Abstract
Background
The posterior interosseous nerve (PIN) is occasionally damaged during distal biceps tendon repair. But to our knowledge, no studies have examined the position of the PIN in relation to the bicipital tuberosity in full supination, which is the recommended position during single-incision distal biceps repair or reconstruction
Questions/purposes
(1) What is the anterior safe zone when exposing the anterior tuberosity with the arm in supination? (2) When drilling the radial tuberosity for bicortical button placement in full supination, how should the drill be angled to avoid PIN injury?
Methods
Fifteen adult cadaver elbows had the PIN dissected around the proximal radius. The position of the PIN was measured relative to the most ulnar aspect of the radius at three sites in full supination: at the bicipital tuberosity (bicipital tuberosity-PIN), 10 mm proximal to the bicipital tuberosity (bicipital tuberosity-proximal), and 10 mm distal to the bicipital tuberosity (bicipital tuberosity-distal). We made another measurement by drawing a line from the lateral humeral epicondyle to the radial styloid. The point where the PIN intersects this line, when viewed laterally and measured from the lateral humeral epicondyle, was marked and measured to indicate where it wraps around the radius laterally (PIN-lateral). The last measurement (bicipital tuberosity-lateral) was made where the line from the lateral humeral epicondyle to the radial styloid intersected the position of the bicipital tuberosity. This was determined by the point where a perpendicular line from the bicipital tuberosity was drawn laterally to meet with the lateral line. We did this to establish if the PIN adopts its most lateral position on the radius at the same level as the bicipital tuberosity.
Results
The anterior safe zone in the approach to the biceps tuberosity extends approximately 15 mm from its prominence (mean, 20.7 mm; range, 16.0–24.1 mm). The PIN crosses the lateral midline from anterior to posterior at 46.0 mm (range, 31.2–67.0 mm) from the lateral epicondyle (lying directly opposite the bicipital tuberosity at nearly the same level); therefore, the drill exit should be posterior to lateral midline while aiming proximally to the bicipital tuberosity.
Conclusion
Our anterior safe zone found that the PIN travels from an anterior position on the radius, when measuring 1 cm proximal to the bicipital tuberosity to a lateral position on the radius at the level of the bicipital tuberosity prominence (on the contralateral cortex), to a slightly more posterior position on the radius 1 cm distal to the bicipital tuberosity. Typically, the PIN sits directly opposite the biceps tuberosity, often directly on the cortex of the radius when the forearm is in full supination.
Clinical Relevance
Because of these findings, perpendicular bicortical drilling starting at the bicipital tuberosity should be avoided. A more proximal and ulnar drilling angle is recommended. Defining a safe zone for an anterior approach seems to be clinically unhelpful due to the high anatomical variability that exists for the position of the PIN around the proximal radius. Future studies could attempt to confirm our findings with the analysis of noncadaveric imaging in three different planes using such modalities as MRI to avoid the effects of tissue distortion during cadaveric preparation and dissection.
Introduction
Posterior interosseous nerve (PIN) palsies are severely debilitating injuries, particularly in the demographic of patients undergoing distal biceps repair or reconstruction [14]. Intraoperative nerve injuries are avoidable with a sound understanding of the relevant anatomy. Birch et al. [4] have found a 3% proportion of neurological injuries in distal biceps repair, for which the PIN was implicated in 6% of patients. Our unit has also experienced these complications, and we feel that this relates to a lack of published evidence on the PIN position during distal biceps repair as well as anatomical variations and anomalies. In their description of the single-incision technique for repair of distal biceps rupture, Bain et al. [3] noted the variable nature of the PIN and the risk of nerve injury. Thus, this study was designed to aid surgeons in understanding the PIN position during distal biceps repair.
Historically, distal biceps repair was performed with a double-incision technique. Rates of PIN palsy were found to be low in a landmark study by Kelly et al. [13] when using this approach. More recently, single-incision techniques have been gained favor due to reduced operative morbidity, improved cosmesis, superior initial repair strength, immediate mobilization, and reduced risk of heterotopic ossification and synostosis [5-7, 10]. These techniques use an anterior incision to retrieve and fix the tendon. Fixation can be achieved with multiple techniques but inserting the distal stump into the radius is thought to enhance tendon healing. This requires tendon fixation on the far cortex, which is usually achieved with a button, as described by Bain et al. [3]. However, damage to the PIN on the far cortex is a concern during bicortical drilling or button flipping as this is not identified during the procedure. The recommended drill direction for bicortical drilling commences just distal and ulnar to the bicipital tuberosity with a medial-to-lateral direction while the forearm is in supination. This allows for excellent reproduction of the more anatomical insertion of the biceps tendon and enhances its biomechanics [15, 16]. Although anterior structures make this difficult to achieve intraoperatively, minimally invasive anterior surgery now offers such trajectories. However, these improved abilities may further endanger posterior structures [15]. Of greatest concern is the PIN. Prior studies suggest that 3% to 5% of patients will experience PIN palsy after biceps tendon repair [8, 9]. The PIN changes position on the radial neck with forearm pronation or supination. Although forearm supination provides the safest position for a volar approach to the proximal radius it may leave the PIN exposed on the contralateral cortex; this is an issue when it comes to bicortical drilling [12].
To date, no studies have examined PIN position in relation to the bicipital tuberosity in full supination. Yet, this is the position recommended during single-incision distal biceps repair or reconstruction to achieve fixation of the biceps on the ulnar and distal aspect of the bicipital tuberosity, which is believed to give the most anatomical repair possible [15, 16]. No other studies have identified a reliable safe-zone for drilling from the bicipital tuberosity in full supination, and no other studies have assessed the appropriate drilling angle that avoids the PIN yet still provides sufficient cortical purchase. Our study addresses the paucity of evidence and specifically, relates to bicortical drilling in supination for distal biceps repair where the only intraoperative landmarks are the bicipital tuberosity, the lateral humeral epicondyle, and the radial styloid. These landmarks are easily found intraoperatively and identify the PIN location to avoid iatrogenic injury during bicortical drilling. Previous authors have also attempted to use anatomical structures to determine the intraoperative position of the PIN. However, the anatomical structures previously used, such as the radial head articular surface, are not typically exposed and are often difficult to identify, making them impractical for clinical use [11]. Thus, in our study we have analyzed easily identifiable and clinically practical anatomical landmarks.
Therefore, we asked: (1) What is the anterior safe zone when exposing the bicipital tuberosity with the arm in supination? (2) When drilling the radial tuberosity for bicortical button placement in full supination, how should the drill be angled to avoid posterior interosseous nerve injury?
Materials and Methods
Our institution’s research ethics committee granted ethical approval to our study (H17/064).
We used 15 adult cadaver upper limbs of average Caucasian size, harvested through the mid-humerus; the limbs had been embalmed through arterial perfusion of a propriety ethanol-phenoxyethanol-based solution. In all, there were six left and nine right limbs as well as seven female and eight male upper limbs. No two limbs were from the same individual. The mean age was 84 years (range, 64–98 years). We included only limbs that did not reveal any signs of previous injury and could achieve full elbow flexion and extension as well as full pronation and supination.
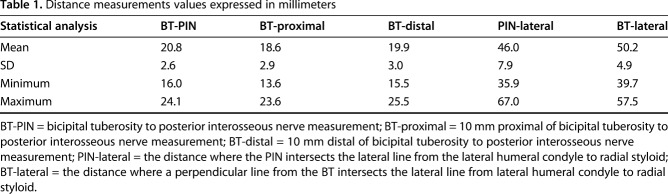
The limbs were placed in a customized device to reproduce the position in which the upper limb is held during biceps repair (partial elbow flexion, full forearm supination; Fig. 1). To ensure reproduction of the position, the experimenter applied a torque to the forearm until resistance was encountered. This was felt to be the point of maximal supination and the typical intraoperative position.
Fig. 1.
The letter “A” depicts the device that we used to keep the forearm in supination during measuring of distances. An overview of the limb dissection is shown by letter “B”. The torque applied to achieve supination is depicted by letter “C”
We made a transverse anterior incision 100 mm proximal and 100 mm distal to the antecubital fossa; this incision was connected to a longitudinal incision to form an “H”. The radial and ulnar skin flaps were raised and the brachioradialis was divided at the mid-forearm level to expose the underlying radial nerve. We followed this plane beneath the brachioradialis proximally to identify the PIN where it separates from the radial nerve. The belly of extensor carpi radialis longus was then divided and the radial nerve was exposed as it emerged from the lateral intermuscular septum into the anterior compartment of the arm to the distal margin of the supinator.
To better visualize the bicipital tuberosity, we divided and reflected the muscle bellies of the pronator teres, flexor carpi radialis, flexor digitorum superficialis and palmaris longus. We divided the supinator muscle to deroof the PIN and to allow adequate exposure and accurate measurements. Throughout, we marked the PIN and maintained its anatomical position, without displacement caused by dissection.
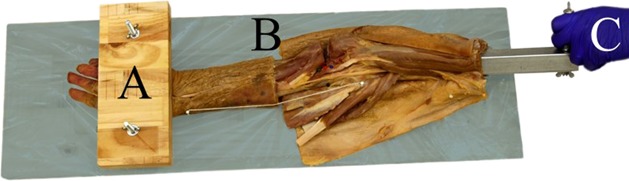
When viewed in a lateral plane, an observer will see the PIN traverse the lateral aspect of the radius from a proximally anterior (volar) to a more posterior (dorsal) position distally in an oblique manner. The point at which the oblique course of the PIN intersects with line F is point E, and it is this distance from the lateral humeral epicondyle that we measured as PIN-lateral (Fig. 2). We concluded that on its own, this measurement is not useful intraoperatively in determining a safe zone because of the great variability in arm sizes. As a result, we proceeded to our final measurement, bicipital tuberosity-lateral, to find a reference point.
Fig. 2.
Dissected upper limb with marker pins for measurement taking. Point A is 1 cm distal to bicipital tuberosity. Point B is at the bicipital tuberosity. Point C is 1 cm proximal to bicipital tuberosity. Point D is the radial nerve. Point E is the posterior interosseous nerve (PIN). Point F is the line from the lateral humeral condyle to the radial styloid.
We defined bicipital tuberosity-lateral as a line originating from the bicipital tuberosity (point B) and extending laterally to intersect at right angles with line F (Fig. 2). When these two measurements in two planes were considered stereotactically, we could determine if the PIN adopted its most lateral position on the radius at the same level as the bicipital tuberosity. Our results indicated that this was the case with moderate-to-strong correlations between the bicipital tuberosity-lateral with PIN-lateral measurements (correlation coefficient [CC] = 0.84).
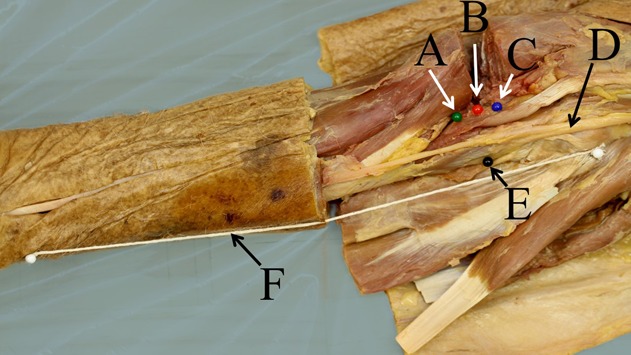
We took several important measurements in our study. Bicipital tuberosity-PIN (line B on Fig. 3) is the distance from the most ulnar aspect of the bicipital tuberosity (point B, Fig. 2) to the closest aspect of the PIN (point E, Fig. 2). Bicipital tuberosity-proximal (line A on Fig. 3) is the distance from the most ulnar aspect 10 mm proximal to the bicipital tuberosity (point C, Fig. 2) to the closest aspect of the PIN. Bicipital tuberosity-distal (line C on Fig. 3) is the distance from the most ulnar aspect 10 mm distal to the bicipital tuberosity (point A, Fig. 2) to the closest aspect of the PIN. PIN-lateral is the distance, when viewed from a lateral position, along the lateral line (measured from the lateral humeral condyle to radial styloid (line F, Fig. 2), where the PIN (point E, Fig. 2) intersects as it moves obliquely from an anterior to posterior position on the radius. Bicipital tuberosity-lateralis the distance, when viewed from a lateral position, along the lateral line (measured from the lateral humeral condyle to radial styloid (line F, Fig 2), where a perpendicular line from the bicipital tuberosity (point B, Fig. 2) intersects this lateral line.
Fig. 3.
Graphical illustration of the posterior interosseous nerve (PIN) course with key measurements to establish the anterior safe zone are shown (lines labelled A, B, and C) with measurements. Line A represents the bicipital tuberosity-proximal measurement; starting from 10 mm proximal of the bicipital tuberosity and going to the posterior interosseous nerve. Line B represents the bicipital tuberosity-PIN measurement; starting at the bicipital tuberosity and going to the posterior interosseous nerve. Line C represents the bicipital tuberosity-distal measurement; starting 10 mm distal of the bicipital tuberosity and going to the posterior interosseous nerve measurement. The anterior radial PIN safe zone is represented by the shaded area.
All measurements were performed with Vernier callipers and measurements recorded in millimeters to one decimal point by two of the authors (DB, FAL-M). Intra- and interrater reliability was assessed using five randomly-selected limbs.
The measurements were compared statistically using SPSS Version 24.0 (SPSS Statistics, Chicago, IL, USA). After performing the Kolmogorov-Smirnov test to determine normality in the values, we used the Student’s t-test to compare the values for sidedness and sex-related differences. The Pearson test was used to assess correlations between the values. Repeated measurement reliability was assessed using the intraclass coefficient (ICC) and Cronbach’s alpha, with a two-way mixed model for the intrarater agreement and a two-way random model for interrater agreement, applying the single measures estimation. P values of 0.05 or less were considered statistically significant. We did not identify differences for any of the measurements related to age, sex or side.
The ICC for all measurements ranged from 0.86 to 0.97, showing strong repeatability of the measurements (Cronbach’s alpha, 0.92–0.98). Equally, interrater agreement was high, with ICCs ranging from 0.90 to 0.96 (Cronbach’s alpha, 0.95–0.98).
Results
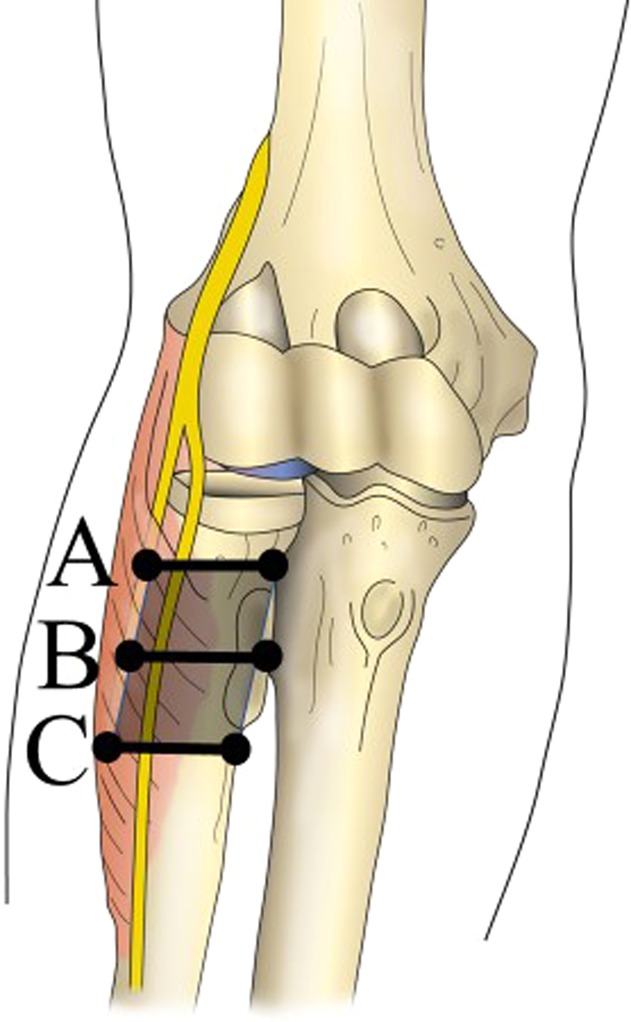
The anterior safe zone in the approach to the biceps tuberosity extends approximately 15 mm from its prominence (mean, 20.7 mm; range, 16.0–24.1 mm) (Fig. 3). The course of the PIN is highly variable, and this was reflected by the broad distribution of measurements (Table 1). The distance from the most prominent part of the bicipital tuberosity to the most medial aspect of the PIN was slightly longer than those measurements from 10 mm proximal or 10 mm distal the bicipital tuberosity (Fig. 4). The distance from the most prominent part of the bicipital tuberosity to the most medial aspect to the PIN was slightly longer than those measurements from 10 mm proximal or 10 mm distal the bicipital tuberosity (Table 1). During the dissection, the PIN was found to sit close to the radius while under the supinator. This ranged from direct contact with the periosteum to 2 mm from the bone surface.
Table 1.
Distance measurements values expressed in millimeters
Fig. 4.
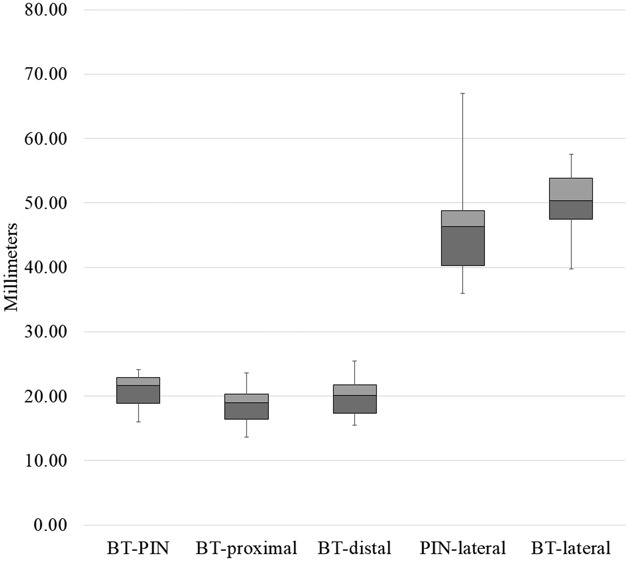
Box-whisker plot of five measurements. The 25% quartile, median and 75% quartile are depicted for averaged values from all arms. The whiskers indicate the minima and maxima. BT-PIN = bicipital tuberosity to the posterior interosseous nerve measurement; BT-proximal = 10 mm proximal of bicipital tuberosity to posterior interosseous nerve measurement; BT-distal = 10 mm distal of bicipital tuberosity to posterior interosseous nerve measurement; PIN-lateral = the distance where the PIN intersects the lateral line from the lateral humeral condyle to radial styloid; BT-lateral = the distance where a perpendicular line from the bicipital tuberosity intersects the lateral line from lateral humeral condyle to radial styloid.
When drilling the radial tuberosity for bicortical button placement, in full supination, the drill exit should be posterior to the lateral midline and proximal to the bicipital tuberosity. The PIN crossed the lateral midline from anterior to posterior at 46.0 mm (range, 35.9–67.0 mm) from the lateral epicondyle; this is at the same level as the bicipital tuberosity, which is located at 50.2 mm (range, 39.7–57.5 mm). From a visual perspective, during full supination, the PIN lies directly on the opposite cortex of the radius to the prominence of the bicipital tuberosity (Fig. 5). Proximal to the level of the bicipital tuberosity the PIN is more anterior, and when distal to this, it is more posterior. When considering a transverse clock face view of the radius with 0 being anterior, and 180° being posterior, our findings showed that the PIN was positioned at around 270° on the radius at the level of the bicipital tuberosity marked by 90° (Fig. 5). We found moderate-to-strong correlations for bicipital tuberosity-PIN with bicipital tuberosity-proximal (CC = 0.75), bicipital tuberosity-PIN with bicipital tuberosity-distal (CC = 0.79), bicipital tuberosity-proximal with bicipital tuberosity-distal (CC = 0.62), and bicipital tuberosity-lateral with PIN-lateral (CC = 0.84).
Fig. 5.
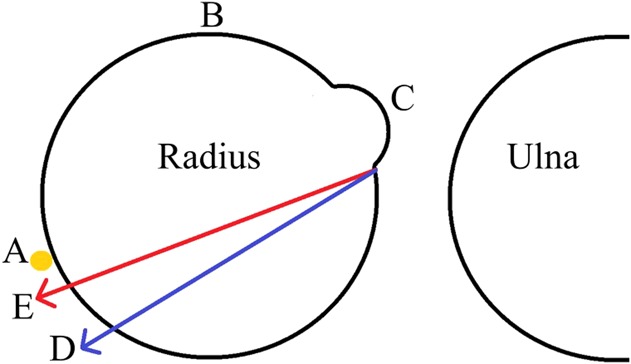
This figure shows an axial view of two drilling vectors. The letter “A” depicts the posterior interosseous nerve (PIN) opposite the bicipital tuberosity, which itself is marked as “C” and sits at almost 70°. “B” is the anterior aspect of the radius in full supination at 0°. Note the drilling angle typically commences slightly distal and ulnar from the bicipital tuberosity. Vector E has greater cross section through bone and is likely biomechanically superior to vector D; however, it places the PIN at risk. Vector D is more ulnarly angulated than vector E and thus reduces the risk of injury to the PIN while sacrificing purchase on the bone.
Discussion
When in full supination, the PIN wraps around the lateral aspect of the radius. A primary aim of the study was to examine the anterior safe zone during bicortical drilling in distal biceps repair to avoid iatrogenic injury to the PIN. Another aim was to determine whether the PIN crosses over the lateral aspect of the radius at the level of the bicipital tuberosity; if it did, it would be directly endangered by bicortical drilling during distal biceps repair. Previous studies, however, have not been able to accurately determine the position of the PIN in relation to the bicipital tuberosity. Such measurements are difficult during dissection without distorting relationships. Our first three measurements allowed us to determine the anterior safe area and the last two measurements allowed us to determine whether the PIN crosses over the lateral aspect of the radius at the same level as the bicipital tuberosity on the contralateral cortex.
Limitations of our study include the small sample size. Although this sample size was bigger than any previous study, we only had deceased Caucasian donors with an average age of 84 years. This could limit the applicability of the data to other populations. Our measurements were obtained through several generous incisions that could have affected tissue integrity and subsequent statistical analysis. The effect of tissue dissection, if any, is likely overestimating true distances. This issue is further compounded through surgical dissection to expose the nerve, although the nerve sheath and its deeper attachments were not disturbed. We endeavoured to maintain PIN position throughout, so that dissection did not affect its relative position and subsequent measurements. Tissue fixation may also have played a role in the positions of the PIN with relation to supination and pronation due to tissue contracture during the fixation process. This is likely to underestimate measurements. Another limitation of the study is that we used absolute differences (distances in millimeters), rather than ratios to determine an anterior safe zone. Very large and very small people will likely not be represented well with these measurements. It is unlikely that our sample size would achieve a significant ratio to determine an anterior safe zone. Furthermore, it would add an extra layer of complexity for the operating surgeon to measure from landmarks that might be covered with ample soft tissue during a minimal incision technique. Furthermore, the landmarks themselves may be distorted and cause any ratio that does exist to be inapplicable in certain limbs. The most important measurement is the minimal distance from the bicipital tuberosity to the PIN and therefore absolute measurements are probably more practical than ratios.
To address our other research aim, whether the PIN crosses over the lateral aspect of the radius at the level of the bicipital tuberosity, we employed a technique which mimics that of a ratio; namely our last two measurements and analysing if these correlated; they did.
A difference between sexes in the measurements for the anterior safe zone likely exists, although we did not find any, perhaps secondary to our sample size. When operating on anatomically smaller, younger females than in our sample it is possible that the minimum safe zone measurement is even smaller. In these instances, our other observations and recommendations should be followed. The results addressing our other research question should be accurate, even in smaller limbs; specifically, that the PIN sits on the contralateral cortex, opposite the bicipital tuberosity, when in supination.
Axial clock face measurements for bicipital tuberosity-proximal or bicipital tuberosity-distal were not performed because this would require fine transverse limb sectioning. Attaining axial views through the radius with dissection and bone sawing would compromise the anatomical position of the PIN substantially, unless the limb was frozen or plastinated. Future studies could look at exploring the position of the PIN on the radius from an axial setting; however, this would likely require radiological imaging.
Our measurements PIN-lateral and bicipital tuberosity-lateral rely on the line from the lateral humeral condyle to the radial styloid (Fig. 2). This line is not straight; it can be seen curving around the tissues. Although this may slightly alter the distances that were measured from the string it is also replicative of a real intraoperative scenario where the forearm muscle bellies are likely to make it a nonlinear measurement.
When it comes to an anterior safe zone, our first three measurements and the correlation coefficients between our first three measurements show that the PIN travels from an anterior position on the radius, when measuring 1 cm proximal to the bicipital tuberosity to a lateral position on the radius at the level of the bicipital tuberosity prominence (on the contralateral cortex), to a slightly more posterior position on the radius 1 cm distal to the bicipital tuberosity. A key finding of our anterior safe zone was the proximity in which the PIN lies relative to the bicipital tuberosity; it is at least 16.0 mm away from the bicipital tuberosity prominence. However, due to the somewhat unpredictable anatomy of the PIN among individuals, this finding is unlikely to have great intraoperative significance when it comes to bicortical drilling. Our safe zone gives the operating surgeon an idea of the course of the PIN around the head of the radius and where it lies in relation to the bicipital tuberosity. However, the finding of this study that has greater intraoperative significance is in the results for our other research question, which focuses on drilling trajectory. Our safe zone is reserved for an anterior approach to dissecting around the proximal radial neck and not for drilling trajectory.
Like our study, Heidari et al. [12] found that the proximity of the PIN may be as little as a few millimeters away during the subperiosteal dissection of supinator. This is an important finding because bicortical drilling will likely injure the nerve if the drill exits at the location of the PIN. Furthermore, even if the drill misses the PIN, the PIN is still at risk of becoming trapped by cortical button repair methods because it sits so close to the periosteum. According to Heidari et al. [12], the course of the PIN through the supinator muscle and after it emerges into the posterior compartment is not constant. This was also echoed in our study; we found that the PIN had numerous and variable branches as it travels under the arcade of Frohse in the supinator. Ay et al. [1] have described the anatomical variations of the PIN at this level.
Bicortical drilling should be approached in full supination for the best possible anatomical repair, but with slight ulnar and proximal angulation to avoid PIN injury when the drill exits the contralateral cortex. When in full supination, the PIN wraps around the lateral aspect of the radius. No previous studies have identified exactly where this occurs on the radius. Our last two measurements found that the PIN lies directly opposite the bicipital tuberosity, on the contralateral cortex, with moderate-to-strong correlations between the last two measurements, bicipital tuberosity-lateral with PIN-lateral (CC = 0.84). The PIN adopts the most lateral position on the radius, at 270° on axial view when the forearm is in full supination. We concluded that perpendicular bicortical drilling from the bicipital tuberosity should be avoided while in supination. A more proximally and more posterior drilling angle is recommended (Fig. 6).
Fig. 6.
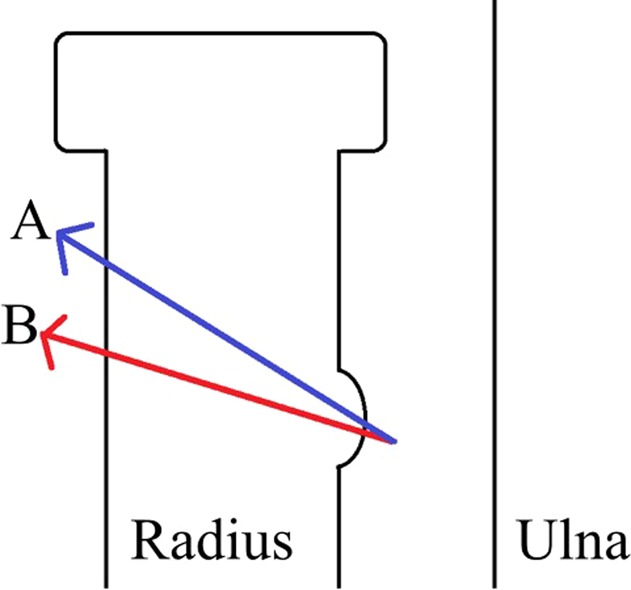
This figure shows a coronal view of possible drilling vectors. A more proximally angulated drilling angle (vector A) is recommended to avoid the posterior interosseous nerve, which is located opposite the bicipital tuberosity.
In our literature review we found research by Lo et al. [15], Saldua et al. [17], and Thumm et al. [18], which focused on drill trajectory and proximity of the PIN during cortical button distal biceps repair. These studies tried to establish safe drilling trajectories across the radius to avoid PIN injury during cortical button distal biceps repair. They also had large confidence intervals and were unable to establish a clear zone of safety for drill placement and trajectory. This is likely due to the variable nature of the PIN at this position. Their data also recommended avoiding drilling distally and radially to minimize risk to the PIN. Our study was the first to do this in supination, in greater numbers, and we described (through our last two measurements) that the PIN sits opposite the bicipital tuberosity in supination and, therefore, drilling across the radius and exiting directly opposite the bicipital tuberosity is likely to increase the risk of iatrogenic PIN injury. Previous studies, such as those by Lo et al. [15] and Prud’homme-Foster et al. [16] have demonstrated that appropriate drill placement for bicortical drilling commences just distal and ulna to the bicipital tuberosity, while the forearm is in supination. This allows for excellent reproduction of the more anatomical insertion of the biceps tendon and enhances its biomechanics. A tendon that is repaired too radially will lose the cam effect and is unlikely to generate full supination torque when the arm is in neutral rotation or in supination [16]. A different study by Baba et al. [2] states that anatomical repair is not required, and they in fact recommend a more proximal starting position. However, their small patient numbers and the shortcomings of their postoperative functional analysis limits the strength of their findings. The evidence is quite clear that for appropriate biomechanics, the drilling should start just distal and ulna to the bicipital tuberosity. Our study found that you can safely do that, if you then angle the drill proximally and ulnarly, which does not compromise biomechanics and avoids the PIN on the other side.
More vertical drilling may be the tendency in some centers, although our findings show that this should only be employed if also drilling more proximally; if drilled distally with a vertical projection, this endangers the PIN more than horizontal distal drilling because the PIN wraps around the radius at the level of the bicipital tuberosity and tends to lie more posteriorly on the radius distal to the BT. With proximal and ulnar angulation of the drill there is a potential trade-off between fixation/mechanics and avoiding PIN injury.
In conclusion, our anterior safe zone found that the PIN travels from an anterior position on the radius, when measuring 1 cm proximal to the bicipital tuberosity to a lateral position on the radius at the level of the bicipital tuberosity prominence (on the contralateral cortex), to a slightly more posterior position on the radius 1 cm distal to the bicipital tuberosity. The anterior safe zone in the approach to the biceps tuberosity extends approximately 15 mm from its prominence (mean, 20.7 mm; range, 16.0–24.1 mm). The PIN crosses the lateral midline from anterior to posterior at 46.0 mm (range, 31.2–67.0 mm) from the lateral epicondyle (lying directly opposite the bicipital tuberosity at nearly the same level); therefore, the drill exit should be posterior to midline while aiming proximally to the bicipital tuberosity. The PIN often lies directly on the cortex of the radius when the forearm is in full supination. Because of these findings, perpendicular bicortical drilling starting at the bicipital tuberosity should be avoided. A more proximal and ulnar drilling angle is recommended. Defining a safe zone for an anterior approach seems to be clinically unhelpful due to the high anatomical variability that exists for the position of the PIN around the proximal radius. Future studies could attempt to confirm our findings with the analysis of noncadaveric imaging in three different planes using such modalities as MRI to avoid the effects of tissue distortion during cadaveric preparation and dissection.
Acknowledgments
We thank Glynny Kieser for proofreading, Christine Hammer for image editing, Robby McPhee for graphic design, and most importantly body donors and their families for their precious gifts and support.
Footnotes
Each author certifies that neither he, nor any member of his immediate family, have funding or commercial associations (consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Clinical Orthopaedics and Related Research® editors and board members are on file with the publication and can be viewed on request.
Clinical Orthopaedics and Related Research® neither advocates nor endorses the use of any treatment, drug, or device. Readers are encouraged to always seek additional information, including FDA approval status, of any drug or device before clinical use.
Each author certifies that his institution approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was completed at the Anatomy Department, University of Otago, Dunedin, New Zealand.
References
- 1.Ay S, Apaydin N, Acar H, Akinci M, Piskin A, Tekdemir I, Elhan A. Anatomic pattern of the terminal branches of posterior interosseous nerve. Clin Anat. 2005;18:290-295. [DOI] [PubMed] [Google Scholar]
- 2.Baba M, Leon JV, Symes M, Dorrestijn O, Young A, Cass B. Clinical outcomes and safety of distal biceps repair using a modified entry point. ANZ J Surg. 2017;87:376-379. [DOI] [PubMed] [Google Scholar]
- 3.Bain GI, Prem H, Heptinstall RJ, Verhellen R, Paix D. Repair of distal biceps tendon rupture: A new technique using the endobutton. J Shoulder Elbow Surg. 2000;9:120-126. [PubMed] [Google Scholar]
- 4.Birch R, Bonney G, Dowell J, Hollingdale J. Iatrogenic injuries of peripheral nerves. J Bone Joint Surg Br. 1991;73:280-282. [DOI] [PubMed] [Google Scholar]
- 5.Boyd HB, Anderson LD. A method for reinsertion of the distal biceps brachii tendon. J Bone Joint Surg. 1961;43:1041-1043. [Google Scholar]
- 6.Chavan PR, Duquin TR, Bisson LJ. Repair of the ruptured distal biceps tendon: A systematic review. Am J Sports Med. 2008;36:1618-1624. [DOI] [PubMed] [Google Scholar]
- 7.Chillemi C, Marinelli M, De Cupis V. Rupture of the distal biceps brachii tendon: Conservative treatment versus anatomic reinsertion--clinical and radiological evaluation after 2 years. Arch Orthop Trauma Surg. 2007;127:705-708. [DOI] [PubMed] [Google Scholar]
- 8.Dobbie RP. Avulsion of the lower biceps brachii tendon. Am J Surg. 1941;51:662-683. [Google Scholar]
- 9.Fajardo MR, Rosenberg Z, Christoforou D, Grossman JA. Multiple nerve injuries following repair of a distal biceps tendon rupture--case report and review of the literature. Bull Hosp Jt Dis (2013). 2013;71:166-169. [PubMed] [Google Scholar]
- 10.Greenberg JA, Fernandez JJ, Wang T, Turner C. Endobutton-assisted repair of distal biceps tendon ruptures. J Shoulder Elbow Surg. 2003;12:484-490. [DOI] [PubMed] [Google Scholar]
- 11.Hackl M, Wegmann K, Lappen S, Helf C, Burkhart KJ, Muller LP. The course of the posterior interosseous nerve in relation to the proximal radius: Is there a reliable landmark? Injury. 2015;46:687-692. [DOI] [PubMed] [Google Scholar]
- 12.Heidari N, Kraus T, Weinberg AM, Weiglein AH, Grechenig W. The risk injury to the posterior interosseous nerve in standard approaches to the proximal radius: A cadaver study. Surg Radiol Anat. 2011;33:353-357. [DOI] [PubMed] [Google Scholar]
- 13.Kelly EW, Morrey BF, O'Driscoll SW. Complications of repair of the distal biceps tendon with the modified two-incision technique. J Bone Joint Surg Am. 2000;82-A:1575-1581. [DOI] [PubMed] [Google Scholar]
- 14.Leighton MM, Bush-Joseph CA, Bach BR., Jr. Distal biceps brachii repair. Results in dominant and nondominant extremities. Clin Orthop Relat Res. 1995:114-121. [PubMed] [Google Scholar]
- 15.Lo EY, Li CS, Van den Bogaerde JM. The effect of drill trajectory on proximity to the posterior interosseous nerve during cortical button distal biceps repair. Arthroscopy. 2011;27:1048-1054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Prud'homme-Foster M, Louati H, Pollock JW, Papp S. Proper placement of the distal biceps tendon during repair improves supination strength--a biomechanical analysis. J Shoulder Elbow Surg. 2015;24:527-532. [DOI] [PubMed] [Google Scholar]
- 17.Saldua N, Carney J, Dewing C, Thompson M. The effect of drilling angle on posterior interosseous nerve safety during open and endoscopic anterior single-incision repair of the distal biceps tendon. Arthroscopy. 2008;24:305-310. [DOI] [PubMed] [Google Scholar]
- 18.Thumm N, Hutchinson D, Zhang C, Drago S, Tyser AR. Proximity of the posterior interosseous nerve during cortical button guidewire placement for distal biceps tendon reattachment. J Hand Surg Am. 2015;40:534-536. [DOI] [PubMed] [Google Scholar]