholar]
- Ogden C.L., Carroll M.D. 6(1) National Center for Health Statistics; 2010. Prevalence of Overweight, Obesity, and Extreme Obesity Among Adults: United States, Trends 1960–1962 Through 2007–2008; pp. 1–6. [Google Scholar]
- Park Y., Neckerman K., Quinn J., Weiss C., Jacobson J., Rundle A. Neighbourhood immigrant acculturation and diet among Hispanic female residents of New York City. Public Health Nutr. 2011;14(9):1593–1600. doi: 10.1017/S136898001100019X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pérez-Escamilla R. Acculturation, nutrition, and health disparities in Latinos. Am. J. Clin. Nutr. 2011;93(5):1163S–1167S. doi: 10.3945/ajcn.110.003467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puhl R.M., Heuer C.A. The stigma of obesity: a review and update. Obesity. 2009;17(5):941–964. doi: 10.1038/oby.2008.636. [DOI] [PubMed] [Google Scholar]
- Reilly J.J., Methven E., McDowell Z.C. Health consequences of obesity. Arch. Dis. Child. 2003;88(9):748–752. doi: 10.1136/adc.88.9.748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Satia-Abouta J., Patterson R.E., Neuhouser M.L., Elder J. Dietary acculturation: applications to nutrition research and dietetics. J. Am. Diet. Assoc. 2002;102(8):1105–1118. doi: 10.1016/s0002-8223(02)90247-6. [DOI] [PubMed] [Google Scholar]
- Seeman T.E., Charpentier P.A., Berkman L.F. Predicting changes in physical performance in a high-functioning elderly cohort: MacArthur studies of successful aging. J. Gerontol. 1994;49(3):M97–M108. doi: 10.1093/geronj/49.3.m97. [DOI] [PubMed] [Google Scholar]
- The State of Obesity Disparities - Latinos. 2017. https://stateofobesity.org/disparities/latinos/
- Tropp L.R., Erkut S., Coll C.G., Alarcón O., García H.A.V. Psychological acculturation: development of a new measure for Puerto Ricans on the US mainland. Educ. Psychol. Meas. 1999;59(2):351–367. doi: 10.1177/00131649921969794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tucker K.L., Mattei J., Noel S.E. The Boston Puerto Rican Health Study, a longitudinal cohort study on health disparities in Puerto Rican adults: challenges and opportunities. BMC Public Health. 2010;10(1):107. doi: 10.1186/1471-2458-10-107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Rompay M.I., McKeown N.M., Castaneda-Sceppa C., Falcón L.M., Ordovás J.M., Tucker K.L. Acculturation and sociocultural influences on dietary intake and health status among Puerto Rican adults in Massachusetts. J. Acad. Nutr. Diet. 2012;112(1):64–74. doi: 10.1016/j.jada.2011.08.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wack J.T., Rodin J. Smoking and its effects on body weight and the systems of caloric regulation. Am. J. Clin. Nutr. 1982;35(2):366–380. doi: 10.1093/ajcn/35.2.366. [DOI] [PubMed] [Google Scholar]
- Wang S., Quan J., Kanaya A.M., Fernandez A. Asian Americans and obesity in California: a protective effect of biculturalism. J. Immigr. Minor. Health. 2011;13(2):276–283. doi: 10.1007/s10903-010-9426-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang D., van Meijgaard J., Shi L., Cole B., Fielding J. Does neighbourhood composition modify the association between acculturation and unhealthy dietary behaviours? J. Epidemiol. Community Health. 2015;69(8):724–731. doi: 10.1136/jech-2014-203881. [DOI] [PMC free article] [PubMed] [Google Scholar]