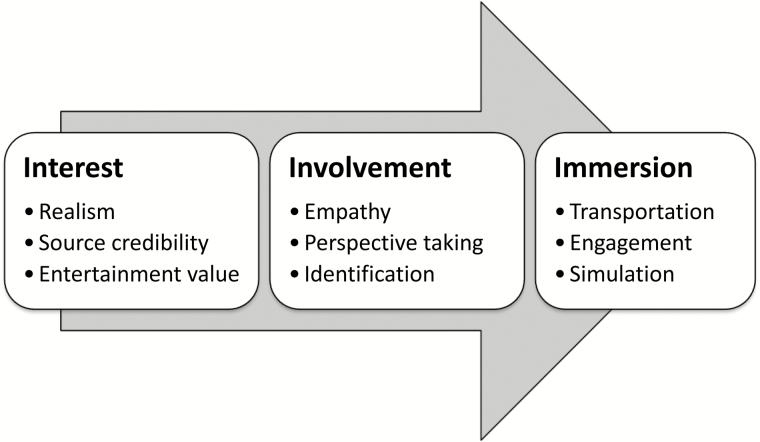
The Narrative Immersion Model identifies parameters that predict the impact of narrative messaging through successive layers of engagement with the narrative: interest, identification, and immersion
Keywords: Narratives, Personal stories, Testimonials, Exemplars, Case studies, Health behavior
Abstract
Background
How can we use stories from other people to promote better health experiences, improve judgments about health, and increase the quality of medical decisions without introducing bias, systematically persuading the listeners to change their attitudes, or altering behaviors in nonoptimal ways? More practically, should narratives be used in health education, promotion, or behavior change interventions?
Method
In this article, we address these questions by conducting a narrative review of a diverse body of literature on narratives from several disciplines to gain a better understanding about what narratives do, including their role in communication, engagement, recall, persuasion, and health behavior change. We also review broad theories about information processing and persuasion from psychology and more specific models about narrative messaging found in the health communication and marketing literatures to provide insight into the processes by which narratives have their effect on health behavior.
Results
To address major gaps in our theoretical understanding about how narratives work and what effects they will have on health behavior, we propose the Narrative Immersion Model, whose goal is to identify the parameters that predict the specific impact of a particular narrative (e.g. persuade, inform, comfort, etc.) based on the type of narrative message (e.g. process, experience, or outcome narrative). Further, the Narrative Immersion Model describes the magnitude of the effect as increasing through successive layers of engagement with the narrative: interest, identification, and immersion. Finally, the Narrative Immersion Model identifies characteristics of the narrative intervention that encourage greater immersion within a given narrative.
Conclusions
We believe there are important communication gaps in areas areas of behavioral medicine that could be addressed with narratives; however, more work is needed in order to employ narrative messaging systematically. The Narrative Immersion Model advances our theoretical understanding about narrative processing and its subsequent effects on knowledge, attitudes, and behavior.
Introduction
Researchers and scholars alike have often written about the extent to which humans rely upon narratives for processing complex information, for entertaining and empowering people, and for communicating with individuals and the public more generally [1–3]. Volumes of research have been devoted to understanding what constitutes the core elements of a narrative, how narratives affect human behavior, and why narratives evoke different responses than other methods of sharing information [4–6]. Yet we are a long way from a science of narrative intervention that can be reliably used to affect health promotion and behavior change. One major reason for this is that research on narratives necessitates an interdisciplinary endeavor, yet the work to date remains largely isolated within disciplinary silos. For example research on narratives in health psychology has been largely removed from research in marketing and health communication, although these fields share similar research questions and experimental methods. Therefore, the purposes of this article are to review relevant research on narratives focused on issues related to behavioral medicine and to present a comprehensive model of how narratives influence health behavior. With this, we hope to advance the science of narrative intervention and to provide a framework for a more effective use of narratives in behavioral health.
Defining Narratives
Narratives have been used by many disciplines for many reasons. Each discipline often has a different term, but these concepts represent similar, if not identical, constructs. For example, journalism has used the term exemplars, defined as individual cases that describe a particular experience, which are used to illustrate abstract concepts and give life to stories [7]. Marketing has used testimonials, or a public declaration about someone or something, as a persuasive tool, typically to encourage consumers to buy a particular product. In psychology, case studies or case histories have been used to make information more vivid (e.g. [8, 9]). Sociologists often refer to personal stories as a vehicle for transmitting cultural norms. In medicine, narratives, or “illustrative examples of others’ experiences,” have been used to provide information, convey empathy, and change behavior [10, 11].
In addition to the use of separate terms, many definitions of the core component of a narrative have been articulated (e.g. [12]). These definitions vary from specifying complex components of a story structure to something as vague as a personal story. For example, Miller-Day and Hecht [13] define a narrative as “talk organized around significant or consequential experiences, with characters undertaking some action within a context, with implicit or explicit beginning and end points, and significance for the narrator or his or her audience” (pp. 2). Alternatively, Shaffer and Zikmund-Fisher [11] describe narratives as illustrative stories about personal experiences. Others have specified that narratives are stories that are characterized by (a) a description of a series of events about a unified subject [14], (b) an emotional cadence [15], (c) causal relationships between actors and events [16], (d) chronological or temporal ordering of events [14, 17], (e) and demarcation signs (e.g. beginnings, middles, and ends) [17].
Beyond differences in terminology, different disciplines have examined different aspects of narratives resulting in several incomplete bodies of work with no single discipline providing a comprehensive model about the effects of narratives and how they work. This disciplinary piecemeal approach to the study of narratives has reduced the ability of behavioral scientists to employ narrative messaging effectively in health education, promotion, and behavior change interventions. A complete understanding about what narratives can do and how they work is essential to the development of a science of narrative health interventions. In the first section of this article, we will review the literature in these areas, providing relevant examples from several disciplines. This review will not be exhaustive, but rather will provide illustrative examples of themes in the literature. In the second section of the article, we will review the theoretical literature that describes how narratives work and introduce a new model, the Narrative Immersion Model, which provides a more comprehensive understanding about how narratives affect health behavior.
What do Narratives do?
Narratives Communicate Information
One of the primary functions of narrative communication is to convey information. For example, narratives have been used in entertainment education to inform women with lower levels of literacy about their treatment choices for early stage breast cancer [18], and narratives about life with dementia have also been used to help with advanced care planning in older adults [19]. Narrative messaging is particularly effective for this purpose because narratives are more engaging than didactic presentations of information [20–22]. For instance, Cox and Cox [23] measured engagement by the endorsement of items such as “I got involved in what the ad had to say”; the authors reported greater engagement with a narrative message than with a statistical message encouraging the use of mammography to screen for breast cancer. Volk and colleagues [22] also reported that participants were very engaged with the testimonials used in their entertainment-based decision aid, with greater engagement reported by participants at a low-literacy site than participants at a high-literacy site. Narrative messaging is also more engaging because narratives are perceived to be more relevant to the recipient [23].
In addition to its value in attracting the attention of viewers, narrative messaging is also a more effective method of communicating information. First, information provided in narrative form is better retrieved than information provided in other formats, such as non-narrative persuasive, expository, or descriptive writing [24]. Specifically, people read narrative text more quickly (about twice as fast) [25] and recalled information from narrative text about twice as accurately [26]. More recently, narratives have been used as a novel method for disseminating clinical guidelines to physicians [27]. Emergency physicians were randomly assigned to read a summary of the American College of Emergency Physicians opioid prescribing guidelines or a fictional narrative designed to match the summary in content and length. One hour after reading, the physicians were asked to recall as much of the guidelines as they could remember, and physicians who read the narrative version recalled more information about the guidelines than physicians who read the summary.
Audiences of narrative interventions also develop fewer counterarguments to the message than didactic communications [20]. Early work by Slater and Rouner [28] demonstrated that message processing was dependent upon whether participants agreed with the message or not. For messages or interventions that were consistent with currently held beliefs, participants rated statistical evidence to be of higher quality (e.g. more persuasive, more believable and better written) than narrative information. In contrast, when messages were value-discrepant (or when information presented conflicted with current beliefs), participants perceived narratives to be higher quality evidence than statistics. Thus, interventions with narratives appear to escape the scrutiny that interventions with statistical evidence receive from people who disagree with the message. This has important implications for health behavior change interventions, where the goal is often to change attitudes towards an unhealthy or harmful health behavior.
Narratives Change Attitudes, Judgments, and Behaviors
While narratives have been used in health to inform the public about complex health issues, social psychologists and researchers studying marketing and consumer behavior have used narratives to change attitudes about people, products, treatments, etc. (e.g. [29, 30]). For example, recent research in psychology has also suggested that narratives may be used to reduce prejudice by inducing the reader to imagine the experiences of another person, increasing the perceived connection between the reader and the person in the narrative [31]. In a series of studies, Kaufman and Libby [32] developed the concept of experience-taking, where readers adopt the role of a specific character in a story and simulate events through their eyes. The authors suggest that narrative prose increases experience-taking, which in turn increases the perceived overlap between self and others, resulting in more positive attitudes toward the character portrayed in the narrative and reductions in stereotyping and prejudice. Experience-taking can also produce behavioral changes; in one study, higher levels of experience-taking with a protagonist that voted on Election Day translated into increased voting among the readers. This work also has important implications for interventions aimed at reducing racial bias in healthcare [33], suggesting that interventions employing narrative elements will be more effective than other education-based methods.
Beyond attitude change, narratives also influence behavioral intentions and health behavior (e.g. [11, 21, 34]). For example, narratives have been used in cancer prevention and control efforts to increase screening behavior [21]. Compared to an educational message alone, an education message plus a narrative was more effective at increasing interest in screening for colorectal cancer [35]. Further, research by Anderson [36] demonstrated that health communication interventions designed to increase breast self-exams in younger women were more effective at increasing behavioral intentions and self-efficacy when they included a narrative of a woman who is taught to perform her own breast self-exam compared with a verbal persuasion to perform breast self-exams or an unrelated video produced by the American Cancer Society. Research by Murphy and colleagues has also demonstrated that narratives can be used to reduce health disparities in cervical cancer screening [37]. Beyond cancer, personal narratives have been shown to broadly increase the effect of communication-based interventions targeting prevention in a number of areas [13]. For example, the use of a narrative-based drug prevention program (keepin it REAL) has reduced substance use in middle school students [38].
Beyond prevention and control, narratives have also been used to promote other positive health behaviors. For example, including narrative information in an eHealth program for breast cancer patients increased healthcare participation above and beyond the increases attributed to didactic information [39]. In addition, patient narratives can improve the behavioral management of chronic diseases. Campbell and colleagues [40] demonstrated that viewing a DVD with several patient narratives in addition to reading an information brochure improved self-care activities (e.g. diet, exercise, blood glucose testing) for patients with type-2 diabetes compared with patients in the control condition who received the information booklet alone. Similarly, Ng and colleagues [41] found that video modeling was more successful than behavioral training at increasing exercise performance in patients with chronic obstructive pulmonary disease. While narrative messaging may be more successful at increasing desired behaviors (e.g. exercise), it is not the most effective method of communicating for every health information goal. A recent study compared the effects of a narrative communication about the benefits of exercise during and after treatment from a breast cancer survivor to a content equivalent message sharing expert recommendations [42]. Intentions to exercise were greater in the narrative message condition than the expert message condition; however, knowledge about the benefits and risks of exercise was greater in the expert message condition. While the narrative intervention had the desired effect on behavioral intentions, it did not improve recall of benefit and risk information. Therefore, a more nuanced approach to narrative selection may be appropriate when the primary goal of the intervention is to increase knowledge. While narrative interventions broadly improve message recall [26], they may also inhibit recall for specific elements of the message.
While the majority of research on narratives has focused on the way in which narratives can positively shape attitudes and health behaviors, narratives can also have negative consequences for our health-related judgments and medical decisions. For example, research by Betsch and colleagues [43] found that narratives describing negative side effects associated with vaccinations increased the perceived risk of vaccination and reduced vaccination intentions. Further, narrative information had a greater effect on perceived risk and behavioral intentions than statistical risk information. Another recent study showed that exposure to brief stories about vaccines causing harm negatively influenced vaccine attitudes even among participants who did not believe that the vaccine actually caused the harm in question [44]. Additional work has shown that even a single narrative in a fact-based program can alter risk perception and behavioral intentions [45, 46]. This occurs because narratives are so compelling that they can cause the decision maker to ignore relevant base rate information [9, 47, 48]. Narratives also increase the availability of the associated event, and information that easily comes to mind will have a greater effect on decision making [46, 49, 50].
Additional work has demonstrated that health news stories about celebrities can shift public opinion and behavior [51, 52]. In March 2000 television news anchor Katie Couric underwent a colonoscopy live on the Today Show to create awareness for colon cancer screening and reduce the stigma associated with the screening test following the death of her husband from colon cancer 2 years earlier. Two separate population-based data sets demonstrated that Katie Couric’s celebrity narrative had a significant effect on screening behavior; the number of colonoscopies performed per month increased significantly for 9 months after the broadcast [51]. Similarly, in 1989 first lady Nancy Regan underwent a mastectomy after being diagnosed with breast cancer, which was covered prominently in the lay press. Data from the Surveillance, Epidemiology, and End Results tumor registry showed that the rate of mastectomy increased for two quarters following the publicity associated with Nancy Regan’s treatment decision [52]. More recently, actress Angelina Jolie wrote an op-ed piece in the New York Times about her decision to undergo a bilateral prophylactic mastectomy with breast reconstruction after undergoing genetic testing for the BRCA1 gene [53]. Since this piece was published in 2013, demand for BRCA1/2 genetic testing has nearly doubled and inquiries about prophylactic mastectomies have also increased [54].
How do Narratives Work?
Across a wide variety of disciplines, research on narratives has demonstrated that narrative interventions can have a powerful effect on knowledge, attitudes, and health behaviors (Table 1). What is less clear are the mechanisms through which narratives have their effect. There are some broad models from cognitive and social psychology that describe information processing and persuasion, which can be applied to this literature. There are also more specific models about narrative messaging found in the health communication and marketing literatures. In this section we will describe the most relevant theories, discuss the predictions they make about narrative communication, and identify the gaps in their coverage of this literature.
Table 1.
Effects of Narratives
| Narrative effects | Citations |
|---|---|
| Communicate information more effectively | |
| 1.More engaging | Cox & Cox, 2001; Green, 2006; Kreuter et al., 2007; Volk et al., 2008 |
| 2.Better recall | Graesser et al., 2002; Graesser et al., 1980a; 1980b; Kilaru et al., 2014 |
| 3.Develop fewer counterarguments | Green, 2006; Slater & Rouner, 1996 |
| Change attitudes, judgments, and behaviors | |
| 1.Increase attitudes toward brands and consumer products | Adaval & Wyer, 1998; Escalas, 2004; Padgett & Allen, 1997 |
| 2.Reduce prejudice | Johnson et al., 2013; Kaufman & Libby, 2012 |
| 3.Promote positive health behaviors | Anderson, 2000; Campbell et al., 2008; Dillard et al, 2010; Falzon et al., 2014; Hinyard & Kreuter, 2007; Kreuter et al., 2007; Ng et al., 1999; Shaffer & Zikmund-Fisher, 2013; Wise et al., 2008 |
| 4.Reduce negative health behaviors | Miller-Day & Hecht, 2013; Warren et al., 2006 |
| 5.Improve work performance | Bal et al., 2011; Miall & Keuiken, 2002; Sonnentag & Fritz, 2007 |
| 6.Ignore base rate information; increase availability of narrative information | Bar-Hillel, 1980; Bar-Hillel & Fischhoff, 1981; Betsch et al., 2011; Taylor, 1982; Taylor & Thompson, 1982; Zillmann, 1999; 2006 |
There are a number of models from cognitive and social psychology that suggest narrative-based interventions are more powerful than other types of health interventions. For the scope of this article, we will briefly describe two of the most widely cited of these models: the Yale Persuasion Model and The Elaboration Likelihood Model. The Yale Model of Persuasion, developed by Hovland, Janis, and Kelley [55], defines four sequential cognitive processes required for attitude and behavior change [56]. In order for a given message to be persuasive, the message must first be attractive enough to grab the audience’s attention, and then the audience must be able to comprehend the message. These first two steps are necessary but not sufficient conditions of persuasion. In order to change attitudes, the audience must also “yield” to the message through further elaboration, and the likelihood of permanent attitude change also increases with message retention. One implication of this model is that narratives should be highly effective at engendering attitude change compared with other interventions because narratives tend to be superior on all four processes: attention, comprehension, elaboration, and retention.
The Elaboration Likelihood Model, developed by Petty and Cacioppo [57], states that elaboration, or the further development of thoughts pertaining to a presented argument, can be achieved through two differing avenues: the central route and the peripheral route. The central route takes into consideration the actual nature and merit of the message being presented. If an individual believes that the message is relevant or important, they are more likely to take the central route. The second route, termed the peripheral route, relies more on secondary cues from the message to provoke attitude change. Based on the tenets on this model, the extended Elaboration Likelihood Model was developed to predict the extent of processing associated specifically with narrative messages [58], focusing on the unique ability of narratives to reduce counterarguments and resistance common to other formats of persuasive messaging [59].
In addition to these broad theories of persuasion or information processing, there are a few models that are more specific to narrative messaging. For example, Busselle and Bilandzic’s [60] theory of narrative engagement uses a mental models perspective to identify four independent dimensions of narrative engagement that predict a story’s affect on attitudes: narrative understanding, attentional focus, emotional engagement, and narrative presence. Narrative understanding represents the degree to which the audience is able to comprehend the storyline, while attentional focus is the capability of the narrative to keep an audience focused on the story. Emotional engagement does not refer to any specific emotion but rather an involvement of the audience with the story on an emotional level. Finally, narrative presence is the feeling of immersion into the story, neglecting your immediate surroundings. The elements of this model (e.g. emotional engagement) favor narrative messages over didactic information. Further, this model predicts that stories with greater values on these dimensions will be more persuasive.
The last model we will consider is the most recent model of narrative engagement, the Extended Transportation-Imagery Model [61]. As the name implies, there was an earlier version of this model that focused on the audience’s ability to be “transported” by narrative, taking on the role of a character or become immersed in the story [62]. In this more recent iteration of the model, Van Laer and colleagues [61] added the antecedents and possible consequences of transportation. The authors describe two types of antecedents of transportation, those of the story/storyteller and those of the audience. For example, having identifiable characters and an imaginable plot (antecedents of the story) increase the likelihood that the audience will be transported. This model also predicts that women and more educated adults (antecedents associated with the audience) are more likely to be transported by a story. In addition to identifying antecedents, the authors describe several affective and cognitive consequences of narrative transportation such as changes in attitudes or behavioral intentions.
Although these models provide some insight into the power of narrative interventions, there are several aspects of narrative interventions that remain poorly understood. First, all of these models focus on attitude change as the primary outcome of narrative messaging, with the implication that narratives are used solely for persuasion. However, this singular focus on attitude and behavior change ignores a large body of literature that uses narratives in health communications to inform, to model behavior, to reduce affective forecasting errors, and to comfort patients and families (c.f. [11]). Second, no single model appropriately captures the complexity of the cognitive process associated with narratives. These models each explain a specific mechanism through which narratives exert their influence (e.g. transportation) but none are comprehensive. Finally, while the Extended-Transportation Imagery Model describes some message characteristics that predict the effect of a given narrative (e.g. having identifiable characters), all of these models ignore the specific content of a message. Besides incorporating research on story structure, these models have treated the specific message content as a black box. To address these major limitations with the current models, we have developed the Narrative Immersion Model, which combines research on message content with literature from psychology, medicine, and consumer behavior that describes cognitive mechanisms associated with the processing of narrative interventions.
Narrative Immersion Model
When examining a given narrative, there are at least two questions one could ask. First, what effects will this story have? Second, how strong will these effects be, compared to another narrative or some other method of communication? Although there is a rich interdisciplinary literature on narratives, relatively little attention has been paid to predicting the specific effect of a narrative. The Narrative Immersion Model described below seeks to provide answers to both of these questions, making predictions about the type and magnitude of the effect of a given narrative. In a recent paper, Shaffer and Zikmund-Fisher suggested that the specific effect of a narrative was directly tied to its content, arguing for a taxonomy of narrative types [11]. The crux of the argument is that behavioral health researchers have historically treated all narratives as if they are functionally the same, when narratives can vary on a number of dimensions. The taxonomy describes narratives differing on three dimensions: (a) purpose, (b) content, and (c) evaluative valence. This distinction forms the foundation of our more comprehensive theoretical model, which describes how narrative health interventions will influence health-related choices and decisions. The first section will describe how different types of narratives differentially affect decisions and behaviors, while the second section will describe characteristics of narratives that predict larger narrative effects.
Predicting the Effect of a Narrative: From Comfort to Persuasion
Reviewing the literature on narratives, Shaffer and Zikmund-Fisher noted five different purposes for using narrative communication: (a) to inform, (b) to engage, (c) to model behavior, (d) to persuade, and (e) to provide comfort [11]. Further, narratives with different purposes had different effects on health behavior. The authors argued that this was because narratives with different purposes had different types of content. They went on to describe three types of narrative content: (a) stories about how people made medical decisions (i.e. process narratives), (b) stories describing what it is like to experience a particular health-related event (i.e. experience narratives), and (c) stories about the psychological or physical outcomes of a health-related event or medical decision (i.e. outcome narratives).
One important reason for highlighting these three story types is that they have different effects on health behavior. Stories about health outcomes can be comforting (particularly when the outcome is positive), but the most noteworthy effect of outcome narratives is their ability to be persuasive, changing attitudes and altering intentions and health behavior. For example, providing decision makers with stories about the outcomes of two types of procedures for treating angina (bypass surgery and angioplasty) led to different treatment preferences than when decision makers only read statistical information about the outcomes (i.e. what % of the time was treatment successful) [63, 64]. More recently, we have demonstrated that reading a single story about a life-threatening reaction to a common over-the-counter medication (ibuprofen) that appeared in The New York Times changed attitudes toward the use of ibuprofen [65]. Perhaps most importantly, ibuprofen use 2 weeks after reading The New York Times article was significantly reduced compared with use before reading the article. Further, intentions to use ibuprofen remained lower, suggesting this change in medication use will continue to persist.
In addition to simply providing stories about outcomes, the persuasive impact of an outcome narrative can be particularly enhanced if it includes a clear counterfactual [66]. For example, imagine a parent telling a tragic story about the death of their young child that could have easily been avoiding by doing X or not doing Y. This simple story coupled with a tragic outcome and an easy solution for preventing future occurrences of that outcome is extremely powerful because it is easy to simulate a world in which this simple solution would save lives [67]. In the future, we would see more of X or less of Y. Consider also the popular narratives about vaccination. Some families tell heartbreaking stories of autism in their young children that coincided with their scheduled MMR vaccinations. Their message is a powerful one: If only I had chosen not to vaccinate my child, they would not have autism today. This message has been effectively communicated by a very small number of stories, such as that of actress Jenny McCarthy [68–71], but has had a huge impact on vaccination choices in USA [43, 68, 72, 73]. This is also a popular method of communicating information in health prevention campaigns. For example, Miller-Day and Hecht [13] have recently described how to use personal narratives in communication-based prevention efforts, citing examples from recent successful drug prevention curricula.
In addition to describing how a story ends (i.e. sharing outcomes), there are many stories that simply describe how a medical decision was made. We have termed these stories process narratives and have given them the distinction of a separate category of narrative content because they have different effects on decision makers than outcome narratives. We argue that the biggest contribution that process narratives can make is to help decision makers identify the relevant decision attributes and/or model optimal decision processes. For example, patients making treatment decisions for cancers with very high survival rates (e.g. breast and prostate cancers) may initially focus exclusively on choosing a treatment with the greatest chance of survival or the lowest cancer recurrence rate. However, given the rates of survival with all current treatments are very high, patients may benefit from considering other aspects of the treatments such as side effects and time and energy that will need to be invested in each treatment. Therefore stories about how other patients made their treatment decisions, particularly those stories that highlight the different aspects of each treatment considered, could help patients to identify the decision attributes most relevant to themselves.
Process narratives could also be used to model optimal decision processes. For example, the Institute of Medicine has recently endorsed the use of shared decision making between doctors and patients as the gold standard of care [74]. Although shared decision making sounds fairly intuitive, patients may have a hard time figuring out how to engage in this process with their physician. Process narratives could be used to model how shared decision making can be accomplished and provide key questions that patients can ask their physicians without describing the particular choices made as a result of these processes [36, 41].
Although the process of identifying additional decision dimensions or using a different decisional process could cause a decision maker to choose a different option, process narratives, unlike outcome narratives, are not necessarily expected to be persuasive or change medical decisions. Shaffer, Hulsey, and Zikmund-Fisher [75] demonstrated that process narratives changed how people searched for information in a hypothetical breast cancer decision task. Specifically, people spent more time reading information about treatment attributes identified by decision makers in the process narratives than people who did not view narratives or from people who viewed other types of narratives. These findings were supported by a second study using eye tracking, which demonstrated that stories with process elements embedded in a web-based patient decision aid globally increased information search [76]. Despite the effects on information processing neither study reported differences in treatment preferences or medical decisions.
The final category of narrative content described in the Narrative Immersion Model is the experience narrative. This type of narrative depicts stories that capture “what something was really like.” Stories of this type provide powerful, real world descriptions that provide the reader or viewer with a unique window into a health-related experience [77]. The insight that develops through sharing experiential information is important because it can reduce affective forecasting errors, a cognitive bias wherein people mispredict their feelings about future experiences [78]. Medical decisions may be reasonably based on how we think we will feel if we choose a given treatment (e.g. What will my quality of life be like if I have surgery to create an ostomy to treat my ulcerative colitis?). However, given we are notoriously poor affective forecasters [79, 80], basing decisions on our affective forecasts may lead us to make medical decisions that we would later come to regret.
For example, most people erroneously imagine that their quality of life with an ostomy (where bodily waste is removed from the body via a pouch connected to an opening in the abdomen) would be greatly reduced [81–83]. This misprediction could cause patients with ulcerative colitis to continue suffering with their condition, which involves several painful bowel movements a day, instead of having the surgery to create an ostomy. Experience narratives have the potential to improve our affective forecasts by facilitating more accurate perspective taking, which could ultimately reduce regret with medical decisions. Angott, Comerford and Ubel [84] recently demonstrated that providing people with a video about a person’s experience with an ostomy significantly reduced affective forecasting errors among low disgust participants. Similarly, Volandes and colleagues have used video narratives depicting a day in the life of an elderly adult with advanced Alzheimer’s disease to decrease decisional conflict and increase the stability of decisions about end of life care [85, 86].
Experience narratives may also improve our resilience under difficult conditions [87]. For example, employees who work in call centers have one of the highest turnover rates, and researchers have used “realistic previews,” in this case real experiences about the very worst aspects of this job, to provide job applicants with a better understanding of what the job entails [88]. Surprisingly after providing applicants with a realistic preview, job turnover rates decreased and, in some instances, ratings of job satisfaction increased [89, 90]. Further this impressive effect was not the function of a self-selection effect, as the number of job candidates who accepted the position did not change after the realistic preview. Rather these previews appeared to bolster resilience by preparing employees for the difficult situations they will face. Experience narratives could function in a similar fashion in health, with narratives providing a “warts and all approach” to health communication recalibrating patient expectations and increasing resilience [77].
In addition to the narrative content, identifying and describing the evaluative valence of a narrative will be important to determining its impact [11]. Evaluative valence is defined as the relative positive or negative affect portrayed within the narrative and represents the overall emotional tone of the narrative message. Although the primary effect of a given narrative is expected to be tied directly to the message content, the evaluative valence of a narrative is expected to enhance the effect of the particular narrative content. However, it is generally expected that negative stories will have a more powerful effect than positive stories [91, 92].
One unique contribution of the Narrative Immersion Model is that it can make predictions about the specific effects of a given narrative based on the content of that narrative. Building upon research in this area, the Narrative Immersion Model has identified at least three areas of narrative content that have differential effects on medical decision making: outcome narratives, process narratives, and experience narratives. While these descriptions of the categories of content in the Narrative Immersion Model are depicted here as orthogonal, this is not a model requirement. In fact, for some narratives there will be elements of more than one category of content. The categories in this model are best depicted as fuzzy categories that allow for gist understanding about the ways in which the specific content of the story may influence medical decision making. In addition, to the specific content of a narrative, the Narrative Immersion Model predicts that the evaluative valence of the story, which is described as a continuum of narrative affect ranging from negative to positive, will further enhance the effect of a narrative’s content.
One element not yet addressed is how to determine the relative impact of two narratives of the same type. That is, when reading two outcome narratives, what characteristics predict which of the two outcome narratives will have a greater effect on health behavior? In this second section of the Narrative Immersion Model, we will describe the process of narrative immersion and the characteristics of the narrative that will promote movement along the continuum from interest through involvement to immersion.
Predicting the Magnitude of Narrative Impact: From Interest to Immersion
Understanding the magnitude of the effect of a given narrative requires an understanding of the process by which narratives function to provide knowledge and alter judgments about health, attitudes and health behavior. In this second section, we will use a hierarchical model of narrative immersion to describe this process; see Fig. 1. We depict this process as a continuum through which a reader or viewer may travel. The deeper into the continuum they move, the more power a given narrative will have to influence their health behavior. Some narratives can start from the bottom of this hierarchy and move up. For example, a patient may become interested in viewing a narrative about another patient’s treatment experience because the credibility and realism of the source (i.e. a real story from a fellow patient with the same condition) first peaked her interest. After starting to watch the video, the patient may become involved with the narrative because she strongly identifies with the storyteller. Finally, the patient may become fully immersed in the story and be able to fully simulate the experiences of this other patient because of the uniquely captivating way this other patient tells her story. But, this continuum is not necessarily a strict hierarchy in the sense that one must always go through one level to get to the next. Rather, a patient could become immediately involved with a narrative and quickly have empathy for the main character and an ability to take their perspective. We argue that the place that the audience finds themselves within the hierarchy is determined by characteristics of the narrative that promote deeper involvement. We will first discuss the immersion process then explore specific narrative characteristics that will lead to greater immersion.
Fig. 1.
Determining the magnitude of the narrative impact.
The first level of the narrative immersion process is interest. To be effective, a narrative must pique the interest of the reader or viewer. It is broadly understood that narrative interventions are naturally more relevant to human beings than other message formats (e.g. fact-based messages) (e.g. [6, 58]). Beyond our general predisposition for narrative information, there are also characteristics of narratives that create greater interest, which are described in greater detail in the next section.
The second level of narrative processing is involvement. Involvement requires more active participation by the audience than interest. By being involved with a narrative, the audience is able to actively identify with the character [93] and take their perspective, which allows them to experience empathy [31, 94]. While Cohen has defined the concept of identification as the interpretation of events in a story by the audience “as if the events were happening to [themselves]” [93], we subsume the concept of identification under the second level of narrative processing—involvement—because the colloquial use of the term identification typically denotes an outside perspective. We suggest that identification is more synonymous with perspective taking, which is to be distinguished from the more transformative experience of immersion, the final stage of narrative processing (described next).
An important consequence of the increased depth of processing associated with involvement in the narrative message is the potential to use narratives to reduce discrimination. For example, studies have shown that narrative-induced perspective taking can reduce prejudice against gay men [32], people with disabilities [95], people who are of Arab descent [31], African Americans [32], and other stigmatized groups [96]. Stigma and racial bias affect the medical care received by marginalized groups [33], and narrative interventions have great promise for improving care to these populations.
The final stage of narrative processing is immersion, which requires a complete transportation into the narrative and a detachment from the physical and psychological world of the audience [6, 62, 94]. When an audience is immersed in a narrative, incoming information will not be processed from the perspective of the audience member but rather from the perspective of the character involved [93, 94]. Narratives that immerse the audience are typically more effective at their goal [61]. However, greater immersion can actually distract from the ability to analytically view an argument [97] and others have suggested that too much transportation would cause deviation from the message embedded within the narrative. Specifically, Miller-Day and Hecht [13] have argued that there may be a curvilinear relationship between transportation and the effect of a message in communication-based prevention efforts, such that greater transportation would lead to immersion in the story at the cost of understanding and taking in the intended message of the intervention.
Which Narratives are More Likely to Result in Immersion?
Beyond our general predisposition to narrative information [1–4, 6], there are also message characteristics that create greater interest. For example, narratives with a greater degree of realism tend to generate more interest. Note that realism does not mean real. For narratives to be influential, they do not have to be provided by “real” people (e.g. [98]). Rather, the stories need to feel realistic. Fictional characters can also be influential, and people judge these characters based on their ability to depict “real” situations [99]. Further, violations of realism within a narrative can negatively impact interest in the story [60]. This has important implications for the development of narrative health interventions because constructed narratives have the potential to be equally as powerful as curated or selected stories from real people. In fact, narratives constructed to illustrate particular elements of health experiences may be more effective as long as the appropriate degree of realism is maintained.
Another strategy to create interest in a narrative is to choose a storyteller or a message that has strong ties to the audience, with the broad understanding that a greater connection between the audience and characters makes the narrative more effective [97, 100]. There are also several factors that contribute to the connection between the audience and the characters of the story including perceived similarity, liking, and parasocial interaction [58, 59, 93]. Perceived similarity refers to the assessment of the degree of commonality shared with the character [59], while liking refers to the positive evaluation of a character, which can occur without similarity to the audience [93], and parasocial interaction is described as the one-sided relationship an audience member has with a media character [101]. Together, these three constructs generally reduce counterarguments and reactance and increase vulnerability and self-efficacy, all of which result in attitudes and health behaviors that are consistent with the narrative intervention [59].
Narratives can also be more persuasive when the protagonist and the audience are known to be members of the same group (e.g. ethnicity, sexual orientation) from the outset of the story [32]. More specifically, narrative health messages can be more effective when the protagonist and audience have similar racial/ethnic backgrounds or social contexts because cultural similarities provide multiple channels for persuasion [21, 102, 103]. Kreuter and colleages have argued that exposure to a story with characters of similar social contexts or ethnic backgrounds improves message encoding, which can later help the audience recall ways to cope with survivorship issues and treatment side effects as well as improve medical decision making. Perceived cultural similarity can also result in increased trust in the characters [104].
A great deal of research in message tailoring (e.g. [105]) has found that narratives, particularly in health communication, can be more impactful when they are tailored to the particular race/ethnicity and culture of the intended audience [106]. For example, Kreuter and colleagues [107] reported that combining culturally tailored messaging and cancer prevention interventions increased uptake of mammography and improved intake of fruits and vegetables among African American women. Thus, a narrative that uses protagonists who are similar to the audience, especially culturally, can be more effective at informing the audience and affecting attitudes and health behavior change, particularly in culturally sensitive health contexts (see also [34]).
However, the relationship between similarity and narrative impact is fairly nuanced and racial and cultural similarity is not a necessary characteristic for the development of an effective narrative health intervention. Similarity does not always produce liking, and characters who are of the opposite sex from the reader/viewer can also strongly influence the effect of narratives on health behavior [58]. Further, similarity between the audience and the characters can also at times decrease the effectiveness of the narrative. Similarity results in greater transportation and requires fewer cognitive resources to process the story, thereby allowing the viewer to spend more time elaborating on the message [108]. Increasing the similarity between the characters and the audience would only be an effective strategy if the message holds up under increased scrutiny. Messages with arguments that are perceived to be weak may ultimately be rejected after further inspection.
In addition to realism and similarity, there are several structural elements of narratives that can lead to greater immersion. For example, Pennington and Hastie [109] have argued that coherence within a story will lead to greater persuasion. Specifically, stories that were more easily constructed and stories that were more complete had a stronger influence on the perception of guilt in judicial decisions [110]. Further, narratives that depict causally related events, are temporally ordered, and are demarcated by a beginning, middle, and end should also lead to greater immersion [14, 17]. Several studies have demonstrated that first-person narratives also have larger effects than third-person narratives; therefore, first-person narratives should lead to greater immersion [32, 111]. These findings suggest that health interventions should choose narratives that are internally coherent, well-ordered, and told by the person who experienced them.
Other structural components of a story that can cause greater narrative immersion are plot elements such as humor and surprise. Loewenstein, Raghunathan, and Heath [112] reported that advertisements employing a narrative structure, termed the repetition-break plot structure [113], are more persuasive then other types of story structures. A story utilizing this type of plot structure repeats an element of the story multiple times to establish a particular pattern [113]. For example in the popular kids story, the Three Little Pigs, the first two pigs build their houses with flimsy materials and the big bad wolf blows down their respective houses. Following the repetition, the story then breaks the established pattern by providing another similar example that has a different ending, thereby generating surprise. In the Three Little Pigs, the third pig chose to build her house of bricks, which is unable to be blown down by the wolf despite his repeated attempts. The unique element of this plot structure is the surprise generated by the repetition break; Loewenstein and colleagues have shown that when this type of surprise is used in advertisements, it results in more views on YouTube, superior brand attitudes, and increased purchase intentions [112].
Similarly, narratives that include humor have also been shown to significantly influence attitudes and behavior and increase immersion in a given narrative. For example, Moyer-Gusé and colleagues [114] examined the effect of pregnancy-related humor on attitudes toward and intentions to engage in unprotected sex in undergraduate students. When pregnancy as a result of unprotected sex was presented in a humorous context within a narrative, there were fewer counterarguments but the consequences of unprotected sex were somewhat trivialized. Further, viewers reported a greater likelihood of having unprotected sex when the pregnancy was presented in a humorous context rather than a serious story context. Taken together, this work suggests that, in order to increase the effectiveness of narrative health interventions, the narratives themselves should be carefully curated such that the retelling of health experiences captures these storytelling principles.
Finally, it is important to emphasize the value of pilot testing all narrative messaging. Even though a particular narrative message may be built for maximum persuasive value based upon the elements of the Narrative Immersion Model, the judgments made about characteristics of the message and the audience should be empirically tested. For example, humor is a subjective characteristic; therefore, messages designed with humor to increase impact should be tested to see if audience members actually find them humorous. Pilot testing all interventions to see if audience reactions are as predicted before rolling out a large intervention can still be very useful.
Conclusions
In this manuscript, we conducted a narrative review of the literature on narratives that has highlighted much of the interdisciplinary work on the topic. This literature demonstrates that while a compelling, persuasive narrative can save lives (e.g. by increasing uptake of cancer screening), an equally compelling, but misinformed, narrative can cost lives (e.g. decrease vaccinations). Narratives can also be incredibly powerful (e.g. the “Katie Couric effect”) or surprisingly benign (e.g. narratives in patient decision aids; [115]). And despite the widespread utilization of narratives in advertising, public health campaigns, and social media, as well as the vast amount of research on the topic in a wide variety of disciplines, until now no one has developed a comprehensive theory about how narratives work. Therefore, designers of health interventions have been unable to predict the type of effect a given narrative will have (i.e. persuasion, communicate information, etc.) and the magnitude of that effect.
To address this gap in the literature, we introduce the Narrative Immersion Model, which seeks to identify the parameters that predict the effectiveness of a given narrative on health behavior. The Narrative Immersion Model makes predictions about: (a) the specific effect of a particular narrative (e.g. persuade, inform, comfort, etc.) based on the type of narrative message (e.g. process, experience, or outcome narrative) and (b) the magnitude of the effect as increasing through successive layers of narrative engagement (e.g. interest, identification, and immersion) based on characteristics of the narrative that encourage greater immersion (e.g. realism, similarity, and likability, and plot elements such as humor and surprise). The Narrative Immersion Model provides a greater understanding about why and how narratives influence health behavior and provides health practitioners a theoretical framework for the development of effective narrative interventions.
While research is needed to better understand how audience characteristics moderate narrative impact on health behavior (e.g. individual differences in transportability; [116]), the Narrative Immersion Model advances our theoretical understanding about narrative processing and its subsequent effects on knowledge, attitudes, and health behavior. Narratives are a powerful tool for communication and persuasion, yet they are also one that needs to be used thoughtfully and carefully in order to achieve optimal outcomes. We believe there are important communication gaps in areas of behavioral medicine that could be addressed with narratives, and we hope that this work will help to bridge the extant communication gaps both between the multiple disciplines that have considered narratives and, perhaps more importantly, between the academic research that has explored narrative effects and the practitioners in healthcare who need to understand how narratives can be most effectively deployed in health education, promotion, and behavior change interventions.
Acknowledgments:
Dr. V. A. Shaffer was supported by Agency for Healthcare Research and Quality grant # R01HS23328-01 and National Science Foundation grant #1529277. Dr. L. D. Scherer was supported by National Science Foundation grant #1529277. Dr. B. J. Zikmund-Fisher was supported by National Science Foundation grant #1529277, National Institutes of Health grant “Exploring Precision Cancer Medicine for Sarcoma and Rare Cancers,” and Agency for Healthcare Research and Quality grant “Systematic Design of Meaningful Presentations of Medical Test Data for Patients.”
Compliance with Ethical Standards
Conflict of Interest: Dr. V. A. Shaffer received honoraria from the Agency for Healthcare Research and Quality. The other authors declare that they have no conflict of interest.
Informed Consent: Given that the manuscript is a review article, we are not directly reporting the results of research involving human participants or animals. Therefore, we did not need to provide informed consent.
References
- 1. Gottschall J. The Storytelling Animal: How Stories Make Us Human. New York, NY: Houghton Mifflin Harcourt; 2012. [Google Scholar]
- 2. Cron L. Wired for Story: The Writer’s Guide to Using Brain Science to Hook Readers from the Very First Sentence. Berkeley, CA: Ten Speed Press; 2012. [Google Scholar]
- 3. Olson R, Barton D, Palermo B.. Connection: Hollywood Storytelling Meets Critical Thinking. Los Angeles, CA: Prairie Starfish Productions; 2013. [Google Scholar]
- 4. Denning S. The Springboard: How Storytelling Ignites Action in Knowledge-Era Organizations. New York, NY: Routledge; 2001. [Google Scholar]
- 5. Simmons A. The Story Factor: Secrets of Influence from the Art of Storytelling. New York, NY: Basic Books; 2006. [Google Scholar]
- 6. Green MC, Strange JJ, Brock TC.. Narrative Impact: Social and Cognitive Foundations. New York, NY: Psychology Press; 2002. [Google Scholar]
- 7. Hinnant A, Len-Ríos ME, Young R. Journalistic use of exemplars to humanize health news. Journal Stud. 2013; 14(4): 1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Borgida E, Nisbett RE. The differential impact of abstract vs. concrete information on decisions. J Appl Soc Psychol. 1977; 7(3): 258–271. [Google Scholar]
- 9. Taylor SE, Thompson SC. Stalking the elusive “vividness” effect. Psychol Rev. 1982; 89(2): 155–181. [Google Scholar]
- 10. Bekker HL, Winterbottom A, Butow P et al. . Using personal stories. BMC Med Inform Decis Mak. 2013; 13 (Suppl 2): S9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Shaffer VA, Zikmund-Fisher BJ. All stories are not alike: a purpose-, content-, and valence-based taxonomy of patient narratives in decision aids. Med Decis Making. 2013; 33(1): 4–13. [DOI] [PubMed] [Google Scholar]
- 12. Shankar A, Elliott R, Goulding C. Understanding consumption: Contributions from a narrative perspective. Journal of Marketing Management. 2001; 17: 429–453. [Google Scholar]
- 13. Miller-Day M, Hecht ML. Narrative means to preventative ends: A narrative engagement framework for designing prevention interventions. Health Commun. 2013; 28(7): 657–670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Carroll N. On the narrative connection. In: Van Peer W, Chatman S, eds. New Perspectives on Narrative Perspective. Albany, NY: State University of New York Press; 2001. [Google Scholar]
- 15. Velleman JD. Narrative explanation. Philos Rev. 2003; 112(1): 1–25. [Google Scholar]
- 16. Currie G. Narrative representation of causes. The Journal of Aesthetics and Art Criticism. 2006; 64(3): 309–316. [Google Scholar]
- 17. Gergen KJ, Gergen MM. Narrative and the self as relationship. Advances in Experimental Social Psychology. 1988; 21: 17–56. [Google Scholar]
- 18. Jibaja-Weiss ML, Volk RJ, Granch TS et al. . Entertainment education for informed breast cancer treatment decisions in low-literate women: development and initial evaluation of a patient decision aid. J Cancer Educ. 2006; 21(3): 133–139. [DOI] [PubMed] [Google Scholar]
- 19. Volandes AE, Lehmann LS, Cook EF, Shaykevich S, Abbo ED, Gillick MR. Using video images of dementia in advance care planning. Arch Intern Med. 2007; 167(8): 828–833. [DOI] [PubMed] [Google Scholar]
- 20. Green MC. Narratives and cancer communication. J Commun. 2006; 56 (Suppl 1): S163–S183. [Google Scholar]
- 21. Kreuter MW, Green MC, Cappella JN et al. . Narrative communication in cancer prevention and control: a framework to guide research and application. Ann Behav Med. 2007; 33(3): 221–235. [DOI] [PubMed] [Google Scholar]
- 22. Volk RJ, Jibaja-Weiss ML, Hawley ST et al. . Entertainment education for prostate cancer screening: a randomized trial among primary care patients with low health literacy. Patient Educ Couns. 2008; 73(3): 482–489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Cox D, Cox AD. Communicating the consequences of early detection: the role of evidence and framing. Journal of Marketing. 2001; 65(3): 91–103. [Google Scholar]
- 24. Graesser AC, Olde B, Klettke B. How does the mind construct and represent stories? In: Green MC, Strange JJ, Brock TC, eds. Narrative Impact: Social and Cognitive Foundations. New York, NY: Psychology Press; 2002. [Google Scholar]
- 25. Graesser AC, Hoffman NL, Clark LF. Structural components of reading time. J Verbal Learning Verbal Behav. 1980; 19(2): 135–151. [Google Scholar]
- 26. Graesser AC, Hauft-Smith K, Cohen AD, Pyles LD. Advanced outlines, familiarity, and text genre on retention of prose. J Exp Educ. 1980; 48(4): 281–290. [Google Scholar]
- 27. Kilaru AS, Perrone J, Auriemma CL, Shofer FS, Barg FK, Meisel ZF. Evidence-based narratives to improve recall of opioid prescribing guidelines: a randomized experiment. Acad Emerg Med. 2014; 21(3): 244–249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Slater MD, Rouner D. Value-affirmative and value-protective processing of alcohol education messages that include statistical evidence or anecdotes. Communic Res. 1996; 23: 210–235. [Google Scholar]
- 29. Adaval R, Wyer RS. The role of narratives in consumer information processing. J Consum Psychol. 1998; 7(3): 207–245. [Google Scholar]
- 30. Padgett D, Allen D. Communicating experiences: a narrative approach to creating service brand image. J Advert. 1997; 26(4): 49–62. [Google Scholar]
- 31. Johnson DR, Jasper DM, Griffin S, Huffman BL. Reading narrative fiction reduces Arab-Muslim prejudice and offers a safe haven from intergroup anxiety. Soc Cogn. 2013; 31(5): 578–598. [Google Scholar]
- 32. Kaufman GF, Libby LK. Changing beliefs and behavior through experience-taking. J Pers Soc Psychol. 2012; 103(1): 1–19. [DOI] [PubMed] [Google Scholar]
- 33. Williams DR, Wyatt R. Racial bias in health care and health: challenges and opportunities. JAMA. 2015; 314(6): 555–556. [DOI] [PubMed] [Google Scholar]
- 34. Hinyard LJ, Kreuter MW. Using narrative communication as a tool for health behavior change: a conceptual, theoretical, and empirical overview. Health Educ Behav. 2007; 34(5): 777–792. [DOI] [PubMed] [Google Scholar]
- 35. Dillard AJ, Fagerlin A, Dal Cin S, Zikmund-Fisher BJ, Ubel PA. Narratives that address affective forecasting errors reduce perceived barriers to colorectal cancer screening. Soc Sci Med. 2010; 71(1): 45–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Anderson RB. Vicarious and persuasive influences on efficacy expectations and intentions to perform breast self-examination. Pub Relat Rev. 2000; 26(1): 97–114. [Google Scholar]
- 37. Murphy ST, Frank LB, Chatterjee JS, Baezconde-Garbanati L. Narrative versus nonnarrative: the role of identification, transportation, and emotion in reducing health disparities. J Commun. 2013; 63(1): 116–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Warren JR, Hecht ML, Wagstaff DA et al. . Communicating prevention: the effects of the keepin’it REAL classroom videotapes and televised PSAs on middle-school students’ substance use. J Appl Commun Res. 2006; 34(2): 209–227. [Google Scholar]
- 39. Wise M, Han JY, Shaw B, McTavish F, Gustafson DH. Effects of using online narrative and didactic information on healthcare participation for breast cancer patients. Patient Educ Couns. 2008; 70(3): 348–356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Campbell T, Dunt D, Fitzgerald JL, Gordon I. The impact of patient narratives on self-efficacy and self-care in Australians with type 2 diabetes: stage 1 results of a randomized trial. Health Promot Int. 2015; 30(3): 438–448. [DOI] [PubMed] [Google Scholar]
- 41. Ng JYY, Tam SF, Yew WW, Lam WK. Effects of video modeling on self-efficacy and exercise performance of COPD patients. Soc Behav Pers. 1999; 27(5): 475–486. [Google Scholar]
- 42. Falzon C, Radel R, Cantor A, d’Arripe-Longueville F. Understanding narrative effects in physical activity promotion: the influence of breast cancer survivor testimony on exercise beliefs, self-efficacy, and intention in breast cancer patients. Support Care Cancer. 2015; 23(3): 761–768. [DOI] [PubMed] [Google Scholar]
- 43. Betsch C, Ulshöfer C, Renkewitz F, Betsch T. The influence of narrative v. statistical information on perceiving vaccination risks. Med Decis Making. 2011; 31(5): 742–753. [DOI] [PubMed] [Google Scholar]
- 44. Scherer LD, Shaffer VA, Patel N, Zikmund-Fisher BJ. Can the vaccine adverse event reporting system be used to increase vaccine acceptance and trust?Vaccine. 2016; 34(21): 2424–2429. [DOI] [PubMed] [Google Scholar]
- 45. Zillmann D. Exemplification theory: judging the whole by some of its parts. Media Psychol. 1999; 1(1): 69–94. [Google Scholar]
- 46. Zillmann D. Exemplification effects in the promotion of safety and health. J Commun. 2006; 56 (Suppl 1): S221–S237. [Google Scholar]
- 47. Bar-Hillel M. The base-rate fallacy in probability judgments. Acta Psychol. 1980; 44(3): 211–233. [Google Scholar]
- 48. Bar-Hillel M, Fischhoff B. When do Base Rates Affect Predictions? Report for Office of Naval Research Washington, DC; 1981. Available at http://www.dtic.mil/get-tr-doc/pdf?AD=ADA099491. Accessibility verified May 29, 2014. [Google Scholar]
- 49. Taylor SE. The availability bias in social perception and interaction. In: Kahneman D, Tversky A, eds. Judgment Under Uncertainty: Heuristics and Biases. Cambridge, UK: Cambridge University Press; 1982. [Google Scholar]
- 50. Tversky A, Kahneman D. Availability: a heuristic for judging frequency and probability. Cogn Psychol. 1973; 5(2): 207–232. [Google Scholar]
- 51. Cram P, Fendrick AM, Inadomi J, Cowen ME, Carpenter D, Vijan S. The impact of a celebrity promotional campaign on the use of colon cancer screening: the Katie Couric effect. Arch Intern Med. 2003; 163(13): 1601–1605. [DOI] [PubMed] [Google Scholar]
- 52. Nattinger AB, Hoffmann RG, Howell-Pelz A, Goodwin JS. Effect of Nancy Reagan’s mastectomy on choice of surgery for breast cancer by US women. JAMA. 1998; 279(10): 762–766. [DOI] [PubMed] [Google Scholar]
- 53. Jolie A. My medical choice 2013. Available at http://www.nytimes.com/2013/05/14/opinion/my-medical-choice.html. Accessibility verified January 7, 2016.
- 54. Evans DG, Barwell J, Eccles DM et al. ; FH02 Study Group; RGC teams. The Angelina Jolie effect: how high celebrity profile can have a major impact on provision of cancer related services. Breast Cancer Res. 2014; 16(5): 442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Hovland CI, Janis IL, Kelley HH.. Communication and Persuasion; Psychological Studies of Opinion Change. New Haven, CT: Yale University Press; 1953. [Google Scholar]
- 56. Cameron KA. A practitioner’s guide to persuasion: an overview of 15 selected persuasion theories, models and frameworks. Patient Educ Couns. 2009; 74(3): 309–317. [DOI] [PubMed] [Google Scholar]
- 57. Petty RE, Cacioppo JT.. Communication and Persuasion: Central and Peripheral Routes to Attitude Change. New York, NY: Springer-Verlag; 1986. [Google Scholar]
- 58. Slater MD, Rouner D. Entertainment—education and elaboration likelihood: understanding the processing of narrative persuasion. Commun Theory. 2002; 12(2): 173–191. [Google Scholar]
- 59. Moyer-Gusé E. Toward a theory of entertainment persuasion: explaining the persuasive effects of entertainment-education messages. Commun Theory. 2008; 18(3): 407–425. [Google Scholar]
- 60. Busselle R, Bilandzic H. Measuring narrative engagement. Media Psychol. 2009; 12(4): 321–347. [Google Scholar]
- 61. Van Laer T, De Ruyter K, Visconti LM, Wetzels M. The extended transportation-imagery model: a meta-analysis of the antecedents and consequences of consumers’ narrative transportation. J Consum Res. 2014; 40(5): 797–817. [Google Scholar]
- 62. Green MC, Brock TC. The role of transportation in the persuasiveness of public narratives. J Pers Soc Psychol. 2000; 79(5): 701–721. [DOI] [PubMed] [Google Scholar]
- 63. Ubel PA, Jepson C, Baron J. The inclusion of patient testimonials in decision aids: effects on treatment choices. Med Decis Making. 2001; 21(1): 60–68. [DOI] [PubMed] [Google Scholar]
- 64. Fagerlin A, Wang C, Ubel PA. Reducing the influence of anecdotal reasoning on people’s health care decisions: is a picture worth a thousand statistics?Med Decis Making. 2005; 25(4): 398–405. [DOI] [PubMed] [Google Scholar]
- 65. Shaffer VA, Scherer LD, Hinnant A, Len-Ríos ME, Zikmund-Fisher BJ. What’s the story with narratives? How using personal narratives in journalism changes health behavior. Health Commun. 2017: 1–7. Available at 10.1080/10410236.2017.1333562. [DOI] [PubMed] [Google Scholar]
- 66. Newman TB. The power of stories over statistics. BMJ. 2003; 327(7429): 1424–1427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Kahneman D, Tversky A. The simulation heuristic. In: Kahneman D, Slovic P, Tversky A, eds. Judgment Under Uncertainty: Heuristics and Biases. Cambridge, UK: Cambridge University Press; 1982: 201–208. [Google Scholar]
- 68. Doucleff M. How vaccine fears fueled the resurgence of preventable diseases; 2014. Available at http://www.npr.org/sections/health-shots/2014/01/25/265750719/how-vaccine-fears-fueled-the-resurgence-of-preventable-diseases. Accessibility verified January 7, 2016.
- 69. Hiltzik M. Jenny McCarthy: Anti-vaxxer, public menace 2015. Available at http://www.latimes.com/business/hiltzik/la-fi-mh-jenny-mccarthy-antivaxxer-public-menace-20150127-column.html. Accessibility verified January 7, 2016.
- 70. Cawkwell PB, Oshinsky D. Storytelling in the context of vaccine refusal: a strategy to improve communication and immunisation. Med Humanit. 2016; 42(1): 31–35. [DOI] [PubMed] [Google Scholar]
- 71. Witteman HO, Zikmund-Fisher BJ. The defining characteristics of Web 2.0 and their potential influence in the online vaccination debate. Vaccine. 2012; 30(25): 3734–3740. [DOI] [PubMed] [Google Scholar]
- 72. Larson HJ, Cooper LZ, Eskola J, Katz SL, Ratzan S. Addressing the vaccine confidence gap. Lancet. 2011; 378(9790): 526–535. [DOI] [PubMed] [Google Scholar]
- 73. Brown K, Sevdalis N. Lay vaccination narratives on the web: are they worth worrying about?Med Decis Making. 2011; 31(5): 707–709. [DOI] [PubMed] [Google Scholar]
- 74. Committee on Quality of Healthcare in America IOM. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academy Press; 2001. [Google Scholar]
- 75. Shaffer VA, Hulsey L, Zikmund-Fisher BJ. The effects of process-focused versus experience-focused narratives in a breast cancer treatment decision task. Patient Educ Couns. 2013; 93(2): 255–264. [DOI] [PubMed] [Google Scholar]
- 76. Shaffer VA, Owens J, Zikmund-Fisher BJ. The effect of patient narratives on information search in a web-based breast cancer decision aid: an eye-tracking study. J Med Internet Res. 2013; 15(12): e273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Focella ES, Zikmund-Fisher BJ, Shaffer VA. Could physician use of realistic previews increase treatment adherence and patient satisfaction?Med Decis Making. 2016; 36(6): 683–685. [DOI] [PubMed] [Google Scholar]
- 78. Shaffer VA, Focella ES, Scherer LD, Zikmund-Fisher BJ. Debiasing affective forecasting errors with targeted, but not representative, experience narratives. Patient Educ Couns. 2016; 99(10): 1611–1619. [DOI] [PubMed] [Google Scholar]
- 79. Wilson TD, Gilbert DT. Affective forecasting. Adv Exp Soc Psychol. 2003; 35: 345–411. [Google Scholar]
- 80. Wilson TD, Gilbert DT. Affective forecasting: knowing what to want. Curr Dir Psychol Sci. 2005; 14(3): 131–134. [Google Scholar]
- 81. Boyd NF, Sutherland HJ, Heasman KZ, Tritchler DL, Cummings BJ. Whose utilities for decision analysis?Med Decis Making. 1990; 10(1): 58–67. [DOI] [PubMed] [Google Scholar]
- 82. Smith D, Loewenstein G, Jepson C, Jankovich A, Feldman H, Ubel P. Mispredicting and misremembering: patients with renal failure overestimate improvements in quality of life after a kidney transplant. Health Psychol. 2008; 27(5): 653–658. [DOI] [PubMed] [Google Scholar]
- 83. Smith DM, Sherriff RL, Damschroder L, Loewenstein G, Ubel PA. Misremembering colostomies? Former patients give lower utility ratings than do current patients. Health Psychol. 2006; 25(6): 688–695. [DOI] [PubMed] [Google Scholar]
- 84. Angott AM, Comerford DA, Ubel PA. Imagining life with an ostomy: does a video intervention improve quality-of-life predictions for a medical condition that may elicit disgust?Patient Educ Couns. 2013; 91(1): 113–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Volandes AE, Barry MJ, Chang Y, Paasche-Orlow MK. Improving decision making at the end of life with video images. Med Decis Making. 2010; 30(1): 29–34. [DOI] [PubMed] [Google Scholar]
- 86. Volandes AE, Paasche-Orlow MK, Barry MJ et al. . Video decision support tool for advance care planning in dementia: randomised controlled trial. BMJ. 2009; 338: b2159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Focella ES, Zikmund-Fisher BJ, Shaffer VA. Could physician use of realistic previews increase treatment adherence and patient satisfaction?Med Decis Making. 2016; 36(6): 683–685. [DOI] [PubMed] [Google Scholar]
- 88. Phillips JM. Effects of realistic job previews on multiple organizational outcomes: a meta-analysis. Acad Manage J. 1998; 41: 673–690. [Google Scholar]
- 89. Ilgen DR, Seely W. Realistic expectations as an aid in reducing voluntary resignations. J Appl Psychol. 1974; 59: 452–455. [Google Scholar]
- 90. Heath C, Heath D.. Decisive: How to Make Better Choices in Life and Work. New York, NY: Random House; 2013. [Google Scholar]
- 91. Baumeister RF, Bratslavsky E, Finkenauer C, Vohs KD. Bad is stronger than good. Rev Gen Psychol. 2001; 5(4): 323–370. [Google Scholar]
- 92. Rozin P, Royzman EB. Negativity bias, negativity dominance, and contagion. Pers Soc Psychol Rev. 2001; 5(4): 296–320. [Google Scholar]
- 93. Cohen J. Defining identification: a theoretical look at the identification of audiences with media characters. Mass Comm Soc. 2001; 4(3): 245–264. [Google Scholar]
- 94. Green MC, Brock TC, Kaufman GF. Understanding media enjoyment: the role of transportation into narrative worlds. Commun Theory. 2004; 14(4): 311–327. [Google Scholar]
- 95. Cameron L, Rutland A. Extended contact through story reading in school: reducing children’s prejudice toward the disabled. J Soc Issues. 2006; 62(3): 469–488. [Google Scholar]
- 96. Oliver MB, Dillard JP, Bae K, Tamul DJ. The effect of narrative news format on empathy for stigmatized groups. Journal Mass Commun Q. 2012; 89(2): 205–224. [Google Scholar]
- 97. Escalas JE. Self referencing and persuasion: narrative transportation versus analytical elaboration. J Consum Res. 2007; 33(4): 421–429. [Google Scholar]
- 98. Vezzali L, Stathi S, Giovannini D, Capozza D, Trifiletti E. The greatest magic of Harry Potter: reducing prejudice. J Appl Soc Psychol. 2015; 45(2): 105–121. [Google Scholar]
- 99. Shapiro MA, Kim H. Realism judgments and mental resources: a cue processing model of media narrative realism. Media Psychol. 2012; 15(1): 93–119. [Google Scholar]
- 100. Escalas JE. Narrative processing: building consumer connections to brands. J Consum Psychol. 2004; 14(1): 168–180. [Google Scholar]
- 101. Horton D, Wohl RR. Mass communication and para-social interaction; observations on intimacy at a distance. Psychiatry. 1956; 19(3): 215–229. [DOI] [PubMed] [Google Scholar]
- 102. Kreuter MW, Buskirk TD, Holmes K et al. . What makes cancer survivor stories work? An empirical study among African American women. J Cancer Surviv. 2008; 2(1): 33–44. [DOI] [PubMed] [Google Scholar]
- 103. Kreuter MW, McClure SM. The role of culture in health communication. Annu Rev Public Health. 2004; 25: 439–455. [DOI] [PubMed] [Google Scholar]
- 104. Bailey EJ, Erwin DO, Belin P. Using cultural beliefs and patterns to improve mammography utilization among African-American women: the Witness Project. J Natl Med Assoc. 2000; 92(3): 136–142. [PMC free article] [PubMed] [Google Scholar]
- 105. Skinner CS, Campbell MK, Rimer BK, Curry S, Prochaska JO. How effective is tailored print communication?Ann Behav Med. 1999; 21(4): 290–298. [DOI] [PubMed] [Google Scholar]
- 106. Kreuter MW, Lukwago SN, Bucholtz RD, Clark EM, Sanders-Thompson V. Achieving cultural appropriateness in health promotion programs: targeted and tailored approaches. Health Educ Behav. 2003; 30(2): 133–146. [DOI] [PubMed] [Google Scholar]
- 107. Kreuter MW, Sugg-Skinner C, Holt CL et al. . Cultural tailoring for mammography and fruit and vegetable intake among low-income African-American women in urban public health centers. Prev Med. 2005; 41(1): 53–62. [DOI] [PubMed] [Google Scholar]
- 108. Bhatnagar N, Wan F. Is self-character similarity always beneficial?J Advert. 2011; 40(2): 39–50. [Google Scholar]
- 109. Pennington N, Hastie R. Cognitive theory of juror decision making: the Story Model. Cardozo L Rev. 1991; 13: 5001–5039. [Google Scholar]
- 110. Pennington N, Hastie R. Explaining the evidence: tests of the Story Model for juror decision making. J Pers Soc Psychol. 1992; 62(2): 189. [Google Scholar]
- 111. Winterbottom A, Bekker HL, Conner M, Mooney A. Does narrative information bias individual’s decision making? A systematic review. Soc Sci Med. 2008; 67(12): 2079–2088. [DOI] [PubMed] [Google Scholar]
- 112. Loewenstein J, Raghunathan R, Heath C. The repetition-break plot structure makes effective television advertisements. J Mark. 2011; 75(5): 105–119. [Google Scholar]
- 113. Loewenstein J, Heath C. The repetition-break plot structure: a cognitive influence on selection in the marketplace of ideas. Cogn Sci. 2009; 33(1): 1–19. [DOI] [PubMed] [Google Scholar]
- 114. Moyer-Gusé E, Mahood C, Brookes S. Entertainment-education in the context of humor: effects on safer sex intentions and risk perceptions. Health Commun. 2011; 26(8): 765–774. [DOI] [PubMed] [Google Scholar]
- 115. Shaffer VA, Tomek S, Hulsey L. The effect of narrative information in a publicly available patient decision aid for early-stage breast cancer. Health Commun. 2014; 29(1): 64–73. [DOI] [PubMed] [Google Scholar]
- 116. Mazzocco PJ, Green MC, Sasota JA, Jones NW. This story is not for everyone: Transportability and narrative persuasion. Soc Psychol Personal Sci. 2010; 1(4): 361–368. [Google Scholar]