Abstract
Purpose
Failure to obtain an accurate medication history can adversely affect patient care in the emergency department (ED) and propagate errors into the inpatient and outpatient settings. Obtaining an accurate medication history in the ED is challenging, however, due to limited time, a suboptimal environment for patient interaction, and inadequate information in the electronic health record (EHR). This article describes the development and initial evaluation of the PictureRx Medication History Application, a tablet computer-based program that queries patients’ prescription fill data from the Surescripts Medication History service and renders it graphically for review and editing at the point of care.
Methods
A quasi-experimental trial of PictureRx was performed in a large academic ED. Adult patients taking at least 1 prescription medication were prospectively eligible for the intervention. Usual care control patients were retrospectively matched 1:1. The main outcomes were updates to the patients’ existing pre-visit medication list in the EHR and patient perceptions of the application.
Results
The medication list was updated for 101/244 (41.4%) of the intervention group and for 43/244 (17.6%) of the control group (difference 23.8%, 95% confidence interval, 16.0–31.6%). Similar differences were observed for medication additions, removals, and corrections in dose. Approximately 80% of intervention patients “strongly agreed” that the application was easy to use, aided medication list accuracy, and the graphical features assisted with recall.
Conclusion
A novel tablet computer-based medication history application was feasible to implement in a busy academic ED. Use of the tool was associated with more updates to patients’ EHR medication list.
Keywords: emergency department, health information technology, medication reconciliation, patient-centered design
KEY POINTS
Use of the PictureRx Medication History application increased the likelihood that a patient’s medication list was updated in the emergency department (ED).
The majority of patients in the intervention group (80%) reported that the tablet application was easy to use.
Use of the PictureRx medication history application may help ED staff to obtain accurate medication histories efficiently.
Incomplete or inaccurate medication histories are of particular concern in emergency departments (EDs),1 where patients commonly have poor knowledge of their medications, exacerbated by low health literacy.2-4 Underserved populations, who are more likely to seek care in EDs,5 and who more often have difficulty providing a complete medication history,2,4 are disproportionately affected. The rapid pace of providing care in EDs is not well suited to obtaining an accurate history,6,7 which can be a time-consuming process. Moreover, the availability of existing medication lists in the electronic health record (EHR) may obviate the perceived need to obtain an accurate and up-to-date medication history. The quality of the medication history obtained in the ED is often poor, reportedly containing errors in 37–87% of cases.8-10 Errors in the initial medication list increase the risk of harmful adverse drug events in the ED and can be propagated downstream as patients return home or are admitted to the hospital.11
There are a number of models for obtaining a medication history in the ED. Commonly, a nurse or other health care professional reviews medications previously documented in the patient’s EHR and briefly discusses current usage with patients. Increasingly, pharmacy technicians or pharmacists are involved in obtaining a more detailed medication history.12 Health information technology provides an opportunity to facilitate either model. Data on the prescriptions that patients fill are available from aggregation services. The Surescripts Medication History service (Surescripts, Arlington, VA), for example, covers more than 90% of U.S. pharmacies and provides access to the medication histories of approximately 220 million patients.13 Some hospitals have contracted to receive a prescription data feed, but the data are provided in a raw format containing unstructured text strings, abbreviations, and duplications. Few examples exist of effectively incorporating these data at the point of care to enhance the process of obtaining a complete and accurate medication history.14-16
We developed a tablet computer-based platform that can be used at the point of care in EDs to query patients’ recent prescription fill data in real time, clean and process the information, and display it for review and editing through a graphical user interface. Here we describe the development and initial assessment of whether use of the application resulted in more frequent updating of the medication history in the EHR than the usual process of obtaining a medication history.
Methods
Intervention development.
The PictureRx Medication History Application was designed in partnership with Bioscape Digital (Atlanta, GA),a technology company that develops healthcare-related applications for tablet computers. The application was based on the illustrated daily medication schedules, icons to illustrate drug indication, and patient-centered medication labels previously developed for use in PictureRx cloud-based software.17-21 Development was funded by a Small Business Innovation Research (SBIR) phase II award from the National Institutes of Health/National Institute on Minority Health and Health Disparities (NIH/NIHMD).
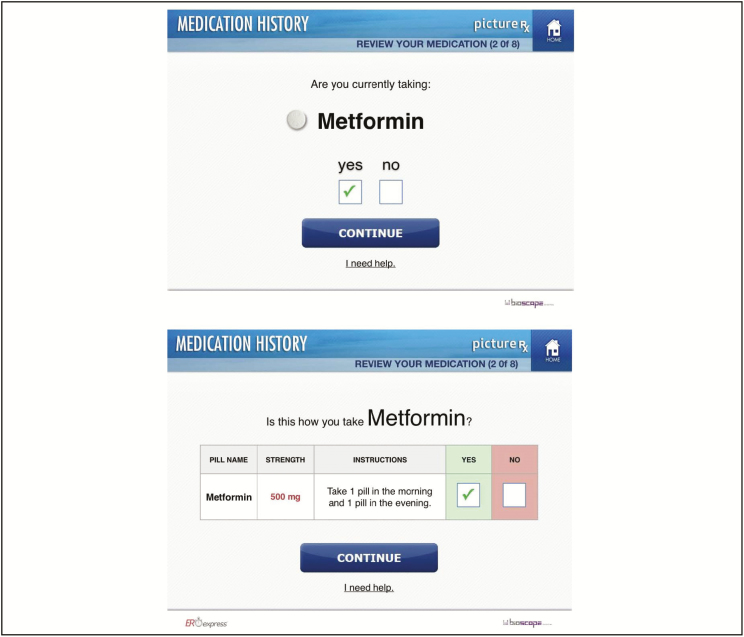
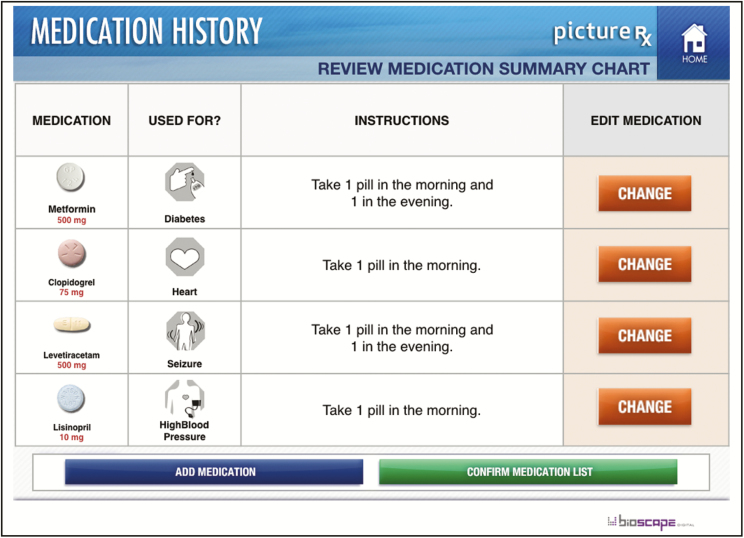
The PictureRx application allows a user to query the national prescription fill data available through Surescripts in order to generate a list of the prescriptions filled by a patient. The application then processes the raw data using automated rules to remove duplicate entries, parse drug information (e.g., time of administration) into discrete fields, and convert common abbreviations (e.g., BID, q6hrs) into plain English language. It presents the information in a graphical format on a tablet computer for review and editing (Figure 1). The user (either a patient or health care professional) can make corrections, fill in gaps (e.g., medication name and strength are present but SIG is missing), delete medications, and add new medications. If no valid data are returned by the query, the application allows the user to enter data to construct a medication list. The application accommodates generic or brand name. Throughout the process, the application shows pictures of the medications from a comprehensive image library, as well as icons depicting common uses for each medication. Once the user has completed the medication history process, the final data are summarized for review (Figure 2). All data are fully encrypted, and the application is equipped with authorization capabilities that prevent unauthorized users from engaging with protected health data and limits final verification of the medication history to an appropriate health care professional. The application was reviewed and certified by the prescription aggregation service’s quality control personnel.
Figure 1.
Examples of graphical interface for medication review in the PictureRx Medication History Application.
Copyright © 2018, Bioscape Digital.
Figure 2.
Review of medication regimen in PictureRx Medication History Application.
Copyright © 2018, Bioscape Digital.
The development team used an iterative process to create the application. There were 5 cycles of iterative development incorporating feedback from team members with expertise in medication reconciliation and software development. Formal user testing was also performed with 26 people, including nurses, pharmacists, and patients. Users were able to initiate a medication query in about 35 to 45 seconds, and the time for medication review ranged from 5 to 7 minutes. Testers gave very favorable ratings to the application’s usability and several changes were incorporated into the application design as a result of user testing. Specifically, 2 views were developed, for patients and health care professionals, respectively, and capabilities were added to allow the user to indicate that a medication was not being taken as directed or was prescribed but not being taken at all. In such situations, the medication was retained in the summary list rather than removing it so that the health care professional could inquire further with the patient. The development, user testing, and modifications were completed prior to beginning the present study.
Study design.
The study was designed as a quasi-experimental trial with pragmatic features that facilitated patient participation and minimized burden on patients and the ED. We prospectively enrolled a cohort of patients for intervention with the application and then used the EHR to retrospectively match a cohort of similar control patients for comparison. We also used the EHR to extract data for outcome assessment. In addition, a subset of the intervention group was surveyed for their opinions about the application. The study was approved by the local institutional review board. A waiver of informed consent was granted for the control group.
Subjects and setting.
The study was performed in the ED of a 665-bed urban, tertiary care, academic hospital that serves as the region’s only level 1 trauma center and safety net. The ED sees more than 70 000 adult patients annually. During the period of this study, which spanned May 5, 2015, through November 30, 2015, about 20% of patients were commercially insured, 15% uninsured, and 65% on Medicare or Medicaid. About 51% were female and about 54% were African American. Pediatric patients were rarely seen at the facility as a dedicated pediatric ED is located nearby, and 16% of patients were age 60 years or older. The Medical Center uses the Epic EHR system (Epic, Verona, WI) which links data across ED, outpatient, and inpatient visits. Each patient’s medication list is stored in structured form in the EHR system. For patients in the ED, usual care is for nurses to review and update this medication list in the EHR as part of the intake process.
Patients were eligible for recruitment into the intervention group if they were located in one of the intervention rooms with a tablet device, able to communicate in English, at least 18 years of age, and reported taking at least one prescription medication. Patients who were too ill or otherwise unable to complete informed consent were excluded. Control group patients were identified retrospectively from the EHR from the pool of patients who received care in the ED during the enrollment period but were not exposed to the intervention; they were matched 1:1 to the intervention group. Patient encounters were eligible as controls if they had an Emergency Severity Index (ESI)22 score of 2 to 5 and completed the intake process. Matching was based on where in the ED the patient was seen, the intake nurse, and ESI. Optimal matching was achieved by requiring exact matching on location and nurse, and by allowing ESI score to vary by 1. Three cases were unable to be matched.
Intervention.
We tethered tablet devices with the PictureRx application installed in certain regular exam rooms in the ED, which were designated as intervention rooms. Other rooms did not have tablet devices. Patients were assigned to rooms through the usual process of bed allocation in the ED. This effectively assigned a random group of patients to intervention rooms where they could be recruited into the study during the period of enrollment. Research staff also had the ability to enroll patients using a mobile tablet device, which was done on a limited basis after having approached all patients in intervention rooms. This tablet device functioned in the same manner as those tethered in intervention rooms.
Research staff interacted directly with patients eligible for the intervention to recruit them into the study and obtain informed consent and Health Insurance Portability and Accountability Act (HIPAA) authorization. Subsequently, research staff initiated the medication query through the application to find the medications that a patient had filled at participating pharmacies. The data were processed and presented to the patient using the PictureRx application. Medications were reviewed one at a time through a series of screens where participants were asked to confirm whether or not they were taking the medication, the dose, the indication, and dosing instructions (e.g., time of day). They were also prompted to enter any additional medications not on the list generated from the medication history service query. Patients used the application directly; they were allowed to receive assistance from family or research staff if needed (just as patients would be able to receive help from nurses or pharmacy staff if such a tool were used in clinical practice). Research staff estimated the amount of assistance required to use the tablet platform and also collected data on patients’ educational attainment and health literacy using a short 3-item screening instrument.23 Upon completion, the research staff provided the resulting medication list to the treating nurse. For this trial, the PictureRx medication list was not directly integrated with the EHR.
Patients enrolled in the intervention group were invited to participate in a telephone survey to gauge their perceptions of the application. Approximately 75 consecutive patients were invited until 50 surveys were completed. Questions included satisfaction with care, the medication history process, and the tablet application, as well as their understanding of their medication regimen (Table 3). Study data were collected and managed using REDCap (Research Electronic Data Capture).24
Table 3.
Patient Satisfaction With Care and Tablet-based Medication History Application (n = 50)
| Number (%) Patients Providing Response | |||||
|---|---|---|---|---|---|
| Survey Question | Very Satisfied | Satisfied | Neutral | Dissatisfied | Very Dissatisfied |
| Overall, how satisfied are you with your care in the Emergency Department? | 29 (58) | 10 (20) | 5 (10) | 3 (6) | 3 (6) |
| How satisfied are you with the process that was used to go over the medicines you were taking? | 38 (76) | 11 (22) | 1 (2) | 0 (0) | 0 (0) |
| Strongly Agree | Agree | Neutral | Disagree | Strongly Disagree | |
| The tablet computer program that was used to go over my medicines was easy to use. | 42 (84) | 5 (10) | 2 (4) | 1 (2) | 0 (0) |
| The graphics and other prompts helped me remember my medicines. | 39 (78) | 6 (12) | 5 (10) | 0 (0) | 0 (0) |
| The computer program helped me provide a more accurate list of my medicines. | 39 (78) | 8 (16) | 3 (6) | 0 (0) | 0 (0) |
| I would like to see computer programs like this used when I come to the hospital. | 40 (80) | 9 (18) | 1 (2) | 0 (0) | 0 (0) |
| I understand what medicines I am supposed to take. | 46 (92) | 3 (6) | 1 (2) | 0 (0) | 0 (0) |
| I understand how much medicine I am supposed to take at a time. | 47 (94) | 2 (4) | 1 (2) | 0 (0) | 0 (0) |
| I understand what time of day to take each of my medicines. | 46 (92) | 4 (8) | 0 (0) | 0 (0) | 0 (0) |
| I understand what each of my medicines is for. | 45 (90) | 4 (8) | 1 (2) | 0 (0) | 0 (0) |
Outcomes.
In both the control and intervention groups, the patient’s nurse was responsible for reviewing the patient’s active medications and updating this information in the EHR. The nurse had access to usual sources of medication information, including what may have been documented previously in the EHR, as well as what the nurse obtained directly from patients, families, or emergency medical technicians. Prescription fill data were not available, unless the nurse called the patient’s pharmacy to obtain this information, which was not the general practice. In the intervention group, the nurse also had access to the medication list generated using the PictureRx Medication History Application. The utility of the PictureRx application in this context can be determined by the extent to which it provided information beyond what the nurse would normally obtain and document.15 The primary outcome was thus defined as whether or not changes were made to the patient’s medication list in the EHR, by comparing the pre-visit medication list available in the EHR to the medication list after completion of the nurse intake process. Secondary outcomes included the type and number of changes made to the medication list (i.e., addition or removal of a medication, or change in dosing instructions). Research staff also recorded the approximate level of assistance needed to use the device: none (0%), some (25%), moderate (50%), substantial (75%), or full (100%).
Statistical analysis.
Patient characteristics were summarized for the intervention and control groups using descriptive statistics. The percentage of patients who had changes made to their medication list was calculated and the difference between intervention and control groups computed with 95% confidence intervals (CI95). The number and type of medication list updates were computed and the difference between groups calculated. The level of assistance required to use the tablet platform was summarized overall and by level of age, education, and health literacy. Data management and statistical analyses were performed solely by one researcher (KH), who had complete access to and control of the data and has no financial interest in PictureRx, Bioscape Digital, LLC, or SAI Interactive, Inc. All statistical analyses were conducted using SPSS 23.0 (IBM Corporation, Armonk, NY).
Results
A total of 250 unique patients were enrolled in the intervention group. Of these, 6 patients were excluded for either lack of complete intake data (n = 3) or difficulty matching to suitable controls (n = 3). Table 1 provides the characteristics of the intervention and control patients included in the analysis. Overall, participants had a mean ± S.D. age of 41 ± 15 years, 51% were female, and 61% were black.
Table 1.
Patient Characteristics
| Variable | Intervention Group (n = 244) | Control Group (n = 244) | Overall (n = 488) | Surveyed Group (n = 50) |
|---|---|---|---|---|
| Age, mean (S.D.), years | 41 (13) | 41 (16) | 41 (15) | 43 (14) |
| Race/ethnicity, no. (%) | ||||
| Black | 144 (59.0) | 151 (61.9) | 295 (60.5) | 36 (72.0) |
| White | 95 (38.9) | 71 (29.1) | 166 (34.0) | 14 (28.0) |
| Hispanic | 1 (0.4) | 13 (5.3) | 14 (2.9) | 0 (0.0) |
| Asian | 0 (0.0) | 1 (0.4) | 1 (0.2) | 0 (0.0) |
| American Indian or Alaskan Native | 1 (0.4) | 0 (0.0) | 1 (0.2) | 0 (0.0) |
| Other | 3 (1.2) | 8 (3.3) | 11 (2.3) | 0 (0.0) |
| Sex, female, no. (%) | 136 (55.7) | 113 (46.3) | 249 (51.0) | 28 (56.0) |
| Education, less than high school graduation, no. (%) | 56 (23.0) | . . .a | . . . | 12 (24.0) |
| Low health literacy, no. (%) | 47 (19.3) | . . . | . . . | 7 (14.0) |
| Medication list already in EHR, no. (%) | 201 (82.4) | . . . | . . . | 37 (74.0) |
| Emergency Severity Index, no. (%) | ||||
| 2 | 32 (13.1) | 32 (13.1) | 64 (13.1) | 8 (16.0) |
| 3 | 102 (41.8) | 102 (41.8) | 204 (41.8) | 21 (42.0) |
| 4 | 96 (39.3) | 97 (39.8) | 193 (39.5) | 18 (36.0) |
| 5 | 14 (5.7) | 13 (5.3) | 27 (5.5) | 3 (6.0) |
aData not available.
Patients in the intervention group had changes made to their medication list in the EHR in 41.4% of cases, compared with 17.6% in the control group (difference in proportions 23.8%, CI95, 16.0–31.6%) (Table 2). All types of medication list updates were more common in the intervention group, including medications being added to the list, doses or instructions being corrected, or discontinuations being noted.
Table 2.
Frequency of Changes to the Medication List in Intervention and Control Groups
| Number (%) Changes | |||
|---|---|---|---|
| Variable | Intervention Group (n = 244) | Control Group (n = 244) | % Difference (95% Confidence Interval) |
| Any change in medication list | 101 (41.4) | 43 (17.6) | 23.8 (16.0 –31.6) |
| Type of medication list changea | |||
| Medication added | 96 (39.3) | 43 (17.6) | 21.7 (13.9–29.5) |
| Medication dose, route, frequency, or instructions changed | 87 (35.7) | 40 (16.4) | 19.3 (11.7–26.9) |
| Medication removed | 84 (34.4) | 40 (16.4) | 18.0 (10.5–25.6) |
aChanges add up to greater than 100% because it was possible to have more than one type of change.
Half of the patients in the intervention group required little to no assistance to review their medication regimen; the remainder required at least moderate assistance. Patients who had more medications in their medication history required a greater level of assistance to review their regimen, as did older patients. Patients’ level of education and health literacy did not appear to be associated with a need for assistance with the device.
The characteristics of the 50 patients included in the survey were similar to those of the overall group (Table 1). The majority of patients (58%) were “very satisfied” with the care overall, and 76% reported being “very satisfied” with the process used to review their medications (Table 3). The majority of patients “strongly agreed” that the medication history application was easy to use (84%), that the features assisted with recall and creation of an accurate medication list (78%), and that they would like to see such programs used in the future (80%). Post intervention, the majority also “strongly agreed” that they understood what medications they were supposed to take (92%), how much to take at a time (94%), what time of day to take each medication (92%), and the purpose of each medication (90%).
Discussion
A point-of-care tablet computer-based medication history application appeared to be an effective tool for updating patients’ medication lists in the ED. The application successfully queried patients’ prescription fill data through a national database and displayed the processed information through a graphical user interface for review and verification. Medication lists were updated more than twice as frequently among patients participating in the intervention, compared to matched controls. To the best of our knowledge, this study is the first evaluation of patient-facing technology to improve medication reconciliation in the ED.
For this initial assessment of the application’s utility, we chose a pragmatic primary outcome, namely whether changes were made to the medication list in the EHR. This outcome assumes that such changes reflect corrections and updates to the medication list and therefore indicate improved medication reconciliation. The approach of using the EHR to extract and calculate the number of medication list changes proved feasible and could be considered for future medication safety studies, which have traditionally relied on taking a gold-standard medication history and manually comparing the medication list to it.16 We did not classify the clinical relevance of changes to the medication list. Previous research has demonstrated that approximately 20% of such changes are clinically relevant.25
The quality of electronic medication lists is of critical importance given the widespread reliance on EHRs. Clinicians and patients often assume that EHR medication lists are fairly accurate, but research shows this is not the case. Errors have been identified in up to 78% of cases.25 Stockton and colleagues studied electronically pre-populated medication reconciliation forms and found that 47% of ED patients had errors in their medication list; 21% of which were deemed clinically significant.10 Leaving inaccurate data in the EHR propagates errors downstream and increases the risk of an adverse drug event.26 This risk makes it all the more important to have an efficient process in place to review and verify medication lists, particularly in the ED where obtaining a medication history is fraught with challenges.
Engaging patients in the process of medication review has the potential to improve medication list accuracy,6 while also reinforcing patient understanding of the regimen and enhancing satisfaction. Few examples of patient-facing technologies are available in the literature.27,28 Lesselroth and colleagues28 described an ambulatory check-in kiosk where patients could review their medication list prior to the appointment. Use of the kiosk detected 4–5 medication discrepancies per patient, saved nursing staff time, and was generally well-accepted by clinicians.29,30 Heyworth and colleagues piloted a tool in a web-based patient portal to the EHR to identify discrepancies after hospital discharge, which was well-received by patients.27 Based on our experience, it is feasible to engage patients in the ED in reviewing and updating their medication list. Approximately half were able to do this fairly independently, and half required assistance, particularly if they were elderly or took many medications. Offering and providing assistance would be an important aspect of deploying such technology in clinical practice. Alternatively, the technology could be used by pharmacists or other health care professionals to facilitate interviewing the patient about current medication use.
There were several limitations to the study. This quasi-experimental study was designed as an initial test of a new technology, with certain features that enhanced its feasibility and efficiency but which may have also affected its rigor in comparison to a randomized controlled trial. Matching was used to minimize bias between groups, but it is possible they differed in other characteristics, leading to residual confounding. For example, because we did not interact directly with patients in the control group, we could not measure their health literacy level. We were also unable to match by baseline number of medications. While to be eligible, intervention patients must have reported being prescribed at least one medication at baseline prior to the ED visit, there was not a way to ask whether control patients also self-reported being prescribed at least one medication at baseline. Finally, in this initial evaluation, we excluded patients who did not speak English because the computer application was available in English only. Additional work is needed to examine and improve medication safety among patients with limited English proficiency.
Conclusion
A novel tablet computer-based medication history application was feasible to implement in a busy academic ED. Use of the tool was associated with more updates to patients’ EHR medication list.
Acknowledgments
We thank Ian Jansen, Henrietta Ofori-Sampong, Krista Swegheimer, and Aubry Colosimo for their assistance with patient enrollment and intervention delivery.
Disclosures
This research was supported by the National Institute on Minority Health and Health Disparities of the National Institutes of Health under Award Number R44MD004048, and in part by an institutional Clinical and Translational Science Award, NIH/NCRR Grant Number 8UL1-TR000077. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Conflicts of interest: Sunil Kripalani, Stuart Bracken, Christopher Lindsell, and Dane R. Boyington have equity in Bioscape Digital.
References
- 1. Institute of Medicine. Preventing medication errors. Washington, DC: National Academies Press; 2007. [Google Scholar]
- 2. Kripalani S, Henderson LE, Chiu EY et al. Predictors of medication self-management skill in a low-literacy population. J Gen Intern Med. 2006; 21:852–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kripalani S, Henderson LE, Jacobson TA, Vaccarino V. Medication use among inner-city patients after hospital discharge: patient-reported barriers and solutions. Mayo Clin Proc. 2008; 83:529–35. [DOI] [PubMed] [Google Scholar]
- 4. Marvanova M, Roumie CL, Eden SK et al. Health literacy and medication understanding among hospitalized adults. J Hosp Med. 2011; 6:488–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Reasons for emergency room use among U.S. adults aged 18–64: National Health Interview Survey, 2013 and 2014. Hyattsville, MD: National Center for Health Statistics; 2016. National health statistics reports; no. 90. [PubMed] [Google Scholar]
- 6. Hummel J, Evans PC, Lee H. Medication reconciliation in the emergency department: opportunities for workflow redesign. Qual Saf Health Care. 2010; 19:531–5. [DOI] [PubMed] [Google Scholar]
- 7. Kulstad EB, Sikka R, Sweis RT et al. ED overcrowding is associated with an increased frequency of medication errors. Am J Emerg Med. 2010; 28:304–9. [DOI] [PubMed] [Google Scholar]
- 8. Mazer M, Deroos F, Hollander JE et al. Medication history taking in emergency department triage is inaccurate and incomplete. Acad Emerg Med. 2011; 18:102–4. [DOI] [PubMed] [Google Scholar]
- 9. Caglar S, Henneman PL, Blank FS et al. Emergency department medication lists are not accurate. J Emerg Med. 2011; 40:613–6. [DOI] [PubMed] [Google Scholar]
- 10. Stockton KR, Wickham ME, Lai S et al. Incidence of clinically relevant medication errors in the era of electronically prepopulated medication reconciliation forms: a retrospective chart review. CMAJ Open. 2017; 5:E345–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Salanitro AH, Osborn CY, Schnipper JL et al. Effect of patient- and medication-related factors on inpatient medication reconciliation errors. J Gen Intern Med. 2012; 27:924–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Pevnick JM, Nguyen C, Jackevicius CA et al. Improving admission medication reconciliation with pharmacists or pharmacy technicians in the emergency department: a randomised controlled trial. BMJ Qual Saf. 2018; 7: 512–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Surescripts Medication history. http://surescripts.com/products-and-services/medication-history-for-reconciliation (accessed 2018 Dec 19).
- 14. Frisse ME, Tang L, Belsito A, Overhage JM. Development and use of a medication history service associated with a health information exchange: architecture and preliminary findings. AMIA Annu Symp Proc. 2010; 2010:242–5. [PMC free article] [PubMed] [Google Scholar]
- 15. Fung KW, Kayaalp M, Callaghan F, McDonald CJ. Comparison of electronic pharmacy prescription records with manually collected medication histories in an emergency department. Ann Emerg Med. 2013; 62:205–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Mueller SK, Sponsler KC, Kripalani S, Schnipper JL. Hospital-based medication reconciliation practices: a systematic review. Arch Intern Med. 2012; 172:1057–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Martin D, Kripalani S, Durapau VJ Jr. Improving medication management among at-risk older adults. J Gerontol Nurs. 2012; 38:24–34; quiz 36–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Mohan A, Riley B, Schmotzer B et al. Improving medication understanding among Latinos through illustrated medication lists. Am J Manag Care. 2014; 20:e547–55. [PubMed] [Google Scholar]
- 19. Mohan A, Riley MB, Boyington D et al. Development of a patient-centered bilingual prescription drug label. J Health Commun. 2013; 18(suppl 1):49–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Mohan A, Riley MB, Boyington D, Kripalani S. Picturerx: illustrated medication instructions for patients with limited health literacy. J Am Pharm Assoc (2003). 2012; 52:e122–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Mohan AV, Riley MB, Boyington DR, Kripalani S. Illustrated medication instructions as a strategy to improve medication management among Latinos: a qualitative analysis. J Health Psychol. 2013; 18:187–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Tanabe P, Travers D, Gilboy N et al. Refining emergency severity index triage criteria. Acad Emerg Med. 2005; 12:497–501. [DOI] [PubMed] [Google Scholar]
- 23. Chew LD, Griffin JM, Partin MR et al. Validation of screening questions for limited health literacy in a large VA outpatient population. J Gen Intern Med. 2008; 23:561–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Harris PA, Taylor R, Thielke R et al. Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009; 42:377–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Monte AA, Anderson P, Hoppe JA et al. Accuracy of electronic medical record medication reconciliation in emergency department patients. J Emerg Med. 2015; 49:78–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Limpahan LP, Baier RR, Gravenstein S et al. Closing the loop: best practices for cross-setting communication at ED discharge. Am J Emerg Med. 2013; 31:1297–1301. [DOI] [PubMed] [Google Scholar]
- 27. Heyworth L, Paquin AM, Clark J et al. Engaging patients in medication reconciliation via a patient portal following hospital discharge. J Am Med Inform Assoc. 2014; 21:e157–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Lesselroth BJ, Felder RS, Adams SM et al. Design and implementation of a medication reconciliation kiosk: the automated patient history intake device (APHID). J Am Med Inform Assoc. 2009; 16:300–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Lesselroth B, Adams S, Felder R et al. Using consumer-based kiosk technology to improve and standardize medication reconciliation in a specialty care setting. Jt Comm J Qual Patient Saf. 2009; 35:264–70. [DOI] [PubMed] [Google Scholar]
- 30. Lesselroth BJ, Holahan PJ, Adams K et al. Primary care provider perceptions and use of a novel medication reconciliation technology. Inform Prim Care. 2011; 19:105–18. [DOI] [PubMed] [Google Scholar]