Supplemental Digital Content is available in the text
Keywords: acute myocardial infarction, bilirubin, major adverse cardiac events, meta-analysis, mortality
Abstract
Background:
Experimental data obtained in animal models supported the protective role of bilirubin. However, clinical studies regarding the prognostic role of total bilirubin in patients with acute myocardial infarction (AMI) are conflicting. We, therefore, undertook this meta-analysis to evaluate the prognostic value of serum total bilirubin in AMI patients.
Methods:
Relevant studies were searched from PubMed and EMBASE databases up to April 15, 2018. Studies evaluating the outcomes in relation to serum total bilirubin in AMI patients and reporting multivariable-adjusted risk estimate of the prognostic value were eligible. The outcome measures were major adverse cardiac events (MACEs), cardiovascular death, and all-cause mortality.
Results:
Six studies involving 14,554 AMI patients were identified. Meta-analysis indicated that higher total bilirubin was associated with an increased risk of MACEs (risk ratio [RR] 1.65; 95% confidence intervals [CI] 1.25–2.19) and cardiovascular death (RR 2.12; 95%CI 1.24–3.64). However, higher serum total bilirubin did not significantly increase all-cause mortality risk (RR 1.31; 95%CI 0.75–2.28). Subgroup analyses by the types of AMI and study design supported the pooled results.
Conclusions:
Higher serum total bilirubin level is a predictor of MACEs and cardiovascular death in patients with AMI. However, interpretation of these findings should be with caution due to the impact of cardiac dysfunction after AMI.
1. Introduction
Despite substantial improvements in reperfusion therapy, acute myocardial infarction (AMI) remains a life-threatening disease worldwide.[1,2] AMI is traditionally divided into ST-segment elevation myocardial infarction (STEMI) or non-ST elevation myocardial infarction (NSTEMI). The prognosis of patients with AMI is still poor, particularly in the STEMI cases.[3] Therefore, early prediction of morbidity and mortality is warranted to guide treatment in these patients.
Biomarkers are frequently used to predict adverse outcomes in AMI patients.[4] Bilirubin is the final product of heme catabolism in the systemic circulation. Clinically, bilirubin is routinely applied for assessment of liver function. Bilirubin is known to be an important endogenous antioxidant.[5] Lower bilirubin level was associated with increased risk of major adverse cardiac events (MACEs) in stable coronary artery disease (CAD) patients.[6,7] By contrast, serum bilirubin level increase acutely after AMI/PCI, peaking 21 h after coronary intervention.[8] AMI patients with higher total bilirubin level had a worse prognosis.[9–11] However, the use of serum total bilirubin level for predicting the MACEs and long-term mortality is conflicting.[12,13] Furthermore, the magnitude of the prognostic value of total bilirubin varied considerably across studies.
To the best of our knowledge, no previous meta-analysis has evaluated the prognostic role of serum total bilirubin among AMI patients. We, therefore, conducted a meta-analysis to evaluate the prognostic value of higher serum total bilirubin level in patients with AMI, in terms of MACEs, cardiovascular death, and all-cause mortality risk.
2. Materials and methods
2.1. Search strategy
Two authors independently searched PubMed and Embase databases from their inception to April 15, 2018. Search keywords used were as follows: “bilirubin” AND “AMI” OR “acute coronary syndrome” AND “death” OR “mortality” OR “major adverse cardiovascular events” OR “prognosis”. Language was restrained as English. Additionally, the reference lists of relevant articles were manually searched to identify any additional articles. This meta-analysis was reported according to the checklist of the Meta-Analysis of Observational Studies in Epidemiology.[14] Ethical approval was not required because the present study only used the study level data
2.2. Study selection
Studies satisfying the following inclusion criteria were included:
-
1.
full-text observational studies that evaluated the association of serum total bilirubin level with the prognosis of AMI patients;
-
2.
outcome of interests were MACEs, cardiovascular death or all-cause mortality; and
-
3.
presented multivariate-adjusted risk estimate on the association between total bilirubin and prognosis for the higher versus the lower total bilirubin level.
Studies were excluded if:
-
1.
the study population was non-AMI patients or specific type of AMI;
-
2.
conference abstract, reviews or letters; and
-
3.
multiple publications adopting the same population.
2.3. Data extraction and quality assessment
The following information was independently extracted by 2 authors: surname of the first author, publication year, geographical location, study design, study population, sample size, mean age or age range at baseline, percentage of men, proportion of diabetes or hypertension, total bilirubin cut-off level, number of outcome event, fully multivariable-adjusted hazard ratio (HR) or odds ratio (OR) with 95% confidence intervals (CI), length of follow-up, and adjustment for potential confounders. A third reviewer was consulted to resolve the differences between the 2 authors in the data abstraction. The methodological quality of the selected studies was evaluated using a nine-star Newcastle–Ottawa Scale (NOS).[15] Study quality was examined on the selection, comparability, exposure, and outcomes assessment. Overall, studies scoring 7 or above indicated good quality.
2.4. Data synthesis and analysis
Multivariate-adjusted risk estimates for the higher versus lower total bilirubin level were used for meta-analysis. HR and OR were assumed to approximate the same measure of the risk ratio (RR). Heterogeneity was assessed by the I2 statistic and Cochrane Q test. If statistically significant heterogeneity was observed (P value of Cochrane Q test <.1 or I2 statistic>50%), we chose a random effect model. Otherwise, a fixed-effect model was applied. To explore heterogeneity, subgroup analyses were performed according to the type of AMI (STEMI versus total AMI) and follow-up duration (in-hospital versus follow-up). To explore the reliability of the pooled effect sizes, sensitivity analysis was conducted by omitting individual studies at each turn. Statistical analyses were performed using STATA version 12.0 (StataCorp, TX).
3. Results
3.1. Search results and study characteristics
We identified 295 potential articles in Pubmed and Embase databases. No additional articles were identified by reviewing the reference lists. After scanning the titles and abstracts, 263 articles were removed. After reviewing the full-text articles, 26 articles were further excluded mainly due to they did not report the outcome of interest or population was not restricted to AMI patients. Finally, 6 studies[12,13,16–19] were included in the meta-analysis. The flow chart of the study selection process is presented in Figure 1.
Figure 1.
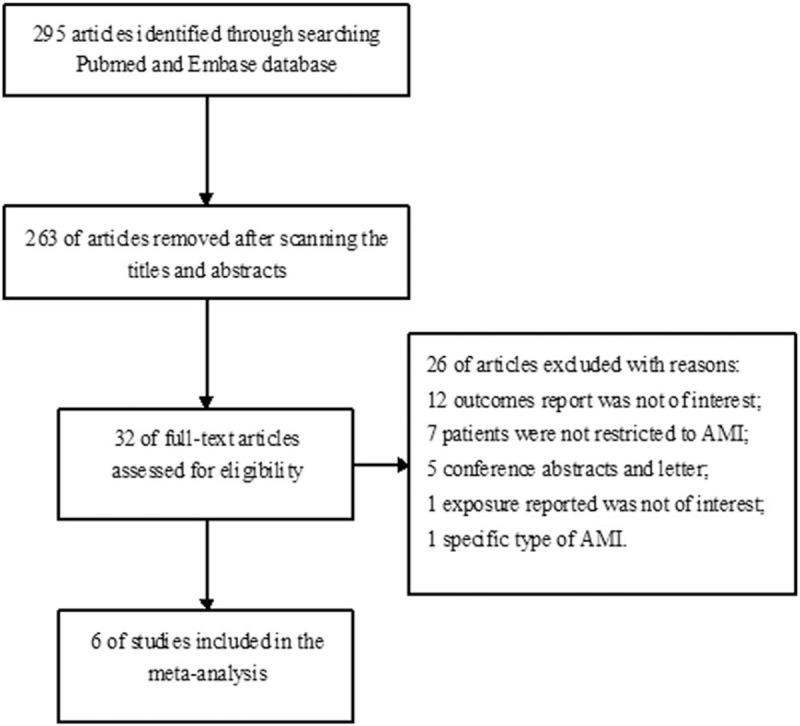
Flow chart showing the study selection process.
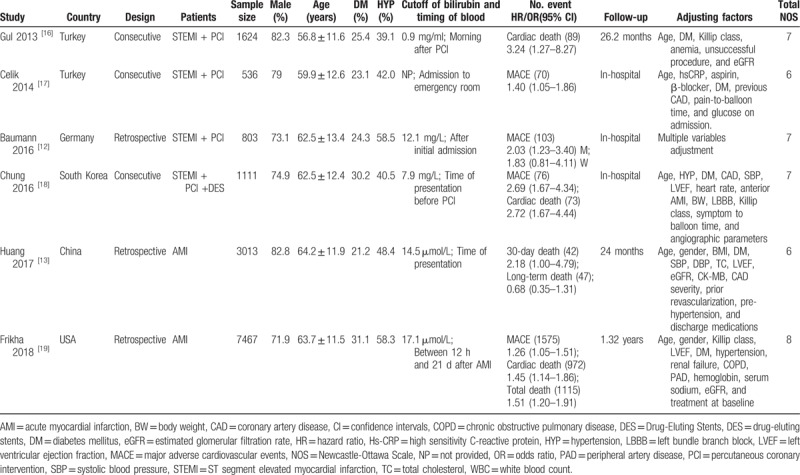
Table 1 summarizes the baseline characteristics of the included studies. These studies were conducted in Turkey,[16,17] Germany,[12] USA,[19] China,[13] and South Korea.[18] Four studies[12,16–18] enrolled STEMI patients undergoing percutaneous coronary intervention (PCI) and 2 studies included patients with STEMI and NSTEMI. Sample sizes varied from 536 to 7467, with a total of 14,554 AMI patients. The mean age of patients ranged from 56.8 to 64.2 years, and the percentage of men ranged from 71.9% to 82.3%. Mean follow-up duration was up to 26.2 months. According to the 9-star NOS scale, 4 studies achieved high-quality score of 7 (Supplemental Table S1).
Table 1.
Summary characteristics of the included studies.
3.2. Total bilirubin and MACEs
Three studies[12,17,18] reported the in-hospital MACEs as an outcome and one study[19] provided data on follow-up MACEs. As shown in Figure 2, AMI patients with higher serum total bilirubin level had an increased risk of MACEs (RR 1.65; 95% CI 1.25–2.19) in a random effect model. There was significant heterogeneity among the studies (I2 = 62.9%; P = .029). A leave-out 1 study sensitivity analysis did not substantially change the combined effect (Data not shown). Stratified analysis by follow-up duration indicated that higher serum total bilirubin significantly increased both in-hospital MACEs (RR 1.87; 95% CI 1.34–2.60) and follow-up MACEs (RR 1.26; 95% CI 1.05–1.51). Moreover, subgroup analysis by the type of myocardial infarction showed that the prognostic value of higher total bilirubin was stronger in the STEMI patients undergoing PCI (RR 1.87; 95% CI 1.34–2.60) than all type of AMI patients (RR 1.26; 95% CI 1.05–1.51).
Figure 2.
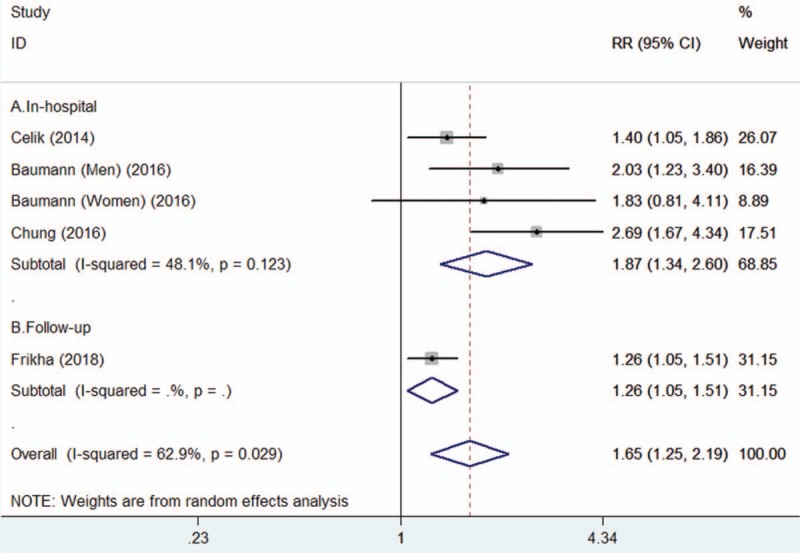
Forest plots showing risk ratio and 95% confidence interval of major adverse cardiac events for the higher versus lower serum total bilirubin level.
3.3. Total bilirubin and cardiovascular mortality
Three studies[16,18,19] reported cardiovascular mortality as an outcome. As shown in Figure 3, AMI patients with higher serum total bilirubin level was associated with an increased risk of cardiovascular mortality (RR 2.12; 95% CI 1.24–3.64) in a random effect model, with significant heterogeneity across the studies (I2 = 71.4%; P = .030). Sensitivity analysis by removing individual studies at each time did not substantially alter the pooled risk estimate (Data not shown). Stratified analysis by follow-up duration showed that the prognostic value of higher total bilirubin was stronger for in-hospital cardiovascular mortality (RR 2.82; 95% CI 1.83–4.36) than the follow-up cardiovascular mortality (RR 1.45; 95% CI 1.14–1.85).
Figure 3.
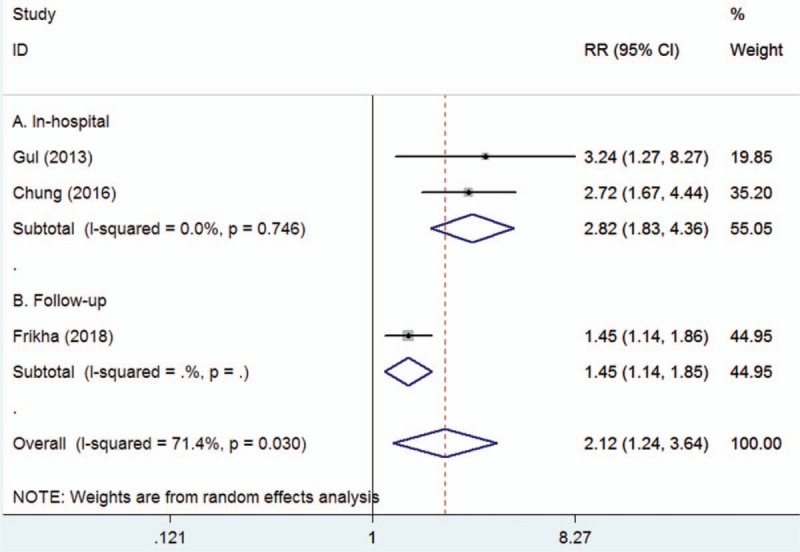
Forest plots showing risk ratio and 95% confidence interval of cardiovascular mortality for the higher versus lower serum total bilirubin level.
3.4. Total bilirubin and all-cause mortality
Two studies[18,19] reported the all-cause mortality as an outcome. As shown in Figure 4, AMI patients with higher serum total bilirubin level was not associated with an increased risk of all-cause mortality (RR 1.31; 95% CI 0.75–2.28) in a random effect model. The heterogeneity among studies was significant (I2 = 67.7%; P = .045). Stratified analysis by follow-up duration revealed that the prognostic value of total bilirubin was not significant in both 30-day and long-term all-cause mortality.
Figure 4.
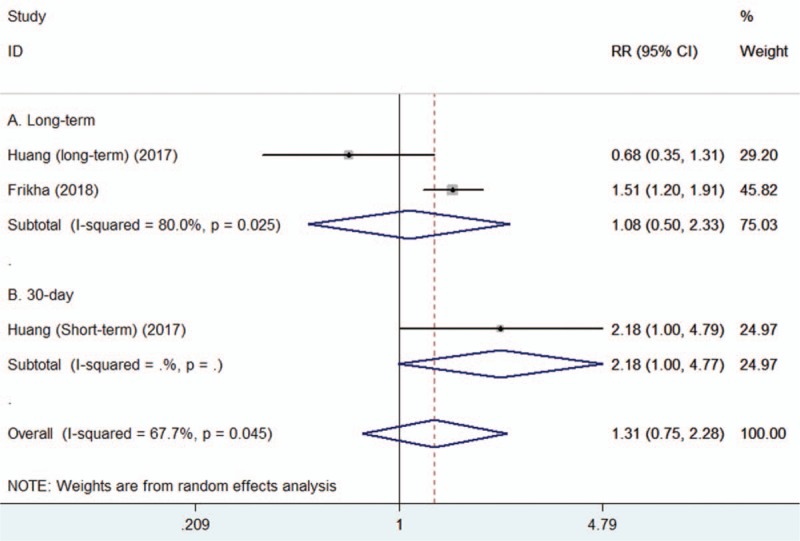
Forest plots showing risk ratio and 95% confidence interval of all-cause of mortality for the higher versus lower serum total bilirubin level.
3.5. Publication bias
The funnel plot is potentially unreliable for less than the recommended arbitrary minimum number of 10 studies included,[20] we, therefore, did not construct the funnel plot to explore publication bias.
4. Discussion
The current meta-analysis suggests that higher serum total bilirubin level is independently associated with an increased risk of MACEs and cardiovascular mortality in patients with AMI. AMI patients with higher serum total bilirubin had an approximately 65% and 2.12-fold greater risk of MACEs and cardiovascular mortality, respectively. However, higher serum total bilirubin was not associated with an increased risk of all-cause mortality risk during follow-up.
Bilirubin has anti-oxidant, anti-inflammatory, and vasodilatory functions.[21] The prognostic value of serum bilirubin is different from CAD and AMI patients. In contrast, increased risk of CAD in individuals with low serum total bilirubin level.[22] For stable CAD patients, increased serum total bilirubin was associated with a better prognosis.[6,13] Accordingly, experimental data obtained in animal models also supported the protective effects of bilirubin. Chronically increased bilirubin protected from cardiac reperfusion injury.[23] Increased cardiac bilirubin could improve postischemic myocardial function.[24] Administration of bilirubin reduced infarct area in a rat coronary ischemia/reperfusion model.[25] In light of these evidence, bilirubin plays a potential protective role in cardiovascular disease.[26] While in AMI patients, elevated total bilirubin level was correlated with high burden thrombus[9] and coronary atherosclerosis,[10] and angiographic coronary no-reflow.[17] Also, AMI patients with higher total bilirubin had a lower in stent restenosis risk than those with lower total bilirubin.[27] Myocardial heme oxygenase-1 enzyme activity was significantly increased in response to acute infarction.[8] Elevated bilirubin level could be mainly caused by stress-induced heme oxygenase enzyme activation in AMI patients. Above findings suggests that bilirubin is a protective factor during chronic elevation in relatively stable CAD patients, whereas acute elevation may be a marker of disease severity.
The exact mechanisms underlying the association between total bilirubin level and adverse outcomes in AMI patients are unclear. Bilirubin is a potent antioxidant under physiological conditions.[28] Increased bilirubin level may be a compensatory mechanism in response to oxidative stress. Impaired perfusion of liver induced by low cardiac output is another important cause of increased bilirubin level.[29] Additionally, bilirubin could exert an effect on the blood pressure and other cardiovascular risk.[30] Circulating bilirubin level may be considered as a surrogate biomarker of cardiac dysfunction and poor hepatic perfusion.
Nevertheless, high serum total bilirubin level may simply reflect the AMI severity.[31] Therefore, bilirubin effects could have confounded by poor cardiac function after AMI. Regardless of whether elevated bilirubin is a surrogate marker of AMI severity or an independent prognostic factor for the adverse prognosis, careful attention is needed for clinicians.
There are several limitations in this meta-analysis. First, total bilirubin was only determined at a single time point and could not reflect the changes during the time of the hospital stay and follow-up. Second, different cut-off values of the serum total bilirubin level were reported in the analyzed studies, and we failed to establish an optimal threshold of total bilirubin in this meta-analysis. Third, inability to perform the publication bias test due to small number of studies included in the analyses and also results of subgroup analysis may be unreliable. Fourth, there were significant between-study heterogeneity and differences in study design, clinical settings, follow-up duration, and types of AMI could contribute to the heterogeneity. Fifth, lack of reporting other medications that may have changed not only the prognosis but the level of bilirubin itself. Finally, bilirubin is likely representing a surrogate marker of MI severity, and therefore, revealing the potential protective effects is almost impossible by the retrospective analysis.
5. Conclusions
AMI patients with higher serum total bilirubin level significantly increased risk of MACEs and cardiovascular mortality but not all-cause mortality risk. However, interpretation of the current findings should be with caution because the prognostic value of bilirubin can be confounded by cardiac dysfunction after AMI.
Author contributions
Conceptualization: Hongyou Shen.
Data curation: Canhui Zeng, Xiaowei Wu.
Formal analysis: Canhui Zeng, Shizhao Liu.
Investigation: Canhui Zeng, Xiaowei Wu, Xiaomin Chen.
Methodology: Hongyou Shen, Canhui Zeng, Xiaowei Wu, Shizhao Liu.
Project administration: Hongyou Shen.
Resources: Canhui Zeng, Xiaowei Wu.
Supervision: Hongyou Shen.
Validation: Hongyou Shen.
Writing – original draft: Shizhao Liu.
Writing – review & editing: Xiaomin Chen.
Supplementary Material
Footnotes
Abbreviations: AMI = acute myocardial infarction, CAD = coronary artery disease, CI = confidence intervals, MACEs = major adverse cardiac events, NOS = Newcastle Ottawa Scale, NSTEMI = non-ST elevation myocardial infarction, RR = risk ratios, STEMI = ST-segment elevation myocardial infarction.
The authors have declared that no competing interests exist.
Supplemental Digital Content is available for this article.
References
- [1].Reed GW, Rossi JE, Cannon CP. Acute myocardial infarction. Lancet 2017;389:197–210. [DOI] [PubMed] [Google Scholar]
- [2].Rentrop KP, Feit F. Reperfusion therapy for acute myocardial infarction: concepts and controversies from inception to acceptance. Am Heart J 2015;170:971–80. [DOI] [PubMed] [Google Scholar]
- [3].Johansson S, Rosengren A, Young K, et al. Mortality and morbidity trends after the first year in survivors of acute myocardial infarction: a systematic review. BMC Cardiovasc Disord 2017;17:53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Wei S, Mao L, Liu B, et al. Serum biomarkers and the prognosis of AMI patients. Herz 2014;39:384–9. [DOI] [PubMed] [Google Scholar]
- [5].Gazzin S, Vitek L, Watchko J, et al. A novel perspective on the biology of bilirubin in health and disease. Trends Mol Med 2016;22:758–68. [DOI] [PubMed] [Google Scholar]
- [6].Yao HM, Shen DL, Zhao XY, et al. Prognostic value of total bilirubin in patients with angina pectoris undergoing percutaneous coronary intervention. Int J Clin Exp Med 2015;8:15930–9. [PMC free article] [PubMed] [Google Scholar]
- [7].Zhang MM, Gao Y, Zheng YY, et al. Association of fasting serum bilirubin levels with clinical outcomes after percutaneous coronary intervention: a prospective study. Cardiovasc Toxicol 2017;17:471–7. [DOI] [PubMed] [Google Scholar]
- [8].Okuhara K, Kisaka T, Ozono R, et al. Change in bilirubin level following acute myocardial infarction is an index for heme oxygenase activation. South Med J 2010;103:876–81. [DOI] [PubMed] [Google Scholar]
- [9].Hamur H, Duman H, Bakirci EM, et al. Bilirubin levels and thrombus burden in patients With ST-segment elevation myocardial infarction. Angiology 2016;67:565–70. [DOI] [PubMed] [Google Scholar]
- [10].Sahin O, Akpek M, Elcik D, et al. Bilirubin levels and the burden of coronary atherosclerosis in patients with STEMI. Angiology 2013;64:200–4. [DOI] [PubMed] [Google Scholar]
- [11].Acet H, Erts F, Akil MA, et al. A novel predictor of infarct-related artery patency before percutaneous intervention and in-hospital outcomes for ST-segment elevation myocardial infarction patients: serum bilirubin level. Postepy Kardiol Interwencyjnej (Adv Interven Cardiol) 2014;10:91–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Baumann S, Huseynov A, Koepp J, et al. Comparison of serum uric acid, bilirubin, and C-Reactive protein as prognostic biomarkers of in-hospital MACE between women and men with ST-segment elevation myocardial infarction. Angiology 2016;67:272–80. [DOI] [PubMed] [Google Scholar]
- [13].Huang FY, Peng Y, Huang BT, et al. The correlation between serum total bilirubin and outcomes in patients with different subtypes of coronary artery disease. Clin Chim Acta 2017;465:101–5. [DOI] [PubMed] [Google Scholar]
- [14].Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA 2000;283:2008–12. [DOI] [PubMed] [Google Scholar]
- [15].Wells G, Shea B, O’Connell D, et al. The Newcastle–Ottawa Scale (NOS) for assessing the quality if nonrandomized studies in meta-analyses. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (Accessed October 15, 2018). in press. [Google Scholar]
- [16].Gul M, Uyarel H, Ergelen M, et al. Prognostic value of total bilirubin in patients with ST-segment elevation acute myocardial infarction undergoing primary coronary intervention. Am J Cardiol 2013;111:166–71. [DOI] [PubMed] [Google Scholar]
- [17].Celik T, Kaya MG, Akpek M, et al. Does Serum Bilirubin level on admission predict TIMI flow grade and in-hospital MACE in patients with STEMI undergoing primary PCI. Angiology 2014;65:198–204. [DOI] [PubMed] [Google Scholar]
- [18].Chung SR, Yang TH, Shin HC, et al. Initial total bilirubin and clinical outcome in patients With ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention with drug-eluting stents. Circ J 2016;80:1437–44. [DOI] [PubMed] [Google Scholar]
- [19].Frikha Z, Ferreira JP, Bozec E, et al. Relation of high serum bilirubin to short-term mortality following a myocardial infarction complicated by left ventricular systolic dysfunction (from the high-risk myocardial infarction database initiative). Am J Cardiol 2018;121:1015–20. [DOI] [PubMed] [Google Scholar]
- [20].Lau J, Ioannidis JP, Terrin N, et al. The case of the misleading funnel plot. Bmj 2006;333:597–600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Gupta N, Singh T, Chaudhary R, et al. Bilirubin in coronary artery disease: Cytotoxic or protective? World J Gastrointest Pharmacol Ther 2016;7:469–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Ghem C, Sarmento-Leite RE, de Quadros AS, et al. Serum bilirubin concentration in patients with an established coronary artery disease. Int Heart J 2010;51:86–91. [DOI] [PubMed] [Google Scholar]
- [23].Bakrania B, Du Toit EF, Ashton KJ, et al. Chronically elevated bilirubin protects from cardiac reperfusion injury in the male Gunn rat. Acta Physiol (Oxf) 2017;220:461–70. [DOI] [PubMed] [Google Scholar]
- [24].Clark JE, Foresti R, Sarathchandra P, et al. Heme oxygenase-1-derived bilirubin ameliorates postischemic myocardial dysfunction. Am J Physiol Heart Circ Physiol 2000;278:H643–51. [DOI] [PubMed] [Google Scholar]
- [25].Ben-Amotz R, Bonagura J, Velayutham M, et al. Intraperitoneal bilirubin administration decreases infarct area in a rat coronary ischemia/reperfusion model. Front Physiol 2014;5:53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Bulmer AC, Bakrania BA, Du Toit EF, et al. Bilirubin acts as a multi-potent guardian of cardiovascular integrity: more than just a radical idea. Am J Physiol Heart Circ Physiol 2018;315:H429–47. [DOI] [PubMed] [Google Scholar]
- [27].Kuwano T, Miura S, Shirai K, et al. Serum levels of bilirubin as an independent predictor of coronary in-stent restenosis: a new look at an old molecule. J Atheroscler Thromb 2011;18:574–83. [DOI] [PubMed] [Google Scholar]
- [28].Stocker R, Yamamoto Y, McDonagh AF, et al. Bilirubin is an antioxidant of possible physiological importance. Science 1987;235:1043–6. [DOI] [PubMed] [Google Scholar]
- [29].Goncalvesova E, Kovacova M. Heart failure affects liver morphology and function. What are the clinical implications? Bratisl Lek Listy 2018;119:98–102. [DOI] [PubMed] [Google Scholar]
- [30].McCallum L, Panniyammakal J, Hastie CE, et al. Longitudinal blood pressure control, long-term mortality, and predictive utility of serum liver enzymes and bilirubin in hypertensive patients. Hypertension 2015;66:37–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Kaya MG, Sahin O, Akpek M, et al. Relation between serum total bilirubin levels and severity of coronary artery disease in patients with non-ST-segment elevation myocardial infarction. Angiology 2014;65:245–9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


