Abstract
Background:
Several studies have reported the benefits of traditional Chinese exercises (TCEs) on hypertension; however, a consensus regarding the effectiveness and safety of TCEs for patients with hypertension has not been reached.
Methods and results:
Only randomized controlled trials were included in our study. A total of 16 articles involving 1164 patients with hypertension met the inclusion criteria. The results showed that TCEs can reduce BP, blood lipids (including total cholesterol and triglyceride levels) and endothelin levels and improves quality of life in hypertensive patients, however, the low-quality of the included studies made the results be of questionable significance.
Conclusions:
The results of this review suggest that there is no firm evidence to support the objective effectiveness and safety of TCEs for hypertension because of the poor quality of the studies. Well-designed, randomized placebo-controlled trial with objective outcome measures should be conducted in the future.
Keywords: hypertension, randomized controlled trials, systematic review, traditional Chinese exercise
1. Introduction
Hypertension is the main cause of cardiovascular disease (CVD) and death globally: it is responsible for at least 7.6 million deaths per year world-wide (13.5% of all deaths) and the major risk factor for CVD.[1] A previous meta-analysis reported that every 10 mmHg reduction in systolic blood pressure (SBP) markedly reduces the risk of major cardiovascular events, stroke, heart failure, and all-cause mortality.[2] Although antihypertensive medication remains the key treatment for hypertension,[3] evidence has shown that isometric exercise, dynamic endurance training, dynamic resistance training, and combined training are associated with decreases in SBP and diastolic blood pressure (DBP).[4–9] In addition to regular daily activities, Hypertension Canada's 2016 Canadian Hypertension Education Program (CHEP) Guidelines recommended 30 to 60 min of medium-intensity exercise 4 to 7 times every week for hypertensive patients.[10] It has been reported that Qi was the vital life force in the body and the most basic element making up the universe and everything in the world, including our body. Alteration of Qi can lead to various diseases, such as Qi stagnation and Qi deficiency. There are several types of TCEs, such as Tai Chi, Baduanjin qigong, Wuqinxi, and YiJinjing. With a long history exceeding 2000 years, TCEs are based on concepts of qi, blood and meridians of traditional Chinese medicine and these exercises have traditionally been practiced for multiple purposes, including self-defense, self-health care, and disease cure.[11,12] Currently, TCEs are popular among middle-aged and elderly patients who are unable to perform moderate- and high-intensity activities.[13]
The different types of TCEs mentioned above are defined as low-level aerobic exercises that can improve limb range of motion, strength, and general health. Nonetheless, they also have their own characteristics. Tai Chi is a traditional Chinese martial art that combines slow, fluid, weight-bearing physical movements with deep, controlled breathing exercises and relaxation techniques, which can be divided into Chen-style and Yang-style Tai Chi. Baduanjin is characterized by coordination between upper limbs and lower limbs through soft and gentle postures. An ancient Chinese exercise, the postures of animals such as tigers, deer, bears, apes, and cranes are imitated when practicing Wuqinxi. In Yijinjing, the function of the viscera is gradually strengthened by breathing induction and static force. Previous studies have also reported benefits of TCEs for cardiovascular patients compared with control groups involving lower levels of triglycerides and improvements in the 6 min walk test and Minnesota Living with Heart Failure Questionnaire results.[14] Moreover, TCEs can also increase 6 min walking walk test, forced expiratory volume in one second (FEV1) and quality of life in patients with chronic obstructive pulmonary disease (COPD).[15] Additionally, the results of a cohort study revealed that TCEs can lower mortality rates from all causes, CVD, cancer and respiratory disease in older individuals.[16] Other studies have shown that TCEs are able to relieve depression and some chronic diseases and alleviate knee osteoarthritis.[17–19] Furthermore, an increasing number of studies have shown that Tai Chi, Baduanjin, Wuqinxi, YiJinjing, and other qigong therapies can lower BP;[20–22] however, most of those studies had small sample sizes or were not rigorously designed large-scale randomized controlled trials (RCTs). Additionally, previous meta-analyses have mainly focused on the effect of only 1 type of TCE (such as Tai Chi or Baduanjin) on hypertension, with no study to date having evaluated the general efficacy of TCEs in reducing hypertension. Therefore, the aim of this study was to summarize the available evidence regarding the ability of TCEs to decrease hypertension.
2. Methods
The study protocol, including objectives, literature search strategies, inclusion and exclusion criteria, outcome measurements, and methods of statistical analyses, was designed in accordance with the PRISMA statement.[23]
2.1. Ethics statement
As all analyses were based on previously published studies, no ethical approval or patient consent was required.
2.2. Literature search strategy
A systematic literature search of the PubMed (1950–March 2018), Embase (1974 to March 2018), Cochrane Library (March 2018 Issue 3), Chinese Biomedical Literature (CBM) (1990 to March 2018), China National Knowledge Infrastructure (CNKI) (1979 to March 2018), Chinese Scientific Journals (VIP) (1989 to March 2018) and Wanfang (1982 to March 2018) databases was conducted. The following MeSH terms or Emtree terms and their combinations were searched in [Title/Abstract]: “TaiChi”, “Tai Ji”, “Tai Chi exercise”, “Taichi Qigong ”, “Ba Duanjin”, “BaDuanJin Qigong”, “Qigong”, “Yi Jinjing”, “Wuqinxi”, “traditional Chinese exercise”, “traditional fitness exercise”, “traditional exercise therapy”, “hypertension”, “high blood pressure”.
2.3. Inclusion criteria and exclusion criteria
To be eligible for inclusion, the original study needed to fulfill the following criteria:
-
1.
an RCT reporting the use of TCEs for the treatment of hypertension;
-
2.
a definition of hypertension that is consistent with past guidelines (SBP ≥140 mmHg or DBP ≥90 mmHg) and subjects older than or equal to 18 and younger than 80 years old;
-
3.
reporting baseline and follow-up mean and SD (or standard error) or the mean change and SD (or standard error) values of resting diastolic BP and systolic BP in TCE and control groups.
The exclusion criteria were as follows:
-
1.
letters to the Editor, historic reviews, commentaries, and case-reports;
-
2.
subjects with hypertension who had other serious CVDs, hepatic failure or renal failure.
2.4. Data extraction and quality assessment
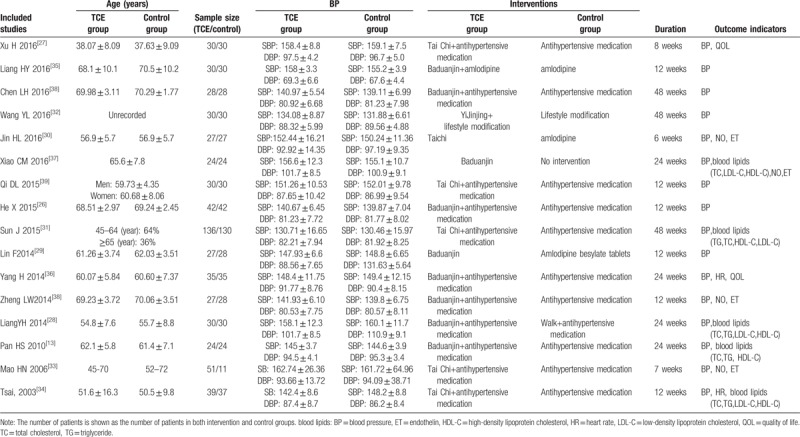
Relevant studies were identified based on the above inclusion criteria and exclusion criteria. The following data were independently extracted from the included studies by 2 investigators (JKP and XJ): authors, name, publication year, sample size, age of subjects, details of intervention, duration, and BP levels before intervention, and main outcomes. All these details were extracted and entered into the data extraction form. Mean changes in outcome measurements compared with baseline levels were used to assess differences between the intervention and control groups. Pooled effect sizes and 95% CIs (confidence intervals) were calculated using the Cochrane Collaboration software RevMan 5.3. The methodological quality of the literature included in the present study was evaluated according to the Jadad quality scale[24] and Cochrane Reviewers’ Handbook 5.1.[25] Any study that did not meet these criteria was excluded. Two reviewers (XJ and DPX) independently assessed all identified articles, and disagreements were resolved by discussion (Table 1).
Table 1.
Characteristics of the included studies.
2.5. Statistical analysis
RevMan 5.3 software was used to conduct statistical analyses in this meta-analysis, and the chi-square test and I2 statistic were employed to analyze heterogeneity. Studies with an I2 statistic of 25% to 50% were considered to have low heterogeneity, those with an I2 statistic ranging from 50% to 75% were defined as having moderate heterogeneity, and those with an I2 >75% were considered to have high heterogeneity. When the homogeneity of the included studies was sufficient (P ≥ .10, I2 ≤ 50%), the fixed-effects model was utilized for the analysis; Otherwise, the random-effects model was selected. As all scales or subscales in the studies were consistent and all studies had the same continuous outcome variables and measurement units, mean differences (MDs) and 95% CIs were used for analysis. Publication bias was determined by a funnel map or Egger test according to the number of included studies. Subgroup analysis was performed based on factors that may lead to heterogeneity (at different points in the evaluation of the outcome of the trial). The test standard of meta-analysis was set as alpha =0.05.
3. Results
3.1. Literature search results
Our initial search identified 3020 articles. After removing duplicates and studies that did not meet the inclusion criteria, 16 studies were included. The search process was depicted in Figure 1.
Figure 1.
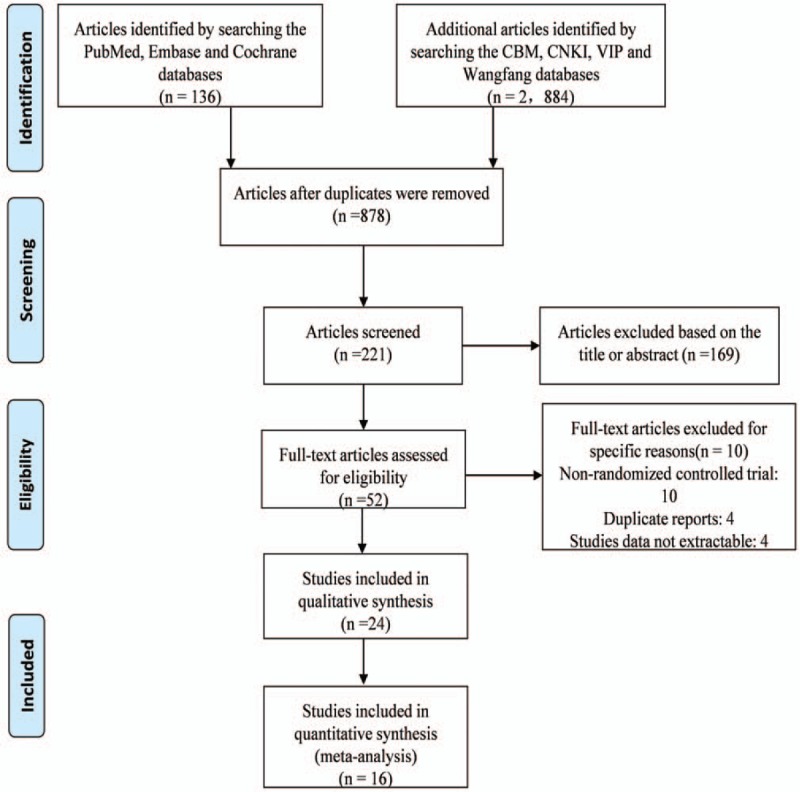
Flow chart of the study selection procedure.
3.2. Study characteristics
First, among the included 16 studies, most of the studies did not describe the details of how the random sequences generated, 4 studies[26–29] wrote that they used a random number table, and however, there existed no details of the process at all. Only 1[30] study described the procedure of the randomized process. Second, none of the studies described whether the subjects and executors were blind, for the reason that TCEs are different kinds of exercise instead of medication, when the patients do exercises, they knew what exercise they do during the process of the study, and it can be very hard to design a double-blind controlled trial. Of the included studies, there was only 1 study[31] described that the chief investigators were blind to the allocation of the participants during the process, the others even did not mention allocation concealment, we can conclude that in most of the included studies, there existed high risks of the studies. Third, only 4 studies mentioned the missing data [13,31–33]: 2 studies reported a high dropout rate and provided detailed explanations but did not perform specific statistical analysis[31–33]; and the other 2 reported that there was no dropout during the process.[13,33] Consequently, as for the attribution bias, we cannot evaluate exactly because of incomplete data. Besides, only 1[31] study had reported that they had registration number, while the rest of the included studies had not been registered on Clinical Trials, the intention-to-treat analysis was not used during the process, as for the selective reporting, it was also difficult to assess because we were not able to obtain access to the trial protocols.
According to the above information, the authors considered that all of the included studies were of low quality and had a high risk of bias. Because the poor quality of the studies, there is no need to access the included studies and perform the Cochrane based risk of bias table. The judgments for each included studies were demonstrated in Figure 2.
Figure 2.
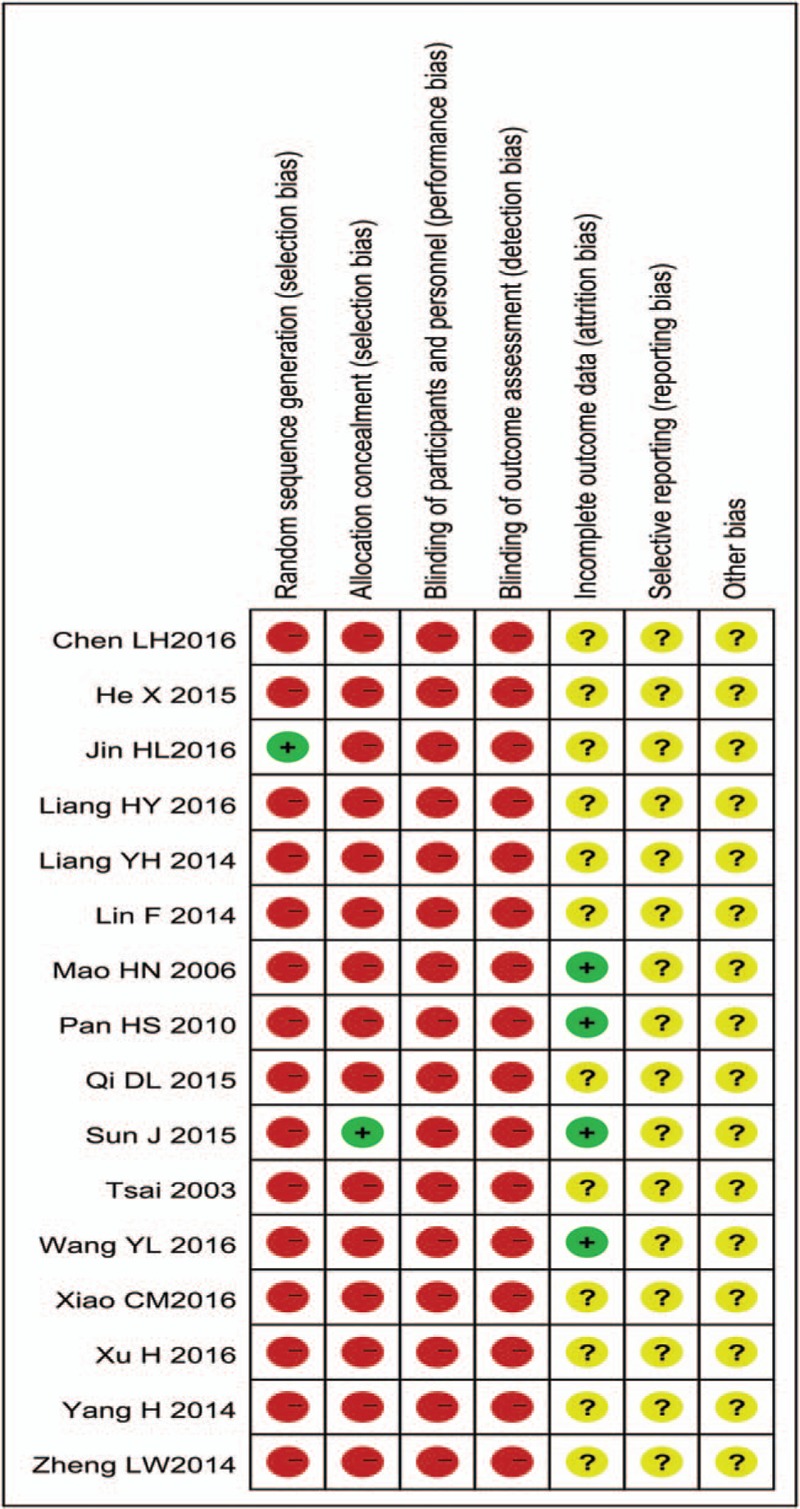
Risk of bias graph.
3.3. Outcomes
3.3.1. Blood pressure (SBP and DBP)
3.3.1.1. TCE combined with medication vs medication
Considering that antihypertensive medication is an important factor for controlling BP, we divided the subjects into a TCE combined with antihypertensive medication group and an antihypertensive medication group. Fourteen[13,26–28,30–39] studies including 1055 subjects utilized an intervention of TCE combined with antihypertensive medication and reported the mean and standard deviation of SBP and DBP before and after the intervention in patients with hypertension. The results indicated lowered SBP, by 13.19 mmHg (95% CI: −16.30 to −10.08, P < .0001; I2 = 100%, P < .0001), and DBP, by 5.47 mmHg (95% CI: −7.76 to −3.18, P < .0001; I2 = 100%, P < .0001), in the TCE combined with antihypertensive medication group compared to the antihypertensive medication group (Figs. 3 and 4).
Figure 3.
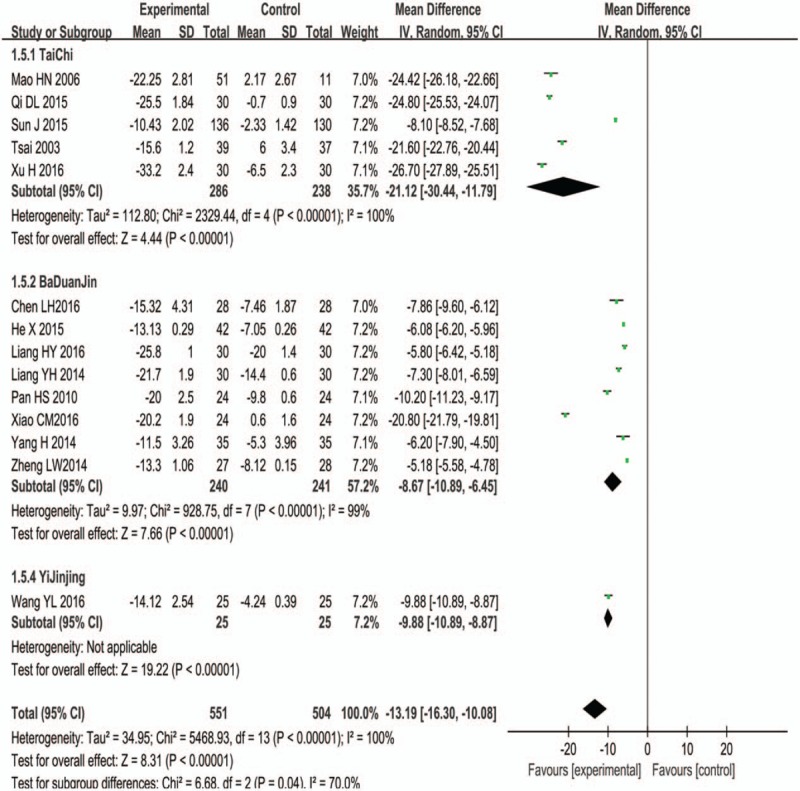
Forest plot and meta-analysis of systolic blood pressure.
Figure 4.
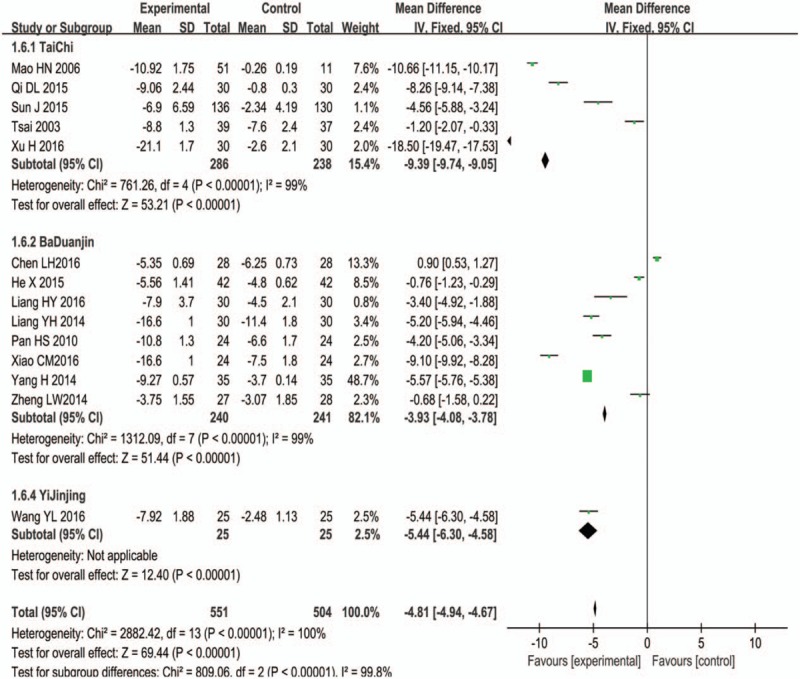
Forest plot and meta-analysis of diastolic blood pressure.
3.3.1.2. TCE vs medication
Two studies[29,30] evaluated TCEs compared with antihypertensive medication, the results showed that TCEs had a better effect on DBP compared with medication (DBP: 2.76 (95%CI: 1.08 to 4.43, P < .001)); While we could not get the same conclusion on SBP (SBP: −1.66 (95% CI: −8.78 to 5.46, P = .65).
3.3.1.3. Blood lipids
Total cholesterol (TC) and triglyceride (TG) levels
Five trials[13,28,31,34,37] reported the levels of TC and TG between TCEs combined with medication group and medication group; because the I2 statistic was greater than 75%, the random-effects model was used for the meta-analysis. The results showed a greater reduction in TC and TG levels in the TCE group than in the control group, and the difference was statistically significant (TC: MD = −0.80 mmol/l, 95% CI: −1.06 to 0.54; P < .00001; TG: MD = −0.57 mmol/l, 95% CI: −0.75 to −0.39; P = .005) (Fig. 5).
Figure 5.
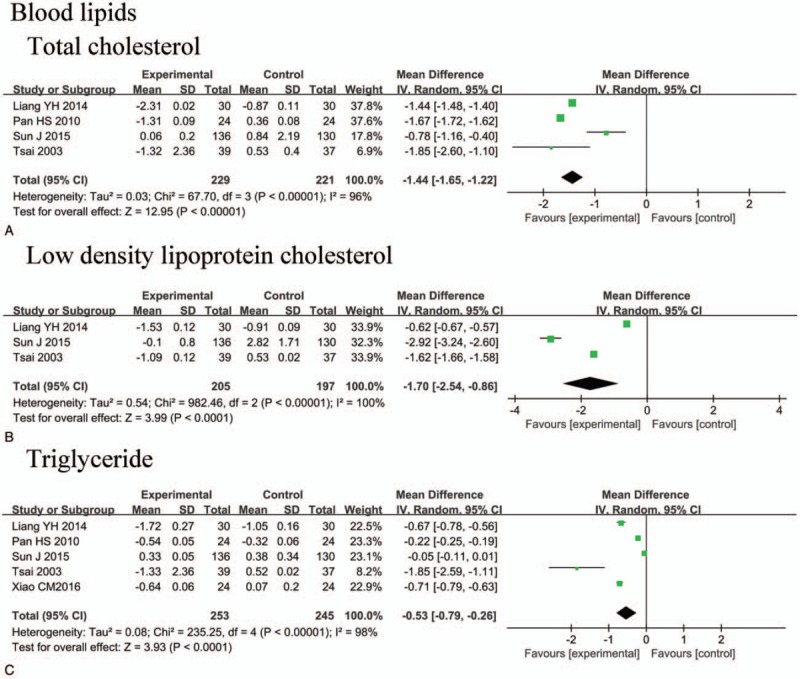
Forest plot and meta-analysis of blood lipids.
3.3.1.4. Low-density lipoprotein cholesterol (LDL-C)
Three trials[28,31,34] including 570 subjects reported the level of LDL-C between the TCE group and control group. Because the I2 static was more than 75%, the random-effects model was employed. Compared with the control group, TCEs significantly decreased the level of LDL-C, by 1.70 mmol/l (95% CI: −2.54 to 0.86, P < .0001) (Fig. 5).
3.3.1.5. Heart rate (HR)
Two trials[34,36] including 146 subjects reported the mean and standard deviation of HR before and after TCE intervention in patients with hypertension. However, no significant difference was observed between the 2 groups based on the random-effects model (MD = −8.27 beat/min, 95% CI: −23.68, 7.15, P = .29).
3.3.1.6. Nitric oxide (NO)
Three trials[30,33,38] involving 213 subjects compared the level of NO between the TCE group and control group. Because I2 was more than 75%, a random-effects model was used. However, no significant difference was identified between the groups (NO: MD = 8.56 pg/ml, 95% CI: −1.45 to 18.56, P = .09)
3.3.1.7. Endothelin (ET)
The level of ET between the TCE and control groups was reported in 4 articles[30,33,37,38] involving 213 subjects. I2 was greater than 75%; thus, the random-effects model was applied. ET levels in patients performing TCEs were significantly decreased compared to those in control patients (ET: MD = −7.72, 95% CI: −8.72 to −5.81, P < .00001).
3.3.1.8. Quality of life
Two studies including 130 subjects estimated the effect of TCEs on quality of life using the SF-36 survey. Compared with patients in the control group, those in the TCE group exhibited improved SF-36 physical function (MD = 6.93, 95% CI: 4.41 to 9.45, P < .0001), SF-36 general health (MD = 7.06, 95% CI: 1.05 to 13.08, P = .02) and SF-36 role-physical (MD = 15.16, 95% CI: 1.74 to 28.59, P = .03). However, no significant difference was observed between the 2 groups in terms of the SF-36 mental health results (MD = 8.54, 95% CI: −2.80 to 19.88, P = .14).
3.3.1.9. Publication bias
Egger regression test results showed an asymmetric distribution, suggesting publication bias, for SBP (asymmetry test P = .001), DBP (asymmetry test P = .003), TC (asymmetry test P = .018), TG (asymmetry test P = .001), and LDL-C (asymmetry test P = .001). Many factors contribute to publication bias, and most of the included studies had a small sample size, and true heterogeneity existed.
4. Discussion
4.1. Summary of findings
In this review, all the studies reported that TCMs had a positive effect on hypertension, TC, LDL-C, and TG, Besides, according to the included studies, the quality of life (such as SF-36 physical function, SF-36 general health, and SF-36 role-physical) of the subjects can also be improved by TCEs. However, because all the included studies were poor-designed, and were of bad quality, consequently, whether the results can be treated as the evidence to control hypertension is still doubtful.
In fact, TCEs has been popularly applied in many chronic diseases as complementary therapies. Until now, no well-designed, randomized placebo-controlled trial with objective outcome measures has been conducted, thus, it is a necessity to conduct high-quality studies in the future. Previous studies had highlighted the important role of exercise training in treating hypertension.[6,40] For example, a systematic review reported that regular physical activity was beneficial for reducing mortality in patients with high BP.[9] The Eighth Joint National Committee (JNC8) Report had recommended physical activity as a lifestyle modification for lowering BP.[41] Besides, it had also been proved that exercise can effectively improve lipid metabolism,[8,19] and a systematic review also showed that Baduanjin exercise was effective in modulating metabolism of lipids. Completely different from common exercises such as running and swimming, TCEs such as Tai Chi, Baduanjin, YiJinjing and Wuqinxi are all ancient martial arts that are practised for health care; the postures of TCEs act via soothing and gentle movements instead of vigorous exercise,[42] consequently, TCEs are especially suitable for such patients with poor health condition.
Though positive results had been described in the meta-analysis, however, they were still of questionable significance because of the low quality of studies. Besides, as for the safety and interactions, one of the available articles reported some safety aspects,[29] the other one study[13] had reported that no cardiovascular and cerebrovascular accident happened, while the rest of the included studies did not mention whether they monitored for adverse effects. Thus, the safety of TECs treatment is still needed to be further discussed. Due to inadequate reporting data, conclusions cannot be made about the safety of TCEs. Most of the trials were of very low methodological quality and the interpretation of any positive results for the efficacy and safety should be made with caution.
Based on this systematic review, there is no firm evidence to support the objective effectiveness and safety of TCEs for hypertension because of the poor quality of the studies. No well-designed, randomized placebo-controlled trial with objective outcome measures had been conducted. However, we can also get inspirations from the included studies and cannot completely deny the efficacy of TCEs for hypertension.
5. Conclusions
This review suggests that TCEs can not only decrease BP and blood lipids in patients with hypertension but also can improve their quality of life, which is especially suitable for elderly and frail patients. However, there is no firm evidence to support the objective effectiveness and safety of TCEs for hypertension because of the poor quality of the studies. But we can also get inspirations from the included studies, we cannot completely deny the efficacy of TCEs for hypertension, consequently, larger sample multi-center RCTs with higher methodological quality are still needed.
Author contributions
Conceptualization: Biqi Pan.
Data curation: Biqi Pan.
Formal analysis: Xiao Jin.
Resources: Huanlin Wu.
Software: Huanlin Wu.
Validation: Danping Xu.
Visualization: Danping Xu.
Xiao Jin orcid: 0000-0002-4676-1062.
Footnotes
Abbreviations: CHEP = Canadian Hypertension Education Program, COPD = chronic obstructive pulmonary disease, CVD = cardiovascular disease, DBP = diastolic blood pressure, FEV1 = forced expiratory volume in one second, HR = heart rate, JNC8 = Eighth Joint National Committee, LDL-C = Low-density lipoprotein cholesterol, NO = nitric oxide, RCT = randomized controlled trial, SBP = systolic blood pressure, TC = total cholesterol, TCEs = traditional Chinese exercises, TG = triglyceride.
This project was funded by Guangzhou Science and Technology Plan project (No. 201710010107), Guangdong Provincial Science and Technology Plan (No. 2016A020226011), Joint Innovation Specific Project in Key Areas from Guangdong Branch Institute of China Academy of Chinese Medical Sciences (No. ZZ0908065).
XJ and BP contributed equally to this work.
The authors declared no competing interests.
References
- [1].Chow CK. Prevalence, awareness, treatment, and control of hypertension in rural and urban communities in high-, middle-, and low-income countries. JAMA 2013;310:959–68. [DOI] [PubMed] [Google Scholar]
- [2].Ettehad D, Emdin CA, Kiran A, et al. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet 2016;387:957–67. [DOI] [PubMed] [Google Scholar]
- [3].Paul A, James M, Suzanne Oparil M, et al. 2014 evidence-based guideline for the management of high blood pressure in adultsreport from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA 2014;5:507–20. [DOI] [PubMed] [Google Scholar]
- [4].Cornelissen VA, Smart NA. Exercise training for blood pressure: a systematic review and meta-analysis. J Am Heart Assoc 2012;2:e004473–14473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Carlson DJ, Dieberg G, Hess NC, et al. Isometric exercise training for blood pressure management: a systematic review and meta-analysis. Mayo Clinic Proc 2014;89:327–34. [DOI] [PubMed] [Google Scholar]
- [6].George A, Kelley D, Kristi A. Kelley, MEd1, and Zung Vu Tran, PhD2 Aerobic Exercise and Resting Blood Pressure: A Meta-Analytic Review of Randomized, Controlled Trials. J Gerontol A Biol Sci Med Sci. 2001; 56: M298–M303. [DOI] [PubMed] [Google Scholar]
- [7].Cornelissen V, H Fagard R. Effect of resistance training on resting blood pressure: a meta-analysis of randomized controlled trials. J Hypertens 2005;23:251–9. [DOI] [PubMed] [Google Scholar]
- [8].Cornelissen VA, Fagard RH, Coeckelberghs E, et al. Impact of resistance training on blood pressure and other cardiovascular risk factors: a meta-analysis of randomized, controlled trials. Hypertension 2011;58:950–8. [DOI] [PubMed] [Google Scholar]
- [9].Rossi A, Dikareva A, Bacon S, et al. The impact of physical activity on mortality in patients with high blood pressure: a systematic review. J Hypertens 2012;30:1277–88. [DOI] [PubMed] [Google Scholar]
- [10].Alexander A, Leung MM, Kara Nerenberg MM. Hypertension Canada's 2016 CHEP guidelines for blood pressure measurement, diagnosis, assessment of risk, prevention and treatment of hypertension. Can J Cardiol 2016;5:589–97. [Google Scholar]
- [11].Jiang Y, Zou J. Analysis of the TCM theory of traditional Chinese health exercise. J Sport Health Sci 2013;2:204–8. [Google Scholar]
- [12].Guo Y, Qiu P, Liu T. Tai Ji Quan: an overview of its history, health benefits, and cultural value. J Sport Health Sci 2014;3:3–8. [Google Scholar]
- [13].Pan HS, Feng Y. Clinical observation of Baduanjin exercise on rehabilitation treatment of elderly patients with grade 1 hypertension. J Nanjing Inst Phys Edu 2010;9:4–6. [Google Scholar]
- [14].Wang XQ, Pi YL, Chen PJ, et al. Traditional Chinese exercise for cardiovascular diseases: systematic review and meta-analysis of randomized controlled trials. J Am Heart Assoc 2016;5:e002562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Luo X, Zhang J, Castelberg R, et al. The effects of traditional Chinese exercise in patients with chronic obstructive pulmonary disease: a meta-analysis. PLoS One 2016;11:e0161564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Shen C, Lee SY, Lam TH, et al. Is traditional Chinese exercise associated with lower mortality rates in older people? Evidence from a prospective Chinese elderly cohort study in Hong Kong. Am J Epidemiol 2015;183:36–45. [DOI] [PubMed] [Google Scholar]
- [17].Zhang Y, Huang L, Su Y, et al. The effects of traditional Chinese exercise in treating knee osteoarthritis: a systematic review and meta-analysis. PLoS One 2017;12:e0170237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Wang X, Pi Y, Chen B, et al. Effect of traditional Chinese exercise on the quality of life and depression for chronic diseases: a meta-analysis of randomised trials. Sci Rep 2015;5:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Mei L, Chen Q, Ge L, et al. Systematic review of Chinese traditional exercise baduanjin modulating the blood lipid metabolism. Evid Based Complement Alternat Med 2012;2012:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Yeh GY, Wang C, Wayne PM, et al. The effect of tai chi exercise on blood pressure: a systematic review. Prev Cardiol 2008;11:82–9. [DOI] [PubMed] [Google Scholar]
- [21].Xiong X, Wang P, Li X, et al. Qigong for Hypertension. Medicine 2015;94:e352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Xiong X, Wang P, Li S, et al. Effect of Baduanjin exercise for hypertension: a systematic review and meta-analysis of randomized controlled trials. Maturitas 2015;80:370–8. [DOI] [PubMed] [Google Scholar]
- [23].Knobloch KYU, Vogt PM. Preferred reporting items for systematic reviews and meta-analyses (PRISMA) statement and publication bias. J Craniomaxillofac Surg 2011;39:91–2. [DOI] [PubMed] [Google Scholar]
- [24].Jørgensen L, Paludan-Müller AS, Laursen DRT, et al. Evaluation of the Cochrane tool for assessing risk of bias in randomized clinical trials: overview of published comments and analysis of user practice in Cochrane and non-Cochrane reviews. Syst Rev 2016;5: [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Higgins J, Green S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. The Cochrane Collaboration. www.cochrane-handbook.org; 2011. [Google Scholar]
- [26].Xu H. Effect of 24-style simplified Taijiquan on blood pressure and quality of life in patients with hypertension. Hubei J Tradit Chin Med 2016;38:38–9. [Google Scholar]
- [27].He X. Rehabilitation effect of BaDuanJin on elderly patients with hypertension. Chin J Cardiovasc Rehab Med 2015;24:252–4. [Google Scholar]
- [28].Liang YH, Niao SQ, Han CL. Effect of Baduanjin exercise intervention on blood pressure and blood lipid in patients with essential hypertension. Henan Tradit Chin Med 2014;7:2380–1. [Google Scholar]
- [29].Lin F, He QX. Observation of curative effects of BaDuanJin on elderly patients with grade 1 hypertension. Chin J Geriatr Care 2014;12:25–6. [Google Scholar]
- [30].Jin HL, Pang J. Effects of Taijiquan on 24-hour dynamic blood pressure and vascular function in patients with primary mild hypertension. Chin J Sports Med 2016;35:224–7. [Google Scholar]
- [31].Sun J, Buys N. Community-based mind-body meditative Tai Chi program and its effects on improvement of blood pressure, weight, renal. Am J Cardiol 2015;10:1–6. [DOI] [PubMed] [Google Scholar]
- [32].Wang YL. Research of Hypertension Intervention Effect Through Shaolin Yijinjing, Henan University; 2016. (PhD thesis). [Google Scholar]
- [33].Mao HN, Sha P. Effect of Tai Chi exercise on blood pressure, plasma nitrogen monoxidum and endothelin in hypertensive patients. Chin J Clin Rehab 2006;10:65–7. [Google Scholar]
- [34].Tsai J-C, Tomlinson B, Yang H-Y, et al. The beneficial effects of Tai Chi Chuan on blood pressure and lipid profile and anxiety status in a randomized controlled. J Altern Complement Med 2003;9:747–54. [DOI] [PubMed] [Google Scholar]
- [35].Liang HY, Huang CY, Li DH. Effect of BaDuanJin on blood pressure and quality of life in patients with isolated systolic hypertension. Massage Rehab Med 2016;7:12–5. [Google Scholar]
- [36].Hebei United University, Yang H. Effect of Baduanjin on Cardiovascular Autonomic Nerve Regulation and on the Quality of Life in Patients with Hypertension. 2014;(PhD thesis). [Google Scholar]
- [37].Xiao C, Yang Y, Zhuang Y. Effect of health qigong ba duan jin on blood pressure of individuals with essential hypertension. J Am Geriatr Soc 2016;64:211–3. [DOI] [PubMed] [Google Scholar]
- [38].Zheng LW, Chen QY, Chen F. The influence of Baduanjin exercise on vascular endothelium function in old patients with hypertension grade 1. Chin J Rehab Med 2014;29:223–7. [Google Scholar]
- [39].Qi DL, Li YM. Influence of taijiquan on eight patients with hypertension blood pressure levels. Sichuan Sports Sci 2015;24–6. [Google Scholar]
- [40].James M, Hagberg JPAM. The role of exercise training in the treatment of hypertension: an update. Sports Med 2000;30:193–206. [DOI] [PubMed] [Google Scholar]
- [41].James PAOS, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA 2014;311:507–20. [DOI] [PubMed] [Google Scholar]
- [42].Siu-Man Ng, Chong-Wen Wang, Rainbow Tin-Hung, et al. Tai chi exercise for patients with heart disease: a systematic review of controlled clinical trials. Altern Ther Health Med 2012;18:16–22. [PubMed] [Google Scholar]


