Abstract
Brugada syndrome is an inherited arrhythmia that increases a patient's risk of sudden cardiac death. Certain pharmacologic agents may induce a transient Brugada pattern on surface electrocardiogram (EKG). One of these is loperamide, an over-the-counter agent commonly used to manage diarrhea. We report the case of a patient who experienced EKG changes that mimicked Brugada pattern after excessive intake of loperamide.
Keywords: Brugada, loperamide, arrhythmia
INTRODUCTION
Brugada syndrome is a heart rhythm disorder characterized by electrocardiographic (EKG) and clinical manifestations. Brugada pattern is defined as ST and J point elevation of at least 2 mm in one or more of the right precordial leads. The diagnosis of Brugada syndrome requires the presence of Brugada pattern in addition to syncope, prior cardiac arrest, polymorphic ventricular tachycardia, ventricular fibrillation, and/or family history of sudden cardiac death.1 EKG changes occur spontaneously or after intravenous administration of class I antiarrhythmic drugs.2 These changes are unrelated to ischemia, electrolyte disturbances, or obvious structural heart disease.3 Although rare, certain pharmacologic agents may induce transient Brugada pattern on surface EKG. One of these is loperamide, an over-the-counter agent commonly used to manage diarrhea, that has become an increasingly popular alternative to prescription opiates. We describe a case of loperamide overdose mimicking Brugada pattern.
CASE DESCRIPTION
A 48-year-old Caucasian woman with a history of anxiety and polysubstance abuse presented with syncope, palpitations, and generalized weakness. A review of systems revealed a 2-week history of intermittent diarrhea, for which she used 6 to 8 tablets of loperamide a day. She had no history of prior syncope nor a family history of sudden cardiac death. On examination, her blood pressure was 137/81 mm Hg, heart rate was 68 beats/min, temperature was 90° F, respiratory rate was 17 breaths/min, and SpO2 was 95%. She was oriented but lethargic. Cardiovascular exam revealed regular heart rate and rhythm and no murmurs, rubs, or gallops. Her lungs were clear to auscultation bilaterally, and her abdomen was soft and nontender, with hypoactive bowel sounds. She had no focal neurological deficits. Basic lab work was unremarkable, although urine drug screen was positive for opiates and benzodiazepines. Neurological work-up including electroencephalogram (EEG) and brain magnetic resonance imaging (MRI) were unremarkable. An EKG (Figure 1) mimicked type 1 Brugada pattern on leads V1-V2 and showed right axis deviation (RAD), first-degree atrioventricular block (AVB) with PR interval 339 ms, and right bundle branch block with QRS duration of 270 ms and QTc of 578 ms. Echocardiogram revealed normal left ventricular (LV) function and no significant structural abnormalities. A computed tomography angiogram of the coronary arteries showed no evidence of coronary artery disease. On telemetry monitoring during hospitalization, there was no evidence of ventricular tachycardia or ventricular fibrillation. Notably, her loperamide level was found to be 69 ng/mL (reference range: < 5 ng/mL).
Figure 1.
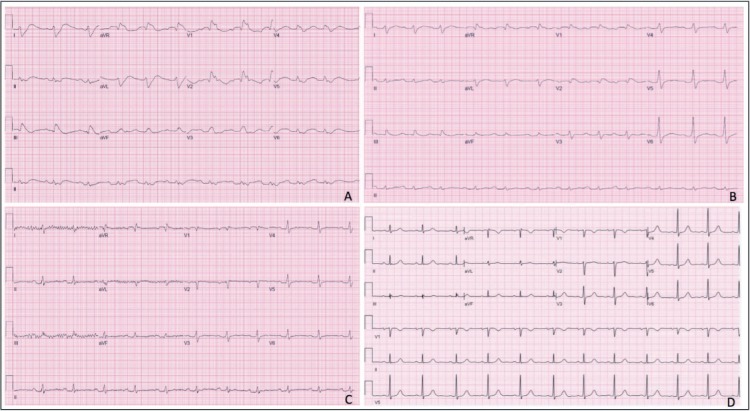
Electrocardiograms (EKGs) at different stages during hospitalization. (A) EKG on admission: mimic of type 1 Brugada pattern on leads V1-V2, RAD, first-degree AVB with PR interval 239 ms, RBBB with QRSd 270 ms, and QTc 578 ms. (B) EKG on day 2 of admission: mimic of type 1 Brugada pattern on leads V1-V2, RAD, first-degree AVB with PR interval 276 ms, RBBB with QRSd 162 ms, and QTc 522 ms. (C) EKG on day 3 of admission: NSR with first-degree AVB with PR 251 ms, QRSd 150 ms, and QTc 458 ms. (D) Baseline EKG from prior admission: NSR, PR 193 ms, QRSd 98 ms, and QTc 458 ms. RAD: right axis deviation; AVB: atrioventricular block; RBBB: right bundle branch block; NSR: normal sinus rhythm
Given the presence of EKG abnormalities that mimicked Brugada pattern in the context of reported syncopal episode, evaluation for sudden cardiac death was considered. However, once her serum loperamide level became available, she was closely monitored, and her electrocardiographic abnormalities resolved within 72 hrs.
DISCUSSION
Drug classes that have been found to induce Brugada pattern include antidepressants, antipsychotics, and antihistamines.4 Loperamide, an over-the-counter μ-opioid receptor agonist used to treat diarrhea, is another medication that on rare occasions may mimic Brugada pattern. Although the efflux by P-glycoprotein should prevent loperamide from effectively crossing the blood-brain barrier (BBB), high-dose consumption allows it to penetrate the BBB and exert its opiate effects in the central nervous system (CNS).5 Its affordability and accessibility have made loperamide a popular alternative for opioid addicts to the point that it is referred to as the “poor man's methadone.”6
The mechanism whereby loperamide appears to exhibit cardiac conduction abnormalities is not well understood. It has been reported to cause QT prolongation and, subsequently, Torsades de Pointes by inhibiting the human ether-a-go-go-related gene responsible for the rapid delayed rectifier potassium current.5 However, prolongation of the QRS segment has also been reported with loperamide overdose.5,7 This has led to the postulation that, at high doses, loperamide may act as class 1A antiarrhythmic given concomitant QT and QRS prolongation.
The threshold of loperamide level that leads to conduction abnormalities is unknown. A literature review reveals a wide range of loperamide levels (32–77 ng/mK) with an equally wide range of presentations, from shortness of breath to cardiac arrest.5 Cessation of loperamide and supportive care may resolve electrocardiographic and clinic manifestations; however, excessive loperamide use in the presence of other comorbidities or without prompt medical attention may lead to death. Loperamide overdose should be considered in the differential diagnosis in all EKGs with abnormalities that mimic Brugada pattern.
CONCLUSION
This case illustrates the rare yet important presentation of Brugada pattern induced by excessive use of loperamide. Given the current opioid epidemic and attempts to restrict the circulation of prescription opiates, excessive use of nonprescription agents such as loperamide may become more prevalent. Hence, it is important that clinicians be able to recognize electrocardiographic and clinical manifestations of such pharmacologic agents.
Footnotes
Conflict of Interest Disclosure: The authors have completed and submitted the Methodist DeBakey Cardiovascular Journal Conflict of Interest Statement and none were reported.
REFERENCES
- 1.Antzelevitch C, Brugada P, Borggrefe M et al. Brugada syndrome: report of the second consensus conference: endorsed by the Heart Rhythm Society and the European Heart Rhythm Association. Circulation. 2005 Feb 8;111(5):659–70. doi: 10.1161/01.CIR.0000152479.54298.51. [DOI] [PubMed] [Google Scholar]
- 2.Writing Committee Members. Shen WK, Sheldon RS et al. 2017 ACC/AHA/HRS guideline for the evaluation and management of patients with syncope. Executive summary: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. Heart Rhythm. 2017 Aug;14(8):e218–e254. doi: 10.1016/j.hrthm.2017.03.005. [DOI] [PubMed] [Google Scholar]
- 3.Yap YG, Behr ER, Camm AJ. Drug-induced Brugada syndrome. Europace. 2009 Aug;11(8):989–94. doi: 10.1093/europace/eup114. [DOI] [PubMed] [Google Scholar]
- 4.Minoura Y, Kobayashi Y, Antzelevitch C. Drug-induced Brugada syndrome. J Arrhythm. 2013 Apr 6;29(2):88–95. [Google Scholar]
- 5.Leung G, Altshuler D, Goldenberg R, Fridman D, Yuriditsky E. Conduction Disturbances and Ventricular Arrhythmias Associated with High-Dose Loperamide. J Clin Toxicol. 2016 Jun 30;6(3):309–13. [Google Scholar]
- 6.Daniulaityte R, Carlson R, Falck R et al. “I just wanted to tell you that loperamide will work”: a web-based study of extra-medical use of loperamide. Drug Alcohol Depend. 2013 Jun 1;130(0):241–4. doi: 10.1016/j.drugalcdep.2012.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Marraffa JM, Holland MG, Sullivan RW et al. Cardiac conduction disturbance after loperamide abuse. Clin Toxicol (Phila) 2014 Nov;52(9):952–7. doi: 10.3109/15563650.2014.969371. [DOI] [PubMed] [Google Scholar]


