Abstract
BACKGROUND
Surgery 5-10 d after stent insertion was recommended by the European Society of Gastrointestinal Endoscopy for obstructing colonic cancer. For some obstructive patients, this may be not a good choice. Here, we report the successful treatment of obstructing colonic cancer by combining self-expandable stent and neoadjuvant chemotherapy.
CASE SUMMARY
The patient was a 72-year-old man who was admitted with a chief complaint of abdominal pain for more than 1 mo. Computed tomography (CT) scanning revealed that there was a mass in the descending colon, which led to intestinal obstruction. On admission, a series of therapeutic measures, such as fasting and water deprivation, gastrointestinal decompression, total parenteral nutrition, and octreotide acetate, were taken to improve the obstructive symptoms. At the same time, a self-expandable metal stent was successfully placed across the stenosis, and a biopsy was obtained and diagnosed as adenocarcinoma. CT scanning 14 d after insertion of the stent revealed that the intestine was swollen significantly. Systemic chemotherapy with modified FOLFOX6 (mFOLFOX6) was administered. After two courses of mFOLFOX6, CT scanning showed clearly that swelling of the intestine was improved. Subsequently, the patient underwent left hemi-colectomy without stoma placement. The postoperative course was uneventful, and he has been disease-free for 6 mo after surgery.
CONCLUSION
This modified treatment strategy may provide an alternative therapy for patients with obstructing colonic cancers.
Keywords: Stent, Colorectal neoplasms, Intestinal obstruction, Chemotherapy, Case report
Core tip: As a bridge to surgery, the use of stents for potentially resectable colorectal cancers makes it possible to convert urgent to elective surgery. The European Society of Gastrointestinal Endoscopy guideline in 2014 recommended a 5-10 d time interval to operation. However, patients who experience a chronic obstruction are usually in a poor state because of inadequate nutritional intake, and the intestine is swollen. We modified the therapeutic strategy by prolonging the time interval to operation; two cycles of chemotherapy were administered before the operation.
INTRODUCTION
About 8%-13% of advanced colonic cancer can cause large-bowel obstruction. The self-expandable metal stent (SEMS) is widely used, and it has become a safe modality to treat colorectal cancer with obstruction. The insertion of SEMS can relieve the symptoms of obstruction quickly and gain preparation time for the patients who have the opportunity to undergo a radical operation. A time interval to operation of 5-10 d is recommended by the European Society of Gastrointestinal Endoscopy (ESGE) as a bridge to elective surgery in patients with potentially curable left-sided colon cancer. However, because of the chronic obstruction, swelling of intestine is common, and patients usually suffer from malnutrition, electrolyte disturbances, and some other disorders[1]. Stoma rate and complication rate are high in surgically treated patients[2]. We here report a case of a male patient who received two cycles of chemotherapy after insertion of the stent. This improved the patient’s condition, inhibited tumor progression, and achieved a satisfactory outcome.
CASE PRESENTATION
Chief complaints
A 72-year-old male was admitted to our hospital by a flat vehicle with a complaint of abdominal pain for more than 1 mo.
History of present illness
One month ago, the patient had a symptom of abdominal pain in the left lower abdomen. He came to the local hospital and was prescribed traditional Chinese medicine. However, the medicine was not effective. The abdominal pain aggravated, and the pain was located in the total abdomen and was accompanied by distention. His appetite lessened as the illness progressed. Three days ago, the patient stopped flatus and defecation, and he was moved to another local hospital. Computed tomography (CT) scanning revealed that there was a mass in the descending colon, which led to intestinal obstruction. For further treatment, the patient was transferred to our hospital. During his illness, he lost 6 kg of body weight and became progressively weaker.
History of past illness
He had no chronic illness.
Physical examination upon admission
Physical examination showed abdominal tenderness in the whole abdomen, and muscle tension was not palpated. The bowel sounded active, with six to eight bowel sounds per min.
Laboratory examinations
Laboratory findings indicated that CA125 was 80.90 U/mL (reference range < 30.2), albumin 28.8 g/L (reference range 40-55 g/L), sodium ions 132.9 mmol/L (reference range 137-147 mmol/L), and hemoglobin 94 g/L (reference range 130-175 g/L).
Imaging examinations
CT scanning revealed that there was a mass in the descending colon, which led to intestinal obstruction. The colon and whole small intestine were swollen.
FINAL DIAGNOSIS
Intestinal obstruction, colon cancer, mild anemia, hyponatremia, and hypoproteinemia.
TREATMENT
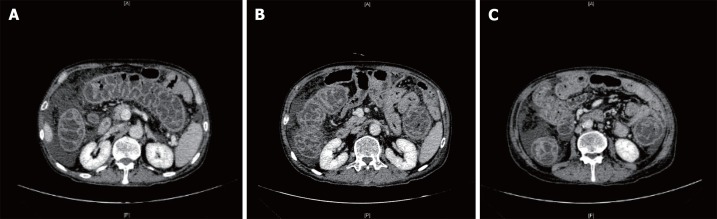
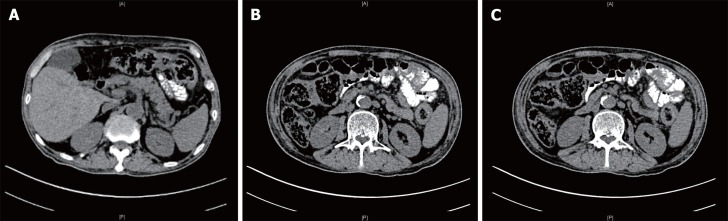
After admission, drinking and eating were prohibited. Total parenteral nutrition was given to improve the nutritional status. Octreotide acetate was administered to inhibit the secretion of digestive juices. To resolve the colonic stenosis, the SEMS was successfully placed across the stenosis. Biopsy was obtained, which was diagnosed as adenocarcinoma. CT scanning 14 d after stent placement revealed that the colon and small intestine were significantly swollen (Figure 1). The patient received systemic chemotherapy with modified FOLFOX6 (mFOLFOX6). The regimen consisted of racemic leucovorin 200 mg/m2, oxaliplatin 130 mg/m2 in a 2-h infusion, bolus fluorouracil 400 mg/m2 on day 1, and a 46-h infusion of fluorouracil 2400 mg/m2. The tumor responded remarkably to chemotherapy, and CA125 returned to normal level. CT scanning 40 d after stent placement revealed that the swelling of the colon and small intestine improved obviously except for the descending colon (Figure 2). The number of metastatic lymph nodes decreased. After two courses of mFOLFOX6, the patient underwent left-side colectomy. During the operation, the small intestine and proximal colon were normal, thus no stoma placement was performed. The pathological diagnosis was moderately differentiated adenocarcinoma of the descending colon. No cancer cells were identified in lymph nodes (0/36). The tumor had invaded the serosal layer. Incisional margins were negative. The pathological TNM stage was ypT4N0M0, and the regression grade was TRG1. The patient received an additional six cycles of chemotherapy with XELOX.
Figure 1.
Computed tomography scanning 14 d after insertion of stent. Transverse colon (A), ascending colon (B), and small intestine (C) were swollen.
Figure 2.
Computed tomography scanning 40 d after insertion of stent. Transverse colon (A), ascending colon (B), and small intestine (C) return to normal.
OUTCOME AND FOLLOW-UP
He recovered well. During a follow-up of 6 mo, there were no signs of recurrence or metastasis.
DISCUSSION
Colorectal cancer is one of the most common malignant tumors, and about 8%-13% of advanced colonic cancer can cause large-bowel obstruction[3,4]. Obstructive colonic cancer is an urgent condition that needs to be managed immediately. Compared to non-emergent surgery or surgery for non-obstructive condition, emergency surgical decompression is associated with both higher operative mortality and poor overall survival[5,6]. Moreover, stoma placement such as colostomy decreases quality of life.
SEMS placement has been applied over 20 years for the treatment of colonic obstruction[7]. As the stent type has evolved, colonic stents have been used to treat colonic malignancies either as a bridge to surgery or as a palliative measure[8,9]. As a bridge to surgery, the use of stents for potentially resectable colorectal cancers makes it possible to convert urgent to elective surgery. According to the literature, the stent-related complication rate, which includes perforation, bleeding, pain, re-obstruction, etc., is about 20%[10]. Perforation is the most serious complication, and the long-term perforation rate is 7.6%[11].
In the present case, the patient was in a poor state and could not eat or drink for more than 7 d. He had a weight loss of 6 kg. After insertion of stent, the symptoms of obstruction were alleviated significantly. The use of the stent converted an urgent surgery to an elective surgery. The guideline of the ESGE suggests an interval of 5-10 d between SEMS and elective resection[11]. However, in this case, the intestinal obstruction had formed for about 1 mo, and the intestine was very swollen. In addition, the patient was in poor nutritional status. If we performed the operation, the stoma would be done, and the complication rate would be relatively high. With a longer interval, the patient would have a better recovery and more optimal nutritional status. Some studies reported, however, that endoscopic stent insertion for colorectal cancer may result in tumor cell dissemination into the peripheral circulation and may induce distant metastases, leading to poor prognosis[12,13]. In order to reduce the complication rate and avoid distant metastases, we did not perform the operation immediately. Instead, two cycles of chemotherapy were administered. About 40 d later, the patient recovered well and the tumor markers returned to normal level. CT scanning revealed that the intestine was not swollen except for the descending colon. The operation was successful, and no stoma placement was performed.
According to the guideline of the ESGE, the recommended interval between SEMS and operation is 5-10 d. This suggestion, however, was based on limited data[11]. Clinically, we found that swollen intestine was commonly found in patients with intestinal obstruction. The longer the obstruction exists, the slower the swelling regresses. Theoretically, a longer interval will allow for better recovery and more nearly optimal nutritional status, but this may increase the risk of stent-related complications and may cause tumor cell dissemination. Based on this case, we believe that an interval of 4-6 wk between SEMS and operation may be a better treatment option. During this time, two to three cycles of chemotherapy can be performed. This modified treatment pattern can improve patient’s nutritional status and inhibit tumor cell dissemination, thereby improving patient prognosis.
Since this case, we have treated 11 similar patients, and the clinical result was satisfactory. This strategy provides an alternative therapy, particularly when the intestine is very swollen, and reduces the stoma placement rate.
CONCLUSION
After stent insertion in patients with obstructing colonic cancer, an interval of 2-3 wk to operation may be a good option for patients with a very swollen intestine. This interval can reduce the stoma and complication rates.
Footnotes
Informed consent statement: Consent was obtained from relatives of the patient for publication of this report and any accompanying images.
Conflict-of-interest statement: The authors declare that they have no conflicts of interest.
CARE Checklist (2016) statement: The manuscript was prepared and revised according to the CARE Checklist (2016).
Peer-review started: September 21, 2018
First decision: November 5, 2018
Article in press: December 1, 2018
Specialty type: Medicine, research and experimental
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P- Reviewer: Kim SJ, Tepetes K, Wei Y S- Editor: Wang JL L- Editor: Filipodia E- Editor: Song H
Contributor Information
Zhu-Lin Li, Department of General Surgery, Beijing Chaoyang Hospital affiliated to Capital Medical University, Beijing 100020, China.
Zhen-Jun Wang, Department of General Surgery, Beijing Chaoyang Hospital affiliated to Capital Medical University, Beijing 100020, China. drzhenjun@163.com.
Jia-Gang Han, Department of General Surgery, Beijing Chaoyang Hospital affiliated to Capital Medical University, Beijing 100020, China.
Yong Yang, Department of General Surgery, Beijing Chaoyang Hospital affiliated to Capital Medical University, Beijing 100020, China.
References
- 1.Gallardo-Valverde JM, Calañas-Continente A, Baena-Delgado E, Zurera-Tendero L, Vázquez-Martínez C, Membrives-Obrero A, Muntané J, Arévalo-Jiménez E. Obstruction in patients with colorectal cancer increases morbidity and mortality in association with altered nutritional status. Nutr Cancer. 2005;53:169–176. doi: 10.1207/s15327914nc5302_6. [DOI] [PubMed] [Google Scholar]
- 2.Arezzo A, Passera R, Lo Secco G, Verra M, Bonino MA, Targarona E, Morino M. Stent as bridge to surgery for left-sided malignant colonic obstruction reduces adverse events and stoma rate compared with emergency surgery: results of a systematic review and meta-analysis of randomized controlled trials. Gastrointest Endosc. 2017;86:416–426. doi: 10.1016/j.gie.2017.03.1542. [DOI] [PubMed] [Google Scholar]
- 3.Ohman U. Colorectal carcinoma in patients with ulcerative colitis. Am J Surg. 1982;144:344–349. doi: 10.1016/0002-9610(82)90017-4. [DOI] [PubMed] [Google Scholar]
- 4.Winner M, Mooney SJ, Hershman DL, Feingold DL, Allendorf JD, Wright JD, Neugut AI. Incidence and predictors of bowel obstruction in elderly patients with stage IV colon cancer: a population-based cohort study. JAMA Surg. 2013;148:715–722. doi: 10.1001/jamasurg.2013.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Serpell JW, McDermott FT, Katrivessis H, Hughes ES. Obstructing carcinomas of the colon. Br J Surg. 1989;76:965–969. doi: 10.1002/bjs.1800760932. [DOI] [PubMed] [Google Scholar]
- 6.Tilney HS, Lovegrove RE, Purkayastha S, Sains PS, Weston-Petrides GK, Darzi AW, Tekkis PP, Heriot AG. Comparison of colonic stenting and open surgery for malignant large bowel obstruction. Surg Endosc. 2007;21:225–233. doi: 10.1007/s00464-005-0644-1. [DOI] [PubMed] [Google Scholar]
- 7.Tejero E, Mainar A, Fernández L, Tobío R, De Gregorio MA. New procedure for the treatment of colorectal neoplastic obstructions. Dis Colon Rectum. 1994;37:1158–1159. doi: 10.1007/BF02049822. [DOI] [PubMed] [Google Scholar]
- 8.Allievi N, Ceresoli M, Fugazzola P, Montori G, Coccolini F, Ansaloni L. Endoscopic Stenting as Bridge to Surgery versus Emergency Resection for Left-Sided Malignant Colorectal Obstruction: An Updated Meta-Analysis. Int J Surg Oncol. 2017;2017:2863272. doi: 10.1155/2017/2863272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Costa Santos MP, Palmela C, Ferreira R, Barjas E, Santos AA, Maio R, Cravo M. Self-Expandable Metal Stents for Colorectal Cancer: From Guidelines to Clinical Practice. GE Port J Gastroenterol. 2016;23:293–299. doi: 10.1016/j.jpge.2016.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kobborg M, Broholm M, Frostberg E, Jeppesen M, Gögenür I. Short-term results of self-expanding metal stents for acute malignant large bowel obstruction. Colorectal Dis. 2017;19:O365–O371. doi: 10.1111/codi.13880. [DOI] [PubMed] [Google Scholar]
- 11.van Hooft JE, van Halsema EE, Vanbiervliet G, Beets-Tan RG, DeWitt JM, Donnellan F, Dumonceau JM, Glynne-Jones RG, Hassan C, Jiménez-Perez J, Meisner S, Muthusamy VR, Parker MC, Regimbeau JM, Sabbagh C, Sagar J, Tanis PJ, Vandervoort J, Webster GJ, Manes G, Barthet MA, Repici A European Society of Gastrointestinal Endoscopy (ESGE) Self-expandable metal stents for obstructing colonic and extracolonic cancer: European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline. Gastrointest Endosc. 2014;80:747–761.e1-75. doi: 10.1016/j.gie.2014.09.018. [DOI] [PubMed] [Google Scholar]
- 12.Yamashita S, Tanemura M, Sawada G, Moon J, Shimizu Y, Yamaguchi T, Kuwai T, Urata Y, Kuraoka K, Hatanaka N, Yamashita Y, Taniyama K. Impact of endoscopic stent insertion on detection of viable circulating tumor cells from obstructive colorectal cancer. Oncol Lett. 2018;15:400–406. doi: 10.3892/ol.2017.7339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Maruthachalam K, Lash GE, Shenton BK, Horgan AF. Tumour cell dissemination following endoscopic stent insertion. Br J Surg. 2007;94:1151–1154. doi: 10.1002/bjs.5790. [DOI] [PubMed] [Google Scholar]