Abstract
Rationale:
Pulmonary embolism is a potentially devastating medical condition. Although deep-vein thrombosis is the most common etiology, a nonthrombotic pulmonary embolism is not uncommon.
Patient concerns:
A 45-year-old woman was admitted to our hospital for progressive effort dyspnea for 3 weeks.
Diagnosis:
Echocardiography revealed a mobile mass extending from the right atrium to the bilateral proximal pulmonary artery. As the mass was no response to thrombotic therapy, intravenous leiomyomatosis was suspected. Computed tomography (CT) revealed a hypo-attenuated tumor extending from the ovarian vein to the pulmonary artery.
Interventions:
A 1-stage operation for the surgical removal of the tumor, right salpingo-oophorectomy and subtotal hysterectomy were performed. Surgical specimen was identified as uterine leiomyomatosis without malignant transformation.
Outcomes:
The patient was followed- up for 2 years and subsequent CT did not reveal any notable lesions.
Lessons:
Nonthrombotic pulmonary embolism is a potentially life-threatening complication. This case indicated intravenous leiomyomatosis should be considered in the differential diagnosis for certain cases. Complete surgical excision was the only curative treatment.
Keywords: cardiac surgery, intravenous leiomyomatosis, nonthrombotic pulmonary embolism
1. Introduction
Pulmonary embolism is a potentially devastating medical condition and is the 3rd leading cause of cardiovascular death in worldwide.[1] Pulmonary embolism occasionally causes right ventricular failure, hypoxemia, and hemodynamic instability.[1] Deep vein thrombosis is the most prevalent etiology.[2] However, nonthrombotic pulmonary artery (PA) embolism might mimic a disease of thrombotic origin and might not respond to thrombolytic therapy. Hepatocellular carcinoma, breast cancer, and renal cell carcinoma are the most prevalent causes of nonthrombotic pulmonary embolisms.[2] A diagnosis of nonthrombotic pulmonary embolism depends on a high index of suspicion and a comprehensive imaging study. Here, we present a case of nonthrombotic pulmonary embolism, which was successfully treated by surgical removal. The patient provided written informed consent.
2. Case report
A 45-year-old woman was referred for progressive effort dyspnea for 3 weeks. She had no family history of cardiovascular, lung, or coagulation diseases. She was not taking any medications, such as contraceptives or other hormones. Echocardiography revealed a mobile mass extending from the right atrium to the bilateral PA. Pulmonary embolism was diagnosed and thrombolytic therapy was started soon after the diagnosis. As the mass did not respond to thrombotic therapy, computed tomography (CT) was performed, and the results are shown in Figure 1A. A hypo-attenuated lesion was traced from the right ovarian vein, inferior vena cava (IVC), and right atrium (RA) and terminated in the bilateral proximal PA. A uterine myoma and bilateral ovarian cyst were also found in the CT scan. From these unique imaging features, intravenous leiomyomatosis was suspected. A 1-stage operation for the surgical removal of the tumor and subtotal hysterectomy were scheduled and performed. The RA and PA were opened after cardiac arrest by histidine-tryptophan-ketoglutarate (HTK solution; CUSTODIOL, Alsbach-Hähnlein, Germany) cardioplegic solution. A tubule-like tumor was noted in the proximal left and right PA. The tumor was not attached to any cardiac structure and could be gently pulled out from the PA and right ventricle. Finally, resistance was encountered on the IVC side. The tumor was removed forcefully at the distal end (Fig. 2).
Figure 1.
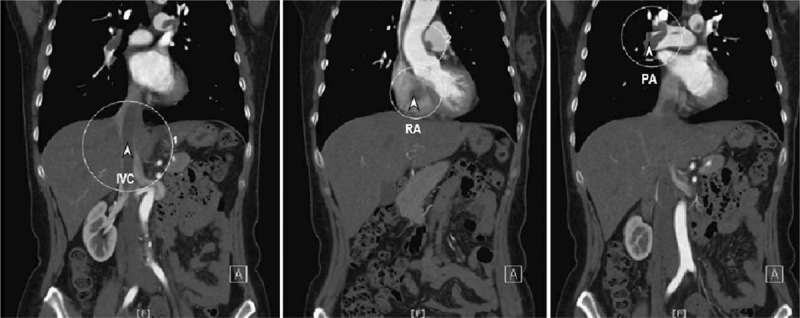
Coronal view of contrast enhanced computed tomography images. A hypo-attenuated mass extended from the IVC to the PA. Arrow head: tumor; IVC = inferior vena cava, PA = pulmonary artery, RA = right atrium.
Figure 2.

(A) Tumor had an umbilical cord-like appearance with a length of 41 cm. The tumor surface was smooth and without any attachment to other structures. (B) Cut-end of the tumor. The cut-end revealed an encapsulated fibroelastic cord with some scattered blood vessels.
Right salpingo-oophorectomy and subtotal hysterectomy were performed after closing the mediastinum. Uterine leiomyomatosis without malignant transformation was noted in the pathologic examination, as shown in Figure 3. The patient was followed up for 2 years and subsequent CT did not reveal any notable lesions.
Figure 3.
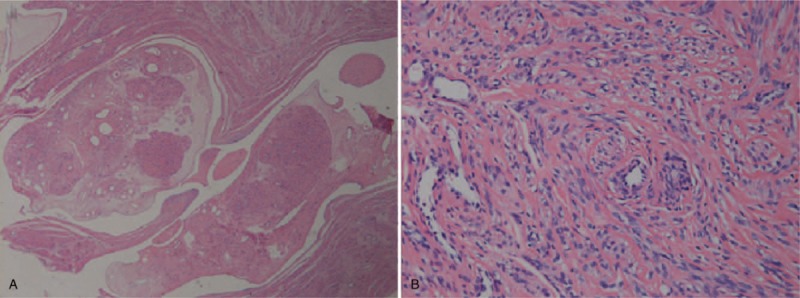
(A) Under 100× microscopic view, the tumor is a benign leiomyomatous tumor with high vascularity; it is edematous and has a hyalinized stroma. The tumor was completely same as the tumor of intravascular growth in the uterine corpus. (B) Under 400× microscopic view, no pleomorphism or increased mitosis suggesting leiomyosarcoma was seen. The microscopic examination concluded intravenous leiomyomatosis without malignant transformation.
3. Discussion
Pulmonary embolism is a potentially life-threatening complication and deep vein thrombosis is the most prevalent etiology.[2] However, embolisms such as nonthrombotic PA embolism, fat embolism, amniotic fluid embolism, tumoral embolism, and septic embolism should be considered as differential diagnoses more often, especially in cases in which thrombolytic therapy fails. Echocardiography is easily performed at the bedside and can provide images of the intracardiac mass pre- and post-thrombolytic therapy. In this case, echocardiography showed failure of thrombolytic therapy to remove the tumor. The results led to the diagnosis of nonthrombotic pulmonary embolism.
Intravenous leiomyomatosis is characterized as benign leiomyoma-like lesions with intraluminal growth in the venous vessels.[3,4] Under microscopic examination, a solid, tubular, or “sausage-like” intravascular structure with heterogeneous signal intensity can also be noted.[5] Intravenous leiomyomatosis is typically unilateral and usually involves the uterine vein or ovarian vein. There are 2 hypotheses for the origin of intravenous leiomyomatosis. The 1st is that the uterine leiomyoma invades the uterine vein and thereafter grows into the venous system. The other suggests that the smooth muscle cells of the vein abnormally proliferate into the venous system.[3,4] Patients present with symptoms related to the locations of tumor growth and sometimes without any symptoms in the early stage. Some nonspecific symptoms, such as lower leg edema, abdominal pain, or hypermenorrhea, were noted. In extreme cases, such as this case, there was right heart involvement and complaints about chest pain, breathlessness, and syncope.[6] There is no specific laboratory examination for intravenous leiomyomatosis. Diagnosis of intravenous leiomyomatosis depends on imaging studies. Echocardiography only shows a possible diagnosis of a nonthrombotic pulmonary embolism and is used to evaluate the results of therapy. Most reports suggest using T1-weighted magnetic resonance images (MRIs) and CT images with contrast medium enhancement.[5,7] The T1-weighted MRI images showed a low to intermediate signal intensity located in the ovarian vein or uterine vein. CT images with contrast medium enhancement usually show a hypoattenuating intravascular filling defect associated with uterine leiomyomas.[5,7]
Complete surgical excision of tumors, including hysterectomy, bilateral adnexectomy, and excision of the extrauterine tumor with high ligation of ovarian veins and arteries, is recommended by most reports due to the tendency for tumor recurrence. However, unilateral salpingo-oophorectomy can be performed in young women with birthing requests.[8] Studies suggest that MRI or CT scans can be conducted in consecutive years postoperatively for screening for residual tumor growth.[8,9]
In summary, we presented a case of an intravenous leiomyomatosis that extended from the ovarian vein to the PA. Intravenous leiomyomatosis should be considered in the differential diagnosis for nonthrombotic pulmonary embolism. Complete surgical excision was the only curative treatment.
Author contributions
Yi-Hsiao Wu: Drafted the manuscript and took care of the patient.
Yung-Tsai Lee: Drafted and reviewed the manuscript.
Chuin-I Lee: Helped to take care of and manage the patient.
Yun-Hsuan Tzeng: Helped to collect medical image.
Jeng Wei: Reviewed the article, performed the operation, and treated the patient.
Conceptualization: Chuin-I Lee.
Resources: Chuin-I Lee, Yun-Hsuan Tzeng.
Supervision: Jeng Wei.
Writing – original draft: Yi-Hsiao Wu.
Writing – review & editing: Yung-Tsai Lee, Jeng Wei.
Footnotes
Abbreviations: CT = computed tomography, HTK = histidine-tryptophan-ketoglutarate, IVC = inferior vena cava, PA = pulmonary artery, RA = right atrium.
The authors have no conflicts of interest to disclose.
References
- [1].Corsi F, Lebreton G, Bréchot N, et al. Life-threatening massive pulmonary embolism rescued by venoarterial-extracorporeal membrane oxygenation. Crit Care 2017;21:76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Konstantinides SV, Barco S, Lankeit M, et al. Management of pulmonary embolism: an update. J Am Coll Cardiol 2016;67:976–90. [DOI] [PubMed] [Google Scholar]
- [3].Nam MS, Jeon MJ, Kim YT, et al. Pelvic leiomyomatosis with intracaval and intracardiac extension: a case report and review of the literature. Gynecol Oncol 2003;89:175–80. [DOI] [PubMed] [Google Scholar]
- [4].Devesa VV, Conley CR, Stone WM, et al. Update on intravenous leiomyomatosis: report of five patients and literature review. Eur J Obstet Gynecol Reprod Biol 2013;171:209–13. [DOI] [PubMed] [Google Scholar]
- [5].Bender LC, Mitsumori LM, Lloyd KA, et al. AIRP best cases in radiologic-pathologic correlation: intravenous leiomyomatosis. Radiographics 2011;31:1053–8. [DOI] [PubMed] [Google Scholar]
- [6].Gaudino M, Spatuzza P, Snider F, et al. Surgical management of a uterine leiomyoma extending through the inferior vena cava into the right heart. Heart Vessels 2002;17:80–2. [DOI] [PubMed] [Google Scholar]
- [7].Fasih N, Prasad Shanbhogue AK, Macdonald DB, et al. Leiomyomas beyond the uterus: unusual locations, rare manifestations. Radiographics 2008;28:1931–48. [DOI] [PubMed] [Google Scholar]
- [8].Du J, Zhao X, Guo D, et al. Intravenous leiomyomatosis of the uterus: a clinicopathologic study of 18 cases, with emphasis on early diagnosis and appropriate treatment strategies. Hum Pathol 2011;42.9:1240–6. [DOI] [PubMed] [Google Scholar]
- [9].Clay TD, Dimitriou J, McNally OM, et al. Intravenous leiomyomatosis with intracardiac extension - a review of diagnosis and management with an illustrative case. Surg Oncol 2013;22:e44–52. [DOI] [PubMed] [Google Scholar]


