Abstract
Background
One potential advantage of arthroscopic shoulder surgery over open approaches is accelerated recovery; however, the functional recovery period of daily activities for specific movements after arthroscopic rotator cuff repair has not yet been reported, to our knowledge.
Questions/purposes
(1) After arthroscopic rotator cuff repair, when are patients able to perform low-level and high-level front-of-body motion, low-level and high-level behind-the-back motion, strength-related activities, and sports/leisure activities? (2) How do tear size, arm dominance, and retear affect performance of these activities? (3) When does the UCLA score cross above 80% in each UCLA score component (28 points)?
Methods
A 2-year prospective study of 135 patients who underwent arthroscopic rotator cuff repair was performed (45 in small-sized, 45 in medium-sized, and 45 in large-to-massive-sized groups). The mean age was 60 years. Thirty-one and 104 shoulders were nondominant and dominant shoulders, respectively. Twenty-seven shoulders showed retear on MRI taken 9 months after surgery. We evaluated the functional recovery periods using the questionnaire and the UCLA scores and assessed influencing factors such as tear size, arm dominance, and retear. The patients were asked to fill out a questionnaire at 1, 2, 3, 6, 9, 12, 15, 18, and 24 months after surgery. The questionnaire evaluated front-of-the-body, behind-the-back, general, simple strength-related, and sports/leisure activities. Based on the UCLA evaluation, the functional recovery period was defined as the time required to achieve a score > 80% in each UCLA score component.
Results
Patients experienced recovery of low-level and high-level ROM front-of-the-body, high-level ROM behind-the-back, simple strength-related, and sports/leisure activities within 2 ± 1, 3 ± 2, 9 ± 0, 10 ± 2, and 14 ± 3 months, respectively, after surgery. Two patients with large-to-massive tears did not gain the recovery of high-level ROM behind-the-back, simple strength-related, and sports/leisure activities. Patients with large-to-massive tears were delayed from some activities compared with patients with small tears (10 ± 0 versus 7 ± 1 for washing back, p = 0.010; 11 ± 0 versus 10 ± 0 for lifting 5 kg, p = 0.020; 15 ± 0 versus 13 ± 0 for sports/leisure). Arm dominance was not associated with functional recovery. Patients with retears, compared with intact healing, had a longer time to return to washing hair (3 ± 2 versus 3 ± 1, p = 0.007), combing (4 ± 3 versus 2 ± 1, p = 0.002), washing the back (10 ± 3 versus 8 ± 3, p = 0.034), and sports/leisure (15 ± 3 versus 14 ± 3, p = 0.010). UCLA score in 134 patients reached 28 points, corresponding to the functional recovery period at 6 ± 3 months. One patient did not reach > 28 points on the UCLA score.
Conclusions
It took patients an average of 14 months to recover their daily motion after surgery. Tear size and retear affected only the recovery period of high-level motion activities and sports/leisure. This study was believed to serve as a guideline to inform patients about functional recovery after arthroscopic rotator cuff repair.
Level of Evidence
Level III, therapeutic study.
Introduction
Several studies have reported excellent clinical outcome scores after arthroscopic rotator cuff repairs [1, 4, 8, 19, 21, 28]. Peters et al. [28] evaluated 105 patients with small- or medium-sized full-thickness tears. They described that pain and shoulder function were improved after arthroscopic rotator cuff repair. Antoni et al. [1] reported that 88.2% of patients returned to recreational sports activities 6 months after surgery. Arthroscopic rotator cuff repair is a well-established operation to alleviate shoulder pain and dysfunction of rotator cuff tears [1, 4, 8, 19, 21, 28] and leads to a positive effect on patients’ lives, strengthening the ability to engage in sports activities and affecting employment [20].
According to previous studies, the factors that influence functional recovery after arthroscopic rotator cuff repair remain controversial [4, 8, 10, 13, 15, 17, 21, 23-26, 31]. Some authors explain tear size as the major factor that influences functional recovery [10, 25]. In addition, some studies have reported that tendon healing after arthroscopic rotator cuff repair has an effect on clinical outcomes [4, 10, 13]. There was a paucity of studies regarding the presence of arm dominance after arthroscopic rotator cuff repair [4].
Although prior studies [18, 27] have in general demonstrated faster recovery after arthroscopic rotator cuff surgery than what is achieved using open surgical techniques, much less is known about exactly when specific functional milestones are achieved by patients after arthroscopic rotator cuff repair. During postoperative evaluation in the outpatient clinic, activities in front of the scapular plane are likely to recover faster than activities behind the scapular plane. All previous studies on functional recovery of daily activities after arthroscopic rotator cuff repair used clinical scores to evaluate functional recovery of daily activities [4, 8, 21], but the functional recovery period of daily activities in front of and behind the scapular plane as well as the time to functional recovery of strength have not yet been reported, to our knowledge. Knowing in more precise terms when a patient might expect to achieve particular functional milestones is important to patients, because it allows them to plan for both personal and professional (that is, work-related) needs after surgery and also to ensure that the surgeon’s and the patient’s expectations are similar. Unmet expectations are a key source of patient dissatisfaction and malpractice litigation [21].
Therefore, we asked: (1) After arthroscopic rotator cuff repair, when were patients able to perform low-level and high-level front-of-body motion, low-level and high-level behind-the-back motion, strength-related activities, and sports/leisure activities? (2) How did tear size, arm dominance, and retear affect performance of these activities? (3) When did the UCLA score cross above 80% in each UCLA score component (28 points)?
Materials and Methods
This study was prospective, and the protocol of this study was approved by the institutional review board.
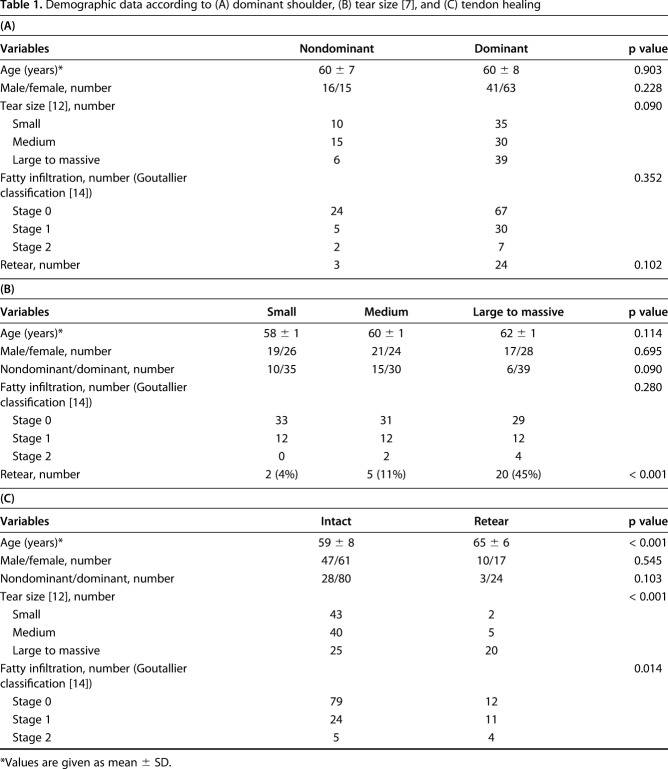
All patients who underwent arthroscopic rotator cuff repair between September 2015 and December 2015 by a single senior author (YGR) at one institution were qualified for inclusion in this prospective study. All the patients were encouraged to remain in the study up to 2 years after surgery. The inclusion criteria included full-thickness supraspinatus tears and complete arthroscopic rotator cuff repair. The exclusion criteria included a history of shoulder surgery, partial-thickness rotator cuff tears, partial rotator cuff repair, shoulder stiffness, and any associated lesions such as a subscapularis tear, infraspinatus tear, progressive glenohumeral arthritis, progressive acromioclavicular arthritis, traumatic unilateral Bankart lesions, superior labrum anterior to posterior lesions, or suprascapular nerve release. Shoulder stiffness was determined to be present when the patient showed a forward flexion of < 120° and external rotation of < 40° [6]. Of 152 shoulders that met the inclusion criteria during the study period, 15 shoulders also met the exclusion criteria. Two shoulders were lost to followup. Thus, a total of 135 shoulders were included in the final analysis (Fig. 1). The followup duration of all patients was 2 years (range, 2.0–2.2 years). The mean patient age at the time of the surgical procedure was 60 ± 8 years. Fifty-seven shoulders were male and 78 shoulders were female. The dominant shoulders were involved in 104 shoulders and 31 shoulders were nondominant shoulders. There were no demographic differences according to whether the operation was performed on the dominant shoulder and the size of the rotator cuff tear before surgery (Table 1).
Fig. 1.
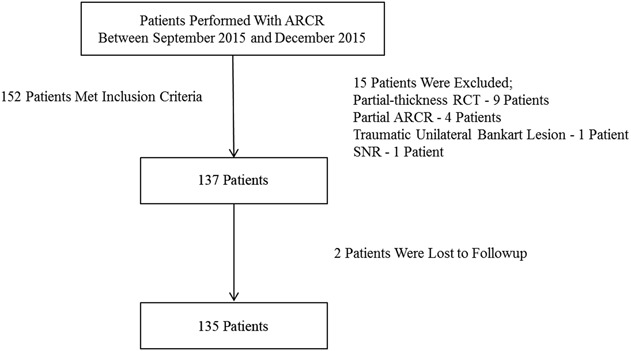
Flowchart showing the number of patients who met the study criteria. ARCR = arthroscopic rotator cuff repair; RCT = rotator cuff repair; SNR = suprascapular nerve release.
Table 1.
Demographic data according to (A) dominant shoulder, (B) tear size [7], and (C) tendon healing
Surgical Technique and Rehabilitation Protocol
Arthroscopic rotator cuff repair is performed on most patients. Open rotator cuff repair is chosen when tear size is ≥ 3 cm and satisfactory repair is difficult as a result of poor tendon quality or tendon mobility. All patients undergoing arthroscopic rotator cuff repair underwent surgery in a 70° beachchair position. The glenohumeral joint was assessed through a standard posterior-viewing portal. Intraarticular injuries were also investigated, including the degree of rotator cuff tear and lesions of the biceps tendon. The subacromial space was entered after arthroscopic examination. Subacromial bursectomy was performed through a lateral portal, and when required, acromioplasty was performed simultaneously. A posterolateral portal was created just behind the posterolateral corner of the acromion to provide a “Grand Canyon view” and was used as a viewing portal during the repair procedure, whereas the portals that had been created before were used as working and waiting portals. The tear size was determined on the basis of the measurements obtained during surgery. The tear size was measured by inserting the calibrated probe through the posterior and lateral portals. The decision of whether to use a single- or double-row technique was made based on the patient’s tendon length and mobility. In all cases of tear size < 1 cm, single-row repair was performed. If the tear size was > 1 cm, double-row repair was performed if the torn tendon could be covered from the medial to the lateral footprint without undue tension when the cuff tendon was pulled with a grasper [7].
For single-row repairs, a hole was made in the greater tuberosity with a bone punch through an accessary superolateral portal. The suture anchor was inserted through the superolateral portal. The single-row repair was performed by placing a suture shuttle through the tendon using a Banana SutureLasso™ (Arthrex, Naples, FL, USA) through the anterior, superior, and posterior portals [29]. The approximation of the tear margins was examined after repair, and an additional tendon-to-tendon repair was performed with Ethilon 2 (Ethicon, Somerville, NJ, USA) when needed.
For double-row repairs, the suture anchor was placed at the sulcus or articular margin. The suture was passed through the tendon as medially as possible, ideally 10 to 12 mm medial to the lateral edge of the torn tendon, to maximize the amount of lateral tendon available for compression. A medial row was repaired with suture anchors. The suture limbs were then used to make suture bridges over the tendon. The lateral fixation was placed 1 cm distal-lateral to the lateral edge of the tuberosity footprint insertion using the lateral anchor.
For all small-sized tears, single-row repair was performed. For all medium-sized tears, double-row repair was performed. For large-to-massive-sized tears, double- and single-row repairs were performed in 43 and two shoulders, respectively.
All patients were given a standard postoperative rehabilitation program. On the first postoperative day, they performed passive ROM exercises such as pendulum and passive forward flexion exercises. The patients first performed the passive ROM exercises within a tolerable range and were instructed to do the exercises four times a day, 10 repetitions each time. Active-assisted motion was initiated starting 6 weeks postoperatively. Three months after the operation, patients were permitted to practice light sports activities. This was followed by muscle-strengthening exercises. Finally, the patients were instructed to return to recreational activities that place heavy demands on the shoulders 6 months postoperatively. We instructed patients to exercise within their possible range from 6 months after surgery.
Clinical Evaluation
The senior author (YGR) examined the patients preoperatively and postoperatively. All the patients underwent a physical examination 1 day before surgery. Postoperative examinations were conducted in the outpatient setting at 1 month, 2 months, 3 months, 6 months, 9 months, 1 years, 15 months, 18 months, and 2 years after surgery. Two patients were lost to followup within 2 years after surgery. One patient was lost to followup during the first month after surgery, and the other patient was lost to followup 6 months after surgery. During the outpatient examinations, the patients were categorized according to the factors that can affect the postoperative recovery period, including their age and sex, whether the operation was performed on the dominant shoulder, the size of the rotator cuff tear before surgery, and fatty infiltration of the infraspinatus [5, 22, 32]. The size of the rotator cuff tear, which was obtained during surgery, was classified by using the DeOrio and Cofield classification [12]. DeOrio and Cofield used the length of the greatest diameter of the tear to divide the tear into small, medium, and large-to-massive tear-sized groups. To compare the demographic data and postoperative daily activities according to tear size, large and massive tears were grouped into one for analysis.
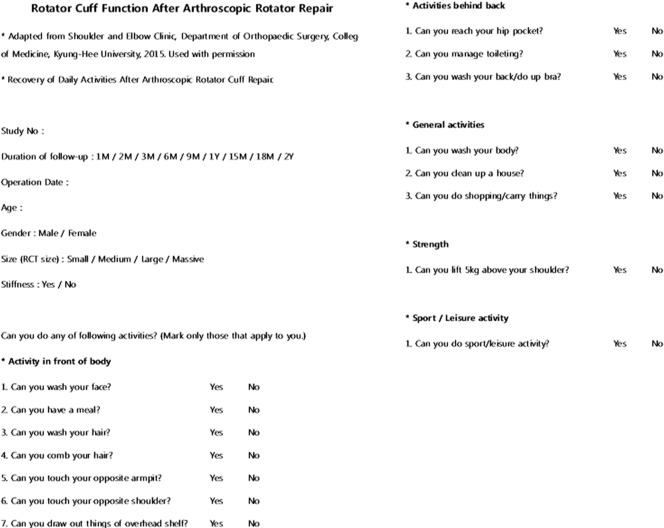
The patients were asked to fill out a questionnaire at every postoperative outpatient visit (Fig. 2). The questions in the questionnaire were created based on the questions patients usually ask in the outpatient clinic and with reference to the functional question of the UCLA score [33] and American Shoulder and Elbow Surgeons score [30]. The questionnaire content was based on the questions that outpatients commonly ask and divided into front-of-the-body, behind-the-back, general, simple strength-related, and sports/leisure activities. The front-of-the-body activities included whether patients can wash their face, have a meal, wash and comb their hair, touch the opposite armpit and shoulder, or retrieve items from an overhead shelf. The behind-the-back activities included whether patients can touch their hip pocket, manage toileting, wash their back, or fasten a bra. General activities included taking a bath, cleaning the house, and shopping. For simple strength-related activities, patients were asked whether they could lift something weighing 5 kg with the operative arm only to shoulder level. For sports/leisure activities, patients were asked whether they engaged in any sports or leisure activities after surgery.
Fig. 2.
The questionnaire included front-of-the-body activities, behind-the-back activities, general activities, simple strength-related activities, and sports/leisure. M = month; Y = year; RCT = rotator cuff repair. Adapted from the Shoulder and Elbow Clinic, Department of Orthopaedic Surgery, College of Medicine, Kyung-Hee University, 2015. Used with permission.
Among the front-of-body activities, washing the hair, combing the hair, and retrieving things from overhead shelves were included as high-level activities, and all other movements were considered low-level activities. Among the activities behind the back, washing the back or fastening a bra were considered high-level activities, whereas reaching the hip pocket and toileting were considered low-level activities.
Forward flexion, external rotation at the side, internal rotation posteriorly, and abduction of the shoulder were measured with a goniometer for preoperative and postoperative shoulder ROM. The patients’ shoulders were assessed preoperatively and postoperatively using the UCLA shoulder score [33]. Based on the UCLA shoulder assessment, we considered functional outcomes > 28 points (score > 80% in each UCLA score component) as favorable; when the pain score was > 8 points, the function score was > 8 points, the active forward flexion score was > 4 points, the strength score of forward flexion was > 4 points, and the satisfaction score of the patient was 4 points.
Radiologic Evaluation
Fatty degeneration of the infraspinatus was assessed on MRI scans in the oblique sagittal Y view and classified according to the Goutallier classification [14]. The classification involved five stages scored 0 to 4 with Stage 0 indicating no fat; Stage 1, the muscle contained some fatty streaks; Stage 2, more muscle than fat; Stage 3, equal fat and muscle; and Stage 4, more fat than muscle.
Nine months after surgery, a followup MRI evaluation was performed on all patients to determine rotator cuff integrity and the healing status of the repaired tendon. When a fluid-equivalent signal or discontinuity in the repaired tendon was observed on at least one of the followup T2-weighted MR images, it was diagnosed as a full-thickness retear and deemed to show structural failure.
Statistical Analyses
The primary outcome of this study was a recovery period for sports/leisure in small, medium, and large-to-massive tear-sized groups. A pilot study was conducted on 15 patients with small-sized tears, 15 patients with medium-sized tears, and 15 patients with large-to-massive-sized tears to investigate the time of sports/leisure recovery. Based on this, six patients were needed for each group with α error protection of 0.05 and a power of 0.95. Considering a 10% followup loss and 10% nonresponse during the study period, we decided that we needed eight patients at least in each group. Assuming α error protection of 0.05 and 45 shoulders in each group, the power analysis showed that the power of this study was > 99%. Therefore, the sample size of this study was considered appropriate.
When comparing three groups according to tear size, two groups according to arm dominance, and two groups according to tendon healing, continuous variables were analyzed with Student’s t-test, and categorical data were analyzed with the chi-square test or Fisher’s exact test. A one-way analysis of variance test was conducted to compare groups differentiated by the size of the rotator cuff tear. SPSS software (Version 20.0; SPSS, Chicago, IL, USA) was used for statistical analysis, and p < 0.05 was considered to indicate statistical significance.
Results
Time to Recovery
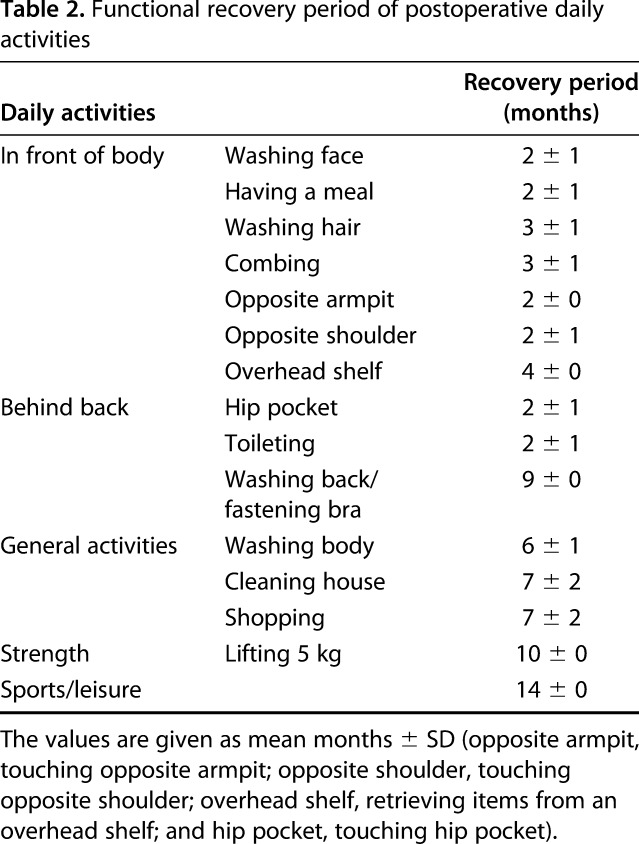
The patients experienced functional recovery of low-level and high-level ROM front-of-the-body, low-level and high-level ROM behind-the-back, simple strength-related, and sports/leisure activities within 2 ± 1, 3 ± 2, 2 ± 1, 9 ± 0, 10 ± 2, and 14 ± 3 months of surgery, respectively, after arthroscopic rotator cuff repair. For front-of-the-body activities after the surgery, the activities of washing their face, having a meal, washing their hair, combing their hair, touching the opposite armpit, and touching the opposite shoulder were recovered at 2 ± 1, 2 ± 1, 3 ± 1, 3 ± 2, 2 ± 0, and 2 ± 1 months, respectively. In addition, they could retrieve an item from an overhead shelf 4 ± 0 months after surgery. For behind-the-back activities, the patients could touch their hip pocket and manage toileting within 3 months after surgery. At 9 ± 0 months after surgery, the patients could wash their back or fasten a bra. For general activities, the patients could take a bath, clean the house, and shop within 7 months after surgery. Moreover, they could lift a 5-kg item above shoulder level at 10 ± 0 months after surgery and engage in sports or leisure activities at 14 ± 0 months after surgery (Table 2). All patients in the small and medium tear-sized groups stated that they achieved functional recovery after surgery. However, two patients in the large-to-massive tear group answered that they recovered most activities, except washing their back or fastening a bra, lifting a 5-kg item above shoulder level, and sports/leisure.
Table 2.
Functional recovery period of postoperative daily activities
Tear Size, Dominance, and Retear
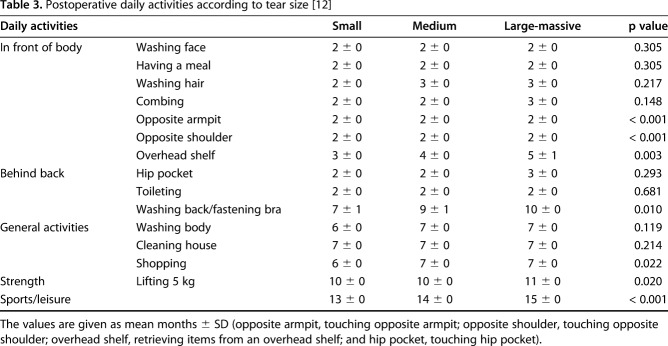
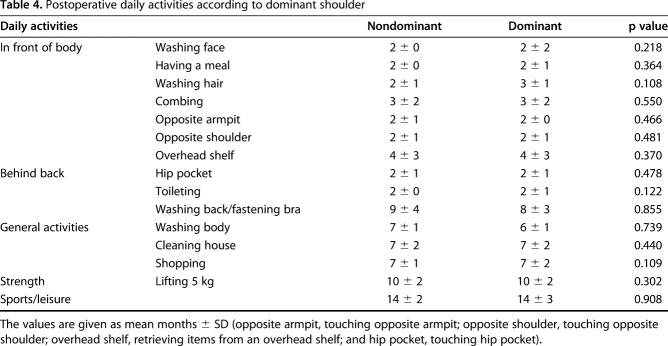
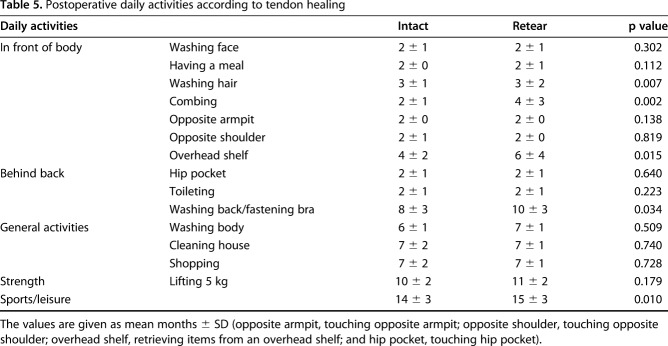
There were no substantial differences in the recovery period of touching the opposite armpit and shoulder among the small, medium, and large-to-massive tear groups, but the differences were statistically different (Table 3). Retrieving items from an overhead shelf, washing the back/fastening a bra, shopping, lifting 5 kg, and sports/leisure took longer to recover in the large-to-massive group than that in the small and medium groups (5 ± 1 versus 3 ± 0 versus 4 ± 0, p = 0.003 for overhead shelf; 10 ± 0 versus 7 ± 1 versus 9 ± 1, p = 0.010 for washing the back/fastening a bra; 7 ± 0 versus 6 ± 0 versus 7 ± 0, p = 0.022 for shopping; 11 ± 0 versus 10 ± 0 versus 10 ± 0, p = 0.020 for lifting 5 kg; 15 ± 0 versus 13 ± 0 versus 14 ± 0, p < 0.001 for sports/leisure) (Table 3). Arm dominance was not associated with functional recovery (Table 4). Between the intact healing and retear groups, there were differences in high-level ROM front-of-the-body activities such as washing hair, combing hair, and retrieving items from an overhead shelf (3 ± 1 versus 3 ± 2, p = 0.007 for washing hair; 2 ± 1 versus 4 ± 3, p = 0.002 for combing hair; 4 ± 2 versus 6 ± 4, p = 0.015 for retrieving items from an overhead shelf). There were also differences in washing the back/fastening a bra and sports/leisure recovery between the intact healing group and the retear group (8 ± 3 versus 10 ± 3, p = 0.034 for washing the back/fastening a bra; 14 ± 3 versus 15 ± 3, p = 0.010 for sports/leisure) (Table 5).
Table 3.
Postoperative daily activities according to tear size [12]
Table 4.
Postoperative daily activities according to dominant shoulder
Table 5.
Postoperative daily activities according to tendon healing
UCLA Score
Only one patient with a large-to-massive tear did not reach the threshold of 28 points during the study period. Other patients (134 patients) recovered to a UCLA score of 28 or higher. The UCLA score crossed the threshold of 28 points at 6 ± 3 months. The UCLA shoulder score improved from 11 ± 2 preoperatively to 34 ± 2 at last followup (p < 0.001). The UCLA shoulder score improved gradually after surgery, but the improvement slowed down with time (Fig. 3).
Fig. 3.
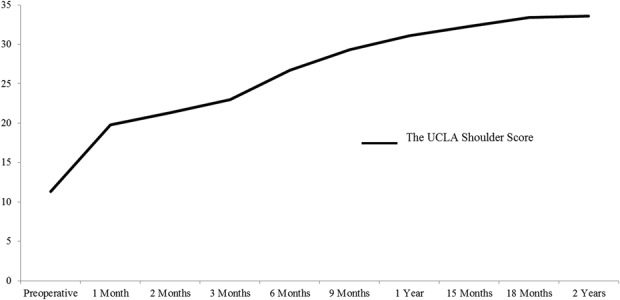
The UCLA shoulder scores [17] were improved after arthroscopic rotator cuff repair. The improvement range of the mean UCLA shoulder scores steadily decreased.
Discussion
When deciding whether to perform arthroscopic rotator cuff repair, the postoperative recovery period is a main factor in the patient’s decision to undergo surgery. However, if patients ask the surgeon about the postoperative recovery period, the surgeon would not be able to give a precise answer. Because all previous studies on functional recovery of daily activities used clinical scores to evaluate recovery [4, 8, 21], the time to functional recovery of specific movements has not yet been reported, to our knowledge. Therefore, we wanted to determine (1) when patients can perform low-level and high-level front-of-body activities, low-level and high-level behind-the-back activities, strength-related activities, and sports/leisure activities after arthroscopic rotator cuff repair; (2) if tear size, arm dominance, and retear affect performance of these activities; and (3) when the UCLA score crosses above 80% in each UCLA score component.
Our study had a few limitations. First, because the followup was set to 2 years, recovery after the second postoperative year could not be examined. However, according to previous studies [4], functional recovery of daily activities plateaus after the first postoperative year. Even in the present study, the UCLA shoulder scores plateaued with time. Therefore, we think that recovery after the second postoperative year would not substantially change the results of our study. Second, large and massive tears were put into the same group for comparison with small and medium tears. Third, there may be a gap between the real recovery period and the recovery period on the questionnaire. It is practically difficult for patients to visit the outpatient clinic every week, so there may be a gap between when they recovered the activities of daily living after surgery and when they answered the questionnaire. Fourth, the degree of difficulty for each activity and level of sports activities was not required on the questionnaire. Because the questionnaire included “yes or no” questions, it was possible that patients might answer “yes” even if they perform an activity with difficulty. However, this study focused on when patients could recover their daily activities after surgery. Thus, additional studies would be necessary to consider the difficulty of each activity in the future. Furthermore, the fact that patients stated that they recovered each activity might suggest that they were satisfied with the surgery.
In this study, patients experienced functional recovery of low-level and high-level ROM front-of-the-body, low-level and high-level ROM behind-the-back, simple strength-related, and sports/leisure activities within 2 ± 1, 3 ± 2, 2 ± 1, 9 ± 0, 10 ± 2, and 14 ± 3 months, respectively, after arthroscopic rotator cuff repair. To our knowledge, the functional recovery period of daily activities for specific movements after arthroscopic rotator cuff repair has not been reported. The findings of this study can more accurately pinpoint the time of recovery after surgery, so it would be helpful to satisfy patients’ personal and socioeconomic needs after surgery.
According to previous studies, the larger the size of a tear, the more adverse effects it has on functional recovery [21, 25]. In our study, recovery was delayed for high-level ROM activities, strength-related activities, and sports/leisure activities with a larger tear size, but there were no differences in time of recovery of low-level ROM activities according to tear size. This was probably because high-demand activities required a longer rehabilitation period after surgery. Charousset et al. [4] reported that the side of the operation (dominant versus nondominant) did not correlate with postoperative functional recovery. Our study also found no correlation between the postoperative functional recovery and the dominance of the shoulder that underwent surgery. On the other hand, the effect of postoperative retears on functional recovery is controversial. Some studies [4, 11, 13] represented a correlation between tendon healing and functional outcome, whereas Namdari et al. [24] reported that structural failure had adverse effects only for labor-intensive workers. Moreover, in other studies [3, 8, 15, 17, 31], a lack of healing did not necessarily affect functional recovery. Our study did not find differences for most activities between the retear and intact healing groups apart from high-level ROM and sports/leisure activities. The group with postoperative retears seemed able to achieve functional shoulders by maintaining a balanced rotator cuff [2, 23].
Several studies have been conducted on periods of functional recovery after arthroscopic rotator cuff repair [4, 8, 21]. Charousset et al. [4] defined favorable outcome of functional recovery after arthroscopic rotator cuff repair as achieving a Constant score [9] of > 70%. They showed functional recovery as early as 3 months after surgery. Manaka et al. [21] considered the functional recovery period as the time required to accomplish a point of > 80% based on the Japanese Orthopaedic Association score [16]. They reported that 31% and 40% of patients attained functional recovery at < 3 and 6 months after arthroscopic rotator cuff repair, respectively. In our study, it took an average of 6 months for patients to reach a UCLA score of 80% or greater, after which they reached a plateau. However, when sports/leisure activities were set as the final stage of recovery of daily activities, the mean duration of recovery was 14 months. Therefore, the recovery period of clinical scores did not coincide with the recovery period of daily activities. This study would be helpful to more accurately identify the time of functional recovery after arthroscopic rotator cuff repair.
In conclusion, it took an average of 14 months to recover activities of daily living after arthroscopic rotator cuff repair. Patients first gained low-level ROM activities, then high-level ROM front-of-body activities, then general activities, then high-level ROM behind-the-back activities, then simple strength-related activities, and finally sports/leisure activities. Tear size and retear affected only the time of recovery of high-level motion activities and sports/leisure. The results of this study were believed to serve as a guideline to inform patients about functional recovery after arthroscopic rotator cuff repair.
Acknowledgments
We thank Dr Young Moon Kee for assistance during surgery and for postoperative patient care.
Footnotes
Each author certifies that neither he or she, nor any member of his or her immediate family, has funding or commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
Each author certifies that his or her institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at the Department of Orthopaedic Surgery, Kyung Hee University Hospital, College of Medicine, Seoul, Republic of Korea.
References
- 1.Antoni M, Klouche S, Mas V, Ferrand M, Bauer T, Hardy P. Return to recreational sport and clinical outcomes with at least 2 years follow-up after arthroscopic repair of rotator cuff tears. Orthop Traumatol Surg Res. 2016;102:563-567. [DOI] [PubMed] [Google Scholar]
- 2.Burkhart SS, Esch JC, Jolson RS. The rotator crescent and rotator cable: an anatomic description of the shoulder's 'suspension bridge.' Arthroscopy. 1993;9:611-616. [DOI] [PubMed] [Google Scholar]
- 3.Castagna A, Delle Rose G, Conti M, Snyder SJ, Borroni M, Garofalo R. Predictive factors of subtle residual shoulder symptoms after transtendinous arthroscopic cuff repair: a clinical study. Am J Sports Med. 2009;37:103-108. [DOI] [PubMed] [Google Scholar]
- 4.Charousset C, Grimberg J, Duranthon LD, Bellaiche L, Petrover D, Kalra K. The time for functional recovery after arthroscopic rotator cuff repair: correlation with tendon healing controlled by computed tomography arthrography. Arthroscopy. 2008;24:25-33. [DOI] [PubMed] [Google Scholar]
- 5.Cho CH, Ye HU, Jung JW, Lee YK. Gender affects early postoperative outcomes of rotator cuff repair. Clin Orthop Surg. 2015;7:234-240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cho NS, Rhee YG. Functional outcome of arthroscopic repair with concomitant manipulation in rotator cuff tears with stiff shoulder. Am J Sports Med. 2008;36:1323-1329. [DOI] [PubMed] [Google Scholar]
- 7.Cho NS, Yi JW, Lee BG, Rhee YG. Retear patterns after arthroscopic rotator cuff repair: single-row versus suture bridge technique. Am J Sports Med. 2010;38:664-671. [DOI] [PubMed] [Google Scholar]
- 8.Collin P, Abdullah A, Kherad O, Gain S, Denard PJ, Ladermann A. Prospective evaluation of clinical and radiologic factors predicting return to activity within 6 months after arthroscopic rotator cuff repair. J Shoulder Elbow Surg. 2015;24:439-445. [DOI] [PubMed] [Google Scholar]
- 9.Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987;214:160-164. [PubMed] [Google Scholar]
- 10.Denard PJ, Ladermann A, Brady PC, Narbona P, Adams CR, Arrigoni P, Huberty D, Zlatkin MB, Sanders TG, Burkhart SS. Pseudoparalysis from a massive rotator cuff tear is reliably reversed with an arthroscopic rotator cuff repair in patients without preoperative glenohumeral arthritis. Am J Sports Med. 2015;43:2373-2378. [DOI] [PubMed] [Google Scholar]
- 11.Denard PJ, Ladermann A, Burkhart SS. Prevention and management of stiffness after arthroscopic rotator cuff repair: systematic review and implications for rotator cuff healing. Arthroscopy. 2011;27:842-848. [DOI] [PubMed] [Google Scholar]
- 12.DeOrio JK, Cofield RH. Results of a second attempt at surgical repair of a failed initial rotator-cuff repair. J Bone Joint Surg Am. 1984;66:563-567. [PubMed] [Google Scholar]
- 13.Gerber C, Schneeberger AG, Perren SM, Nyffeler RW. Experimental rotator cuff repair. A preliminary study. J Bone Joint Surg Am. 1999;81:1281-1290. [DOI] [PubMed] [Google Scholar]
- 14.Goutallier D, Postel JM, Bernageau J, Lavau L, Voisin MC. Fatty muscle degeneration in cuff ruptures. Pre- and postoperative evaluation by CT scan. Clin Orthop Relat Res. 1994;304:78-83. [PubMed] [Google Scholar]
- 15.Hanusch BC, Goodchild L, Finn P, Rangan A. Large and massive tears of the rotator cuff: functional outcome and integrity of the repair after a mini-open procedure. J Bone Joint Surg Br. 2009;91:201-205. [DOI] [PubMed] [Google Scholar]
- 16.Ide J, Tokiyoshi A, Hirose J, Mizuta H. Arthroscopic repair of traumatic combined rotator cuff tears involving the subscapularis tendon. J Bone Joint Surg Am. 2007;89:2378-2388. [DOI] [PubMed] [Google Scholar]
- 17.Jost B, Zumstein M, Pfirrmann CW, Gerber C. Long-term outcome after structural failure of rotator cuff repairs. J Bone Joint Surg Am. 2006;88:472-479. [DOI] [PubMed] [Google Scholar]
- 18.Kang L, Henn RF, Tashjian RZ, Green A. Early outcome of arthroscopic rotator cuff repair: a matched comparison with mini-open rotator cuff repair. Arthroscopy. 2007;23:573-582, 582.e1-2. [DOI] [PubMed] [Google Scholar]
- 19.Klouche S, Lefevre N, Herman S, Gerometta A, Bohu Y. Return to sport after rotator cuff tear repair: a systematic review and meta-analysis. Am J Sports Med. 2016;44:1877-1887. [DOI] [PubMed] [Google Scholar]
- 20.Lazarides AL, Alentorn-Geli E, Choi JH, Stuart JJ, Lo IK, Garrigues GE, Taylor DC. Rotator cuff tears in young patients: a different disease than rotator cuff tears in elderly patients. J Shoulder Elbow Surg. 2015;24:1834-1843. [DOI] [PubMed] [Google Scholar]
- 21.Manaka T, Ito Y, Matsumoto I, Takaoka K, Nakamura H. Functional recovery period after arthroscopic rotator cuff repair: is it predictable before surgery? Clin Orthop Relat Res. 2011;469:1660-1666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.McElvany MD, McGoldrick E, Gee AO, Neradilek MB, Matsen FA., 3rd Rotator cuff repair: published evidence on factors associated with repair integrity and clinical outcome. Am J Sports Med. 2015;43:491-500. [DOI] [PubMed] [Google Scholar]
- 23.Mesiha MM, Derwin KA, Sibole SC, Erdemir A, McCarron JA. The biomechanical relevance of anterior rotator cuff cable tears in a cadaveric shoulder model. J Bone Joint Surg Am. 2013;95:1817-1824. [DOI] [PubMed] [Google Scholar]
- 24.Namdari S, Donegan RP, Chamberlain AM, Galatz LM, Yamaguchi K, Keener JD. Factors affecting outcome after structural failure of repaired rotator cuff tears. J Bone Joint Surg Am. 2014;96:99-105. [DOI] [PubMed] [Google Scholar]
- 25.Nho SJ, Shindle MK, Adler RS, Warren RF, Altchek DW, MacGillivray JD. Prospective analysis of arthroscopic rotator cuff repair: subgroup analysis. J Shoulder Elbow Surg. 2009;18:697-704. [DOI] [PubMed] [Google Scholar]
- 26.Ozbaydar MU, Tonbul M, Tekin AC, Yalaman O. [Arthroscopic rotator cuff repair: evaluation of outcomes and analysis of prognostic factors] [in Turkish]. Acta Orthop Traumatol Turc. 2007;41:169-174. [PubMed] [Google Scholar]
- 27.Pearsall AW, 4th, Ibrahim KA, Madanagopal SG. The results of arthroscopic versus mini-open repair for rotator cuff tears at mid-term follow-up. J Orthop Surg Res. 2007;2:24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Peters KS, McCallum S, Briggs L, Murrell GA. A comparison of outcomes after arthroscopic repair of partial versus small or medium-sized full-thickness rotator cuff tears. J Bone Joint Surg Am. 2012;94:1078-1085. [DOI] [PubMed] [Google Scholar]
- 29.Rhee YG, Vishvanathan T, Thailoo BKBR, Rojpornpradit T, Lim CT. The '3 sister portals' for arthroscopic repair of massive rotator cuff tears. Tech Shoulder Elbow Surg. 2007;8:53-57. [Google Scholar]
- 30.Richards RR, An KN, Bigliani LU, Friedman RJ, Gartsman GM, Gristina AG, Iannotti JP, Mow VC, Sidles JA, Zuckerman JD. A standardized method for the assessment of shoulder function. J Shoulder Elbow Surg. 1994;3:347-352. [DOI] [PubMed] [Google Scholar]
- 31.Russell RD, Knight JR, Mulligan E, Khazzam MS. Structural integrity after rotator cuff repair does not correlate with patient function and pain: a meta-analysis. J Bone Joint Surg Am. 2014;96:265-271. [DOI] [PubMed] [Google Scholar]
- 32.Saccomanno MF, Sircana G, Cazzato G, Donati F, Randelli P, Milano G. Prognostic factors influencing the outcome of rotator cuff repair: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2016;24:3809-3819. [DOI] [PubMed] [Google Scholar]
- 33.Wolf EM, Pennington WT, Agrawal V. Arthroscopic rotator cuff repair: 4- to 10-year results. Arthroscopy. 2004;20:5-12. [DOI] [PubMed] [Google Scholar]