Abstract
Background
Geriatric patients are susceptible to respiratory and hemodynamic adverse events during endotracheal intubation and extubation due to anatomic and physiological changes with aging. Supraglottic airway devices (SADs) provide reduced airway morbidity and increased hemodynamic stability in adults. However, studies that have compared the clinical performance of SADs in geriatric patients are limited. Therefore, we evaluated the clinical performance of airway management with i-gel® and laryngeal mask airway Supreme (LMA SupremeTM) in geriatric patients.
Methods
The subjects were American Society of Anesthesiologists physical status classification I–III geriatric (65–85 years) patients who underwent elective surgery with general anesthesia and were randomly allocated into the i-gel® group and the LMA SupremeTM group. We compared the time for successful insertion on a first attempt as a primary outcome, and the secondary outcomes were success rate, ease of insertion, maneuver for successful ventilation, oropharyngeal leak pressure, gastric insufflation, fiberoptic view grades, ventilator problems, and adverse events.
Results
Insertion time was significantly shorter for the i-gel® than the LMA SupremeTM (21.4 ± 6.8 vs. 29.3 ± 9.9 s; P = 0.011). The i-gel® was also easier to insert than the LMA SupremeTM (P = 0.014). Gastric insufflation was less frequent with the i-gel® than the LMA SupremeTM (0% vs. 31.3%; P = 0.013). Other measurements were comparable between groups.
Conclusions
Both devices can be safely applied to geriatric patients with similar success rates and oropharyngeal leak pressures. However, inserting the i-gel® was faster and easier compared to the LMA SupremeTM in geriatric patients.
Keywords: Aging, Airway management, Geriatric, Intubation, Morbidity, Supraglottic devices
Introduction
Geriatric patients are vulnerable to perioperative pulmonary complications during intubation and extubation [1,2]. Supraglottic airway devices (SADs) have been used for resuscitation and difficult intubation as a relatively easy airway management method [3] and in elective general anesthesia with reduced airway complications [4]. SADs can maintain stable hemodynamics, as less anesthetic agent is required compared to endotracheal intubation [5].
Among the SADs, the i-gelⓇ (Intersurgical Ltd., UK) has a gel-like flexible and non-inflatable cuff, which accommodates the anatomic surface after insertion. The laryngeal mask airway SupremeTM (LMA SupremeTM, Teleflex Medical Europe Ltd., Ireland) has a characteristic high sealing pressure due to a curveshaped inflatable cuff [6]. Both SADs were recently introduced and have a gastric channel for suction to minimize the risk of aspiration due to gastric insufflation. In addition, both can be used for elective laparoscopic surgery as well as difficult intubations and resuscitation [6].
Parapharyngeal fat deposition increases with age and causes pharyngeal collapse in elderly patients [7]. In addition, structural changes in the respiratory tract combined with respiratory physiologic changes can depress oxygen saturation, blunt the hypoxia response, and increase postoperative respiratory complications [8]. The possibility of bone structural changes, such as retrognathia, which is usually considered a difficult airway, has been suggested due to acquired changes in pharyngeal muscle activity with aging [7]. Therefore, these changes due to aging can affect the clinical performance of the SADs. Certainly, the clinical efficacy of the laryngeal mask airway ClassicTM (LMA ClassicTM, Laryngeal Mask Company Ltd., UK) in geriatric patients is inferior to that in young patients; geriatric patients show lower success rates, prolonged insertion times, and more frequent inadequate ventilation [2]. These findings suggest the importance of selecting appropriately among the several SADs that can be used in geriatric patients. Although there have been a number of investigations of these two SADs [1,6,9–15], few studies have compared time for successful insertion, success rate of insertion, ease of insertion, oropharyngeal leak pressure, gastric insufflation, fiberoptic view grades, and ventilator problems in the elderly. Therefore, we designed this comparative study to compare the clinical performance between i-gelⓇ and LMA SupremeTM devices in geriatric patients.
Materials and Methods
After receiving approval from the Institutional Review Board of our hospital (KYUH 2017-06-017-001), this prospective randomized study was registered at the Korea Clinical Research Information Service (permit number: KCT 00002674). Informed consent was provided by the patients themselves or by a legal representative.
The 65–85 year-old patients of American Society of Anesthesiologist Physical Status classification I–III, undergoing an elective operation expected to last < 3 hours under general anesthesia in our hospital, were included as the subjects in this study. Patients with a high risk of aspiration (e.g., history of gastrectomy, body mass index > 35 kg/m2, gastroesophageal reflux disease, or hiatal hernia), loose teeth, unstable vital signs, cervical spine problems, abnormality of the oral cavity or pharynx, or high possibility of respiratory complications (e.g., asthma, chronic obstructive pulmonary disease, or recent pneumonia) were excluded.
Subjects were randomly allocated into the i-gelⓇ group or the LMA SupremeTM group using online randomization software (Researcher Randomizer; www.randomizer.org). The trained researcher who would insert the device opened a non-translucent envelope, which contained the group allocations, just before inducing anesthesia.
All patients fasted for at least 8 h and did not receive any premedication. When the patient was admitted to the operating room, noninvasive blood pressure, pulse oximetry, electrocardiography, bispectral index (BIS) monitoring, and neuromuscular train-of-four (TOF) monitoring on the adductor pollicis muscle were prepared in the supine position. Preoxygenation was carried out for at least 3 min with 100% O2 at 8 L/min fresh gas flow. The anesthetic induction agent was injected following attainment of 100% SpO2. Anesthesia was induced with 1–1.5 mg/kg propofol after injecting 1 mg/kg lidocaine. After confirming disappearance of the eyelash reflex and BIS < 65 followed by automatic calibration with CAL-2 mode of acceleromyography (TOF-WatchⓇ SX, Organon Ltd., Ireland), 0.6 mg/kg rocuronium was injected. When the TOF count was zero, the randomly assigned SAD (i-gelⓇ or LMA SupremeTM) was inserted by the same (board-certified) anesthesiologist who had experience of at least 150 insertions of each SAD to minimize bias due to familiarity with any specific device.
Each device was prepared in accordance with the manufacturer’s recommendations. The posterior and lateral sides of each device were lubricated with water-soluble gel. The size of the device was determined, depending on the patient’s weight and according to the manufacturer’s instructions [11]. The LMA SupremeTM required cuff insufflation with a cuff pressure of 60 cmH2O by manometry (PortexⓇ pressure gauge, Smiths Medical Intl. Ltd., UK). Immediately after inserting the device, mechanical ventilation was commenced: volume-controlled ventilation at 7 ml/kg and respiratory rate of 14 breaths/min. Anesthesia was maintained with 3–5 vol% desflurane and remifentanil at an effect site concentration of 2–4 ng/ml using a target-controlled infusion pump (OrchestraⓇ Base Primea, Fresenius Kabi, France) with the Minto model to keep the BIS level at 40–60.
The primary outcome of this study was the time required to insert the device successfully on the first attempt, which was defined as the time interval from picking up the device to the appearance of the first square waveform on capnography.
As secondary outcomes, we measured the first attempt and overall success rates, ease of insertion, maneuver for successful ventilation, oropharyngeal leak pressure (OLP), gastric insufflation, fiberoptic view grade, ventilation problems, and adverse events. The overall success rate was counted as the sum of the success rates of the first plus the second attempt. If more than two insertion attempts were needed, the selection of other airway management was left to the anesthesiologist’s discretion, and the subject was excluded from further evaluation. Ease of insertion was graded as follows: grade 1 = success on one attempt, and no tactile resistance during insertion; grade 2 = success on one attempt, but presence of tactile resistance during insertion; and grade 3 = success after more than two attempts [16]. Maneuvers for successful ventilation included a head extension, inserted depth adjustment, and/or jaw thrust. Successful ventilation was defined as a square waveform on capnography, at least two consecutive tidal volume ventilations, and no audible sounds from the mouth of the patient at a peak airway pressure ≤ 20 cmH2O [6]. OLP was measured by detecting an audible leak over the patient’s mouth upon closing the expiratory valve to 40 cmH2O with gas flow at 3 L/min [6,17]. Gastric insufflation was defined as the presence of a stethoscope sound in the epigastrium when OLP was measured [6,17]. The fiberoptic view by bronchoscopy was graded by a method used previously as follows: grade 1 = only vocal cord visible; 2 = vocal cord and/or arytenoid visible; 3 = only epiglottis visible; 4 = other structure (e.g., cuff, pharynx) visible [18]. The operation started after all data had been collected. If an abrupt increase in airway pressure and/or the presence of an abnormal waveform on capnography persisted during surgery despite an injection of additional rocuronium, it was considered a ventilation problem and recorded.
Ten minutes before the end of surgery, 1 μg/kg fentanyl was injected for postoperative pain control. At the end of surgery, all anesthetics were stopped, and the neuromuscular block was reversed with 2 or 4 mg/kg sugammadex based on neuromuscular monitoring. The device was removed when the BIS level was > 80 and the patient could follow verbal commands. During emergence, the occurrence of desaturation (SpO2 ≤ 95% for more than 10 s), coughing, and bronchospasm was recorded, as well as the presence of tongue, teeth, and lip injuries or a bloody tip after removing the device. All patients were observed for 1 h in the post-anesthesia care unit (PACU). Adverse events, such as sore throat, dysphagia, and dysphonia, were evaluated using a numerical rating scale (NRS; 0 = no symptoms, 10 = worst symptoms imaginable) immediately before leaving the PACU and after 24 hours. Primary and secondary outcome variables except ease of insertion, which was graded by the anesthesiologist who inserted the devices, were assessed by a registered research observer who was blinded to the purpose of this study.
Statistical analysis
The insertion times of both devices were measured in a preliminary study (n = 12 for each), and average insertion times of the i-gelⓇ and LMA SupremeTM were 22.5 s (SD 8.1 s) and 32.7 s (SD 11.3 s), respectively. Sample size was calculated with an effect size of 1.032, power of 0.8, and α-value of 0.05 (two-sided) and 16 patients were required per group. Taking into consideration a potential dropout rate of 15%, 19 patients were enrolled in each group. The data were analyzed with SPSS StatisticsTM software (IBM SPSS Inc., USA) version 18.
Continuous data were analyzed by Student’s t test or the Mann-Whitney U test where appropriate, after determining the data distribution using the Kolmogorov–Smirnov test. The chisquare test or Fisher’s exact test was used for categorical data, as appropriate. Differences in ease of insertion and the fiberoptic view between the two groups were analyzed using the chi-square test. In all analyses, P < 0.05 was taken to indicate statistical significance.
Results
Forty-two patients were assessed for eligibility for inclusion in this study, four of whom were excluded: two presented with uncontrolled blood pressure and two had loose teeth. Thus, 38 patients were randomly allocated into the i-gelⓇ or LMA SupremeTM group (Fig. 1).
Fig. 1.
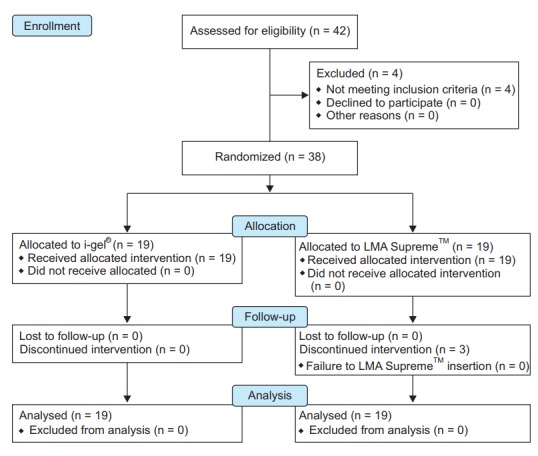
CONSORT flow diagram. Thirtyeight patients were randomly allocated into the i-gel® or LMA SupremeTM group. Three patients in the LMA SupremeTM group were excluded due to failed device insertion. However, data were collected before and during device insertion. LMA: laryngeal mask airway.
The patient characteristics and demographic data did not differ between the groups (Table 1). A comparison of the two devices during insertion is presented in Table 2. Insertion time was significantly shorter in the i-gelⓇ group than in the LMA SupremeTM group (21.4 ± 6.8 vs. 29.3 ± 9.9 s, respectively; mean difference −7.9 s; 95% CI −13.8 to −1.9 s; effect size 0.93; P = 0.011). In three patients in the LMA SupremeTM group the insertion failed, so these were excluded from further evaluation; i-gelⓇ was inserted in one after failure of LMA SupremeTM insertion and successful ventilation and the operation was conducted without any problem. i-gelⓇ insertion was attempted in the remaining two patients with the aid of a laryngoscope blade, but this also failed; thus, endotracheal intubation was conducted. The first attempt success rate and overall success rate did not differ between the two groups. However, ease of device insertion was significantly higher in the i-gelⓇ group than in the LMA SupremeTM group (grade 1/grade 2/grade 3 [number/%], [78.9%]/3 [15.8%]/1 [5.3%] vs. 7 [36.8%]/8 [42.2%]/4 [21.1%], respectively, P = 0.014).
Table 1.
Demographic Data
| Characteristic | i-gel® (n = 19) | LMA-S (n = 19) | P value |
|---|---|---|---|
| Age (yr) | 72.6 ± 6.2 | 70.9 ± 5.0 | 0.361 |
| Sex (M/F) | 11/8 | 10/9 | 0.744 |
| Type of operation | 0.770 | ||
| Urologic surgery | 10 | 8 | |
| Orthopedic surgery | 8 | 11 | |
| General surgery | 1 | 0 | |
| Height (cm) | 158.1 ± 8.9 | 159.2 ± 9.0 | 0.712 |
| Weight (kg) | 57.8 ± 11.6 | 63.8 ± 11.2 | 0.115 |
| BMI (kg/m2) | 23.4 ± 4.4 | 25.2 ± 4.0 | 0.199 |
| ASA (I/II/III) | 2/12/5 | 2/17/0 | > 0.999 |
| Mallampati classification (1/2/3/4) | 2/11/5/1 | 3/10/6/0 | 0.645 |
| Dental status (total/partial/edentulous) | 8/9/2 | 12/4/3 | 0.498 |
| Anesthesia time (min) | 90.9 ± 39.8 | 92.4 ± 40.3 | 0.914 |
| Surgical duration (min) | 67.3 ± 32.6 | 65.0 ± 38.3 | 0.851 |
Values are expressed as mean ± SD or numbers. LMA-S: LMA SupremeTM, BMI: body mass index, ASA: American Society of Anesthesiologists physical status classification.
Table 2.
Comparisons of the i-gel® and LMA SupremeTM during Insertion
| Variable | i-gel® (n = 19) | LMA-S (n = 19) | Difference of means (95% CI) | P value |
|---|---|---|---|---|
| Insertion time (s)* | 21.4 ± 6.8 | 29.3 ± 9.9 | −7.9 (−13.8, −1.9) | 0.011 |
| First attempt success (n [%]) | 18 (94.7) | 15 (78.9) | 15.8% (−7%, 38%) | 0.340 |
| Overall insertion success (n [%]) | 19 (100) | 16 (84.2) | 15.8% (−4%, 38%) | 0.230 |
| Ease of insertion† | NA | 0.014 | ||
| Grade 1 (n [%]) | 15 (78.9) | 7 (36.8) | ||
| Grade 2 (n [%]) | 3 (15.8) | 8 (42.1) | ||
| Grade 3 (n [%]) | 1 (5.3) | 4 (21.1) |
Values are numbers (%) or mean ± SD. LMA-S: LMA SupremeTM.
Insertion time was analyzed in cases of successful device insertion on first attempt (n = 18 for i-gel® and n = 15 for LMA-S).
Grade of ease of insertion: grade 1, success on first attempt without tactile resistance; grade 2, success on first attempt with tactile resistance; grade 3, success on second attempt or later with/without tactile resistance, NA: not applicable.
After inserting each device, the required maneuver for proper ventilation, OLP, fiberoptic view, and ventilation problem did not differ significantly between the two groups (Table 3). However, the i-gelⓇ group showed a significantly lower incidence of gastric insufflation than the LMA SupremeTM group (0% vs. 31.3%, respectively; mean difference −31.3; 95% CI −56% to −7%; P = 0.013; Table 3). The frequencies of adverse events were similar between the two groups (Table 4).
Table 3.
Comparisons of i-gel® and LMA SupremeTM after Insertion
| Variable | i-gel® (n = 19) | LMA-S (n = 16) | Mean difference (95% CI) | P value |
|---|---|---|---|---|
| Maneuver for ventilation (n [%]) | 6 (31.6) | 6 (37.5) | −5.9% (−35%, 23%) | 0.713 |
| Oropharyngeal leak pressure (cmH2O) | 26.9 ± 5.9 | 24.1 ± 4.3 | −7.9 (−13.8, −1.9) | 0.116 |
| Gastric insufflations (n [%]) | 0 (0) | 5 (31.3) | −31.3% (−56%, −7%) | 0.013 |
| Fiberoptic view (1/2/3/4, n)* | 2/12/5/0 | 0/13/3/0 | NA | 0.865 |
| Ventilation problem (n [%]) | 2 (10.5) | 5 (31.3) | −21.8% (−46%, 6%) | 0.207 |
Values are mean ± SD, number (%), or number. LMA-S: LMA SupremeTM, NA: not applicable.
Fiberoptic view grading: grade 1, only vocal cord visible; 2, vocal cord and/or arytenoid visible; 3, only epiglottis visible; 4, other structure (e.g., cuff, pharynx) visible.
Table 4.
Adverse Events
| Event | i-gel® (n = 19) | LMA-S (n = 19) | P value |
|---|---|---|---|
| Tongue injury | 0 | 0 | NA |
| Lip injury | 0 | 0 | NA |
| Dental injury | 0 | 1 (6.3) | 0.457 |
| Bloody tip | 1 (5.3) | 3 (17.6) | 0.326 |
| Desaturation | 2 (10.5) | 0 (0) | 0.489 |
| Coughing | 0 | 0 | NA |
| Bronchospasm | 0 | 0 | NA |
| Sore throat NRS (0–10) | |||
| 1 h | 0 (0–2) | 0 (0–6) | 0.357 |
| 24 h | 0 (0–1) | 0 (0–3) | 0.251 |
| Dysphonia NRS (0–10) | |||
| 1 h | 0 (0–5) | 0 (0–5) | 0.125 |
| 24 h | 0 (0–1) | 0 (0–5) | 0.267 |
| Dysphagia NRS (0–10) | |||
| 1 h | 0 (0–2) | 0 (0–5) | 0.398 |
| 24 h | 0 (0–4) | 0 (0–3) | 0.251 |
Values are expressed as number (%) or median (ranges). LMA-S: LMA SupremeTM, NA: not applicable, NRS: numerical rating scale (0 = no symptom, 10 = worst symptom imaginable).
Discussion
The main findings of this study are that inserting the i-gelⓇ was faster and easier than that of the LMA SupremeTM in geriatric patients, although the success rates on the first attempt and the overall success rates were comparable. Moreover, gastric insufflation was less frequent with the i-gelⓇ than with the LMA SupremeTM, despite a similar OLP. These findings suggest that the i-gelⓇ may be more appropriate for emergency airway management of geriatric patients than the LMA SupremeTM. Another advantage of the i-gelⓇ in a difficult airway situation is that it can be used as a conduit for intubation after proper positioning, unlike the LMA SupremeTM [19].
In this comparative study of two devices in geriatric patients, we set the duration for successful device insertion as the primary outcome variable. Reducing insertion time was important because geriatric patients are highly susceptible to respiratory and/or neurological morbidity and mortality due to decreased functional reserve of the respiratory system and a delayed ventilatory response to oxygen desaturation or CO2 retention [20]. The risk of respiratory or neurological complications increases as apnea time is increased due to difficult airway management [8].
Diverse outcomes have been reported with identical devices in different subjects. Previous studies in pediatric [13] or mainly adult patients [6,9,12] indicated similar [6,12,13] or longer insertion times [9] for the i-gelⓇ compared to the LMA SupremeTM. In a previous randomized controlled study that applied a difficult airway scenario without a neuromuscular blocking agent before insertion [9], the LMA SupremeTM showed a shorter insertion time than the i-gelⓇ in patients with an average age of 47 years (34 vs. 42 s, respectively) and the mean insertion time of i-gelⓇ (42 s) was double our insertion time (21 s). It was speculated that the large design of the i-gelⓇ resulted in a longer insertion time. In contrast, the insertion time of the i-gelⓇ was shorter than the LMA SupremeTM in our study. In the present study, the shorter insertion time of i-gelⓇ may have been because it does not require cuff inflation. However, when considering that the time required for cuff inflation is just 2–3 s, it could not fully explain the difference in mean insertion time (about 8 s). Another possible reason for faster insertion of the i-gelⓇ in our study is anatomic changes from aging or the characteristics of each device. The ratio of tongue and parapharyngeal fat deposition in the face and the presence of retrognathia can increase along with a decrease in the muscle ratio with aging [7]. In elderly patients whose soft tissue ratio in the face is relatively high and who are prone to sleep apnea [7,21], the i-gelⓇ compresses the tongue, whereas insertion of the pre-curved (or fixed shaped) LMA SupremeTM would be difficult because the LMA SupremeTM does not press the lingual soft tissue for proper positioning [10]. In addition, a device of predetermined shape like the LMA SupremeTM, compared to the i-gelⓇ, which has a thermoplastic elastomer cuff, may have difficulty reflecting the age-related changes. This notion is supported by the ease of insertion results; the i-gelⓇ could be inserted with less tactile resistance than the LMA SupremeTM (incidence of easy insertion; i-gelⓇ 78.9% vs. LMA SupremeTM 36.8%, Table 2). Furthermore, we defined the insertion time until confirming successful ventilation. As epiglottic down-folding is caused less by the i-gelⓇ than the LMA SupremeTM [10], the time until presenting the appearance of the first square waveform in capnography would decrease.
In contrast to the results of the present study, the insertion time was comparable between the two devices in a recently published study that compared the clinical performance of the i-gelⓇ and LMA SupremeTM in elderly patients (i-gelⓇ 34.7 ± 64.4 vs. LMA SupremeTM 48.8 ± 45.6 s; P = 0.2) [11]. The difference in insertion time between this and previous studies may have been due to the different definition of insertion time; three insertion attempts were allowed and the time between each insertion attempt and any bag-mask ventilation was included as the insertion time in the previous study [11]. However, when the patients were subdivided by insertion time < 30 s or > 1 min, the results were similar to those in the present study; significantly more patients required < 30 s to insert the i-gelⓇ than the LMA SupremeTM (84.9% vs. 48.1%; P < 0.001), while > 1 min was required to insert the LMA SupremeTM in a significantly greater number of patients than the i-gelⓇ (25.0% vs. 7.5%; P = 0.018).
In this study, the first attempt success rate and overall success rate were comparable between the i-gelⓇ and the LMA SupremeTM. Similar to the results of our study, most previous studies that compared the two devices did not show a significant difference in the first attempt or overall success rates regardless of the airway situation (normal or difficult), use of a neuromuscular blocking agent (paralyzed or non-paralyzed), or age of the subject (child, adult, or elderly) [6,9,11–13]. On the other hand, in a study comparing the success rates of two SADs by airway novices in female patients over 18 years of age [14], the success rate of first insertion was higher for the LMA SupremeTM than the i-gelⓇ (77% vs. 54%, respectively). The authors explained that the higher insertion success rate of the LMA SupremeTM could be accounted for by the bulky design of the i-gelⓇ, making for a difficult insertion by airway novices. However, our study was conducted in the context of a normal airway by an experienced anesthesiologist for the safety of the elderly patients. Accordingly, insertion success rates of both devices in our study were higher than in the study with novices and may not have caused the intergroup difference in success rate.
Ease of insertion was significantly different for the two SADs. The rates of ‘easy’ when each SAD was inserted were 78.9% and 36.8% for the i-gelⓇ and LMA SupremeTM, respectively. Unlike in our study, ease of insertion was comparable in the two studies on adult patients [9,15] and the LMA SupremeTM was easier to insert than the i-gelⓇ in another study [12]. However, these previous three studies evaluated the ease of insertion with other standards (5- or 4-point scales), and the standards were completely subjective without definite criteria. On the other hand, our study set up a relatively objective standard by applying the number of attempts and measuring resistance. The reason why insertion of the i-gelⓇ was easier than the LMA SupremeTM in our study was probably due to the difference in shape of the two SADs. The i-gelⓇ is nearly straight in the tube portion and flexible, so that insertion in the pharyngeal direction is possible without handling. However, because the tube portion of LMA SupremeTM is pre-curved and relatively rigid compared to the i-gelⓇ, it feels resistant and more difficult to insert based on this tube curvature.
The i-gelⓇ significantly decreased the incidence of gastric insufflation in this study. This may have been due not only to the difference in shape of the two SADs, but also to variations in anatomical structures in the elderly. Muscle atrophy, which is a major change in the elderly, may prevent proper esophageal sphincter function. Although the length of insertion into the esophagus is deeper for the LMA SupremeTM than for the i-gelⓇ, the inserted cuff width, which protects against aspiration, is narrower in the LMA SupremeTM [10]. Consequently, gastric insufflation may occur more in LMA SupremeTM, even with a similar leak pressure. The difference suggests that the risk of gastric regurgitation might decrease for the i-gelⓇ when the recruitment maneuver is performed in elderly patients.
Adverse events related to each device were comparable in this study. A meta-analysis that compared the i-gelⓇ with the LMA SupremeTM in adults aged 18–80 years [1] showed similar incidences of blood on the removed tip, but more sore throats in patients who received the LMA SupremeTM. This meta-analysis does not practically reflect elderly patients, because the age range of subjects was broad and the subjects included a higher number of younger patients than elderly patients.
Some limitations and topics for further study are worthy of consideration here. First, the sample size of this study was calculated to use insertion time as the primary outcome variable. Thus, our study may have been underpowered to assess the secondary endpoints of success rate and adverse events. A further study in a larger geriatric population is needed to evaluate these outcome variables accurately. Second, the existence of teeth can affect the insertion of a SAD. When teeth make a space between the maxilla and mandible, insertion of a SAD may be easier than when no teeth are present [21,22]. In this study, although dental status did not differ between the two groups, a study conducted with all teeth, partial teeth, and edentulous patients in one group could affect the results. In addition, although the present study was conducted in elderly patients aged 65–85 years, the age range of 20 years makes it difficult to regard this as a homogenous group in airway management due to differences in alveolar bone resorption [23]. Therefore, further studies are needed to compare the two devices in only edentulous patients or in patients subdivided by age group. Third, this study could not be conducted in a double-blind manner due to the difference in shape of the two devices. Accordingly, there was a potential risk for some bias. However, insertion time was the primary outcome measured and the definition of insertion time was objective and quite clear. Finally, we used a neuromuscular blocking agent before inserting the SAD because of the higher success rate, higher sealing pressure, lower leakage volume, lower insertion difficulty, and reduced anesthetic requirement for insertion [5,24]. Unless the surgery is long, future study should be conducted without a neuromuscular blocking agent. The original purpose of these SADs is to secure a safe airway in an emergency situation by a non-anesthesiologist or paramedical staff without using a neuromuscular blocking agent; thus, a further study should analyze the clinical difference of both devices in elderly patients without a neuromuscular blocking agent [25].
In conclusion, both the i-gelⓇ and the LMA SupremeTM were safe and usable in elderly patients without a significant difference in adverse events. However, the i-gelⓇ can be quickly and easily used compared to the LMA SupremeTM in geriatric patients, with less concern about gastric insufflation. Thus, the i-gelⓇ should be primarily considered in anesthetized and paralyzed geriatric patients.
References
- 1.Chen X, Jiao J, Cong X, Liu L, Wu X. A comparison of the performance of the I-gelTM vs. the LMA-STM during anesthesia: a meta-analysis of randomized controlled trials. PLoS One. 2013;8:e71910. doi: 10.1371/journal.pone.0071910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kim EM, Kim MS, Koo BN, Lee JR, Lee YS, Lee JH. Clinical efficacy of the classic laryngeal mask airway in elderly patients: a comparison with young adult patients. Korean J Anesthesiol. 2015;68:568–74. doi: 10.4097/kjae.2015.68.6.568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lalit G, Kapil C, Poonam B. I-Gel: a rescue intubation device in unanticipated difficult intubation for emergency laparotomy. Open J Anesthesiol. 2012;2:44–6. [Google Scholar]
- 4.Yu SH, Beirne OR. Laryngeal mask airways have a lower risk of airway complications compared with endotracheal intubation: a systematic review. J Oral Maxillofac Surg. 2010;68:2359–76. doi: 10.1016/j.joms.2010.04.017. [DOI] [PubMed] [Google Scholar]
- 5.Cho SA, Sung TY, Cho CK, Jee YS, Kang PS. Optimal propofol dosage for i-gel® insertion in healthy paralyzed patients. Korean J Anesthesiol. 2018;71:22–9. doi: 10.4097/kjae.2018.71.1.22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Teoh WH, Lee KM, Suhitharan T, Yahaya Z, Teo MM, Sia AT. Comparison of the LMA Supreme vs the i-gel in paralysed patients undergoing gynaecological laparoscopic surgery with controlled ventilation. Anaesthesia. 2010;65:1173–9. doi: 10.1111/j.1365-2044.2010.06534.x. [DOI] [PubMed] [Google Scholar]
- 7.Malhotra A, Huang Y, Fogel R, Lazic S, Pillar G, Jakab M, et al. Aging influences on pharyngeal anatomy and physiology: the predisposition to pharyngeal collapse. Am J Med. 2006;119:72. doi: 10.1016/j.amjmed.2005.01.077. e9-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sprung J, Gajic O, Warner DO. Review article: age related alterations in respiratory function - anesthetic considerations. Can J Anaesth. 2006;53:1244–57. doi: 10.1007/BF03021586. [DOI] [PubMed] [Google Scholar]
- 9.Theiler LG, Kleine-Brueggeney M, Kaiser D, Urwyler N, Luyet C, Vogt A, et al. Crossover comparison of the laryngeal mask supreme and the i-gel in simulated difficult airway scenario in anesthetized patients. Anesthesiology. 2009;111:55–62. doi: 10.1097/ALN.0b013e3181a4c6b9. [DOI] [PubMed] [Google Scholar]
- 10.Russo SG, Cremer S, Eich C, Jipp M, Cohnen J, Strack M, et al. Magnetic resonance imaging study of the in vivo position of the extraglottic airway devices i-gelTM and LMA-SupremeTM in anaesthetized human volunteers. Br J Anaesth. 2012;109:996–1004. doi: 10.1093/bja/aes314. [DOI] [PubMed] [Google Scholar]
- 11.Kim MH, Lee JH, Choi YS, Park S, Shin S. Comparison of the laryngeal mask airway supreme and the i-gel in paralysed elderly patients: a randomised controlled trial. Eur J Anaesthesiol. 2018;35:598–604. doi: 10.1097/EJA.0000000000000700. [DOI] [PubMed] [Google Scholar]
- 12.Chew EE, Hashim NH, Wang CY. Randomised comparison of the LMA Supreme with the I-Gel in spontaneously breathing anaesthetised adult patients. Anaesth Intensive Care. 2010;38:1018–22. doi: 10.1177/0310057X1003800609. [DOI] [PubMed] [Google Scholar]
- 13.Jagannathan N, Sommers K, Sohn LE, Sawardekar A, Shah RD, Mukherji II, et al. A randomized equivalence trial comparing the i-gel and laryngeal mask airway Supreme in children. Paediatr Anaesth. 2013;23:127–33. doi: 10.1111/pan.12078. [DOI] [PubMed] [Google Scholar]
- 14.Ragazzi R, Finessi L, Farinelli I, Alvisi R, Volta CA. LMA SupremeTM vs i-gelTM--a comparison of insertion success in novices. Anaesthesia. 2012;67:384–8. doi: 10.1111/j.1365-2044.2011.07002.x. [DOI] [PubMed] [Google Scholar]
- 15.Wang F, Zhang R. Application of the LMA-SupremeTM and i-gelTM laryngeal masks during pelvic operations in adults. Asian J Surg. 2016;39:1–5. doi: 10.1016/j.asjsur.2015.01.011. [DOI] [PubMed] [Google Scholar]
- 16.Brimacombe J, Holyoake L, Keller C, Brimacombe N, Scully M, Barry J, et al. Pharyngolaryngeal, neck, and jaw discomfort after anesthesia with the face mask and laryngeal mask airway at high and low cuff volumes in males and females. Anesthesiology. 2000;93:26–31. doi: 10.1097/00000542-200007000-00009. [DOI] [PubMed] [Google Scholar]
- 17.Keller C, Brimacombe JR, Keller K, Morris R. Comparison of four methods for assessing airway sealing pressure with the laryngeal mask airway in adult patients. Br J Anaesth. 1999;82:286–7. doi: 10.1093/bja/82.2.286. [DOI] [PubMed] [Google Scholar]
- 18.Verghese C, Berlet J, Kapila A, Pollard R. Clinical assessment of the single use laryngeal mask airway--the LMA-unique. Br J Anaesth. 1998;80:677–9. doi: 10.1093/bja/80.5.677. [DOI] [PubMed] [Google Scholar]
- 19.Almeida G, Costa AC, Machado HS. Supraglottic airway devices: a review in a new era of airway management. J Anesth Clin Res. 2016;7:1000647. [Google Scholar]
- 20.Liu LL, Wiener-Kronish JP. Perioperative anesthesia issues in the elderly. Crit Care Clin. 2003;19:641–56. doi: 10.1016/s0749-0704(03)00058-7. [DOI] [PubMed] [Google Scholar]
- 21.Johnson KN, Botros DB, Groban L, Bryan YF. Anatomic and physiopathologic changes affecting the airway of the elderly patient: implications for geriatric-focused airway management. Clin Interv Aging. 2015;10:1925–34. doi: 10.2147/CIA.S93796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Genez M, Küçükgüçlü S, Özbilgin Ş, Kuvaki B, Beydeş T, Aksoy Sari M. A comparison of usage of the laryngeal mask UniqueTM in denticulate and edentulate geriatric patients. Turk J Med Sci. 2017;47:854–60. doi: 10.3906/sag-1603-206. [DOI] [PubMed] [Google Scholar]
- 23.Streckfus CF, Parsell DE, Streckfus JE, Pennington W, Johnson RB. Relationship between oral alveolar bone loss and aging among African-American and Caucasian individuals. Gerontology. 1999;45:110–4. doi: 10.1159/000022072. [DOI] [PubMed] [Google Scholar]
- 24.Fujiwara A, Komasawa N, Nishihara I, Miyazaki S, Tatsumi S, Nishimura W, et al. Muscle relaxant effects on insertion efficacy of the laryngeal mask ProSeal® in anesthetized patients: a prospective randomized controlled trial. J Anesth. 2015;29:580–4. doi: 10.1007/s00540-015-1982-3. [DOI] [PubMed] [Google Scholar]
- 25.Soar J. The I-gel supraglottic airway and resuscitation--some initial thoughts. Resuscitation. 2007;74:197. doi: 10.1016/j.resuscitation.2007.02.012. [DOI] [PubMed] [Google Scholar]


