Abstract
Rationale:
Periprosthetic osteolysis secondary to septic loosening and aseptic loosening is a well-described phenomenon associated with artificial hip arthroplasty. Periprosthetic bone loss as a result of metastatic infiltration is an uncommon cause of early, progressive loosening of joint replacement prosthesis and is rarely described in the literature.
Patient concerns:
The present study describes a 70-year-old male patient who was diagnosed with pulmonary squamous cell carcinoma 5 years after total hip arthroplasty (THA) and developed a metastasis from squamous cell carcinoma in the periprosthetic neosynovial tissue 1 year after formal chemotherapy. The main complaint was hip pain with limited activity for about 3 months.
Diagnoses:
Expansive bone destruction and periprosthetic osteolysis at the right femoral trochanter were identified through X-ray and 99mTc bone scan. The diagnosis of pulmonary squamous cell carcinoma metastasis was finally confirmed on the basis of postoperative pathological examination.
Interventions:
The patient underwent open surgery with proximal femoral prosthesis revision and tumor prosthesis resection to completely remove the tumor tissue and relieve pain.
Outcomes:
The patient was completely relieved of pain at discharge 2 weeks after surgery and experienced no complications. However, the patient died of respiratory failure due to disease progression 3 months after surgery.
Lessons:
We believe that clinicians should maintain a high index of suspicion and consider metastatic disease in differential diagnosis of cases of aseptic loosening, particularly if the patient has a history of malignant disease and the osteolytic lesion involves the outer cortex. In addition, patients with a known history of malignancy should be screened with a pre-operative bone scan to rule out any metastatic infiltration and regularly followed up at short intervals to detect any early bone loss.
Keywords: lung cancer, osteolysis, periprosthetic metastasis, squamous cell carcinoma, total hip arthroplasty
1. Introduction
Periprosthetic osteolysis is a common complication in patients who undergo total hip arthroplasty (THA). In the vast majority of cases, aseptic or septic loosening is responsible for periprosthetic osteolysis and subsequent THA failure, but with the use of antibiotic prophylaxis and biomechanical properties and immobilization of the implant, the lifespan of THA increases.[1,2] Lung cancer is the most common malignant tumor in the world, with the highest mortality and bone metastasis rates. In Western countries, it has been reported that the incidence of bone metastases in lung cancer patients is approximately 30–40%, and the median survival time (MST) of patients with such metastases is only 6 to 10 months.[3] Some examples of primary malignancies associated with surgical implants have previously been described, but the development of metastasis associated with joint replacement is rare. In this study, we described a rare case of squamous cell carcinoma metastasis in the periprosthetic neosynovial tissue in a 70-year-old male patient 5 years post THA.
2. Presenting concerns
A 70-year-old male patient presented to our clinic with the chief complaints of right hip pain and limitation of hip motion. Six years prior, the patient suffered a right femoral neck fracture after a fall and received a corrective THA in another medical center (Fig. 1A). After the operation, the patient recovered satisfactorily and performed well without any discomfort. In October 2016, the patient experienced repeated cough and hemoptysis. Computed tomography (CT) showed a mass in the right upper lung and a large lymph node in the mediastinal and right hilum, indicating central lung cancer and lymph node metastasis (Fig. 2). Electronic bronchoscopy revealed squamous cell carcinoma in the right lung. The patient was followed up regularly and received chemotherapy.
Figure 1.
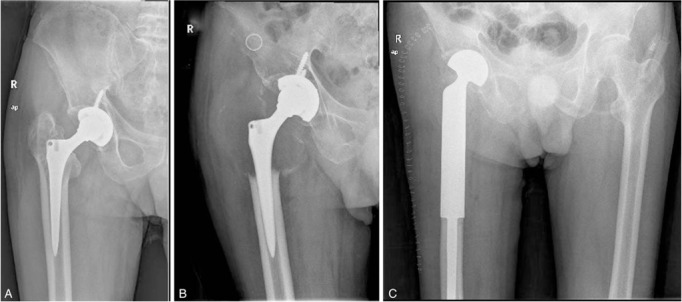
(A) Anteroposterior radiographs acquired 6 years after total hip arthroplasty show the right hip. (B) Radiograph acquired 6 years after total hip arthroplasty shows expansion and dissolution of the small trochanter region. (C) Postoperative radiograph of the hip at 4 days shows proximal femoral prosthesis revision and tumor prosthesis resection.
Figure 2.

Computed tomography of the chest shows a malignant mass in the right upper lung.
3. Clinical findings
The patient had no related family or allergy history, past medical illness, or other comorbidities but had a history of smoking for about 40 years. In the general physical examination, the range of motion of the right hip was reduced, the muscles of the right thigh were slightly atrophied, and the muscle strength of the right lower limb was slightly worse than that of the left side.
4. Diagnostic focus and assessment
In September 2017, the patient presented to our outpatient department with continuous pain in the right hip and right groin, with further aggravation upon joint movement. Radiologic studies showed expansive bone destruction and periprosthetic osteolysis at the right femoral trochanter (Fig. 1B). The erythrocyte sedimentation rate (ESR) was 70 mm/h (normal range <30 mm/h), and the C-reactive protein (CRP) concentration was 2.01 mg/dL (normal range <0.8 mg/dL). 99mTc bone scan revealed strong uptake in the upper segment of the right femoral shaft and confirmed the presence of metastasis (Fig. 3). Based on the above information, the patient was suspected to have bone metastasis of lung cancer.
Figure 3.
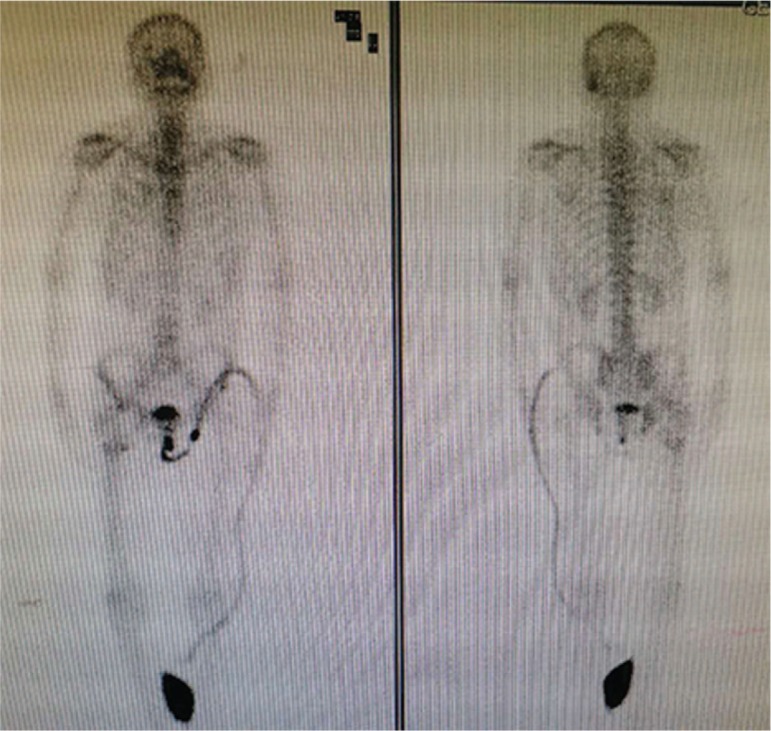
Radionucleotide bone scan confirms strong uptake in the upper segment of the right femoral shaft.
5. Therapeutic focus and assessment
Because the patient's pain in the right hip was so severe and the bone destruction was so extensive, revision surgery using a proximal femoral allograft was recommended. In October 2017, experienced orthopedic surgeons performed open surgery including proximal femoral prosthesis revision and tumor prosthesis resection after excluding any surgical contraindications (Fig. 1C). The pathological section of the periprosthetic tissue suggested squamous cell carcinoma (Fig. 4). After the operation, the patient's pain was completely relieved, and he recovered well and was discharged after 2 weeks.
Figure 4.
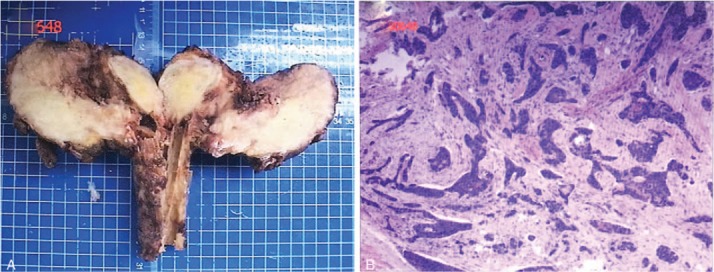
(A) A photograph of the removed upper femoral tumor. (B) Hematoxylin and eosin staining of metastatic squamous cell carcinoma.
6. Follow-up and outcomes
Three months after operation, the patient suddenly developed lethargy, anorexia, and fatigue. CT showed right central lung cancer with right pleural effusion. In January 2018, the patient died of respiratory failure due to disease progression.
7. Discussion
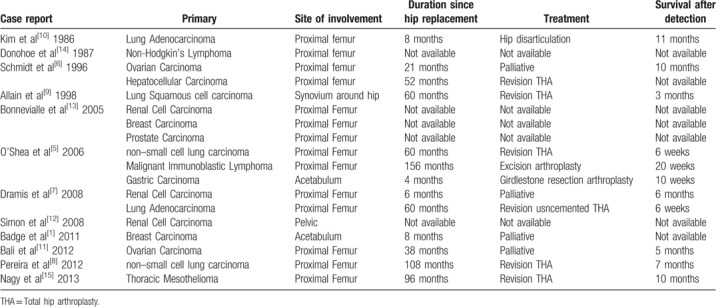
Infection, aseptic loosening, and periprosthetic osteolysis can result in massive periprosthetic bone loss after joint replacement surgery, leading to loosening of the components and periprosthetic fractures.[1,4] Apart from periprosthetic fractures and recurrent dislocations, the most common delayed complications of arthroplasties include septic loosening and aseptic loosening. Metastasis in and around joint arthroplasty sites is rare, and periprosthetic loosening secondary to metastasis in the hip arthroplasty site is even more rare. To our knowledge, primary malignancies (mostly sarcomas) around prosthetic joint replacements are more common than metastatic infiltrates.[5–8] There have been several reports of cases in which THA failure occurred as a result of periprosthetic malignant metastasis. These cases involved metastatic disease from the following primary malignancies: 5 cases of bronchogenic carcinoma; 3 cases of renal cell carcinoma; 2 cases of ovarian carcinoma; and 2 cases of breast cancer, gastric adenocarcinoma, malignant immunoblastic lymphoma, non-Hodgkin's lymphoma, thoracic mesothelioma, hepatocellular carcinoma, and prostate cancer (Table 1).[1,5–15]
Table 1.
Review of reported cases of metastatic infiltration around hip replacement from English language literature.
By reviewing the relevant literature, we found that lung cancer metastasis to the hip replacement and periprosthetic site is more common than other primary malignancies. Bone tissue is one of the most common distant metastatic sites of lung cancer. Common bone metastasis sites include ribs, thoracic vertebrae, and lumbar vertebrae.[16] In addition, we found that the pathological type of lung cancer with bone metastases is most often adenocarcinoma, and it is an independent factor affecting the prognosis of patients with bone metastases from lung cancer. Bone metastasis of lung adenocarcinoma can be explained by the following: Firstly, adenocarcinoma is often located in the periphery of the lung and can easily directly invade the rib bone. Secondly, adenocarcinoma is highly infiltrative with destructive growth characteristics and thus can easily invade blood vessels and lymphatic vessels, resulting in distant metastasis.
However, bone metastases in lung squamous cell carcinoma are relatively rare, and metastasis in joint replacement and periprosthetic sites is even more rare. To our knowledge, Allain et al[9] reported the first case of squamous cell carcinoma of the lung metastasizing to the neosynovium of a THA, which presented as pain and femoral loosening. The present study is the second reported case in the literature of this rare metastasis of lung squamous cell carcinoma to THA.
The pathological mechanism of bone metastasis of malignant tumors involves the interaction of tumor cells, osteoblasts, and osteoclasts, which destroys the dynamic balance between bone formation and bone resorption; bone metastasis can be divided into 3 types: osteolytic bone metastasis, osteogenic bone metastasis, and mixed bone metastases.[17,18] Goto et al[19] proposed that lung cancer cells can form an osteolytic metastasis by enhancing osteolytic bone resorption, generating an environment that facilitates cancer cell colonization and spread, and the interaction between cancer cells and the bone microenvironment leads to progression of metastatic tumors and bone. A vicious circle of metastatic bone destruction is thus created. In addition, some investigators have speculated regarding the possibility of increased susceptibility of periprosthetic tissues to metastatic seeding. It was reported that abnormalities in blood flow as a result of surgical injury and the healing process may predispose the patient to development of metastases around surgical implants.[11] Furthermore, Allain et al[9] reported that metastases had a predilection for bone where there is an abnormal increase in blood supply. The inflammatory reaction to metastatic tumor includes the presence and activation of macrophages, giant cells, and leukocytes and is mostly associated with necrosis of bone. Activation of these inflammatory cells may lead to aseptic loosening of the implant, but the immune processes involved in these metastatic seeds are very complex, and their role in local defense against malignancies needs to be further understood.
In conclusion, we believe that clinicians should maintain a high index of suspicion and consider metastatic disease in differential diagnosis of cases of aseptic loosening, particularly when there is rapid progression of symptoms, the history is atypical, the patient has a history of malignant disease, and the osteolytic lesion involves the outer cortex. In addition, patients with a known history of malignancy should be screened with a pre-operative bone scan to rule out any metastatic infiltration and followed-up regularly at short intervals to detect any early bone loss. Once the presence of malignancy has been confirmed, a THA must be performed in order to allow the patient to have a painless joint for the short time for which they are likely to survive.
Acknowledgments
We greatly appreciate the patient and his family for allowing us to use the medical documents and information that led to the present article. We would like to thank Editage for English language editing.
Author contributions
Investigation: Xiaolong Yu.
Project administration: Bin Zhang.
Writing – original draft: Haibo Zhan, Tian Gao.
Writing – review & editing: Jin Zeng, Min Dai.
Footnotes
Abbreviations: CRP = C-reactive protein, CT = computed tomography, ESR = erythrocyte sedimentation rate, MST = median survival time, THA = total hip arthroplasty.
Haibo Zhan and Tian Gao have contributed to the work equally and should be regarded as co-first authors.
The study protocol was approved by the Ethical Institutional Review Board of the First Affiliated Hospital of Nanchang University, and written informed consent was obtained from the study participant.
The consent for publication of the manuscript and the related images from the patient and/or his relatives has been obtained by the First Affiliated Hospital of Nanchang University.
The authors have no conflicts of interest to disclose.
References
- [1].Badge R, Divecha H, Sochart D. Early periprosthetic metastasis following total hip replacement in a patient with breast carcinoma: a case report and review of literature. J Clin Med Res 2011;3:203–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Archibeck MJ, Jacobs JJ, Roebuck KA, et al. The basic science of periprosthetic osteolysis. Instr Course Lect 2001;50:185–95. [PubMed] [Google Scholar]
- [3].Tsuya A, Kurata T, Tamura K, et al. Skeletal metastases in non-small cell lung cancer: a retrospective study. Lung Cancer 2007;57:229–32. [DOI] [PubMed] [Google Scholar]
- [4].Troop JK, Mallory TH, Fisher DA, et al. Malignant fibrous histiocytoma after total hip arthroplasty. A case report. Clin Orthop Relat Res 1990;297–300. [PubMed] [Google Scholar]
- [5].O'Shea K, Kearns SR, Blaney A, et al. Periprosthetic malignancy as a mode of failure in total hip arthroplasty. J Arthroplasty 2006;21:926–30. [DOI] [PubMed] [Google Scholar]
- [6].Schmidt AH, Walker G, Kyle RF, et al. Periprosthetic metastatic carcinoma. Pitfalls in the management of two cases initially diagnosed as osteolysis. J Arthroplasty 1996;11:613–9. [DOI] [PubMed] [Google Scholar]
- [7].Dramis A, Desai AS, Board TN, et al. Periprosthetic osteolysis due to metastatic renal cell carcinoma: a case report. Cases J 2008;1:297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Pereira A, Massada M, Sousa R, et al. Metastatic carcinoma as an unusual cause of failure in total hip arthroplasty. J Surg Case Rep 2012;2012:9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Allain J, Le Mouel S, Voicin MC, et al. The importance of systematic histological examination after loosening of an implant. J Bone Joint Surg Br 1998;80:591–4. [DOI] [PubMed] [Google Scholar]
- [10].Kim YH, Yun YH. Metastasis of lung carcinoma to proximal femur after hip implant. Orthop Rev 1986;15:534–9. [PubMed] [Google Scholar]
- [11].Bali K, Prabhakar S, Krishnan V, et al. Hip hemiarthroplasty periprosthetic loosening caused by papillary ovarian carcinoma metastasis in a 78-year-old woman: a rare presentation and a literature review. Am J Orthop 2012;41:33–6. [PubMed] [Google Scholar]
- [12].Simon JP, Bellemans J, Samson I. Metastasis from renal cell carcinoma presenting as osteolysis in total hip arthroplasty: a case report. Acta Orthop Belg 2008;74:122–4. [PubMed] [Google Scholar]
- [13].Bonnevialle P, Brouchet A, Sans N, et al. Metastasis on previous hip arthroplasty: three cases. Rev Chir Orthop Reparatrice Appar Mot 2005;91:558–63. [DOI] [PubMed] [Google Scholar]
- [14].Donohoe KJ, Patton DD. Metastatic non-Hodgkin's lymphoma on bone scintigraphy mimicking loosening or infection of hip prosthesis. Clin Nucl Med 1987;12:888–9. [DOI] [PubMed] [Google Scholar]
- [15].Nagy MT, Young AF, Gorgees N, et al. Periprosthetic metastasis: a rare cause for prosthetic loosening. BMJ Case Rep 2013;2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Quint LE, Tummala S, Brisson LJ, et al. Distribution of distant metastases from newly diagnosed non-small cell lung cancer. Ann Thorac Surg 1996;62:246–50. [DOI] [PubMed] [Google Scholar]
- [17].Esposito M, Guise T, Kang Y. The biology of bone metastasis. Cold Spring Harb Perspect Med 2018;8: [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Luo Q, Xu Z, Wang L, et al. Progress in the research on the mechanism of bone metastasis in lung cancer. Mol Clin Oncol 2016;5:227–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Goto T, Hirotsu Y, Amemiya K, et al. Distribution of circulating tumor DNA in lung cancer: analysis of the primary lung and bone marrow along with the pulmonary venous and peripheral blood. Oncotarget 2017;8:59268–81. [DOI] [PMC free article] [PubMed] [Google Scholar]


