Abstract
A survey of community-based outpatient clinic health care providers suggests the need for additional education and training to increase their cultural competencies.
Lesbian, gay, bisexual and transgender (LGBT) populations face significant social stigmatization, discrimination, and marginalization that contribute to negative patient outcomes. Consequently, the LGBT population experiences high rates of mental health issues, such as suicide and depression, as well as sexually transmitted diseases (STDs), drug abuse, poverty, and homelessness.1,2
BACKGROUND
According to the CDC, gay men are at highest risk and have increased incidences of gonorrhea, chlamydia, herpes, human papilloma virus (HPV), and HIV.3 Lesbians and bisexual women are less likely to get preventive cancer screenings, such as Pap smears and mammograms, and have higher incidences of HIV, hepatitis C, self-reported gonorrhea, and are more likely to be overweight or obese.3–6 In addition, LGBT populations have high rates of use of tobacco, alcohol, and other drugs.
The National Transgender Discrimination Survey of 6,450 transgender and nonconforming participants also provides extensive data on the challenges faced by transgender individuals. Discrimination was frequently experienced in accessing health care. Due to their transgender status, 19% were denied care, and 28% postponed care due to perceived harassment and violence within a health care setting.1
The LGBT populations experience personal and structural barriers that interfere with their ability to access high-quality care. Sexual gender minority individuals also experience health care barriers due to isolation, insufficient social services, and a lack of culturally competent providers.4 At the same time, many health care providers (HCPs) experience various barriers to providing LGBT care and need to increase their cultural competence by improving awareness, receptivity, and knowledge.7,8 One personal barrier to quality care is stigmatization toward LGBT persons as expressed through HCP prejudices, beliefs, attitudes, and behaviors.2 Factors such as gender, race, and religious beliefs also influence attitudes to LGBT health care.
A study by Chapman and colleagues found significant differences in attitudes toward gay men by male and female medical and nursing students.9 Male students had a significantly more negative attitude toward gay men compared with the attitudes of female students. Cultural competence, defined in the study as gay affirmative action principles scores, were statistically significant and strongly correlated with negative attitudes. In this study there also was a statistically significant negative correlation between attitudes and knowledge scores indicating a considerable potential for personal values to influence the provision of health care.9
Various barriers inherent in the health care system restrict access to high-quality care. Institutional barriers that include a lack of legal recognition of same-sex partners, equality in visitation rights, and the ability of same-sex partners to access partner’s medical records hamper health care quality. The HCPs’ lack of knowledge of the health risks or health care needs of the LGBT population also present a structural barrier to quality of care and affects patient outcomes.2
Culturally competent interventions in health care delivery also have been studied to reduce LGBT health disparities. A systematic review of 56 studies by Butler and colleagues found that the term cultural competence was not well defined and often was denoted with the terms patient-centered or individualized care.10 A review on the impact of these interventions in LGBT populations also noted that the long-term effects of culturally competent interventions on health disparities in LGBT populations are still unknown.
The Joint Commission has identified the health and welfare of LGBT populations as a major priority. Beginning in 2012, The Joint Commission started assessing compliance with standards for cultural competence and patient-centered care for LGBT recipients as part of the accreditation criteria.11 The Joint Commission recommended that health care facilities begin to transform the health care environment to be a more welcoming, safe, and inclusive environment for LGBT patients and their families.11 Health care providers can play an important role in reducing the significant health disparities and unequal treatment.12
Problem Identification
Improving health outcomes and reducing health disparities are an important part of the HCP’s role. Yet, many HCPs lack the significant knowledge, skills, and cultural competencies needed to provide quality LGBT care.10 Evidence suggests that HCPs continue to receive little or no training to prepare them to manage this vulnerable population. 10 Due to the growing evidence of health disparities and negative health outcomes affecting LGBT populations, the federal government has identified LGBT care and patient outcomes as a major health concern and priority under the Healthy 2020 goals.2,4
About 3.5% (9 million) of the U.S. adult population are identified as lesbian, gay, or bisexual and 0.3% or 700,000 as transgender.13,14 The VHA serves 9 million veterans at 1,245 facilities.15 The 2000 census estimated that about 1 million veterans reported having same-sex partners.16 The number of LGBTs in the VHA system is unknown because the VHA has not historically collected LGBT demographic data. The estimation of LGBT veterans that use the VHA is based on a proportion of the population of LGBT military service personnel and may not provide the best representation of LGBT veterans enrolled or seeking care in the VHA.17 By conservative estimates, about 134,000 veterans are thought to be transgender.14 Between 2006 and 2013, the reported prevalence and incidence of transgender-related diagnoses in the VHA have steadily increased with 40% of new diagnoses occurring since 2011.18 In fiscal year 2013, there were 32.9 per 100,000 veterans with transgender-related diagnoses, and the numbers are increasing.18
Because the cooperation of HCPs can play a significant part in reducing health disparities and unequal treatment in the care LGBT patients receive, the VHA launched several initiatives to create a more welcoming, inclusive, and empowering environment for LGBT veterans and families. Among the initiatives, VHA established the Office of Health Equity to address health disparities and ensure that patient-centered care is provided in a positive environment. 19,20 The VHA also issued a national directive mandating standardized services be provided for transgender veterans.20
Despite these initiatives, obstacles remain to the delivery of patient-centered LGBT care at the VA. A first step to identifying barriers to patient-centered, high-quality care to LGBT veterans is to evaluate personal and institutional barriers as expressed through HCPs’ preceptions and knowledge about the health of LGBT patients. The magnitude of barriers to providing patient-centered care must first be identified and understood before institutional recommendations can be made and implemented at the facility or national level.
METHODS
This study examined attitudes and knowledge about LGBT patient health among 45 primary care providers (PCPs) in 4 VA community-based outpatient clinics (CBOCs). The first clinical question examined whether PCPs desired more education and training on LGBT health. The second clinical question asked whether there were gender differences in attitudes among providers about the need for LGBT health education. Subsequently, the study’s findings are expected to be disseminated to VHA stakeholders to further examine HCP education and training needs on LGBT topics to facilitate improvement of HCP point of care behaviors, patient outcomes, and LGBT empowerment within the VHA environment.
The model presented in The Process of Cultural Competence in the Delivery of Healthcare Services by Campinha-Bacote provides an applicable conceptualization to guide HCPs’ actions toward delivering culturally responsive health care services to increasingly diverse health populations.21 The model defines cultural competence as an ongoing dynamic process of striving to effectively work within the cultural context of the client (person, family, or community). The model integrates 5 constructs that are fundamental to becoming culturally competent to provide appropriate culturally responsive care to diverse clients: cultural awareness, cultural knowledge, cultural skill, cultural encounters, and cultural desires.21 The level of competence of the HCP is believed to have a direct relationship with their ability to provide culturally competent health care services. Table 1 provides the definitions of the 5 constructs and highlights the role of education and training in influencing competence in providing LGBT health services.21
Table 1.
Cultural Competency Definitions
| Competency | Definition |
|---|---|
| Cultural awareness | A self-examination process through which health care providers start to explore their own culture and professional values. The awareness process allows for personal recognition of biases, prejudices, and assumptions about those with different values, ways of life, and practices. |
| Cultural knowledge | Obtaining a thorough educational foundation on diverse cultures with a goal of understanding the client values about their lives and the client’s perspective of his or her worldviews. |
| Cultural skill | Learning how to collect clients’ health histories and culturally specific physical health assessments of diverse clients. |
| Cultural encounter | A process in which health care providers directly interact cross-culturally with diverse client groups to refine or modify beliefs about a cultural group. |
| Cultural desire | The process of motivating the health care provider to want to rather than have to engage in the process of becoming culturally aware, knowledgeable, and skilled in cultural encounters. |
This project used a descriptive, cross-sectional one-group design to target physicians, nurse practitioners (NPs), and physician assistants (PAs) at VA Southern Nevada Healthcare System (VASNHS) CBOCs. Participation in the project was voluntary. The duration of project from data collection to completion of analysis and summation of the results was 4 months. The study was approved by the institutional review board (IRB) at the University of Alabama in Huntsville, and it was exempt from the VA IRB. The survey consisted of 74 questions, including 8 demographic questions and 66 LGBT-related questions.
The survey instrument, renamed the Perception and Knowledge of Sexual and Gender Minority Health (PKSGMH) survey was adapted with permission from an original study by Jabson and colleagues and used its format without revision or restructuring.22
Attitudinal questions asked personal opinions on LGBT orientation and gender identity (eAppendix, available at www.fedprac.com). For example, is being LGBT right, wrong, or disgusting? Is LGBT a natural expression of sexuality or gender identity? Did providers feel competent in giving LGBT care; would providers prefer not to provide LGBT care; could providers give LGBT care in a sensitive manner? Was medical training adequate to address the needs of LGBT patients? Knowledge questions asked about the prevalence of depression, anxiety, obesity, alcohol, drug abuse, tobacco, obesity, STDs and chronic diseases in LGBT populations. Belief questions asked about respect for LGBT clients, the need for more training, education, and skills in LGBT care, and provider awareness of antidiscrimination and visitation policies in the workplace.
Measures
The survey instrument integrated components of 4 different measures on attitudes and knowledge of LGBT health with questions about familiarity with organizational policies on discrimination, visitation, and staff training in LGBT care. The PKSGMH survey measured attitudes and knowledge levels on LGBT health by calculating the mean scores for each of 4 measures.
General Attitudes Toward LGBT Nonpatients
The attitudes toward LGBT nonpatients measure includes 4 subscales with 3 identical questions on how providers felt about LGBT individuals: (a) attitudes toward lesbians (α: .78); (b) attitudes toward gay men (α: .76); (c) attitudes toward bisexuals (α: 78); and (d) attitudes toward transgender people (α: .70). Each subscale used a 5-point Likert scale (5 = strongly agree).
Physician Attitudes Toward LGBT (ATLG) Patients
The attitudes toward LGBT scale assessed physicians’ feelings toward providing care to LGBT patients. This scale of 6 questions had modest reliability with a Cronbach α of .5. The measure used a 5-point Likert scale (5 = strongly agree). For this project, this scale was renamed the Provider subscale.
Knowledge of LGBT (KLGBT) Patients
The knowledge of LGBT patients’ scale included 13 true/false questions and had a Cronbach α of .74.
Gender and Sexual Minority Affirmative Practice (GSMAP)
The GSMAP affirmative practice scale evaluated HCPs’ attitudes and beliefs about the treatment of LGBT patients. The 11-question measure with 2 subscales used a 5-point Likert scale with high reliability on the clinicians’ beliefs and behaviors subscales. Both subscales had a Cronbach α of .93 and .94, respectively.
Demographics and Data Analyses
Health care providers answered demographic questions about gender, sexual orientation, and marital status. They also were asked whether they had ever received any focused training in LGBT patient care. Descriptive and demographic data analyses were performed using SPSS version 24.0 (Armonk, New York). A significance level of P < .05 was used for all analyses. Analysis of variance (ANOVA) statistical analysis was conducted to evaluate the differences in mean scores between male and female PCP groups on the 4 attitudes toward LGBT subscales and the Provider subscale.
RESULTS
Seventy-two PCPs participated in completing the PKSGMH survey. Fifty-seven surveys were returned; however, only 45 surveys were completely answered and included in the final analysis. Twelve surveys containing unanswered questions to the knowledge sections were excluded from the data analysis, and 14 distributed surveys were not returned. The overall response rate for completed surveys was 62.5% (Table 2).
Table 2.
Primary Care Provider Demographics (n = 45)
| Characteristics | Provider, % |
|---|---|
|
| |
| Sex | |
| Male | 42 |
| Female | 58 |
|
| |
| Sexual orientation | |
| Heterosexual | 96 |
| Homosexual | 2 |
| Bisexual | 2 |
| Transgender | 0 |
|
| |
| Marital status | |
| Married | 80 |
| Partnered | 3 |
| Single | 13 |
| Divorced | 4 |
|
| |
| Had acquaintance, peers, colleagues, friends, or family who are LGBT | |
| Yes | 87 |
| No | 13 |
|
| |
| Primary care providers providing care to LGBT patient subgroups | |
| Lesbian | 78 |
| Gay | 91 |
| Bisexual | 56 |
| Transgender | 67 |
|
| |
| Received focused training on LGBT patient care | |
| Yes | 15 |
| No | 85 |
|
| |
| Mean experience (SD), y | 14.7 (12.1) |
Abbreviation: LGBT, lesbian, gay, bisexual, transgender.
Attitudes Toward Care
Attitudes about competence in providing LGBT care was answered in question 23 of the PKSGMH survey. Overall, a total of 51.1% (n = 23) of PCPs agreed that they were competent to provide LGBT care, and 15.5% (n = 7) disagreed. By gender, 50% (n = 9) of males said they were competent in providing LGBT care compared with 51.8% (n = 14) of females.
Analysis of variance was used to test for differences between groups on the 5 ATLG subscales (gay, lesbian, bisexual, transgender, provider) of the PKSGMH survey (Table 3). A grouping variable was created by separating participants by gender and by their responses to a question that asked about their desire for more education about the health care needs of LGBT patients. The grouping resulted in 4 groups: (1) males who responded yes to need for additional education; (2) males who responded no to need for additional education; (3) females who responded yes to need for additional education; and (4) females who responded no to need for additional education. Results of the ANOVA demonstrated significant differences between groups for the bisexual subscale (F = 3.005, df = 3, 32; P = .045), transgender subscale (F = 4.545, df = 3, 32; P = .009), and the provider subscale (F = 12.602, df = 3, 32; P < .001).
Table 3.
ANOVA Group Differences Between Bisexual, Transgender, and Provider Subscales
| ANOVA | Sum of Squares | df | Mean Square | F | P Value | |
|---|---|---|---|---|---|---|
|
| ||||||
| Gay subscale | Between groups | 3.716 | 3 | 1.239 | 2.712 | .061 |
| Within groups | 14.617 | 32 | .457 | |||
| Total | 18.333 | 35 | ||||
|
| ||||||
| Lesbian subscale | Between groups | 3.018 | 3 | 1.006 | 2.336 | .092 |
| Within groups | 13.784 | 32 | .431 | |||
| Total | 16.802 | 35 | ||||
|
| ||||||
| Bisexual subscale | Between groups | 4.201 | 3 | 1.400 | 3.005 | .045 |
| Within groups | 14.910 | 32 | .466 | |||
| Total | 19.111 | 35 | ||||
|
| ||||||
| Transgender subscale | Between groups | 4.591 | 3 | 1.530 | 4.545 | .009 |
| Within groups | 10.776 | 32 | .337 | |||
| Total | 15.367 | 35 | ||||
|
| ||||||
| Provider subscale | Between groups | 9.322 | 3 | 3.107 | 12.602 | .001 |
| Within groups | 7.890 | 32 | .247 | |||
| Total | 17.212 | 35 | ||||
Abbreviation: ANOVA, analysis of variance.
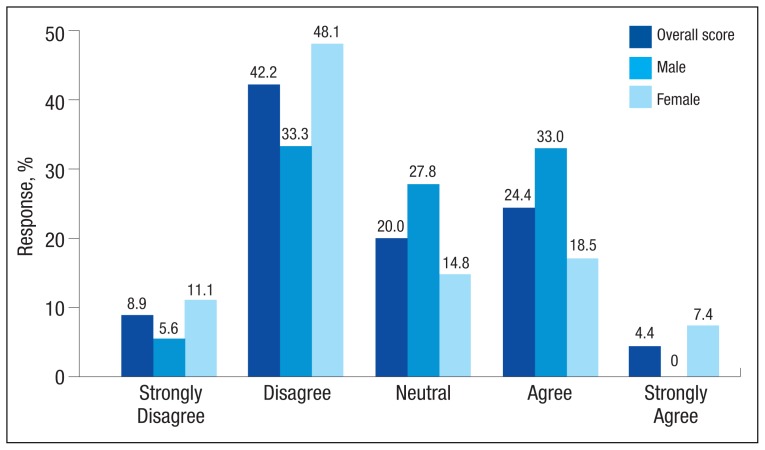
Attitudes toward adequacy of their medical training to address the health needs of the LGBT population were answered in question 26 of the PKSGMH survey. Overall a total of 29% (n = 13) of PCPs agreed that their training adequately prepared them to address the needs of the LGBT population while 51.1% (n = 23) disagreed (Figure). There also was evidence of gender differences on this question. More females disagreed that training was adequate (59.2%, n = 16) compared with male responses (50%, n = 7). By contrast, 33.3% of males (n = 6) agreed training was adequate compared with 25.9% (n = 7) of female responses.
Figure.
Survey Responses to Question About Adequacy of Training of Health Needs in the LGBT Population
Knowledge of LGBT Care
Knowledge level responses among PCPs were not found to be statistically significant. However, 98% of PCPs agreed that practitioners should be knowledgeable about issues unique to LGBT patients and acquire the knowledge necessary to practice effectively. A review of answers to knowledge-specific questions in the KLGBT and GSMAP scales found more than 50% of PCPs responded correctly to true/false questions about prevalence of depression and anxiety, alcohol use, substance abuse, sexual transmitted infections, and physical and sexual trauma in LGBT patients. However, < 50% of the sample correctly answered true in 3 knowledge areas of LGBT health: increased prevalence of tobacco use; increased prevalence of obesity/overweight; and greater risk for chronic disease.
DISCUSSION
Federal health care agencies consider the health and welfare of LGBT persons to be a health priority despite the lack of available science-based knowledge about this population.2 In 2011, the National Academies of Medicine (NAM) noted that there are still research gaps concerning the well-being of LGBT individuals. The report stated that a significant contributor of health care inequities in LGBT patients is the lack of provider training and medical education.2 A major recommendation of the NAM is that additional training and education is needed to reduce barriers and improve patient outcomes in the LGBT population.
Provider attitudes and education are among the gaps that contribute to inequities in the health care of LGBT populations as previously discussed. The findings from this survey suggest that PCPs in the VHA perceive that they have deficits in competencies and knowledge levels on LGBT care and that education influences attitudes toward LGBT care. The association between providers’ self-assessment of their competency and their knowledge and attitudes toward care for LGBT patients was not stated in the clinical question and was not investigated in this study.
An online search of 12,966 courses at the VA Talent Management System (TMS) was conducted to find web-based and/or instructor-led training courses focused on LGBT care. The search found 4 LGBT-focused courses that targeted physicians and nurses. Two 90-minute courses presented clinical and public health data on sexual health and addressed how providers can improve skills on taking sexual histories and incorporating these data into routine practice. Training and skills development in sexual history taking by clinicians is vital in reducing health disparities, such as STDs, and in helping LGBT patients feel more comfortable in accessing health care.4
A 1-hour TMS course focused on training HCPs to develop as researchers, teachers, and leaders in improving the LGBT veteran experience by providing competent care. Information on LGBT-related subjects, such as sexual and physical trauma and STDs, were included in the content of some online courses. However, no other comprehensive courses specifically focused on LGBT care. The only exceptions were the Specialty Care Access Network Extension of Community Healthcare outcome video conferencing-based sequential training on transgender care and the VA Lesbian, Gay and Bisexual Education sharepoint and the transgender education sharepoint. At the VA, online LGBT health training is still limited.
Recommendations
Providing additional LGBT-focused TMS courses could help increase provider knowledge and cultural competencies. An online introductory LGBT health course could be offered at VA facilities for all new employees and HCPs as part of employee orientation. More specific courses with continuing education credits geared toward the HCP and focused on LGBT health could be included in the TMS learning portfolio for each HCP as annual learning refresher courses. This course could include specific knowledge questions on LGBT care and a posttest with a required passing score of 80%.
Training HCPs as designated LGBT educators in VA facilities should be considered. Classroom training could be offered annually or during times of increased LGBT patient focus, such as during LGBT Pride month when learning activities can be planned and/or coordinated with the VA Office of Diversity and Inclusion. Nurses, social workers, pharmacists, and medical assistants who provide supportive care to LGBT patients also should be included in the target audience for LGBT health education and training.
Limitations
The use of a cross-sectional project design with such a small convenience sample prevents generalizability of the findings to all PCPs. The lack of a survey design that included randomization and blinding in survey distribution could certainly deter participants from offering candid responses, particularly to some attitudinal questions that were emotional in context. The true-false responses wherein respondents had a 50% chance at guessing the correct response was not the most reliable method of measuring knowledge levels and thereby limited the ability to draw any strong conclusions about providers’ knowledge levels. Additionally, the project design did not allow for measures of other confounding factors, such as age, race/ethnicity, religion, and other social factors that could have influenced how participants responded. Additional randomized controlled studies with larger samples are needed to test specific interventions that evaluate the influence of gender on provider attitudes and knowledge as well as the effect of more HCP education and training on LGBT patient outcomes. Moreover, a literature review found no guidelines on how to specifically address provider gender differences in LGBT education and training or strategies for education and training interventions to address these differences.
CONCLUSION
Findings suggest that PCPs need additional education and training involving LGBT health issues. Although both male and female providers want more education, female PCPs as a group expressed a greater desire for more training compared with the responses of male PCPs. However, given the study’s small sample size, a strong conclusion regarding gender differences cannot be made. Research has shown that education is a factor that positively influences attitudes and feelings about providing LGBT care. The availability of education and training that is focused on LGBT health topics is still limited within the VHA. Within its stated mission to provide patient-centered care to all veterans, the VHA’s Office of Health Equity has a specific objective for addressing LGBT health disparities and ensuring the delivery of standardized services to LGBT veterans.
Better training on LGBT health topics is vital to improving health care delivery to LGBT populations. To meet this goal, ongoing HCP training to improve attitudes and knowledge and develop the skills necessary to effectively address LGBT health issues also must be a priority at VHA facilities. The VHA also should consider institutional changes that incorporate increased LGBT-focused health education into the learning activities of PCPs. This is essential to evaluating the quality of care given the impact on patient outcomes and health disparities in LGBT populations.
Supplementary Information
Footnotes
Author disclosures
The authors report no actual or potential conflicts of interest with regard to this article.
Disclaimer
The opinions expressed herein are those of the authors and do not necessarily reflect those of Federal Practitioner, Frontline Medical Communications Inc., the U.S. Government, or any of its agencies.
REFERENCES
- 1.Grant JM, Mottet LA, Tanis J, Harrison J, Herman JL, Keisling M. Injustice at every turn: a report of the National Transgender Discrimination Survey. [Accessed October 5, 2017]. http://www.thetaskforce.org/static_html/downloads/reports/reports/ntds_full.pdf. Published 2011.
- 2.Institute of Medicine Committee on Lesbian, Gay, Bisexual, and Transgender Health Issues and Research Gaps and Opportunities. The Health of Lesbian, Gay, Bisexual, and Transgender People: Building a Foundation for Better Understanding. Washington, DC: National Academies Press; 2011. [PubMed] [Google Scholar]
- 3.Centers for Disease Control Prevention. Reported STDs in the United States. 2014 national data for chlamydia, gonorrhea, and syphilis. [Accessed October 5, 2017]. www.cdc.gov/std/stats14/std-trends-508.pdf. Published November 2015.
- 4.U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion. Lesbian, gay, bisexual, and transgender health. [Accessed October 5, 2017]. http://www.healthypeople.gov/2020/topics-objectives/topic/lesbian-gay-bisexual-and-transgender-health. Updated October 4, 2017.
- 5.Kerker BD, Mostashari F, Thorpe L. Health care access and utilization among women who have sex with women: sexual behavior and identity. J Urban Health. 2006;83(5):970–979. doi: 10.1007/s11524-006-9096-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Khan MA, Evans AT, Shah S. Caring for uninsured patients with diabetes: designing and evaluating a novel chronic care model for diabetes care. J Eval Clin Pract. 2010;16(4):700–706. doi: 10.1111/j.1365-2753.2009.01178.x. [DOI] [PubMed] [Google Scholar]
- 7.Herek GM. Sexual prejudice. In: Nelson TD, editor. Handbook of Prejudice, Stereotyping, and Discrimination. New York: Psychology Press; 2009. pp. 441–467. [Google Scholar]
- 8.McKay B. Lesbian, gay, bisexual, and transgender health issues, disparities, and information resources. Med Ref Serv Q. 2011;30(4):393–401. doi: 10.1080/02763869.2011.608971. [DOI] [PubMed] [Google Scholar]
- 9.Chapman R, Watkins R, Zappia T, Nicol P, Shields L. Nursing and medical students’ attitude, knowledge and beliefs regarding lesbian, gay, bisexual and transgender parents seeking health care for their children. J Clin Nurs. 2012;21(7‐8):938–945. doi: 10.1111/j.1365-2702.2011.03892.x. [DOI] [PubMed] [Google Scholar]
- 10.Butler M, McCreedy E, Schwer N, et al. Improving cultural competence to reduce health disparities. Review No. 170. [Accessed October 5, 2017]. https://ahrq-ehc-application.s3.amazonaws.com/media/pdf/cultural-competence_research.pdf. Published March 29, 2016. [PubMed]
- 11.The Joint Commission. Advancing effective communication, cultural competence, and patient-and family-centered care: a roadmap for hospitals. [Accessed October 5, 2017]. https://www.jointcommission.org/assets/1/6/ARoadmapforHospitalsfinalversion727.pdf. Published 2010.
- 12.Snelgrove JW, Jasudavisius AM, Rowe BW, Head EM, Bauer GR. “Completely out-at-sea” with “two-gender medicine”: a qualitative analysis of physician-side barriers to providing healthcare for transgender patients. BMC Health Serv Res. 2012;12:110. doi: 10.1186/1472-6963-12-110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Gates GJ. How many people are lesbian, gay, bisexual, and transgender? [Accessed October 5, 2017]. http://williamsinstitute.law.ucla.edu/wp-content/uploads/Gates-How-Many-People-LGBT-Apr-2011.pdf. Published April 2011.
- 14.Gates GJ, Herman J. Transgender military service in the United States. [Accessed October 5, 2017]. https://williamsinstitute.law.ucla.edu/wp-content/uploads/Transgender-Military-Service-May-2014.pdf. Published May 2014.
- 15.U.S. Department of Veteran Affairs. Veterans Health Administration. [Accessed October 5, 2017]. http://www.va.gov/health. Updated October 2, 2017.
- 16.Gates GJ. Gay men and lesbians in the U.S. military: estimates from the 2000 census. [Accessed October 5, 2017]. http://www.lgbtdata.com/uploads/1/0/8/8/10884149/ds008_uscensus_gates.pdf. Published September 28, 2014.
- 17.Mattocks KM, Kauth MR, Sandfort T, Matza AR, Sullivan JC, Shipherd JC. Understanding healthcare needs of sexual and gender minority veterans: how targeted research and policy can improve health. LGBT Health. 2014;1(1):50–57. doi: 10.1089/lgbt.2013.0003. [DOI] [PubMed] [Google Scholar]
- 18.Kauth MR, Shipherd JC, Lindsay J, Blosnich JR, Brown GR, Jones KT. Access to care for transgender veterans in the Veterans Health Administration 2006–2013. Am J Public Health. 2014;104(suppl 4):S532–S534. doi: 10.2105/AJPH.2014.302086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Uchendu US. Veterans Health Administration Office of Health Equity: what is it a about? [Accessed October 5, 2017]. http://www.hsrd.research.va.gov/for_researchers/cyber_seminars/archives/769-notes.pdf. Published November 4, 2013.
- 20.U.S. Department of Veterans Affairs, Veterans Health Administration. VHA Directive 2013-003: Providing Health Care for Transgender and Intersex Veterans. [Accessed October 5, 2017]. http://www.transequality.org/sites/default/files/docs/resources/VHAHealthcareDirective_2013.pdf. Published February 8, 2013.
- 21.Campinha-Bacote J. The process of cultural competence in the delivery of healthcare services: a model of care. J Transcult Nurs. 2002;13(3):181–184. doi: 10.1177/10459602013003003. [DOI] [PubMed] [Google Scholar]
- 22.Jabson JM, Mitchell JW, Doty SB. Associations between non-discrimination and training policies and physicians’ attitudes and knowledge about sexual and gender minority patients: a comparison of physicians from two hospitals. BMC Public Health. 2016;16:256. doi: 10.1186/s12889-016-2927-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.