Abstract
Background
The importance of spinopelvic motion and its influence on THA stability are well recognized but poorly defined. With dynamic motion, compensatory changes in spine and pelvic positions are required to keep the necessary balance between the axial skeleton and lower extremity to maintain an erect posture. Although prior studies have shown spinal fusions to be an independent risk factor for hip dislocations after primary THA, the direct impact of fusion levels on spinopelvic motion remains unknown.
Questions/purposes
The purposes of this study were (1) to determine if acetabular orientation changes with flexion and extension of the lumbar spine; (2) to determine if the amount of change is different in patients who have undergone spinal fusion at the L5-S1 level; and (3) to identify if the amount of change in acetabular motion is increased in patients who have undergone fusion at additional or other spinal levels.
Methods
We reviewed 100 flexion-extension spine films of patients older than 18 years of age with a history of back pain who had not undergone spinal or hip surgery and compared them with 50 flexion-extension spine films of patients who had undergone lumbar fusion at various levels. These radiographs were acquired between 2012 and 2017 and stored in our institutional radiology database. Only patients with flexion and extension films able to visualize the greater trochanter of the femur were included. For each film, measurements of acetabular version, acetabular version relative to the femoral shaft, lumbar lordosis angle, and sacral slope were digitally performed by two independent observers. Intra- and interrater variability was assessed using Lin’s concordance correlation (Rho_c) ranging from 0.59 to 0.91. The change in acetabular version for each patient when going from spinal flexion to extension was compared between patients with no prior spinal or hip surgery and those with prior spinal fusions using a two-tailed t-test.
Results
Acetabular version changed -21° as the lumbar spine changed position from flexion to extension in patients without spine surgery (95% confidence interval [CI], -24° to -18°). Acetabular version changed 15° as the lumbar spine changed position from flexion to extension in patients who had undergone prior lumbar spine fusion at all levels (95% CI, -18° to -12°). There was a difference in the change in acetabular version between these two groups of -6° (95% CI, -11° to -1°; p = 0.01). In patients with prior L5-S1 fusion, the change in acetabular version was decreased when compared with patients without prior spine surgery. The change was -10° (95% CI, -15° to -6°), which is less than the change of acetabular version of -21° that we saw in patients without prior spinal fusion (p < 0.01). The difference between these groups was -10° (95% CI, -18° to -3°). Fusion levels above L5 that did not cross the L5-S1 joint did not have a difference in change in acetabular version when compared with patients without surgery with a mean difference of -4° (95% CI, -9° to 2°).
Conclusions
Spinal fusion, specifically at the L5-S1 level, reduces pelvic mobility as the spine moves from flexion to extension. This reduction in motion can reduce the distance to impingement and place patients undergoing THA at risk for dislocation. Further research utilizing three-dimensional imaging modalities and motion analysis can further help define the best hip implant position in these patients.
Level of Evidence
Level III, prognostic study.
Introduction
In recent years, the contributions of the spine and spine-pelvic relationship to hip implant stability have been recognized [7]. Additionally, there has been increased awareness that prior lumbar surgery places patients who have undergone THA at higher risk of postoperative instability [6]. With activities, compensatory changes in spine and pelvic positions are required to keep the correct alignment between the axial skeleton and lower extremities to maintain an erect posture. In patients with spine pathology, the acetabular opening angle and functional arc of motion before impingement are decreased, leading to increased risk for dislocation [5].
In the stiff spine, there is a relative decrease in acetabular anteversion because there is a lack of pelvic extension leading to relative acetabular retroversion in a seated position. Furthermore, in patients in whom the spine is rigid and/or unbalanced in the sagittal plane, the risk of impingement is further magnified. Therefore, it is recommended that placement of the acetabular component should be adjusted to account for both the position and rigidity of the lumbar spine [10]. However, although multiple studies have shown spinal disease and prior spinal fusion as risk factors for postoperative instability [1, 3, 7, 11], the impact of the level of lumbar fusion and the number of levels fused on the degree of restriction to pelvic mobility remain undefined. Additionally, there is currently no information on whether a threshold exists in terms of fused segments above which the hip is always at risk for impingement and/or dislocation.
Therefore, the purposes of this study were (1) to determine if acetabular orientation changes with flexion and extension of the lumbar spine; (2) to determine if the amount of change is different in patients who have undergone spinal fusion at the L5-S1 level; and (3) to identify if the amount of change in acetabular motion is increased in patients who have undergone fusion at additional or other spinal levels.
Materials and Methods
We retrospectively studied lumbar flexion-extension films of 100 adult patients who presented with the chief complaint of lower back pain and had not undergone spinal or hip surgery and compared them with 50 lumbar flexion-extension films of patients who had undergone lumbar fusions at various levels during the same time. The most common diagnoses included lumbago, degenerative disc disease, mechanical low back pain, spinal stenosis, and spondylolisthesis. The films were acquired and stored in our institutional radiology database (University of Pennsylvania Health System, Montage) from the period ranging from January 1, 2012, to January 1, 2017. Inclusion criteria included any patients older than 18 years with standing lumbar flexion and extension films that included visualization of the greater trochanter of the femur. In addition, the films needed to be of sufficient quality and clarity to allow multiple radiographic measurements. Exclusion criteria included any history of spine surgery other than lumbar fusion, a history of hip surgery, a history of lumbar compression fracture, a history of ankylosing spondylitis, scoliosis, and neurologic or musculoskeletal disorders, which could impact motion or muscle tone. Consecutive patients meeting these precise criteria were selected beginning from images acquired in 2017 and the radiographs screened until 100 patients without spine surgery and 50 patients with spine surgery who had appropriate flexion-extension films. In sum, 573 sets of images were screened to identify these 150 appropriate patients for this study.
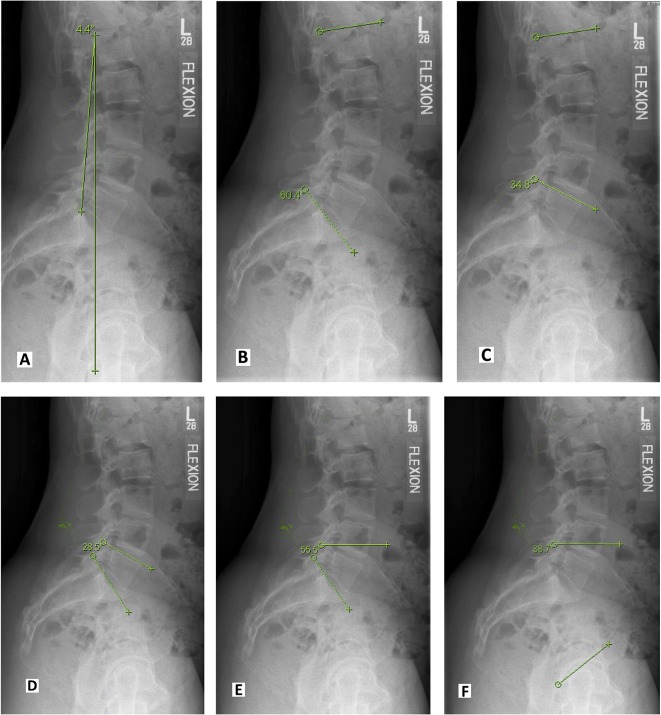
For each patient, the following radiographic variables were collected for both flexion and extension views. First, the angle that the film was rotated off the vertical axis of the screen was measured so that the flexion and extension views for each patient could be compared. The angle formed by a line connecting the posterior aspect of the superior endplate of L1 to the posterior aspect of the superior endplate of S1 was compared with a line perpendicular to the vertical axis of the film (Fig. 1A). This angle was used to standardize all other subsequent radiographic measurements. Second, the lumbar lordosis angle, formed by the line tangent to the superior endplate of L1 with the line tangent to the superior endplate of S1 for each film, was determined (Fig. 1B). Next, the L1 to L5 angle, determined by the line tangent to the superior endplate of L1 with the line tangent to the superior endplate of L5, was calculated (Fig. 1C). The L5 to S1 angle (line tangent to the superior endplate of L5 with the line tangent to the superior endplate of S1) was determined along with the sacral slope (angle of the tangent to the superior endplate of S1 horizontal to the axis of the film) (Fig. 1D-E). Finally, the acetabular version angle was determined by the line connecting the superior and inferior acetabular opening to the horizontal axis (Fig. 1F). Anteversion was defined by a positive value and retroversion was defined by a negative value.
Fig. 1 A-F.
(A) The angle formed by a line connecting the posterior aspect of the superior endplate of L1 to the posterior aspect of the superior endplate of S1 was compared with a line perpendicular to the vertical axis of the film. (B) This angle was used to standardize all other subsequent radiographic measurements. Second, the lumbar lordosis angle, formed by the line tangent to the superior endplate of L1 with the line tangent to the superior endplate of S1 for each film, was determined. (C) Next, the L1 to L5 angle, determined by the line tangent to the superior endplate of L1 with the line tangent to the superior endplate of L5, was calculated. (D-E) The L5 to S1 angle (line tangent to the superior endplate of L5 with the line tangent to the superior endplate of S1) was determined along with the sacral slope (angle of the tangent to the superior endplate of S1 horizontal to the axis of the film). (F) Finally, the acetabular version angle was determined by the line connecting the superior and inferior acetabular opening to the horizontal axis.
Once all measurements were completed, the acetabular version angle was corrected for the rotation of the image by subtracting the angle the film was rotated off of the vertical axis. The change of acetabular version angle from each flexion and extension film set was calculated by subtracting the corrected acetabular version in flexion from the corrected acetabular version in extension. All measurements were independently performed on two separate occasions by two observers (JB, RC) on the same equipment. The intra- and interobserver reliabilities were calculated.
Statistical Analysis
As a result of the nature of the radiographic evaluation, blinding of the reviewers was not possible. Intraobserver reliability measured by intraclass correlation for flexion views was 0.91 (95% confidence interval [CI], 0.87-0.95) and for extension views was 0.80 (95% CI, 0.70-0.89). Interobserver reliability measured by intraclass correlation for flexion views was 0.85 (95% CI, 0.78-0.92) and for extension views was 0.59 (95% CI, 0.42-0.76).
A priori power analysis was performed on review of the first 20 patients to determine the necessary sample size. Among these patients, there was a mean change in acetabular version from flexion to extension of 5° (SD 10). Based on these results, with a two-to-one sampling strategy, the current sample size was powered at 80% to detect a difference of 3° between groups with a type I error rate, α, set at 0.05.
Groups were analyzed by comparing the change in acetabular version for patients who had undergone spinal fusion with those who had not undergone prior spinal surgery. The spinal fusion group was stratified into fusions including the L5 to S1 levels and those that did not include this level. The comparisons were made using a two-way t-test. A p value < 0.05 was considered statistically significant. All analyses were performed using Stata Version 14.2 (Statacorp, College Station, TX, USA).
Results
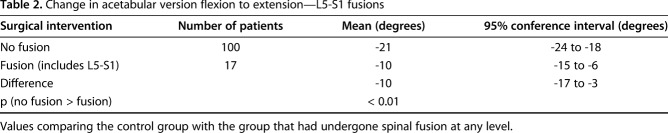
When the spine goes from flexion to extension, the acetabulum goes into relative retroversion, which in our data is reported as a negative change in angle. Acetabular version became 21° more retroverted (or -21°) as the lumbar spine changed position from flexion to extension in patients without spine surgery (SD 2; 95% CI, -24° to -18°). Acetabular version changed -15° as the lumbar spine changed position from flexion to extension in patients who had undergone prior lumbar spine fusion at all levels (SD 1; 95% CI, -18° to -12°). There was a difference in the change in acetabular version between these two groups of -6° (SD 2; 95% CI, -11° to -1°; p = 0.01; Table 1; Fig. 2 A-D).
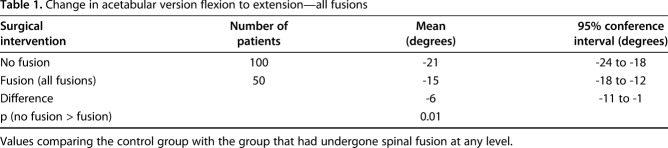
Table 1.
Change in acetabular version flexion to extension—all fusions
Fig. 2 A-D.
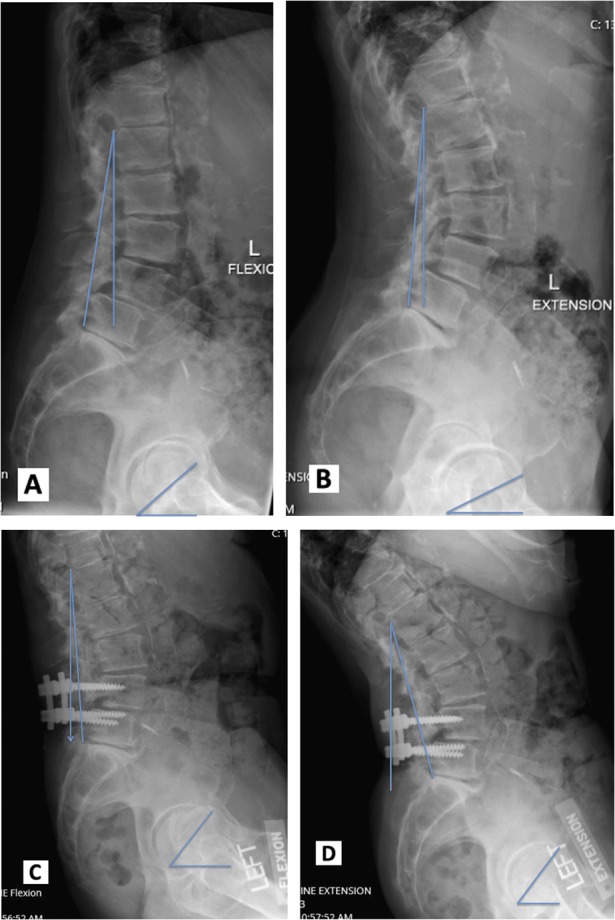
(A) Preoperative fusion flexion films mark acetabular version angle and correction for spine rotation angle. (B) Preoperative fusion extension films mark acetabular version angle and correction for spine rotation angle. (C) Postoperative fusion flexion films mark acetabular version angle and correction for spine rotation angle. (D) Postoperative fusion extension films mark acetabular version angle and correction for spine rotation angle.
Patients with a fusion at L5-S1 were found to have further decreased pelvic mobility and arc of motion. In the 17 patients with L5 to S1 fusion segments, the change in acetabular version was decreased when compared with patients without prior spine surgery. The change was -10° (SD 2; 95% CI, -15° to -6°), which is less than the change of acetabular version of -21° that we saw in patients without prior spinal fusion (p < 0.01). The difference between these groups was -10° (SD 4; 95% CI, -18° to -3°; Table 2).
Table 2.
Change in acetabular version flexion to extension—L5-S1 fusions
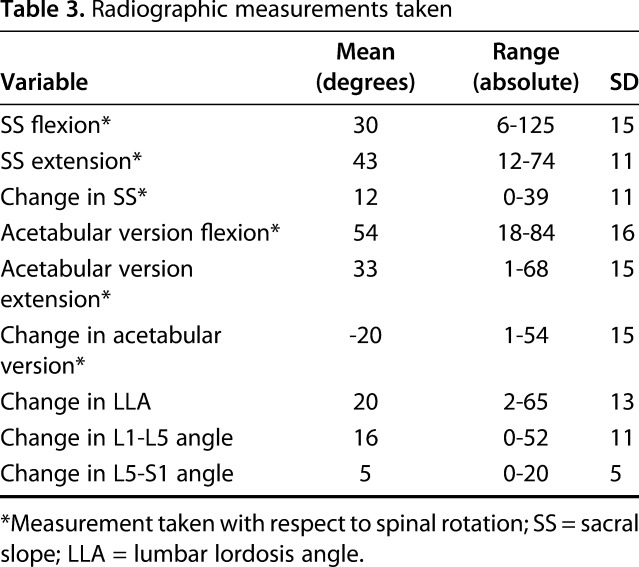
Fusion levels above L5 that did not cross the L5-S1 joint did not have a difference in change in acetabular version when compared with patients without surgery with a mean difference of -4° (SD 3; 95% CI, -9° to 2°; Table 3).
Table 3.
Radiographic measurements taken
Discussion
In recent years, the association of the spinopelvic relationship with hip stability after THA has been recognized. However, although multiple studies have shown spinal disease and prior spinal fusion as risk factors for postoperative instability [1, 3, 11], the impact of the level of lumbar fusion and the number of levels fused on the degree of restriction to pelvic mobility remain undefined. Additionally, there is currently no information on whether a threshold exists in terms of fused segments above which the hip is always at risk for impingement and/or dislocation. Therefore, the purposes of this study were (1) to determine if acetabular orientation changes with flexion and extension of the lumbar spine; (2) to determine if the amount of change is different in patients who have undergone spinal fusion at the L5-S1 level; and (3) to identify if the amount of change in acetabular motion is increased in patients who have undergone fusion at additional or other spinal levels.
This study has several limitations. First, this is a retrospective study and therefore subject to selection bias. Because the films were not obtained to specifically study and needed to visualize the greater trochanters to measure the change in acetabular position across lumbar motion, only a small fraction (26%) of flexion and extension films in our film archives could be used for the study. Additionally, because the patients in the control group had some underlying diagnosis of spinal pathology, the mobility of the spine and the pelvis in this group may already be compromised or diminished and thus lead to an underestimation of the impact of spinal fusion on pelvic mobility. Furthermore, because we do not have complete sets of images for all patients meeting the technical radiographic inclusion criteria to allow measurement of pelvic mobility before and after lumbar fusion, the precise impact of spinal fusion on pelvic mobility could not be determined. Second, a lack of standardized image acquisition during the study period (ie, films not including the greater trochanters) and small variations in pelvic rotation of the films can introduce both source bias and impact measurement accuracy. Although our measurement protocol successfully corrected for rotation as demonstrated by overall good intra- and-interobserver reliabilities, the lower interrater reliability for extension films compared with flexion films potentially highlights this shortcoming. A prospective study with a standardized image acquisition protocol would minimize the need for additional corrections, which could compound measurement inaccuracies. Third, the use of serial manual measurements on radiographs obtained using a variable technique can introduce error to the data. However, we attempted to mitigate these errors by standardizing our measurement technique and procedure, performing multiple independent measurements by two observers, and calculating intra- and interrater reliabilities with good concordant results, therefore demonstrating that our observations on these general trends are valid, accurate, and reproducible. Finally, caution should be taken with the interpretation of the results because they represent a two-dimensional extrapolation of a three-dimensional problem. Pelvic motion is complex and exists in multiple planes. In this study we only sought to investigate motion in one plane, which allowed for an easier explanation of change in version. Future studies using advanced imaging such as CT or EOSTM imaging (EOS imaging, SA, Paris, France) may allow more accurate determination of spinopelvic mobility during activities in multiple planes.
These results show that as the lumbar spine goes from flexion into extension, the pelvis compensates by retroverting the acetabulum. However, the excursion of the pelvis can be variable. These observations are consistent with other published reports. Esposito et al. [2] described differences in posterior pelvic tilt as the person goes from a sitting to a standing position and warned against the relative decrease in anteversion in patients with degenerative disc disease. Furthermore, Nam et al. [8] also reported great variability in pelvic motion and functional component position after implantation of THA. In their series, the difference in pelvic motion preoperatively to postoperatively ranged from 5° to 10°. However, our findings also highlight the complexity of spinopelvic motion and difficulty in predicting pelvic mobility after spinal fusion as shown by the variability in pelvic mobility even in patients with similarly fused lumbar spinal segments. Consequently, although spinal stiffness is associated with decreased pelvic excursion during lumbar flexion and extension, the effect of the spine on pelvic motion is complex, variable, and exists in multiple planes.
Fusion of the L5 to S1 segment was associated with the greatest loss of pelvic mobility compared with fusion at other lumbar spinal segments. However, fusion of lumbar segments above L5 to S1 was not associated with a decrease in spinal motion if the L5-S1 segment was not included in the fusion. Although this result is not unexpected, it has not been previously described. The L5 to S1 segment generates the greatest amount of sagittal motion and therefore locking it (as occurs with fusion) to the pelvis would have the greatest impact on pelvic motion. Lazennec et al. [4] also described that the lumbosacral junction accounted for most of the variation in acetabular anteversion when moving from a sitting to a standing position. Although our study did not find any additional decrease in pelvic mobility associated with additional levels fused, others have reported increased risk of prosthetic dislocation with increasing number of fusion levels. Buckland and colleagues [1] reported that patients with three to seven levels fused were at greater risk for postoperative instability compared with patients with one- to two-level fusion. The authors did not break out the L5-S1 fusions for subgroup analysis. Another possible explanation is that increasing the levels of spinal fusion increases the risk of alteration of the resting sagittal balance of the spine with respect to the pelvis. For example, in a patient with a flat-back deformity, the pelvis is fixed in extension and can increase the risk for posterior impingement and anterior dislocation without affecting pelvic excursion if the L5-S1 segment is not fused [11].
The reduced flexibility of the spine and resultant reduction in pelvic motion can impact hip stability after spinal fusion if the acetabulum does not open normally during sitting activities [1, 11]. However, the impact of spinal stiffness on pelvic motion is highly individual. Although our results are consistent with other published reports, it also highlights the unpredictability of the impact of spinal fusion on pelvic motion. Ochi and colleagues [9] showed that as the person goes from the standing to the sitting position, the lumbar lordosis was reduced; pelvic rotation was extended. Similarly, Stefl et al. [12] demonstrated that patients with stiff and fused spines were at greatest risk for impingement, which was associated with decreased pelvic mobility and sagittal plane imbalance. In the setting of THA, the most important contributors to hip stability are impingement and soft tissue tension. Although not all hips that impinge will become unstable if the components are reasonably positioned and the soft tissue constraints are competent, alterations in the functional position of the pelvis (ie, sagittal balance) and loss of pelvic mobility after fusion can increase the risk of impingement during activities compared with a patient with a flexible and well-balanced spine.
The influence of spinal stiffness on pelvic motion is complex and variable. Lumbar fusion is associated with reduced pelvic motion as the spine moves from flexion to extension. Fusion of the L5-S1 segment had the greatest impact on this observation, whereas fusion of other lumbar segments above L5 did not greatly impact pelvic motion even when increasing the number of fused levels. Although it is appealing to attempt to develop individual target safe zones for acetabular component positioning in patients with prior spinal fusion to minimize postoperative instability, the variability and complexity of spinopelvic motions make developments of generalizable algorithms challenging. Future studies utilizing three-dimensional imaging and functional motion analysis are necessary to advance our understanding of spinopelvic relationships and optimize component positioning in patients with prior spinal fusions undergoing THA.
Footnotes
Each author certifies that neither he or she, nor any member of his or her immediate family, has funding or commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, of any drug or device before clinical use.
Each author certifies that his or her institution approved for the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Buckland AJ, Vigdorchik J, Schwab FJ, Errico TJ, Lafage R, Ames C, Bess S, Smith J, Mundis GM, Lafage V. Acetabular anteversion changes due to spinal deformity correction: bridging the gap between hip and spine surgeons. J Bone Joint Surg Am. 2015;97:1913–1920. [DOI] [PubMed] [Google Scholar]
- 2.Esposito CI, Miller TT, Kim HJ, Barlow BT, Wright TM, Padgett DE, Jerabek SA, Mayman DJ. Does degenerative lumbar spine disease influence femoroacetabular flexion in patients undergoing total hip arthroplasty? Clin Orthop Relat Res. 2016;474:1788–1797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lazennec JY, Brusson A, Rousseau MA. Hip-spine relations and sagittal balance clinical consequences. Eur Spine J. 2011;20:686–698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lazennec JY, Charlot N, Gorin M, Roger B, Arafati N, Bissery A, Saillant G. Hip-spine relationship: a radio-anatomical study for optimization in acetabular cup positioning. Surg Radiol Anat. 2004;26:136–144. [DOI] [PubMed] [Google Scholar]
- 5.Lazennec JY, Clark IC, Folinais D, Tahar IN, Pour AE. What is the impact of a spinal fusion on acetabular implant orientation in functional standing and sitting positions? J Arthroplasty. 2017;32:3184–3190. [DOI] [PubMed] [Google Scholar]
- 6.Malkani AL, Garber AT, Ong KL, Dimar JR, Baykal D, Glassman SD, Cochran AR, Berry DJ. Total hip arthroplasty in patients with previous lumbar fusion surgery: are there more dislocations and revisions? J Arthroplasty. 2017. Oct 31. pii: S0883–5403(17)30953-1. 10.1016/j.arth.2017.10.041. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 7.McNamara MJ, Barrett KG, Christie MJ, Spengler DM. Lumbar spinal stenosis and lower extremity arthroplasty. J Arthroplasty. 1993;8:273–277. [DOI] [PubMed] [Google Scholar]
- 8.Nam D, Riegler V, Clohisy JC, Nunley RM, Barrack RL. The impact of total hip arthroplasty on pelvic motion and functional component position is highly variable. J Arthroplasty. 2017;32:1200–1205. [DOI] [PubMed] [Google Scholar]
- 9.Ochi H, Baba T, Homma Y, Matsumoto M, Nokiri H, Kaneko K. Importance of the spinopelvic factors on the pelvic inclination from standing to sitting before total hip arthroplasty. Eur Spine. 2016;25:3699–3706. [DOI] [PubMed] [Google Scholar]
- 10.Phan D, Bederman SS, Schwarzkopf R. The influence of sagittal spinal deformity on anteversion of the acetabular component in total hip arthroplasty. Bone Joint J. 2015;97:1017–1023. [DOI] [PubMed] [Google Scholar]
- 11.Ranawat CS, Ranawat AS, Lipman JD, White PB, Meftah M. Effect on spinal deformity on pelvic orientation from standing to sitting position. J Arthroplasty. 2016;31:1222–1227. [DOI] [PubMed] [Google Scholar]
- 12.Stefl M, Lundergan W, Heckmann N, McKnight B, Ike H, Murgai R, Dorr LD. Spinopelvic mobility and acetabular component position for total hip arthroplasty. Bone Joint J. 2017;99(Suppl A):37–45. [DOI] [PubMed] [Google Scholar]