Abstract
Background
The risk of early complications is high after monoblock acetabular metal-on-metal (MoM) THA revisions. However, there is a paucity of evidence regarding clinical complications after isolated head-liner exchange of modular MoM THA.
Questions/purposes
The purposes of this study were (1) to describe the frequency of early complications after an isolated head-liner exchange revision of modular MoM THA; and (2) to determine whether patients who experienced complications or dislocation after head-liner exchanges had higher serum chromium (Cr) or cobalt (Co) ion levels than those who did not.
Methods
A review of our institution’s total joint registry retrospectively identified 53 patients who underwent 54 liner exchange revisions of a modular acetabular MoM THA. The study period was from April 2008 to April 2016 at a single tertiary care center. During this period, isolated head-liner exchanges (rather than more extensive revisions) were performed in patients if they did not have evidence of loosening of the acetabular or femoral components. Reasons for revision surgery included pain, mechanical symptoms, radiographic evidence of osteolysis, elevated serum metal ions, and MRI abnormalities with 40 of the 54 hips having pain or mechanical symptoms and 38 of 54 hips having multiple reasons for revision before surgery. Patients were excluded if they did not meet the minimum postrevision followup or had the modular liner exchange secondary to infection. All revisions were from a single manufacturer with one head-liner exchange of a MoM THA from another manufacturer excluded during the study period. The mean time from index MoM THA to modular exchange was 96 (SD ± 36) months. Because the focus of this study was early complications, we had a minimum 90-day followup duration for inclusion. Mean followup after revision was 15 months (SD ± 12); a total of 56% (30 of 54) had followup of at least 12 months’ duration. Complications (dislocation, infection) and reoperations were obtained by chart review performed by individuals other than the treating physician(s). Serum metal ion levels were obtained before head-liner exchange. The median serum Cr and Co levels were 6 µg/L (range, 0-76 µg/L) and 12 µg/L (range, 0-163 µg/L), respectively.
Results
Of the 54 revision THAs, 15 (28%) developed complications. Nine (17%) occurred within 90 days of the revision surgery and 11 (20%) resulted in reoperation. The most common complication was dislocation (12 of 54 [22%]) with recurrent dislocation noted in eight of these 12 patients. All patients with recurrent dislocation continued to dislocate and underwent repeat revision. Patients with dislocation had higher median serum Cr and Co ion levels than those without dislocation (Cr: 24 [range, 11-76] versus 4 [range, 0-70], p = 0.001 [95% confidence interval {CI}, 10-57]; Co: 41 [range, 6-163] versus 8 [range, 0-133], p = 0.016 [95% CI, 6-141]). Three (6%) of the 54 patients underwent repeat surgery for deep space infection.
Conclusions
Complications and reoperations are common after modular head-liner exchange in the setting of a failed MoM THA. Our study likely underestimates the frequency of complications and revisions because the followup period in this report was relatively short. Dislocation is the most common complication and elevated serum metal ion levels may be a predictor of dislocation. These findings are concerning and surgeons should be aware of the high complication risk associated with this procedure.
Level of Evidence
Level IV, therapeutic study.
Introduction
Early observations after isolated monoblock acetabular revision surgery of metal-on-metal (MoM) THA suggest a high prevalence of complications and revisions with dislocation and infection being the two that are most commonly reported [14, 15, 17, 19, 21, 23]. However, there is a paucity of evidence regarding modular acetabular (head and liner) revision in this patient population [15, 19].
A recent Medicare database analysis showed a high occurrence of dislocation and infection in patients undergoing an isolated acetabular component revision; however, this study design did not allow for differentiation between modular and full acetabular component revisions [19]. An analysis from the National Joint Registry for England and Wales identified modular acetabular component-only revision (head and liner exchange) as a predictor of rerevision after MoM THA revision surgery [15]. The inherent nature of this registry-based study cannot report data on variables such as serum metal ion levels, which may play a role in complications in patients with MoM articulations [12]. At our institution, we have noted a high risk of complications in patients with a MoM bearing surface undergoing an isolated modular head-liner exchange.
We therefore sought to determine (1) the frequency of early complications after an isolated head-liner exchange revision of modular MoM THA; and (2) whether patients who experienced major complications or dislocation after head-liner exchanges had higher serum chromium (Cr) or cobalt (Co) ion levels than those who did not.
Patients and Methods
Our institutional review board approved this retrospective study. We utilized our institution’s longitudinally maintained total joint registry to identify all patients undergoing revision of a MoM THA. The study period was from April 2008 to April 2016. We included all patients who had revision of a MoM THA with a modular acetabular component from a single manufacturer. This acetabular component can accept a metal, ceramic, or polyethylene insert. Patients were excluded if they did not meet the minimum postrevision followup of 90 days or had the modular liner exchange secondary to infection. One head-liner exchange of a MoM THA from another manufacturer was excluded during the study period. We excluded this patient because the modularity options differed for the acetabular component in this patient and this did not allow for comparison given the disparity in number of patients between the two groups. After exclusion, this left 54 revision procedures performed at a single tertiary care center by six fellowship-trained arthroplasty surgeons in 53 patients. Because the focus of this study was early complications, we chose a minimum 90-day followup duration for inclusion in this study. Mean followup after revision was 15 (SD ± 12) months; a total of 56% (30 of 54) had followup of at least 12 months’ duration. No patient in this study was lost to followup.
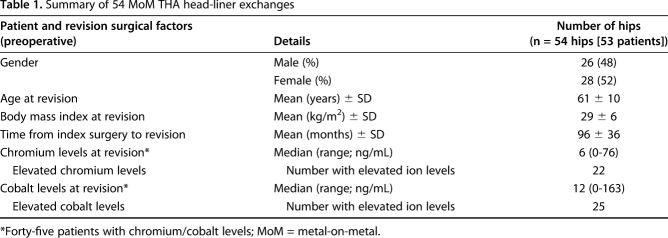
The mean time from index MoM THA to modular exchange was 96 (SD ± 36) months. Forty-eight percent of the patients were men (26 of 54) and 52% were women (28 of 54), and the mean patient age at index revision surgery was 61 (SD ± 10) years. The mean patient body mass index (BMI) at the time of revision was 29 (SD ± 6) kg/m2 (Table 1).
Table 1.
Summary of 54 MoM THA head-liner exchanges
All 54 hips were implanted with the Pinnacle® modular (Ultamet® metal liner; DePuy Orthopaedics, Inc, Warsaw, IN, USA) acetabular component. The mean acetabular component abduction angle was 44° (SD ± 8). The femoral stems used included the Summit® (DePuy Orthopaedics, Inc) in 28 patients, AML® (DePuy Orthopaedics, Inc) in 13 patients, S-ROM® (DePuy Orthopaedics, Inc) in six patients, Trilock® (DePuy Orthopaedics, Inc) in three patients, and the Corail® and Endurance® (DePuy Orthopaedics, Inc) stems in two patients each.
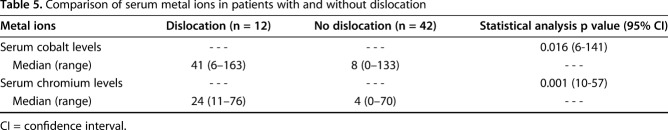
In general, revision surgery was performed based on a constellation of findings, including patient symptoms (pain or mechanical symptoms), radiographic findings, metal ion levels, and metal artifact reduction sequence MRI in the absence of another clear diagnosis. Reasons for revision surgery included pain, mechanical symptoms, radiographic evidence of osteolysis, elevated serum metal ions, and MRI abnormalities with 40 of the 54 hips having pain or mechanical symptoms and 38 of 54 hips having multiple reasons for revision before surgery (Table 2). During this period, isolated head-liner exchanges (rather than more extensive revisions) were performed in patients if they did not have evidence of loosening of the acetabular or femoral components.
Table 2.
Summary of diagnostic reason for revision
Serum metal ion analysis samples were collected, stored (certified metal-free transfer tubes), and transported according to laboratory guidance. Analysis was performed at an accredited laboratory (LabCorp, Burlington, NC, USA) with expertise in trace metal element analysis. The serum Co and Cr ions were utilized to determine whether patients who experienced complications or dislocation after head-liner exchanges differed from those who did not. The median serum Cr and Co levels preoperatively were 6 µg/L (range, 0-76 µg/L) and 12 µg/L (range, 0-163 µg/L), respectively. Twenty-two patients had elevated (> 7 µg/L) Cr and 25 patients had elevated Co levels preoperatively.
Preoperative radiographic imaging (AP pelvis, AP and lateral hip views) were critically assessed for loosening, component migration or subsidence, and osteolysis on the femoral and acetabular components. An isolated head-liner exchange was considered preoperatively in patients without evidence of acetabular or femoral failure in the setting of a well-positioned acetabular component. Intraoperatively, acetabular and femoral components were examined for signs indicative of revision (loosening, subsidence) before proceeding with an isolated head-liner exchange. Specifically, the acetabular component was inspected for damage such as fretting or corrosion and/or inadequate function of the locking mechanism. In this cohort, there were no patients with documented indications for full revision of their acetabular component.
Complications (dislocation, infection) and reoperations were obtained by chart and our institution’s registry review with individuals other than the treating physician(s). In patients who experienced a dislocation, conservative interventions such as physical therapy, bracing, and/or strict hip precautions were used at the discretion of the surgeon. In general, patients returned to the clinic for evaluation at 2 weeks, 6 weeks, 3 months, 1 year, and 2 and 5 years. Radiographic followup was performed at 6 weeks, 1 year, 2 years, and 5 years.
Descriptive statistics were calculated to derive means and SDs for data that were normally distributed as well as medians and ranges for data that were not normally distributed. We also used descriptive statistics to find proportions for the categorical variables used in the article. Comparisons of group sample distributions, dislocation versus no dislocation, were evaluated with Mood’s median test for significance between groups as a result of nonparametric data. Differences were considered to be significant at p < 0.05. Minitab Version 17 (State College, PA, USA) was used for all statistical analysis. We were unable to perform a multivariate analysis secondary to our small sample size.
Results
Postoperative Complications
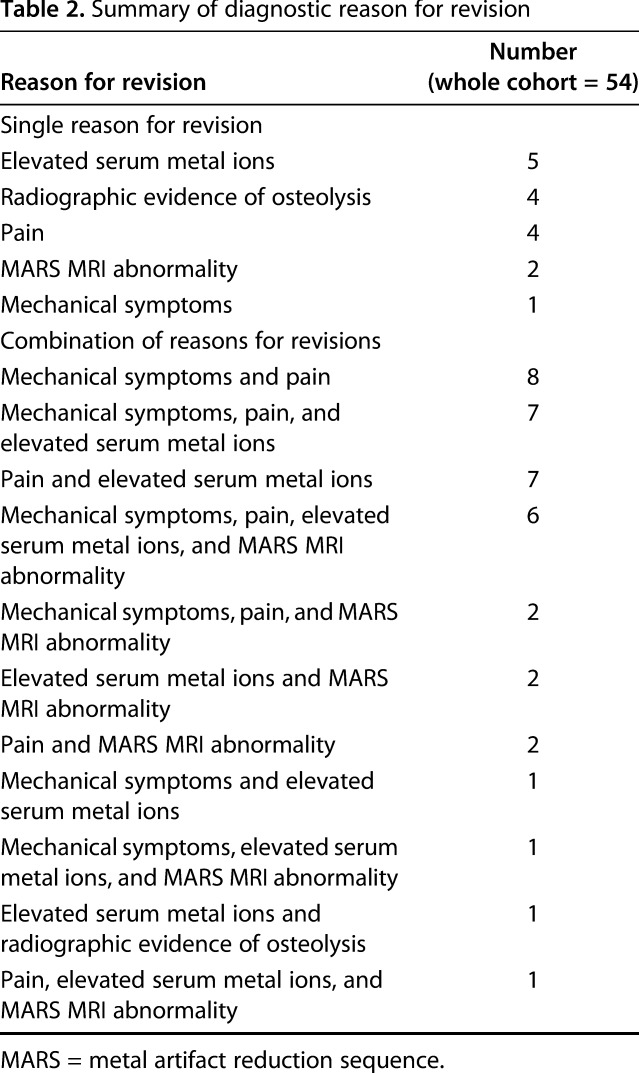
A total of 15 of 54 (28%) complications occurred, including 12 of 54 (22%) patients with dislocation and three of 54 with deep infection (6%). The median time between revision surgery and complication was 2 months (range, 0-27 months). Nine of 54 (17%) procedures involved at least one early (within 90 days of surgery) complication. Of the 12 patients with postoperative dislocation, seven of the 12 occurred within 90 days of revision with a mean time of 23 (SD ± 19) days. Five of the 12 occurred > 90 days postrevision with a mean time of 275 (SD ± 298) days. Eight of the 12 patients had recurrent dislocation with all undergoing a reoperation (Table 3).
Table 3.
Summary of dislocation-related complications after head-liner exchange
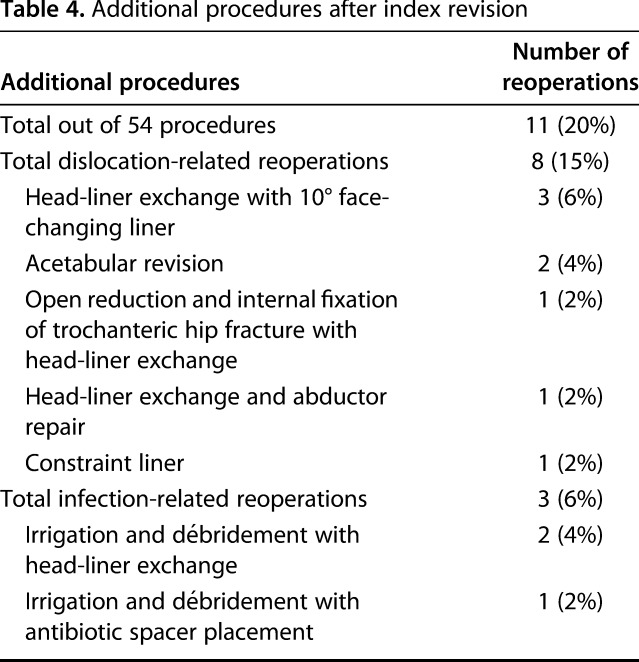
Eleven of the 54 (20%) patients had a reoperation (Table 4). Eight of these 11 reoperations were secondary to dislocation and included three face-changing liner exchanges; two acetabular component revisions; one head-liner exchange with advancement and repair of the abductors; one conversion to a constraint liner; and one open reduction with internal fixation of a trochanteric hip fracture with a head-liner exchange. Three of the 11 reoperations were secondary to deep infection and included one irrigation and débridement with a head-liner exchange; one irrigation and débridement with an explant and two-stage revision; and one evacuation of an infected hematoma.
Table 4.
Additional procedures after index revision
Serum Cobalt and Chromium Levels
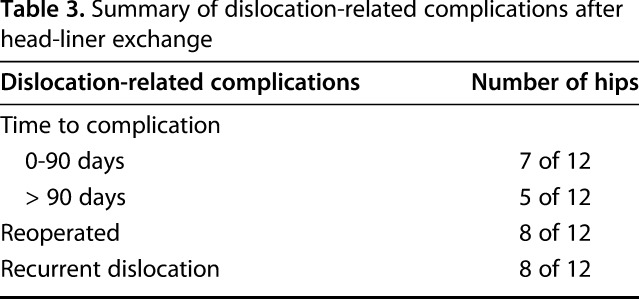
Median serum Cr levels were higher among patients who developed complications (22 µg/L; range, 0-76 µg/L) than among those who did not develop complications (4 µg/L; range, 0-70 µg/L; p = 0.012; 95% confidence interval [CI], 5-34). Likewise, median serum Co levels were higher among patients who developed complications (22 µg/L; range, 1-163 µg/L) than among those who did not develop complications (8 µg/L; range, 0-133 µg/L; p = 0.069; 95% CI, -6 to 108). Patients who dislocated had higher median Cr and Co levels than those who did not (Cr: 24 [range, 11-76] versus 4 [range, 0-70], p = 0.001 [95% CI, 10-57]; Co: 41 [range, 6-163] versus 8 [range, 0-133], p = 0.016 [95% CI, 6-141]; Table 5).
Table 5.
Comparison of serum metal ions in patients with and without dislocation
Discussion
MoM THAs have experienced a higher risk of revision than THAs using metal-on-polyethylene bearing couples, and the causes for revisions in MoM THAs have differed from those previously observed in THAs using conventional bearing surfaces [2, 3, 5-9, 12, 16, 20, 22]. Research at short-term followup has identified a high risk of early complications in monoblock acetabular component revisions in patients with MoM THAs [21]. The risk of complications after an isolated modular MoM head-liner revision appears greater than it is among patients undergoing acetabular-only or all-component revision (acetabular and femoral), and modular liner exchange revision for MoM THA is associated with a higher risk of rerevision surgery in these patients [15]. We report an alarmingly high risk of complications, dislocations, and reoperations in patients with a modular head-liner exchange revision MoM THA at short-term followup. Additionally, the serum Cr and Co ion levels were elevated in patients who experienced dislocation compared with those who did not. To our knowledge, this is the first study examining serum metal ion levels and its potential association with complications and dislocations in patients undergoing an isolated modular head-liner exchange in a MoM THA.
Our study is not without limitations. Transfer bias is a concern, because our followup is insufficiently long and complete to be sure all of the outcomes of interest have been captured. None of the patients in this study were lost to followup before 90 days; however, only 56% (30 of 54) had followup of at least 12 months’ duration. The actual proportion of patients with complications and dislocations therefore is likely higher than what we report. Additional followup would likely cause us to uncover a greater variety of postrevision complications as well. Although longer followup would be preferable, we feel the percentage of early complications in this cohort justifies immediate presentation of these results. A study about isolated MoM monoblock acetabular THA revisions recently found a similarly high risk of complications [21]. We concede that a selection bias may also exist because the diagnosis and reason for revision were not uniform in the patients who we evaluated here. Additionally, we did not document trunnionosis, which has now been identified as a cause for revision in metal-on-polyethylene and MoM bearing surfaces [4, 10, 11]. Although this likely would not have changed our findings about the risk of complications in this cohort, there may have been a different reason listed for the primary reason for revision (ie, isolated trunnionosis may have been the reason for revision). Furthermore, there was no histologic examination performed on hip or paraarticular tissues, and we therefore are unable to correlate our findings at the time of surgery with complications like dislocation. All patients were from a single surgical center with six different fellowship-trained arthroplasty surgeons performing the revision surgery, which may create some variability with regard to operative techniques that we are unable to account for in a retrospective design. Our cohort was small and therefore we were unable to perform statistical analysis that accounts for confounding variables with a multivariate analysis. Finally, the current study was underpowered to correlate clinical and demographic factors with complications and revisions that might be studied best in the future through a multicenter study.
We found that 28% of our patients experienced complications, and 20% underwent reoperation. The two most common complications in our cohort were dislocation (12 of 54 [22%]) and infection (three of 54 [6%]). Eight of 12 patients who experienced a dislocation underwent repeat revision. These findings are similar to a recent national registry study reporting dislocation and infection as the two most common reasons for rerevision after modular head-liner exchange in patients with MoM THA [15]. Maintaining a well-fixed, well-positioned acetabular component at revision surgery is an attractive option to avoid the reported morbidity of cup removal [21]. However, a recent study identified modular exchange (head-liner) in patients undergoing a revision of MoM THA as a risk factor for rerevision surgery when compared with monoblock acetabular revision or full (acetabular and femoral) revision surgery [15]. Surgeons must be aware that although modular exchanges seem straightforward, complications appear to be disturbingly common after these procedures; we especially caution the reader that our relatively short followup here likely underestimates the magnitude of that risk in these procedures. Further investigation, likely a multicenter study, should focus on demographic and operative (revision approach, types of liners utilized, downsizing of the femoral head, and quantifying the amount of adverse local tissue reaction present) factors associated with adverse outcomes in this patient population.
Patients who experienced postoperative dislocation had higher serum Cr and Co levels than those patients whose THA did not dislocate. To our knowledge, no other report has explored the association of elevated serum metal ion levels with postoperative dislocation in patients undergoing revision modular head-liner exchange in a MoM THA. The role of serum metal ions in the diagnosis and its relationship with complications remain controversial in patients with MoM THA [6, 8, 12, 13, 18, 20]. Additionally, corrosion from the trunnion [4, 11] and backside wear of the acetabular liner [1, 5] must be considered in all patients undergoing revision arthroplasty in this patient population as a primary or contributing cause of revision and as potential sources of postoperative complications. Elevated serum Cr and Co ion levels in patients undergoing modular head-liner exchange in MoM THA should alert surgeons to a potentially increased risk of dislocation after surgery. This may cause surgeons to apply a lower threshold for face-changing or constraining liner options. Future studies are needed with larger cohorts, longer durations of followup, and different component manufacturers to determine whether our results are generalizable.
In conclusion, complications and reoperations are common after modular head-liner exchange in patients undergoing revision MoM THA. Our study likely underestimates the frequency of complications and rerevisions because of our short duration of followup. Dislocation is the most common complication and elevated serum metal ion levels may be associated with dislocation. These findings are concerning, and surgeons should be aware of the high complication risk associated with this seemingly straightforward procedure. As revision of MoM THA becomes more common, it will be important to continue monitoring outcomes and further define treatment strategies to decrease complications for these patients. Future studies should determine whether demographic, clinical, technique-related, or laboratory factors (such as metal ion levels) may be most closely tied to complications and adverse outcomes in these patients.
Acknowledgments
We thank Marc Angerame MD, David Holst MD, Roseann Johnson, Daniel Levy, and Catie Eschen for their help in assisting with the preparation of the manuscript.
Footnotes
One of the authors (DAD) has or may receive payments or benefits from DePuy (Warsaw, IN, USA), Innomed (Savannah, GA, USA), Joint Vue (Columbus, OH, USA), and Wolters Kluwer Health (Philadelphia, PA, USA) not related to this work. One of the authors (JMJ) has or may receive payments or benefits from DePuy, Total Joint Orthopedics (Salt Lake City, UT, USA), and Xenex (San Antonio, TX, USA) not related to this work. One of the authors (CCY) has or may receive payments or benefits from DePuy, Medtronic (Minneapolis, MN, USA), and Zimmer (Warsaw, IN, USA) not related to this work. One of the authors (TMM) has or may receive payments or benefits from DePuy and Zimmer not related to this work.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA-approval status, of any drug or device prior to clinical use.
Each author certifies that his institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at Colorado Joint Replacement, Denver, CO, USA.
References
- 1.Agne MT, Underwood RJ, Kocagoz SB, MacDonald DW, Day JS, Parvizi J, Kraay MJ, Mont MA, Klein GR, Cates HE, Kurtz SM. Is there material loss at the backside taper in modular CoCr acetabular liners? Clin Orthop Relat Res. 2014;473:275–285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bayley N, Khan H, Grosso P, Hupel T, Stevens D, Snider M, Schemitsch E, Kuzyk P. What are the predictors and prevalence of pseudotumor and elevated metal ions after large-diameter metal-on-metal THA? Clin Orthop Relat Res. 2014;473:477–484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Browne JA, Bechtold CD, Berry DJ, Hanssen AD, Lewallen DG. Failed metal-on-metal hip arthroplasties: a spectrum of clinical presentations and operative findings. Clin Orthop Relat Res. 2010;468:2313–2320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cooper HJ, Della Valle CJ, Berger RA, Tetreault M, Paprosky WG, Sporer SM, Jacobs JJ. Corrosion at the head-neck taper as a cause for adverse local tissue reactions after total hip arthroplasty. J Bone Joint Surg Am. 2012;94:1655–1661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gascoyne TC, Dyrkacz RM, Turgeon TR, Burnell CD, Wyss UP, Brandt J-M. Corrosion on the acetabular liner taper from retrieved modular metal-on-metal total hip replacements. J Arthroplasty. 2014;29:2049–2052. [DOI] [PubMed] [Google Scholar]
- 6.Griffin WL, Fehring TK, Kudrna JC, Schmidt RH, Christie MJ, Odum SM, Dennos AC. Are metal ion levels a useful trigger for surgical intervention? J Arthroplasty. 2012;27:32–36. [DOI] [PubMed] [Google Scholar]
- 7.Haddad FS, Thakrar RR, Hart AJ, Skinner JA, Nargol AV, Nolan JF, Gill HS, Murray DW, Blom AW, Case CP. Metal-on-metal bearings: the evidence so far. J Bone Joint Surg Br. 2011;93:572–579. [DOI] [PubMed] [Google Scholar]
- 8.Hannemann F, Hartmann A, Schmitt J, Lützner J, Seidler A, Campbell P, Delaunay CP, Drexler H, Ettema HB, García-Cimbrelo E, Huberti H, Knahr K, Kunze J, Langton DJ, Lauer W, Learmonth I, Lohmann CH, Morlock M, Wimmer MA, Zagra L, Günther KP. European multidisciplinary consensus statement on the use and monitoring of metal-on-metal bearings for total hip replacement and hip resurfacing. Orthop Traumatol Surg Res. 2013;99:263–271. [DOI] [PubMed] [Google Scholar]
- 9.Hart AJ, Satchithananda K, Liddle AD, Sabah SA, McRobbie D, Henckel J, Cobb JP, Skinner JA, Mitchell AW. Pseudotumors in association with well-functioning metal-on-metal hip prostheses: a case-control study using three-dimensional computed tomography and magnetic resonance imaging. J Bone Joint Surg Am. 2012;94:317. [DOI] [PubMed] [Google Scholar]
- 10.Jennings JM, Dennis DA, Yang CC. Corrosion of the head-neck junction after total hip arthroplasty. J Am Acad Orthop Surg. 2016;24:349–356. [DOI] [PubMed] [Google Scholar]
- 11.Lash NJ, Whitehouse MR, Greidanus NV, Garbuz DS, Masri BA, Duncan CP. Delayed dislocation following metal-on-polyethylene arthroplasty of the hip due to 'silent' trunnion corrosion. Bone Joint J. 2016;98:187–193. [DOI] [PubMed] [Google Scholar]
- 12.Lombardi AV, Jr, Barrack RL, Berend KR, Cuckler JM, Jacobs JJ, Mont MA, Schmalzried TP. The Hip Society: algorithmic approach to diagnosis and management of metal-on-metal arthroplasty. J Bone Joint Surg Br. 2012;94:14–18. [DOI] [PubMed] [Google Scholar]
- 13.Matharu GS, Judge A, Eskelinen A, Murray DW, Pandit HG. What is appropriate surveillance for metal-on-metal hip arthroplasty patients? Acta Orthop. 2018;89:29–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Matharu GS, Judge A, Murray DW, Pandit HG. Outcomes after metal-on-metal hip revision surgery depend on the reason for failure. Clin Orthop Relat Res. 2018;476:245–258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Matharu GS, Judge A, Pandit HG, Murray DW. Which factors influence the rate of failure following metal-on-metal hip arthroplasty revision surgery performed for adverse reactions to metal debris? Bone Joint J. 2017;99:1020–1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Milošev I, Kovač S, Trebše R, Levašič V, Pišot V. Comparison of ten-year survivorship of hip prostheses with use of conventional polyethylene, metal-on-metal, or ceramic-on-ceramic bearings. J Bone Joint Surg Am. 2012;94:1756–1763. [DOI] [PubMed] [Google Scholar]
- 17.Munro JT, Masri BA, Duncan CP, Garbuz DS. High complication rate after revision of large-head metal-on-metal total hip arthroplasty. Clin Orthop Relat Res. 2014;472:523–528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nicolli A, Bisinella G, Padovani G, Vitella A, Chiara F, Trevisan A. Predictivity and fate of metal ion release from metal-on-metal total hip prostheses. J Arthroplasty. 2014;29:1763–1767. [DOI] [PubMed] [Google Scholar]
- 19.Penrose CT, Seyler TM, Wellman SS, Bolognesi MP, Lachiewicz PF. Complications are not increased with acetabular revision of metal-on-metal total hip arthroplasty. Clin Orthop Relat Res. 2016;474:2134–2142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Randelli F, Banci L, Favilla S, Maglione D, Aliprandi A. Radiographically undetectable periprosthetic osteolysis with ASR implants: the implication of blood metal ions. J Arthroplasty. 2013;28:1259–1264. [DOI] [PubMed] [Google Scholar]
- 21.Stryker LS, Odum SM, Fehring TK, Springer BD. Revisions of monoblock metal-on-metal THAs have high early complication rates. Clin Orthop Relat Res. 2014;473:469–474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Voleti PB, Baldwin KD, Lee G-C. Metal-on-metal vs conventional total hip arthroplasty. J Arthroplasty. 2012;27:1844–1849. [DOI] [PubMed] [Google Scholar]
- 23.Wyles CC, Van Demark RE, 3rd, Sierra RJ, Trousdale RT. High rate of infection after aseptic revision of failed metal-on-metal total hip arthroplasty. Clin Orthop Relat Res. 2014;472:509–516. [DOI] [PMC free article] [PubMed] [Google Scholar]