Abstract
Objectives
This study describes adolescent attitudes towards online therapies and explores the factors that predict these attitudes.
Method
Australian adolescents (N = 217) were surveyed on their knowledge of, attitudes towards (including perceived problems, perceived benefits, and perceived helpfulness), recommended availability of, and intentions to use online therapies. In addition, demographic and clinical factors, factors relating to technology use, adolescents' mental health attitudes, and personality traits were also measured.
Results
The findings suggested that 72.0% of adolescents would access an online therapy if they experienced a mental health problem and 31.9% would choose an online therapy over traditional face-to-face support. The most valued benefits of these programs included alleviation of stigma and increased accessibility. Knowledge of online therapies was found to positively predict perceived helpfulness and intended uptake.
Conclusions
This study provides insight into adolescent attitudes towards online therapies and highlights the need to investigate strategies for increasing uptake.
Keywords: Online, Adolescent, Attitudes, Services, Mental health
Highlights
-
•
Online therapies are able to increase the accessibility of mental health treatment for adolescents, yet uptake remains low.
-
•
Adolescents reported their attitudes towards and intentions to use online therapies.
-
•
72% of adolescents would access an online therapy if they required support.
-
•
Adolescents valued the benefits of stigma reduction and accessibility.
-
•
Online therapy knowledge predicted perceived helpfulness and uptake intentions.
1. Introduction
The emergence of mental health problems during adolescence is well documented and the evidence supporting psychological intervention during this period is clear (Lawrence et al., 2015, Lee et al., 2013, Chorpita et al., 2011). However, even gold standard treatments are ineffectual if young people in the community do not access them. At present, an estimated 35% of Australian adolescents with clinical mental health disorders fail to utilise professional services (Lawrence et al., 2015). It is evident that more needs to be done to ensure young people access support for their mental health.
There are a number of barriers that prevent young people from accessing mental health services, including, perceived stigma (Gulliver et al., 2010), an expectation or preference for self-reliance (Wilson et al., 2011), concerns around confidentiality (Gulliver et al., 2010), and a lack of knowledge and accessibility of services (Gulliver et al., 2010). One of the most recent strategies to circumvent such barriers has been online service delivery.
Online therapies are well-placed to address barriers to mental health services (Elkins et al., 2011, Hosie et al., 2014). The efficacy of online therapies is well established in the treatment of a number of mental health conditions (including depression, anxiety, substance misuse, and more) among adolescents (Donovan and March, 2014, Ebert et al., 2015, Reyes-Portillo, 2014). Online treatment programs have also demonstrated comparable efficacy to face-to-face psychotherapy (Christensen et al., 2014, Sethi, 2013, Spence et al., 2011). In addition, while not all programs have been disseminated, there are still a number of programs that are currently available to adolescents, such as MoodGYM (O'Kearney et al., 2007), OCD? Not Me (Rees et al., 2016), BRAVE Self-Help (March et al., 2009), OnTrack Get Real (Queensland University of Technology, 2015), and MindSpot Mood Mechanic (Titov et al., 2015).
Unfortunately, uptake of online therapies remains low (Lawrence et al., 2015). There is evidence to suggest that young people consider the choice to access mental health services online as being up to them, in contrast to accessing face-to-face services, where they feel more strongly influenced by their family (Rickwood et al., 2015). Following this, if young people perceive greater independence in the decision to seek online support, then understanding adolescents' attitudes towards these services may inform strategies to improve uptake.
Only three studies to date have asked young people about their perceptions of online therapies. Of these, two featured university students (Horgan and Sweeney, 2010, Mitchell and Gordon, 2007) and one examined adolescents' attitudes towards online counselling (Glasheen et al., 2015). Intentions to access online therapies have been found to be consistently high among university students, although they maintain a preference for face-to-face alternatives (Horgan and Sweeney, 2010, Mitchell and Gordon, 2007). University students also appear to value the benefits of online therapies, including privacy, accessibility, anonymity, and confidentiality (Horgan and Sweeney, 2010, Mitchell and Gordon, 2007). Finally, Glasheen et al. (2015) found that 80–84% of adolescents would consider using online counselling if it was available at school. They also found that adolescents preferred going online to discuss sensitive issues (such as sexuality), and preferred face-to-face support for other topics (such as peer conflict, bullying, and guidance). Perhaps adolescents perceive online services as more appropriate for issues around which there is a greater perceived stigma.
It appears that the benefits of accessibility and privacy offered by online therapies may encourage young people to use these programs, yet are insufficient for them to prefer online therapies, over face-to-face support. This suggests that additional factors may be influencing their service decisions. Research in this area is clearly in its early stages and limited in its current scope and depth, particularly in relation to the adolescent population. However, understanding adolescents' attitudes towards these programs is an important step towards informing strategies to increase the uptake of mental health treatment.
In addition to understanding the content of adolescents' attitudes, examining the factors that influence these attitudes may also inform strategies for increasing uptake. To date, research exploring the factors contributing to attitudes towards online therapies has been limited to adults (Becker and Jensen-Doss, 2013, Tsan and Day, 2007), health professionals (Donovan et al., 2015, Stallard et al., 2010, Fleming and Merry, 2013, Gun et al., 2011), and parents (Sweeney et al., 2015). Based on this literature, factors that may influence service preferences have included personality, technology use, and knowledge or experience with online therapies. Though yet to be studied in the online therapy literature, stigmatized attitudes towards mental health have also been linked to poor psychological help-seeking in adolescents (Clement et al., 2015, Cometto, 2014, Jorm, 2012), and thus warrants consideration. Examination of the factors influencing adolescents' attitudes and intentions to use online therapies is absent to date.
Following this, the first aim of the present study was to detail adolescents' perceptions of online therapies, including 1) knowledge of online therapies, 2) attitudes towards online therapies (perceived problems, perceived benefits, and perceived helpfulness), 3) intentions to use online therapies, and 4) recommended availability of online therapies. The second aim was to assess factors predicting attitudes and intentions to use online therapies. Adolescent factors of interest included, 1) demographic and clinical factors, 2) technology factors, 3) knowledge of online therapies, 4) mental health attitudes, and 5) personality factors.
2. Method
2.1. Procedure
Following ethical clearance, participants from the general community were recruited via Facebook posts on youth interest groups, and advertising through secondary schools. All recruitment materials featured a link to access the online information/consent form and survey site. Participants were encouraged to voluntarily discuss participation with their parents prior to giving consent. After providing informed consent, participants were directed to an online survey. Upon completion, participants were offered the opportunity to submit their email address for entry into the draw to win an iPad Mini. All participants were invited to contact the authors for a summary of results from the study.
2.2. Measures
To the best of our knowledge, there is an absence of psychometrically validated measures that assess adolescent perceptions of online therapies. Subsequently, the present study utilised a number of author-developed measures that were adapted from those used in prior online therapy research (with adults and clinicians) and/or developed in consultation with research colleagues in the field.1
2.2.1. Online therapy knowledge2
A 14-item true-false test was developed to assess knowledge of online therapies (e.g. ‘All online therapies involve therapist contact’). Items were generated in collaboration with researchers in the online therapy field to ensure external validity. Correct responses were summed to produce a total score (ranging from 0 to 14), with higher scores indicating greater knowledge of online therapies.
2.2.2. Online therapy attitudes
Adolescents' attitudes towards online therapies were measured using an author-developed questionnaire adapted from previous research in the field (Stallard et al., 2010, Klein and Cook, 2010). The questionnaire comprised of three scales: perceived problems, benefits, and helpfulness.
2.2.2.1. Perceived problems
Perceived problems with online therapies were measured with a 10-item scale whereby participants rated the degree to which they thought each item (e.g. ‘finding time to do it’) was problematic on a five-point scale (1 = not at all problematic to 5 = extremely problematic). Responses were summed to produce a total score that could range from 10 to 50, with higher scores indicating greater perceived problems with online therapies (Cronbach's α = 0.85).
2.2.2.2. Perceived benefits
Perceived benefits of online therapies were measured with a 9-item scale whereby participants rated the degree to which they thought each item (e.g. ‘use at home’) was beneficial on a five-point scale (1 = not at all beneficial to 5 = extremely beneficial). Responses were summed to produce a total score that could range from 9 to 45, with higher scores indicating greater perceived benefits of online therapies (Cronbach's α = 0.95).
2.2.2.3. Perceived helpfulness
Participants rated how helpful they considered online therapies in the treatment of adolescent mental health problems, on a single-item five-point scale (1 = not helpful at all, to 5 = extremely helpful).
2.2.3. Intention to use services
Adolescents' intentions to use services were measured using a 5-item author-developed questionnaire adapted from previous research (Stallard et al., 2010, Klein and Cook, 2010). Items 1–4 were used for descriptive purposes. Item one asked adolescents to rate how likely they would be to use eleven mental health services (e.g., ‘psychologist’) on a five-point scale (1 = not at all likely to 5 = extremely likely). Item two asked adolescents to report whether they would access an available online therapy program if they experienced mental health problems (yes/no). Item three asked adolescents to state their preference for face-to-face or online therapy. Item four asked adolescents to indicate their preferred modes of access to online therapies (i.e. ‘smartphone’, ‘tablet’, ‘CD-ROM’, ‘internet’, and ‘virtual reality’), with the option to select multiple modes. The fifth item was used as the outcome variable and asked adolescents to rate their intention to use an online therapy on a five-point scale (1 = not at all likely to 5 = extremely likely).
2.2.4. Recommended availability
Participants were asked if they believed online therapies should be made available to adolescents in six different ways (i.e. ‘available for use in school’). Responses were scored on a five-point scale (1 = definitely yes to 5 = definitely no).
2.2.5. Additional predictor variables
The second aim of the study was to assess factors predicting perceptions of online therapies, including: demographic and clinical factors, technology factors, knowledge of online therapies (Section 2.2.1), mental health attitudes, and personality factors.
2.2.5.1. Demographic and clinical factors
Demographic factors included gender (male/female), age (years), and residential location (urban/rural). Clinical factors included total number of self-reported mental health problems and prior experience with online therapies (yes/no).
2.2.5.2. Technology factors
Participants reported if they had access (yes/no) to four technologies (personal computer, internet, smartphone, and tablet), with responses summed to produce a technology access score (ranging from 1 to 4). Participants rated their confidence in using each of these technologies on a five-point scale (1 = not confident at all to 5 = very confident), with scores summed to produce a technology confidence score (ranging from 1 to 20, Cronbach's α = 0.86). Participants also rated their liking for using new technologies on a single-item five-point scale (1 = strongly dislike to 5 = strongly like).
2.2.5.3. Mental health attitudes
The 19-item Attitudes Scale of the Mental Health Questionnaire (Sheffield et al., 2004) was administered to measure attitudes towards mental illness. Participants rated their agreement with each statement on a six-point scale (1 = strongly disagree to 6 = strongly agree). Items were summed to provide a total score ranging from 19 to 114, with higher scores indicating more negative attitudes towards mental health (Cronbach's α = 0.90).
2.2.5.4. Personality factors
The 44-item Big Five Inventory (BFI; John et al., 1991, John et al., 2008) was administered to measure personality traits. Previous research estimates the BFI subscales to have adequate internal consistency (r = 0.83), convergent validity with other personality measures (John et al., 2008), and adequate validity in an adolescent sample (Fossati et al., 2011). Participants were asked to rate their agreement with each item on a five-point scale (1 = strongly disagree to 5 = strongly agree). The mean was calculated for each of the five subscales to produce a subscale score ranging from 1 to 5, such that higher scores on each subscale indicate greater characteristic endorsement.
2.3. Data analytic plan
The analyses were divided into two sections corresponding to the two aims of the study. Descriptive statistics were used to describe adolescents' 1) knowledge, 2) attitudes (perceived problems, benefits, and helpfulness), 3) intentions to use, and 4) recommended availability of online therapies.
The second aim of the study was to assess factors predicting adolescent attitudes and intentions to use online therapies. A series of four hierarchical multiple regression analyses (HMRs) were conducted, one for each of the four outcome variables (perceived helpfulness, problems, benefits, and intentions to use online therapies). Adolescent factors examined included demographic and clinical factors (gender, age, residential location, number of mental health problems, experience with online therapies), technology factors (liking, access, confidence), knowledge of online therapies, mental health attitudes, and personality factors (extraversion, agreeableness, conscientiousness, neuroticism, openness). The hierarchy was determined in order to control for extraneous variables (step one: demographic and clinical factors), focus on factors presumed to be of greater importance to attitudinal outcomes (step two: technology factors, step three: knowledge of online therapies), and determine if factors identified in prior research had additional value (step four: mental health attitudes, step five: personality factors).
All analyses were conducted using IBM SPSS Statistics (Version 22.0). Power analyses determined that a sample size of 139 would be sufficient to detect a medium effect size, with a power of 0.80, an alpha of 0.05, and 15 predictor variables (Erdfelder et al., 1996); while a sample size of 954 would be sufficient to detect a small effect size with the same parameters. The current sample (N = 217) is therefore adequately powered to detect a medium effect, yet underpowered to detect a small effect size.
3. Results
3.1. Participant characteristics
3.1.1. Demographics
Participants were 217 adolescents aged 13–18 years (M = 16.98, SD = 1.32), of whom the majority were female, resided in an urban location, had completed secondary school, and identified as single (see Table 1).
Table 1.
Participant demographics (N = 217).
| Category | Group | n | % |
|---|---|---|---|
| Gender | Female | 156 | 71.9 |
| Male | 61 | 28.1 | |
| Residential location | Urban | 196 | 90.3 |
| Rural | 21 | 9.7 | |
| Education | Enrolled in secondary | 73 | 33.6 |
| Completed secondary | 133 | 61.3 | |
| Completed TAFE certificate | 4 | 1.8 | |
| Completed tertiary diploma | 7 | 3.2 | |
| Relationship | Single | 137 | 63.1 |
| In a relationship | 80 | 36.9 |
3.1.2. Mental health experiences
In total, 74.2% (n = 191) of participants reported experiencing a mental health challenge, most commonly anxiety/worry (n = 134, 61.8%), depression/mood (n = 106, 48.8%), anger (n = 82, 37.8%), bullying (n = 57, 26.3%), and grief (n = 45, 20.7%). One in three participants (n = 81, 37.3%) reported previously accessing a mental health service, most commonly a counsellor (n = 63, 29.0%), GP (n = 55, 25.3%), psychologist (n = 53, 24.4%), or information website (n = 51, 23.5%). Only 3.7% (n = 8) of participants reported experience with online therapies.
3.1.3. Technology use
Most adolescents reported access to at least one technology mode at home (n = 210, 99.1%), reported at least liking (n = 195, 92.0%) using technology, and were at least somewhat confident using computers (n = 206, 97.2%), internet (n = 210, 99.1%), smartphones (n = 207, 97.6%), and tablets (n = 192, 90.6%).
3.2. Perceptions of online therapies
3.2.1. Online therapy knowledge
Adolescents completed a quiz on online therapies.3 All items were correctly identified by less than half of participants, including: treatment effectiveness (n = 90, 42.9%), interactivity (n = 103, 49.0%), therapist contact (n = 94, 44.8%), user satisfaction (n = 47, 22.4%), availability (n = 45, 21.4%), comparable helpfulness to face-to-face therapy (n = 51, 24.3%), and program tailoring (12.4%, n = 26). Few participants identified online therapies as effective treatments of anxiety (n = 96, 45.7%) and depression (n = 81, 38.6%).
3.2.2. Online therapy attitudes
3.2.2.1. Perceived problems
The majority of adolescents rated the following factors as at least moderately problematic: the inability to ask questions (n = 128, 61.5%), not finishing the program (n = 116, 55.8%), information being too general (n = 112, 53.8%), being without therapist support (n = 107, 51.5%), and the privacy of personal information (n = 106, 51.0%). Fewer adolescents considered losing interest (n = 95, 45.7%), finding time (n = 88, 42.4%), computer problems (n = 81, 39.0%), computer access (n = 80, 38.5%), and difficulty of tasks (n = 78, 37.5%) to be problematic.
3.2.2.2. Perceived benefits
Over two thirds of participants rated the following factors as at least moderately beneficial: use at home (n = 166, 79.9%), use any time (n = 159, 76.4%), low cost (n = 159, 76.4%), the alleviation of embarrassment (n = 150, 72.1%), ability to track progress (n = 150, 72.1%), ease of accessibility (n = 150, 72.1%), avoiding waitlists to support (n = 130, 62.5%), and greater interactivity that self-help resources (n = 127, 61.1%). One in three considered programs being interesting (n = 78, 37.5%) as beneficial.
3.2.2.3. Perceived helpfulness
The majority of adolescents perceived online therapies as helpful, albeit to different degrees. Approximately one in six did not find them helpful.
3.2.3. Intention to use
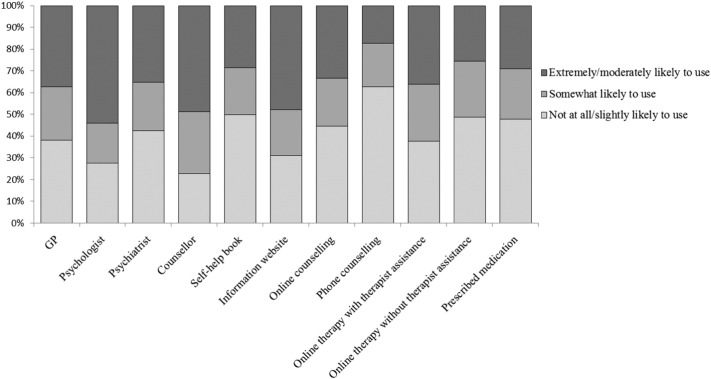
The majority of adolescents indicated they would access an online therapy (n = 149, 72.0%), and a third indicated they would choose an online therapy (n = 66, 31.9%) over face-to-face support. Fig. 1 illustrates adolescent intention to use a variety of mental health services in the context of experiencing a mental health difficulty. Adolescents were at least moderately likely to access psychologists, information websites, and counsellors. Most adolescents were at least somewhat likely to access an online therapy and favoured use with therapist assistance.
Fig. 1.
Likelihood of services use for future mental health difficulties by type of service.
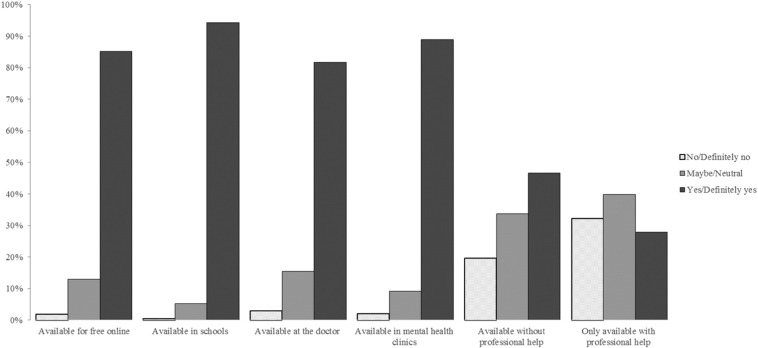
3.2.4. Recommended availability
Adolescents strongly endorsed the availability of online therapies freely online, in schools, at the doctor, and in mental health clinics (see Fig. 2). Around half of adolescents endorsed availability without professional support.
Fig. 2.
Recommended availability of online therapies.
3.3. Predictors of perceptions of online therapies
Table 2 provides the means, standard deviations, and bivariate correlations for all variables. Table 3 provides statistics for the final model (step five) of each HMR for the four outcome variables: perceived problems, benefits, helpfulness and intentions to use online therapies. Predictor variables are grouped as demographic and clinical factors (1), technology factors (2), knowledge (3), mental health attitudes (4), and personality factors (5).
Table 2.
Descriptive statistics and bivariate correlations for all predictor and criterion variables.
| M | SD | Helpfulness | Problems | Benefits | Intentions | ||
|---|---|---|---|---|---|---|---|
| Demographic & clinical | Gender | 0.21⁎⁎ | 0.06 | 0.23⁎⁎ | 0.13 | ||
| Age | 16.98 | 1.32 | 0.04 | 0.11 | 0.12 | − 0.01 | |
| Location | − 0.07 | − 0.09 | − 0.11 | − 0.12 | |||
| Number of mental health problems | 2.14 | 1.77 | 0.02 | 0.05 | 0.10 | 0.11 | |
| Experience with online therapies | − 0.21⁎⁎ | 0.04 | 0.01 | − 0.04 | |||
| Technology | Technology liking | 4.44 | 0.65 | 0.23⁎⁎ | < 0.01 | 0.20⁎⁎ | 0.06 |
| Technology access | 2.98 | 0.82 | − 0.02 | 0.06 | 0.16⁎ | − 0.06 | |
| Technology confidence | 17.65 | 2.93 | 0.09 | 0.15⁎ | 0.15⁎ | − 0.08 | |
| Knowledge | Knowledge of online therapies | 4.18 | 3.43 | 0.15⁎ | − 0.03 | 0.11 | 0.17⁎ |
| Mental health | Mental health attitudes | 48.81 | 15.58 | − 0.28⁎⁎⁎ | − 0.16⁎ | − 0.40⁎⁎⁎ | − 0.13 |
| Personality | Extraversion | 3.24 | 0.69 | 0.04 | 0.06 | 0.03 | − 0.08 |
| Agreeableness | 3.58 | 0.53 | 0.12 | 0.14⁎ | 0.13 | − 0.04 | |
| Conscientiousness | 3.22 | 0.63 | 0.11 | 0.16⁎ | 0.14⁎ | 0.01 | |
| Neuroticism | 3.22 | 0.70 | < 0.01 | − 0.03 | 0.11 | 0.09 | |
| Openness | 3.44 | 0.50 | 0.08 | 0.17⁎ | 0.10 | 0.02 | |
| Criterions | M | 3.55 | 33.23 | 35.00 | 3.02 | ||
| SD | 0.97 | 7.53 | 8.16 | 1.23 |
p < 0.05.
p < 0.01.
p < 0.001.
Table 3.
Statistics for the final regression equation (step five) examining adolescent predictors of attitudinal outcomes.
| Group | Variable | Perceived problems |
Perceived benefits |
Perceived helpfulness |
Intentions to use |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| β | t | p | sr2 | β | t | p | sr2 | β | t | p | sr2 | β | t | p | sr2 | ||
| 1 | Gender | 0.04 | 0.47 | 0.639 | < 0.01 | 0.13 | 1.77 | 0.078 | 0.01 | 0.20 | 2.62 | 0.010 | 0.03 | 0.11 | 1.34 | 0.182 | 0.01 |
| Age | 0.11 | 1.49 | 0.138 | 0.01 | 0.06 | 0.98 | 0.328 | < 0.01 | − 0.03 | − 0.42 | 0.672 | < 0.01 | − 0.06 | − 0.82 | 0.414 | < 0.01 | |
| Location | − 0.10 | − 1.36 | 0.176 | 0.01 | − 0.06 | − 0.88 | 0.378 | < 0.01 | − 0.04 | − 0.57 | 0.569 | < 0.01 | − 0.09 | − 1.27 | 0.205 | 0.01 | |
| Number of mental health problems | 0.01 | 0.14 | 0.889 | < 0.01 | 0.03 | 0.50 | 0.620 | < 0.01 | 0.03 | 0.44 | 0.661 | < 0.01 | 0.10 | 1.35 | 0.179 | 0.01 | |
| Experience with online therapies | 0.04 | 0.55 | 0.584 | < 0.01 | − 0.01 | − 0.16 | 0.875 | < 0.01 | − 0.22 | − 3.27 | 0.001 | 0.04 | − 0.10 | − 1.34 | 0.181 | 0.01 | |
| 2 | Technology liking | − 0.08 | − 1.09 | 0.276 | 0.01 | 0.15 | 2.17 | 0.031 | 0.02 | 0.22 | 3.10 | 0.002 | 0.04 | 0.10 | 1.31 | 0.193 | 0.01 |
| Technology access | 0.02 | 0.21 | 0.830 | < 0.01 | 0.10 | 1.56 | 0.121 | 0.01 | − 0.06 | − 0.88 | 0.379 | < 0.01 | − 0.05 | − 0.71 | 0.476 | < 0.01 | |
| Technology confidence | 0.15 | 1.95 | 0.053 | 0.02 | 0.03 | 0.41 | 0.679 | < 0.01 | − 0.01 | − 0.18 | 0.857 | < 0.01 | − 0.11 | − 1.38 | 0.170 | 0.01 | |
| 3 | Knowledge of online therapies | − 0.04 | − 0.57 | 0.568 | < 0.01 | 0.12 | 1.88 | 0.062 | 0.01 | 0.18 | 2.75 | 0.007 | 0.03 | 0.18 | 2.64 | 0.009 | 0.03 |
| 4 | Mental health attitudes | − 0.08 | − 1.03 | 0.303 | < 0.01 | − 0.31 | − 4.31 | 0.000 | 0.07 | − 0.22 | − 3.02 | 0.003 | 0.04 | − 0.12 | − 1.46 | 0.145 | 0.01 |
| 5 | Extraversion | 0.06 | 0.76 | 0.446 | < 0.01 | 0.02 | 0.30 | 0.766 | < 0.01 | − 0.01 | − 0.17 | 0.868 | < 0.01 | − 0.09 | − 1.20 | 0.233 | 0.01 |
| Agreeableness | 0.08 | 1.11 | 0.267 | 0.01 | 0.02 | 0.24 | 0.808 | < 0.01 | 0.03 | 0.41 | 0.681 | < 0.01 | − 0.07 | − 0.96 | 0.337 | < 0.01 | |
| Conscientiousness | 0.06 | 0.86 | 0.388 | < 0.01 | 0.02 | 0.36 | 0.721 | < 0.01 | 0.01 | 0.10 | 0.923 | < 0.01 | − 0.03 | − 0.44 | 0.662 | < 0.01 | |
| Neuroticism | − 0.05 | − 0.62 | 0.537 | < 0.01 | − 0.04 | − 0.46 | 0.644 | < 0.01 | − 0.11 | − 1.33 | 0.185 | 0.01 | − 0.02 | − 0.26 | 0.792 | < 0.01 | |
| Openness | 0.14 | 1.82 | 0.070 | 0.02 | 0.07 | 1.03 | 0.303 | < 0.01 | 0.09 | 1.22 | 0.226 | 0.01 | 0.04 | 0.55 | 0.585 | < 0.01 | |
3.3.1. Perceived problems
In the final regression, adolescent factors failed to significantly predict perceived problems and accounted for only 11% of variance in the outcome, R2 = 0.11, F = 1.62(15,192), p = 0.071. No individual factors were found to significantly contribute to the prediction of perceived problems.
3.3.2. Perceived benefits
The final regression equation accounted for 25% of variance in the outcome of perceived benefits, R2 = 0.25, F = 4.23(15,192), p < 0.001. Demographic and clinical factors (∆ R2 = 0.07, ∆ F(5202) = 3.04, p = 0.011), technology factors (∆ R2 = 0.07, ∆ F(3199) = 4.98, p = 0.002), and mental health attitudes (∆ R2 = 0.09, ∆ F(1197) = 23.72, p < 0.001) contributed significantly to the model. In the final model, greater technology liking and less stigmatized mental health attitudes significantly predicted greater perceived benefits.
3.3.3. Perceived helpfulness
The final regression equation accounted for 24% of variance in the outcome of perceived helpfulness, R2 = 0.24, F = 4.00(15,192), p < 0.001. Clinical and demographic factors (∆ R2 = 0.09, ∆ F(5202) = 3.96, p = 0.002), technology factors (∆ R2 = 0.06, ∆ F(3199) = 4.33, p = 0.006), knowledge (∆ R2 = 0.03, ∆ F(1198) = 7.39, p = 0.007), and mental health attitudes (∆ R2 = 0.05, ∆ F(1197) = 11.36, p = 0.001) contributed significantly to the model. In the final model, participants who were female, had no prior experience with online therapies, and reported greater technology liking, greater knowledge of online therapies and less stigmatized mental health attitudes reported significantly greater perceived helpfulness.
3.3.4. Intentions to use
In the final regression equation, adolescent factors failed to significantly predict intentions to use online therapies and accounted for only 11% of variance in the outcome, R2 = 0.11, F = 1.60(15,192), p = 076. Individually, knowledge of online therapies (∆ R2 = 0.03, ∆ F(1197) = 6.27, p = 0.013) contributed significantly to the prediction of intentions to use. In the final model, greater knowledge of online therapies significantly predicted greater uptake intentions.
4. Discussion
The primary aims of this study were to describe adolescents' perceptions of online therapies and investigate factors influencing their attitudes and uptake intentions. Despite the majority of participants reporting experience with mental health challenges, only around a third had accessed a mental health service and even fewer individuals (3.7%) reported having used an online therapy. These rates confirm previous observations (Lawrence et al., 2015) that uptake of online therapies is low in the community.
In spite of demonstrating poor knowledge about the effectiveness and accessibility of online therapies, adolescents' perceptions of these programs were found to be generally positive. While adolescents' reported concerns around the likelihood of not finishing the program, inability to ask questions, privacy and level of therapist support; these were less strongly endorsed than perceived benefits, such as the alleviation of embarrassment, ability to track progress, and increased accessibility. These findings are consistent with benefits perceived by university students (Horgan and Sweeney, 2010) and ratify that the capacity of online therapies to increase treatment accessibility and reduce service-related stigma is important to adolescents. These key factors identified as important to adolescents may be highlighted in strategies (such as educational programs) to improve program uptake.
Adolescents also strongly supported the availability of online therapies for free online, in schools and mental health clinics, and at the doctor; yet were divided on their preference for availability with or without therapist support. Promotional strategies aimed at improving uptake of these services should therefore educate adolescents on the options for self-help or adjunct therapist support programs, and empower them to access support services most suitable to their needs.
Finally, although the majority of adolescents believed online therapies were helpful and reported they would use them if necessary, only one third would choose online therapy over face-to-face support. Comparatively, adolescent preference for online therapy was found to be stronger than that reported previously by university students (Horgan and Sweeney, 2010, Mitchell and Gordon, 2007). One explanation for this is that adolescents may be more receptive to online services than young adults, though it remains clear that this receptivity does not always lead to actual program use.
This study also investigated the factors influencing adolescent attitudes and intentions to use online therapies. Demographic and clinical factors associated with higher uptake intentions included female gender, and the absence of prior experience with online therapies. The absence of experience increasing intentions is inconsistent with findings from the psychological help-seeking literature (Gulliver et al., 2010), and may have arisen due to the neutrality (rather than negativity) of adolescents with prior experience, compared to the optimism of the inexperienced. Adolescents who had a liked using technology more also perceived online therapies as more helpful and with greater benefits. This relationship suggests that when disseminating online therapies, implementation materials also need to be online to provide the greatest exposure to technology-friendly adolescents.
Consistent with prior research in the youth mental health help-seeking literature (Rickwood et al., 2007), perceived helpfulness and uptake intentions were found to be higher among adolescents with greater knowledge of online therapies. It is suggested that adolescents who have a greater knowledge of online therapies are more likely to be well-informed on the programs' positive aspects and thus see them as more helpful, leading to greater uptake intentions. Also consistent with psychological help-seeking literature (Clement et al., 2015, Cometto, 2014, Jorm, 2012), adolescents with less stigmatized mental health attitudes were found to have more positive attitudes towards online therapies. This finding highlights that the issue of mental health stigmatization continues to influence young peoples' choices around accessing support, even online.
Finally, adolescent personality traits failed to significantly predict any outcomes. These findings are in contrast with prior literature that has found significant relationships between personality and attitudes towards online therapies among adults (Klein and Cook, 2010, Tsan and Day, 2007). One explanation is that this contrast can be attributed to a difference in assessment measures. Alternatively, we also know that personality traits are less stable during the adolescent period than during adulthood (Soto et al., 2011, Hampson and Goldberg, 2006), thus perhaps this instability could explain the less robust influence of personality on help-seeking attitudes among youth. It would seem that for adolescents, personality traits may not determine their perceptions of online therapies.
Following this, we present three potential strategies to improve the uptake of these programs among adolescents. The first is to target the dissemination of online therapies towards adolescents who like technology, by focusing dissemination strategies on digital forums, such as social media and other popular websites among adolescents. The second strategy is to improve knowledge about online therapies among all adolescents in the community, through awareness and educational campaigns. The third strategy is to reduce mental health stigma among adolescents, by promoting healthy attitudes towards mental health and associated services.
The present study had several strengths. It was the first of its kind to describe in detail, adolescent attitudes towards online mental health interventions and quantitatively examine the factors that influenced these attitudes. By surveying adolescents themselves, this study importantly recognised the changing landscape of mental health services, such that adolescents can now access evidence-based treatments for a number of mild to moderate mental health concerns from their own homes.
Despite its strengths, this study was not without limitations. First, the sample of participants were relatively well-educated, English-speaking, and had technology access; thereby reducing the generalizability of the findings to adolescents without such privileges. Second, given the use of a cross-sectional research design, this study cannot inform temporal changes in adolescents' attitudes and uptake intentions, nor their actual program uptake. Future research using a longitudinal design to monitor change in attitudes over time and follow-up assessment of uptake behaviour is strongly encouraged. Third, several measures used in this study were not psychometrically validated, thus the development of validated measures specific to adolescent attitudes towards online therapies is encouraged. Fourth, it is recommended that future research is conducted with a larger sample of prior service users, than found the present sample, before drawing conclusions around the impact of service experience on attitudes towards online therapies. Fifth, multiple analyses conducted with a large number of predictors in this study may have inflated the Type I error rate, therefore future research is recommended to recruit a larger sample.
Finally, though beyond the scope of this study, future research is also warranted to 1) examine the mediating relationships between knowledge, attitudes, intentions, and uptake, 2) explore the impact of age cohort on psychological service attitudes among young people, and 3) examine adolescent preferences for specific program features in online therapies.
5. Conclusions
The current study represents an important step towards increasing the use of online psychological interventions for adolescents. It is evident we need to invest more resources in implementation strategies for online programs, alongside investment into their development and research. We recommend such strategies focus on increasing knowledge of online therapies among adolescents, and target adolescents who are already engaged in digital platforms. If adolescents are willing to give online interventions a go, then we need to begin developing these strategies to improve their knowledge and awareness of these services in order to enhance uptake in the community.
Footnotes
Contact the authors for additional details.
Contact the authors for additional details.
Contact the authors for additional details.
References
- Becker E.M., Jensen-Doss A. Computer-assisted therapies: examination of therapist-level barriers to their use. Behav. Ther. 2013;44(4):614–624. doi: 10.1016/j.beth.2013.05.002. [DOI] [PubMed] [Google Scholar]
- Chorpita B.F., Daleiden E.L., Ebesutani C., Young J., Becker K.D., Nakamura B.J.…Starace N. Evidence-based treatments for children and adolescents: An updated review of indicators of efficacy and effectiveness. Clin. Psychol. Sci. Pract. 2011;18(2):154–172. [Google Scholar]
- Christensen H., Batterham P., Calear A. Online interventions for anxiety disorders. Curr. Opin. Psychiatry. 2014;27(1):7–13. doi: 10.1097/YCO.0000000000000019. [DOI] [PubMed] [Google Scholar]
- Clement S., Schauman O., Graham T., Maggioni F., Evans-Lacko S., Bezborodovs N., Morgan C., Rusch N., Brown J.S.L., Thornicroft G. What is the impact of mental health-related stigma on help-seeking? A systematic review of quantitative and qualitative studies. Psychol. Med. 2015;45(1):11–27. doi: 10.1017/S0033291714000129. [DOI] [PubMed] [Google Scholar]
- Cometto J.L. University of Windsor; Canada: 2014. Factors Predicting Adolescents' and Parents' Help Seeking Behaviour. (Doctoral thesis) (Retrieved from http://dissexpress.umi.com/dxweb/search.html) [Google Scholar]
- Donovan C.L., March S. Online treatment programs for youth anxiety: a systematic review. Psychopathol. Rev. 2014;1(1):130–156. [Google Scholar]
- Donovan C.L., Poole C., Boyes N., Redgate J., March S. Australian mental health worker attitudes towards cCBT: what is the role of knowledge? Are there differences? Can we change them? Internet Interv. 2015;2(4):372–381. [Google Scholar]
- Ebert D.D., Zarski A.-C., Christensen H., Stikkelbroek Y., Cuijpers P., Berking M., Riper H. Internet and online cognitive behavioral therapy for anxiety and depression in youth: a meta-analysis of randomized controlled outcome trials. PLoS One. 2015;10(3) doi: 10.1371/journal.pone.0119895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elkins R.M., McHugh R.K., Santucci L.C., Barlow D.H. Improving the transportability of CBT for internalizing disorders in children. [review] Clin. Child. Fam. Psychol. Rev. 2011;14(2):161–173. doi: 10.1007/s10567-011-0085-4. [DOI] [PubMed] [Google Scholar]
- Erdfelder E., Faul F., Buchner A. GPOWER: a general power analysis program. Behav. Res. Methods Instrum. Comput. 1996;28(1):1–11. [Google Scholar]
- Fleming T., Merry S. Youth work service providers' attitudes towards computerized CBT for adolescents. Behav. Cogn. Psychother. 2013;41(3):265–279. doi: 10.1017/S1352465812000306. [DOI] [PubMed] [Google Scholar]
- Fossati A., Borroni S., Marchione D., Maffei C. The big five inventory (BFI) Eur. J. Psychol. Assess. 2011;27(1):50–58. [Google Scholar]
- Glasheen K.J., Shochet I., Campbell M.A. Online counselling in secondary schools: Would students seek help by this medium? Br. J. Guid. Couns. 2015;44(1):108–122. [Google Scholar]
- Gulliver A., Griffiths K.M., Christensen H. Perceived barriers and facilitators to mental health help seeking in young people: a systematic review. BMC Psychiatry. 2010;10:113. doi: 10.1186/1471-244X-10-113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gun S.Y., Titov N., Andrews G. Acceptability of internet treatment of anxiety and depression. Australas. Psychiatry. 2011;19(3):259–264. doi: 10.3109/10398562.2011.562295. [DOI] [PubMed] [Google Scholar]
- Hampson S.E., Goldberg L.R. A first large-cohort study of personality-trait stability over the 40 years between elementary school and midlife. J. Pers. Soc. Psychol. 2006;91(4):763–779. doi: 10.1037/0022-3514.91.4.763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horgan A., Sweeney J. Young students' use of the internet for mental health information and support. J. Psychiatr. Ment. Health Nurs. 2010;17(2):117–123. doi: 10.1111/j.1365-2850.2009.01497.x. [DOI] [PubMed] [Google Scholar]
- Hosie A., Vogl G., Hoddinott J., Carden J., Comeau Y. Crossroads: Rethinking the Australian Mental Health System. 2014. http://apo.org.au/node/38336 (Retrieved from)
- John O.P., Donahue E.M., Kentle R.L. University of California, Berkeley, Institute of Personality and Social Research; Berkeley, CA: 1991. The Big Five Inventory — Versions 4a and 54. [Google Scholar]
- John O.P., Naumann L.P., Soto C.J. Paradigm shift to the integrative big five trait taxonomy: history, measurement, and conceptual issues. In: John O.P., Robins R.W., Pervin L.A., editors. Handbook of Personality: Theory and Research. Guilford Press; New York, NY: 2008. pp. 114–158. [Google Scholar]
- Jorm A.F. Mental health literacy: empowering the community to take action for better mental health. Am. Psychol. 2012;67(3):231–243. doi: 10.1037/a0025957. [DOI] [PubMed] [Google Scholar]
- Klein B., Cook S. Preferences for e-mental health services amongst an online Australian sample. Electron. J. Appl. Psychol. 2010;6(1):28–39. [Google Scholar]
- Lawrence D., Johnson S., Hafekost J., Boterhoven de Haan K., Sawyer M., Ainley J., Zubrick S.R. Department of Health; Canberra: 2015. The Mental Health of Children and Adolescents: Report on the Second Australian Child and Adolescent Survey of Mental Health and Wellbeing. [Google Scholar]
- Lee C.M., Horvath C., Hunsley J. Does it work in the real world? The effectiveness of treatments for psychological problems in children and adolescents. Prof. Psychol. Res. Pract. 2013;44(2):81–88. [Google Scholar]
- March S., Spence S.H., Donovan C.L. The efficacy of an internet-based cognitive-behavioral therapy intervention for child anxiety disorders. J. Pediatr. Psychol. 2009;34(5):474–487. doi: 10.1093/jpepsy/jsn099. [DOI] [PubMed] [Google Scholar]
- Mitchell N., Gordon P. Attitudes towards computerized CBT for depression amongst a student population. Behav. Cogn. Psychother. 2007;35(4):421–430. [Google Scholar]
- O'Kearney R., Gibson M., Christensen H., Griffiths K.M. Effects of a cognitive-behavioural internet program on depression, vulnerability to depression and stigma in adolescent males: a school-based controlled trial. Cogn. Behav. Ther. 2007;35(1):43–54. doi: 10.1080/16506070500303456. [DOI] [PubMed] [Google Scholar]
- Queensland University of Technology OnTrack Get Real [Online Program] 2015. https://www.ontrack.org.au (Retrieved from)
- Rees S.C., Anderson A.R., Kane T.R., Finlay-Jones L.A. Online obsessive-compulsive disorder treatment: preliminary results of the ?OCD? Not me!? Self-guided internet-based cognitive behavioral therapy program for young people. J. Med. Internet Res. Ment. Health. 2016;3(3) doi: 10.2196/mental.5363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reyes-Portillo J.A. Web-based interventions for youth internalizing problems: A systematic review. J. Am. Acad. Child Adolesc. Psychiatry. 2014;53(12):1254–1270. doi: 10.1016/j.jaac.2014.09.005. [DOI] [PubMed] [Google Scholar]
- Rickwood D.J., Deane F.P., Wilson C.J. When and how do young people seek professional help for mental health problems? Med. J. Aust. 2007;187(7):535–539. doi: 10.5694/j.1326-5377.2007.tb01334.x. [DOI] [PubMed] [Google Scholar]
- Rickwood D.J., Mazzer K.R., Telford N.R. Social influences on seeking help from mental health services, in-person and online, during adolescence and young adulthood. BMC Psychiatry. 2015;15(1):40. doi: 10.1186/s12888-015-0429-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sethi S. Treating youth depression and anxiety: a randomised controlled trial examining the efficacy of computerised versus face-to-face cognitive behaviour therapy. Aust. Psychol. 2013;48(4):249–257. [Google Scholar]
- Sheffield J.K., Fiorenza E., Sofronoff K. Adolescents' willingness to seek psychological help: promoting and preventing factors. J. Youth Adolesc. 2004;33(6):495–507. (Retrieved from http://www.springer.com/psychology/child+%26+school+psychology/journal/10964) [Google Scholar]
- Soto C.J., John O.P., Gosling S.D., Potter J. Age differences in personality traits from 10 to 65: big five domains and facets in a large cross-sectional sample. J. Pers. Soc. Psychol. 2011;100(2):330–348. doi: 10.1037/a0021717. [DOI] [PubMed] [Google Scholar]
- Spence S.H., Donovan C.L., March S., Gamble A., Anderson R.E., Prosser S., Kenardy J. A randomized controlled trial of online versus clinic-based CBT for adolescent anxiety. J. Consult. Clin. Psychol. 2011;79(5):629–642. doi: 10.1037/a0024512. [DOI] [PubMed] [Google Scholar]
- Stallard P., Richardson T., Velleman S. Clinicians' attitudes towards the use of computerized cognitive behaviour therapy (cCBT) with children and adolescents. Behav. Cogn. Psychother. 2010;38(5):545–560. doi: 10.1017/S1352465810000421. [DOI] [PubMed] [Google Scholar]
- Sweeney G.M., Donovan C.L., March S., Laurenson S.D. Logging into therapy: parent attitudes and intentions to access computer-based therapies for youth mental health. Internet Interv. 2015;2(4):437–445. [Google Scholar]
- Titov N., Dear B.F., Staples L.G., Bennett-Levy J., Klein B., Rapee R.M.…Purtell C. MindSpot clinic: an accessible, efficient, and effective online treatment service for anxiety and depression. Psychiatr. Serv. 2015;66(10):1043–1050. doi: 10.1176/appi.ps.201400477. [DOI] [PubMed] [Google Scholar]
- Tsan J.Y., Day S.X. Personality and gender as predictors of online counselling use. J. Technol. Hum. Serv. 2007;25(3):39–55. [Google Scholar]
- Wilson C.J., Bushnell J.A., Caputi P. Early access and help seeking: practice implications and new initiatives. Early Interv. Psychiatry. 2011;5(s1):34–39. doi: 10.1111/j.1751-7893.2010.00238.x. [DOI] [PubMed] [Google Scholar]