ABSTRACT
Background:
Quality measurements are crucial to healthcare quality improvement, and patient satisfaction with nursing care is widely adopted as a key outcome indicator of the overall quality of healthcare. There is a lack of instruments to measure patient satisfaction with nursing care in an Arabic context.
Purpose:
The purpose of this study was to develop and validate an Arabic version of the Patient Satisfaction with Nursing Care Quality Questionnaire and to explore patient satisfaction with nursing care across hospital units.
Methods:
This was a cross-sectional, methodological research study. A forward–backward translation process and face and content validation using a panel of experts and a pilot test were used to produce an Arabic version of the Patient Satisfaction with Nursing Care Quality Questionnaire. A convenience sampling technique was employed to recruit 292 adult patients who were hospitalized for more than 48 hours. Data were collected over the first quarter of 2016 using a secure electronic survey method.
Results:
The item-level content validity index ranged from .83 to 1, and the scale-level content validity index was .94. Evidence of construct validity was obtained. Exploratory factor analysis revealed a two-factor model that explained 69.3% of the total variance. Confirmatory factor analysis showed that the two-factor model fits the observed data. Internal consistency was satisfactory and similar across different hospital units. Cronbach’s alpha estimates for Factors 1 and 2 were .83 and .96, respectively, with an overall Cronbach’s alpha estimate of .96. Level of patient satisfaction with nursing care was quite high (mean = 4.30/5, SD = 0.74).
Conclusions:
This study provides a 17-item, Likert-scaled, self-reporting instrument, which is psychometrically sound for its content, comprehension, readability, and practicality, to measure patient satisfaction with nursing care quality in an Arabic context.
Key Words: nursing care, Oman, quality, patient satisfaction, Patient Satisfaction with Nursing Care Quality Questionnaire (PSNCQQ)
Introduction
Over the last two decades, increased attention has been paid on quantifying and improving quality of care. Accordingly, measuring nursing care quality has been recognized as a priority for healthcare providers and policymakers. There are two critical factors indicating the need to measure nursing care quality. First, nurses represent the largest segment of healthcare professionals, and therefore measuring nursing care quality is critical to improving practice (Freitas, Silva, Minamisava, Bezerra, & de Sousa, 2014). Second, measuring nursing care quality is a necessary step in determining the level of success that healthcare systems achieve in providing high-quality, high-value care in an equitable manner (Freitas et al., 2014). Patient satisfaction with nursing care (PSNC) is considered a principal outcome indicator of quality of care (Laschinger, Hall, Pedersen, & Almost, 2005), and it is seen as an important aspect for evaluating and improving overall healthcare (Dudkiewicz, 2014; Koy, Yunibhand, & Angsuroch, 2016). As nurses provide the key aspects of healthcare, their contribution influences significantly the level of patient satisfaction with the overall healthcare services provided (de-la-Cueva-Ariza et al., 2014; Laschinger et al., 2005).
The following two sections provide an overview of the literature that explores the published evidence relating to the concept of patient satisfaction and measures of PSNC.
Patient Satisfaction
As a subjective concept, patient satisfaction is difficult to measure and analyze. Moreover, inconsistencies between patient satisfaction and PSNC measures have been identified in the literature (Al-Abri & Al-Balushi, 2014; de-la-Cueva-Ariza et al., 2014; Junewicz & Youngner, 2015). Some authors attempt to provide a conceptual definition for PSNC that includes the actual outcome of the interaction between patients’ expectations and previous experiences, respectively, and their perceptions of actual nursing behaviors (Abdel Maqsood, Oweis, & Hasna, 2012; Atallah, Hamdan-Mansour, Al-Sayed, & Aboshaiqah, 2013; Eriksen, 1995). Similarly, Linder-Pelz (1982) emphasizes that patient satisfaction is individual and subjective and may change based on standards of comparisons or expectations, although the quality of care may remain unchanged over time. In contrast, Pascoe (1983) describes PSNC as the emotional reaction of patients to nursing care.
The antecedents of PSNC include personal characteristics, social–economic influence, previous experience, involvement, motivation, cognition, and environment (Castro, Van Regenmortel, Vanhaecht, Sermeus, & Van Hecke, 2016; de-la-Cueva-Ariza et al., 2014; Milutinović, Simin, Brkić, & Brkić, 2012). These factors affect the ability of patients to judge quality of care. On the other hand, the consequences of PSNC include healthcare outcomes, compliance with healthcare instructions, treatment models, and intention to try the same healthcare provider or facility in the future and to recommend this provider or facility to family and friends (Castro et al., 2016; de-la-Cueva-Ariza et al., 2014; Milutinović et al., 2012).
For the purpose of this study, we define PSNC as the extent to which a patient is content with the care that is received from nurses and influenced by patient characteristics and expectations.
Measures of Patient Satisfaction
A review of the relevant literature revealed that measures of patient satisfaction vary widely and that overall patient satisfaction has often been used as a measure in place of PSNC (Al-Abri & Al-Balushi, 2014; de-la-Cueva-Ariza et al., 2014). Moreover, it has been noticed that a limited number of validated instruments are available to measure PSNC in particular. The identified scales measure dimensions such as attitude and communication, interpersonal relationships, competence, productivity, and provision of support and health information (Abdel Maqsood et al., 2012; La Monica, Oberst, Madea, & Wolf, 1986; Thomas, McColl, Priest, Bond, & Boys, 1996).
The three instruments mostly widely used to measure PSNC in the literature are (a) the 42-item La Monica–Oberst Patient Satisfaction Scale (La Monica et al., 1986), (b) the 56-item Newcastle Satisfaction with Nursing Scale (Thomas et al., 1996), and (c) the 19-item Patient Satisfaction with Nursing Care Quality Questionnaire (PSNCQQ; Laschinger et al., 2005). Evidence shows that these three instruments show sound psychometrics and that they have been used widely to assess PSNC in English-speaking patients (La Monica et al., 1986; Laschinger et al., 2005; Thomas et al., 1996). The PSNCQQ is preferred over the other instruments because it is generally believed to be the easiest to read and comprehend. Each item of the PSNCQQ has a label (e.g., “information you were given”) and a question (e.g., “How clear and complete nurses’ explanations were about tests, treatments, and what to expect?”). In addition, the PSNCQQ is relatively short, which helps minimize the burden on respondents and raise response rates.
The PSNCQQ measures PSNC during the hospital stay. The original English version of the instrument consists of 19 items related to PSNC (including two items related to discharge instructions and coordination of care after discharge) and two additional items related to overall quality of care and hospital recommendation. All PSNCQQ items were used in this study except the two items of discharge instructions and coordination of care after discharge because these two items are not measures of interest in this study. All items were scored using a Likert-type scale, with responses ranging from 1 (poor) to 5 (excellent). The reported Cronbach’s alpha reliability estimate was .97, and the item–total correlations ranged from .61 to .89 (Laschinger et al., 2005). The PSNCQQ reliability estimates were similar across different hospital types, suggesting satisfactory readability and applicability. These results are consistent with the results from a Serbian study in which the PSNCQQ was translated into the Serbian language (Milutinović et al., 2012).
In Oman and the Middle East, the vast majority of patients are Arabic speakers. Although studies conducted in the region have translated some instruments to measure PSNC (Abdel Maqsood et al., 2012; Alasad, Abu Tabar, & AbuRuz, 2015; Atallah et al., 2013), these studies did not report evidence of a systematic transcultural adaptation and validation. Valid and reliable quality measures are integral to evaluation, planning, decision making, and research healthcare quality improvement. Therefore, there is a need for psychometrically sound instruments to measure PSNC in an Arabic context.
Study Aims
The primary aim of this study was to develop and validate an Arabic version of the PSNCQQ (PSNCQQ-Ar) to use it in an Arabic context. The secondary aim was to investigate PSNC in a tertiary hospital in Oman. This study is part of a larger project that aims to establish baseline measures of the nursing workforce and quality of patient care to gain knowledge for policy making and strategy development in Oman.
Methods
A cross-sectional, methodological design was employed to attain the study aims. Data collection was carried out in a large tertiary hospital in Oman with a total bed capacity of 500 during the first quarter of 2016. Participants were selected from different units of the hospital using a convenience sampling technique. The inclusion criteria for the current study are as follows: being an adult patient, hospitalized for more than 48 hours in the same unit, fully conscious and oriented, and able to read and understand the PSNCQQ-Ar. Selected patients were asked to respond directly using a computer-based electronic survey. Trained research assistants were available at the time of data collection to provide any technical assistance required by the participants to complete the survey.
Data were collected anonymously. Participants were asked to fill out electronic informed consent before accessing the electronic survey. After reading the study instructions, participants were asked to click “I agree to participate” to enter to the study survey. Those who clicked “I don’t agree to participate” were thanked and not included in the survey. Permission to use the original instrument was obtained from the corresponding author. In addition, approval from the institutional review board at the affiliated university of the investigators and permission from the target healthcare facility were obtained.
Transcultural Adaptation
The transcultural adaptation of the PSNCQQ was guided by the work of Sousa and Rojjanasrirat (2011) and by the procedure described by Gjersing, Caplehorn, and Clausen (2010).
Translation of the tool
A forward translation from English into Arabic was done by two independent translators who are fluent in both original and target languages. The first translator has a healthcare background and is knowledgeable about the related healthcare terminologies and expressions in both languages. The second translator is not from the healthcare field but is familiar with the slang and jargon related to the relevant terminologies used in the target language by the target population. Two Arabic versions were generated.
After completing the above procedures, a third independent translator who is bilingual compared the two translated versions to generate one Arabic version. The generated version and all suggestions made by the third translator were discussed by a panel comprising the initial two translators and two investigators who are bilingual to assess the compatibility between the original and translated instruments. The panel assessed whether the generated words and items have the same meaning and confirmed that the utilized equivalent expressions did not change the cultural meaning of the words and items.
Subsequently, two independent bilingual Arabic–English translators respectively executed blind backward translations from Arabic into English. The first translator is from the healthcare field, and the other is not a health professional but is knowledgeable regarding the related terminologies and expressions. The two translators were completely blind to the original version of the PSNCQQ. Two English versions were generated.
Face and content validity
A panel of six experts looked into the overall appearance of the prefinal version of the scale to assess its accuracy in measuring PSNC. All of the potential differences in words, items, and meanings were discussed, and discrepancies were resolved through the consensus of the panel members to confirm the semantic, idiomatic, and conceptual equivalencies between the original version and the translated version. Thereafter, to support the scale’s content validity index (CVI), the panel was asked to evaluate each item of the instrument using a 4-point scale (1 = not relevant, 2 = somewhat relevant, 3 = quite relevant, and 4 = highly relevant).
Pilot test
At this stage, 15 native Arabic-speaking participants were recruited from the target population. All participants expressed willingness to be included in the study. Each participant was asked to complete the PSNCQQ-Ar. The research team asked the participants to express any concerns related to the tool and its items and instructions using open-ended questions. All concerns were taken into consideration in finalizing the ready-to-use tool. The data collected in the pilot study were not included in the main study analysis.
Data Analysis
SPSS Version 23 was used for all statistical analyses with a significance level of .05. Descriptive statistics, including frequency, percentages, means, and standard deviations, were used to describe the sample. The reliability of the 17-item scale was derived using standard statistical procedures described by Cronbach, and a Cronbach’s alpha higher than .80 was considered satisfactory (Cronbach, 1951).
To obtain the scale’s CVI, items were dichotomized into relevant and irrelevant. The CVI for the item (I-CVI) was obtained by dividing each item score by 6, which equaled the total number of the expert raters. The CVI for the scale was obtained using the average method (S-CVI/ave; Polit & Beck, 2006). For a panel of six expert raters, the I-CVI of .78 or above and the S-CVI/ave of .90 or above were the minimum acceptable indices (Polit & Beck, 2006).
The suitability of data for factor analysis was assessed using the correlation matrix, Kaiser–Meyer–Olkin (KMO), and Bartlett’s test of sphericity (Williams, Onsman, & Brown, 2010). An exploratory factor analysis (EFA) using maximum likelihood factor extraction was carried out using an oblique method of rotation (Promax, κ = 4) to clarify the data structure and to test the loading strength of the items on factors (Costello & Osborne, 2005). An item value of communality of .3 was considered as the cutoff point. Factors with eigenvalue greater than 1.0 were retained, and factor loadings greater than .4 were considered significant. For the scree plot, number of factors was determined by locating the point where the slope of the downward curve was clearly leveling off (Costello & Osborne, 2005). A confirmatory factor analysis (CFA) was performed using AMOS to assess how well the model gleaned from the EFA matches the observed data and to assess whether a one- or two-factor model fits data better. We estimated the degree of model fit with the data using normed chi-square (χ2/df) ≤ 5, Tucker–Lewis Index (TLI) ≥ .9, Bentler’s comparative fit index (CFI) ≥ .9, and root mean square error of approximation (RMSEA) ≤ .08 (Hu & Bentler, 1999; Schermelleh-Engel, Moosbrugger, & Müller, 2003; Schumacker & Lomax, 2004).
The scale’s construct validity was achieved by assessing its convergent validity (Campbell & Fiske, 1959). Theoretically, perception of nursing care quality and the overall quality of care in the hospital both relate to PSNC. Convergent validity was obtained by testing the correlation between perception of nursing care quality and the overall quality of care in the hospital and then by testing patterns of intercorrelations between these two measures along with PSNC.
Patient satisfaction levels were then compared across different demographics using a t test and a one-way, between-subjects analysis of variance. Tukey’s honestly significant difference (HSD) was used for post hoc analyses.
Results
Sample Description
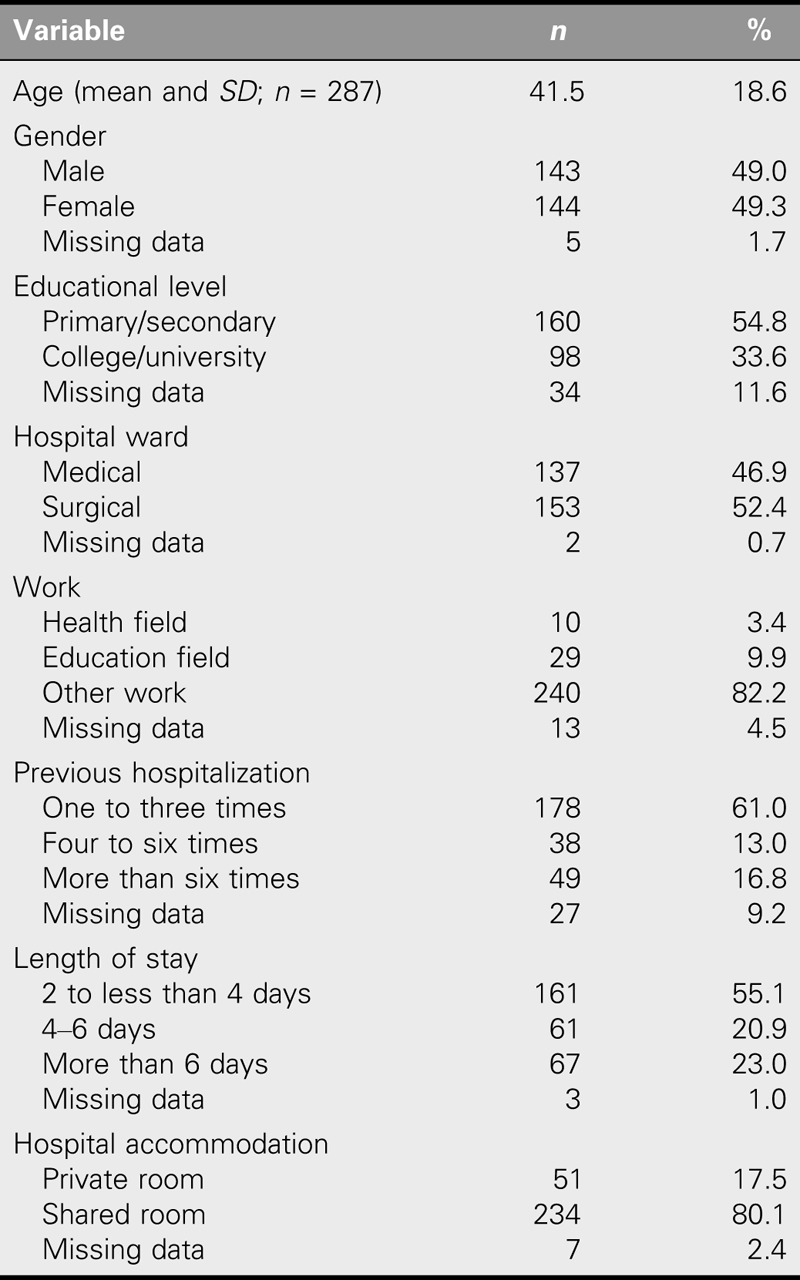
Two hundred ninety-two patients completed the survey, of which 49.3% were female. The mean age of the participants was 41.5 years (SD = 18.6 years). Of the total sample, 54.8% were educated to the primary/secondary level. Only 3.4% of the participants worked in the healthcare field. Most of the participants (61.0%) had been hospitalized at least once. Most of the participants (55.1%) were hospitalized for 2 to less than 4 days, and the vast majority (80.1%) were accommodated in shared rooms (Table 1).
TABLE 1.
Sample Characteristics (N = 292)
Psychometrics
In the current sample (N = 292), the overall Cronbach’s alpha coefficient for the PSNCQQ-Ar was excellent and similar across different hospital units (.96). The split-half coefficients were .91 and .95 for Parts 1 and 2, respectively, with a Guttman split-half coefficient of .94. Analysis of responses of the six expert raters showed that the I-CVI of the 17 items ranged from .83 to 1 and that the S-CVI/ave was .94.
Before EFA, incomplete cases were treated with listwise deletion, which yielded a final sample size of 264 with over 15 subjects per item. Inspection of the correlation matrix revealed that all correlation coefficients were above .3. The KMO measure was satisfactory (.96). Bartlett’s test of sphericity was significant (χ2 = 3878.065, df = 136, p < .001). Accordingly, all assessment results fulfilled the prerequisites for conducting EFA.
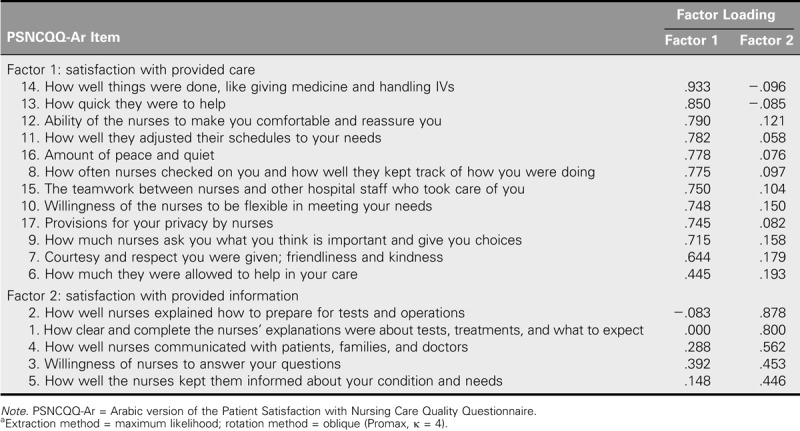
Regarding the dimensionality of the PSNCQQ-Ar, EFA revealed two factors with eigenvalues greater than 1 (10.75, 1.02), suggesting a two-factor model that explained 69.3% of the variance. The scree plot showed that the downward curve leveled off after the second component, confirming the two-factor model. Table 2 shows the pattern matrix from EFA. Factor 1 was composed of Items 6–17 and explained 46.4% of the variance, whereas Factor 2 consisted of Items 1–5 and accounted for 22.9% of the variance. The Cronbach’s alpha coefficients for Factors 1 and 2 were .83 and .96, respectively.
TABLE 2.
Pattern Matrix From Exploratory Factor Analysisa of the 17 Items of the PSNCQQ-Ar (N = 264)
Results of the CFA showed that the one-factor model had a poor data fit, with χ2/df = 4.56, TLI = .86, CFI = .89, and RMSEA = .11, whereas the two-factor model had relatively adequate data fit, with χ2/df = 3.90, TLI = .90, CFI = .91, and almost acceptable RMSEA = .09.
Perception of nursing care quality and the overall quality of care in the hospital significantly and positively correlated with each other (r = .67, p < .001). PSNC scores significantly and positively correlated with perception of nursing care quality (r = .72, p < .001) and with the overall quality of care in the hospital (r = .81, p < .001), supporting the theoretical correlation between these measures and suggesting acceptable convergent validity (Campbell & Fiske, 1959).
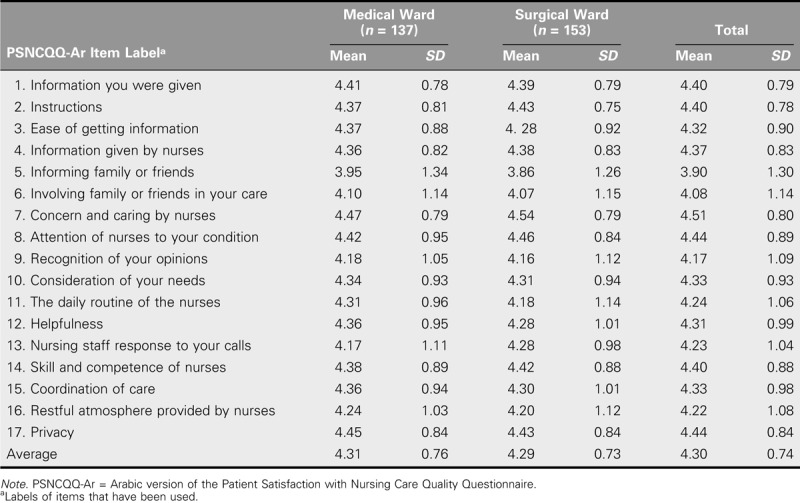
Patient Satisfaction
The total mean score of PSNC was 4.30 of 5 (SD = 0.74). The average score of individual items in the PSNCQQ-Ar ranged from 3.90 to 4.51, with higher scores indicating higher PSNC (Table 3).
TABLE 3.
Means and Standard Deviations of Individual Items and Average at the Hospital Ward Level (N = 290)
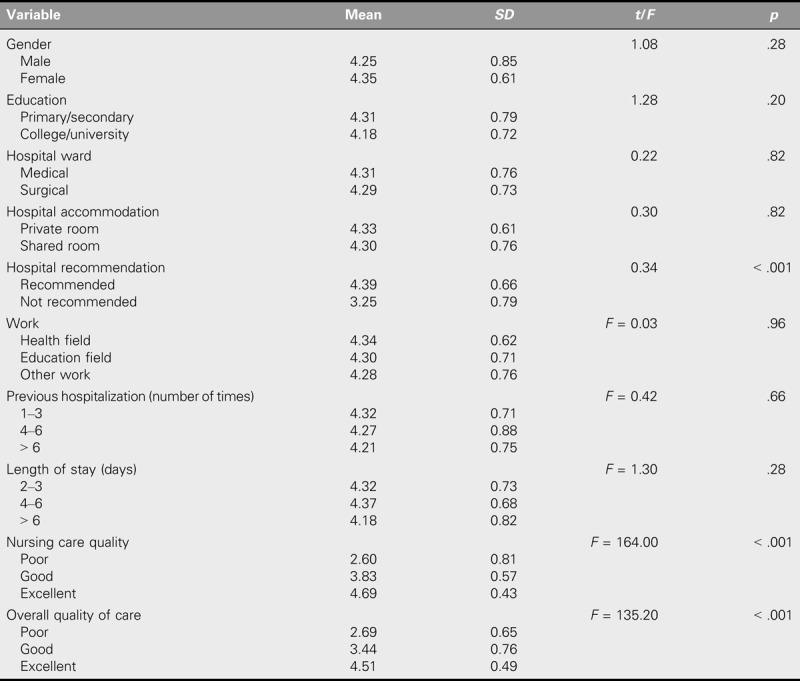
There was a significant difference in the scores of patients who recommended the hospital (M = 4.39, SD = 0.66) and those who did not recommend the hospital (M = 3.25, SD = 0.79; t = 0.34, p < .001). The overall patient satisfaction levels were statistically different in terms of perceived nursing care quality (F = 164, p < .001). Post hoc analysis (Tukey’s HSD) revealed that patients who reported excellent nursing care were more satisfied (M = 4.69, SD = 0.43) than both those who reported good nursing care (M = 3.83, SD = 0.57) and those who reported poor nursing care (M = 2.60, SD = 0.81). In addition, the overall patient satisfaction levels were statistically different in terms of the overall quality of care (F = 135.2, p < .001). Post hoc analysis (Tukey’s HSD) revealed that patients who reported excellent quality of care (M = 4.51, SD = 0.49) were more satisfied than both those who reported good quality of care (M = 3.44, SD = 0.76) and those who reported poor quality of care (M = 2.69, SD = 0.65; Table 4).
TABLE 4.
Comparison of Patient Satisfaction Levels (N = 292)
In terms of PSNC at the ward level, no significant difference was identified between medical (M = 4.31, SD = 0.76) and surgical (M = 4.29, SD = 0.73) wards (t = 0.22, p < .82).
Discussion
We sought to adapt and validate the PSNCQQ-Ar using a sample of Arabic speakers who were adult inpatients in a tertiary hospital in Oman. We employed a structured process of transcultural adaptation and used sophisticated psychometric techniques to create a scale that would be valid, reliable, and ready for use in an Arabic context.
The Cronbach’s alpha for the PSNCQQ-Ar was excellent and similar to that of both the original, English scale (Laschinger et al., 2005) and the Serbian version (Milutinović et al., 2012), suggesting that each has good internal consistency (Cronbach, 1951). For content validity, six expert raters evaluated the 17 items on a 4-point scale. Analysis revealed that none of the 17 items had an I-CVI of less than .79 and that the S-CVI/ave was above .90. Accordingly, an evidence of acceptable content validity of the PSNCQQ-Ar was supported (Polit & Beck, 2006). The former two studies of the PSNCQQ did not report evidence of obtained content validity (Laschinger et al., 2005; Milutinović et al., 2012).
Listwise deletion yielded a final sample size of 264, with over 15 subjects per item, suggesting an adequate sample size for EFA to avoid computational difficulties (Costello & Osborne, 2005; Hair, Black, Babin, & Anderson, 2010). In addition, inspection of the correlation matrix for factorability of R revealed that, although variables were intercorrelated, the correlations were not excessive (all variables were above 0.3 and below 0.8), indicating that the unique contribution of each of the 17 variables was maintained (Williams et al., 2010). Furthermore, the excellent KMO value (.96; Kaiser, 1974) and the significant result of Bartlett’s test (p < .001; Hair et al., 2010) suggested sample adequacy and appropriateness for the EFA (Tabachnick & Fidell, 2013).
Maximum likelihood factor extraction is the best method when data are relatively normally distributed because “it permits statistical significance testing of factor loadings and correlations among factors” (Fabrigar, Wegener, MacCallum, & Strahan, 1999). In addition, maximum likelihood is suggested when the intention of the EFA is to obtain interpretable factors rather than to remove items (Costello & Osborne, 2005). As the data obtained in this study were relatively normally distributed and all of the 17 items of the PSNCQQ-Ar are believed to be important in measuring PSNC, maximum likelihood factor extraction is considered appropriate for this study.
Considering the fact that oblique methods allow factors to correlate but orthogonal rotations do not, Costello and Osborne (2005) argued that orthogonal methods lead to loss of valuable data if factors being studied correlate and that oblique rotations are best when factors are believed to correlate with each other. In this study, items of the PSNCQQ-Ar belong to factors that represent the study’s concept of interest, PSNC. As an evolving concept, PSNC’s attributes are believed to reflect the perspective of patients. Obviously, correlations among PSNC factors are inevitable in this study, and therefore the oblique rotation method is more appropriate than orthogonal rotation.
Whereas the Serbian study used principal component analysis with varimax rotation method (Milutinović et al., 2012), the extraction method that was used in the original Canadian study is not known (Laschinger et al., 2005). On the basis of the findings of previous studies (Laschinger et al., 2005; Milutinović et al., 2012), we expected either a one- or two-factor model for the PSNCQQ-Ar.
Results from this study revealed a two-factor model with eigenvalues greater than 1. CFA showed that the two-factor model had better fit indices than the one-factor model. In addition, CFA revealed that Factors 1 and 2 had adequate fit indices. These findings suggest that the factor structure gleaned from the EFA fits data better than the single-factor model.
Inspection of the pattern matrix indicates that Items 3, 5, and 6 are close to the cutoff of 0.4, which is considered fair (Tabachnick & Fidell, 2013). The inability of Items 3, 5, and 6 to measure well may relate to the sample size used in this study (Tabachnick & Fidell, 2013). Another potential reason may be an insufficient level of respondent awareness of the functions that are described in these three items. The functions described in the three items are theoretically related to the job of nurses, and thus respondents may not be sufficiently cognizant of these. Although these three items did not measure well, we still believe that they make important contributions to the overall PSNC. Hence, Items 3, 5 and 6 were retained in the factor structure of the PSNCQQ-Ar.
Theoretically, Items 6–17 are believed to measure patient satisfaction with actions done by nurses. Therefore, Factor 1 could be labeled “satisfaction with provided care.” In addition, Factor 2 could be labeled “satisfaction with provided information” because Items 1–5 are believed to measure patient satisfaction with information provided by nurses.
Construct validity of the PSNCQQ-Ar was obtained by testing the correlations between PSNC and other constructs. Pearson’s correlation coefficients revealed strong associations between PSNC quality, perceived nursing care quality, and the overall quality of care in the hospital, which is consistent with the results of the original study (Laschinger et al., 2005) and of the Serbian version (Milutinović et al., 2012).
The overall mean of patient satisfaction was quite high, suggesting that patients had a good experience with nursing care. However, comparisons across hospital wards revealed no significant differences in terms of PSNC. Patients were mostly satisfied with aspects such as “concern and caring by nurses” and “attention of nurses to your condition,” suggesting that nurses pay significant attention to patient care tasks, which is the core concept of nursing. Moreover, patients were least satisfied with aspects such as “informing family or friends,” “involving family or friends in your care,” and “recognition of your opinions,” suggesting that nurses pay less attention to involving patients and their families and friends in planning and implementing nursing care. Likewise, these findings are congruent with the findings of the Canadian and Serbian studies (Laschinger et al., 2005; Milutinović et al., 2012).
Limitations
This study was conducted in one setting. Thus, the current lack of comparability between different hospitals may limit the generalizability of the findings. In addition, because of time constraints, researchers were unable to collect data on two different occasions to obtain a test–retest estimate of reliability, which would have added value to the psychometrics of the PSNCQQ-Ar. Furthermore, the electronic survey method may have introduced confounding factors because of lack of control over the sample, stakeholder bias, unverified respondents, and nonresponse bias (Duda & Nobile, 2010). However, researchers maintained the recommended measures to ensure that only eligible participants were involved in filling out the survey, that participants filled out the survey only once, and that each participant received the required instructions.
Conclusions
In view of its sound psychometric properties for content, comprehension, readability, and practicality, the PSNCQQ-Ar is a promising instrument for measuring PSNC in an Arabic context, further equipping nurses and managers with useful information related to care strengths and weaknesses and to areas that require improvement. The information provided by the PSNCQQ-Ar has the potential to help communities of interest discriminate between different care experiences at the unit and hospital levels, which may be further used in (a) planning and resource allocation at the organizational level, (b) marketing and awareness at the community level, and (c) policy development and strategic planning at the national level. In addition, the PSNCQQ-Ar may be useful in better understanding how patients perceive what nurses actually do. Furthermore, the results of this study may serve as baseline data for future quality improvement projects and research in Oman and the Middle East.
We recommend applying the PSNCQQ-Ar in different settings and using electronic as well as traditional survey methods to collect data. In addition, we recommend using test–retest estimates of reliability. Moreover, we recommend further validation studies of the PSNCQQ-Ar to standardize this instrument for general use in Oman and across the Middle East. For Oman in particular, we recommend that healthcare stakeholders adopt the PSNCQQ-Ar to measure PSNC quality, to identify differences among hospitals, and to facilitate further improvements in quality of care.
Acknowledgments
This work was supported by a grant from Sultan Qaboos University (IG/CON/DEAN/15/01). All of the authors would like to acknowledge Sultan Qaboos University for supporting this study and facilitating its conduct. Furthermore, authors would like to thank all of the patients and research assistants for their time and efforts taken to make this study successful.
Footnotes
Accepted for publication: January 2, 2018
The authors declare no conflicts of interest.
Cite this article as: Albashayreh, A., Al-Rawajfah, O. M., Al-Awaisi, H., Karkada, S., & Al Sabei, S. D. (2019). Psychometric properties of an arabic version of the patient satisfaction with nursing care quality questionnaire. The Journal of Nursing Research, 27(1), e1. https://doi.org/10.1097/jnr.0000000000000273
References
- Abdel Maqsood A. S., Oweis A. I., Hasna F. S. (2012). Differences between patients’ expectations and satisfaction with nursing care in a private hospital in Jordan. International Journal of Nursing Practice, 18(2), 140–146. 10.1111/j.1440-172X.2012.02008.x [DOI] [PubMed] [Google Scholar]
- Al-Abri R., Al-Balushi A. (2014). Patient satisfaction survey as a tool towards quality improvement. Oman Medical Journal, 29(1), 3–7. 10.5001/omj.2014.02 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alasad J., Abu Tabar N., AbuRuz M. E. (2015). Patient satisfaction with nursing care: Measuring outcomes in an international setting. The Journal of Nursing Administration, 45(11), 563–568. 10.1097/NNA.0000000000000264 [DOI] [PubMed] [Google Scholar]
- Atallah M. A., Hamdan-Mansour A. M., Al-Sayed M. M., Aboshaiqah A. E. (2013). Patients’ satisfaction with the quality of nursing care provided: The Saudi experience. International Journal of Nursing Practice, 19(6), 584–590. 10.1111/ijn.12102 [DOI] [PubMed] [Google Scholar]
- Campbell D. T., Fiske D. W. (1959). Convergent and discriminant validation by the multitrait-multimethod matrix. Psychological Bulletin, 56(2), 81–105. 10.1037/h0046016 [DOI] [PubMed] [Google Scholar]
- Castro E. M., Van Regenmortel T., Vanhaecht K., Sermeus W., Van Hecke A. (2016). Patient empowerment, patient participation and patient-centeredness in hospital care: A concept analysis based on a literature review. Patient Education and Counseling, 99(12), 1923–1939. 10.1016/j.pec.2016.07.026 [DOI] [PubMed] [Google Scholar]
- Costello A. B., Osborne J. W. (2005). Best practices in exploratory factor analysis: Four recommendations for getting the most from your analysis. Practical Assessment, Research & Evaluation, 10(7), 1–9. [Google Scholar]
- Cronbach L. J. (1951). Coefficient alpha and the internal structure of tests. Psychometrika, 16(3), 297–334. 10.1007/BF02310555 [DOI] [Google Scholar]
- de-la-Cueva-Ariza L., Romero-García M., Delgado-Hito P., Acosta-Mejuto B., Jover-Sancho C., Ricart-Basagaña M. T., Solà-Ribó M. (2014). Development of an instrument to measure the degree of critical patient’s satisfaction with nursing care: Research protocol. Journal of Advanced Nursing, 70(1), 201–210. 10.1111/jan.12184 [DOI] [PubMed] [Google Scholar]
- Duda M. D., Nobile J. L. (2010). The fallacy of online surveys: No data are better than bad data. Human Dimensions of Wildlife, 15(1), 55–64. 10.1080/10871200903244250 [DOI] [Google Scholar]
- Dudkiewicz P. B. (2014). Utilizing a caring-based nursing model in an interdepartmental setting to improve patient satisfaction. International Journal for Human Caring, 18(4), 30–33. 10.20467/1091-5710-18.4.30 [DOI] [Google Scholar]
- Eriksen L. R. (1995). Patient satisfaction with nursing care: Concept clarification. Journal of Nursing Measurement, 3(1), 59–76. [PubMed] [Google Scholar]
- Fabrigar L. R., Wegener D. T., MacCallum R. C., Strahan E. J. (1999). Evaluating the use of exploratory factor analysis in psychological research. Psychological Methods, 4(3), 272–299. 10.1037/1082-989X.4.3.272 [DOI] [Google Scholar]
- Freitas J. S., Silva A. E., Minamisava R., Bezerra A. L., de Sousa M. R. (2014). Quality of nursing care and satisfaction of patients attended at a teaching hospital. Revista Latino-Americana de Enfermagem, 22(3), 454–460. 10.1590/0104-1169.3241.2437 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gjersing L., Caplehorn J. R., Clausen T. (2010). Cross-cultural adaptation of research instruments: Language, setting, time and statistical considerations. BMC Medical Research Methodology, 10, 13 10.1186/1471-2288-10-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hair J. F., Jr., Black W. C., Babin B. J., Anderson R. E. (2010). Multivariate data analysis (7th ed.) Retrieved from https://www.pearsonhighered.com/program/Hair-Multivariate-Data-Analysis-7th-Edition/PGM263675.html [Google Scholar]
- Hu L. t., Bentler P. M. (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal, 6(1), 1–55. [Google Scholar]
- Junewicz A., Youngner S. J. (2015). Patient-satisfaction surveys on a scale of 0 to 10: Improving health care, or leading it astray? The Hastings Center Report, 45(3), 43–51. 10.1002/hast.453 [DOI] [PubMed] [Google Scholar]
- Kaiser H. F. (1974). An index of factorial simplicity. Psychometrika, 39(1), 31–36. 10.1007/BF02291575 [DOI] [Google Scholar]
- Koy V., Yunibhand J., Angsuroch Y. (2016). The quantitative measurement of nursing care quality: A systematic review of available instruments. International Nursing Review, 63(3), 490–498. 10.1111/inr.12269 [DOI] [PubMed] [Google Scholar]
- La Monica E. L., Oberst M. T., Madea A. R., Wolf R. M. (1986). Development of a patient satisfaction scale. Research in Nursing & Health, 9(1), 43–50. 10.1002/nur.4770090108 [DOI] [PubMed] [Google Scholar]
- Laschinger H. S., Hall L. M., Pedersen C., Almost J. (2005). A psychometric analysis of the patient satisfaction with nursing care quality questionnaire: An actionable approach to measuring patient satisfaction. Journal of Nursing Care Quality, 20(3), 220–230. [DOI] [PubMed] [Google Scholar]
- Linder-Pelz S. U. (1982). Toward a theory of patient satisfaction. Social Science & Medicine, 16(5), 577–582. 10.1016/0277-9536(82)90311-2 [DOI] [PubMed] [Google Scholar]
- Milutinović D., Simin D., Brkić N., Brkić S. (2012). The patient satisfaction with nursing care quality: The psychometric study of the Serbian version of PSNCQ questionnaire. Scandinavian Journal of Caring Sciences, 26(3), 598–606. 10.1111/j.1471-6712.2012.00969.x [DOI] [PubMed] [Google Scholar]
- Pascoe G. C. (1983). Patient satisfaction in primary health care: A literature review and analysis. Evaluation and Program Planning, 6(3–4), 185–210. 10.1016/0149-7189(83)90002-2 [DOI] [PubMed] [Google Scholar]
- Polit D. F., Beck C. T. (2006). The content validity index: Are you sure you know what’s being reported? Critique and recommendations. Research in Nursing & Health, 29(5), 489–497. 10.1002/nur.20147 [DOI] [PubMed] [Google Scholar]
- Schermelleh-Engel K., Moosbrugger H., Müller H. (2003). Evaluating the fit of structural equation models: Tests of significance and descriptive goodness-of-fit measures. Methods of Psychological Research Online, 8(2), 23–74. [Google Scholar]
- Schumacker R. E., Lomax R. G. (2004). A beginner’s guide to structural equation modeling (2nd ed.) Mahwah, NJ: Taylor & Francis. [Google Scholar]
- Sousa V. D., Rojjanasrirat W. (2011). Translation, adaptation and validation of instruments or scales for use in cross-cultural health care research: A clear and user-friendly guideline. Journal of Evaluation in Clinical Practice, 17(2), 268–274. 10.1111/j.1365-2753.2010.01434.x [DOI] [PubMed] [Google Scholar]
- Tabachnick B. G., Fidell L. S. (2013). Using multivariate statistics (6th ed.). Boston, MA: Pearson. [Google Scholar]
- Thomas L. H., McColl E., Priest J., Bond S., Boys R. J. (1996). Newcastle satisfaction with nursing scales: An instrument for quality assessments of nursing care. BMJ Quality & Safety, 5(2), 67–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams B., Onsman A., Brown T. (2010). Exploratory factor analysis: A five-step guide for novices. Journal of Emergency Primary Health Care, 8(3), Article 990399. [Google Scholar]


