History
Calcaneus fracture classification systems have evolved since Malgaine [10] first described them in 1843, before the advent of roentgenography. The French surgeon described two types of fracture mechanisms: an avulsion injury resulting from muscular pull and a crushing injury. In 1931, Böhler described the first comprehensive calcaneal fracture classification scheme with eight fracture patterns based on plain radiographs, proposing two major groups: intraarticular and extraarticular [1, 2]. In 1952, Essex-Lopresti [5] further distinguished intraarticular fracture patterns into two types (depending on the exit point of the secondary fracture line): “tongue type” and “joint depression” fractures. This classification scheme aided the surgeon in determining the treatment plan but had limited prognostic relevance. Subsequently, in 1975, Soeur and Remy [19] proposed a classification scheme based on the number of articular fragments and fracture displacement as determined on AP, lateral, and Harris axial heel views of the calcaneus. This classification was based on the extent of posterior facet articular involvement. First-degree fractures were nondisplaced shear-type fractures with widening of the joint surface. Second-degree fractures included a secondary fracture line, which produced at least three fragments. Third-degree fractures were highly comminuted, and as such, they could not be classified. Soeur et al. recommended operative management of displaced intraarticular fracture of the calcaneus, but their clinical results did not correlate with the proposed classification scheme [15].
The advent of CT in the 1980s revolutionized the characterization and management of calcaneal fractures, leading to a better understanding of the fracture anatomy. Zwipp et al. [22] were the first to use information garnered from CT imaging to classify calcaneal fractures. Their scheme, similar to previous classification systems based on radiographs, divided the entire calcaneus into a total of five possible fragments. They also incorporated the number of affected joint facets and the degree of soft tissue damage into a 12-point scoring system that was of prognostic relevance [11]. In 1990, Crosby and Fitzgibbons [4] developed a classification system based on articular surface displacement (nondisplaced, displaced, and comminuted fractures). They were the first to correlate clinical outcomes with a CT-based classification scheme [4]. This clinical correlation was limited to nonoperative treatment of a calcaneus fracture; nonetheless, they were able to predict which fracture type would do well with closed treatment and which would not [4]. In 1993, Sanders et al. [13] described their classification system as the rational extension of the fracture patterns identified by Soeur and Remy [19]. This system was based on the number and location of articular fracture fragments seen on coronal and axial CT images. It became the pillar for understanding calcaneus fractures, preoperative planning, and predicting patient prognosis.
Recently an AO classification for calcaneal fractures has been developed by the foot expert group [21]. This classification scheme uses the ABC classification regularly used for long bone fractures, which is organized into three hierarchical types with 27 subgroups. Furthermore, a new type, D, representing pure dislocation with soft tissue injury has been added. Type A are extraarticular fractures. Type B are intraarticular fractures with at least half of the articular surface within the regular confines of the joint. Type C are articular fractures with dislocation. In this system the calcaneus is divided into three segments: proximal (body including the tuberosity and posterior facet), middle (sustentaculum tali with the middle facet and sulcus), and distal (anterior process including the anterior facet and the cuboidal facet).
Purpose
The calcaneus is the most commonly fractured tarsal bone, accounting for 2% of all fractures that present to the emergency department [18]. Most calcaneal fractures are caused by high-energy mechanisms, where concentrated axial loading forces from the heel drive the talus distally into the calcaneus. Intraarticular fractures cause loss of height and subtalar joint disruption. Most intraarticular calcaneus fractures are treated surgically, but it is challenging because of associated soft tissue damage, primary cartilage damage resulting from the impact at the time of the injury, complex fracture configuration with numerous articular fragments, and a steep learning curve required before obtaining consistent and predictable results with operative fixation. Inaccurate reductions can result in substantial deformity, functional impairment, disability, and chronic pain; however, even when anatomic reduction is achieved, pain and disability may still follow, because the high loads experienced by the articular cartilage may predispose even well-reduced fractures to subsequent posttraumatic arthritis. Furthermore, because most calcaneal fractures occur during the peak earning years of men who perform labor for a living, the economic implications of poorly treated calcaneal fractures can also be substantial [12].
In general, fracture classification schemes should (1) allow the orthopaedic surgeon to identify and communicate injury patterns; (2) help guide treatment decision-making; (3) facilitate preoperative planning and guide surgical management if surgery is indicated; and (4) provide prognostic information.
The intended purpose of the landmark publication by Sanders et al. [13] was to describe intraarticular calcaneal fractures with an emphasis on guiding restoration of the articular surface from a lateral surgical approach. The authors noted that previous publications focused more on correction of calcaneal body shape and restoration of Böhler’s angle. Sanders et al. [13] argued that by solely using a lateral surgical approach, one may address both calcaneal articular and body disruptions.
The prognostic importance of the Sanders classification was established in their original series of 120 displaced calcaneal fractures [13]. This was intended to aid in surgical decision-making by demonstrating that outcomes as assessed with the Maryland Foot Score deteriorated as the number of articular fragments increased. The authors attributed poor clinical outcomes such as the failure to achieve anatomic reduction with greater fracture comminution resulting from the operative difficulty [13]. Anatomic articular reduction verified by CT scan at 1 year was greatest for Type II fractures (86%) compared with Type III (60%) and Type IV (0%) fractures. Long-term (10–20 years) outcomes reported by Sanders [12] in a subsequent study demonstrated that Type III fractures had a higher risk for subtalar arthrodesis (18 of 38 [47.4%]) compared with Type II fractures (13 of 70 [18.6%]). The authors also stated that the Sanders ABC subclassification of calcaneal fractures that refers to the location of the primary fracture line was useful for surgical planning but was not prognostic for posterior facet articular reduction nor for restoring the calcaneocuboid joint.
Description
Sanders et al.’s [13] original description of intraarticular calcaneal fracture classification was based on coronal and axial CT cross-sections with the widest undersurface of the posterior facet of the talus (Fig. 1). Ideally, the CT scans are formatted in two planes: the semicoronal or oblique coronal plane, which is perpendicular to the posterior facet of the calcaneus’ normal position, and the axial plane, which is parallel to the sole of the foot. The talus is divided into three equal columns by two lines, A and B. These lines extend across the posterior facet of the calcaneus and represent potential fracture lines [12, 13]. A third fracture line (line C) represents the medial edge of the posterior facet. Together, the three lines (A, B, and C from lateral to medial) divide the posterior facet into four potential fracture fragments: lateral, central, medial, and sustentaculum fragments [12, 13].
Fig. 1.
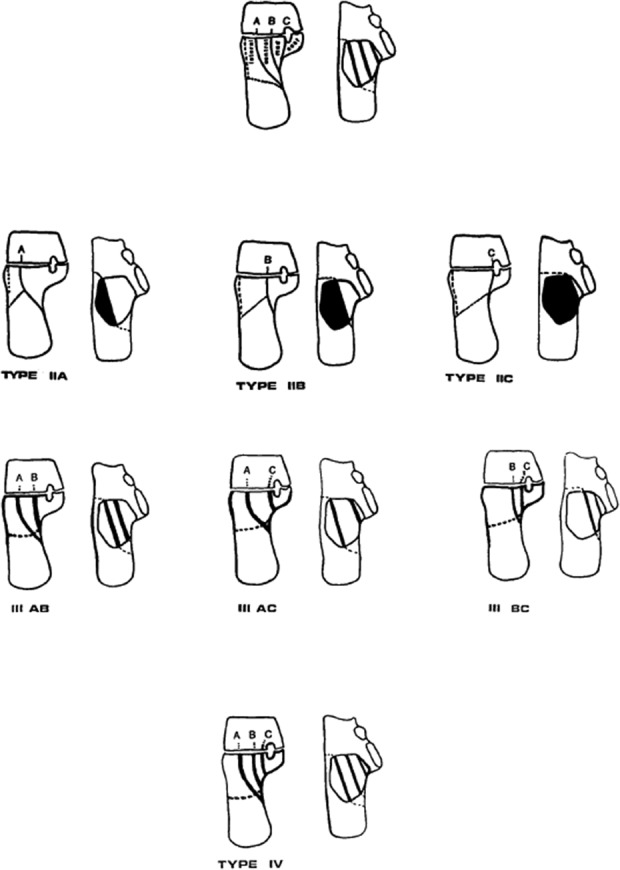
Schematic illustrates the Sanders classification of intraarticular fractures of the calcaneus in coronal and axial CT cross-sections with the widest undersurface of the posterior facet of the talus. Fracture lines A, B, and C describe the position of the primary fracture line in relation to the posterior facet and the subtalar joint. Type 1 fractures are minimally displaced and are not depicted. Reprinted with permission from Sanders R, Fortin P, DiPasquale T, Walling A. Operative treatment in 120 displaced intraarticular calcaneal fractures. Results using a prognostic computed tomography scan classification. Clin Orthop Relat Res. 1993;290:87-95.
Type I fractures include all minimally displaced (≤ 2 mm) articular fractures, regardless of the number of fracture lines and fragments present. The original publication by Sanders et al. [13] did not specify the degree of articular incongruity but did recommend surgical management in patients with ≥ 3 mm of articular displacement [13]. A subsequent multicenter, prospective, randomized controlled trial on operative versus nonoperative treatments of displaced calcaneus fractures defined displacement as > 2 mm of articular incongruity [3]. The authors of that randomized controlled trial performed operative treatment on patients with ≥ 3 mm of articular displacement based on axial and coronal CT imaging of the posterior facet [3]. Sanders [12] recommended nonoperative treatment for Type I fractures.
Type II fractures are displaced two-part fractures of the posterior facet with one primary fracture line that can be accompanied by one or more accessory fracture lines that do not involve the posterior articular facet. Three Type II subtypes exist, IIA, IIB, and IIC, with the letter corresponding to the location of the primary fracture line.
Type III fractures include three-part fractures of the posterior facet from two primary fracture lines commonly accompanied by a central area of depression. Sanders et al. described this phenomenon as akin to a split-depression tibial plateau fracture. Subtypes include IIIAB, IIIAC, and IIIBC, according to the location of the two primary fracture lines.
Type IV fractures involve three or more primary fracture lines, resulting in four or more articular fragments with severe comminution (Fig. 1).
Validation
The Sanders classification is extensively utilized and popularized by orthopaedic surgeons, radiologists, and other clinicians [17, 18]. Despite its widespread use, the value of this classification scheme has been a point of debate as a result of its limited reliability and validity. Attempts to validate the Sanders classification have demonstrated, at best, fair interobserver reliability and fair-to-moderate intraobserver reliability [8, 9, 16, 17, 21]. In these studies, the interobserver reliability ranged from 0.25 to 0.52, whereas the intraobserver reliability ranged from 0.31 to 0.57. Therefore, these results demonstrate that the clinician should be cautious when using this classification system to guide treatment and as communication tool as a result of its limited reproducibility.
Several studies have demonstrated that reliability declines substantially when subclassification is used. Lauder et al. [9] evaluated reliability using two residents, two foot and ankle fellows, and four fellowship-trained orthopaedic surgeon observers at two different time points. They demonstrated moderate interobserver agreement (κ = 0.48) and greater agreement (κ = 0.55) when Sanders subclasses were excluded. However, intraobserver agreement was greater (κ = 0.57) particularly when subclasses were excluded (κ = 0.77) [12]. In another study by Bhattacharya et al. [1], five attending orthopeadic surgeons classified CT scans of 28 calcaneal fractures. They found only fair interobserver reliability (κ = 0.32) and moderate intraobserver reliability (κ = 0.42). Both improved when the subclassification scheme was removed (κ = 0.33 and κ = 0.45, respectively).
Humphrey et al. [8] demonstrated that when using a single carefully defined CT image as opposed to the full CT scan to simplify viewing, agreement of the fracture line location decreased as fracture complexity increased (90% agreement of Type II fractures and 52% of Type III fractures). Within that study, the mean interobserver κ value was 0.41 among 10 orthopaedic traumatologists with 5 years of postresidency experience [8]. In this study, the results indicated that the Sanders classification system has greater reliability for fractures at the extreme of the spectrum, but has poor reliability in discriminating between fractures in the midrange of the classification scheme [8].
Schepers et al. [17] evaluated reliability with 12 observers: six orthopaedic traumatologists and six radiologists who specialized in trauma and musculoskeletal radiology. They found moderate interobserver agreement using the Sanders classification when including the primary fracture line location and the ABC subclassification component with κ = 0.49. When not including the ABC subclassification component, it was also moderate with κ = 0.48. Radiologists in the same study demonstrated an interobserver κ value of 0.43 without subclasses, which decreased to 0.30 with subclasses [17]. Radiologists in this study demonstrated an interobserver κ value of 0.43 without subclasses, which decreased to 0.30 with subclasses [17]. Other studies, however, have demonstrated that the level of training and experience of the observers did not correlate with observer reliability and reproducibility [1, 7, 12].
Finally, the Sanders classification has not been shown to be more reproducible or reliable than other calcaneal classification systems such as the Zwipp, Essex-Lopreti, or Crosby classification [7, 9, 16].
Limitations
Although widely used since its introduction in 1993, the Sanders classification has several noted limitations. The Sanders classification system is specific for intraarticular calcaneal fractures and requires the use of CT images in the coronal plane adjusted to a perpendicular plane to the normal position of the posterior facet of the talus. Therefore, this system does not account for fracture displacement in the sagittal or axial planes relative to the widest undersurface of the posterior facet of the talus. Regarding operative treatment, as the fracture line goes lateral to medial, the operative view and the ability to obtain an anatomic reduction become more difficult [1, 13]. This reflects the prognostic value of the classification scheme, because there is good correlation with fracture type and clinical result [1, 13].
Perhaps the most widely articulated criticism of the Sander classification is its inconsistent reproducibility among orthopaedic surgeons and other clinicians [18]. Validity studies have demonstrated improved inter- and intraobserver reliability when the Sanders classification system is used without the subclassification that it was originally described with [6, 9], but this subclassification is one of the key components that makes this system an improvement over earlier classification schemes. Also, the descriptive utility of the Sanders classification relies on the inclusion of these fracture subclasses. Nonetheless, multiple studies on this classification scheme suggest poor reproducibility overall limiting the utility of this system as a communication and research tool [6, 8, 9, 16, 17]. In addition, intraobserver reliability for selecting operative treatment based on this classification system has been shown to be moderate, whereas interobserver reliability has been shown to be fair at best [20]. This may demonstrate that even if surgeons agree on how to classify a fracture according to this scheme, they may still disagree on how the patient should be treated.
Conclusions
Since its introduction > 20 years ago, the Sanders classification has been one of the most well-known and used systems for describing intraarticular calcaneal fractures [17, 18]. Multiple studies [13, 14] have also highlighted the utility of the system as a prognostic tool to assist the surgeon in counseling the patient with respect to expected outcomes. As the number of intraarticular fragments increases, the ability to obtain a satisfactory reduction and achieve a good-to-excellent outcome decreases. However, the Sander classification system does not have a direct correlation with the patient’s treatment [17].
Despite the popularity of the Sanders classification, multiple studies have demonstrated that this scheme lacks the reproducibility to be considered ideal and its reliability has not consistently demonstrated superiority over other classification systems. Surgeons and clinicians should be aware of the limitations regarding the interobserver and intraobserver reliability for this system. Multiple studies have demonstrated only fair-to-moderate reliability; therefore, this shortcoming greatly limits the application of this system to communicate with other physicians, to guide the treatment algorithm, and to anticipate prognosis. The Sanders classification system fails to meet all of the criteria required for an appropriate classification scheme. Ultimately, without stronger evidence supporting its validity and reliability, it cannot be recommended as a tool with which to routinely guide management and treatment options.
Footnotes
One of the authors (EM) received personal fees from Zimmer Biomet (Warsaw, IN, USA), outside the submitted work.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, of any drug or device before clinical use.
Each author certifies that his institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at the University of Kentucky, Lexington, KY, USA.
References
- 1.Bhattacharya R, Vassan UT, Finn P, Port A. Sanders classification of fractures of the os calcis. An analysis of inter- and intra-observer variability. J Bone Joint Surg Br. 2005;87:205-208. [DOI] [PubMed] [Google Scholar]
- 2.Böhler L. The Treatment of Fractures . Bristol, UK: John Wright & Sons; 1935. [Google Scholar]
- 3.Buckley R, Tough S, McCormack R, Pate G, Leighton R, Petrie D, Galpin R. Operative compared with nonoperative treatment of displaced intra-articular calcaneal fractures: a prospective, randomized, controlled multicenter trial. J Bone Joint Surg Am. 2002;84:1733-1744. [DOI] [PubMed] [Google Scholar]
- 4.Crosby LA, Fitzgibbons T. Computerized tomography scanning of acute intra-articular fractures of the calcaneus. A new classification system. J Bone Joint Surg Am. 1990;72:852-859. [PubMed] [Google Scholar]
- 5.Essex-Lopresti P. The mechanism, reduction technique, and results in fractures of the os calcis. Br J Surg. 1952;39:395-419. [DOI] [PubMed] [Google Scholar]
- 6.Furey A, Stone C, Squire D, Harnett J. Os calcis fractures: analysis of interobserver variability in using Sanders classification. J Foot Ankle Surg. 2003;42:21-23. [DOI] [PubMed] [Google Scholar]
- 7.Howells NR, Hughes AW, Jackson M, Atkins RM, Livingstone JA. Interobserver and intraobserver reliability assessment of calcaneal fracture classification systems. J Foot Ankle Surg. 2014;53:47-51. [DOI] [PubMed] [Google Scholar]
- 8.Humphrey CA, Dirschl DR, Ellis TJ. Interobserver reliability of a CT-based fracture classification system. J Orthop Trauma. 2005;19:616-622. [DOI] [PubMed] [Google Scholar]
- 9.Lauder AJ, Inda DJ, Bott AM, Clare MP, Fitzgibbons TC, Mormino MA. Interobserver and intraobserver reliability of two classification systems for intra-articular calcaneal fractures. Foot Ankle Int. 2006;27:251-255. [DOI] [PubMed] [Google Scholar]
- 10.Malgaine JF. Operative Surgery, Based on Normal and Pathological Anatomy . Philadelphia, PA, USA: Blanchard and Lea; 1851:1806-1865. [Google Scholar]
- 11.Rammelt S, Barthel A, Biewener J, Gavlik H, Zwipp H. [Calcaneus fractures. Open reduction and internal fixation] [in German]. Zentralblatt Chir. 2003;128:517-528. [DOI] [PubMed] [Google Scholar]
- 12.Sanders R. Displaced intra-articular fractures of the calcaneus. J Bone Joint Surg Am. 2000;82:225-250. [DOI] [PubMed] [Google Scholar]
- 13.Sanders R, Fortin P, DiPasquale T, Walling A. Operative treatment in 120 displaced intraarticular calcaneal fractures. Results using a prognostic computed tomography scan classification. Clin Orthop Relat Res. 1993;290:87-95. [PubMed] [Google Scholar]
- 14.Sanders R, Vaupel ZM, Erdogan M, Downes K. Operative treatment of displaced intraarticular calcaneal fractures: long-term (10-20 years) results in 108 fractures using a prognostic CT classification. J Orthop Trauma. 2014;28:551-563. [DOI] [PubMed] [Google Scholar]
- 15.Sanders RW. Fractures of the calcaneus. In: Coughlin MJ, Saltzman CL, Anderson RB, eds. Mann's Surgery of the Foot and Ankle. Philadelphia, PA, USA: Elsevier Inc; 2014:2041-2100. [Google Scholar]
- 16.Sayed-Noor AS, Agren PH, Wretenberg P. Interobserver reliability and intraobserver reproducibility of three radiological classification systems for intra-articular calcaneal fractures. Foot Ankle Int. 2011;32:861-866. [DOI] [PubMed] [Google Scholar]
- 17.Schepers T, van Lieshout EM, Ginai AZ, Mulder PG, Heetveld MJ, Patka P. Calcaneal fracture classification: a comparative study. J Foot Ankle Surg. 2009;48:156-162. [DOI] [PubMed] [Google Scholar]
- 18.Schepers T, van Lieshout EM, van Ginhoven TM, Heetveld MJ, Patka P. Current concepts in the treatment of intra-articular calcaneal fractures: results of a nationwide survey. Int Orthop. 2008;32:711-715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Soeur R, Remy R. Fractures of the calcaneus with displacement of the thalamic portion. J Bone Joint Surg Br. 1975;57:413-421. [PubMed] [Google Scholar]
- 20.Veltman ES, van den Bekerom MP, Doornberg JN, Verbeek DO, Rammelt S, Steller EP. Three-dimensional computed tomography is not indicated for the classification and characterization of calcaneal fractures. Injury. 2014;45:1117–1120. [DOI] [PubMed] [Google Scholar]
- 21.Zwipp H, Baumgart F, Cronier P, Jorda E, Klaue K, Sands AK, Yung SW. Integral classification of injuries (ICI) to the bones, joints, and ligaments—application to injuries of the foot. Injury . 2004;35:3-9. [DOI] [PubMed] [Google Scholar]
- 22.Zwipp H, Tscherne H, Wulker N. [Osteosynthesis of dislocated intra-articular calcaneus fractures] [in German]. Unfallchirurg. 1988;91:507-515. [PubMed] [Google Scholar]


