Introduction
The science of heart failure (HF) dyadic self-care is advancing rapidly as evidenced by recent theoretical work,1 literature reviews,2,3 and multiple empiric studies.4–7 In HF self-care, a dyad refers to a person diagnosed with HF and his/her informal caregiver. This informal caregiver may or may not be a family member but must contribute to self-care without financial compensation. With this increased focus on dyads comes a commensurate need for clinically relevant advancements in dyadic care and development of a deeper understanding of the impact of dyads on HF self-care.
One such scientific advancement is Lyons and Lee’s1 new dyadic illness management theoretical model which proposes that the dyad itself, rather than either individual patients or caregivers should be the unit of analysis. As such, examination of the appraisal of the illness, management behaviors, and physical and mental health occur at the dyadic rather than individual level. In a dyadic analysis, risk or protective factors are now conceptualized as risk (or protection) to the dyad’s ability to collaborate successfully in managing the illness. This theory creates a new framework that allows examination of, for example, the impact of incongruent appraisal, poor collaboration, and unhealthy dyadic behaviors, with the potential to move science beyond the atheoretical barriers noted by dyadic researchers.2,3
While the Theory of Dyadic Illness Management is an important advancement, it has not yet been operationalized in clinical practice. The central elements of the Theory of Dyadic Illness Management, particularly dyadic appraisal and management behaviors, are supported by data generated from the development and testing of a dyadic HF care typology developed by our group and first introduced in 2013.8 This suggests that our dyadic HF care typology may be useful in implementing the Theory of Dyadic Illness Management in clinical practice.
Typologies, once considered archaic, are now viewed as person-oriented classification systems that allow a whole system view of information patterns.9,10 The purpose of this article is to describe the initial conceptualization of the HF care dyadic typology, present advances in our thinking, and suggest future directions for this clinically relevant classification system.
Initial Conceptualization of the HF care Dyadic Typology
The initial conceptualization of the HF care dyadic typology was derived from Interdependence Theory, which states that human interaction is a function of the needs, thoughts and motives of two people in a particular situation.11 This theoretical conceptualization is mathematically and empirically testable with the Actor-Partner Interdependence Model (APIM),12 an analytic strategy frequently used in dyadic studies.7,13,14 Actor effects occur when the individual’s independent variable impacts his/her own dependent variable. For example, when a person’s anxiety level makes it difficult for that person to listen to another person, that is an actor effect. Partner effects occur when the individual’s independent variable impacts his/her partner’s dependent variable. For example, when an individual’s anxiety level makes it hard for another person to concentrate, that is a partner effect. The APIM posits that Actors (patients in this case) and Partners (caregivers) can interact with 1) primarily actor (A>P) or 2) partner effects (A<P); 3) equal actor and partner effects (A=P); or 4) unequal actor and partner effects (A≠P).15
The HF care dyadic typology integrates Interdependence Theory and the APIM by operationalizing human interaction in self-care as two individuals who work on HF self-care can do so in one of four potential ways – the patient or caregiver can take sole responsibility for the patient’s HF self-care (A>P; A<P). Alternately, they may work together in collaborative (they work together on the same self-care task; [A=P]) or complementary (they work together but on different self-care tasks; [A≠P]) ways (Figure 1). For example, in collaborative and complementary dyads, the dyad may monitor the patient’s weight together with the patient stepping on the scale and caregiver writing the weight down (collaborative) or the patient may weigh herself while the caregiver is preparing a low sodium breakfast for the patient (complementary).
Figure 1.
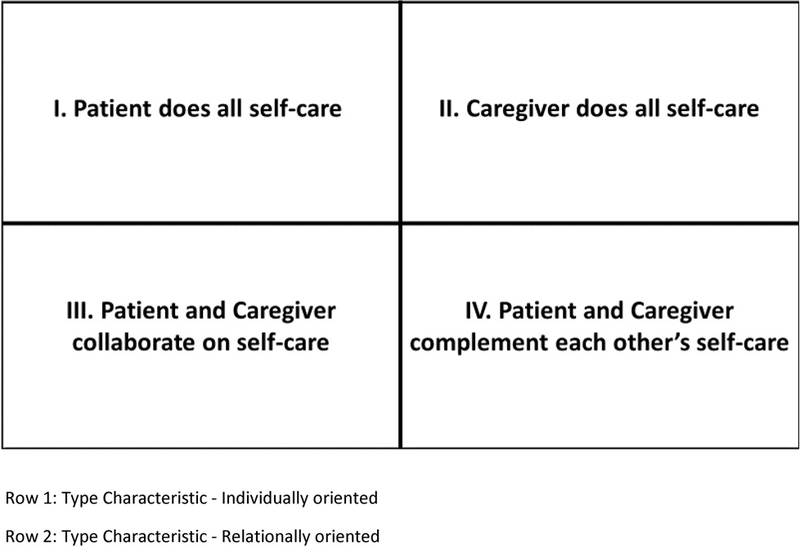
Initial Conceptualization of the HF care Dyadic Typology
As part of this first conceptualization, defining features, subtypes, characteristics, contexts within which the particular type is prevalent were developed for each of the four types (Table 1) .8 For example, in the patient oriented type, the defining feature is that the patient takes care of the majority of his/her self-care without input from the caregiver. This behavior may occur because the patient refuses the caregiver’s help, or the caregiver may refuse to help (subtypes). The patient oriented type is considered an individually oriented type (characteristic) and expected to occur most commonly early in the HF trajectory (context).8 Once the types were proposed, the next steps were to empirically characterize, attempt to measure, and then begin examining them in a series of developmental studies. The first three studies involved sub-analyses from a larger, parent study (Hupcey, PI) examining the palliative care needs of HF patients and caregivers in the last two years of life.
Table 1.
The HF care Dyadic Typology: Initial Conceptualization of the Theoretically Derived Typology
| Dyadic Type | Defining feature | Subtypes | Characteristics | Context |
| Patient oriented dyads |
The patient takes care of the majority of their self-care without input from the caregiver |
The patient may either choose to take control their HF care without the involvement of the caregiver OR The caregiver may choose to be uninvolved in the HF care |
Individually oriented |
Most common early in the HF trajectory (Stage A & B) |
| Caregiver oriented dyads |
The caregiver, not the patient, takes care of the majority of the patient’s self-care without input from the patient |
The patient may defer all care decisions and actions to the caregiver OR The caregiver may take responsibility for the care from the patient |
Individually oriented |
Most common in the last stage (D) of HF where patients are no longer able to care for their own HF |
| Collaboratively oriented dyads |
Patients and caregivers actively and together make decisions and take action when needed to maintain and manage the patient’s HF |
This collaboration reflects either a healthy OR Unhealthy (enmeshed) collaboration determined by dyadic report and successful HF outcomes |
Relationally oriented |
Found across the trajectory of HF but less frequently in the advanced stages of HF |
| Complementarily oriented dyads |
The patient and caregiver have negotiated spheres of non- overlapping responsibilities for HF care |
One takes the lead on a particular activity (for example HF care) while the other takes the lead on another activity (ADLs or IADLs) OR The patient and caregiver may have differential functional or cognitive limitations resulting in one taking the lead on decision making while the other provides the actual behavior when cued |
Relationally oriented |
Found across the trajectory of HF but less frequently in the advanced stages of HF |
Study 1: Qualitative Characterization of the Theoretically Derived Types
In the first study8, Stake’s instrumental case study methodology was used to describe the four types by their characteristics (i.e. individually or relationally oriented): two individually oriented types – Type I. patient oriented; Type II. caregiver oriented; and two relationally oriented types -Type III. collaboratively oriented; and Type IV. complementary oriented HF care (Table 2). Nineteen spousal dyads (patient mean age 72, caregiver mean age 69; mean time married 45 years) with moderate to severe HF (NYHA class IIIB-IV) were qualitatively interviewed on how they managed the patient’s HF self-care at home. Evidence of the credibility of the four types was supported by presenting four cases, but a fifth case for the incongruent dyad, arose during this examination. The incongruent dyad type was characterized by a disagreement between the patient and caregiver on who conducts the patient’s self-care. A content analysis across dyads resulted in identifying an overarching theme of Sharing Life which included sub-themes: connected by each other, by other people, or by intangibles (i.e. faith, loss, identity).8 Sharing Life illustrated how dyads use already established behavioral patterns developed across the lifecourse (e.g. a sequence of roles and events enacted over time)16 of the relationship. This first study extended the work of other investigators17,18 who were just beginning to examine dyadic incongruence, while identifying the role of the lifecourse dimensions of dyadic interaction in HF self-care.
Table 2.
The HF care Dyadic Typology: Empiric Support for Initial Conceptualization and Advances in Thinking
| Characterizing, measuring, and assessing the initial conceptualization | ||
|---|---|---|
| Study 1 | • Four theoretically derived dyadic types characterized • Fifth type, incongruent, emerges • Lifecourse dimension of types identified |
|
| Study 2 | • One-item clinical questionnaire developed and tested • Clarity and acceptability of questionnaire supported • Dyads had difficulty distinguishing between two relationally oriented dyads |
|
| Study 3 | • Stability of types across time assessed • Collaborative dyad type most stable • Internal and external factors impact dyadic type stability |
|
| Examining the re conceptualized HF care Dyadic Typology | ||
| Study 4 | • Lifecourse patterns confirmed in a 2nd sample • Lifecourse pattern more stable in dyads scoring higher in self-care self- efficacy and management • Dyadic type incongruence negatively impacts caregiver engagement in self-care maintenance |
|
| Study 5 | • Frequency and distribution of dyadic types compared in U.S. and Spanish sample • Differences and similarities between two U.S samples noted with each other AND with Spanish sample |
|
Study 2: Typology Instrument Development and Preliminary Testing
A 1-item question was developed concurrently with the typology to assess the proposed HF self-care dyadic types.19 This question was designed to quickly evaluate in the clinical setting who takes primary responsibility for the patient’s HF self-care. The questionnaire first defines self-care for the respondent and then gives them four mutually exclusive options (patient, caregiver, collaborative, complementary) to indicate who provides daily HF self-care. Each member of the dyad (patient, caregiver) answers the question individually and their answers are then compared. Preliminary testing in the same sample as the first study8 resulted in evidence for clarity and acceptability by patients and caregivers. Patients were most likely to indicate that they collaborated. Caregivers were most likely to indicate that the patient did all the self-care. When their responses were compared only 9 out of 19 dyads agreed on their type (kappa 0.28; p 0.025) suggesting greater occurrence of dyadic incongruence (disagreement on who is responsible for the HF self-care) then previously found when qualitatively examined by other investigators.17,18 Dyads were most likely to agree if they were in collaborative dyads (n=4 of 9). However, research assistants reported that the dyads found the two relationally oriented dyadic types – collaborative (they work together on the same self-care tasks) and complementary (they work together but on different self-care tasks) a distinction without real difference. Dyads reported that context often determined when and how they worked together on the same task or not, but they viewed both types as collaborative. With this introduction of context determining degree or kind of collaboration, we began to wonder how stable the dyadic types were.
Study 3: Preliminary Assessment of Stability of the HF Care Dyadic Typology Across Time
In the next step we explored how stable or dynamic these dyadic types were.20 To do that we used the data from Studies 18 and 219 as baseline data and then collected the same data (qualitative interviews and 1-item question) a second time between 4–12 months later. A content analysis of concurrent qualitative interviews was conducted. Ten, generally NYHA class III HF (n=6) patients (mean age 64.8) with spousal caregivers (mean age 64.4) were examined. Seven dyads (characterized as relational; i.e. collaborative or complementary oriented) selected the same type at T1 and T2. The three dyads that changed type were characterized as individual; patient or caregiver oriented, suggesting the relationally oriented types may be more stable. In addition, two of those three individually oriented dyads became incongruent at T2 with each member selecting a different type from each other and from their selection at T1. The narratives supported this apparent instability with 100% concordance between the quantitative/qualitative data (using the i-item question and an “I vs. we” analysis of the qualitative data) for the stable dyads and only 50% concordance in the dyads that changed. Examination of the narratives suggested that internal factors, such as one partner perceiving things changing while the other does not, and external factors, such as individual health status of either partner contributed to this instability in dyadic type.
Advances in Thinking
Concurrent with our examination, other scientists were examining the role of dyads in HF.21–24 All of these studies (ours and others) led to advances in our thinking on the initial conceptualization of the HF care dyadic types. Where we proposed four types, the case study suggested that there was a fifth type – the incongruent type. Where we proposed two, distinct, relationally oriented types (collaborative and complementary) the qualitative interviews and subsequent feedback from participants suggested that both types were considered “collaborative” by the dyads – they didn’t consider these two different types but rather one type. In response we collapsed the collaborative and complementary type into “collaborative” and designated the new 4th type as “incongruent” characterized as a patient and caregiver who disagree on who does self-care (Figure 2, Type IV). This re-conceptualization is supported by the APIM, which posits unequal actor and partner effects for this 4th type.12 The questionnaire did not change, we make the adjustment during analysis. After this re-conceptualization we were ready to examine dyadic types further in new studies.
Figure 2.

Reconceptualization of the HF care Dyadic Typology
Study 4: Dyadic Mutual Engagement and Hypothesis Testing
The next mixed method study25–27 was prospectively designed to describe dyadic engagement in HF self-care. We enrolled 78 mixed (spousal, adult child, other) dyads. Patients were primarily male (67%) and mean age 75. Caregivers were primarily female (78%) and mean age 63. Most (96%) were White. The qualitative data supported our earlier findings (Study 1) that mutual engagement involved maintaining established lifecourse patterns. Dyads create interpersonal efficiencies or patterns across the lifecourse that involve matching current situations to previous similar situations and then responding according to these patterns.11 The discovery (Study 1) and confirmation (Study 4) of these lifecourse patterns also supports the use of typologies that allow a whole system view of information patterns. However, the data also added to our understanding that dyad’s patterns for self-care maintenance (day to day care) and self-care management (symptom response)28 may differ in some dyads but not others when escalating symptoms challenge the lifecourse pattern. Dyads who scored higher in self-care self-efficacy and self-care management were more likely to continue using their usual lifecourse pattern while those who scored lower were more likely to access outside support.27 One main finding from this study was that caregivers scored lower on self-care maintenance (day to day care)28 in dyads who also disagreed on type. This suggests to us that we need to examine the role of dyadic congruence or agreement on type more closely if we expect caregivers to engage in daily self-care behaviors.25
Study 5: Cultural Variations in the HF Care Dyadic Typology
In the final study, data from three unique datasets (2 US; 1 Spanish) were examined for frequency and distribution of dyadic types to assess if the number and kind of dyadic types are similar outside of their original context in the US. Established clinical guidelines29–31 and multi-national examinations of both patient32 and caregiver self-care activities 33 suggest that while there may be geographical variations in self-care maintenance or adherence,32 the activities themselves and who is responsible for them are fairly similar across cultures. Data from two different northeastern US studies (Hupcey, PI; Buck, PI) were compared with data from an ongoing Spanish study (Juárez-Vela, PI) to examine this question of similarity. Cultural similarities and differences were compared side by side (Table 3). The Spanish sample shared a similar percent of patient oriented types with the first but not the second US sample. The largest difference was found in the percentage of caregiver oriented types (US .02%, .04% vs. Spanish 47%). Further differences were found in the percentage of dyads who collaborate (US 37%, 39% vs. Spanish 12%) and incongruent dyads (US 49%, 51% vs. Spanish 27%). These findings suggest cultural variations in caregiver engagement in self-care that have not previously been captured.
Table 3.
Frequency and Distribution of HF Self-care Dyadic Types in the US vs. Spanish HF Dyads
| 1) US Study (n=45) | 2) US Study (n=49) | 3) Spanish Study (data n=109) |
|---|---|---|
| Patient Oriented- 5 (11%) | Patient Oriented- 3 (.06%) | Patient Oriented- 16 (15%) |
| Caregiver Oriented- 1 (.02%) | Caregiver Oriented- 2 (.04%) | Caregiver Oriented- 51 (47%) |
| *Collaborative- 11 (24%) | Collaborative- 19 (39%) | Collaborative- 13 (12%) |
| *Complementary- 6 (13%) | Incongruent −25 (51%) | Incongruent- 29 (27%) |
| Incongruent- 22 (49%) |
Legend
Two dyadic types collapsed together as “Collaborative” in subsequent studies. If collapsed here, they would equal 37%. Percentages ± 100% due to rounding.
Future Directions
In summary, development and testing of the HF care dyadic typology across studies has resulted in a well characterized, pragmatic and parsimonious, person-oriented classification system that can facilitate our understanding of how patients and informal caregivers perform the patient’s HF self-care at home. It has also resulted in a practical way to measure the types directly. The outcomes of the studies described in this paper suggest that further testing is needed on whether the particular dyadic type OR if the dyad agrees on their type is more predictive of adequate self-care. Why is this important? If dyads disagree on who is responsible for the self-care, neither partner may take responsibility, or the dyad may waste valuable time and resources in interpersonal conflict. Either outcome may result in self-care failures with subsequent HF advancement, hospitalization and mortality.
Research Directions
The next logical step is to conduct further study using a larger, more heterogeneous sample in a longitudinal trial. If these earlier finding are supported, then we will move forward with intervention studies. For example, it is currently unknown whether incongruent types result in poorer patient outcomes such HF advancement or mortality. Linking the types to patient outcomes is needed before we can recommend testing implementation strategies such as imbedding the 1-item question in electronic health records. It is also recommended that future studies in other countries examine the relationships between dyadic types and patient outcomes as has been done in the US to determine if any of the differences noted in the Study 5 sample are clinically meaningful. Additional next steps include developing further testable hypotheses from this data such as the role of dyadic congruence. While individual34 and dyadic self-care typologies35 have been examined previously, these typologies were data driven, either derived from qualitative data or comparisons of dyadic data from self-care instruments rather than directly measuring the typology with a specific, theoretically derived instrument as in our studies. Therefore, our data may allow for the generation of hypotheses which are more generalizable to other chronic illness populations with similar self-care requirements. Finally, intervention studies should examine whether adapting self-care instruction to dyadic type results in better patient outcomes.
Clinical Directions
This typology and the instrument that measures it were initially developed for clinical use. The research to date was conducted to provide preliminary evidence for its validity as a clinical tool. How is the instrument administered? Both patient and caregiver respond to the 1-item question. The clinician then reviews the responses of both parties (checking if they agree or not) and personalizes the plan of care to the realities of the dyad. This may involve identifying who takes primary responsibility for the self-care and directing any education to them; it may involve referring the couple to supportive care if the dyad disagrees on type; or even couples’ therapy if dyadic incongruence signifies an inability to care for the patient’s HF because of relational issues.
Conclusion
In this paper we have described the initial conceptualization of a clinically meaningful HF care dyadic typology, presented advances in our thinking related to the typology, and suggested future directions for research and clinical practice. As the HF dyadic self-care science has advanced, so has our understanding of the effect of dyadic interaction on HF self-care. But with this increased understanding has come an appreciation of the complexity that ensues when two individuals work together on one complex task – HF self-care.
Acknowledgements:
Research reported in this paper was supported by the National Institute of Nursing Research of the National Institutes of Health under award number R01NR013419–02 (Hupcey, PI); R03NR014524 (Buck, PI). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Additionally, the authors acknowledge the Aragon Institute for Health Research (IIS Aragon) where Dr. Juárez-Vela is a researcher.
Contributor Information
Harleah G. Buck, College of Nursing University of South Florida, Tampa FL.
Judith Hupcey, Graduate Education & Research, College of Nursing, The Pennsylvania State University, University Park, PA.
Raul Juárez-Vela, Faculty of Health Sciences, University San Jorge, Zaragoza, Spain. Researcher, IIS- Aragón, Hospital Clinico Lozano Blesa, Zaragoza, Spain.
Ercole Vellone, Department of Biomedicine and Prevention, University of Rome “Tor Vergata”, Rome, Italy.
Barbara Riegel, School of Nursing, University of Pennsylvania, Philadelphia, PA.
References
- 1.Lyons KS, Lee CS. The Theory of Dyadic Illness Management. Journal of Family Nursing 2018;0(0):1074840717745669. [DOI] [PubMed] [Google Scholar]
- 2.Buck HG, Stromberg A, Chung M, et al. A Systematic Review of Heart Failure Dyadic Self-care Interventions Focusing on Intervention Components, Contexts, and Outcomes. International Journal of Nursing Studies 2018;77:232–242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Strömberg A, Luttik ML. Burden of caring: risks and consequences imposed on caregivers of those living and dying with advanced heart failure. Current Opinion in Supportive and Palliative Care 2015;9(1):26–30. [DOI] [PubMed] [Google Scholar]
- 4.Lee CS, Mudd JO, Auld J, et al. Patterns, relevance and predictors of heart failure dyadic symptom appraisal. European Journal of Cardiovascular Nursing 2017;0(0):1474515117700760. [DOI] [PubMed] [Google Scholar]
- 5.Buck HG, Hupcey J, Wang H-L, Fradley M, Donovan KA, Watach A. Heart Failure Self-care Within the Context of Patient and Informal Caregiver Dyadic Engagement: A Mixed Methods Study. Journal of Cardiovascular Nursing 2018;Publish Ahead of Print. [DOI] [PubMed]
- 6.Chen Y, Zou H, Zhang Y, Fang W, Fan X. Family Caregiver Contribution to Self-care of Heart Failure: An Application of the Information-Motivation-Behavioral Skills Model. Journal of Cardiovascular Nursing. 2017;Publish Ahead of Print. [DOI] [PubMed]
- 7.Vellone E, Chung ML, Cocchieri A, Rocco G, Alvaro R, Riegel B. Effects of Self-Care on Quality of Life in Adults with Heart Failure and Their Spousal Caregivers: Testing Dyadic Dynamics Using the Actor–Partner Interdependence Model. Journal of Family Nursing 2014;20(1):120–141. [DOI] [PubMed] [Google Scholar]
- 8.Buck HG, Kitko L, & Hupcey J. Dyadic Heart Failure Care Types: Qualitative Evidence for a Novel Typology. Journal of Cardiovascular Nursing 2013;28(6):37–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Crane DR, and Marshall ES. Handbook of Families & Health: Interdisciplinary Perspectives In: Sage Publications; 2006: [Google Scholar]
- 10.Bergman LR, Wångby M. The person-oriented approach: a short theoretical and practical guide. Eesti Haridusteaduste Ajakiri 2014;2(1):29. [Google Scholar]
- 11.Rusbult CE, Van Lange PA. Interdependence, interaction, and relationships. Annual review of psychology 2003;54:351–375. [DOI] [PubMed] [Google Scholar]
- 12.Cook WL, Kenny DA . The Actor-Partner Interdependence Model: A model of bidirectional effects in developmental studies. International Journal of Behavioral Development 2005;29(2):101–109. [Google Scholar]
- 13.Buck HG, Mogle J, Riegel B, McMillan S, Bakitas M. Exploring the Relationship of Patient and Informal Caregiver Characteristics with Heart Failure Self-Care Using the Actor-Partner Interdependence Model: Implications for Outpatient Palliative Care. J Palliat Med 2015;18(12):1026–1032. [DOI] [PubMed] [Google Scholar]
- 14.Chung ML, Moser DK, Lennie TA, Rayens MK. The effects of depressive symptoms and anxiety on quality of life in patients with heart failure and their spouses: Testing dyadic dynamics using Actor-Partner Interdependence Model. Journal of Psychosomatic Research 2009;67(1):29–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kenny DA, Kashy DA, Cook WL. Dyadic data analysis In: Methodology in the social sciences; Variation: Methodology in the social sciences: Guilford Press; 2006. [Google Scholar]
- 16.Giele JZ, Elder GH. Methods of life course research: Qualitative and quantitative approaches Sage; 1998. [Google Scholar]
- 17.Retrum JH, Nowels CT, Bekelman DB. Patient and caregiver congruence: The importance of dyads in heart failure care. Journal of Cardiovascular Nursing 2013;28(2):129–136. [DOI] [PubMed] [Google Scholar]
- 18.Kitko LA, Hupcey JE, Pinto C, Palese M. Patient and Caregiver Incongruence in Advanced Heart Failure. Clinical Nursing Research 2014;24(4):388–400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Buck HG, Zambroski C, and Hupcey J. Assessing the Response of Patients and Spousal/Partner Caregivers to a New Instrument Measuring Dyadic Heart Failure Care Types. European Journal of Cardiovascular Nursing 2013;12(2):209–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Buck HG, Kitko L, Hupcey JE, Palese M. Shift Happens: Assessing the Complexity of Dyadic Heart Failure Self-Care in End Stage Heart Failure. Symposium presentation presented at Council for the Advancement of Nursing Science; September 18–20, 2014, 2014; Washington, D.C. [Google Scholar]
- 21.Bidwell JT, Vellone E, Lyons KS, et al. Determinants of heart failure self-care maintenance and management in patients and caregivers: A dyadic analysis. Research in Nursing & Health 2015;38(5):392–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lyons KS, Vellone E, Lee CS, et al. A Dyadic Approach to Managing Heart Failure With Confidence. Journal of Cardiovascular Nursing 2015;30(4S):S64–S71. [DOI] [PubMed] [Google Scholar]
- 23.Hooker SA, Schmiege SJ, Trivedi RB, Amoyal NR, Bekelman DB. Mutuality and heart failure self-care in patients and their informal caregivers. European Journal of Cardiovascular Nursing 2017;0(0). [DOI] [PMC free article] [PubMed]
- 24.Ågren S, Evangelista LS, Hjelm C, Strömberg A. Dyads Affected by Chronic Heart Failure: A Randomized Study Evaluating Effects of Education and Psychosocial Support to Patients With Heart Failure and Their Partners. Journal of cardiac failure 2012;18(5):359–366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Buck HG, Hupcey JE, Mogle J, Rayens MK. Caregivers’ Heart Failure Knowledge Is Necessary but Not Sufficient to Ensure Engagement With Patients in Self-care Maintenance. Journal of Hospice & Palliative Nursing 2017;19(2):170–176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Buck HG, Hupcey J, Watach A . Patterns vs. change: Community-based dyadic heart failure self-care. Clinical nursing research 2017:1–14. [DOI] [PMC free article] [PubMed]
- 27.Buck HG, Hupcey J, Wang H, Fradley M, Donovan KA, Watach A. Heart Failure Self-care Within the Context of Patient and Informal Caregiver Dyadic Engagement: A Mixed Methods Study. Journal of Cardiovascular Nursing In Press:1–7. [DOI] [PubMed]
- 28.Riegel B, Dickson VV, Faulkner KM. The Situation-Specific Theory of Heart Failure Self-Care: Revised and Updated. Journal of Cardiovascular Nursing 2016;31(3):226–235. [DOI] [PubMed] [Google Scholar]
- 29.Yancy CW, Jessup M, Bozkurt B, et al. 2017 ACC/AHA/HFSA Focused Update of the 2013 ACCF/AHA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. Circulation 2017. [DOI] [PubMed]
- 30.Antman EM, Bax J, Chazal RA, et al. Updated Clinical Practice Guidelines on Heart Failure: An International Alignment. Circulation 2016;134(13):e280–e281. [DOI] [PubMed] [Google Scholar]
- 31.Ponikowski P, Voors AA, Anker SD, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J 2016;37(27):2129–2200. [DOI] [PubMed] [Google Scholar]
- 32.Jaarsma T, Strömberg A, Ben Gal T, et al. Comparison of self-care behaviors of heart failure patients in 15 countries worldwide. Patient education and counseling 2013;92(1):114–120. [DOI] [PubMed] [Google Scholar]
- 33.Buck HG, Harkness K, Wion R, et al. Caregivers’ contributions to heart failure self-care: A systematic review. European journal of cardiovascular nursing : journal of the Working Group on Cardiovascular Nursing of the European Society of Cardiology 2015;14(1):79–89. [DOI] [PubMed] [Google Scholar]
- 34.Dickson VV, Deatrick JA, Riegel B. A typology of heart failure self-care management in non-elders. European Journal of Cardiovascular Nursing 2008;7(3):171–181. [DOI] [PubMed] [Google Scholar]
- 35.Lee CS, Vellone E, Lyons KS, et al. Patterns and predictors of patient and caregiver engagement in heart failure care: a multi-level dyadic study. International Journal of Nursing Studies 2015;52(2):588–597. [DOI] [PubMed] [Google Scholar]


