Abstract
Purpose:
Conduct an individual-level analysis of hospital utilization during the first year of life to test the hypothesis that community material deprivation increases healthcare utilization.
Methods:
We used a population-based perinatal data repository based on linkage of electronic health records (EHR) from regional delivery hospitals to subsequent hospital utilizations at the region’s only dedicated children’s hospital. Zero-inflated Poisson and Cox proportional hazards regression models were used to quantify the causal role of a census tract based deprivation index on the total number, length, and time until hospital utilizations during the first year of life.
Results:
After adjusting for any neonatal intensive care unit (NICU) admission, chronic complex conditions, race and ethnicity, insurance status, birth season, and very low birth weight we found that a 10% increase in the deprivation index caused a 1.032 fold increase (95% CI: [1.025, 1.040]) in post initial hospitalization length of stay, a 1.011 fold increase (95% CI: [1.002, 1.021]) in number of post initial hospital encounters, and 1.022 fold increase (95% CI: [1.009, 1.035]) in hazard for hospitalization utilization during the first year of life.
Conclusions:
Interventions designed to reduce material deprivation and income inequalities could significantly reduce infant hospital utilization.
Keywords: infant, socioeconomic factors, hospitalization, electronic health records
Introduction
Emergency department (ED) utilization and hospital admission among infants represents a substantial cost and strain on limited healthcare resources (Underwood, 2007). Previous analyses have identified gestational age at birth to be a significant predictor for hospital utilization after the initial birth encounter (Escobar, 2005; Jain, 2006; Ray, 2013; Goyal, 2015). Besides biomarkers like gestational age or birth weight, studies have identified community-level and environmental factors associated with health outcomes during the first year of life, including risk for preterm birth and stillbirth (DeFranco, 2015; DeFranco, 2016; Hall, 2014). Analyses have also detected community factors associated with higher utilization of hospital resources including ED services (Beck, 2014). However, the contribution of community factors independent of individual socioeconomic status to the variability in hospital utilization during the first year of life has not been examined.
The Maternal and Infant Data Hub (MIDH), a population-based, perinatal data repository based in Cincinnati, Ohio provides a unique opportunity to analyze infant hospital utilization patterns (Hall, 2017). The MIDH captures hospital encounters occurring throughout the region including inpatient newborn care from each of the region’s delivery hospitals as well as subsequent inpatient hospitalizations, ED, or urgent care (UC) encounters at the region’s children’s hospital, Cincinnati Children’s Hospital Medical Center (CCHMC). The MIDH integrates electronic health record (EHR) data from each of these encounters and enables linkage to ancillary data sets including area-level census measures, individual-level vital statistics, and patient registry data.
Our objective was to conduct a retrospective, individual-level analysis of hospital utilization, including inpatient stays and ED or UC visits during the first year of life, to test the hypothesis that community material deprivation increases healthcare utilization including ED/UC encounters and hospital admissions.
Methods
Study Population
We created a county-wide population cohort by using births occurring between 2013 and 2015 in Hamilton County Ohio, the county in which Cincinnati and CCHMC are located. Hamilton County has about 190,000 children living across 222 urban, suburban, and rural census tracts. CCHMC is a 629-bed pediatric academic health center that has a market share of 99% of all hospital admissions and 81% of all hospital encounters among 0 – 14 year olds (Beck, 2018). Physicians employed by CCHMC provide neonatal clinical care throughout each of greater Cincinnati’s delivery hospitals, serving >80% of the region’s newborn infants. Physician billing records maintained by the CCHMC EHR system capture each encounter. These physician billing records are used as a core data set within the MIDH which also supports individual-level and area-level linkages to relevant health data sets including US census data, vital records, and more (Hall, 2017). Through linkage between physician billing records representing birth encounters and subsequent CCHMC hospitalization records, we gathered all inpatient hospitalizations and ED/UC encounters during the first year of life for our study population. Transfers from a normal newborn or special care nursery to any of the five regional neonatal intensive care units (NICUs) contributed to the initial hospitalization measures. The CCHMC Institutional Review Board approved this study and granted a waiver of informed consent.
Outcomes and Covariates
We used general linear models to evaluate the contribution of community deprivation on hospital utilization during the first year of life defined as (1) the length of stay (number of in-hospital days) for the initial birth hospital encounter (including transfers to a regional neonatal intensive care unit), (2) the cumulative length of stay for all post-initial hospital admissions, (3) the total number of post-initial encounters (ED, UC, or hospital readmission), and (4) the number of days from birth until the first subsequent encounter with the ED, UC, or related to a hospital admission). Residential addresses obtained during the initial birth encounter were geocoded using a custom TIGER/Line address range software package (Brokamp, 2018) and assigned to a corresponding census tract. Deprivation index values were assigned to each child based on their residential census tract. To adjust for confounding by individual-level factors, we used a causal inference approach (Keohane, 2009) and created a directed acyclic graph (Figure 3) to identify the set of variables that needed to be adjusted for to quantify the direct causal effect of community deprivation on hospital utilization during the first year of life. All models were adjusted for (1) the presence of any NICU admission during the initial birth encounter, (2) the presence of chronic complex conditions (CCC) based on ICD-10 codes as defined by the Pediatric CCC Classification System Version 2 (Feudtner, 2014), (3) race and ethnicity, (4) insurance status, (5) birth season, and (6) very low birth weight (defined as < 1500 g). Although environmental pollutants were identified as a confounder that required adjustment in the model, we did not have any measurements or estimations available and these were not included in our statistical models. Insurance status was used as a surrogate for individual-level socioeconomic status. See Table 1 for detailed levels of each categorical covariate.
Figure 3.
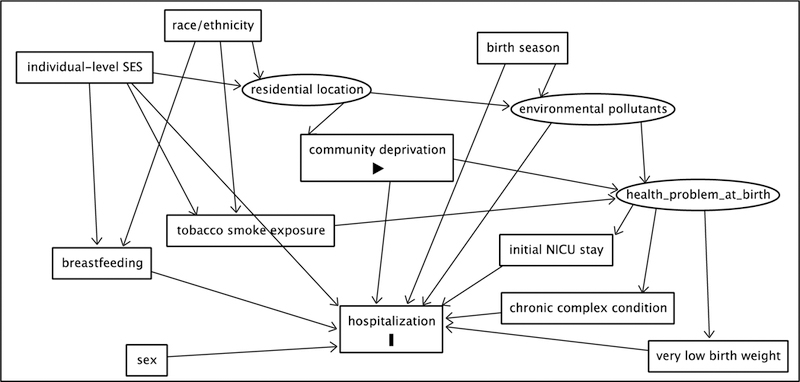
A directed acyclic graph developed as a part of our causal inference framework used for covariate selection in our statistical models. Here, the box labeled “community deprivation” is the exposure and the box labeled “hospitalization” is the outcome. Latent, unobservable, or unmeasured covariates are represented by ovals and other covariates are represented by rectangles.
Table 1.
Population demographics, characteristics and initial hospital utilization comparing patients with and without first year hospital utilization subsequent to initial newborn care. Table values represent either n (%) or median (25th percentile, 75th percentile). P-values are from either a chi-squared or Wilcoxon test comparing the difference in each measure between those who ever utilized the hospital and those who never utilized the hospital.
| Overall | Ever Utilized | Never Utilized | P-value | |
|---|---|---|---|---|
| N | 27,287 | 12,184 (44.7%) | 15,103 (55.3%) | |
| NICU Admission | 2,639 (9.7%) | 1,488 (12.2%) | 1,151 (7.6%) | < 0.001 |
| Complex Chronic Condition | 5,298 (19.4%) | 3,312 (27.2%) | 1,986 (13.1%) | < 0.001 |
| Very Low Birth Weight (< 1.5 kg) | 456 (1.7%) | 264 (2.2%) | 192 (1.3%) | < 0.001 |
| Season of Birth | 0.055 | |||
| Autumn | 6,679 (24.5%) | 3,039 (24.9%) | 3,640 (24.1%) | |
| Spring | 6,851 (25.1%) | 2,986 (24.5%) | 3,865 (25.6%) | |
| Summer | 7,219 (26.5%) | 3,186 (26.1%) | 4,033 (26.7%) | |
| Winter | 6,538 (24.0%) | 2,973 (24.4%) | 3,565 (23.6%) | |
| Gestational Age (weeks) | < 0.001 | |||
| < 27 | 141 (0.5%) | 67 (0.5%) | 74 (0.5%) | |
| 28 – 31 | 354 (1.3%) | 219 (1.8%) | 135 (0.9%) | |
| 32 – 33 | 345 (1.3%) | 188 (1.5%) | 157 (1.0%) | |
| 34 – 36 | 2,086 (7.6%) | 1,104 (9.1%) | 982 (6.5%) | |
| > 36 | 23,328 (85.5%) | 10,288 (84.4%) | 13,040 (86.3%) | |
| Unknown | 1,033 (3.8%) | 318 (2.6%) | 715 (4.7%) | |
| Insurance | < 0.001 | |||
| Private | 11,994 (44.0%) | 3,242 (26.6%) | 8,752 (57.9%) | |
| Public or Self-Pay | 15,193 (55.7%) | 8,876 (72.8%) | 6,317 (41.8%) | |
| Unknown | 100 (0.4%) | 66 (0.5%) | 34 (0.2%) | |
| Race/Ethnicity | ||||
| Black, non-Hispanic | 8,016 (29.4%) | 5,723 (47.0%) | 2,293 (15.2%) | < 0.001 |
| Black, Hispanic | 1,329 (4.9%) | 771 (6.3%) | 558 (3.7%) | |
| Other Race, non-Hispanic | 1,184 (4.3%) | 512 (4.2%) | 672 (4.4%) | |
| White, non-Hispanic | 9,186 (33.7%) | 3,732 (30.6%) | 5,454 (36.1%) | |
| Unknown | 7,572 (27.7%) | 1,446 (11.9%) | 6,126 (40.6%) | |
| Sex | < 0.001 | |||
| Female | 13,364 (49.0%) | 5,749 (47.2%) | 7,615 (50.4%) | |
| Male | 13,923 (51.0%) | 6,435 (52.8%) | 7,488 (49.6%) | |
| Birth Weight (kg) | 3.27 (2.91, 3.61) | 3.20 (2.84, 3.54) | 3.33 (2.98, 3.66) | < 0.001 |
| Deprivation Index | 0.38 (0.28, 0.5) | 0.42 (0.32, 0.58) | 0.34 (0.26, 0.44) | < 0.001 |
| Gestational Age | 39 (38, 40) | 39 (37,39) | 39 (38, 40) | < 0.001 |
| Length of stay during initial hospitalization | 3 (2, 3) | 3 (2, 4) | 2 (2, 3) | < 0.001 |
Deprivation Index
To quantify community deprivation for each residential birth address, we created a census-tract level deprivation index. Five different census tract level variables related to material deprivation and previously used in a 2010 deprivation index for Greater Cincinnati (Brokamp, 2016) were derived from the 2015 five-year American Community Survey (ACS) for all 2015 US census tracts: (1) the fraction of households with income in past 12 months below poverty level, (2) the median household income in the past 12 months in 2015 inflation-adjusted dollars, (3) the fraction of population 25 and older with educational attainment of at least high school graduation or GED equivalency, (4) the fraction of population with no health insurance coverage, (5) the fraction of households receiving public assistance income or food stamps or SNAP in the past 12 months, and (6) the fraction of houses that are vacant. Detailed methods are in the Supplementary Information. Briefly, we used principal components analysis (PCA) and selected the first principal component, which represented about 60% of the total variation in the census tract level measurements, to reduce them to a single index that ranges from 0 to 1, with higher values indicative of more material deprivation. An online repository containing the data and code used to reproduce the deprivation index is available at https://github.com/cole-brokamp/dep_index (Brokamp, 2018).
Statistical Analysis
Population characteristics were initially compared between those who ever utilized the hospital and those who never utilized the hospital using a chi-squared or Wilcoxon test, as appropriate. We used Poisson regression to model the length of stay for the initial birth hospital encounter, but used zero inflated Poisson (ZIP) regression models (Hilbe, 2011) for both the cumulative length of stay for all post-initial hospital encounters and for the total number of encounters. We opted for this analytic method given that a large fraction of individuals in the study population had no hospital encounters after their initial birth encounter. In both cases, we used a Vuong non-nested test (Vuong, 1989) to determine that a ZIP model was more appropriate than a Poisson regression model based on raw, AIC-corrected, and BIC-corrected criteria (p < 0.001). To deal with the excess zeros that the Poisson distribution cannot handle, the ZIP model assumes that counts come from a mixture of two distributions. Specifically, counts of zero come from a binary distribution that are mixed in with counts of non-negative integers. This is modeled as a combination of logistic regression for the zero counts and Poisson regression for the non-negative counts, giving both an odds ratio for always having zero counts and a risk ratio for the change in the non-negative counts.
A Cox proportional hazards model was used to model the days from birth until the first hospital encounter. Observations were right censored at one year of age if they did not have a utilization event during the first year of life. The proportional hazards assumption was verified by testing the correlation between the transformed time to event and scaled Shoenfeld residuals.
Each statistical model was fitted using only observations for which data on all model covariates was not missing. To test our assumption that race and ethnicity data was missing completely at random, we completed a sensitivity analysis where we imputed race through multivariate imputation by chained equations using all variables described in Table 1 and repeated our regression models for hospitalization length of stay and number of encounters as well as the Cox proportional hazards model for the time to first utilization event using only those children that were admitted.
To test the impact of our choice of considering hospital utilization as all encounters, rather than just those severe enough to be admitted to the hospital, we conducted a sensitivity analysis wherein we repeated our regression models for hospitalization length of stay and number of encounters as well as the Cox proportional hazards model for the time to first utilization event using only those children that were admitted.
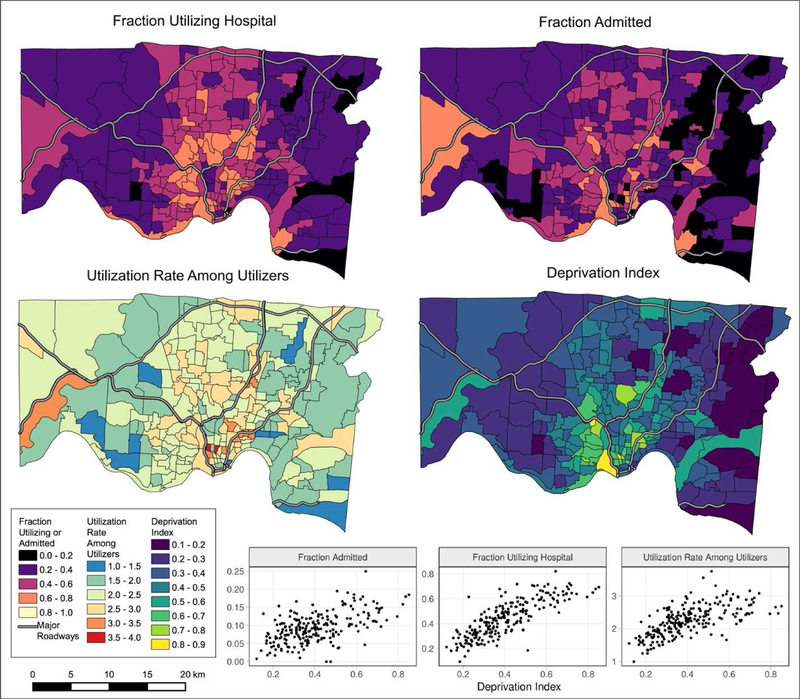
We created tract level “fraction utilizing hospital” and “fraction admitted” measures; each defined as the number of total children utilizing the ED/UC and admitted to the hospital, respectively, divided by the total number of MIDH birth records in each census tract. We also defined a census tract “utilization rate among utilizers” as the total number of hospital encounters divided by the number of children ever utilizing the hospital in each census tract. We created census tract level rate maps and corresponding scatter plots to visually examine the ecological association of deprivation index and each tract level outcome.
Statistical and geospatial computing was done with R (R Core Team, 2017) using the “pscl” package to implement zero inflated Poisson regression (Jackman, 2017; Zeileis, 2008), the “sf” package for geospatial calculations (Pebesma, 2018), and the “tmap” package for creating maps (Tennekes, 2017).
Results
Individual Summary and Comparison Across Hospital Utilization.
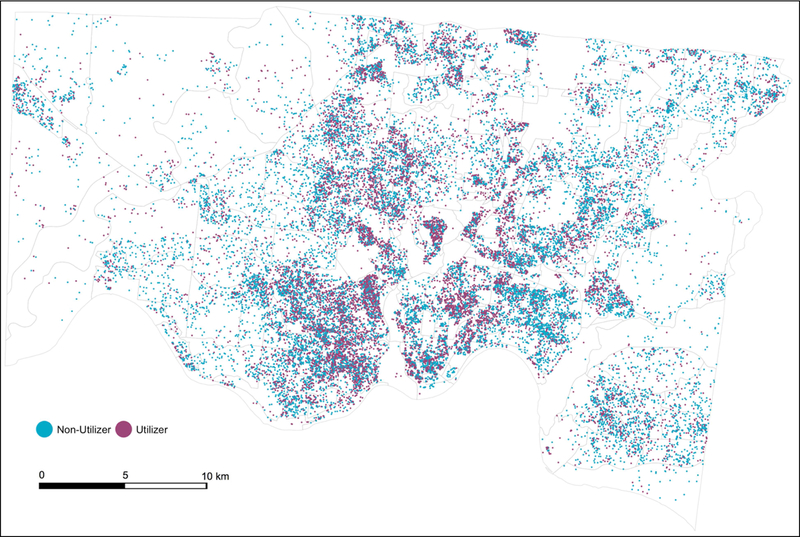
We obtained 53,452 billing records within the eight-county primary region surrounding CCHMC from 2013 to 2015. Of these, 27,287 had a precisely geocoded residential address located within Hamilton County, equivalent to 83% of the total 32,736 total reported births in Hamilton County from 2013 to 2015. The 17% of total births in Hamilton County that were not captured within the MIDH were either seen by non-CCHMC (private practice) pediatricians in the delivery hospital setting or were Hamilton county resident births born outside of the region. A total of 12,184 (44.7%) of all children had at least one subsequent, linked ED/UC utilization event or hospital admission within their first year of life. Overall, these children accounted for 28,702 unique encounters, equivalent to a utilization rate of 1.05 encounters per infant. Those that utilized the hospital at least once during their first year of life had an average of 2.36 total encounters, a median total length of stay of 2 days (IQR: [1, 4]) and a median time until first encounter of 117 days (IQR: [44, 223]). Figure 1 shows the geographic location of each birth (randomized within each census block to maintain privacy) within Hamilton County, colored by hospital utilization status during the first year of life.
Figure 1.
Dot density map of Hamilton County births from 2013 to 2015 with linked electronic health records. Each dot represents 1 birth and is colored per hospital utilization status during the first year of life. Dots are randomly jittered within each census block.
Table 1 summarizes individual characteristics of the cohort both overall and when stratified by hospital utilization during the first year of life. Overall, our study population was 51% male, 29.4% non-Hispanic black, 33.7% non-Hispanic white and 44% with private insurance. All characteristics in Table 1 except for season of birth significantly differed by hospital utilization status (p < 0.001), with utilizers having a higher prevalence of NICU admission at birth (12.2% versus 7.6%), higher prevalence of CCCs (27.2% versus 13.1%), higher prevalence of very low birth weight (2.2% versus 1.3%), lower prevalence of full term birth (84.4% versus 86.3%), lower usage of private insurance (26.6% versus 57.9%) compared to non-utilizers.
Deprivation Index and Census Tract Level Associations
The bottom left panel of Figure 2 shows the deprivation index for each census tract within Hamilton County, Ohio. Our study population had a median deprivation index of 0.38 and those who ever utilized the hospital during the first year of life after birth had a significantly higher median deprivation index compared to those that never utilized (0.42 versus 0.34, p < 0.001).
Figure 2.
Census tract level hospital utilization rates and the deprivation index. Scatter plots at the bottom illustrate the relationship between each of the utilization rates and the deprivation index at the census tract level.
We calculated the fraction of children in each tract that utilized and were admitted to the hospital at least once during their first year of life, as well as the rate of total utilizations among those that ever utilized. Figure 2 contains census tract maps of Hamilton County with each panel colored by the hospital utilization measures and the deprivation index. Scatter plots of the utilization measures according to the tract deprivation index (bottom right of Figure 2) showed relatively strong correlations significantly different from zero (p < 0.001). Specifically, the deprivation index had a Pearson correlation coefficient of 0.82 with the fraction of utilizers, 0.56 with the fraction of admissions, and 0.66 with the utilization rate among the utilizers.
Individual Level Assessment of the Role of Deprivation Index on Hospital Utilization
To assess the direct causal effect of community deprivation on the likelihood, length of stay, and time until post initial hospitalizations and hospital encounters, we used regression models that were adjusted for NICU admission, CCC, race and ethnicity, insurance status, birth season, and very low birth weight. Using a Poisson regression model, we found that a 0.1 unit increase in the deprivation index caused a 0.994 fold (95% CI: [0.990, 0.998]) change in the length of stay for the initial birth hospitalization. Although statistically significant, a 0.6% decreased length of stay equates to about 38 minutes and is likely not clinically meaningful. The logistic portion of our zero inflated Poisson regression models found that an increase of 0.1 in the deprivation index caused a relative decrease in the odds of having a zero number of hospital encounters (OR: 0.88, 95% CI: [0.86, 0.91]) and a zero length of stay for post-initial hospitalizations (OR: 0.90, 95% CI: [0.88, 0.93]). The Poisson portion of these models found that a 0.1 unit increase in the deprivation index caused a 1.011 fold (95% CI: [1.002, 1.021]) increase in the number of total hospital encounters and a 1.032 fold increase (95% CI: [1.025, 1.040]) in the total length of hospitalization. A Cox proportional hazards model showed that a 0.1 unit increase in the deprivation index caused a relative increase in the hazard for the first post-initial hospital utilization of 1.022 (95% CI: [1.009, 1.035]).
A total of 2,609 (9.6%) of all infants were admitted to CCHMC at least once during their first year of life after discharge from the birth hospital. Among this sub-group, infants were admitted an average of 3.26 times during the first year of life. As a sensitivity analysis, we repeated our regression models for hospitalization length of stay and number of encounters as well as the Cox proportional hazards model for the time to first utilization event using only those children that were admitted. We found similar results, with a 0.1 unit increase in the deprivation index corresponding to a 1.039 (95% CI: [1.029, 1.49]) fold increase for hospitalization LOS and a hazard ratio of 1.017 (95% CI: [0.989, 1.046]) for the time to first hospitalization. The number and percentage of missing data for race/ethnicity and gestational age are denoted as “Unknown” categories in Table 1. Because of the large amount of missing data, we conducted a sensitivity analysis in which we imputed race/ethnicity for the 28% of children in which it was missing. These results showed no meaningful differences compared to the complete case analysis and did not change our overall conclusions.
Discussion
Using a population-based cohort and statistical models adjusted for several individual confounders, we showed that increased community material deprivation during the first year of life contributes to (1) an increase in the likelihood and length of stay of post initial hospitalizations, (2) an increase in the likelihood and number of hospital encounters, and (3) a decreased time until first hospital utilization. Within our study period and population, the 25% most deprived census tracts (n = 56 of 222 total tracts) produced 25.5% (n = 6,947) of the total births, but were responsible for 39.8% (n = 11,414) of the total encounters and 40.7% (n = 17,918) of the total bed days spent in the hospital. Per the estimated incidence ratios from our models, reducing the median census tract deprivation of these 56 total census tracts from 0.61 to the median deprivation index of 0.33 for the remaining 166 census tracts would result in 1,287 fewer children ever utilizing the hospital and 405 fewer visits among those that did utilize the hospital.
Although numerous studies have identified the role of poverty on infant mortality (e.g., Woodbury, 1924) and low birth weight (e.g., Parker, 1994), few have studied its effect of hospital utilization. Guttmann (2004) used population-based survey data in Canada to show that low income adequacy was associated with hospitalization during the first two years of life, but mainly focused on single parenthood and maternal depression as the most significant causes. Beck (2018) used an ecological analysis to show that census tract-level poverty was associated with disparities in inpatient bed day rates across conditions and subspecialties among children in our study region, but stopped short of identifying causal or dose-response relationships. To our knowledge, this is the first study to adjust for individual level confounders to quantify the role of material community deprivation on hospital utilization in infants.
The MIDH provides our study with the unique strength of being able to prospectively follow nearly all children born in the county and track their hospital utilization, rather than starting with hospital utilizers based on EHRs and using census populations to derive rates. Furthermore, our prospective cohort study design at the individual-level allowed us to control for individual level confounders like race and socioeconomic status that would not have been possible with an ecological time-series study design using hospitalization rates. Our analysis was able to utilize records on 83% of all reported births in Hamilton County from 2013 – 2015, allowing us to minimize selection biases that are common in other cohort-based epidemiological studies, although this bias is still possible if the missingness was related to any of our confounders or outcomes, but we have no reason to believe this is the case.
As with all causal inference studies, unmeasured and unknown confounding is always a possibility; however, a strength of our study is that we used a causal inference framework and a directed acyclic graph to identify a set of confounders and we were able to adjust for all confounders except for environmental pollutants. As with nearly all EHR-based studies, the MIDH is limited to using insurance status to quantify individual-level SES and using this binary measure to capture the multi-dimensional nature of socioeconomic status could result in unmeasured confounding. In the future, we plan to supplement quantification of individual-level socioeconomic status with individual housing and parcel characteristics. Another limitation is that we relied on the residence at the time of birth to quantify community material deprivation and families could have moved to a different location or out of the study region completely during the first year of life. However, we have previously found that only 6.5% of a cohort of 762 children born in Cincinnati, Ohio moved during the first year of life and that these families tended to move to areas less than 2 miles away with a median decrease in their deprivation index of 7.2% (Brokamp, 2016). Finally, although race was missing on about 28% of the observations, this missingness was not related to the deprivation index and is due to individual physicians choosing to not report newborn race in the birth encounter billing record. Given that this missingness is not differential, it is only possible that our estimates could be biased towards the null and we could be underestimating the effect of community deprivation on risk of hospitalization during the first year of life. Furthermore, a sensitivity analysis in which we imputed race/ethnicity revealed no changes in our results or overall conclusions.
Although effect sizes that we found in our study (a 1.1% increase in number of total hospital encounters and a 3.2% increase in the total length of hospitalization per 0.1 unit increase in the deprivation index) might be perceived as small, the health effects are quite large given the ubiquitous exposure of community deprivation. Indeed, we calculated that equating the deprivation index of the top quarter of the most deprived census tracts to the median deprivation index of the remaining three quarters of census tracts would result in 1,287 fewer children ever utilizing the hospital and 405 fewer visits among those that did visit the hospital.
Based on our results, interventions designed to reduce material deprivation and income inequalities could reduce infant hospital utilization. Indeed, the earned income tax credit (EITC), a benefit designed to increase the income and reduce material deprivation for working people who have low to moderate income (Scholz, 1994), has been previously shown to improve child health (Chetty, 2011; Hoynes, 2015). Specifically, increasing the EITC by 10 percent reduced infant mortality by 23.2 per 100,000 (Arno, 2009) and increasing the EITC by $10,000 reduced the incidence of low birthweight births by 6.7 to 10.8 percent (Hamad, 2015; Strully, 2010). We have identified further benefits by showing that decreased material deprivation can reduce infant hospital utilization independently of low birthweight status. Future epidemiologic studies of hospital utilization could include community deprivation in their causal frameworks to further understand the role of community- and individual-level material deprivation within hospital utilization. Furthermore, the interaction between individual- and community-level deprivation could be an important determinant of hospital utilization and requires further research.
Supplementary Material
Acknowledgments
Funding: This work was supported by the National Institutes of Health [grant number 1K23AI112916]; National Center for Advancing Translational Sciences of the National Institutes of Health through the Center for Clinical and Translational Science and Training at the University of Cincinnati [5UL1TR001425-02]; and Cincinnati Children’s Hospital Medical Center, Cincinnati, OH.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Financial disclosure statement: The authors have no financial relationships relevant to this study to disclose.
Conflict of interest statement: The authors have no conflicts of interest to disclose.
References
- Arno PS, Sohler N, Viola D, Schechter C. Bringing health and social policy together: the case of the earned income tax credit. Journal of public health policy 2009. July 1;30(2):198–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AF, Huang B, Chundur R, Kahn RS. Housing code violation density associated with emergency department and hospital use by children with asthma. Health Aff (Millwood) 2014, 33(11): 1993–2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AF, Riley CL, Taylor S, Brokamp C, Kahn RS. Toward a Culture of Health in Hospitals: Pervasive population disparities in inpatient bed-day rates across conditions and subspecialties. Health Affairs 2018, In Press. [DOI] [PMC free article] [PubMed]
- Brokamp C, LeMasters GK, Ryan PH. Residential mobility impacts exposure assessment and community socioeconomic characteristics in longitudinal epidemiology studies. Journal of Exposure Science and Environmental Epidemiology 2016. June;26(4):428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brokamp C, Wolfe C, Lingren T, Harley J, Ryan P. Decentralized and Reproducible Geocoding and Characterization of Community and Environmental Exposures for Multi-Site Studies. Journal of American Medical Informatics Association 25(3). 309–314. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brokamp C (2018, January 3). cole-brokamp/dep_index v0.1 (Version v0.1). Zenodo 10.5281/zenodo.1134946. [DOI]
- Chetty R, Friedman JN, Rockoff JE. New evidence on the long-term impacts of tax credits. IRS Statistics of Income White Paper 2011. Nov.
- DeFranco E, Hall E, Hossain M, Chen A, Haynes EN, Jones D, et al. Air pollution and stillbirth risk: exposure to airborne particulate matter during pregnancy is associated with fetal death. PLoS One 2015, 10(3): e0120594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeFranco E, Moravec W, Xu F, Hall E, Hossain M, Haynes EN, et al. Exposure to airborne particulate matter during pregnancy is associated with preterm birth: a population-based cohort study. Environ Health 2016, 15(1): 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Escobar GJ, Greene JD, Hulac P, Kincannon E, Bischoff K, Gardner MN, et al. Rehospitalisation after birth hospitalisation: patterns among infants of all gestations. Arch Dis Child 2005, 90(2): 125–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feudtner C, Feinstein JA, Zhong W, Hall M, Dai D. Pediatric complex chronic conditions classification system version 2: updated for ICD-10 and complex medical technology dependence and transplantation. BMC Pediatr 2014, 14: 199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goyal NK, Folger AT, Hall ES, Ammerman RT, Van Ginkel JB, Pickler RS. Effects of home visiting and maternal mental health on use of the emergency department among late preterm infants. J Obstet Gynecol Neonatal Nurs 2015, 44(1): 135–144. [DOI] [PubMed] [Google Scholar]
- Guttmann A, Dick P, To T. Infant hospitalization and maternal depression, poverty and single parenthood–a population-based study. Child: care, health and development 2004. January 1;30(1):67–75. [DOI] [PubMed] [Google Scholar]
- Hall ES, Connolly N, Jones DE, DeFranco EA. Integrating public data sets for analysis of maternal airborne environmental exposures and stillbirth. AMIA Annu Symp Proc 2014, 2014: 599–605 [PMC free article] [PubMed] [Google Scholar]
- Hall ES, Greenberg JM, Muglia LJ, Divekar P, Zahner J, Gholap J, Leonard M, Marsolo K. Implementation of a Regional Perinatal Data Repository from Clinical and Billing Records. Maternal and child health journal 2017. December 23:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamad R, Rehkopf DH. Poverty, pregnancy, and birth outcomes: a study of the Earned Income Tax Credit. Paediatric and perinatal epidemiology 2015. September 1;29(5):444–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hilbe JM. Negative binomial regression Cambridge University Press; 2011. March 17. [Google Scholar]
- Hoynes H, Miller D, Simon D. Income, the earned income tax credit, and infant health. American Economic Journal: Economic Policy 2015. February;7(1):172–211. [Google Scholar]
- Jackman S (2017). pscl: Classes and Methods for R Developed in the Political Science Computational Laboratory United States Studies Centre, University of Sydney; Sydney, New South Wales, Australia: R package version 1.5.2. URL https://github.com/atahk/pscl/. [Google Scholar]
- Jain S, Cheng J. Emergency department visits and rehospitalizations in late preterm infants. Clin Perinatol 2006, 33(4): 935–945; abstract xi. [DOI] [PubMed] [Google Scholar]
- Keohane RO. Counterfactuals and Causal Inference: Methods and Principles for Social Research. Social Forces 2009;88(1):466–7. [Google Scholar]
- Parker JD, Schoendorf KC, Kiely JL. Associations between measures of socioeconomic status and low birth weight, small for gestational age, and premature delivery in the United States. Annals of epidemiology 1994. July 1;4(4):271–8. [DOI] [PubMed] [Google Scholar]
- Pebesma E (2018). sf: Simple Features for R. R package version 0.6–0 https://CRAN.R-project.org/package=sf
- R Core Team (2017). R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria: URL https://www.R-project.org/. [Google Scholar]
- Ray KN, Lorch SA. Hospitalization of Early Preterm, Late Preterm, and Term Infants During the First Year of Life by Gestational Age. Hospital Pediatrics 2013, 3(3): 194–203. [DOI] [PubMed] [Google Scholar]
- Scholz JK. The earned income tax credit: Participation, compliance, and antipoverty effectiveness. National tax journal 1994. March 1:63–87. [Google Scholar]
- Strully KW, Rehkopf DH, Xuan Z. Effects of prenatal poverty on infant health: state earned income tax credits and birth weight. American Sociological Review 2010. August;75(4):534–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tennekes M (2017). tmap: Thematic Maps. R package version 1.11 https://CRAN.R-project.org/package=tmap
- Underwood MA, Danielsen B, Gilbert WM. Cost, causes and rates of rehospitalization of preterm infants. J Perinatol 2007, 27(10): 614–619. [DOI] [PubMed] [Google Scholar]
- Vuong QH. Likelihood ratio tests for model selection and non-nested hypotheses. Econometrica: Journal of the Econometric Society 1989. March 1:307–33. [Google Scholar]
- Woodbury RM. Economic factors in infant mortality. Journal of the American Statistical Association 1924. June 1;19(146):137–55. [Google Scholar]
- Zeileis A, Kleiber C, Jackman S (2008). Regression Models for Count Data in R. Journal of Statistical Software 27(8). URL http://www.jstatsoft.org/v27/i08/. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.