Abstract
Background:
Income volatility is on the rise and presents a growing public health problem. Since in many epidemiologic studies income is measured at a single point in time, the association of long-term income volatility with incident cardiovascular disease (CVD) and mortality has not been adequately explored. The goal of this study was to examine associations of income volatility from 1990 to 2005 with incident CVD and all-cause mortality in the subsequent 10 years.
Methods:
The Coronary Artery Risk Development in Young Adults Study is an ongoing prospective cohort study conducted within urban field centers in Birmingham, AL; Chicago, IL; Minneapolis, MN; and Oakland, CA. We studied 3,937 black and white participants aged 23–35 years old in 1990 (our study baseline). Income volatility was defined as the intra-individual standard deviation of the percent change in income across five assessments from 1990 to 2005. An income drop was defined as a decrease of 25% or more from the previous visit and less than the participant’s average income from 1990 to 2005. CVD events (fatal and non-fatal) and all-cause mortality between 2005 and 2015 were adjudicated using medical records and death certificates. CVD included primarily acute events related to heart disease and stroke.
Results:
A total of 106 CVD events and 164 deaths occurred between 2005 and 2015 (incident rates 2.76 and 3.66 per 1,000 person-years, respectively). From Cox models adjusted for socio-demographic, behavioral, and CVD risk factors, higher income volatility and more income drops were associated with greater CVD risk (high vs. low volatility HR=2.07, 95% CI=1.10, 3.90; 2+ vs. 0 income drops HR=2.54, 95% CI= 1.24, 5.19) and all-cause mortality (high vs. low volatility HR=1.78, 95% CI=1.03, 3.09; 2+ vs. 0 income drops HR=1.92, 95% CI=1.07, 3.44).
Conclusions:
In a cohort of relatively young adults, income volatility and drops during a 15-year period of formative earning years were independently associated with a near two fold risk of CVD and all-cause mortality.
Keywords: Socio economic status, income, cardiovascular disease, mortality
Introduction
In the United States, the recent rise in income inequality suggests that a larger proportion of the population faces poverty and economic difficulties.1 In addition, while most individuals experience some sort of income change,2,3 income volatility has been on the rise and has reached a record high level since 1980.4,5 Income volatility is generally considered to be a sudden and unpredictable change in income over time, and most often it consists of declines in income.6 The rise in income volatility is especially true for low income households who experience a significant number of income drops that exceed 25% of their average income7 and presents a growing public health problem.
Income volatility may have pervasive effects on health, potentially mediated by behavioral changes, psychological stress, or access to medical care. Increasing evidence suggests income volatility is associated with an array of unfavorable health outcomes, including worse mental health, overall health quality, and all-cause mortality.8–11 Income volatility may also play a role in acute or chronic health outcomes – for example, low income patients with chronic diseases may give up medications and medical visits to cope with unexpected financial instability, consequently resulting in increased risk of disease, including heart attack and stroke.6,12 While income volatility and other longitudinal conceptualizations of income have gained recognition in medical research on the social determinants of health,6 in many epidemiologic studies, income is measured at a single point in time in the life course rather than repeatedly over time.13,14
The Coronary Artery Risk Development in Young Adults (CARDIA) study has collected longitudinal income data on a multisite population-based sample of white or black adults since the early 1990s, which makes it well-suited for assessing the volatility of income over an influential time in the life course and how it relates to incident cardiovascular disease (CVD) and all-cause mortality in a relatively young cohort. Additionally, this study allows us to examine income patterns during a period of the formative earning years in participants lives (ages 30–45), rather than examining earnings later in life when CVD risk factors may be more proximal. In this study, we aim to examine the relationship of income volatility and frequency of income drops, from 1990 to 2005, with incident CVD and all-cause mortality over the subsequent 10 years.
Methods
The data, analytic methods, and study materials can be been made available to other researchers who apply to the CARDIA Publications and Presentations Subcommittee for purposes of reproducing the results or replicating the procedure.
Study population
CARDIA is an ongoing prospective cohort study of the determinants of CVD. In 1985–86, 5,115 adults were recruited from four field centers in Birmingham, AL; Minneapolis, MN; Chicago, IL; and Oakland, CA. Recruitment was approximately balanced within center by sex, age (18–24 vs. 25–32), race (black, white), and education ≤high –school vs. >high-school). Enrollees were asked to participate in a baseline examination and then eight follow up examinations over 30 years. Upon study enrollment, participants agreed to be contacted every 6 months to ascertain vital status and update contact information and yearly to ascertain certain CVD outcomes. Standardized protocols were used to gather demographic, socioeconomic, and clinical data at each follow-up visit. Details of the study protocol have been described elsewhere.15 Appropriate informed consent was obtained from each study participant. The study was approved annually by the institutional review boards from each field center and the coordinating center. Going forward we refer to each CARDIA follow-up visits by the calendar year in which it began. The majority of the participants were re-examined at each visit, with more than 70% examined at year 30.
Measurement of economic predictors between 1990 and 2005
During CARDIA examinations at years 1990, 1992, 1995, 2000, and 2005, pre-tax household income for the past 12 months from all sources was self-reported and recorded in the following pre-specified income brackets: $0-$2500, $2,500–8,500, 8,500-$14,000, $14,000-$20,500, $20,500-$30,000, $30,000-$42,500, $42,500-$62,500, 62,500-$75,000, and $75,000+. The income category midpoint was chosen as the participant’s income for each given exam year.16,17 All incomes in the top (highest) open ended bracket were coded as $75,000.
Primary Economic Predictors
Income Volatility:
To account for inflation between 1990 and 2005, we deflated all nominal dollars into real 1990 dollars using the consumer price index for each corresponding year.18 We defined income volatility, as the intra-individual standard deviation (SD) of the percent change in inflation-adjusted income from 1990–2005.4 To do so, we calculated, for each participant, the percent change in inflation-adjusted income between every two consecutive exam years as [(Yt2-Yt1)/ 0.5(Yt1+Yt2)] x 100. If a participant was missing an income measure for a given exam year, the income measure at the next available visit was used. Then, for each participant, we calculated the SD of those percent changes. Income volatility, in percentage points, was then categorized into tertiles of “low volatility” (SD=0%−21% change), “medium volatility” (SD=22%−51% change), and “high volatility” (SD=52%−242% change).
Number of income drops:
Because volatility may capture both positive and negative income changes, we also measured the number of income drops. An income drop was defined as a decrease of 25% or more in income, compared to the previous study visit’s income, and less than the participant’s average income from 1990 to 2005. Given that inflation alone could result in a 25% income drop for some categories but not others, for this measure we did not adjust income for inflation. The number of those drops between 1990 and 2005 (range 0–3) was the predictor of interest and was categorized into ‘0’, ‘1’, or ‘2 or more’ drops.
Secondary Economic Predictors:
Income trajectory:
To help further distinguish the directionality of income volatility (i.e. positive, negative, or both), we created an income trajectory measure with four mutually exclusive groups corresponding to income measures from 1990 to 2005: 1) no income changes, 2) at least one income increase with no decreases, 3) fluctuating income (at least one income increase and decrease), or 4) at least one income decrease with no increases. Income trajectory groups 1 and 2 (no income change/increase only) were then combined due to the small sample size of the ‘no income change’ group.
Large income changes:
To characterize absolute changes in income and also to examine large income changes, we created a measure of large income changes, which we defined as an income drop (decrease) or income jump (increase) from the prior visit that was greater than $20,000. We chose $20,000 as it was a minimal threshold value that defined at least a two category income change at any income level – for example, at the lowest income a $20,000 increase represents a three category income jump, at higher income categories this represents a two category income jump. Large income changes was then categorized into four mutually exclusive groups: 1) no large income changes, 2) at least one large income increase with no large decrease, 3) large fluctuating income (at least one large income increase and decrease), or 4) at least one large income decrease with no large increase.
Measurement of Outcomes between 2005 and 2015
CVD:
Fatal and non-fatal CVD events related to both coronary heart disease, cerebrovascular disease, and other heart or vascular diseases, specifically fatal and nonfatal myocardial infarction, acute coronary syndrome, stroke, transient ischemic attack, hospitalization for heart failure, intervention for peripheral arterial disease, or death from cardiovascular causes were included.
All-cause mortality:
If a participant could not be contacted, study personnel reviewed several databases including the national death index to obtain the vital status of a study participant, in addition to contacting friends and family members. If a participant was identified as deceased, study personnel requested death certificates and/or autopsy reports, which were reviewed by the endpoints committee.
Possible events were obtained through collection of study participant medical records (i.e. hospital discharge summaries, hospital stay International Classification of Disease codes, and documents for specific cases such as chest pain, possible MI), as well as death certificates. Records were first reviewed by a nurse reviewer/abstractor to first rule out obvious non-CVD or death events. Any potential events recorded during this step were then forwarded to an adjudication panel of CARDIA study physicians for verification, according to the CARDIA study manual of operations.19 Incident CVD (fatal and non-fatal) and death events were ascertained through August 31, 2015.
Measurement of other Covariates
At baseline in 1990, all CARDIA participants reported age at enrollment, race, sex, years of education completed, employment status (unemployed vs. employed), number of individuals living in the household, marital status, and health insurance status (not collected until 1992). Also at baseline in 1990, smoking status (defined as never, current, and former), alcohol consumption (yes/no), and physical activity were ascertained by interview at each study examination. Total physical activity in exercise units was calculated using reports of the amount of time per week spent in 13 categories of physical activity over the past year. Symptoms of depression were assessed using the 20-item Center for Epidemiologic Studies Depression Scale (CES-D; range 0 to 60).20 Blood pressure was measured while seated using a mercury sphygmomanometer. Glucose levels (not collected until 1992 and measured in mg/dl), total cholesterol (mg/dl), and HDL cholesterol (mg/dl) were measured from fasting blood draws. BMI was calculated as weight in kilograms divided by height in meters squared (kg/meters2).
For categorical covariates which could vary over time, including unemployment, marital status, health insurance status, smoking, and alcohol consumption, we also calculated cumulative measures from 1990–2005. Participants were coded as always, sometimes, or never having the condition or behavior from 1990–2005 (e.g. always, sometimes, or never married from 1990–2005). For continuous covariates including: number of individuals in the household, physical activity, BMI, fasting glucose, total cholesterol, HDL cholesterol, and depressive symptoms, we calculated the average for each of these measures from 1990 to 2005.
Statistical Analysis
At least three of five possible income measurements between 1990 and 2005 were required for inclusion in the analytical sample, and a total of 4,033 participants met this criteria. For the CVD analysis, we further excluded individuals censored (n=41) or with a CVD event (n=79) prior to 2005. For the mortality analysis, we further excluded 65 participants who died prior to the 2005 visit. A total of 3,977 participants were included in either the CVD (n=3,913) or the mortality analyses (n=3,968), and we presented their baseline characteristics in 1990 across categories of income volatility and number of income drops.
We calculated incidence density rates of CVD and all-cause mortality (per 1000 person-years) by category of economic predictor. We also graphically illustrated the risk (cumulative incidence) of CVD and all-cause mortality by category of economic predictor. The excess risk of CVD or all-cause mortality was defined as the risk difference among those with medium or high volatility (vs. low volatility) and among those with 1 or 2+ income drops (vs. no drops).
Participants contributed observed time at risk beginning July 1st 2005. Time was considered as study year and accordingly an entry point (year 2005) and an ending point (year of a CVD event or death or censoring) were modeled. Participants without a CVD event or death by the end of study period were right censored at the latest known 2015 exam date. After verifying that the proportional hazards assumption was met, a series of four Cox proportional hazards models were used to estimate the risk of CVD or mortality according to our primary economic predictors (income volatility and number of income drops). Model 1 was unadjusted. Model 2 adjusted for year 1990: sociodemographic factors (age, sex, years of education, race, marital status, number of people in the household, health insurance in 1992 and study site). Model 3 additionally adjusted for 1990 behavioral and comorbid conditions (BMI, smoking, alcohol, physical activity, systolic blood pressure, total cholesterol, HDL cholesterol, fasting glucose (year 1992), and depressive symptoms). Finally, model 4 additionally adjusted for 1990 income and unemployment status. Non-parametric fully-adjusted survival curves based on model 4 were graphed. In a sensitivity analysis, we repeated all Cox-proportional hazards regression models adjusting for cumulative covariates from 1990 to 2005. Additionally, we repeated all-Cox proportional hazards regression analyses using our secondary economic predictors (income trajectories and large income changes). Analyses were conducted using SAS version 9.4.21
Results
Participants with high income volatility were more likely to be black, female, have less than a high school education, be unemployed, be unmarried, and more likely to be current smokers and have elevated depressive symptoms (Table 1). Similar distributions are observed across categories of income drops.
Table 1:
Characteristics of study participants across tertiles of income volatility and number of income drops, CARDIA study, 1990.
| Tertile of Income Volatility |
Number of Income Drops |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| Overall | Low (n=1,325) |
Medium (n=1,326) |
High (n=1,326) |
Trend P- value |
0 (n=2,356) |
1 (n=1,365) |
2+ (n=256) |
Trend p-value |
|
| Age | 30.0 (3.6) | 31.0 (3.1) | 29.9 (3.7) | 29.2 (3.8) | <0.01 | 30.2 (3.5) | 29.7 (3.8) | 30.0 (3.9) | <0.01 |
| Black, n (%) | 1,894 (47.6) | 458 (34.6) | 624 (47.1) | 812 (61.2) | <0.01 | 979 (41.6) | 767 (56.2) | 148 (57.8) | <0.01 |
| Female, n (%) | 2,236 (56.2) | 711 (53.7) | 741 (55.9) | 784 (59.1) | <0.01 | 1278 (54.4) | 804 (58.9) | 150 (58.6) | 0.01 |
| < High school, n (%) | 209 (5.3) | 23 (1.7) | 47 (3.54) | 139 (10.5) | <0.01 | 79 (3.4) | 97 (7.1) | 33 (12.9) | <0.01 |
| Unemployed, n (%) | 629 (15.8) | 104 (7.9) | 175 (13.2) | 350 (26.4) | <0.01 | 299 (12.7) | 253 (18.5) | 77 (30.1) | <0.01 |
| Married, n (%) | 1,578 (39.7) | 765 (57.7) | 507 (38.2) | 306 (23.1) | <0.01 | 1,034 (43.9) | 461 (33.8) | 83 (32.4) | <0.01 |
| Household number | 2.9 (1.5) | 2.8 (1.3) | 2.9 (1.6) | 3.1 (1.7) | <0.01 | 2.8 (1.4) | 3.1 (1.6) | 3.4 (1.8) | <0.01 |
| Income, $ | $35,635 (21,423) | $49,824 (20,739) | $32,276 (16,140) | $24,603 (18,720) | <0.01 | $37,552 (22,556) | $32,297 (19,216) | $35,913 (19,858) | <0.01 |
| *Health insurance, n (%) | 3,367 (84.7) | 1,212 (91.2) | 1,142 (86.1) | 1,013 (76.4) | <0.01 | 2,051 (87.1) | 1,122 (82.2) | 194 (75.8) | <0.01 |
| BMI, kg/m2 | 26.1 (5.8) | 25.7 (5.2) | 26.2 (5.8) | 26.5 (6.4) | <0.01 | 25.8 (5.5) | 26.6 (6.3) | 27.0 (6.6) | <0.01 |
| Physical activity, exercise units | 378.3 (291.6) | 389.3 (286.0) | 381.8 (302.9) | 362.1 (284.7) | 0.02 | 383.1 (291.9) | 372.3 (294.3) | 359.2 (272.0) | 0.13 |
| Current smoking n (%) | 1,026 (25.8) | 243 (18.3) | 314 (23.7) | 469 (35.4) | <0.01 | 499 (21.2) | 427 (31.3) | 100 (39.1) | <0.01 |
| Current drinker, n (%) | 3,166 (79.6) | 1,113 (84.0) | 1,046 (78.9) | 1,007 (76.1) | <0.01 | 1,903 (80.8) | 1,062 (77.8) | 201 (78.5) | <0.01 |
| Systolic BP, mmHg | 107.6 (11.4) | 106.6 (10.8) | 107.4 (11.1) | 108.7 (12.2) | <0.01 | 107.0 (10.9) | 108.4 (12.1) | 108.3 (12.4) | <0.01 |
| HDL cholesterol, mg/dL | 53.4 (14.0) | 53.4 (13.8) | 52.6 (13.7) | 54.4 (14.5) | 0.07 | 53.4 (13.9) | 53.4 (14.1) | 53.7 (15.0) | 0.94 |
| Fasting glucose, mg/dLa | 91.4 (15.6) | 91.0 (10.9) | 91.8 (16.8) | 91.5 (18.1) | 0.42 | 91.2 (13.1) | 91.6 (15.6) | 92.8 (29.3) | 0.12 |
| Total cholesterol, mg/dL | 178.0 (33.7) | 179.8 (32.9) | 178.2 (34.2) | 175.9 (34.0) | <0.01 | 178.3 (33.4) | 177.5 (34.4) | 177.6 (32.9) | 0.55 |
| CES-D score ≥ 16, n (%) | 891 (22.4) | 201 (15.2) | 280 (21.1) | 410 (30.9) | <0.01 | 430 (18.3) | 378 (27.7) | 83 (32.4) | <0.01 |
Abbreviations: BMI: Body Mass Index; CARDIA: Coronary Artery Risk Development in Young Adults; CES-D: Center for Epidemiological Studies Depression Scale
Data are presented as mean (SD) unless otherwise noted
health insurance and fasting glucose information was not collected in 1990; these rows represents health insurance and glucose in 1992 (the following visit)
Adults with the highest income volatility were more likely to have more income drops, fluctuating income trajectories, and large fluctuating income changes (Supplemental Table 1).
A total of 106 incident CVD events and 164 deaths occurred between 2005 and 2015 for an overall CVD and death incidence rate of 2.76 and 3.66 per 1,000 PYs at risk, respectively (Table 2). The incidence rates for CVD and all-cause mortality were higher (p for trends < 0.01) with higher income volatility and greater number of income drops. For example, the incidence rate of death was more than two times higher among persons with high income volatility (IR=5.28/1,000 PYs) compared to low income volatility (IR=2.12/1,000 PYs), p for trend < 0.01.
Table 2.
Incidence of cardiovascular disease events and all-cause mortality (2005–2015) across categories of income volatility and number of income drops, CARDIA study.
| Cardiovascular disease |
All-cause mortality |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | Number of Events |
Person- years |
IR* (95% CI) |
IRD* (95% CI) |
N | Number of Events |
Person- years |
IR* (95% CI) |
IRD* (95% CI) |
|
| Overall | 3,913 | 106 | 38,402 | 2.76 (2.23, 3.29) |
- | 3,968 | 164 | 44,783 | 3.66 (3.10, 4.22) |
- |
| Tertile of Income volatility | ||||||||||
| Low | 1,303 | 22 | 12,916 | 1.70 (0.99, 2.41) |
ref | 1,323 | 32 | 15,076 | 2.12 (1.39, 2.86) |
ref |
| Medium | 1,306 | 29 | 12,894 | 2.25 (1.43, 3.07) |
0.55 (−0.54, 1.63) |
1,322 | 54 | 14,932 | 3.62 (2.65, 4.58) |
1.49 (0.28, 2.71) |
| High | 1,304 | 55 | 12,592 | 4.37 (3.21, 5.52) |
2.66 (1.31, 4.02) |
1,323 | 78 | 14,775 | 5.28 (4.11, 6.45) |
3.16 (1.77, 4.54) |
| Number of Income Drops | ||||||||||
| 0 | 2,326 | 44 | 22,984 | 1.91 (1.35, 2.48) |
ref | 2,352 | 79 | 26,649 | 2.96 (2.31, 3.62) |
ref |
| 1 | 1,339 | 47 | 13,064 | 3.60 (2.57, 4.63) |
1.68 (0.51, 2.86) |
1,361 | 61 | 15,336 | 3.98 (2.98, 4.98) |
1.01 (−0.18, 2.21) |
| 2+ | 248 | 15 | 2,354 | 6.37 (3.15, 9.60) |
4.46 (1.18, 7.73) |
255 | 24 | 2,798 | 8.58 (5.15, 12.01) |
5.61 (2.12, 9.11) |
Abbreviations: CARDIA: Coronary Artery Risk Development in Young Adults; CI: confidence interval; IR: incidence rate; IRD: incidence rate difference
Boldface indicates statistical significance, p < 0.05
P-values for trend analyses for income volatility and number of income drops with CVD and mortality were all significant, p <0.01
per 1,000 person years
From fully adjusted Cox proportional hazards models, those with high vs. low income volatility had significantly greater hazard of CVD (HR= 2.07, 95% CI=1.10, 3.90) and all-cause mortality (HR= 1.78, 95% CI=1.03, 3.09, Table 3). Similarly, compared to 0 income drops, those with 2+ income drops had significantly greater hazard of CVD (HR= 2.54, 95% CI=1.24, 5.19) and all-cause mortality (HR= 1.92, 95% CI=1.07, 3.44). Results from a sensitivity analysis adjusting for cumulative measures (from 1990 to 2005) of time-varying covariates were similar (Supplementary Table 2).
Table 3.
Multivariable adjusted Cox proportional hazards models of income volatility and number of income drops (1990–2005) with incident cardiovascular events and all-cause mortality (2005–2015), CARDIA study
| Cardiovascular Disease |
All-Cause Mortality |
|||||||
|---|---|---|---|---|---|---|---|---|
| Model 1 HR (95% CI) |
Model 2 HR (95% CI) |
Model 3 HR (95% CI) |
Model 4 HR (95% CI) |
Model 1 HR (95% CI) |
Model 2 HR (95% CI) |
Model 3 HR (95% CI) |
Model 4 HR (95% CI) |
|
| Tertiles of Income Volatility | ||||||||
| Low | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref |
| Medium | 1.32 (0.76, 2.30) |
1.29 (0.70, 2.38) |
1.13 (0.60, 2.15) |
1.03 (0.53, 1.99) |
1.43 (0.87, 2.34) |
1.24 (0.88, 1.76) |
1.53 (0.92, 2.57) |
1.38 (0.80, 2.38) |
| High |
2.57 (1.57, 4.22) |
2.32 (1.27, 4.25) |
2.30 (1.24, 4.25) |
2.07 (1.10, 3.90) |
2.23 (1.37, 3.64) |
2.51 (1.57, 4.00) |
2.14 (1.27, 3.61) |
1.78 (1.03, 3.09) |
| Number of Income Drops | ||||||||
| 0 | Ref | Ref | Ref | Ref | Ref | Ref | Ref | Ref |
| 1 |
1.88 (1.25, 2.84) |
1.58 (0.99, 5.25) |
1.44 (0.89, 2.34) |
1.43 (0.87, 2.33) |
1.34 (0.96, 1.87) |
1.10 (0.74, 1.62) |
0.94 (0.62, 1.42) |
0.92 (0.61, 1.40) |
| 2+ |
3.35 (1.87, 6.03) |
2.62 (1.31, 5.25) |
2.70 (1.34, 5.43) |
2.54 (1.24, 5.19) |
2.90 (1.83, 4.57) |
2.39 (1.41, 4.06) |
2.07 (1.19, 3.61) |
1.92 (1.07, 3.44) |
Abbreviations: CARDIA: Coronary Artery Risk Development in Young Adults; HR: Hazard ratio.
Boldface indicates statistical significance, p < 0.05
Model 1 is unadjusted; model 2 is adjusted for 1990 age, sex, race, less than a high school education, marital status, number of people in the household, 1992 health insurance status, and study site; model 3 is additionally adjusted for 1990 BMI, systolic blood pressure, total cholesterol, HDL cholesterol, smoking, alcohol use, physical activity, elevated depressive symptoms, and 1992 fasting glucose; and model 4 is additionally adjusted for 1990 income and unemployment status
Excess risks of CVD and all-cause mortality associated with categories of income volatility and income drops are presented in Figure 1: compared to those with low income volatility or no income drops, there was a 3.48% and 6.05% excess risk of death events among those with high income volatility or with 2+ income drops, respectively. Similar patterns observed with CVD risk.
Figure 1:
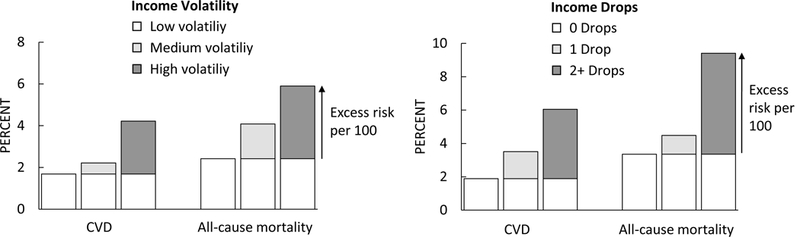
Cumulative incidence of cardiovascular disease and all-cause mortality associated with income volatility and number of income drops. Cumulative incidence was calculated by dividing the number of events (CVD or all-cause mortality) by the total number of participants within each category, and then multiplied by 100.
Fully adjusted survival curves are presented in Figure 2 and show that adults with higher income volatility and a greater number of income drops had worse CVD free survival (Panels A and B) and worse overall survival (Panels C and D).
Figure 2:
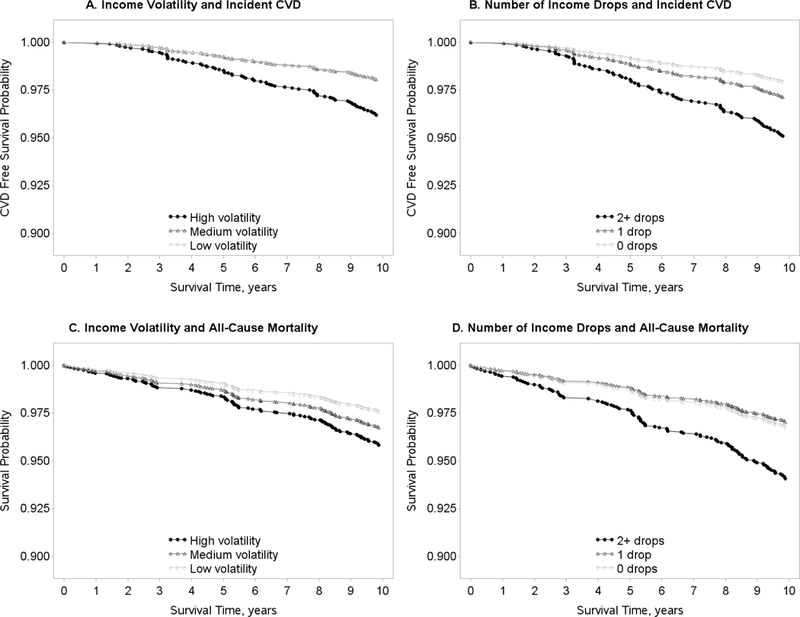
Adjusted survival curves for income volatility and number of income drops (1990 – 2005) with cardiovascular disease free survival and overall survival (2005 – 2015). All models are adjusted for 1990: age, sex, race, less than a high school education, marital status, number of people in the household, study site, BMI, systolic blood pressure, total cholesterol, HDL cholesterol, smoking, alcohol use, physical activity, elevated depressive symptoms, income, unemployment status, and 1992 fasting glucose and health insurance status. Panel A depicts the adjusted survival curve for the association between income volatility with CVD; Panel B depicts the adjusted survival curve for the association between the number of income drops with CVD; Panel C depicts the adjusted survival curve for the association between income volatility with all-cause mortality; Panel D depicts the adjusted survival curve for the association between the number of income drops with all-cause mortality.
Results from the sensitivity analysis using the secondary economic predictors (Supplementary Table 3), showed that compared to individuals whose income did not change or only increased from 1990–2005, those with income that fluctuated had greater hazard of CVD (HR: 1.71, 95% CI: 1.06, 2.74), from fully-adjusted Cox proportional hazard models. Compared to individuals without any large income changes from 1990–2005, those with at least 1 large income decrease (and no large income increases) had greater hazard of CVD (HR: 3.74, 95% CI: 1.83, 7.67) and all-cause mortality (HR: 2.47, 95% CI: 1.30, 4.69), from fully-adjusted models.
Discussion
Our findings support strong associations of income volatility and income drops with incident CVD and all-cause mortality in a relatively young cohort of white and black adults. Compared with low volatility or no income drops, high volatility or 2+ income drops over 15 years was associated with a two-fold risk of CVD and death in the subsequent 10 years. Our findings were consistent across our measures of overall income volatility as well as negative volatility, conceptualized as income drops. Our findings also reveal a clear graded relationship such that risk of CVD and all-cause mortality was greater with increased exposure to economic adversity, after accounting for multiple socioeconomic factors and cardiovascular risk factors. Taken together, these findings suggest that income volatility and income drops experienced in early to mid-adulthood are important independent predictors of CVD risk and overall mortality.
There are several pathways by which income volatility influences health outcomes. First, volatility implies episodes of lower income. In the current study, individuals in the highest volatility group indeed had the lowest baseline income. Low income is associated with an array of unhealthy behaviors22–25 such as alcohol use, smoking and inadequate physical activity which can act as mediating factors for CVD and all-cause mortality. Further, the protective benefit of social networks or coping resources26 developed by people with persistently low income, though the amount of such benefit may be arguable,27 may not be available to individuals with unpredictable and episodic low income. Stress is another mediating factor implicated in the relationship between income volatility and adverse health outcomes.28 For example, adverse health outcomes among individuals who experienced negative wealth shocks during the great depression, were found to be at least partially mediated by C-reactive protein,29 a measure of inflammation30 which is also associated with stress.31 Further, income volatility has been shown to be associated with increases in blood pressure29—which can also be induced by stress,32 all of which are associated with CVD28,33 and mortality.34,35
Though income volatility has previously received limited attention, there is growing evidence that it is associated with health outcomes. For example, a measure of the frequency of significant downward drops in income over a 10-year period was associated with psychological depression.8 A similar measure of downward volatility was found to be associated with decreased overall mental health scores in an Australian population.10 In a sample of adults living in Sweden, income decreases over a 5-year period were associated with a general measure of self-reported “poor” health.9 Additionally, downward income volatility measured in drops over 5 years was associated with all-cause mortality in a US sample from the Panel Study of Income Dynamics.11 More recently, in a representative sample of US adults ages 50+ years from the Health and Retirement Study (HRS), a loss of 75% of net-worth over a two year period was found to be associated with an increased risk of all-cause mortality.36 Our study findings add to those from the HRS study in a number of ways. First, compared to 25% of the HRS population experiencing a 75% loss of net-worth, income volatility (our primary predictor of interest) is more common and is likely representative of habitual changes in income, especially among young adults. For example, in our study sample, over 95% of participants had at least one income change (positive or negative), with at least 47% having at least one negative decrease. Further, our analysis focused on longer-term volatility rather than short-term shocks. Finally, the mean age of our study population was considerably younger which enabled us to study the association of income volatility in young adulthood, a period of peak earning years, with CVD and pre-mature mortality in mid-life.
However, there are some notable limitations. First, while the sample included participants from four different cities and both African Americans and Caucasians, additional research is needed to assess the associations of income volatility and health among other racial/ ethnic groups as well as rural Americans. Further, during our event follow-up time (2005 to 2015), most of our sample was still relatively young at ages 45–60, and therefore we were underpowered to test for important interactions by sex, race, or baseline socio-economic status (given the relatively small number of CVD and mortality events). Additionally, reverse causation may limit the interpretation of our findings. Any chronic conditions or illnesses may theoretically result or precipitate income changes. In an attempt to address this issue, we conducted a sensitivity analysis adjusting for cumulative covariates throughout the 1990–2005 income assessment period, and results were similar. The measurement of income in brackets rather than discreet numbers presents a major limitation and may have resulted in misclassification of our exposure and a loss of precision. For example, large income changes within income brackets were not detected. Likewise, small income changes occurring close to bracket thresholds could be detected as income category changes. Despite this, on average, such misclassification is likely to be non-differentially distributed across the study population, and therefore any potential impact on the effect size estimates would be biased towards the null. Finally, we acknowledge that income volatility in itself (as the SD of % income change) is on a relative scale and does not differentiate between positive or negative volatility. To address this pitfall, we conducted a series of additional analyses. First our analysis of income trajectories, to address directionality of income volatility, showed that compared to an income that did not change or only increased over 15 years, fluctuating income (income that both increased and decreased) was associated with increased risk of CVD – these results are in line with our main income volatility result. Second, in our analysis of large income changes, a measure of large ($20,000) absolute changes in income, we found that compared to individuals without any large income changes, having at least one large decrease in income over the study period was associated an over three fold hazard of CVD and an over two-fold hazard of all-cause mortality.
Despite these limitations, this study has several strengths and contributes to scarce literature on the relationship between income volatility, CVD and all-cause mortality in several ways. First, we built upon previous literature by using recent income data in a young and bi-racial cohort. The repeated income data in the CARDIA study population (from as early as young adulthood), provide a unique opportunity to capture cumulative socio-economic status and reflect upon how such economic instability influences health. Second, with a long follow up period for both exposure (15 years) and outcome (10 years), this study allowed us to assess a 25-year period of these participants’ lives, at an age where most adults are in the workforce. We were able to preserve clear temporal order by using income volatility during the first 15 years of follow-up to predict CVD and mortality in the subsequent decade. Fourth, while it is possible that other socioeconomic, behavioral and CVD risk factors could have influenced our results, our findings were only moderately attenuated after adjustment for some pertinent behavioral and cardiovascular risk factors cumulatively from 1990–2005. Finally, because the CARDIA study focuses specifically on CVD risks, the outcome adjudication process was designed to ensure the accuracy of outcome ascertainment.
In summary, the findings of this study reinforce the urgency and growing public health threat associated with income volatility in the U.S. Our findings show high vs. low income volatility from 1990 through 2005 is associated with a near two-fold risk of CVD and all-cause mortality in the subsequent 10 years. Given the current economic environment of increasing income instability,4–6 understanding how income volatility is associated with health has become increasingly important. Future studies focused on understanding mechanisms underlying the association between income volatility with CVD and mortality are warranted.
Supplementary Material
Clinical Perspective.
What is new?
From young adulthood through midlife, most individuals experience at least some increases in income; with almost half experiencing at least some decreases in income.
Income volatility (or fluctuating income) is more common among individuals who experience drops in income.
Income volatility and income drops throughout young adulthood are associated with an increased risk of cardiovascular disease and all-cause mortality.
What are the clinical implications?
Individuals experiencing income volatility may be at increased risk of CVD and may subsequently be a high priority group for CVD screening and interventions in a clinical setting.
It is likely that there are specific psychosocial and biologic pathways through which income volatility is associated with CVD and premature mortality.
Further research should focus on better understanding these pathways, so that modifiable preventive targets can be identified.
Acknowledgments
Sources of Funding
Funding for this study was supported in part by a grant from the NIH, National Institute on Aging (K01AG047273) and a grant from the American Heart Association (17POST32490000). The Coronary Artery Risk Development in Young Adults Study (CARDIA) is supported by contracts HHSN268201300025C, HHSN268201300026C, HHSN268201300027C, HHSN268201300028C, HHSN268201300029C, and HHSN268200900041C from the National Heart, Lung, and Blood Institute and the Intramural Research Program of the National Institute on Aging.
Footnotes
Disclosures:
The authors report no conflicts of interest or relevant disclosures.
References
- 1.Heathcote J, Perri F, Violante GL. Unequal we stand: An empirical analysis of economic inequality in the United States, 1967–2006. Rev Econ Dyn. 2010;13:15–51. [Google Scholar]
- 2.Duncan GJ. Income dynamics and health. Int J Health Serv. 1996;26:419–444. [DOI] [PubMed] [Google Scholar]
- 3.Matthews KA, Kiefe CI, Lewis CE, Liu K, Sidney S, Yunis C. Socioeconomic trajectories and incident hypertension in a biracial cohort of young adults. Hypertension. 2002;39:772–776. [DOI] [PubMed] [Google Scholar]
- 4.Dynan K, Elmendorf D, Sichel D. The evolution of household income volatility. The BE Journal of Economic Analysis & Policy. 2012;12:1935–1682. [Google Scholar]
- 5.Hardy B Income instability and the response of the safety net. Contemp Econ Policy. 2017;35:312–330. [Google Scholar]
- 6.Basu S Income Volatility: A Preventable Public Health Threat. Am J Public Health. 2017;107:1898–1899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Morduch J, Schneider R. The Financial Diaries: How American Families Cope in a World of Uncertainty. Princeton, NJ: Princeton University Press; 2017. [Google Scholar]
- 8.Prause J, Dooley D, Huh J. Income Volatility and Psychological Depression. Am J Community Psychol. 2009;43:57–70. [DOI] [PubMed] [Google Scholar]
- 9.Miething A, Aberg Yngwe M. Stability and variability in income position over time: exploring their role in self-rated health in Swedish survey data. BMC Public Health. December 18 2014;14:1300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rohde N, Tang KK, Osberg L, Rao P. The effect of economic insecurity on mental health: Recent evidence from Australian panel data. Soc Sci Med. 2016;151:250–258. [DOI] [PubMed] [Google Scholar]
- 11.McDonough P, Duncan GJ, Williams D, House J. Income dynamics and adult mortality in the United States, 1972 through 1989. Am J Public Health. September 1997;87:1476–1483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bartfeld J, Gundersen C, Smeeding T, Ziliak J. SNAP Matters: How Food Stamps Affect Health and Well-Being. . 1st ed. Stanford, CA: Stanford University Press; 2015. [Google Scholar]
- 13.Beydoun MA, Beydoun HA, Mode N, Dore GA, Canas JA, Eid SM, Zonderman AB. Racial disparities in adult all-cause and cause-specific mortality among us adults: mediating and moderating factors. BMC Public Health. 2016;16:1113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.de Mestral C, Stringhini S. Socioeconomic Status and Cardiovascular Disease: an Update. Curr Cardiol Rep 2017;19:115. [DOI] [PubMed] [Google Scholar]
- 15.Friedman GD, Cutter GR, Donahue RP, Hughes GH, Hulley SB, Jacobs DR Jr, Liu K, Savage PJ. CARDIA: study design, recruitment, and some characteristics of the examined subjects. J Clin Epidemiol. 1988;41:1105–1116. [DOI] [PubMed] [Google Scholar]
- 16.Elfassy T, Glymour MM, Kershaw KN, Carnethon M, Llabre MM, Lewis CE, Schneiderman N, Zeki Al Hazzouri A. Association Between Sustained Poverty and Changes in Body Mass Index From 1990 to 2015: The Coronary Artery Risk Development in Young Adults Study. Am J Epidemiol. 2018;187:1240–1249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zeki Al Hazzouri A, Elfassy T, Sidney S, Jacobs D, Perez Stable EJ, Yaffe K. Sustained Economic Hardship and Cognitive Function: The Coronary Artery Risk Development in Young Adults Study. Am J of Prev Med. 2017;52:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.US Department of Labor. Consumer Price Iindex Inflation Calculator. 2017; https://www.bls.gov/data/inflation_calculator.htm. Accessed December 21 2017.
- 19.CARDIA Endpoint Events Manual of Operations. 2015; http://www.cardia.dopm.uab.edu/images/more/recent/CARDIA_Endpoint_Events_MOO_v03_20_2015.pdf. Accessed December 21, 2017.
- 20.Radloff L The CES-D scale: A self-report depression scale for research in the general population. Appl Psychol Meas 1977;1:385–401. [Google Scholar]
- 21.SAS Software [computer program]. Cary, NC, USA: SAS Institute Inc.; 2012. [Google Scholar]
- 22.Lynch JW, Kaplan GA, Salonen JT. Why do poor people behave poorly? Variation in adult health behaviours and psychosocial characteristics by stages of the socioeconomic lifecourse. Soc Sci Med 1997;44:809–819. [DOI] [PubMed] [Google Scholar]
- 23.Moore LV, Diez Roux AV, Evenson KR, McGinn AP, Brines SJ. Availability of recreational resources in minority and low socioeconomic status areas. Am J Prev Med. 2008;34:16–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yang S, Lynch JW, Raghunathan TE, Kauhanen J, Salonen JT, Kaplan GA. Socioeconomic and psychosocial exposures across the life course and binge drinking in adulthood: population-based study. Am J Epidemiol. 2007;165:184–193. [DOI] [PubMed] [Google Scholar]
- 25.Marmot M The influence of income on health: views of an epidemiologist. Health Aff. 2002;21:31–46. [DOI] [PubMed] [Google Scholar]
- 26.Berkman LF, Syme SL. Social networks, host resistance, and mortality: a nine-year follow-up study of Alameda County residents. Am J Epidemiol. 1979;109:186–204. [DOI] [PubMed] [Google Scholar]
- 27.Dercon S Income Risk, Coping Strategies, and Safety Nets. World Bank Res Obs. 2002;17:141–166. [Google Scholar]
- 28.Hamer M, Molloy GJ, Stamatakis E. Psychological distress as a risk factor for cardiovascular events: pathophysiological and behavioral mechanisms. J Am Coll Cardiol. 2008;52:2156–2162. [DOI] [PubMed] [Google Scholar]
- 29.Boen C, Yang YC. The physiological impacts of wealth shocks in late life: Evidence from the Great Recession. Soc Sci Med 2016;150:221–230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Fortmann SP, Ford E, Criqui MH,Folsom AR, Harris TB, Hong Y, Pearson TA, Siscovick D, Vinicor F, Wilson PF, CDC, AHA. CDC/AHA Workshop on Markers of Inflammation and Cardiovascular Disease: Application to Clinical and Public Health Practice: report from the population science discussion group. Circulation. 2004;110:e554–559. [DOI] [PubMed] [Google Scholar]
- 31.Hamer M, Gibson EL, Vuononvirta R, Williams E, Steptoe A. Inflammatory and hemostatic responses to repeated mental stress: individual stability and habituation over time. Brain Behav Immun. 2006;20:456–459. [DOI] [PubMed] [Google Scholar]
- 32.Matthews KA, Katholi CR, McCreath H, Whooley MA, Williams DR, Zhu S, Markovitz JH. Blood pressure reactivity to psychological stress predicts hypertension in the CARDIA study. Circulation. 2004;110:74–78. [DOI] [PubMed] [Google Scholar]
- 33.Lagrand WK, Visser CA, Hermens WT, Niessen HW, Verheught FW, Wolbink GJ, Hack CE. C-reactive protein as a cardiovascular risk factor: more than an epiphenomenon? Circulation. 1999;100:96–102. [DOI] [PubMed] [Google Scholar]
- 34.Taylor BC, Wilt TJ, Welch HG. Impact of Diastolic and Systolic Blood Pressure on Mortality: Implications for the Definition of “Normal”. J Gen Intern Med. 2011;26:685–690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Chesney E, Goodwin GM, Fazel S. Risks of all-cause and suicide mortality in mental disorders: a meta-review. World Psychiatry. 2014;13:153–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Pool LR, Burgard SA, Needham BL, Elliott MR, Langa KM, Mendes de Leon CF. Association of a Negative Wealth Shock With All-Cause Mortality in Middle-aged and Older Adults in the United States. JAMA. 2018;319:1341–1350. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


