Abstract
Objective:
To compare self-reported maternal marijuana use to quantitative biological sampling for a marijuana metabolite, 11-nor-delta-9-tetrahydrocannabinol-9-carboxylic acid (THC-COOH), in umbilical cord homogenate in a state with legalized marijuana.
Methods:
Cross-sectional study of women approached at time of admission for delivery with live, singleton pregnancies ≥ 24 weeks at two urban medical centers in Colorado. Maternal marijuana use was estimated by (1) report to health care provider on admission history and physical, (2) survey of self-reported use, and (3) liquid chromatography tandem mass spectrometry analysis of umbilical cord homogenate for THC-COOH. Women were categorized by survey-reported last use (≤30 days ago, 30 days to 1 year, more than 1 year, never), and proportion of women with cord results above the limit of detection and limit of quantification for THC-COOH was reported for each group. Comparisons between groups were made using contingency tables. Correlation between survey-reported frequency of use and quantitative THC-COOH cord homogenate results was evaluated.
Results:
We included 116 women with self-report surveys linked to cord assay results. Six percent (95% CI 2.5–12.0%) of participants reported use in the last 30 days on survey and 2.6% (95% CI 0.5–7.4%) of participants reported marijuana use to health care providers. On umbilical cord assay, 22.4% (95% CI 15.2–31.1%) had detectable THC-COOH. The proportion of women with detectable THC-COOH increased with more recent self-reported use. Survey-reported frequency of use in the past 30 days had moderate correlation with quantified umbilical cord THC-COOH (correlation coefficient 0.44, 95% CI 0.28–0.58, p<0.001).
Conclusions:
Umbilical cord sampling results in higher estimates of prenatal marijuana use than self-report even in the setting of legalization. Umbilical cord assays for THC-COOH demonstrate promise for quantifying use. Future studies should examine how the use of biological sampling informs the association between marijuana use and perinatal outcomes.
Précis:
Umbilical cord sampling for marijuana metabolites detected prenatal marijuana use at a higher rate than self-reported estimates even in a state with legalized marijuana.
Introduction
Marijuana use in pregnancy has been associated with adverse perinatal outcomes such as fetal growth restriction, small for gestational age, preterm birth, neonatal intensive care unit admission, and adverse neurodevelopmental outcomes.1,2 Yet, prevalence of past month marijuana use among pregnant women has increased from 2.37% in 2002 to 3.85% in 2014 based on data from the National Survey on Drug Use and Health.3 In addition, self-report likely underestimates use. In a Kaiser Permanente Northern California study, prevalence of first trimester marijuana use as detected by self-report or urine toxicology was 7.1% in 2016, and exceeded 20% in high risk groups.4 Rates may be even higher in states with legalization.
Accurate ascertainment of marijuana use is important both for estimation of prevalence of use and for outcomes-based research. Ideally biological sampling could detect use over time. While urine testing only detects use over the past 2–3 days, umbilical cord homogenate testing detects marijuana use from the second trimester onward, and may be useful for quantification of use in late pregnancy.5 Cord homogenate testing for the most stable marijuana metabolite,11-nor-delta-9-tetrahydrocannabinol-9-carboxylic acid (THC-COOH), is being used widely clinically as it has a similar performance to meconium testing.
Our primary objective was to compare the prevalence of self-reported maternal marijuana use to the prevalence of use ascertained by biological sampling of the umbilical cord in a state with legalized marijuana. Our secondary objective was to evaluate if reported frequency of use in the month prior to delivery correlated with the amount of THC-COOH detected in the cord.
Methods
This was a cross-sectional multi-site study of women admitted for delivery at two urban medical centers in Colorado, a state with legalized marijuana for both medicinal and recreational use. All women with a viable singleton gestation ≥ 24 weeks of gestation who delivered on 12 consecutive weekdays in November 2016 at either University of Colorado Hospital or Denver Health Hospital were eligible for inclusion. University of Colorado Hospital is an academic tertiary referral center in Aurora, Colorado serving a predominantly Caucasian population. Denver Health Hospital is a safety net hospital for the city and county of Denver serving a predominantly low-income, Hispanic population.
During the delivery admission, maternal marijuana use was estimated by (1) a survey detailing frequency and recency of marijuana use in pregnancy, (2) report to a healthcare provider at time of admission, and (3) assay of the umbilical cord for THC-COOH, which is the most stable marijuana metabolite. Both new admissions and women who were moved from the antepartum service for delivery were considered eligible. Women were excluded if they were currently incarcerated, spoke a language other than English or Spanish, delivered prior to 24 weeks, had a multiple gestation, or a stillbirth. If women spent less than two hours on labor and delivery from admission to delivery, we considered this insufficient time to allow study staff to approach for enrollment and those women were not included in the analysis.
Study staff approached eligible women for participation in a survey about prenatal marijuana use. Approach was completed prior to delivery. Participants were informed that the care team would not have access to the survey responses. They were instructed to complete the survey and return it to the study staff in a sealed envelope with only a study identification number. The same study identification number was used to enter self-report data regarding prenatal marijuana use (past or current) from report to the health care provider as documented in the history and physical at the time of admission, and to label a sterile specimen cup which was provided to the Labor and Delivery nurse for collection of a cord segment at the time of delivery.
This study was approved by the Colorado Multiple Institutional Review Board (COMIRB #16–0175). Waiver of consent was granted for collection of umbilical cord segments from all women who delivered over the study time period. Cord segments are routinely collected at both hospitals and would typically be discarded after clinical collection of umbilical cord gases; consent was not required for collection of these otherwise discarded specimens. Waiver of consent was reviewed and approved for the collection of otherwise discarded umbilical cord on all deliveries over the period of the study because the research involves no more than minimal risk to the subjects; the waiver or alteration will not adversely affect the rights and welfare of the subjects; the research could not practicably be carried out without the waiver or alteration; and the study was not subject to FDA regulations.
Over the same time period, all women were approached for participation in the survey portion of this study. Women were given written IRB-approved instructions explaining that completion of the survey constituted consent for participation in that portion of the study. The consent for the survey did not specifically address anonymous coded correlation between the survey and testing of the umbilical cord segment. This minor deception was determined to be minimal risk, essential to the research question, and therefore appropriate. In addition, the IRB required that the survey and results of the cord testing be coded with an anonymous study identification number, and that assays be performed as a batched analysis at the conclusion of the enrollment period so that cord testing results could not be linked back to any individual research participants. Linkage between the survey, chart abstraction, and umbilical cord result was completed via a shared study identification number. No patient identifiers were recorded at any time.
The study survey asked if women had ever used marijuana and if they used marijuana during the pregnancy. For women who reported marijuana use during pregnancy, the survey asked detailed questions about time of last marijuana use, method of use (smoking, edibles, vaping, topical, other), and reasons for use. In addition the survey asked participants to estimate the number of days of use over the past 30 days indicative of past month use. Past month use is a standardized measure of drug use on validated surveys such as the National Survey of Drug Use and Health.6
Basic demographic and clinical characteristics were collected from participants’ medical records and entered into a secure data entry system called Research Electronic Data Capture (REDCap)7 using the same study identification number. In order to preserve anonymity several demographic variables were categorized. Maternal age was categorized as less than 21 years, 22–25 years, 26–29 years, 30–34 years, and 35 years or older. Gestational age at delivery was categorized as less than 37 weeks, 37 weeks and 0 days to 38 weeks and 6 days, 39 weeks and 0 days to 41 weeks and 0 days, and over 41 weeks. Race, ethnicity and reported use of marijuana on the admission history and physical were also documented. At both participating hospitals, all women are asked by a healthcare provider (midwife, resident physician or attending physician) about drug use at the time of admission for delivery and at entry to prenatal care. Current employment, completed education level, annual income, marital status, insurance (unknown, private insurance, Medicaid or Medicare), tobacco use, and whether there are other children in the home were ascertained by self-report on the survey.
Umbilical cord segments of participants were drained of blood, rinsed with saline, and patted dry. Six-inch segments were stored in sterile specimen cups labeled with the study identification number. Cord segments were frozen at −80 oC and were thawed just prior to processing for analysis. The cord tissue was processed and analyzed for THC-COOH by liquid chromatography-tandem mass spectrometry (LC-MS/MS), according to methods similar to those previously published.8 Briefly, cord tissue was weighed and homogenized in methanol. Supernatant was subjected to hydrolysis, solid phase extraction, concentration and reconstitution. Extracts were analyzed on an Agilent 1260 infinity series HPLC pump and AB SCIEX 5500 mass spectrometer. Liquid chromatography (LC) separation was performed on an Agilent Poroshell 120 EC-C18 column with mobile phase A: 5mM ammonium bicarbonate pH 9.5 in water and mobile phase B: methanol. Detection was performed by tandem mass spectrometry (MS/MS) in negative electrospray ionization mode. Two ion transitions were monitored for THC-COOH and its respective deuterated internal standard (THC-COOH-d3). Data were acquired by multiple reaction monitoring (MRM) mode.
Calibration curves were prepared with drug-free cord matrix. Assay performance criteria were correlation coefficient over the analytical measurement range of R≥0.995, average imprecision (% coefficient of variation) ≤20%, limit of detection signal to noise (S/N) ratio ≥3, limit of quantitation S/N≥10 and correlation/accuracy ≥80%. The limits of detection and quantification for THC-COOH were verified at 100 pg/g and 200 pg/g, respectively.
A preliminary anonymous self-report survey at the two enrollment sites estimated that 10% of our cohort would use marijuana during pregnancy. However, given that umbilical cord homogenate sampling will detect use from the second trimester onward, we anticipated that the detected prevalence of use would be slightly higher and closer to 15% in our population. With an anticipated prevalence of marijuana use of 15% in our population, a sample size of 100 was selected to be able to demonstrate that ascertainment of marijuana use by self-report is equivalent (within 5%, range 10–20%) to detecting THC-COOH in the umbilical cord homogenate with 80% power at a 5% significance level using a two-sided equivalence test of correlated proportions.
We estimated the prevalence of any marijuana use by all three methods of ascertainment with 95% confidence intervals. Confidence intervals were calculated using exact methods. The agreement between different measures of prenatal marijuana use was evaluated using Kappa coefficients with 95% confidence intervals. Women were categorized by survey-reported last use (≤30 days ago, 30 days to 1 year, more than 1 year, never), and the proportion of women with umbilical cord results above the limit of detection and limit of quantification for THC-COOH was reported for each group. Between group comparisons of the proportion of women with positive cord results were made using contingency tables. Women with positive cord homogenate results were also compared to women with negative cord homogenate results for basic demographic characteristics.
In order to evaluate if the quantified amount of THC-COOH in the umbilical cord could estimate recent prenatal marijuana use, the relationship between survey-reported number of days of use in the past 30 days and quantitative THC-COOH cord homogenate result was evaluated using Spearman correlation. A P value <0.05 was considered statistically significant. All analyses were performed in SAS, and graphics were created with GraphPad Prism.
Results
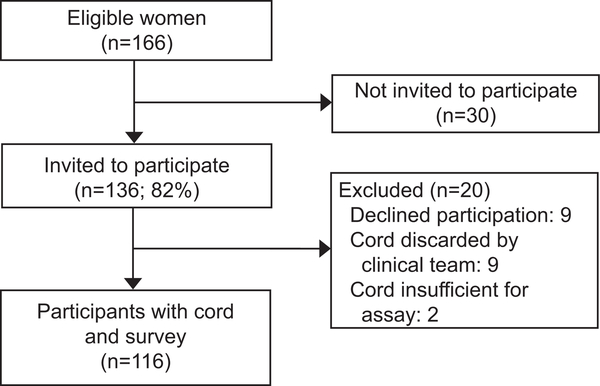
Of 166 eligible women, 136 (82%) were approached for the study; 9 declined participation in the survey portion, 9 cords were discarded by the clinical team prior to research collection and 2 cord samples were insufficient for assay, leaving 116 participants with surveys linked to cord assay results (Figure 1). The nine women who declined participation in the survey portion of the study all had negative cord homogenate assays for THC-COOH.
Figure 1.
Study population.
Of the total cohort, 57 delivered at Denver Health Hospital and 59 delivered at University of Colorado Hospital. The population differed by study site. Women who delivered at Denver Health Hospital were more likely to be Hispanic, have public insurance and to report lower income and lower education level than those delivered at University of Colorado Hospital. Demographics of the study population by site are presented in Table 1.
Table 1.
Characteristics by enrollment site and umbilical cord homogenate result
| Characteristic | UCH n=59 | DHHA n=57 | P value | THC-COOH positive n=26 | THC-COOH negative n=90 | P value |
|---|---|---|---|---|---|---|
| Race | 0.108 | 0.606 | ||||
| White | 42 (71.2) | 41 (73.2) | 20 (80.0) | 63 (70.0) | ||
| Black | 10 (16.9) | 4 (7.1) | 3 (12.0) | 11 (12.2) | ||
| Asian | 3 (5.1) | 1 (1.8) | 0 (0.0) | 4 (4.4) | ||
| Other | 4 (6.8) | 10 (17.9) | 2 (8.0) | 12 (13.3) | ||
| Hispanic ethnicity | 23 (39.0) | 41 (73.2) | <.001 | 16 (64.0) | 48 (53.3) | 0.342 |
| Maternal age | 0.193 | 0.017 | ||||
| 21 years or less | 14 (23.7) | 10 (18.2) | 4 (16.0) | 20 (22.5) | ||
| 22–25 years | 10 (16.9) | 16 (29.1) | 12 (48.0) | 14 (15.7) | ||
| 26–29 years | 12 (20.3) | 11 (20.0) | 4 (16.0) | 19 (21.3) | ||
| 30–34 years | 19 (32.2) | 10 (18.2) | 3 (12.0) | 26 (29.2) | ||
| Over 35 years | 4 (6.8) | 8 (14.5) | 2 (8.0) | 10 (11.2) | ||
| Gestational age | 0.199 | 0.306 | ||||
| Less than 37 weeks | 7 (11.9) | 8 (14.3) | 6 (24.0) | 9 (10.0) | ||
| 37–38 weeks 6 days | 16 (27.1) | 8 (14.3) | 4 (16.0) | 20 (22.2) | ||
| 39–41 weeks 0 days | 31 (52.5) | 38 (67.9) | 14 (56.0) | 55 (61.1) | ||
| Greater than 41 | 5 (8.5) | 2 (3.6) | 1 (4.0) | 6 (6.7) | ||
| Education level | 0.035 | 0.217 | ||||
| No high school diploma | 7 (12.1) | 16 (28.1) | 6 (23.1) | 17 (19.1) | ||
| High school or equivalent | 16 (27.6) | 19 (33.3) | 11 (42.3) | 24 (27.0) | ||
| Vocational orsome college | 14 (24.1) | 13 (22.8) | 6 (23.1) | 21 (23.6) | ||
| Bachelors, Masters, Doctoral | 21 (36.2) | 9 (15.8) | 3 (11.5) | 27 (30.3) | ||
| Other children in home | 28 (50.0) | 31 (56.4) | 0.502 | 10 (40.0) | 49 (57.0) | 0.134 |
| Insurance type | 0.004 | 0.038 | ||||
| None ordon’t know | 2 (3.4) | 7 (12.5) | 0 (0.0) | 9 (10.2) | ||
| Private insurance | 26 (44.8) | 10 (17.9) | 5 (19.2) | 31 (35.2) | ||
| Medicaid orMedicare | 30 (51.7) | 39 (69.6) | 21 (80.8) | 48 (54.5) | ||
| Annual income | 0.006 | 0.367 | ||||
| Less than $10,000 | 24 (41.4) | 23 (40.4) | 11 (42.3) | 36 (40.4) | ||
| $10,001-$49,999 | 13 (22.4) | 26 (45.6) | 11 (42.3) | 28 (31.5) | ||
| More than $50,000 | 21 (36.2) | 8 (14.0) | 4 (15.4) | 25 (28.1) | ||
| Employment status | 0.087 | 0.688 | ||||
| Employed full/part-time | 30 (51.7) | 18 (31.6) | 12 (46.2) | 36 (40.4) | ||
| Student | 2 (3.4) | 1 (1.8) | 1 (3.8) | 2 (2.2) | ||
| Homemaker | 9 (15.5) | 21 (36.8) | 6 (23.1) | 24 (27.0) | ||
| Out of and looking for work | 4 (6.9) | 4 (7.0) | 3 (11.5) | 5 (5.6) | ||
| Out of or unable to work | 13 (22.4) | 13 (22.8) | 4 (15.4) | 22 (24.7) | ||
| Married or domestic partner | 29 (50.0) | 30 (52.6) | 0.961 | 11 (42.3) | 48 (53.9) | 0.69 |
| Self-reported prenatal tobacco use | 3 (5.1) | 2 (3.5) | 0.676 | 2 (7.7) | 3 (3.3) | 0.335 |
DHHA is Denver Health and Hospital Authority. UCH is University of Colorado Hospital. THC-COOH positive is 11-nor-delta-9-tetra-hydrocannabinol-9-carboxylic acid assay above the limit of detection (100 pg/g).
Of the eligible participants, 2.6% (95% CI, 0.5%−7.4%) reported marijuana use to healthcare providers as documented on the admission history. On the self-report survey, 55 (47.4%) women reported marijuana use at some point in their lifetimes while 14.7% (95% CI, 8%−21%) reported past year use and 6.0% (95% CI, 2.5%−12.0%) reported past-month use. Of those with past year use (n=17), 82% smoked marijuana, 24% used edibles, 24% used a vaporizer, and 29% used other methods of use such as topical lotions; many used more than one method of administration. Women were most likely to report using marijuana for recreation (41%) and to help with sleep (41%). Other reported reasons for use were to help with to help with anxiety (35%), nausea (29%), pain (24%), weight gain (12%), and because of habit (12%). Seven women reported marijuana use in the past 30 days on the survey. Among them, the median reported frequency of use was 2.5 of the last 30 days. Three women reported only one day of use, with the four other women each reporting 2, 3, 5 and 10 days of use.
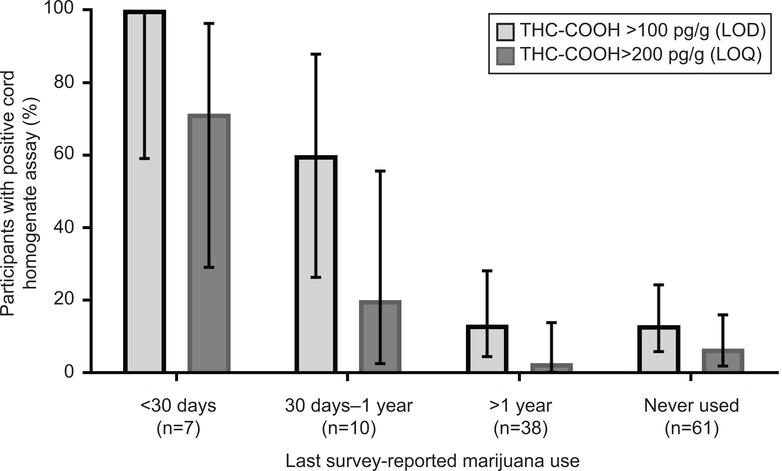
Among 116 umbilical cord homogenate assays, 26 (22.4%, 95% CI 15.2%−31.1%) had THC-COOH above the limit of detection (100 pg/g), with 12 (10.3%, 95% CI, 5.5%−17.4%) also above the limit of quantification (200 pg/g). Demographic characteristics of women by cord homogenate result are presented in Table 1. The observed demographic differences were derived predominantly from a large proportion of women with THC-COOH above the limit of detection being in the 22 to 25 year-old age group (48.0%) with only 15.7% of the cord negative group in this age strata (p<0.001). Similar differences were noted in the insurance category with 80.8% of cord positive women having Medicaid compared to 54.5% in the negative cord group (p=0.016). The prevalence of tobacco use did not differ between cord positive and cord negative groups. All women with survey-reported use in the last 30 days had a THC-COOH above the limit of detection, and cord THC-COOH concentrations differed based on self-reported recency of use (Figure 2).
Figure 2.
Relationship between positive cord homogenate results for 11-nor-delta-9-tetrahydrocannabinol-9-carboxylic acid (THC-COOH) and last survey-reported marijuana use (n=116). Percentages are graphed with exact 95% CIs. LOD, limit of detection; LOQ, limit of quantification.
Overall there was not substantial agreement between the measures of marijuana use (report to the healthcare provider, self-reported use on survey, and cord homogenate assay). There was moderate agreement between 30-day use on the survey and umbilical cord homogenate above the limit of detection for THC-COOH (kappa 0.52, 95% CI 0.32–0.72). The agreement between report to the health care provider and self-reported use in the past year on the survey was fair (kappa 0.27, 95% CI 0.02–0.51). The agreement between medical record review and umbilical cord homogenate above the limit of detection for THC-COOH was slight (kappa 0.17, 95% CI 0.0–0.34).
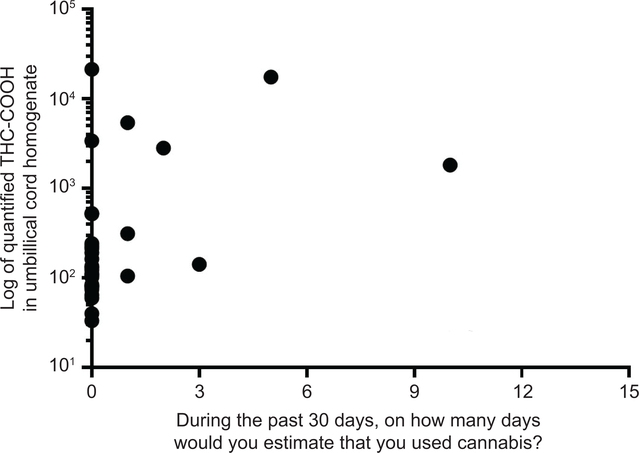
Survey self-reported frequency of marijuana use in the past 30 days had moderate correlation with quantified umbilical cord THC-COOH (correlation coefficient 0.44, 95% CI 0.28–0.58, p<0.001; Figure 3). Consistent with the observed differences in prevalence based on self-reported versus biological sampling-detected use, many women who reported no marijuana use in the past 30 days had a cord result positive for THC-COOH (Figure 3).
Figure 3.
Correlation between quantified 11-nor-delta-9-tetrahydrocannabinol-9-carboxylic acid (THC-COOH) by liquid chromatography-tandem mass spectrometry and survey self-reported frequency of marijuana use over the past 30 days. P=.44 (95% CI 0.28, 0.58).
Discussion
The majority of existing studies of prenatal marijuana use have ascertained marijuana use with self-report, and often through chart abstraction from clinical documentation. In our study, there was poor agreement between self-reported measures of marijuana use and biological sampling. Prevalence of use estimates from biological sampling were higher than those from self-report even in a state with legalized marijuana. These differences in ascertainment of marijuana exposure suggest potential uncertainty in prior estimates of the association between marijuana use and maternal and neonatal outcomes.
In our cohort, 1 in 10 women tested positive for THC-COOH above the clinical test threshold demonstrating that use was common. In the Kaiser Permanente Northern California study, the prevalence of use was 7.1% based on self-report and urine testing in 2016 with approximately 3–4% disclosing use to a healthcare provider on a prenatal questionnaire.4 Our results were similar in that 3% of women self-reported use to a healthcare provider. In comparison, 6% of our cohort reported use in the last 30 days on an anonymous survey, 10% had cord results over the limit of quantification (clinical test threshold), and 22% were above the limit of detection (research test threshold). Our higher estimates of use prevalence might be expected since cord homogenate testing identifies use from the second trimester onward in comparison to urine testing which only detects use over 2 to 3 days. Additionally, marijuana is legal for both medicinal and recreational use in Colorado while marijuana was not fully legalized in California when the Kaiser Permanente study was performed.
When compared to women with a negative cord testing result, women with a positive result were more likely to be 22 to 25 years old. Marijuana was available for recreational use to women over 21 years of age in Colorado during the study period. Our results are consistent with other studies demonstrating an increased prevalence of use among younger women, which may allow for targeted interventions in this age group.4
We found moderate correlation between self-reported past 30-day marijuana use and quantified THC-COOH in the cord homogenate demonstrate the promise of umbilical cord assays to estimate prenatal use. Exactly how far back in time marijuana use can be detected with umbilical cord homogenate sampling remains unknown. Prior studies compared umbilical cord sampling to meconium sampling and demonstrated similar detection results.5, 9 However, in order to more thoroughly evaluate the capacity of umbilical cord testing to quantify use over time, women would need to be queried regarding marijuana use throughout pregnancy. In addition, factors which may affect clearance of metabolites such as body mass index or other drug use need to be considered. The impact of second-hand marijuana smoke exposure on cord homogenate results remains unknown, though observational studies demonstrate detectable metabolites in serum and urine of non-pregnant adults with environmental exposure.10
Strengths of this study include its cross-sectional design and the use of a single time point of marijuana measurement (at delivery) by different methods for direct comparison. We utilized an otherwise discarded biological sample so consent for use of the sample was not required; therefore, self-report data were not biased by participant knowledge of pending biological testing. All women who delivered during the pre-specified time period were eligible and approached regardless of a reported history of substance use or other sociodemographic factors previously associated with use.
Our study has limitations. We only considered women eligible if they spent at least two hours on labor and delivery to allow time for study staff approach. Even with this eligibility criterion, 18% of eligible women were not approached by study staff and cords were not collected due to limited staff availability. In addition, our population had a high proportion of white, low-income women so the results may not be generalizable. The process by which healthcare providers queried women about use was not standardized; however, this is likely consistent with other studies11–13 utilizing self-reported measures of marijuana use. In addition, we could not identify a validated survey to collect detailed information about contemporary marijuana use patterns prior to starting the study; therefore, we developed the survey questions. Finally, we had insufficient sample size to evaluate differences in perinatal outcomes by marijuana exposure status.
There is public health concern about the increasing use of marijuana in pregnancy given mixed findings about its maternal and neonatal effects.2 Recent studies using umbilical cord testing have suggested an association between marijuana use and adverse outcomes including stillbirth and neonatal morbidity.14,15 Future studies should examine how the use of biological sampling for ascertainment of exposure impacts the association between marijuana use and perinatal outcomes.
Supplementary Material
Acknowledgements
Dr. Metz was supported by the National Institute on Child Health and Human Development under award number 5K12HD001271–18 during the completion of this work. This project was funded by the Colorado Clinical and Translational Sciences Institute (CCTSI) under award number UL1 RR025780. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Financial Disclosure
The authors did not report any potential conflicts of interest.
Each author has confirmed compliance with the journal’s requirements for authorship.
Presented as a poster at the Society for Maternal-Fetal Medicine Annual Meeting, Dallas, TX, January 29-February 3, 2018.
References
- 1.Marijuana use during pregnancy and lactation. Committee Opinion No. 722. American College of Obstetricians and Gynecologists. Obstet Gynecol 2017;130:e205–e9. [DOI] [PubMed] [Google Scholar]
- 2.Metz TD and Borgelt LM. Marijuana use in pregnancy and while breastfeeding. Obstet Gynecol 2018; epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brown QL, Sarvet AL, Shmulewitz D, Martins SS, Wall MM, Hasin DS. Trends in Marijuana Use Among Pregnant and Nonpregnant Reproductive-Aged Women, 2002–2014. JAMA 2017; 317(2): 207–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Young-Wolff KC, Tucker LY, Alexeeff S, et al. Trends in Self-reported and Biochemically Tested Marijuana Use Among Pregnant Females in California From 2009–2016. JAMA 2017;318:2490–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Montgomery D, Plate C, Alder SC, Jones M, Jones J, Christensen RD. Testing for fetal exposure to illicit drugs using umbilical cord tissue vs meconium. J Perinatol 2006;26:11–4. [DOI] [PubMed] [Google Scholar]
- 6.National Survey on Drug Use and Health. https://nsduhweb.rti.org/respweb/homepage.cfm. Accessed October 12, 2018.
- 7.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 2009;42:377–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wu F, Scroggin TL, Metz TD, McMillin GA. Development of a Liquid Chromotography-Tandem Mass Spectrometry Method for the Simultaneous Determination of Four Cannabinoids in Umbilical Cord Tissue. J Anal Toxicol 2018; 42(1): 42–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Colby JM. Comparison of umbilical cord tissue and meconium. Clin Biochem 2017; 50(13–14):784–90. [DOI] [PubMed] [Google Scholar]
- 10.Rohrich J, Schimmel I, Zorntlein S, et al. Concentrations of delta-9-tetrahydrocannabinol and 11-nor-9-carboxytetrahydrocannabinol in blood and urine after passive exposure to cannabis smoke in a coffee shop. J Analytic Toxicol 2010; 34:196–203. [DOI] [PubMed] [Google Scholar]
- 11.Chabarria KC, Racusin DA, Antony KM, et al. Marijuana use and its effect in pregnancy. Am J Obstet Gynecol 2016; 215(4):506.e1–7. [DOI] [PubMed] [Google Scholar]
- 12.Warshak CR, Regan J, Moore B, Magner K, Kritzer S, Van Hook J. Association between marijuana use and adverse obstetrical and neonatal outcomes. J Perinatol 2015; 35(12):991–5. [DOI] [PubMed] [Google Scholar]
- 13.Conner SN, Carter EB, Tuuli MG, Macones GA, Cahill AG. Maternal marijuana use and neonatal morbidity. Am J Obstet Gynecol 2015; 213(3):422.e1–4. [DOI] [PubMed] [Google Scholar]
- 14.Metz TD, Allshouse AA, Hogue CJ, et al. Maternal marijuana use, adverse pregnancy outcomes, and neonatal morbidity. Am J Obstet Gynecol 2017; 217(4): 478.e1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Varner MW, Silver RM, Rowland Hogue CJ, et al. Association between stillbirth and illicit drug use and smoking during pregnancy. Obstet Gynecol 2014;123:113–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.