Abstract
Objective.
This study compared barium esophagram with high-resolution esophageal manometry (HRM) results to determine whether esophagram is an adequate screening examination for esophageal motility disorders, a common cause of dysphagia.
Study Design.
Case series with chart review.
Setting.
Tertiary academic medical center.
Subjects and Methods.
A retrospective review was completed of 281 patients who underwent both HRM and esophagram from March 2012 to June 2014. Inclusion criteria included a specific assessment of the presence or absence of dysmotility on both examinations.
Results.
Eighty-four males and 197 females were included in the study. Average age was 57 years (range, 16–84). Average time between studies was 19 days (range, 0–90). Motility was judged to be normal in 40.2% (113 of 281) of esophagrams and 46.6% (131 of 281) of HRM studies. However, disagreement between the study findings was significant (P = .04). The sensitivity of esophagram for detecting esophageal dysmotility was 0.69, and specificity was 0.50. The positive and negative predictive values of esophagram for dysmotility were 0.61 and 0.58, respectively.
Conclusions.
Esophagram is useful in the assessment of anatomic abnormalities but is a poor screening examination for the detection of esophageal dysmotility. Patients with suspected esophageal dysphagia should be referred for HRM to evaluate motility disorders and identify potential treatment targets, regardless of esophagram results.
Keywords: esophagram, esophageal dysphagia, esophageal dysmotility, esophageal manometry
There are several diagnostic procedures that can be helpful in the evaluation of esophageal dysphagia. These include esophagography, manometry, esophagoscopy, and pH impedance testing. Of these examinations, high-resolution esophageal manometry (HRM), particularly with the addition of impedance testing, is generally considered the gold standard for the diagnosis of motility disorders.1 Because motility disorders are a common cause of esophageal dysphagia, it is important to appropriately assess for dysmotility in these patients.
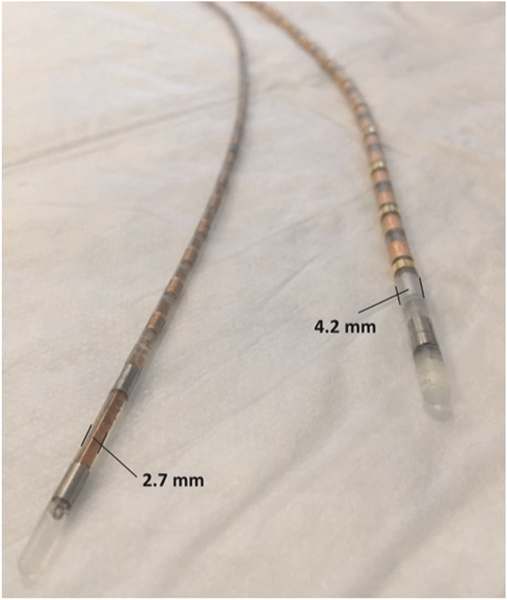
High-resolution manometry involves placement of a 2.7-or 4.2-mm catheter through the nares and into the stomach, spanning the upper and lower esophageal sphincters.2 The patient is placed in a recumbent position and asked to swallow 10 thin and 10 viscous saline swallows. Patients may better tolerate the 2.7-mm catheter, but the smaller catheter either lacks impedance data or has a decreased number of sensors at each pressure-recording location. The 4.2-mm catheter can produce high-resolution manometry and impedance measurements, providing information on contractility as well as bolus clearance.3 In addition to its invasive nature, another drawback of HRM is its limited availability when compared with other modalities.
The barium esophagram is a common radiographic examination and available at most institutions. The utility of barium sulfate, as an insoluble radiopaque contrast medium, gained attention as early as 1910.4 The test involves having the patient drink single- and double-contrast media while still images and videofluoroscopy are recorded in various patient positions (eg, upright, supine, left posterior oblique).5,6 Esophageal anatomic and functional characteristics are evaluated during an esophagram.6 There are 2 limitations of the barium esophagram: the patient has to drink what might be an unpleasant liquid, and the patient is exposed to a certain degree of radiation during the examination.
Given the less invasive nature of the esophagram and its more widespread availability, our study aimed to compare the barium esophagram with HRM to ascertain whether this test could be utilized as a screening examination for motility disorders. The findings of this study could assist dysphagia clinicians in recommending appropriate referrals for esophageal dysphagia evaluation.
Methods
A retrospective review of electronic medical records was completed for patients who underwent both HRM and esophagram from March 2012 to June 2014 (2.25 years). Inclusion criteria included a specific comment on the presence or absence of dysmotility on both examinations. Examinations were included only if they were completed within 90 days of each other and both were completed at our institution. Exclusion criteria included patients with missing data on either examination. The Medical University of South Carolina Institutional Review Board approved this study.
At our institution, the esophagram is completed in the usual standardized fashion, although order and technique may vary slightly.5,6 Fluoroscopy of the chest is performed. High-density barium sulfate suspension is ingested by the patient, and rapid sequence cervical esophagography is performed in anterior-posterior, oblique, and/or lateral projections. Double-contrast thoracic esophagography (following ingestion of effervescent granules and high-density barium) is performed in the lateral posterior oblique projection with the patient upright. Peristalsis and full-column imaging of the thoracic esophagus are evaluated in the prone position. A 13-mm barium tablet is given and visualized in the upright anterior-posterior projection to evaluate for stricture. A “template type” report is utilized to report most esophagram results. This template prompts the radiologist to comment on esophageal dysmotility, resulting in the majority of studies having a specific assessment of motility.
All HRM studies were completed in our gastroenterology motility laboratory and interpreted by a single gastroenterologist (D.O.C.) with extensive experience in the interpretation of these examinations. HRM examinations were completed with a 4.2-mm solid-state manometry-impedance catheter (Figure 1) with the commonly used standardized protocol as detailed in the introduction. The Chicago classification was used to evaluate and categorize motility disorders.7
Figure 1.
Esophageal manometry (2.7 mm) and manometry-impedance catheters (4.2 mm). Given Imaging (Covidien Inc, Sunnyvale, California).
Data regarding medications were collected through 2 approaches. First, the subjects were asked specifically about any gastrointestinal-related medications at the time of their HRM study and were prompted by a list of common antacid and promotility agents for this information. In addition, a chart review of medications listed in the subject’s electronic medical record was completed.
Descriptive and classification statistical analyses were completed. Paired t test was used to assess for agreement between examination findings. A P value <.05 was considered significant. Results were dichotomized into normal versus abnormal for classification analysis.
Results
During the study period, 800 patients underwent HRM at our center. Of these patients, 290 had an esophagram completed within 90 days of their HRM study, and 281 (84 males and 197 females) had a specific assessment of esophageal motility on both examinations. The average age was 57 years (range, 16–84). Average time between studies was 19 days (range, 0–90), with 61 (21.6%) examinations on the same day, 134 (47.5%) within 1 week, and 212 (75.2%) completed within 30 days. The various indications for the examinations are listed in Table 1. Esophageal motility was judged to be normal in 40.2% (113 of 281) of esophagrams and 46.6% (131 of 281) of HRM studies. However, there was significant disagreement between the studies (P = .04). With HRM as the gold standard for the evaluation of esophageal motility, the sensitivity of esophagram for detecting esophageal dysmotility was 0.69, and the specificity was 0.50 (Table 2). The positive and negative predictive values of esophagram for dysmotility were 0.61 and 0.58, respectively. A comparison was also completed of the data for patients who had the esophagram completed within 30 days of the HRM study (Table 2). This revealed comparable results to the 90-day data with a specificity of 0.59, a sensitivity equal to 0.63, a positive predictive value of 0.69, and a negative predictive value 0.52.
Table 1.
Indications for Esophagram and High-Resolution Manometry.a
| Patient-Reported Presenting Complaint | n | % |
|---|---|---|
| Heartburn | 164 | 58.4 |
| Cough | 132 | 47.0 |
| Chest pain | 104 | 37.0 |
| Throat clearing | 98 | 34.9 |
| Regurgitation | 71 | 25.3 |
| Hoarseness | 71 | 25.3 |
| Difficulty swallowing | 57 | 20.3 |
| Nausea | 35 | 12.5 |
| Asthma attacks | 31 | 11.0 |
| Indigestion | 29 | 10.3 |
| Stomach pain | 28 | 10.0 |
| Sore throat | 5 | 1.8 |
Note that the majority of patients exhibited >1 concurrent complaint.
Table 2.
Accuracy of Esophagram in the Detection of Dysmotility, Utilizing High-Resolution Esophageal Manometry as the Gold Standard.
| Time between Examinations | ||
|---|---|---|
| ≤30 d (n = 212) | ≤90 d (n = 281) | |
| Sensitivity | 0.59 | 0.69 |
| Specificity | 0.63 | 0.50 |
| Positive predictive value | 0.69 | 0.61 |
| Negative predictive value | 0.52 | 0.58 |
Examination results completed within 30 and 90 days of each other are reported.
Of patients with complete medication-related data (n = 278), only 53 (19.1%) were taking no gastrointestinal-related medications. A majority of patients (n = 210, 75.5%) were taking proton pump inhibitors; 71 (25.5%) were taking H2 blockers; and 32 (11.5%) were taking some other type of acid-neutralizing agent (eg, calcium carbonate). Three patients were taking metoclopramide, a prokinetic agent.
Tertiary (nonpropulsive) contractions were noted on 34 esophagrams, and in all but 1 examination, the motility on the esophagram was judged to be “abnormal” overall. However, only 16 of 34 (47.1%) of these studies were ultimately found to have abnormal motility on HRM. Regarding specific motility disorders, achalasia was reported in 47 of 281 (16.7%) HRM studies and 24 of 281 (8.5%) esophagrams. The sensitivity of esophagram to detect achalasia was 0.39, but the specificity was high at 0.98. Of the HRM studies, nutcracker esophagus was noted in 8 of 281 (2.8%) and jackhammer esophagus in 2 of 281 (0.7%). Only 1 esophagram noted a nutcracker sign, but this diagnosis was not supported by the corresponding HRM results for that patient. No esophagram findings in patients with spasm, hypertensive peristalsis, or nutcracker or jackhammer esophagus indicated a hyperperistaltic process. Table 3 details the motility disorders, according to the Chicago classification system,7 that were detected on HRM.
Table 3.
Specific Motility Disorders Detected on High-Resolution Manometry.
| Motility Disorders | n | % |
|---|---|---|
| Ineffective esophageal motility | 79 | 28.1 |
| Achalasia | 47 | 16.7 |
| Nutcracker esophagus | 8 | 2.8 |
| Esophageal spasm | 6 | 2.1 |
| Jackhammer esophagus | 2 | 0.7 |
Since esophagram is also an assessment of the anatomic and structural integrity of the esophagus, these findings were compared with HRM results (utilizing esophagram as the gold standard). The only consistent anatomic abnormality noted on HRM was manometric evidence of a hiatal hernia, which was noted in 45 of 281 patients (16.0%). Hiatal hernia was noted on the esophagram in 83 of 281 patients (30%), a common finding in this population. The specificity for HRM in the detection of hiatal hernia was good at 0.90, but sensitivity was poor at 0.29 when compared with esophagram as the standard. One stricture and 1 web were suspected on HRM but not seen on the corresponding esophagrams for those particular patients. Six strictures in total were diagnosed on esophagram.
Discussion
There are conflicting reports in the literature regarding the utility of esophagography in the evaluation of esophageal motility disorders, a major cause of esophageal dysphagia. Ott et al compared perfusion manometry results with radio-graphic records in 172 patients and found an overall sensitivity of esophagram in the detection of motility disorders as 0.56.8 However, Schima et al reported a higher overall sensitivity of 0.79 for esophagram when evaluating 88 patients with dysphagia.9
Few prior investigations compared esophagography with high-resolution manometry, which is the gold standard in the evaluation of motility disorders today. Halland et al found poor correlation between the limited specific finding of tertiary contractions on esophagram and the diagnosis of motility disorders on HRM.10 In our study, it was difficult to identify a consistent radiographic finding that was indicative of motility dysfunction on esophagram. Many examinations included only a general statement, such as “esophageal dysmotility” or “weak primary peristalsis.” While tertiary waves may be one of the signs used by radiologists on esophagram to identify dysmotility (97% of examinations with this finding were judged as abnormal), we also found a poor correlation between tertiary waves and dysmotility on HRM (47.1%).
Interestingly, we also found a poor correlation between esophagram and HRM in the diagnosis of achalasia, a primary motility disorder with characteristic anatomic changes readily identifiable on esophagography. In our study, esophagram had a poor sensitivity (0.29) for this diagnosis, although specificity was good. It is important to note, however, that 44 of 47 examinations diagnosed with achalasia on HRM were also judged to have abnormal motility, although not specifically achalasia, on esophagram. Our low sensitivity is contradictory to previous investigations that found a combined sensitivity of 0.95 for esophagram in the detection of achalasia and scleroderma.8 It is possible that the advent of solid-state HRM is more sensitive in the evaluation of early achalasia when compared with previous manometric studies. Therefore, in previous investigations, advanced cases with more obvious radiologic signs may have better correlated with the less sensitive manometric results.
A screening examination should have a high sensitivity and good predictive value. In our study, we found that the sensitivity of esophagram for diagnosing dysmotility is poor, indicating that many cases of dysmotility, as a possible cause for patient’s dysphagic symptoms, could be missed. While some investigators may assert that esophageal manometry is a procedure that should be performed only if endoscopic or fluoroscopic examination is negative,11 our data (including 65 false-positive results) support the need to further evaluate motility with HRM, regardless of the results of other studies. It should be stressed, however, that the evaluation of mucosal surfaces and anatomic abnormalities by either esophagoscopy or esophagography is important as well. In our study, hiatal hernia was “missed” by HRM in nearly half of the patients with this finding on esophagram. HRM is complementary to, but not a replacement for, these other examinations.
Our study has several limitations. It is a retrospective study, and the clinicians interpreting the esophagrams and manometry studies were not blinded to patients’ diagnoses or histories. In addition, the studies were not performed simultaneously. The average time between examinations was 19 days. Another limitation of our study is that, while we collected information regarding gastrointestinal-related medications, we were unable to specify when the patient began the medication. For example, we were unable to tell whether patients had the esophagram and then started on a promotility agent prior to the HRM study. However, since only 0.01% patients were taking promotility agents, this confounding effect would be expected to be low.
Conclusion
Esophagram may be useful in the assessment of structural and anatomic abnormalities but is a poor screening examination for detection of esophageal dysmotility. Patients with suspected esophageal dysphagia should be referred for HRM to evaluate for motility disorders regardless of esophagram results.
Acknowledgments
Disclosures
Competing interests: Ashli O’Rourke and Bonnie Martin-Harris received a onetime equipment grant from Given Imaging (Covidien Inc) in 2014 for an unrelated research protocol. This equipment was not utilized in this project. Bonnie Martin-Harris, Northern Speech Services—royalty and speaking fee; Veterans Affairs—grant research support (RR&D).
Funding source: Grant support: NIH/NIDCD K24 DC 12801–01 award for mentorship (Bonnie Martin-Harris, principal investigator; Ashli O’Rourke, mentee).
References
- 1.Rice TW, Steven SS. A primer of high-resolution manometry. Semin Thorac Cardiovasc Surg. 2011;23:181–190. [DOI] [PubMed] [Google Scholar]
- 2.Murray JA, Clouse RE, Conklin JL. Components of the standard oesophageal manometry. Neurogastroenterol Motil. 2003; 15:591–606. [DOI] [PubMed] [Google Scholar]
- 3.Fox M, Sweis R. Future directions in esophageal motility and function: a new technology and methodology. Neurogastroentrol Motil. 2004;24(suppl 1):48–56. [DOI] [PubMed] [Google Scholar]
- 4.Schott GD. Some observations on the history of the use of barium salts in medicine. Med Hist. 1974;18:9–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Levine MS, Rubesin SE, Herlinger H, et al. Double-contrast upper gastrointestinal examination: technique and interpretation. Radiology. 1988;168:593–602. [DOI] [PubMed] [Google Scholar]
- 6.Katzka DA. The role of barium esophagography in an endoscopy world. Gastrointest Endoscopy Clin N Am. 2014;24:563–580. [DOI] [PubMed] [Google Scholar]
- 7.Bredenoord AJ, Fox M, Kahrilas PJ, et al. Chicago classification criteria of esophageal motility disorders defined in high resolution esophageal pressure topography. Neurogastroenterol Motil. 2012;24(suppl 1):57–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ott DJ, Richter JE, Chen YM, et al. Esophageal radiography and manometry: correlation in 172 patients with dysphagia. AJR Am J Roentgenol. 1987;149:307–311. [DOI] [PubMed] [Google Scholar]
- 9.Schima W, Stacher G, Pokieser P, et al. Esophageal motor disorders: videofluoroscopic and manometric evaluation—prospective study in 88 symptomatic patients. Radiology. 1992;185:487–491. [DOI] [PubMed] [Google Scholar]
- 10.Halland M, Ravi K, Barlow J, Arora A. Correlation between the radiological observation of isolated tertiary waves on an esophagram and findings on high-resolution esophageal manometry [published online October 20, 2014]. Dis Esophagus. [DOI] [PubMed] [Google Scholar]
- 11.Feussner H, Kauer W, Siewert JR. The place of esophageal manometry in the diagnosis of dysphagia. Dysphagia. 1993;8: 98–104. [DOI] [PubMed] [Google Scholar]