Abstract
Rationale:
To report a case of herpes simplex virus (HSV) linear endotheliitis in a 57-year-old male who had underwent keratoplasty 10 years ago. The characteristic linear keratic precipitates (KPs) resembled the Khodadoust line in graft rejection. The differential diagnosis is essential, because the treatment regimen is different between HSV linear endotheliitis and graft rejection.
Patient concerns:
The patient developed a sudden onset of ocular pain and a decrease in visual acuity in his right eye. The patient had received penetrating keratoplasty in the eye 10 years ago.
Diagnoses:
The ocular disease was evaluated using several ocular examinations, including best-corrected visual acuity (BCVA), intraocular pressure, slit lamp examination, fundus examination, and aqueous humor tap. Characteristic linear endothelial KPs were found both in the host cornea and graft cornea. Stromal edema was evident in both the donor and recipient corneas. The aqueous humor was sampled for viral polymerase chain reaction (PCR) analysis. The sample was investigated for the possible presence of HSV I, HSV II, cytomegalovirus, and varicella zoster virus. The PCR was positive for HSV I and negative for HSV II, cytomegalovirus, and varicella zoster virus.
Interventions:
The patient was treated with both antiviral and steroid treatments for 1 month. Thereafter, prophylactic antiviral treatment was continued.
Outcomes:
The subjective symptoms had improved and the cornea edema and the linear endothelial KPs had disappeared. The BCVA improved from 20/200 to 20/80.
Lessons:
HSV linear endotheliitis is the most severe form of HSV endotheliitis. This case showed characteristic endothelial KPs, which were different from the Khodadoust line of graft rejection.
Keywords: acyclovir, cornea, endotheliitis, herpes simplex virus, steroid
1. Introduction
Herpes simplex virus (HSV) causes various corneal diseases, including epithelial keratitis, neurotrophic keratopathy, stromal keratitis, and endotheliitis.[1] HSV endotheliitis is known to manifest in 3 different forms: disciform, diffuse, and linear.[2] Linear endotheliitis is a rare manifestation of HSV keratitis.[3] A characteristic finding in HSV linear endotheliitis involves linear endothelial keratic precipitates (KPs) starting from the limbus. The involved area between the limbus and KP shows both stromal and epithelial edema. This line resembles a rejection line (Khodadoust line), which is a characteristic finding of graft rejection in keratoplasty.[4] The rejected graft cornea also shows corneal edema in the involved area. Because the treatments for HSV linear endotheliitis and the corneal graft rejection line are totally different, differential diagnosis is essential.[4,5]
We treated a patient who developed HSV linear endotheliitis in the post-keratoplasty cornea. The linear KPs started from the limbus, crossed the host-graft junction, and extended into the endothelium of the graft cornea. The pathological virus was confirmed using polymerase chain reaction (PCR) examination of the aqueous humor. We have also added a brief review of this ocular disease.
2. Case presentation
The study adhered to the tenets of the Declaration of Helsinki and was conducted in compliance with the regulations of the Institutional Review Board of Daejeon St. Mary's Hospital, Daejeon, Republic of Korea. Informed consent was obtained from the patient.
A 57-year-old male visited our clinic for recently developed ocular discomfort and decreased visual acuity in his right eye. The patient had received penetrating keratoplasty in his right eye 10 years ago by another surgeon, and the exact preoperative diagnosis could not be identified. Ocular examinations were performed including best-corrected visual acuity (BCVA), slit lamp examination, tonometry, and a fundus examination. The BCVA was 20/200 and the intraocular pressure (IOP) was 48 mmHg by applanation. The slit lamp examination showed mild corneal edema with KPs scattered at the lower half of both the donor and recipient corneas. No specific abnormality was found in the vitreous and retinal examination. Intravenous injection of 25% mannitol (250 mL) was prescribed to decrease the IOP. On the presumption of graft rejection, the patient received oral prednisolone (40 mg/day), topical 1% prednisolone (q1h), and topical glaucoma medications. Despite treatment for 1 week, the patient complained of persistent ocular discomfort. A subsequent slit lamp examination showed linear endothelial KPs, which seemed to emanate from the temporal limbus (Fig. 1A). The linear KPs crossed the host-graft junction and were evident on the endothelial side of both the donor and recipient corneas (Fig. 1B). Localized corneal edemas were evident on both the donor and recipient corneas (Fig. 1C). The edema was bordered by the linear KPs.
Figure 1.
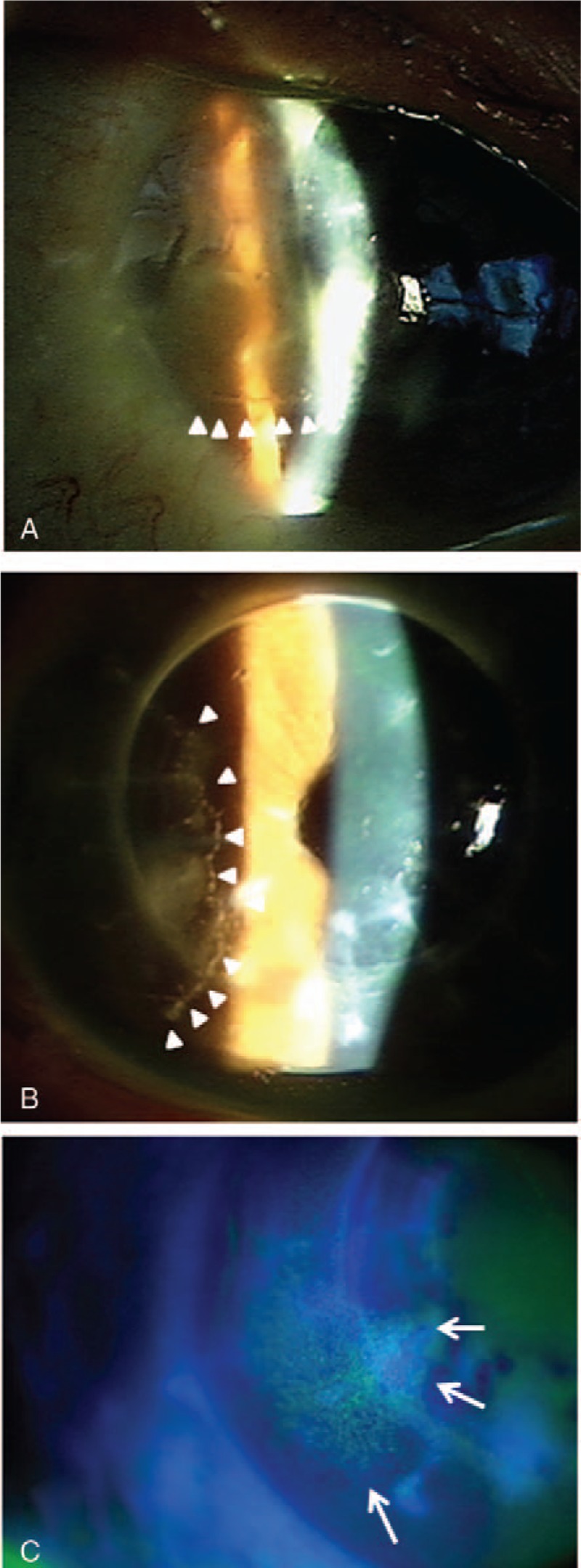
Linear KPs and corneal edema in a post-keratoplasty cornea of the right eye. (A) Linear KPs emanating from the temporal limbus (white wedge). (B) Linear KPs crossing the donor and recipient junction (white wedge). (C) Localized edema on both the donor and recipient cornea (white arrow). KPs = keratic precipitates.
On suspicion of viral endotheliitis, the patient was sent to the operating room and the aqueous humor was sampled for viral PCR analysis. The sample was investigated for the possible presence of HSV I, HSV II, cytomegalovirus, and varicella zoster virus. Systemic and topical corticosteroids were maintained, and oral acyclovir was added at 400 mg, five times daily. The PCR was positive for HSV I and negative for HSV II, cytomegalovirus, and varicella zoster virus. One week after systemic antiviral treatment, the subjective symptoms had improved and the cornea edema and the linear endothelial KPs had disappeared (Fig. 2). The BCVA improved to 20/80. The patient was prescribed with prophylactic antiviral treatment using acyclovir, 400 mg, 2 times daily. The graft cornea has remained clear for 1 year since the HSV endotheliitis.
Figure 2.
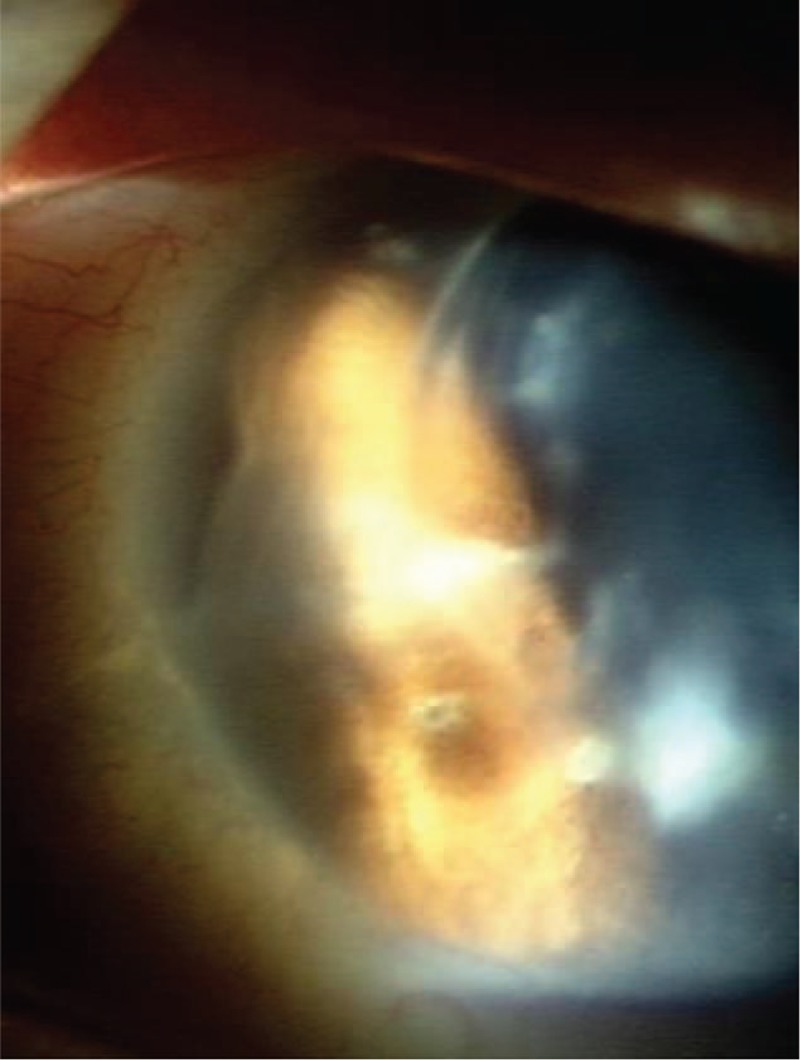
Linear KPs and stromal edema were resolved after antiviral and immunosuppressive treatment. KPs = keratic precipitates.
3. Discussion
This case showed a molecularly confirmed HSV linear endotheliitis in a post-keratoplasty patient.
The corneal endothelial cell count decreases continuously after penetrating keratoplasty. Considering the natural decline of the endothelium after keratoplasty, it is necessary to minimize the rejection-related endothelial cell loss. Graft rejection is the most important cause of graft failure.[6] A specific finding in endothelial graft rejection is the Khodadoust line. The KPs appear as a linearly oriented wave that starts at the periphery of the graft and moves to the center of the graft.[7] The border of the corneal edema is characterized by this line.
A line of KPs on the corneal endothelium is also found in HSV linear endotheliitis. The line progresses centrally from the limbus and is located at the advancing edge of the edema.[5] It is important to differentiate between graft rejection and HSV linear endotheliitis in a patient who develops corneal edema and linear KP. The treatment plan differs according to the etiology. Corticosteroids are the primary treatment for cornea graft rejection.[8] In contrast, systemic and topical antiviral drugs are necessary in addition to systemic corticosteroids for the treatment of HSV linear endotheliitis,[5] Three observations suggested that the cause of the corneal edema was not graft rejection. First, linear KPs crossed the donor-recipient junction, and stromal edema developed both in the donor and the recipient corneas. Second, the disease responded poorly on steroids alone, but improved dramatically when an antiviral agent was added. Finally, the disease was confirmed using PCR of an aqueous humor sample. It is, therefore, necessary to identify the etiological virus by PCR of the aqueous humor, because linear KPs can also appear in other virus-associated forms of endotheliitis such as cytomegalovirus.[9,10]
Proper treatment is necessary after diagnosis. HSV linear endotheliitis is known as the most severe form of the 3 types of HSV endotheliitis. Delayed treatment can deteriorate the corneal endothelium, resulting in bullous keratopathy.
Author contributions
Conceptualization: Chang Rae Rho.
Data curation: Jeongah Shin, Chang Rae Rho.
Funding acquisition: Chang Rae Rho.
Investigation: Ho Ra.
Methodology: Ho Ra, Chang Rae Rho.
Resources: Jeongah Shin.
Supervision: Chang Rae Rho.
Writing – original draft: Jeongah Shin, Ho Ra, Chang Rae Rho.
Writing – review & editing: Jeongah Shin, Ho Ra, Chang Rae Rho.
Chang Rae Rho orcid: 0000-0003-2542-3352.
Footnotes
Abbreviations: BCVA = best-corrected visual acuity, HSV = herpes simplex virus, IOP = intraocular pressure, KP = keratic precipitate, PCR = polymerase chain reaction.
This work was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Science, ICT & Future Planning (2016R1C1B2012933).
The authors have no conflicts of interest to disclose.
References
- [1].Tsatsos M, MacGregor C, Athanasiadis I, et al. Herpes simplex virus keratitis: an update of the pathogenesis and current treatment with oral and topical antiviral agents. Clin Exp Ophthalmol 2016;44:824–37. [DOI] [PubMed] [Google Scholar]
- [2].Kaye S, Choudhary A. Herpes simplex keratitis. Prog Retin Eye Res 2006;25:355–80. [DOI] [PubMed] [Google Scholar]
- [3].Shen YC, Wang CY, Chen YC, et al. Progressive herpetic linear endotheliitis. Cornea 2007;26:365–7. [DOI] [PubMed] [Google Scholar]
- [4].Panda A, Vanathi M, Kumar A, et al. Corneal graft rejection. Surv Ophthalmol 2007;52:375–96. [DOI] [PubMed] [Google Scholar]
- [5].Olsen TW, Hardten DR, Meiusi RS, et al. Linear endotheliitis. Am J Ophthalmol 1994;117:468–74. [DOI] [PubMed] [Google Scholar]
- [6].Alldredge OC, Krachmer JH. Clinical types of corneal transplant rejection. Their manifestations, frequency, preoperative correlates, and treatment. Arch Ophthalmol 1981;99:599–604. [DOI] [PubMed] [Google Scholar]
- [7].Khodadoust AA, Silverstein AM. Transplantation and rejection of individual cell layers of the cornea. Invest Ophthalmol 1969;8:180–95. [PubMed] [Google Scholar]
- [8].Randleman JB, Stulting RD. Prevention and treatment of corneal graft rejection: current practice patterns (2004). Cornea 2006;25:286–90. [DOI] [PubMed] [Google Scholar]
- [9].Morishige N, Morita Y, Yamada N, et al. differential changes in intraocular pressure and corneal manifestations in individuals with viral endotheliitis after keratoplasty. Cornea 2016;35:602–6. [DOI] [PubMed] [Google Scholar]
- [10].Koizumi N, Inatomi T, Suzuki T, et al. Clinical features and management of cytomegalovirus corneal endotheliitis: analysis of 106 cases from the Japan corneal endotheliitis study. Br J Ophthalmol 2015;99:54–8. [DOI] [PMC free article] [PubMed] [Google Scholar]


