Abstract
Study Objectives
High school start times (SSTs) directly impact adolescents’ sleep timing and duration. This study investigated the associations between SSTs and actigraphically-measured 24-hour sleep duration, sleep onset, sleep offset and sleep quality.
Methods
This study included 383 adolescents (Mage = 15.5, SDage = 0.6 years) participating in the age 15 wave of the Fragile Families & Child Wellbeing Study, a national birth cohort study sampling from 20 large US cities. Multilevel models used daily observations (N = 1116 school days, Mdays = 2.9, SDdays = 1.4 per adolescent) of sleep and SSTs from concordant daily diary and actigraphy.
Results
A diverse range of SSTs were included in our analyses (MSST = 08:08, SDSST = 39 minutes, RangeSST = 06:00–11:05), and are presented in the following categories for ease of interpretation: before 07:30, 07:30–07:59, 08:00–08:29, and 08:30 or later. Adolescents starting school at 08:30 or later exhibited significantly longer actigraphically-assessed 24-hour sleep duration (by 21–34 minutes, p < .05) and later sleep offset (by 32–64 minutes, p < .001) when compared with the adolescents grouped by earlier SSTs. SSTs were also analyzed continuously for comparison with existing literature, and results indicated that every 1-hour delay in SST was significantly associated with 21 minutes longer 24-hour sleep duration (p < .001), 16 minutes later sleep onset (p < .01), and 39 minutes later sleep offset (p < .001). All models controlled for covariates including socioeconomic status.
Conclusion
These findings support pediatric and public health expert recommendations for SSTs after 08:30. In our diverse national urban sample, adolescents with SSTs at 08:30 or later, compared with adolescents with earlier SSTs, had significantly longer actigraphy-measured sleep.
Keywords: school start times, actigraphy, adolescence, sleep duration, sleep timing, education policy, pediatric sleep, sleep quality
Statement of Significance
Early high school start times (SSTs) require early wake times and can lead to insufficient sleep during adolescence. This study is among the first to measure high school students’ sleep objectively, using actigraphy to investigate the associations between SSTs and sleep timing, duration, and quality. High school students in this study represent a national sample of urban adolescents, with diverse sociodemographic characteristics and SSTs. We found that SSTs at 08:30 or later, compared to start times before 07:30, from 07:30 to 07:59, and from 08:00 to 08:29, were associated with later sleep offset by 32, 44, and 64 minutes, respectively, and longer 24-hour sleep duration by 21, 23, and 34 minutes, respectively.
Introduction
Sufficient sleep is important for physical and mental health during adolescence. However, studies estimate that between 66% and 92% of adolescents are not getting the recommended 8–10 hours of nighttime sleep [1–5]. Insufficient sleep during adolescence has been linked to numerous adverse academic, safety, mental health, and physical health outcomes, including increased tardiness [6], greater need for disciplinary actions [6], poor performance at school [6, 7], higher rates of motor vehicle incidents [8–11], risky behavior [7], depressive and anxious symptoms [12, 13], and obesity [14, 15].
The prevalence of insufficient sleep during adolescence is increasing, potentially due to heightened academic pressures and increased use of the internet and social media [16, 17]. Nighttime sleep duration typically decreases across childhood and adolescence, but data from a nationally representative sample of adolescents from 1991 to 2012 suggest an even steeper decline in adolescent sleep duration trending over the past two decades [18]. Healthy People 2020 acknowledged this worsening trend by establishing an objective to “increase the proportion of students in grades 9 through 12 who get sufficient sleep” [19], highlighting the importance of investigating potential mechanisms to increase sleep across societal and community factors, such as high school start times (SSTs).
During puberty, adolescents experience a circadian-driven delay in melatonin secretion that delays the timing of their sleep cycles [20–24]. The misalignment between early SSTs and this delayed circadian timing contributes to insufficient sleep in adolescence [21, 25, 26]. To address this issue, medical organizations and health advocacy groups, including the American Academy of Pediatrics [12], the American Medical Association [27], the American Academy of Sleep Medicine [28, 29], and the Society of Behavioral Medicine [30] recommend that high schools begin at 08:30 or later. Studies have shown that delays in SSTs can lengthen self-reported sleep duration [31, 32], improve mood [31, 32], increase attendance and graduation rates [32–35] and decrease both daytime sleepiness [31, 32, 35], and caffeine consumption [31]. Decreases in tardiness rates and the need for disciplinary action have been identified as sustainable benefits of a 45-minute SST delay in a New York high school, however, the 20-minute sleep duration extension following the delay was diminished by the 1-year follow-up [6] in contrast to longitudinal studies that show persistent sleep extension benefits several months after an SST delay [35, 36].
Associations between later SSTs and longer sleep duration have been observed in both longitudinal [31, 32, 37–39] and cross-sectional studies [8, 35, 40–44]; however, few studies [45] have used objective measures of sleep and many focus on one school, one school district, or one county. The current study expands upon existing literature by using multiple observations of actigraphic sleep, objectively assessing sleep quality, and incorporating a wide range of SSTs from a national sample of urban adolescents. Our recent study using daily diaries from a subsample of adolescents in the same cohort [40] found that later SSTs were associated with significantly longer self-reported nightly time in bed and later wake times; for bedtimes, only very early SSTs (i.e. earlier than 07:30) were associated with earlier bedtimes, presumably due to adolescents’ circadian drive to go to bed later in general. Based on this finding and recent literature [31, 34, 46], we expected that SSTs would predict actigraphically-derived measures of sleep. We tested two specific hypotheses: Hypothesis (1) Later SSTs are associated with longer 24-hour sleep duration; Hypothesis (2) Later SSTs are associated with later sleep offset (but not necessarily with sleep onset). Additionally, we used the actigraphic sleep data as an opportunity to investigate associations between sleep quality and SSTs.
Methods
Data
The data for this study come from the larger Fragile Families and Child Wellbeing Study (FFCWS) (www.fragilefamilies.princeton.edu), a longitudinal cohort study of families from 20 large US cities. The FFCWS recruited pregnant women in hospitals between 1998–2000, oversampling non-marital births, resulting in a higher proportion of families with low socioeconomic status and a higher proportion of racial/ethnic minorities. Mothers were interviewed within 2 days of the focal youth’s birth, and follow-up interviews were conducted in waves when the cohort reached ages 1, 3, 5, 9, and 15.
Procedure
At the age 15 wave of the FFCWS, separate interviews were conducted with the primary caregiver and the focal youth (N = 3055), now adolescents. Field interviewers collected information including grade in school, household income, caregiver education, school type, living arrangement, and race. Child sex was collected at the first interview following birth. A randomly selected subsample (n = 1090) of the wave 15 adolescent participants were asked to complete a web-based daily diary every evening and wear a wrist-worn accelerometer (Philips-Respironics, Murrysville, PA), concurrently, for about 1 week. The daily diary was used to determine which days the adolescent went to school and what time his/her school started on those days. Only school days, defined as weekdays when the adolescent reported attending school, were used in these analyses. The wrist-worn accelerometers were used to collect sleep onset, sleep offset, 24-hour sleep duration, wake after sleep onset (WASO), and sleep maintenance efficiency. Most participants (57%) wore the accelerometer and completed the daily diary on 3 or more school days (M = 2.9 ± 1.4 days, Range = 1–6 days). Data collection occurred year round, with 22% of observations occurring between December through February, 39% between March through May, 10% between June through August, and 28% between September through November, reflective of the school-day inclusion criteria.
Sleep intervals were initially set in the actigraphy recording using a validated SAS-based (version 9.4 SAS Institute, 2008) algorithm [47], followed by independent double-scorer review and corrections as needed. A third scorer adjudicated any discrepancies greater than 15 minutes per sleep interval between the two scorers. No sleep intervals were set on invalid days, defined by off-wrist detection indicating ≥4 hours of non-wear, non-wear time exceeding 1 hour within 10 minutes of sleep onset or offset, or evidence of device failure.
Participants
Out of 1049 assenting adolescents, 823 adolescents wore the accelerometer for at least 1 school day and completed at least 1 entry in the daily diary. Adolescents were excluded from the analytic sample if they (1) were in middle school or did not report grade (n = 122), (2) reported no school days (n = 238), (3) failed to report SST (n = 25), (4) had no overlap between days of accelerometer wear and daily diary completion (n = 23), (5) were missing covariate data (n = 2), (6) reported time zones in the daily diary discordant from accelerometer time zone (n = 9), (7) had insufficient duration of wear (≤20 hours) deeming actigraphy data invalid (n = 7), (8) woke up later than their daily reported SST (n = 7), and (9) were in summer school, which we defined as adolescents who went to school in June, July, or August and had SSTs later than 09:30 (n = 3). The final analytic sample included 383 adolescents with 1116 school-day observations.
Measures
Predictor (daily diary)
School start time
The daily diary asked adolescents “Did you go to school?” and (if yes), “What time did your school day begin?” (hour, minute, am/pm). To account for variation between days within a participant, SST was defined as the mode of SSTs. Ninety percent of adolescents reported the same SST across all school days; the remaining 10% of adolescents who reported two or more different SSTs were likely due to occasional school delays such as weather or exams. SST was first coded continuously, and then divided into four categories for ease of interpreting the results: (1) before 07:30, (2) 07:30–07:59, (3) 08:00–08:29, and (4) 08:30 or later (reference group). Ten adolescents had more than one most frequently occurring SST (i.e. bi-modal) spanning more than one SST group. The analyses used both categorical and continuous SSTs for comprehensive comparison with current literature.
Outcomes (actigraphy)
24-hour sleep duration
Sleep duration was calculated as the sum of the duration of all sleep intervals within a day, in minutes.
Sleep onset
Sleep onset refers to the actigraphically-determined start time of the sleep interval. Consistent with prior definitions [47], sleep onset was defined as the military time (e.g. 11:30 pm = 23:30) of the last epoch with activity count >10 followed by five consecutive 30-second epochs ≤10 for a sleep interval. If there was more than one sleep interval in a day, the sleep onset of the interval with the longest duration between 22:00 and 08:00 was used.
Sleep offset
Sleep offset refers to the actigraphically-determined end time of the sleep interval. Consistent with the standard algorithm used for scoring [47], sleep offset was defined as the military time of the first epoch with activity count >10 preceded by 5 consecutive 30-second epochs ≤ 10. If there was more than one sleep interval in a day, the sleep offset of the interval with the longest time between 22:00 and 08:00 was used.
Wake after sleep onset
WASO was measured as minutes of wake after sleep onset and before sleep offset for the sleep interval with the longest time between 22:00 and 08:00 in a given day [47, 48]. WASO during nap intervals is not included. Increased WASO indicates lower sleep quality.
Sleep maintenance efficiency
Sleep maintenance efficiency was used to measure sleep quality. Sleep maintenance efficiency was calculated by subtracting minutes of WASO from the nighttime sleep interval duration, excluding naps. The difference was divided by the length of the sleep interval and then multiplied by 100 to produce a percentage of time spent asleep between sleep onset and offset [49]. Higher sleep maintenance efficiency indicates better quality sleep.
Covariates
We adjusted for the adolescents’ sociodemographic characteristics that may influence sleep behaviors [50–53]. Those included age (in years), sex at birth (1 = male vs. 2 = female), and race (1 = black, non-Hispanic, 2 = Hispanic/Latino, 3 = multiracial/other, vs. 4 = white, non-Hispanic). The multiracial/other race category included those who responded “don’t know,” or did not provide their race. We also considered primary caregiver’s educational attainment (1 = less than high school, 2 = high school or equivalent, 3 = some college or technical schooling, vs. 4 = college or more) and household income to poverty threshold (1 ≤ 49%, 2 = 50%–99%, 3 = 100%–199%, 4 = 200%–299%, vs. 5 ≥300%) constructed using the US Census Bureau threshold for poverty for households of the same composition during the same year (http://www.census.gov/cps/data/povthresholds.Html). To account for any potential influence on SST, we adjusted for school type (1 = private or religious school, vs. 2 = public school). Finally, we included the adolescent’s living arrangement (1 = biological mother only, 2 = biological mother and her new partner, 3 = other, including biological father and his new partner, biological father only, or other primary caregiver, vs. 4 = biological mother and biological father). Within-person variance of SSTs was also controlled for in the models; however, 90% of participants did not differ in SST between days. All continuous variables were centered at the sample means. For categorical variables, the last category served as the reference group.
Statistical analysis
To investigate the associations between sleep and SST across 383 adolescents with 1116 school-day observations, we used multilevel modeling (Proc Mixed) in SAS 9.4. Separate models were used to test the associations between SST and the following actigraphically-assessed sleep outcomes of interest: 24-hour sleep duration (model 1), sleep onset (model 2), sleep offset (model 3), WASO (model 4), and sleep maintenance efficiency (model 5), all adjusting for covariates and occasional within-person variation of SST. Incorporating multiple observations per participant allowed us to test the associations of SST with nightly sleep, providing a more precise picture of how SST and adolescents’ day-to-day sleep are associated than using a single recall of typical sleep timing and duration in an unspecified time period.
Results
Descriptive results
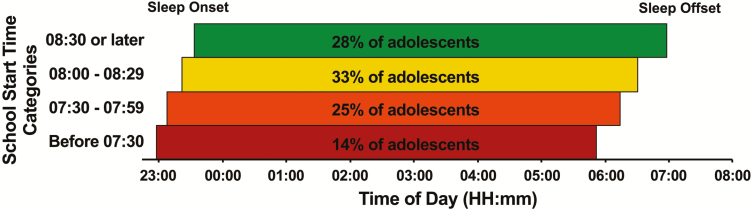
The descriptive characteristics of our study sample of 383 adolescents are shown in Table 1. On average, adolescents were 15.5 years old (SD = 0.6, Range = 14.7–17.7 years). Our sample was 47% male, ethnically diverse (e.g. 44% black, 26% Hispanic/Latino), and had varied family structures (32% lived with biological mother and biological father). The household incomes for 27% of the sample were below the poverty line, and 34% of primary caregivers completed high school or less education. Most of the adolescents attended public school (89%). The proportion of adolescents and observations included in each SST category are presented in Table 1 and Figure 1.
Table 1.
Sample characteristics by school start times
| Total | Before 07:30 | 07:30–07:59 | 08:00–08:29 | 08:30 or later | |
|---|---|---|---|---|---|
| M or % (SD) | M or % (SD) | M or % (SD) | M or % (SD) | M or % (SD) | |
| Number of adolescents | 383 | 53 (14%) | 96 (25%) | 126 (33%) | 108 (28%) |
| Number of daily observations | 1116 | 146 (13%) | 288 (26%) | 379 (34%) | 303 (27%) |
| Mean age | 15.5 ± 0.6 | 15.2 ± 0.3 | 15.3 ± 0.4 | 15.5 ± 0.5 | 15.7 ± 0.7 |
| Sex | |||||
| Male | 47% | 12% | 22% | 39% | 26% |
| Female | 53% | 15% | 28% | 27% | 30% |
| Race | |||||
| White | 16% | 18% | 47% | 19% | 16% |
| Black | 44% | 17% | 20% | 33% | 30% |
| Hispanic/Latino | 26% | 5% | 11% | 42% | 42% |
| Multiracial/Other | 14% | 15% | 43% | 31% | 11% |
| Income to poverty threshold | |||||
| <49% | 10% | 13% | 26% | 26% | 36% |
| 50%–99% | 17% | 16% | 28% | 34% | 22% |
| 100%–199% | 27% | 11% | 19% | 40% | 30% |
| 200%–299% | 16% | 13% | 16% | 34% | 37% |
| >300% | 30% | 16% | 34% | 28% | 22% |
| Caregiver’s education | |||||
| Less than high school | 19% | 7% | 18% | 43% | 32% |
| High school or equivalent | 15% | 16% | 21% | 29% | 34% |
| Some college or technical school | 46% | 14% | 25% | 31% | 30% |
| College or more | 20% | 18% | 34% | 32% | 16% |
| School type | |||||
| Private/Religious school | 11% | 0% | 35% | 33% | 33% |
| Public school | 89% | 16% | 24% | 33% | 28% |
| Living arrangement | |||||
| Biological mother and father | 32% | 14% | 28% | 34% | 24% |
| Biological mother and new partner | 25% | 20% | 22% | 30% | 29% |
| Biological mother only | 34% | 11% | 24% | 37% | 27% |
| Other | 8% | 6% | 28% | 19% | 47% |
Figure 1.
Distribution of sample adolescents’ high school start times and unadjusted means of sleep onset and sleep offset. N = 383 adolescents, with the following school start time categorical sample sizes: n = 53 before 07:30, n = 96 from 07:30 to 07:59, n = 126 from 08:00 to 08:29 and n = 108 at 08:30 or later; adolescents with more than one most frequently occurring school start time (i.e. bi-modal) were grouped by the category of their first observation. The mean time of sleep onset for adolescents were 22:57, 23:07, 23:21, and 23:32 when school start times were before 07:30, 7:30–7:59, 08:00–08:29, and 08:30 or later, respectively. The mean time of sleep offset for adolescents were 05:51, 06:14, 06:30, and 06:58 when school start times were before 07:30, 07:30–07:59, 08:00–08:29, and 08:30 or later, respectively.
As shown in Table 1, Hispanic study participants were disproportionately more likely to have later SSTs compared to white, black, and participants of other/mixed races (χ2 =57.6, p < .0001). Stratified by race, 42% of Hispanic adolescents had SSTs at 08:30 or later, compared to 30% of black students, 16% of white adolescents, and 11% of adolescents of other/mixed races. There was no difference in household income by SST categories (χ2 = 17.1, p = .1463). Hispanic students and students of other/mixed race had longer sleep duration than white students by 27 (p < .001) and 17 (p < .05) minutes, respectively. Sleep duration did not differ significantly by household income to poverty line ratios groups.
The unadjusted means of sleep onset and sleep offset for the entire sample and stratified by SST category are presented in Table 2 and Figure 1, with Table 2 also presenting 24-hour sleep duration, WASO, and sleep maintenance efficiency. On average, 24-hour sleep duration was 7.4 hours (M = 445.0 ± 81.6 minutes, Range = 116.5–773.5), with average sleep onset at 23:17 (SD = 1.3 hours, Range = 18:15–6:23), average sleep offset at 6:28 (SD = 1.0 hour, Range = 00:12–09:19), average WASO was 37.6 minutes (SD = 16.5, Range = 1.5–106.5), and average sleep maintenance efficiency was 91.3% (SD = 3.3%, Range = 78.3%–98.7%).
Table 2.
Unadjusted means and SD of SSTs and actigraphic 24-hour sleep duration, timing, and quality for the entire study sample and also stratified by categorical SSTs
| Whole sample (SD) | Before 07:30 (SD) | 07:30–07:59 (SD) | 08:00–08:29 (SD) | 08:30 or later (SD) | |
|---|---|---|---|---|---|
| School start time (military time) | 08:08 (39.4) | 07:16 (13.2) | 07:41 (9.5) | 08:08 (9.0) | 08:57 (29.4) |
| 24-hour sleep duration (minutes) | 445.0 (81.6) | 430.9 (75.1) | 439.2 (72.8) | 442.2 (81.2) | 460.8 (90.4) |
| Sleep onset (military time) (SD is in minutes) | 23:17 (80.9) | 22:57 (69.8) | 23:07 (71.5) | 23:21 (78.4) | 23:32 (93.5) |
| Sleep offset (military time) (SD is in minutes) | 06:28 (57.4) | 05:51 (49.4) | 06:14 (46.1) | 06:30 (55.2) | 06:58 (58.4) |
| Wake after sleep onset (minutes) | 37.6 (16.5) | 34.9 (15.4) | 35.5 (14.3) | 38.9 (17.6) | 39.4 (17.2) |
| Sleep maintenance efficiency (percentage) | 91.3 (3.3) | 91.6 (3.4) | 91.8 (2.7) | 91.0 (3.5) | 91.2 (3.3) |
Unadjusted means of 24-hour sleep duration, sleep onset, sleep offset, were calculated from 1116 daily observations, and unadjusted means of school start time (SST) were calculated from 383 adolescents. Sleep duration and wake after sleep onset are presented in minutes, while sleep onset and sleep offset are presented in military time, with SD in minutes. Sleep maintenance efficiency is presented as a percentage.
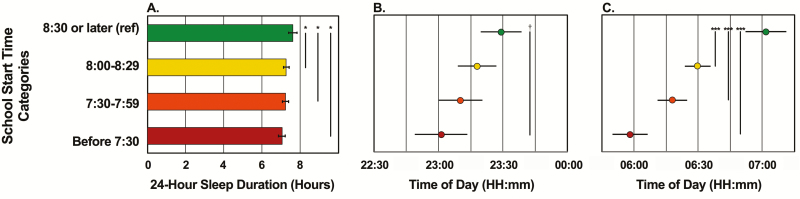
Association between SST and 24-hour sleep duration
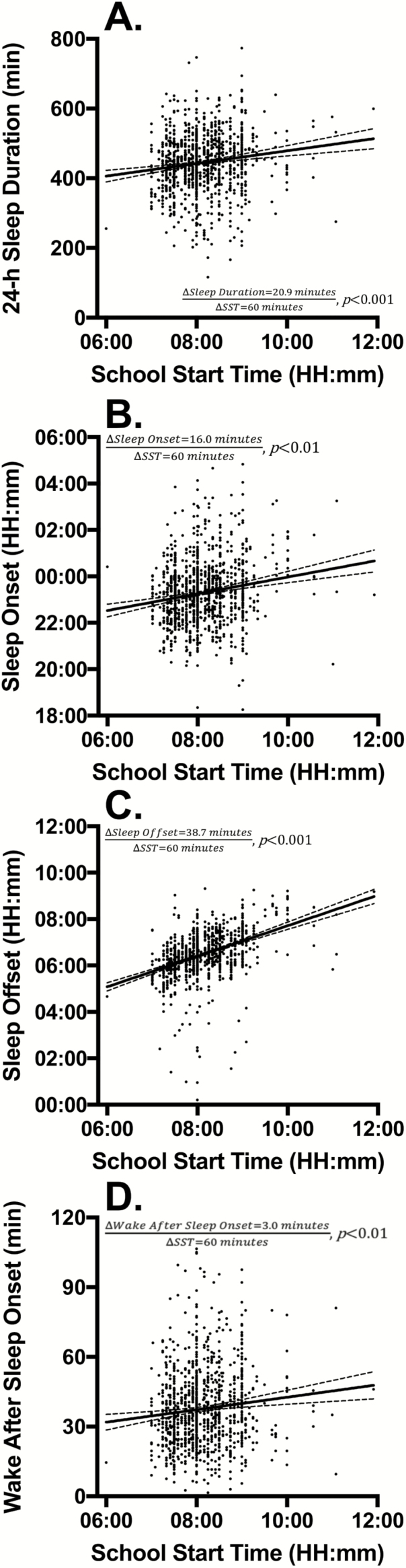
Tables 3 and 4 show results from multilevel modeling examining the associations between SST and actigraphic sleep outcomes, after adjusting for covariates. In model 1 predicting 24-hour sleep duration, adolescents with early SST categories all slept significantly (p < .05) less than the adolescents in the reference category, with SSTs at 08:30 or later, who slept for 456.8 minutes (7 hours and 37 minutes). Adolescents with SSTs before 07:30 slept 34.4 minutes less, 07:30–07:59 slept 23.3 minutes less, and 08:00–08:29 slept 20.9 minutes less (Figure 2A). Post-hoc tests comparing 24-hour sleep duration among early SST categories (i.e. before 07:30 vs. 07:30–07:59, before 07:30 vs. 08:00–08:29, and 07:30–07:59 vs. 08:00–08:29) yielded no significant differences. Analyses using a continuous SST variable found a consistent result, presented in Table 4 and Figure 3A, such that every 1 hour later SST was associated with a significantly longer 24-hour sleep duration, as much as 20.9 minutes longer (p < .001). Thus, our hypothesis 1 that later SSTs would be associated with longer 24-hour sleep duration was fully supported.
Table 3.
Results of multilevel models examining the association between categorical school start times and actigraphic 24-hour sleep duration, sleep onset, and sleep offset
| Model 124-hour sleep duration (minutes) | Model 2Sleep onset (military time, minutes) | Model 3Sleep offset (military time, minutes) | |
|---|---|---|---|
| Fixed effects | B (SE) | B (SE) | B (SE) |
| Intercept (in minutes or military time) | 456.8 (12.6)*** | 23:29 (14.0)* | 07:02 (9.5)*** |
| School start time categories (ref 08:30 or later) | |||
| Before 07:30 | −34.4 (11.1)* | −27.9 (12.2)† | −63.5 (8.2)*** |
| 07:30–07:59 | −23.3 (9.2)* | −18.9 (10.2) | −43.6 (6.9)*** |
| 08:00–08:29 | −20.9 (8.2)* | −11.2 (8.9) | −31.9 (6.0)*** |
| Daily variation of school start times | 13.4 (4.8)** | −1.9 (4.4) | 13.1 (2.7)*** |
| Age (years) | −5.5 (6.2) | 6.6 (6.9) | 7.4 (4.7) |
| Sex (ref female) | |||
| Male | −14.7 (6.4)* | 9.0 (7.1) | −0.5 (4.8) |
| Race (ref. white) | |||
| Black | 10.1 (10.1) | 2.6 (11.1) | −2.5 (7.6) |
| Hispanic/Latino | 22.3 (11.0)* | −1.8 (12.2) | 13.7 (8.3)† |
| Multiracial/Other | 19.6 (11.6)† | 2.0 (12.9) | 19.0 (8.8)* |
| Caregiver’s education (ref college or more) | |||
| Less than high school | −0.5 (11.9) | −7.5 (13.3) | −7.6 (9.0) |
| High school or equivalent | 1.2 (11.9) | 7.9 (13.2) | 8.8 (9.0) |
| Some college or technical school | −6.2 (9.4) | 6.5 (10.4) | −5.3 (7.0) |
| Income to poverty threshold (ref >300%) | |||
| <49% | −3.2 (13.3) | 12.4 (14.7) | 4.7 (9.9) |
| 50%–99% | 2.3 (10.7) | −4.2 (12.0) | −5.4 (8.2) |
| 100%–199% | −2.1 (9.3) | 12.6 (10.4) | −2.0 (7.0) |
| 200%–299% | −6.4 (10.2) | 6.0 (11.4) | −2.5 (7.7) |
| School type (ref public school) | |||
| Private/Religious school | −7.4 (10.0) | −5.6 (11.2) | −2.6 (7.6) |
| Living arrangement (ref biological mother and father) | |||
| Biological mother only | 1.6 (8.3) | −6.0 (9.3) | −3.1 (6.3) |
| Biological mother and new partner | 12.4 (8.5) | −24.6 (9.5)* | −8.6 (6.4) |
| Other | −5.0 (12.2) | 0.2 (13.6) | −0.1 (9.3) |
Multilevel models 1–3 clustered 1116 school-day observations among 383 adolescents. All models adjusted for age, sex, race, household income, primary caregiver’s education, school type, and living arrangement and daily-level variation of school start times. Sleep onset and sleep offset intercepts are presented in military time, and all other values are in minutes.
† p ≤ .10, *p < .05, **p < .01, ***p < .001.
Table 4.
Results of multilevel models examining the association between continuous school start times and actigraphic 24-hour sleep duration, sleep onset, and sleep offset
| Model 124-hour sleep duration (minutes) | Model 2Sleep onset (military time, minutes) | Model 3Sleep offset (military time, minutes) | |
|---|---|---|---|
| Fixed effects | B (SE) | B (SE) | B (SE) |
| Intercept (in minutes or military time) | 270.7 (40.9)*** | 21:07 (44.2)*** | 01:19 (28.4)** |
| School start times (in minutes) | 20.9 (5.1)*** | 16.0 (5.4)** | 38.7 (3.5)*** |
| Daily variation of school start times | 14.2 (4.8)** | −85.4 (4.4) | 13.9 (2.7)*** |
| Age (years) | −5.4 (6.1) | 6.8 (6.7) | 7.3 (4.4)† |
| Sex (ref. female) | |||
| Male | −14.2 (6.3)* | 9.9 (7.0) | 1.1 (4.5) |
| Race (ref. white) | |||
| Black | 8.2 (9.8) | 2.0 (10.9) | −5.0 (7.1) |
| Hispanic/Latino | 20.4 (10.7)† | −1.8 (11.9) | 11.9 (7.7) |
| Multiracial/Other | 18.4 (11.5) | 1.4 (12.8) | 17.2 (8.3)* |
| Caregiver’s education (ref college or more) | |||
| Less than high school | −1.3 (11.8) | −7.7 (13.2) | −8.8 (8.5) |
| High school or equivalent | 1.5 (11.8) | 7.7 (13.1) | 8.6 (8.5) |
| Some college or technical school | −7.0 (9.3) | 5.7 (10.3) | −6.8 (6.7) |
| Income to poverty threshold (ref > 300%) | |||
| <49% | −3.8 (13.2) | 11.5 (14.6) | 3.0 (9.4) |
| 50%–99% | 1.6 (10.6) | −4.8 (11.9) | −6.3 (7.7) |
| 100%–199% | −2.3 (9.2) | 13.0 (10.2) | −1.6 (6.6) |
| 200%–299% | −7.2 (10.1) | 5.5 (11.3) | −4.0 (7.3) |
| School type (ref public school) | |||
| Private/religious school | −8.0 (9.8) | −6.0 (11.0) | −3.8 (7.2) |
| Living arrangement (ref biological mother and father) | |||
| Biological mother only | 2.1 (8.2) | −5.2 (9.2) | −1.9 (6.0) |
| Biological mother and new partner | 14.2 (8.4)† | −23.4 (9.4)* | −5.7 (6.1) |
| Other | −4.8 (12.1) | −0.2 (13.5) | −0.8 (8.8) |
Multilevel models 1–3 clustered 1116 school-day observations among 383 adolescents. All models adjusted for age, sex, race, household income, primary caregiver’s education, school type, and living arrangement and daily-level variation of school start times. Sleep onset and sleep offset intercepts are presented in military time, and all other values are in minutes.
† p ≤ .10, *p < .05, **p < .01, ***p < .001.
Figure 2.
Adjusted estimates of 24-hour sleep duration, sleep onset, sleep offset by categorical school start time. N = 383 adolescents with 1116 school-day observations clustered in multilevel models to measure actigraphic 24-hour sleep duration (panel A), sleep onset (panel B), and sleep offset (panel C), as predicted by categorical school start times. Vertical bars begin and end at groups that differ significantly, and the absence of a bar reflects no statistical difference (p > .10). Post-hoc tests were only significant in the model testing school start times and sleep offset when comparing adolescents with school start times before 07:30 with adolescents with school start times from 07:30 to 07:59 (β = 19.9 minutes, SE = 8.0 minutes, p < .05) and comparing adolescents with school start times before 07:30 with adolescents with school start times from 08:00 to 08:29 (β = 31.6 minutes, SE = 7.8 minutes, p < .01). †p ≤ .10, *p < .05, **p < .01, ***p < .001.
Figure 3.
Adjusted estimates of 24-hour sleep duration, sleep onset, sleep offset, and wake after sleep onset by continuous school start time. N = 383 adolescents with 1116 school-day observations clustered in multilevel models to measure actigraphic 24-hour sleep duration (panel A), sleep onset (panel B), sleep offset (panel C), and wake after sleep onset (panel D) as predicted by continuous school start times. Each dot represents one of the 1116 observations and the slope of the lines, from left to right, can be interpreted as the change in 24-hour sleep duration, change in sleep onset, change in sleep offset, and change in wake after sleep onset for every 1 hour later school start time.
In addition to 24-hour sleep duration, we conducted supplementary analyses with nighttime sleep duration (restricting days with multiple sleep intervals to include only the longest sleep interval spanning 22:00 to 08:00, thereby excluding naps). Results with both categorical and continuous SST were similar to those of 24-hour sleep duration (results available upon request). SSTs before 07:30 and 07:30–07:59 were associated with significantly shorter nighttime sleep duration by 34.3 (p < .05), and 23.2 (p < .05) minutes, respectively, compared to adolescents with SSTs at 08:30 or later. SSTs from 08:00–08:29 trended toward shorter nighttime sleep duration by 19.2 (p = .052) minutes compared to SSTs at 08:30 or later. Analysis of the SST continuous data showed that for every 1-hour delay in SSTs, there was an associated extension of nighttime sleep by 22.0 minutes (p < .001). Only 12.5% of daily observations included naps, and there was no significant association between SSTs and duration napping. The proportion of adolescents who napped at least one time during the study was 28%, 30%, 27%, and 31% for those with start times before 07:29, 07:30–07:59, 08:00–08:29, and 08:30, respectively, with no statistically significant differences (χ2 = 0.38, p = .94).
Association between SST and sleep timing
Model 2 in Table 3 and Table 4 tested the associations between SSTs and sleep onset. Compared to adolescents with SSTs at 08:30 or later, adolescents in the middle two categories of SSTs, spanning 07:30 to 08:29, did not significantly differ in sleep onset. The earliest SSTs (before 07:30) were marginally associated with (p = .051) earlier sleep onset by 27.9 minutes, when compared to SSTs at 08:30 or later (Figure 2B). There were no significant differences in sleep onset among the earlier SST categories. Analyses using a continuous SST variable (model 2, Table 4) found that every 1 hour later SST was associated with 16 minutes later sleep onset (p < .01), presented in Figure 3B.
Model 3 in Tables 3 and 4 tested the associations between SSTs and sleep offset. Adolescents with SSTs 08:30 or later had significantly (p < .001) later sleep offset than adolescents in all other earlier SST groups, shown in Figure 2C. Compared to adolescents with SSTs 08:30 or later, those with SSTs before 07:30 woke up 63.5 minutes earlier, from 07:30–07:59 woke up 43.6 minutes earlier, and from 08:00 to 08:29 woke up 31.9 minutes earlier. Similarly, using a continuous SST variable (model 3, Table 4) resulted in 38.7 minutes later sleep offset for every 1 hour later SST (p < .001), shown in Figure 3C. Post-hoc tests revealed later sleep offset for adolescents in both the 07:30–07:59 and the 08:00–08:29 groups, compared to the before 07:30 group (19.9 minutes, p < .05 and 31.6 minutes, p < .01, respectively). There were no significant differences in sleep offset when comparing the two middle groups, 07:30–07:59 and 08:00–08:29, to each other. Taken together, later SSTs were associated with later sleep offset, but not with sleep onset (based on categorical SSTs), thus our hypothesis 2 was also supported.
Association between SST and sleep quality
Models 4 and 5 tested the associations between SSTs and sleep quality, measured by WASO and sleep maintenance efficiency. There was no significant difference in WASO or sleep maintenance efficiency between adolescents grouped by SSTs before 07:29, 07:30–07:59, 08:00–08:29, or after 08:30. However, when the continuous measure of SST was used, each 1-hour later SST was associated with 3.0 minutes more of WASO (p < .01), shown in Figure 3D. There was no significant relationship between continuous SSTs and sleep maintenance efficiency.
Discussion
Later SSTs, at 08:30 or later, are strongly associated with actigraphically-assessed adolescent sleep timing, particularly, later wake times (by 32–64 minutes) that permit longer sleep duration (by 21–34 minutes) when compared to adolescents within earlier categories of SSTs (before 07:30, 07:30–07:59, and 08:00–08:29). Results followed a dose-response pattern as adolescents with the earliest SSTs had the earliest sleep offset, just before 06:00, and the shortest sleep duration, 422.4 minutes (7.0 hours). Adolescents with the latest SST achieved an estimated 456.8 minutes (7.6 hours) of sleep duration, significantly longer than the adolescents in other categories, but still not meeting the 8 hours of sleep per night minimum recommended amount by the American Academy of Sleep Medicine and the National Sleep Foundation [5, 54]. Over the course of one school-week, adolescents with SSTs at 08:30 or later accumulated 172 minutes, 117 minutes, and 105 minutes more sleep when compared to their peers starting school before 07:30, 07:30–07:59, and 08:00–08:29, respectively. Sleep maintenance efficiency did not differ significantly by SSTs, suggesting no difference in sleep quality when accounting for the duration of the sleep interval. The null relationship between actigraphic sleep quality and categorical SSTs is consistent with single-question self-reports of sleep quality [13] but contrasts with the perceived lower quality sleep associated with earlier SSTs reported in other studies [2, 6].
We also tested the associations of sleep timing, duration, and quality with a continuous SST variable, and found that for every 1 hour later SST, associated sleep onset was 16 minutes later, sleep offset was 39 minutes later, sleep duration was 21 minutes longer with 3 more minutes of WASO and no difference to sleep maintenance efficiency. The lower sleep quality indicated by WASO may be driven by the longer opportunity for wake given longer sleep duration and the high correlation between sleep duration and WASO (r = 0.53, p < .0001, observation-level). These findings suggest that adolescents are likely to delay sleep offset when given the opportunity. However, factors such as delayed circadian preference, electronic media use, and caffeine consumption may also delay sleep onset [55], helping to explain the observed 21-minute extension in sleep duration despite a theoretical 1-hour increase in sleep opportunity. The continuous model of SSTs incorporates a diverse range of SSTs clustered (93% of students) between 07:00 and 09:30, and caution should be taken in extrapolation of these findings beyond those included in this study.
Though our study is cross-sectional, the findings are consistent with longitudinal studies, such as a recent study measuring sleep actigraphically in a Singapore girls’ school [45] and a 2017 meta-analysis [35]. The study in Singapore found that a 45-minute SST delay led to bedtimes 9 minutes later, wake times 32 minutes later, and 23 minutes longer time in bed, with sustained results observed a month later [45]. According to the meta-analysis, delaying SSTs increased self-reported sleep duration from 7 hours and 4 minutes to 7 hours and 24 minutes, with longer sleep times permitted by later delays [35]. Our findings contribute to this literature showing that later SSTs allow adolescents to have longer 24-hour and nighttime sleep duration measured via actigraphy. Collectively, these findings suggest delaying SSTs as an effective policy-level modification to improve sleep health across the adolescent population [56].
Other studies suggest that delaying SSTs and extending adolescent sleep can have a wide range of benefits on adolescents, such as less time spent watching television and more time spent completing homework [24]. Notably, delays in SSTs yielded improvements in test scores that were more substantial for students on the lower end of the test score distribution curve, and were ultimately less expensive than reducing class size [57]. Other benefits to the students and the community included improved academic performance and increased potential lifetime earnings while also reducing motor vehicle accident rates [58] and potentially saving costs on transportation [55, 59]. A study delaying SSTs from 08:50 to 10:00 found significant reductions in absences due to illness and improvements in test scores, which were reversed when start times reverted back to 08:50, signifying that 08:30 is the earliest clinically recommended start time, and even later SSTs could be considered [60].
Our study is innovative for capturing actigraphically-measured sleep and a diverse range of SSTs in a national sample of urban adolescents. Our participants are part of a cohort that oversampled unwed mothers, allowing us to include youths at high risk for adverse health and school outcomes. Tables 3 and 4 show variation in sleep outcomes by race/ethnicity. In particular, Hispanic and multiracial/other students are sleeping longer with later sleep offset compared to white students in this sample. These analyses did not show variation in sleep outcomes by maternal education or household income to poverty threshold ratios. Study participants are mostly from large urban areas, and thus the results may provide policy implications for urban schools where SSTs are generally earlier than rural schools [61]. We were limited by the use of self-reported SSTs, thus future studies should consider obtaining this information directly from schools. Future research should also consider the racial/ethnic and socioeconomic disparities associated with SSTs and the systematic differences in schools within urban, suburban and rural communities. Additionally, future experimental and actigraphy-based studies should investigate the causal impact of a later SST on sleep-related health and academic outcomes.
Conclusion
Pediatric, sleep, and medical experts recommend that high schools begin no earlier than 08:30. Adolescents starting school before 08:30 woke up significantly earlier and slept significantly less than adolescents starting school at 08:30 or later. Inadequate sleep during adolescence is a concern for parents, schools, communities, and public health. Delaying SSTs provide a potential policy-level intervention that could improve adolescent sleep, and therefore adolescent health and well-being, at the population level.
Funding
Research reported in this publication was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development of the National Institutes of Health under award numbers R01HD073352 (to L.H.), R01HD36916, R01HD39135, and R01HD40421, as well as a consortium of nonprofit foundations. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Conflict of interest statement. L.H. serves on the Board of Directors of the National Sleep Foundation and receives an honorarium for her role as Editor-in-Chief of Sleep Health. Outside of the current work, O.M.B. received two subcontract grants to Pennsylvania State University from Mobile Sleep Technologies (NSF/STTR #1622766, NIH/NIA SBIR R43AG056250).
Acknowledgments
The authors wish to thank Donald Miller at the Penn State Population Research Institute for data management and programming support. The authors would also like to thank Sindhuja Kancharla, Dylan Smith, and Ahmed Belazi at Stony Brook University for their statistical support.
References
- 1. Wolfson AR, et al. . Understanding adolescents’ sleep patterns and school performance: a critical appraisal. Sleep Med Rev. 2003;7(6):491–506. [DOI] [PubMed] [Google Scholar]
- 2. Ming X, et al. . Sleep insufficiency, sleep health problems and performance in high school students. Clin Med Insights Circ Respir Pulm Med. 2011;5:71–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Noland H, et al. . Adolescents’ sleep behaviors and perceptions of sleep. J Sch Health. 2009;79(5):224–230. [DOI] [PubMed] [Google Scholar]
- 4. Carskadon MA, et al. . Pubertal changes in daytime sleepiness. Sleep. 1980;2(4):453–460. [DOI] [PubMed] [Google Scholar]
- 5. Hirshkowitz M, et al. . National sleep foundation’s sleep time duration recommendations: methodology and results summary. Sleep Health. 2015;1(1):40–43. [DOI] [PubMed] [Google Scholar]
- 6. Thacher PV, et al. . Longitudinal outcomes of start time delay on sleep, behavior, and achievement in high school. Sleep. 2016;39(2):271–281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Shochat T, et al. . Functional consequences of inadequate sleep in adolescents: a systematic review. Sleep Med Rev. 2014;18(1):75–87. [DOI] [PubMed] [Google Scholar]
- 8. Danner F, et al. . Adolescent sleep, school start times, and teen motor vehicle crashes. J Clin Sleep Med. 2008;4(6):533–535. [PMC free article] [PubMed] [Google Scholar]
- 9. Vorona RD, et al. . Adolescent crash rates and school start times in two central Virginia counties, 2009-2011: a follow-up study to a southeastern Virginia study, 2007-2008. J Clin Sleep Med. 2014;10(11):1169–1177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Vorona RD, et al. . Dissimilar teen crash rates in two neighboring southeastern Virginia cities with different high school start times. J Clin Sleep Med. 2011;7(2):145–151. [PMC free article] [PubMed] [Google Scholar]
- 11. Wheaton AG, et al. . Sleep duration and injury-related risk behaviors among high school students–United States, 2007-2013. MMWR Morb Mortal Wkly Rep. 2016;65(13):337–341. [DOI] [PubMed] [Google Scholar]
- 12. Group ASW, Adolescence Co, Health CoS. School start times for adolescents. Pediatrics. 2014;134(3):642–649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Peltz JS, et al. . A process-oriented model linking adolescents’ sleep hygiene and psychological functioning: the moderating role of school start times. Sleep Health. 2017;3(6):465–471. [DOI] [PubMed] [Google Scholar]
- 14. Arora T, et al. . Exploring the complex pathways among specific types of technology, self-reported sleep duration and body mass index in UK adolescents. Int J Obes. 2013;37(9):1254–1260. [DOI] [PubMed] [Google Scholar]
- 15. Cappuccio FP, et al. . Meta-analysis of short sleep duration and obesity in children and adults. Sleep. 2008;31(5):619–626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Roberts RE, et al. . Restricted sleep among adolescents: prevalence, incidence, persistence, and associated factors. Behav Sleep Med. 2011;9(1):18–30. [DOI] [PubMed] [Google Scholar]
- 17. Cain N, et al. . Electronic media use and sleep in school-aged children and adolescents: a review. Sleep Med. 2010;11(8):735–742. [DOI] [PubMed] [Google Scholar]
- 18. Keyes KM, et al. . The great sleep recession: changes in sleep duration among US adolescents, 1991-2012. Pediatrics. 2015;135(3):460–468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. US Department of Health and Human Services. Healthy People 2020 Objective Topic Areas and Page Numbers. 2010 2011/01/04/ [cited; 300–1].http://healthypeople.gov/2020/topicsobjectives2020/default.aspx Accessed August 18, 2018.
- 20. Carskadon MA, et al. . Regulation of sleepiness in adolescents: update, insights, and speculation. Sleep. 2002;25(6):453–460. [DOI] [PubMed] [Google Scholar]
- 21. Crowley SJ, et al. . Sleep, circadian rhythms, and delayed phase in adolescence. Sleep Med. 2007;8(6):602–612. [DOI] [PubMed] [Google Scholar]
- 22. Jenni OG, et al. . Homeostatic sleep regulation in adolescents. Sleep. 2005;28(11):1446–1454. [DOI] [PubMed] [Google Scholar]
- 23. Hagenauer MH, et al. . Adolescent changes in the homeostatic and circadian regulation of sleep. Dev Neurosci. 2009;31(4):276–284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Edwards F. Early to rise? The effect of daily start times on academic performance. Econ Edu Rev. 2012;31:970–983. [Google Scholar]
- 25. Carskadon MA, et al. . Regulation of adolescent sleep: implications for behavior. Ann N Y Acad Sci. 2004;1021:276–291. [DOI] [PubMed] [Google Scholar]
- 26. Carskadon MA, et al. . Association between puberty and delayed phase preference. Sleep. 1993;16(3):258–262. [DOI] [PubMed] [Google Scholar]
- 27. American Medical Association. Insufficient sleep in adolescents H-60.930. 2016. https://policysearch.ama-assn.org/policyfinder/detail/school%20start%20time?uri=%2FAMADoc%2FHOD.xml-0-5024.xml.
- 28. Watson NF, et al. ; American Academy of Sleep Medicine Board of Directors. Delaying middle school and high school start times promotes student health and performance: an American academy of sleep medicine position statement. J Clin Sleep Med. 2017;13(4):623–625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Medicine AAoS. Health advisory: school start times [press release]. American Academy of Sleep Medicine Board of Directors; 2017https://aasm.org/advocacy/initiatives/school-start-times/. [Google Scholar]
- 30. Trevorrow T, et al. . Position statement: start middle and high schools at 8:30 am or later to promote student health and learning. Transl Behav Med. 2018. [DOI] [PubMed] [Google Scholar]
- 31. Boergers J, et al. . Later school start time is associated with improved sleep and daytime functioning in adolescents. J Dev Behav Pediatr. 2014;35(1):11–17. [DOI] [PubMed] [Google Scholar]
- 32. Owens JA, et al. . Impact of delaying school start time on adolescent sleep, mood, and behavior. Arch Pediatr Adolesc Med. 2010;164(7):608–614. [DOI] [PubMed] [Google Scholar]
- 33. Carroll JE, et al. . Negative affective responses to a speech task predict changes in interleukin (IL)-6. Brain Behav Immun. 2011;25(2):232–238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Wahlstrom KL. Changing times: findings from the first longitudinal study of later high school start times. NAASP Bulletin. 2002;86(633):3–21. [Google Scholar]
- 35. Bowers JM, et al. . Effects of school start time on students’ sleep duration, daytime sleepiness, and attendance: a meta-analysis. Sleep Health. 2017;3(6):423–431. [DOI] [PubMed] [Google Scholar]
- 36. Morgenthaler TI, et al. . High school start times and the impact on high school students: what we know, and what we hope to learn. J Clin Sleep Med. 2016;12(12): 1681–1689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Carskadon MA, et al. . Adolescent sleep patterns, circadian timing, and sleepiness at a transition to early school days. Sleep. 1998;21(8):871–881. [DOI] [PubMed] [Google Scholar]
- 38. Lufi D, et al. . Delaying school starting time by one hour: some effects on attention levels in adolescents. J Clin Sleep Med. 2011;7(2):137–143. [PMC free article] [PubMed] [Google Scholar]
- 39. Winsler A, et al. . Sleepless in Fairfax: the difference one more hour of sleep can make for teen hopelessness, suicidal ideation, and substance use. J Youth Adolesc. 2015;44(2):362–378. [DOI] [PubMed] [Google Scholar]
- 40. Nahmod NG, et al. . High school start times after 8:30 am are associated with later wake times and longer time in bed among teens in a national urban cohort study. Sleep Health. 2017;3(6):444–450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Dexter D, et al. . Sleep, sleepiness and school start times: a preliminary study. WMJ. 2003;102(1):44–46. [PubMed] [Google Scholar]
- 42. Meltzer LJ, et al. . Start later, sleep later: school start times and adolescent sleep in homeschool versus public/private school students. Behav Sleep Med. 2016;14(2):140–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Short MA, et al. . A cross-cultural comparison of sleep duration between US And Australian adolescents: the effect of school start time, parent-set bedtimes, and extracurricular load. Health Educ Behav. 2013;40(3): 323–330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Perkinson-Gloor N, et al. . Sleep duration, positive attitude toward life, and academic achievement: the role of daytime tiredness, behavioral persistence, and school start times. J Adolesc. 2013;36(2):311–318. [DOI] [PubMed] [Google Scholar]
- 45. Lo JC, et al. . Sustained benefits of delaying school start time on adolescent sleep and well-being. Sleep. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Wolfson AR, et al. . Middle school start times: the importance of a good night’s sleep for young adolescents. Behav Sleep Med. 2007;5(3):194–209. [DOI] [PubMed] [Google Scholar]
- 47. Marino M, et al. . Measuring sleep: accuracy, sensitivity, and specificity of wrist actigraphy compared to polysomnography. Sleep. 2013;36(11):1747–1755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Buxton OM, et al. . Work-family conflict and employee sleep: evidence from it workers in the work, family and health study. Sleep. 2016;39(10):1871–1882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Chen X, et al. . Racial/ethnic differences in sleep disturbances: the multi-ethnic study of atherosclerosis (MESA). Sleep. 2015;38(6):877–888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Hale L. Who has time to sleep? J Public Health (Oxf). 2005;27(2):205–211. [DOI] [PubMed] [Google Scholar]
- 51. Stamatakis KA, et al. . Short sleep duration across income, education, and race/ethnic groups: population prevalence and growing disparities during 34 years of follow-up. Ann Epidemiol. 2007;17(12):948–955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Reichman NE, et al. . Fragile families: sample and design. Child Youth Serv Rev. 2001;23(4/5):303–326. [Google Scholar]
- 53. Troxel WM, et al. . Single-parent family structure and sleep problems in black and white adolescents. Sleep Med. 2014;15(2):255–261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Paruthi S, et al. . Recommended amount of sleep for pediatric populations: a consensus statement of the American academy of sleep medicine. J Clin Sleep Med. 2016;12(6):785–786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Owens J; Adolescent Sleep Working Group; Committee on Adolescence Insufficient sleep in adolescents and young adults: an update on causes and consequences. Pediatrics. 2014;134(3):e921–e932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Hale L, et al. . Embracing the school start later movement: adolescent sleep deprivation as a public health and social justice problem. Am J Public Health. 2018;108(5):599–600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Krueger AB. Experimental estimates of education production functions*. The Q J Econ. 1999;114(2):497–532. [Google Scholar]
- 58. Hafner M, et al. . The economic implications of later school start times in the United States. Sleep Health. 2017;3(6):451–457. [DOI] [PubMed] [Google Scholar]
- 59. Barnes M, et al. . Setting adolescents up for success: promoting a policy to delay high school start times. J Sch Health. 2016;86(7):552–557. [DOI] [PubMed] [Google Scholar]
- 60. Kelley P, et al. . Is 8:30 a.m. Still too early to start school? A 10:00 a.m. School start time improves health and performance of students aged 13-16. Front Hum Neurosci. 2017;11:588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Wolfson AR, et al. . A survey of factors influencing high school start times. NAASP Bulletin. 2005;89(642):47–66. [Google Scholar]