Abstract
Aims
The Ponseti method is an effective evidence-based treatment for clubfoot. It uses gentle manipulation to adjust the position of the foot in serial treatments towards a more physiological position. Casting is used to hold the newly achieved position. At first, the foot resists the new position imposed by the plaster cast, pressing against the cast, but over time the tissues are expected to adapt to the new position and the force decreases. The aim of this study was to test this hypothesis by measuring the forces between a clubfoot and the cast during treatment with the Ponseti method.
Patients and Methods
Force measurements were made during the treatment of ten idiopathic clubfeet. The mean age of the patients was seven days (2 to 30); there were nine boys and one girl. Force data were collected for several weeks at the location of the first metatarsal and the talar neck to determine the adaptation rate of the clubfoot.
Results
In all measurements, the force decreased over time. The median (interquartile range) half-life time was determined to be at 26 minutes (20 to 53) for the first metatarsal and 22 minutes (9 to 56) for the talar neck, suggesting that the tissues of the clubfoot adapt to the new position within several hours.
Conclusion
This is the first study to provide objective force data that support the hypothesis of adaptation of the idiopathic clubfoot to the new position imposed by the cast. We showed that the expected decrease in corrective force over time does indeed exist and adaptation occurs after a relatively short period of time. The rapid reduction in the forces acting on the foot during treatment with the Ponseti method may allow significant reductions in the interval between treatments compared with the generally accepted period of one week.
Keywords: Clubfoot, Ponseti, Force, Adaptation
Clubfoot (talipes equinovarus) is a common congenital deformity that may be treated by the Ponseti method.1 In this method, the treating physician manipulates the clubfoot by applying manual pressure on the medial side of the first metatarsal (FM) with counter pressure on the lateral side of the talar neck (TN). This causes the forefoot to align with the talus while the calcaneus is manipulated into its proper position in the subtalar joint. The newly imposed position stretches and remodels the tissues of the clubfoot and is maintained for a week with a plaster cast. Most cases of clubfoot are corrected, sometimes with the addition of a percutaneous Achilles tenotomy, after five or six changes of cast.2 After the period of casting, an abduction brace needs to be worn for several years to prevent relapse.3
It is suggested that in serial casting, most of the correction is obtained by the manipulation. It is hypothesized that the plaster does not produce the correction but maintains the improved orientation of the foot, which is gained by the manipulation.4,5 The mechanical behaviour of clubfoot tissues can be characterized as visco-elastic.6,7 Thus, their behaviour is partly elastic, in which deformation is recovered after removal of the load, and partly plastic, in which deformation is permanent. Initially, the tissues resist correction, acting as a spring pressing on the cast. When the cast is removed after a week, the foot does not immediately return to its original position. It appears that the tissues adapt to the applied force over time. The decreasing stress in response to an initial stretch is known as stress-relaxation and the rate at which the force decreases is the rate of adaptation. It can be characterized by a half-life time t1/2, which is the time required for the force to decrease to half of its original value.
Quantifying the Ponseti method objectively would allow a better understanding of the corrective processes. Force sensors may be used to measure the corrective forces. We hypothesized that the force that the clubfoot exerts on the plaster cast will decrease with time, as a result of the adaptation of the tissues in the clubfoot to the position imposed by the plaster cast. The aim of this study was to test this hypothesis, to determine the forces exerted by the foot on the cast with the passage of time and to calculate the half-life time in a clubfoot undergoing correction using the Ponseti method.
Patients and Methods
This was an exploratory observational study performed at the University Medical Centre of Groningen (UMCG) in the Netherlands. The ethical evaluation committee of the UMCG reviewed the study in accordance with the declaration of Helsinki, and found that it did not meet the criteria as stated by the Medical Research Involving Human Subjects Act (WMO), and therefore did not require ethical approval (document number M16.196266).
Ten children with an idiopathic clubfoot, who were all aged less than three months and who had not undergone any previous treatment, were included in the study after obtaining informed written consent from their parents. Their mean age was seven days (2 to 30); there were nine boys and one girl. In those with bilateral clubfoot, the foot with the highest Pirani8 and Diméglio9 scores was included.
Figure 1a shows a custom-made force sensor, based on inductive sensing,10 that was specifically developed for the study. The output signal of the sensor is LHR_DATA, a 28-bit digital value proportional to the resonance frequency, which is a measure of the applied force. The design of the sensor and its performance, as summarized in Table I, have been previously described.10 A digital DS1825 thermometer (Maxim Integrated, San Jose, California) was included to allow removal of the temperature-induced signal error.
Table I.
The characteristics of the force sensor; for more details, see Giesberts et al10
| Characteristic | Value |
|---|---|
| Dimensions (ø × thickness), mm | 10 × 2.3 |
| Resolution, N | 0.15 × 10−3 |
| Accuracy, % | 3.4 |
| Sample rate, Hz | 18 |
| Drift, % / log10(hr) | < 2.1 |
| Hysteresis, % | 6.0 |
| Temperature sensitivity, N / ˚C | -0.1 |
An acquisition unit equipped with a small battery and microSD card was used to store the measurements of both the force sensors and the thermometer locally (Fig. 1b).
Fig. 1.
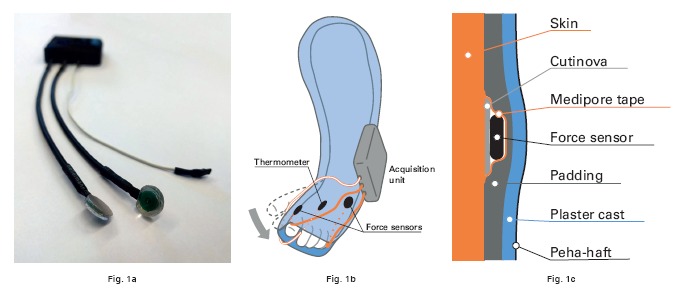
Use of the force sensor. a) Two custom-made inductive sensors were placed on the foot to measure the force of the foot on the cast. b) Wires were routed distally and the acquisition unit was attached to the cast laterally. c) The different layers on the skin.
Before use, the sensors were calibrated using ten weights of 100 g each. Both the Pirani and Diméglio scores were recorded to assess the severity of the deformity and the progress of treatment. Successful correction was defined as a Pirani score of ≤ 1.0 after treatment.
Before manipulation of the foot, the physician carefully placed a force sensor on both the first metatarsal and the talar neck using a Cutinova Hydro dressing (Smith & Nephew, Hull, United Kingdom) to protect the skin, and Medipore tape (3M, Neuss, Germany) to attach it (Fig. 1c). The thermometer was placed on the plantar aspect of the foot (Fig. 1b). A strip of Coban tape (3M) was applied between the skin and the thermometer and wires.
The foot was treated following the routine Ponseti method, without modifications. Wires were routed distally and, as soon as the plaster had set, the acquisition unit was attached to the cast laterally with a Peha-haft bandage (Hartmann GmbH, Heidenheim, Germany) (Fig. 1b).
At the next scheduled meeting, the cast and sensors were removed, after which the data were copied to a computer and the battery replaced while the parents had the opportunity to bathe their child. The foot was inspected for signs of skin damage and the protocol was repeated until the final cast before tenotomy.
The system was programmed to store time, force, and temperature data continuously for the first four hours, after which it entered a low power state to extend the battery life. It woke from this state four times per hour to collect data for ten seconds (Fig. 2). The timing of specific steps in the protocol, such as the placing of the sensors, the application of the cast, and the releasing of the foot, were recorded to identify important events in the data.
Fig. 2.
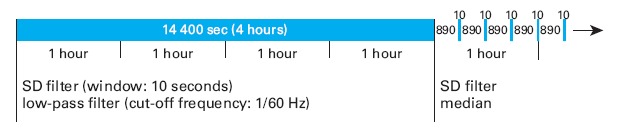
The measurement protocol. The system was programmed to measure the force continuously for the first four hours, after which it switched to a battery-saving protocol with four ten-second-long periods per hour.
Assuming that tissue mechanically behaves as a visco-elastic material, the resistive force when it is stretched to a certain length can be modelled using equation (1).11
| (1) |
In this equation, F(t) is the (resistive) force at time t, and F0 and F∞ are the starting (t = 0) and end force after a long time (at infinity), respectively. The parameter t1/2 is the half-life time. The equation means that the force decays from F0 to F∞. The lower the t1/2, the faster the force decays. t1/2 represents the time after which the force has dropped from F0 to half of the final value F∞. Figure 3 illustrates how the force decays to 95% after 4.3 half-life times.
Fig. 3.
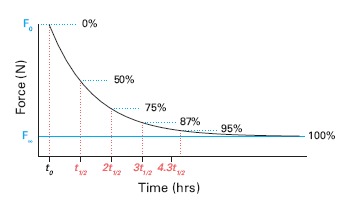
Expected decrease in force. The effect of equation (1) is shown. After t1/2 hours, the force will have decreased from F0 to F∞ with 50%, after 2t1/2 with 75%. After 4.3t1/2, 95% of the decrease will have happened.
Each set of retrieved data consisted of the time, force, and temperature of one week. All data were processed using Matlab version R2017b (Mathworks Inc., Natick, Massachusetts). Erroneous data points, that is LHR_DATA = 228 - 1, or T = 85°C, were removed from the data sets.12,13
The data were corrected for temperature changes and filtered to reduce the influence of noise caused by movements of the child. The first four hours of continuous force sensor data were processed using a moving standard deviation filter (stdfilt) with a window of ten seconds to identify and remove spikes. Next, the data were low-pass filtered (cut-off frequency 1/60 Hz) and resampled to have one data point per ten seconds. Each ten-second period in the data was filtered using the same standard deviation filter and the median was taken over the filtered data (Fig. 2). The force sensor data (LHR_DATA) were then converted to a force value (F(t)) using the calibration data. The start of each measurement (t0) was defined as the exact moment the physician released the foot, when casting was finished.
Each data set was then fit to equation (1) using Matlab 2017b’s fit function, which generates values and 95% confidence intervals (CIs) for F0, F∞, and t1/2. The restrictions (bounds) which were used for the fit function were 0.001·ln(2) < t1/2 < 1000·ln(2) hrs and F∞ < F0. Data sets for which t1/2 could not be calculated (R2 < 0.50) were excluded from further analysis.
Statistical analysis
The values for F0, F∞, and t1/2 were tested for normality using Lilliefors’ test and presented as median (interquartile range (IQR)). Statistical significance was defined as p < 0.05.
Results
The characteristics of the children are shown in Table II. All the clubfeet were treated successfully. Complications in the form of pressure marks on the skin were encountered in four children after a cast was removed. In one child, this was after the first cast; in the others, it was at a later stage (the third or fourth cast). Further measurements were cancelled in two of these four children but the data that had been obtained were included in the analysis. Technical malfunctioning occurred in ten measurements (insufficient battery power in eight, one disconnected force sensor, and one disconnected thermometer). In total, 29 successful measurements were performed on ten clubfeet.
Table II.
The characteristics of the children
| Characteristic | Value |
|---|---|
| Children, n | 10 |
| Mean age, days (range) | 7 (2 to 30) |
| Boys:girls, n | 9:1 |
| Bilateral, n | 6 |
| Mean pre-treatment Pirani score (sd) | 4.3 (0.7) |
| Mean pre-treatment Diméglio score (sd) | 14.0 (1.6) |
The results of a typical measurement are shown in Figure 4. For five data sets (three for the first metatarsal, and one for both the first metatarsal and the talar neck), the goodness of fit was too small (R2 < 0.50) to determine a relationship between the force and the time elapsed, and were excluded from further analysis. In total, 25 data sets for the force on the first metatarsal and 28 for the force on the talar neck were analyzed. The values for t1/2, F0, and F∞ are shown in Table III.
Fig. 4.
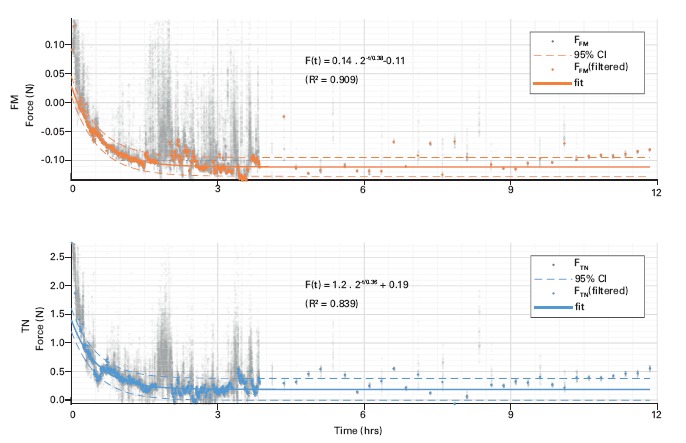
A typical example of the force on the first metatarsal (top) and the talar neck (bottom). The raw data in grey was first processed to get the filtered data in orange and blue. The filtered data was fitted to equation (1) to find the half-life time t1/2.
Table III.
Data are presented as median (interquartile range) as it was not normally distributed
| Sensor location | Parameter | Median (interquartile range) |
|---|---|---|
| First metatarsal | t1/2 (h:mm) | 0:26 (0:20 to 0:53) |
| F0 (N) | 0.29 (0.20 to 0.49) | |
| F∞ (N) | 0.09 (0.00 to 0.21) | |
| Talar neck | t1/2 (h:mm) | 0:22 (0:09 to 0:56) |
| F0 (N) | 0.41 (0.21 to 0.57) | |
| F∞ (N) | 0.03 (-0.42 to 0.16) |
Discussion
Previous authors have estimated the forces14 and torque15 on the clubfoot. Ours is the first report of force measurements in many children over several weeks of treatment each. This allowed the change of the force applied using the Ponseti method to be graphically visualized. There was a clear decrease in force in all measurements, with almost all data showing a typical stress-relaxation curve, supporting the hypothesis of a decrease of force over time. The adaptation may have taken place in the foot, in the cast, or both. However, the creep behaviour of cast materials is too limited for this effect,16 indicating that the tissues in the clubfoot adapt to the position imposed by the cast.
The study has limitations. Since the sensors are attached to the skin with tape, each measurement has an unknown baseline force acting on it. The exact location of the sensor is also unknown since both the skin and the padding can move in relation to the cartilaginous structures below. This makes the absolute values that are registered by the sensors unreliable as can be seen in the unlikely negative values for F∞. However, this does not affect the calculation of the half-life time (t1/2), since this is only determined by the shape of the curve and not its absolute value.
The small sample size did not allow for statistical analysis of differences within the group, such as laterality or gender.
Although a clear decrease in force was observed, it does not necessarily say anything about the internal structures in a clubfoot. No imaging techniques were used to allow correlation between the measured force and physical changes within the foot. Although a mechanical equilibrium was reached within several hours during every period of measurement, this does not imply that a biological equilibrium is reached during the same time span.
Stress-relaxation
As shown in Figure 3, after 4.3 times the half-life time (4.3t1/2, which under these circumstances corresponds to less than two hours), the corrective force has been reduced by 95% with respect to its final value (F∞). The forces do not change much after the first period; the tissues are in a stable position.
MRI studies comparing the appearances of the tarsal bones before and about ten minutes after casting show immediate changes in the shape of the cartilage anlagen of the tarsal bones.5,17,18 Stress-relaxation is said to occur within 15 to 20 minutes after the application of a cast,19,20 but therapists are warned that “this phenomenon cannot be repeated many times in rapid succession, because once the relaxation has occurred, the tissue length is maintained by the elastic restraints within the tissue components”.20,21 Our observation that the clubfoot reaches a mechanical equilibrium within two hours suggests that most of the correction is complete long before the end of one week and the treatment could be accelerated drastically. However, the biological processes that may influence the speed of correction are not yet fully understood. Decreasing the duration of casting has been proposed before5,17,18 and performed in studies in which the intervals between cast changes was altered from weekly to twice a week22,23 and even to three times a week.24 The studies all report a reduced time of treatment without adverse effects.25 More research is needed to find the optimal interval between changes of casts. Our findings suggest that if there is a limit to the reduction in the interval between cast changes, it is more likely to be related to biological rather than mechanical factors.
In conclusion, in the treatment of clubfoot using the Ponseti method, the foot is manipulated and held in place with a plaster cast. The applied forces rapidly decrease and reach an equilibrium within hours of casting, suggesting that the tissues of the clubfoot adapt and stresses within the foot reduce within a very short time. The rapid reduction of force between the foot and the cast suggests that the duration of treatment could be reduced significantly. More research is required to determine the optimal time interval between cast changes.
Take home message
- Stress on soft tissue is relaxed to a low level within hours after the application of the plaster cast.
- From a force-level point of view, there is room to shorten the time interval between consecutive castings.
Author contributions
R. B. Giesberts: Conceived and designed the experiments, Performed the experiments, Analyzed the data, Wrote the manuscript.
E. E. G. Hekman: Critically edited and reviewed the test protocol, the data interpretation, and the manuscript.
G. J. Verkerke: Critically edited and reviewed the test protocol, the data interpretation, and the manuscript.
P. G. M. Maathuis: Performed the experiments, Critically edited and reviewed the test protocol, the data interpretation, and the manuscript.
Funding statement
The authors report grant funding from Technology Foundation STW.
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
This is an open-access article distributed under the terms of the Creative Commons Attributions license (CC-BY-NC), which permits unrestricted use, distribution, and reproduction in any medium, but not for commercial gain, provided the original author and source are credited.
This article was primary edited by D. Johnstone and first proof edited by J. Scott.
Follow the authors @UTwente and @umcg
References
- 1.Ponseti IV, Smoley EN.. Congenital club foot: the results of treatment. J Bone Joint Surg [Am] 1963;45-A:261–344. [Google Scholar]
- 2.Morcuende JA, Dolan LA, Dietz FR, Ponseti IV.. Radical reduction in the rate of extensive corrective surgery for clubfoot using the Ponseti method. Pediatrics 2004;113:376–380. [DOI] [PubMed] [Google Scholar]
- 3.Dobbs MB, Rudzki JR, Purcell DB, et al. Factors predictive of outcome after use of the Ponseti method for the treatment of idiopathic clubfeet. J Bone Joint Surg [Am] 2004;85-A:22–27. [DOI] [PubMed] [Google Scholar]
- 4.Carroll N. Clubfoot In: Lovell WW, Winter RB, eds.. Lovell and Winter’s Pediatric Orthopaedics. Vol. 2 Philadelphia: Lippincott Williams & Wilkins, 1990. [Google Scholar]
- 5.Brand RA, Siegler S, Pirani S, Morrison WB, Udupa JK.. Cartilage anlagen adapt in response to static deformation. Med Hypotheses 2006;66:653–659. [DOI] [PubMed] [Google Scholar]
- 6.Lis A, de Castro C, Nordin M.. Biomechanics of tendons and ligaments In: Nordin M, Frankel VH, eds.. Basic Biomechanics of the Musculoskeletal System. Fourth ed. Baltimore: Wolters Kluwer/Lippincott Williams & Wilkins, 2012. [Google Scholar]
- 7.Özkaya N, Nordin M, Goldsheyder D, Leger D.. Fundamentals of Biomechanics: Equilibrium, Motion, and Deformation. Third ed. New York: Springer, 2012: 221–236. [Google Scholar]
- 8.Pirani S. Clubfoot scoring. In: Lynn S, ed.. Clubfoot: Ponseti Management. Third ed. Global Help; 2009. www.global-help.org/products/clubfoot_ponseti_management (date last accessed 31October2018). [Google Scholar]
- 9.Diméglio A, Bensahel H, Souchet P, Mazeau P, Bonnet F.. Classification of clubfoot. J Pediatr Orthop B 1995;4:129–136. [DOI] [PubMed] [Google Scholar]
- 10.Giesberts RB, Sluiter VI, Verkerke GJ.. Design and test of a new inductive force sensor. Sensors 2018;18:E2079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Murata H. Rheology - Theory and application to biomaterials. In: De Souza Gomes A, ed.. Polymerization. InTechOpen, 2012:403–426. https://www.intechopen.com/books/polymerization/rheology-theory-and-application-to-biomaterials (date last accessed 21September2018). [Google Scholar]
- 12.No authors listed.. LDC1612, LDC1614 Multi-Channel 28-Bit Inductance to Digital Converter (LDC) for Inductive Sensing (Computer software manual No. SNOSCY9A). December 2014, revised March 2018. Texas Instruments; www.ti.com/lit/ds/symlink/ldc1614.pdf (date last accessed 21September2018). [Google Scholar]
- 13.No authors listed.. DS1825 Programmable Resolution 1-Wire Digital Thermometer With 4-Bit ID. January 2005. Maxim Integrated https://datasheets.maximintegrated.com/en/ds/DS1825.pdf (date last accessed 21September2018).
- 14.Giesberts RB, Hekman EEG, Maathuis PGM, Verkerke GJ.. Quantifying the Ponseti method. J Mech Behav Biomed Mater 2017;66:45–49. [DOI] [PubMed] [Google Scholar]
- 15.Cohen TL, Altiok H, Tarima S, Smith PA, Harris GF.. Creep evaluation of (orthotic) cast materials during simulated clubfoot correction. Conf Proc IEEE Eng Med Biol Soc 2012;2012:3352–3355. [DOI] [PubMed] [Google Scholar]
- 16.Cohen TL, Altiok H, Wang M, et al. Evaluation of cast creep occurring during simulated clubfoot correction. Proc Inst Mech Eng H 2013;227:919–927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mahmoodian R. Mechanics and development of tarsal cartilage anlagen - insights from a human study [PhD Thesis]. Philadelphia: Drexel University, 2010. [Google Scholar]
- 18.Philip P. Volumetric and growth changes induced by serial casting treatment of congenital clubfoot on tarsal bones [MSc Thesis]. Philadelphia: Drexel University, 2014. [Google Scholar]
- 19.Fung YC. Biomechanics: Mechanical Properties of Living Tissues. First ed. Springer-Verlag, 1981. [Google Scholar]
- 20.Flowers KR. A proposed decision hierarchy for splinting the stiff joint, with an emphasis on force application parameters. J Hand Ther 2002;15:158–162. [DOI] [PubMed] [Google Scholar]
- 21.Peacock EE Jr.. Wound Repair. Philadelphia: Saunders, 1984. [Google Scholar]
- 22.Elgohary HS, Abulsaad M.. Traditional and accelerated Ponseti technique: a comparative study. Eur J Orthop Surg Traumatol 2015;25:949–953. [DOI] [PubMed] [Google Scholar]
- 23.Xu RJ. A modified Ponseti method for the treatment of idiopathic clubfoot: a preliminary report. J Pediatr Orthop 2011;31:317–319. [DOI] [PubMed] [Google Scholar]
- 24.Harnett P, Freeman R, Harrison WJ, Brown LC, Beckles V.. An accelerated Ponseti versus the standard Ponseti method: a prospective randomised controlled trial. J Bone Joint Surg [Br] 2011;93-B:404–408. [DOI] [PubMed] [Google Scholar]
- 25.Giesberts RB, van der Steen MC, Maathuis PGM, et al. Influence of cast change interval in the Ponseti method: a systematic review. PLoS One 2018;13: e0199540. [DOI] [PMC free article] [PubMed] [Google Scholar]


