ABSTRACT
Background:
Coronary artery disease (CAD) is a leading cause of death in women. Many of the risk factors for CAD relate to lifestyle and thus may be influenced by lifestyle modification. However, middle-aged women often find it difficult to adjust their lifestyle behaviors. Thus, providing individualized treatment is crucial to reducing the risk and incidence of CAD in this population.
Purpose:
The aim of this study was to explore the effectiveness of a tailored lifestyle management program (TLMP) for middle-aged women with CAD.
Methods:
An experimental design was employed. Thirty-five middle-aged women with CAD (with stenosis [> 50%] of at least one main artery as determined by cardiac catheterization examination results) were recruited. The 35 women were randomlyassigned to the experimental group (n = 17) or the control group (n = 18). Both groups received regular health education during their hospitalization. After discharge, the experimental group received the 12-week, home-based TLMP. A generalized estimating equation was used to examine the effects of the TLMP on metabolic and biomarker indicators for CAD.
Results:
The average age of participants was 56.1 ± 5.6 years. No significant demographic differences were identified between the two groups. Compared with the control group, the experimental group had a significantly higher high-density lipoprotein level (B = 7.83, p < .001), a lower level of total cholesterol (B = −49.21, p = .04), and a lower waist circumference (B = −6.42, p < .001).
Conclusions/Implications for Practice:
This study suggests that using tailored interventions is an effective approach to improving high-density lipoprotein, total cholesterol, and waist circumference in middle-aged women with CAD. This result is expected to have important implications for women’s healthcare, particularly in terms of preventing the incidence of CAD.
Key Words: lifestyle management, middle-aged women, coronary artery disease
Introduction
Coronary artery disease (CAD) is the leading cause of death in women worldwide (World Health Organization, 2016). In Taiwan, heart disease is the second leading cause of death in women aged 45–64 years (Ministry of Health and Welfare, Taiwan, ROC, 2017). Even with drug and/or invasive treatments, patients with CAD may still experience coronary occlusion or other cardiovascular diseases. A systematic review study found that 4%–30% of patients continue to experience coronary occlusion 1 year after coronary stent implantation (Bennett & Dubois, 2013). In a previous study (in which 62% of the interviewees were adult women, of whom 72% were aged 45–59 years), three fourths of the adult interviewees were unaware that most risk factors for CAD were preventable. In addition, some patients with diabetes mellitus and smokers in the study did not believe that they faced a higher risk of developing CAD than their peers without diabetes mellitus/nonsmoking peers of the same age (Chen, Yu, & Glaser, 2009). Therefore, preventing CAD is extremely crucial for middle-aged women in Taiwan. Traditional cardiac rehabilitation (CR) programs disregard gender differences. Although many previous studies indicate that CR affects both men and women with CAD similarly (Angus et al., 2015), some studies have found different effects on men and women as well as on individuals in different age groups (Kent et al., 2014; Lavie & Milani, 2006). Thus, it has been suggested that gender differences should be considered when developing CR programs (Kent et al., 2014).
The American Heart Association (AHA) has identified women as a risk group for CAD and emphasized that a healthy lifestyle is crucial for women’s health (Mosca et al., 2007). As indicated in the 2011 AHA guidelines, people without risk factors and with healthy lifestyles are classified as the low-risk group, which is defined to include people with a total cholesterol (TC) of < 200 mg, blood pressure (BP) of < 120/80 mmHg, fasting blood sugar (FBS) of < 100 mg/dl, and a body mass index of < 25 kg/m2. Furthermore, people in this group should be nonsmokers, perform moderate-intensity exercise for ≥ 150 minutes per week or vigorous-intensity exercise for ≥ 75 minutes per week, and control their diet (Mosca et al., 2011). However, maintaining a healthy lifestyle is more challenging for women than men. It is typically difficult for women to change their lifestyle behaviors because of older age, transportation, low social status, low self-efficacy, and lack of spousal support (Grace, Racco, Chessex, Rivera, & Oh, 2010). Therefore, effective and flexible strategies should be applied to help women adjust their lifestyle behaviors to improve their overall health and reduce CAD risk factors.
In comparison with conventional CR, tailored intervention programs have been shown to enhance participation and completion rates for women and may thus be more ideal and effective (Beckie & Beckstead, 2010). The definition of a tailored intervention is an intervention that has been designed according to personal characteristics such as personality traits, objectives, needs, preferences, and resources. Although better compliance rates, results, and cost-effectiveness have been observed, executing tailored interventions is more complicated than conventional CR programs (Beck et al., 2010). It is a common strategy in effective health education to use pattern theories of behavioral change such as the social cognitive theory, transtheoretical model, and health belief model, which incorporate face-to-face motivational discussions with patients. By exploring and solving psychological contradictions, intrinsic motivation is initiated, which enhances the change and maintenance of healthy behavior (Wanyonyi, Themessl-Huber, Humphris, & Freeman, 2011). The AHA (2010) suggested using cognitive–behavioral intervention processes or delivery and addressing cultural and social context strategies to help people change their lifestyles (as cited in Artinian et al., 2010). As motivation is a crucial factor in helping women undertake lifestyle changes, physicians should begin interacting with patients during hospitalization to establish mutual trust and involve patient family members and spouses in the process to provide social support. Because home-based programs are highly flexible and feasible, they are better able to encourage women to follow healthy lifestyles and may be employed together with supportive strategies such as self-management and counseling (Beswick et al., 2005).
According to the findings of a previous systematic review study of 65 population-based studies between 1980 and 1998, women may reduce their BP, body weight (BW), FBS, TC, and triglyceride (TG) levels and raise their fiber intake and high-density lipoprotein (HDL) level by changing their diet, increasing physical activity, and/or quitting smoking, thus increasing cardiovascular health. In the future, tailored lifestyle-changing programs should be developed for women according to the various stages of the life cycle (Krummel et al., 2001). Two recent studies conducted randomized controlled trials on women with CAD using a new program that combined conventional CR with motivational discussion and a 10-week psychological education course (1 hour per week). Results revealed that the new program enhanced the participation rate in exercise and education courses significantly and improved inflammatory biomarkers and indicators of metabolic syndrome (MS) more effectively than a conventional CR program (Beckie, Beckstead, & Groer, 2010; Beckie, Beckstead, Kip, & Fletcher, 2013). However, the research targets in the aforementioned studies were not restricted to middle-aged women. Regardless of their employment status, middle-aged women are typically responsible for attending to the older adults, children, and other family members and thus often ignore their own health problems (Papakonstantinou, Stamou, Baikoussis, Goudevenos, & Apostolakis, 2013). A previous study indicated that participation rates of women in CR programs are typically lower than those of men (Artinian et al., 2010). In addition, institutional interventions only satisfy the needs of a limited number of people. Therefore, home-based programs that are tailored to the lifestyle of individual participants represent a feasible and potentially effective alternative.
In Taiwan, most patients with CAD receive a standard health education program that comprises a single health education handout and oral explanations during their short period of hospitalization. Moreover, only 6.7%–18.9% of patients with myocardial infarction and patients who have received heart surgery in medical centers participate in a CR program after hospital discharge (Hung, Hung, Chou, & Chen, 2014; Liu, Chen, Hung, & Chou, 2013). To our knowledge, this study is the first to investigate the effectiveness of a home-based tailored lifestyle management program (TLMP) in middle-aged women with CAD. The purpose of this study was to explore the effects of a TLMP on the primary CAD risk factors for this population, with a particular focus on metabolic and biomarker factors.
Methods
Participants and Group Assignments
An experimental design was employed. Patients at cardiology wards in two medical centers in Taipei City, Taiwan, were recruited as participants between February 2010 and September 2014. The research targets were women who had experienced coronary artery stenosis (> 50%) in at least one of the following major coronary arteries: left anterior descending artery, left circumflex artery, and right coronary artery. The inclusion criteria for participants were as follows: (a) aged 40–64 years, (b) able to communicate, (c) met the criteria for Levels I–III on the New York Heart Association Functional Classification, (d) have a left ventricular ejection fraction of > 30%, (e) have no history of severe arrhythmia (e.g., ventricular tachycardia or complete atrioventricular block), and (f) are not planning to receive surgery (e.g., coronary artery bypass graft). The exclusion criteria were patients (a) who had received a medical diagnosis of a severe disease such as cancer, mental disorders, systemic inflammatory disease, or end-stage renal disease; (b) who had received in the past 2 weeks a severe infection, injury, or surgery; (c) who did not live in Taipei after hospital discharge; and (d) whose physical activity was influenced by neurological, respiratory, skeletal, or peripheral vascular disease.
Two hundred forty-six women aged 40–64 years who were suspected of having CAD were referred by physicians to the researcher of this study. According to the examination results, 88 women (35.8%) were experiencing coronary artery stenosis in at least one major coronary artery (> 50%). Among these, 10 did not meet the inclusion criteria and eight met the exclusion criteria. Therefore, 70 women (79.5%) met the inclusion criteria. However, 35 of these women refused to participate for reasons that included inconvenience, a lack of free time, physical discomfort, or family members’ disapproval. Thus, 35 women (50%) were enrolled as participants. No significant difference in terms of age, number of stenotic coronary arteries, or the presence of left ventricular ejection fraction was identified between the 35 participants and the 35 women who had refused to participate (p > .05).
First, a statistician who was not otherwise involved in this study fabricated a random number table using the ratio of the experimental group to the control group (1:1) and a block size of 10. Subsequently, according to the random number table, sealed envelopes were produced. After the 35 participants had completed the pretest, the researcher opened the sealed envelopes one by one and randomly assigned each participant to the experimental or the control group based on the designation specified in each envelope. The experimental and control groups consisted of 17 and 18 participants, respectively. During the study period, one participant in the experimental group discontinued her participation because she moved out of Taipei and one participant in the control group did not complete the posttest. In the study, the intention-to-treat method was applied, and all data collected from the 35 participants were analyzed (Figure 1).
Figure 1.
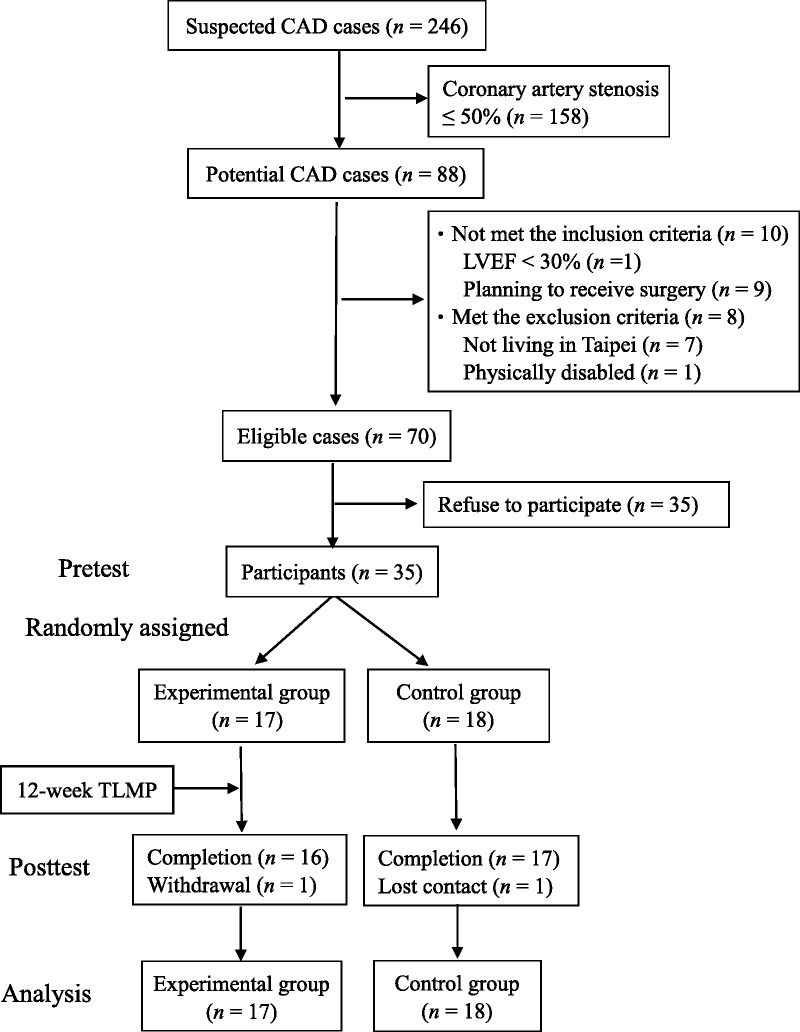
Participation flowchart. CAD = coronary artery disease; LVEF = left ventricular ejection fraction; TLMP = tailored lifestyle management program.
Tailored Lifestyle Management Program
The TLMP comprises three parts: the motivational discussion, the lifestyle adjustment plan, and self-management and follow-ups. During the motivational discussion, the researcher-developed manual Methods for Preventing Cardiovascular Diseases: Living a Healthy Lifestyle was used to frame a discussion with participants regarding how their current lifestyle varied from a more ideal lifestyle. During the lifestyle adjustment plan, the items that related to the unhealthy lifestyle behaviors of each participant, which were extracted from pretest data, were identified. The researcher then encouraged the participants to implement changes, set personal goals, and take personal responsibility to live a healthy lifestyle to fulfill the objective of tailored and individualized intervention. Finally, for self-management and follow-ups, participants were taught to record the execution statuses of changes in their lifestyle behavior, BP, blood glucose level, and BW to provide a reference for subject assessment and self-management. The researcher called participants regularly (once per week during Weeks 1–4 and once every 2 weeks during Weeks 5–12, for a total of eight times). In addition, the researcher made a 24-hour consultation line available to participants to provide timely assistance.
The participants in the experimental group received all three parts of the TLMP intervention. However, the lifestyle adjustment plan is a tailored and individualized plan.
Measurements
A structured questionnaire was used to obtain basic information. The researcher reviewed the relevant medical records and collected disease information, including data from a cardiac catheterization examination and a list of prescribed medications.
Regarding metabolic markers, the researcher reviewed medical records and determined FBS levels, systolic BP (SBP), diastolic BP (DBP), TG levels, HDL levels, low-density lipoprotein levels, TC levels, body height (BH), and BW. Pretest data were collected from data obtained upon the hospitalization of the participants or from their most recent clinical visit, which needed to have been taken within 6 months of hospitalization. Posttest data were collected after the completion of the intervention treatment and at the closest time possible to the last telephone call. The formula for calculating the body mass index was as follows: (BW; kg)/ (BH; m)2. The research assistant used a ruler with a minimum unit of 0.1 cm to measure the waist circumference (WC) and hip circumference (HC) of the participants. In measuring the WC, the participant was asked to stand and wear a minimal number of clothes. The WC measurement point was the midpoint between the upper edge of the ilium and the lower edge of the rib cage, and measurements were taken at the end of exhalation. The HC was measured as the widest width of the hip. The formula for calculating the waist–hip ratio was as follows: WC / HC. Before formal data collection, the WC and HC of 15 volunteers were measured three times, with intraclass correlation coefficients of .94 (WC) and .95 (HC).
The biological indicators included levels of high-sensitivity C-reactive protein (hsCRP), homocysteine (Hcy), and leptin. Blood samples for the pretest were collected before cardiac catheterization, and blood samples for the posttest were collected after the intervention treatment was completed. After fasting, 6 ml of a blood sample was collected and equally divided into two test tubes, with each tube containing 3 ml of a blood sample. One of the 3ml blood samples contained ethylenediaminetetraacetic acid, and the other contained gel. The blood samples were centrifuged in a hospital laboratory, stored in a refrigerator at 4°C, and then sent within 24 hours of collection to an accredited government laboratory for analysis. A latex-enhanced immunoturbidimetric analysis was used to examine hsCRP levels (Siemens ADVIA 1800, Tarrytown, NY, USA). The analytical range was 0.12–164 mg/L, with any figure < 0.12 mg/L recorded as 0.12 mg/L. A chemiluminescence assay (Siemens ADVIA Centaur, Tarrytown, NY, USA) was used to examine Hcy levels. The analytical range was 0.5–65 μmol/L. An enzyme-linked immunosorbent assay was used to examine leptin levels (Bio-Rad CODA, St. Louis, MO, USA). The analytical range was 0.5–100 ng/ml. The coefficients of variation for hsCRP, Hcy, and leptin levels were 1.36%, 6.26%, and 6.34%, respectively.
Data Collection
This study was approved by the institutional review boards of two research institutions (institutional review board numbers TMU-JIRB-99001 and FEMH-IRB-099073-E). All of the pretest and posttest data were collected by the same well-trained research assistant. The study purpose was explained to participants who met the selection criteria, signed consent was obtained from participants, and then pretest data were collected from participants during their hospitalization period. Subsequently, the first author, a registered nurse with over 20 years of cardiology experience, opened the sealed envelopes and randomly assigned each participant to either the experimental group or the control group according to the designation contained in the envelope. Both groups received the standard health education program from hospital staffs during hospitalization. After hospital discharge, the experimental group received 90- to 150-min TLMPs for 1–3 weeks, followed by a 12-week telephone follow-up survey and consultation service (eight calls in total, with each call lasting approximately 30 minutes) that the researchers used to assess TLMP effectiveness and to address participant questions. Participants in the control group were asked to maintain their normal lifestyle. A 12-week telephone follow-up survey (eight calls in total, with each call lasting approximately 10 minutes) was conducted, with survey questions largely related to cardiac catheterization wounds, drug side effects, and other symptoms. The two groups received treatment separately after being discharged from the hospital and visited the hospitals at different times. Therefore, neither medical professionals nor participants were aware of which group they belonged to. The research assistant collected the posttest data after completion of the 12-week telephone survey. The pretest and posttest data collection items and methods were identical. During the posttest data collection period, the research assistant was still unaware of the group assignments of participants. To protect the right of the participants in the control group to receive beneficial treatment, this study provided this group with 90- to 150-min instructions on the TLMP upon completion of the posttest.
Data Analysis
The SPSS 20.0 (IBM Corporation, Armonk, NY, USA) software package was used for data analysis. A chi-squared test (Fisher’s exact test was performed if a predictive value was < 5) and a Mann–Whitney U test were performed to compare the basic information of the experimental and control groups. To assess the effectiveness of the TLMP, a generalized estimating equation (GEE) was used to assess the differences in pretest–posttest changes between the two groups. Before performing the GEE analysis, Little’s missing completely at random test was performed, with results showing that all variables met the missing completely at random assumption (p > .05). In addition, a P–P plot test and a Kolmogorov–Smirnov test were performed, with results indicating that none of the FBS, TG, BW, hsCRP, or leptin levels was normally distributed (p < .05). Accordingly, we converted the aforementioned variables into a natural logarithm and then performed the GEE analysis. Afterward, the regression coefficient B value was converted into a natural logarithm. In accordance with previous studies, the effect size (ES) of increasing motivational interviewing to initiate a healthy lifestyle reached 0.84 (Artinian et al., 2010). Thus, ES = 0.84, alpha = .05, and power = 0.8 were used in this study, with a sample size of 48 participants (24 in each group).
Results
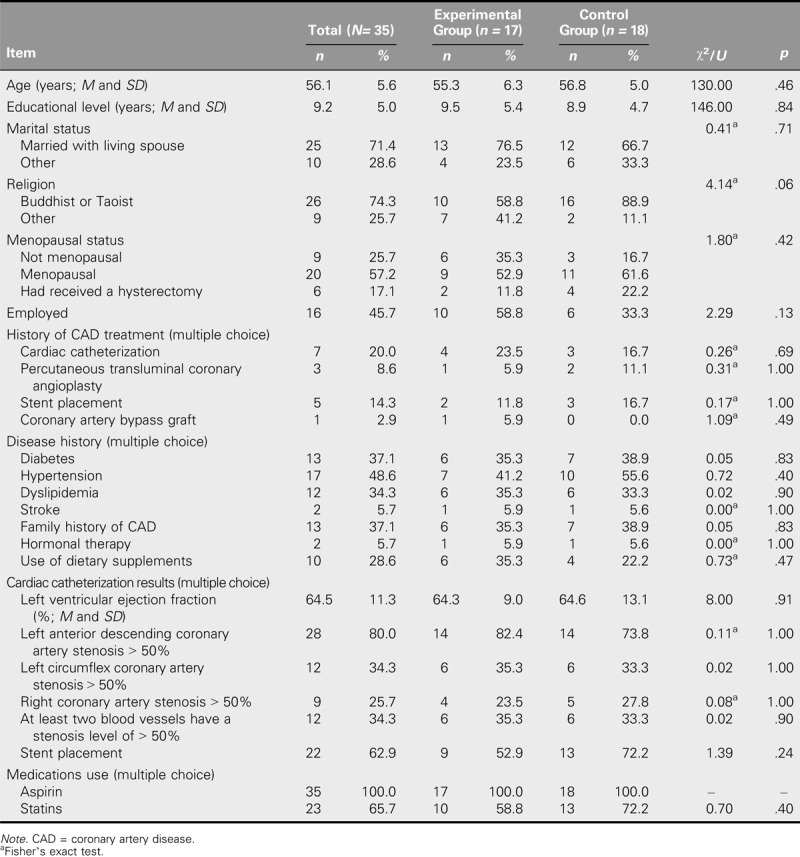
The average age of the 35 participants was 56.1 ± 5.6 years. All of the participants used aspirin, and 65.7% used statins. According to the chi-squared test and Mann–Whitney U test results, no significant difference in demographic variables existed between the two groups (p > .05; Table 1).
TABLE 1.
Demographic Information for the Experimental and Control Groups
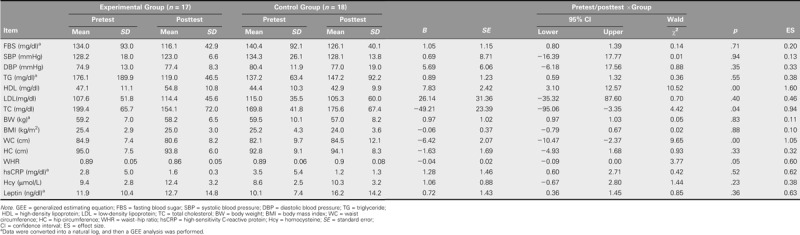
In Table 2, according to the GEE interaction analysis, significant differences existed between the experimental and control groups regarding differences between the pretest and posttest data for HDL levels, TC, and WC (p < .05). After the experimental group had implemented the TLMP, the HDL level (B = 7.83) significantly increased and TC (B = −49.21) and WC (B = −6.42) decreased. The average HDL level of the experimental group increased from 47.1 mg/dl (pretest) to 54.8 mg/dl (posttest), whereas that of the control group decreased from 44.4 mg/dl (pretest) to 42.9 mg/dl (posttest). After controlling for the pretest values and growth effect, the difference in pretest–posttest data for the experimental group was 7.83 mg/dl higher than for the control group; Cohen’s d was 1.6. The average TC of the experimental group dropped from 199.4 mg/dl (pretest) to 154.1 mg/dl (posttest), whereas that of the control group increased from 169.8 mg/dl (pretest) to 175.6 mg/dl (posttest). The difference in pretest–posttest data for the experimental group was 49.21 mg/dl lower than for the control group; Cohen’s d was 0.94. The average WC of the experimental group dropped from 84.9 cm (pretest) to 80.6 cm (posttest), whereas that of the control group increased from 82.1 cm (pretest) to 84.5 cm (posttest). The difference in pretest–posttest data for the experimental group was 6.42 cm less than for the control group; Cohen’s d was 1.05. No significant improvements in biological indicators were observed.
TABLE 2.
GEE Analyses of the Metabolic and Biological Indicators: Pretest and Posttest
Discussion
This study explored the effectiveness of a home-based TLMP. The results showed that HDL levels had increased and the TC and WC had significantly decreased after completion of the TLMP intervention. These findings echo those of previous studies on middle-aged women with CAD who had received 12-week institutional intervention treatments (Beckie et al., 2013; Daubenmier et al., 2007). A prospective long-term study on women showed that following a healthy lifestyle frequently substantially reduces CAD mortality and enhances the dose–response relationship (Petersen et al., 2015). Changes in the lipid profile are related to lifestyle. Adjusting alcohol intake and dietary patterns, undertaking regular exercise, and quitting smoking have been shown to increase HDL levels and reduce CAD risk. However, as these methods produce multiple effects, the effect of a single method cannot be easily identified (Escolá-Gil, Julve, Griffin, Freeman, & Blanco-Vaca, 2015). According to one systematic review, CR increased HDL levels by 6%–16% and reduced TC by 5% (Lavie, Thomas, Squires, Allison, & Milani, 2009). These findings accorded with those of our study, which determined that HDL levels increased by 16.3% and TC decreased by 22.7%. Savage, Brochu, and Ades (2004) compared the results of men and women in terms of differences in the HDL levels measured before and after CR and found that women exhibited a significantly higher increase in HDL levels than men (14% vs. 7.1%, p < .0001). The reason may be that the obesity indicator also improved after CR for women. The WC and the percentage of fat mass in women are highly positively correlated (r = .82, p = .0001; Jaeschke, Steinbrecher, & Pischon, 2015). Adipose tissue is known to affect lipid metabolism and reduce HDL functioning (Escolá-Gil et al., 2015). Jaeschke et al. (2015) reported a significantly negative correlation in women between WC and HDL level (r = −.49, p = .005). This study found a slightly negative correlation between these two variables (r = −.27, p = .15 for the pretest; r = −.35, p = .19 for the posttest; data not shown). In this study, after completing the TLMP, the experimental group’s WC decreased by 6.42 cm (−5.1%). In other words, women in the experimental group became less obese, a result that may partially account for their reduced blood lipid levels.
MS is closely related to the occurrence of CAD. The prevalence of MS worldwide is 10%–40%, and MS is a multiplex risk factor for CAD, with obesity as its main cause (Grundy, 2016). According to the Ministry of Health and Welfare in Taiwan, the definition of MS is (a) having a WC of ≥ 80 cm, (b) requiring the use of BP-lowering drugs (SBP of ≥ 130 mmHg and/or DBP of ≥ 85 mmHg), (c) requiring the use of hypoglycemic drugs (and/or an FBS level of ≥ 100 mg/dl), (d) an HDL level of < 50 mg/dl, and (e) a TG level of ≥ 150 mg/dl. A woman is diagnosed with MS if she meets three of the aforementioned five conditions. The prevalence of MS in Taiwanese women aged ≥ 20 years is 19.3% (Ministry of Health and Welfare, Taiwan, ROC, 2007). Changing one’s lifestyle may improve his or her metabolism. A systematic review indicated that CR reduced the occurrence of MS by 37% (Lavie et al., 2009). According to a meta-analysis of previous studies, adjusting one’s lifestyle reduced WC by 2.7 cm, SBP by 6.4 mmHg, DBP by 3.3 mmHg, FBS levels by 11.5 mg/dl, and TG levels by 12 mg/dl and increased HDL levels by 1.3 mg/dl (Yamaoka & Tango, 2012). This study determined that adjusting one’s lifestyle reduced WC and increased HDL levels. Although adjusting one’s lifestyle did not significantly improve TG levels, after implementation of the TLMP, the average TG level of the experimental group dropped by 57.1 mg/dl, that is, from 176.1 mg/dl at pretest to 119 mg/dl at posttest. Therefore, implementation of the TLMP also contributed to improving MS.
From 1997 to 2007, the AHA investigated how a lifestyle-adjusting intervention in adults affected their risk factors for CAD. According to a systematic review, a weight reduction program with motivational discussion produced the maximal effect (ES = 0.84), whereas other methods (e.g., education, diet, exercise) produced limited effects (ES = 0.1–0.33; Artinian et al., 2010). Previous studies have indicated that women tend to feel stressed and anxious when participating in a CR program and therefore require substantial social and emotional support and prefer to undertake their favorite types of exercise (Angus et al., 2015). Moreover, the content of intervention treatment, the duration of the intervention, the frequency of follow-up surveys, and the compliance rate may all affect the effectiveness of an intervention program (Strid, Lingfors, Fridlund, & Mårtensson, 2012). In this study, despite the relatively small sample size, the ES of the intervention treatment reached levels as high as 0.94–1.6. The TLMP applied in this study was a home-based program, and participants were highly motivated to participate. In addition, the content of the intervention treatment was tailored for individual participants, the strategies adopted were diverse, and the frequency of follow-up surveys was high. For example, the researcher established an excellent, trusting relationship with participants and their family members when holding motivational discussions and providing health education. Thus, the support and encouragement of family members helped the participants change their lifestyles. The home-based, individualized suggestions addressed the needs of each participant and were thus more easily integrated into their daily lives. In the TLMP, participants were taught self-relaxation techniques and how to monitor their physiological status. Over a 12-week period, the researcher telephoned the participants at least eight times, and participants were advised that they could contact the researcher at any time. The follow-up procedures motivated participants to overcome difficulties, clarify their questions, and relieve pressures, whereas the long-term interactions helped the researcher establish a professional relationship with participants and increase their compliance. Previous studies have shown that home-based programs and institutional CR have similar effects. However, the compliance rate in these studies was higher for home-based programs than for an institutional CR program (Taylor et al., 2015). Although the compliance rate was not monitored in this study, only one participant did not complete the program (because of a change in residence). All of the remaining participants completed the 12-week, home-based CR and follow-up survey.
Previous studies have shown that CR significantly reduces hsCRP, SBP, DBP, and FBS levels in women (Beckie et al., 2010, 2013; Daubenmier et al., 2007). However, this study did not show similar results. In this study, although patients who experienced systemic inflammatory diseases or had serious infections, injuries, or surgery in the previous 2 weeks were excluded, numerous other factors that may influence biomarker levels in blood could not be excluded. Previous studies have reported that the effectiveness of a lifestyle management program is proportional to the baseline value before the intervention (Kent et al., 2014; Razavi et al., 2014). In this study, for the experimental and control groups, the SBP, DBP, and FBS values were not markedly higher than average values. In addition, physicians adjusted medications according to patient conditions in outpatient services, leading to a medical compliance level of 80%. Therefore, the relatively nonsignificant improvements in SBP, DBP, and FBS levels may have been caused by a floor effect. In addition, in this study, 20% of participants had received cardiac catheterization, both the experimental and control groups received regular health education during their hospitalization, and after hospital discharge, both groups received telephone call follow-ups for 12 weeks, all of which may have resulted in decreasing the difference in the measured factors between the two groups.
Because no previous study has examined the effectiveness of CAD secondary prevention in middle-aged women, the present results may provide a reference for future studies. This preliminary study confirmed the clinical applicability of home-based, client-tailored programs. Larger samples and longer-term follow-ups are necessary to verify the benefits of the intervention on metabolic status. The predominant focus of women’s health concerns on the prevention of breast and cervical cancers has largely overlooked the potential that gender differences affect other disease categories. It is recommended that the potential effects of gender on disease risk and treatment be taught as part of the regular medical education curriculum to enhance the concept of CAD prevention for middle-aged women, especially in terms of implementing and maintaining healthy lifestyles to achieve early detection and prevention of CAD in women.
Limitations
Although the statistical powers based on the four outcome indicators that reached significant differences were between 0.77 and 0.99, with an average of 0.87, the small sample size of this study may have affected the applicability and generalizability of results. Moreover, as the participants comprised only middle-aged women with CAD in northern Taiwan, the research results should not be generalized to other groups. In addition, not monitoring the rate of TLMP compliance may have caused an overestimation or underestimation of program effectiveness. In the future, researchers should use dietary records and exercise logs to closely monitor participant compliance. Because of the limited research budget and regulations on paying National Health Insurance examination fees, metabolic indexes were collected from medical records, which resulted in large variations in collection duration, which also may have influenced the results.
Conclusion
The home-based TLMP is an effective intervention for helping middle-aged women live a healthy lifestyle and improve their HDL levels, TC, and WC. Women should be encouraged to live a healthy lifestyle to reduce the risk factors and occurrence of CAD.
Acknowledgments
This study was supported by Grant NSC98-2314-B-038-021-MY3 from the National Science Council/Ministry of Science and Technology, Taiwan, ROC.
Footnotes
Accepted for publication: October 16, 2017
The authors declare no conflicts of interest.
Cite this article as: Tsai, C. C., Li, A. H., Tu, C. M., Hwang, K. L., & Jeng, C. (2019). Effectiveness of a tailored lifestyle management program for middle-aged women with coronary artery disease: A preliminary study. The Journal of Nursing Research, 27(1), e5. https://doi.org/10.1097/jnr.0000000000000271
References
- Angus J. E., King-Shier K. M., Spaling M. A., Duncan A. S., Jaglal S. B., Stone J. A., Clark A. M. (2015). A secondary meta-synthesis of qualitative studies of gender and access to cardiac rehabilitation. Journal of Advanced Nursing, 71(8), 1758–1773. 10.1111/jan.12620 [DOI] [PubMed] [Google Scholar]
- Artinian N. T., Fletcher G. F., Mozaffarian D., Kris-Etherton P., Van Horn L., Lichtenstein A. H., … American Heart Association Prevention Committee of the Council on Cardiovascular Nursing. (2010). Interventions to promote physical activity and dietary lifestyle changes for cardiovascular risk factor reduction in adults: A scientific statement from the American Heart Association. Circulation, 122(4), 406–441. 10.1161/CIR.0b013e3181e8edf1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck C., McSweeney J. C., Richards K. C., Roberson P. K., Tsai P. F., Souder E. (2010). Challenges in tailored intervention research. Nursing Outlook, 58(2), 104–110. 10.1016/j.outlook.2009.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beckie T. M., Beckstead J. W. (2010). Predicting cardiac rehabilitation attendance in a gender tailored randomized clinical trial. JCRP: Journal of Cardiopulmonary Rehabilitation and Prevention, 30(3), 147–156. 10.1097/HCR.0b013e3181d0c2ce [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beckie T. M., Beckstead J. W., Groer M. W. (2010). The influence of cardiac rehabilitation on inflammation and metabolic syndrome in women with coronary heart disease. Journal of Cardiovascular Nursing, 25(1), 52–60. 10.1097/JCN.0b013e3181b7e500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beckie T. M., Beckstead J. W., Kip K., Fletcher G. (2013). Physiological and exercise capacity improvements in women completing cardiac rehabilitation. JCRP: Journal of Cardiopulmonary Rehabilitation and Prevention, 33(1), 16–25. 10.1097/HCR.0b013e3182763192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bennett J., Dubois C. (2013). A novel platinum chromium everolimus-eluting stent for the treatment of coronary artery disease. Biologics: Targets and Therapy, 7(1), 149–159. 10.2147/BTT.S34939 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beswick A. D., Rees K., West R. R., Taylor F. C., Burke M., Griebsch I., Ebrahim S. (2005). Improving uptake and adherence in cardiac rehabilitation: Literature review. Journal of Advanced Nursing, 49(5), 538–555. 10.1111/j.1365-2648.2004.03327.x [DOI] [PubMed] [Google Scholar]
- Chen W. C., Yu Y. C., Glaser K. (2009). The knowledge and attitudes of coronary heart disease prevention among middle and older aged people in a community in Taipei. Taiwan Geriatrics and Gerontology, 4(4), 251–262. [Google Scholar]
- Daubenmier J. J., Weidner G., Sumner M. D., Mendell N., Merritt-Worden T., Studley J., Ornish D. (2007). The contribution of changes in diet, exercise, and stress management to changes in coronary risk in women and men in the multisite cardiac lifestyle intervention program. Annals of Behavioral Medicine, 33(1), 57–68. 10.1207/s15324796abm3301_7 [DOI] [PubMed] [Google Scholar]
- Escolá-Gil J. C., Julve J., Griffin B. A., Freeman D. J., Blanco-Vaca F. (2015). HDL and lifestyle interventions. In von Eckardstein A., Kardassis D. (Eds.), High density lipoproteins: From biological understanding to clinical exploitation (pp. 569–592). New York, NY: Springer; 10.1007/978-3-319-09665-0 [DOI] [PubMed] [Google Scholar]
- Grace S. L., Racco C., Chessex C., Rivera T., Oh P. (2010). A narrative review on women and cardiac rehabilitation: Program adherence and preferences for alternative models of care. Maturitas, 67(3), 203–208. 10.1016/j.maturitas.2010.07.001 [DOI] [PubMed] [Google Scholar]
- Grundy S. M. (2016). Metabolic syndrome update. Trends in Cardiovascular Medicine, 26(4), 364–373. 10.1016/j.tcm.2015.10.004 [DOI] [PubMed] [Google Scholar]
- Hung Y. Y., Hung S. Y., Chou C. L., Chen S. A. (2014). Cardiac rehabilitation among patients with acute myocardial infarction receiving percutaneous coronary intervention after acute myocardial infarction indicator was activated. Taiwan Journal of Physical Medicine and Rehabilitation, 42(3), 153–160. 10.6315/2014.42(3)03 (Original work published in Chinese) [DOI] [Google Scholar]
- Jaeschke L., Steinbrecher A., Pischon T. (2015). Measurement of waist and hip circumference with a body surface scanner: Feasibility, validity, reliability, and correlations with markers of the metabolic syndrome. PLoS One, 10(3), e0119430 10.1371/journal.pone.0119430 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kent L. M., Morton D. P., Rankin P. M., Mitchell B. G., Chang E., Diehl H. (2014). Gender differences in effectiveness of the Complete Health Improvement Program (CHIP) lifestyle intervention: An Australasian study. Health Promotion Journal of Australia, 25(3), 222–229. 10.1071/HE14041 [DOI] [PubMed] [Google Scholar]
- Krummel D. A., Koffman D. M., Bronner Y., Davis J., Greenlund K., Tessaro I., Wilbur J. (2001). Cardiovascular health interventions in women: What works. Journal of Women’s Health and Gender-Based Medicine, 10(2), 117–136. 10.1089/152460901300039467 [DOI] [PubMed] [Google Scholar]
- Lavie C. J., Milani R. V. (2006). Adverse psychological and coronary risk profiles in young patients with coronary artery disease and benefits of formal cardiac rehabilitation. Archives of Internal Medicine, 166(17), 1878–1883. 10.1001/archinte.166.17.1878 [DOI] [PubMed] [Google Scholar]
- Lavie C. J., Thomas R. J., Squires R. W., Allison T. G., Milani R. V. (2009). Exercise training and cardiac rehabilitation in primary and secondary prevention of coronary heart disease. Mayo Clinic Proceedings, 84(4), 373–383. 10.1016/S0025-6196(11)60548-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu D. H., Chen Y. C., Hung S. Y., Chou C. L. (2013). Cardiac rehabilitation after coronary artery bypass graft or heart valve replacement surgery—Experience of a medical center. Taiwan Journal of Physical Medicine and Rehabilitation, 41(3), 181–188. 10.6315/2013.41(3)04 (Original work published in Chinese). [DOI] [Google Scholar]
- Ministry of Health and Welfare, Taiwan, ROC. (2007). Criteria for the diagnosis of metabolic syndrome in adults (20 years of age and older). Retrieved from http://www.hpa.gov.tw/Pages/Detail.aspx?nodeid=639andpid=1219 (Original work published in Chinese)
- Ministry of Health and Welfare, Taiwan, ROC. (2017). List of gender indicators report. Retrieved from http://www.mohw.gov.tw/cht/DOS/Statistic.aspx?f_list_no=312andfod_list_no=6143 (Original work published in Chinese)
- Mosca L., Banka C. L., Benjamin E. J., Berra K., Bushnell C., Dolor R. J., Wenger N. K. (2007). Evidence-based guidelines for cardiovascular disease prevention in women: 2007 update. Circulation, 115(11), 1481–1501. 10.1161/CIRCULATIONAHA.107.181546 [DOI] [PubMed] [Google Scholar]
- Mosca L., Benjamin E. J., Berra K., Bezanson J. L., Dolor R. J., Lloyd-Jones D. M., Wenger N. K. (2011). Effectiveness-based guidelines for the prevention of cardiovascular disease in women—2011 update: A guideline from the American Heart Association. Circulation, 123(11), 1243–1262. 10.1161/CIR.0b013e31820faaf8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Papakonstantinou N. A., Stamou M. I., Baikoussis N. G., Goudevenos J., Apostolakis E. (2013). Sex differentiation with regard to coronary artery disease. Journal of Cardiology, 62(1), 4–11. 10.1016/j.jjcc.2013.03.001 [DOI] [PubMed] [Google Scholar]
- Petersen K. E. N., Johnsen N. F., Olsen A., Albieri V., Olsen L. K., Dragsted L. O., Egeberg R. (2015). The combined impact of adherence to five lifestyle factors on all-cause, cancer and cardiovascular mortality: A prospective cohort study among Danish men and women. British Journal of Nutrition, 113(5), 849–858. 10.1017/S0007114515000070 [DOI] [PubMed] [Google Scholar]
- Razavi M., Fournier S., Shepard D. S., Ritter G., Strickler G. K., Stason W. B. (2014). Effects of lifestyle modification programs on cardiac risk factors. PLoS One, 9(12), e114772 10.1371/journal.pone.0114772 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Savage P. D., Brochu M., Ades P. A. (2004). Gender alters the high-density lipoprotein cholesterol response to cardiac rehabilitation. Journal of Cardiopulmonary Rehabilitation, 24(4), 248–256. 10.1097/00008483-200407000-00007 [DOI] [PubMed] [Google Scholar]
- Strid C., Lingfors H., Fridlund B., Mårtensson J. (2012). Lifestyle changes in coronary heart disease—Effects of cardiac rehabilitation programs with focus on intensity, duration and content—A systematic review. Open Journal of Nursing, 2(4), 420–430. 10.4236/ojn.2012.24060 [DOI] [Google Scholar]
- Taylor R. S., Dalal H., Jolly K., Zawada A., Dean S. G., Cowie A., Norton R. J. (2015). Home-based versus centre-based cardiac rehabilitation. Cochrane Database of Systematic Reviews, 2015(8), CD007130 10.1002/14651858.CD007130.pub3 [DOI] [PubMed] [Google Scholar]
- Wanyonyi K. L., Themessl-Huber M., Humphris G., Freeman R. (2011). A systematic review and meta-analysis of face-to-face communication of tailored health messages: Implications for practice. Patient Education and Counseling, 85(3), 348–355. 10.1016/j.pec.2011.02.006 [DOI] [PubMed] [Google Scholar]
- World Health Organization. (2016). Women’s health. Retrieved from http://www.who.int/topics/womens_health/en/
- Yamaoka K., Tango T. (2012). Effects of lifestyle modification on metabolic syndrome: A systematic review and meta-analysis. BMC Medicine, 10(1), 138 10.1186/1741-7015-10-138 [DOI] [PMC free article] [PubMed] [Google Scholar]


