Abstract
Although patients desire safe care, they are reluctant to perform safety-related behaviors when they worry it could harm the relationships they have with clinicians. This influence of the clinician-patient relationship on patient engagement in safety is poorly understood, and most patient-facing safety interventions ignore its influence, focusing instead on helping patients access information about their care and report errors. We conducted semi-structured interviews with hospitalized patients to uncover their needs for patient-facing information systems that could help them prevent medical errors. We found that the clinician-patient relationship could either encourage or discourage patients and caregivers from engaging in patient safety actions. We describe our findings and discuss the implications for the design of patient-facing interventions to promote patient engagement in safety. Our findings shed light on how patient-facing safety interventions can be designed to effectively engage patients and caregivers.
Introduction
Since the publication of To Err is Human1 and Crossing the Quality Chasm,2 healthcare organizations and researchers have invested heavily in the prevention of medical errors. In addition to improvements in clinical structures and workflows, researchers have begun to investigate the role patients can play in preventing errors.3,4 This movement has gained momentum in recent years as researchers have found that not only are patients willing to participate in their own safety,3 but patient involvement in their safety is associated with fewer adverse events,5 and fewer medication errors.6 Patient engagement more broadly is associated with shorter lengths of inpatient stays7 and better patient self-management.8 Yet, the prevalence of medical errors remains high—according to some estimates, the third leading cause of death in the United States.9 Thus, we urgently need to understand how to develop new interventions that involve patients in their own safety.
To safeguard themselves against medical errors, patients are generally encouraged to engage in specific behaviors. First, patients are encouraged to make sure their health care institution is accredited.10 Before and during hospitalization, safety initiatives typically suggest that patients seek out information about their care, including information about procedures and medications.10–12 During hospitalization, patients have also been encouraged to make sure that information is properly communicated to and from providers,13 ask questions and speak up if they notice anything amiss,10,11 bring along an advocate,10 participate in medical decisions,10 attend to both clinicians’ (nurses, doctors, or technicians) and their own hand hygiene,14 help mark the surgical site,3,5,15 and report errors.5,16 Overall, these actions describe the patient role in safety as a “vigilant monitor,”17 where patients in particular monitor communication with clinicians3 and compliance with easily understood hospital protocols such as hand hygiene.14
To perform this role, patients need access to information about their care and the system that provides it. Researchers have sought to understand what patients want to know about their care18–21 and have explored a variety of interventions to help hospitalized patients access and understand information about their care, including in-room paper-based displays mimicking the capabilities of large screens,22 mobile apps,23 inpatient portals,24–32 and virtual nurses.33 To support the development of this type of intervention, Collins et al. identified the need to understand patient information priorities for research in patient and family empowerment,34 although the impact of personalized information about the care plan compared to generic safety recommendations is unclear.3,35 Researchers have also explored interventions to involve patients in other aspects of their safety, including efforts to design technologies—such as patient-facing interfaces to encourage patients to report errors,16,36 a visible fall risk plan by the patient’s bedside,37 a bedside screensaver featuring a patient safety plan dashboard,12 a tablet application including an interactive safety module,38 and a visual novel to increase patients’ self-efficacy in managing their stay.39 Work in this field has also investigated the potential of social support from caregivers40 and peers41 to help patients engage with their care and safety.
These interventions have focused on getting patients access to information about their own care, but generally do not attempt to influence the clinician-patient relationship. Yet, the clinician-patient relationship influences patients’ willingness to engage with their safety. In particular, patients are reluctant to engage in safety behaviors that appear confrontational or that require patients to digress from the traditional patient role by questioning or challenging clinicians’ judgments.3,42,43 For instance, patients are reluctant to ask clinicians if they have washed their hands,14 and less willing to check that they have received the correct medication than to seek information about their care plan.5 Perceptions of staff time pressure,44,45 fear of negative reactions from clinicians,46,47 and the fear of being seen as a “difficult” patient48 have been found to inhibit patient engagement in safety.
Overall, existing work thus far suggests that a positive relationship with clinicians, where clinicians encourage patient participation, should promote patient engagement in safety. Studies have found that encouragements or invitations to participate in safety from health care providers increases patient performance of safety behaviors.6 Researchers have thus suggested that clinicians should wear buttons encouraging patients to ask them about hand hygiene,49 and that clinicians should present themselves as caring and attentive, do not act rushed, and legitimize patients’ input with appropriate responses.48 However, there is some suggestion in the existing literature that the influence of this relationship is complex, and that a positive relationship does not invariably promote patient engagement. For example, while most researchers discussing the influence of the clinician-patient relationship on patient engagement in safety stress the need to maintain a positive relationship and not erode trust,3,48,49 one study found that trust could act as a negative influence on patient engagement in safety50.
Moreover, the clinician-patient relationship itself is multifaceted, and there is no generally accepted ontology describing what this relationship actually is. Eveleigh et al., reviewing 19 instruments measuring the doctor-patient relationship, found very different conceptualizations of the nature of this relationship across instruments, with some frequently occurring themes like “alliance,” including shared goals and collaboration, “empathy,” “trust,” and “relational communication”.51 Given patients’ dependence on clinicians in the hospital environment, we need clarity on how different aspects of the clinician-patient relationship influence patient engagement in safety, and how the design of patient safety interventions should support that relationship. To address this need, we conducted a series of interviews with patients and caregivers in the hospital, in both adult and pediatric settings, to understand their needs and desires for engaging with their care. In this paper, we describe how different aspects of the clinician-patient relationship inhibited or promoted patient and caregiver engagement in error prevention. We discuss the implications of our findings for the design of patient-facing safety technologies in the hospital. Our findings suggest new possibilities for how patient-facing information technology can help patients prevent medical errors.
Methods
We conducted two interview studies with hospitalized patients and their caregivers, at a children’s hospital and an adult-only hospital in an urban setting, to understand what kinds of tools could help hospitalized patients and their family members engage with their safety. We describe each study below. Both studies were approved by the researchers’ Institutional Review Board, and in both studies, we employed a maximum variance sampling strategy to recruit patients and caregivers from different services and conditions.
Study 1: Low-fidelity prototype interviews, “L-”
To understand how information technology could meet the needs of hospitalized patients and their caregivers, we conducted semi-structured interviews with patients and caregivers at both sites. In these interviews, we offered patients a set of “feature cards” depicting low-fidelity designs of different features that could be included in a patient-facing system. The features included communicating with clinicians, tracking the patient’s health status, and viewing information from the EHR (see Fig 1. for example cards). We asked patients about what features would be important, why they were important, and how they would use or change each feature. In both hospital settings, we conducted the interview with the patient, but invited caregivers present in the room to participate. In the children’s hospital setting, we also conducted 3 interviews with caregivers (L-Y13, L-Y14, L-Y15) to expand our sample. In all, we conducted 12 interviews with patients and 3 with caregivers at the children’s hospital, and 15 interviews with patients at the adult hospital, for a total of 30 interviews. Our pediatric patients’ ages ranged from 7 to 17 (mean and median age 10.5), and our adult patients’ ages ranged from 18-75 (mean 57.5, median 64). Across both groups, 15 participants were female and 15 male; 27 participants were White, 1 African-American, 1 Native Hawaiian, and 1 Asian. 3 additionally said their ethnicity was Hispanic/Latino. We did not collect information about participants’ specific conditions, but participants were recruited from a range of services including medical, hospitalist, surgery, hematology-oncology, and pulmonology. The interviews lasted 40-60 minutes each.
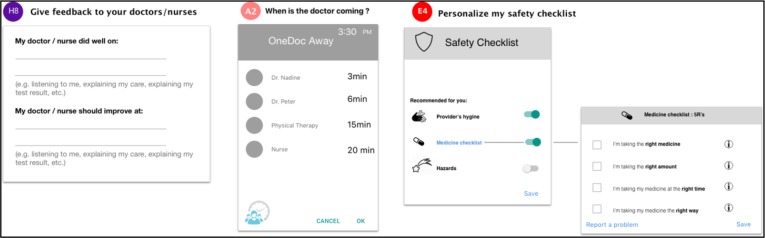
Figure 1.
Example “feature cards” showing a way to give clinicians feedback (H8), the arrival time of the doctor to the patient’s room (A2), and a personalized safety checklist (E4 and the card to its right).
Study 2: Tracking interviews, “T-”
To understand the needs of hospitalized patients and their caregivers to keep track of information about their care in the context of error prevention, we conducted another round of semi-structured interviews at the same two hospital sites. In Study 2, subjects participated in up to 2 interviews occurring during their stay and 1 follow up interview post-discharge. In Interview 1, we asked participants to sketch the ending to a story that starts by describing a hypothetical medical error, then we asked follow-up questions about the story they created. We also asked participants about who on their team made them feel safe and what information about their care they wanted to keep track of. If participants were still in the hospital more than 24 hours later, we invited them to participate in a second interview, where we asked follow-up questions about how their attitudes had changed since the previous interview. After participants were discharged, we contacted them by phone to conduct a brief follow-up interview, asking questions about their reflections on their stay, what information would have been useful for them to keep track of, and whether they had experienced any undesirable events during their stay. Interview 1 typically lasted 40-60 minutes; Interview 2 typically lasted 30-40, and Interview 3 typically lasted 10-20 minutes. As in Study 1, we focused our interview on the patient, but invited caregivers in the room to participate if they wanted to. We interviewed a total of 14 patients at the adult hospital and 13 patients at the children’s hospital. Our pediatric participants’ ages ranged from 9-17 (average age 12.9, median age 13), with 6 male and 7 female participants. Our adult participants’ ages ranged from 34-78 (average age 61.9, median age 69), with 4 male and 10 female participants. Across both groups, 16 were White, 2 African-American, 2 Asian, 3 said they were another race, and 4 preferred not to answer. 3 participants additionally said their ethnicity was Hispanic/Latino. As before, we did not collection information about participants’ specific conditions, but they were recruited from a range of services including medical, surgical, and rehab. Because not all participants were eligible for Interview 2 and some participants were lost to follow up, we conducted a total of 53 interviews in Study 2.
Analysis
The interviews from Studies 1 and 2 were transcribed with identifiers removed. A member of the research team thematically coded the transcripts from both studies in an iterative process. Although the focus of our studies was initially on patients’ information needs and the tools that could support them, themes relating to how patients and caregivers interacted with their clinicians arose from our data. As part of the analysis of these themes, a member of the research team held discussions with other members of the research team and iteratively coded the data to examine the role of the clinician-patient relationship in patient engagement.
Findings
Overall, our studies revealed a population deeply invested in engaging with their care. However, different aspects of the clinician-patient relationship either promoted or inhibited participants’ desire to engage in their safety. This influence occurred even with safety behaviors that did not obviously deviate from the traditional patient role, and was exhibited by both patient and caregiver participants. Below we discuss how participants’ desires to trust, keep the peace with, and protect their clinicians inhibited their engagement with their safety, while their desire to ease clinicians’ burden and their sense of personal connection with their clinicians promoted their engagement. We count as engagement with safety any behavior related to information-seeking about care or care schedule, communicating problems to clinicians, and actively monitoring and involving oneself in care.
We refer to participants from Study 1 with an “L-” prefix, and participants from Study 2 with a “T-” prefix. Participants from the children’s hospital are denoted with a “Y” and participants from the adult hospital with an “A”. Caregiver participants are denoted with a “-C” suffix.
Aspects of the Clinician-Patient Relationship that Inhibited Engagement
We found that participants were discouraged from engaging with their safety due to several factors: trusting clinicians, keeping the peace, and protecting clinicians’ feelings or professional interests. Sometimes these factors were powerful enough to stop participants from engaging with their safety at all; in other cases, participants reported the factor as a concern even if they acted anyway.
Trusting clinicians
For some participants, trusting their clinicians demotivated them to engage with their safety. Several participants were reluctant to seek out information about their care because of their trust in clinicians. For example, T-A10 refused to look up information about his upcoming procedure online, saying, “I didn’t want to know too much and I trust the team …. that’s just the way I decided to do it, because again, the bottom line is I trusted the team that they knew what they were doing.” Trust discouraged T-Y03 from tracking his medication schedule: he said, “I don’t keep track of too much because they do do their job around here [sic]”. L-Y04, responding to a feature card depicting a “safety checklist” of actions patients can take to prevent medical errors, explained her lack of interest by saying, “I feel like I trust my doctors and nurses to be taking care of that.” For one participant, trust was such a powerful influence that he said he would not act even if he had reason to suspect a medical error:
I: So if you were suspecting that something is wrong and you′re getting the wrong medication, what would you do to prevent that?
T-A14: I′d just go – I mean, you′ve got to trust somebody. I mean certainly you and everybody that I know aren′t pharmacists, so you′ve got to trust somebody. So yeah, I would end up primarily trusting what they said.
Our findings here illustrate how trust in clinicians, ostensibly part of a positive clinician-patient relationship, erodes patients’ interest in engaging with their safety. This influence is observed both before and during a hospitalization, and inhibits information seeking behavior, possibly the most fundamental act of patient engagement.
Keeping the peace
Participants’ desire to maintain a cordial relationship with their clinicians also discouraged or deterred action, even when the action was not obviously confrontational. In other words, participants worried about potential conflict or friction with clinicians even when the behavior was in line with the traditional patient role. For instance, T-Y08-C was so concerned about the possibility of conflict with his clinicians that he was willing to forego seeing specific information about his child’s plan of care:
“So there′s this path, there′s this workflow which seems to be well documented … . it would be nice to have that to be referred to, but I could also understand if the doctors don′t want me to literally have that referred to, because at the end of the day, for them that′s guidance. They still have to make their judgment based on reading the situation, and I′m sure they don′t want to argue with me about like – hey, your procedure says this and why are we here? So I could also understand why it might be nice for me to know, but it doesn′t necessarily change my outcome and it may end up generating more friction between me and [the clinician].” –T-Y08-C
Participants’ desires to avoid conflict with clinicians had physical and emotional impact. For example, T-A13 was so anxious to keep the peace between her and her nurse that she gave up on her own needs. Although she wanted anesthetic for a gastric tube, “… it sounded like it was a major inconvenience. So I just figured oh, what the heck, I′ll try it without. … I didn′t really want to go ahead and tick her off too much more than what I obviously did with my question.” As a result, “I threw up a lot. It was very uncomfortable.” In another case, because of T-A12’s equipment and fall risk, she and her caregiver were supposed to summon a nurse to help her go to the bathroom, but as T-A12-C said, “I don′t mind stepping in and helping them. I know it′s a busy job….” Although they knew what to do and made the trip on their own, they described significant anxiety about causing conflict with clinicians. T-A12 expressed her concern, saying, “ We’re laughing, but if she’d have caught us, it wouldn’t have been funny.” Both T-A12 and her caregiver felt ashamed of their own anxiety to please their clinicians, likening themselves to “little bitty kids, afraid that Mommy and Daddy are [going to find out]”, but nevertheless could not shake their worries about “break[ing] their rules” and causing conflict.
Our findings here show that a reluctance to challenge or cause conflict with clinicians extends not just to more clearly confrontational behaviors like asking clinicians if they have washed their hands(3,14,49), but also to information seeking (in the case of T-Y08-C), incipient self-management (T-A12 and her caregiver), and requests for pain management support (T-A13). Additionally, patients and caregivers suffered considerable emotional and physical distress to maintain what they saw as a positive relationship with clinicians.
Protecting clinicians
Participants also exhibited a desire to protect their clinicians’ emotional or professional needs that at times interfered with their desire to engage with their own safety. Some participants were reluctant to seek out information because of these empathetic impulses. L-A02, responding to a feature card about getting second opinions while in the hospital, made a point of saying that even though he would be willing to seek out a second opinion, he would try “[n]ot being rude or anything”. L-A08, responding to a feature card that displayed when the doctor would visit their room, was concerned that her clinicians would be hampered in their job performance by such a tool because they “don′t … have the flexibility to give other people more time when they need it.” L-A04, responding to the same card, felt that although the information would be valuable to her, it would impose an undue burden on her clinicians. She voiced concern not just that her clinicians would be “very busy”, but that the clinician might feel uncomfortable if they could not show up as planned: “And of course it would be awkward for him to say ‘I′m going to stop by in the morning’ because something might come up and he might not do it.” Notably, L-A04 did desire such information about her clinicians’ whereabouts as long as it did not appear to constrain or burden them: when offered the alternative of a “marauder’s map” of the hospital—a map showing the location of everyone in the hospital—she responded positively: “… that would answer your question and my question, like when is my doctor going to be in the area, and did he choose to come visit me during that time. That would work.”
A couple of participants were reluctant to report undesirable events because of their concern over repercussions to hospital staff. L-A14 observed an aide not wearing gloves in a situation where he would be exposed to blood. Although she ultimately reported the incident, she “really debated whether I should say anything because I didn′t want to get him in trouble”. Similarly, T-A12-C was reluctant to report his and his wife’s fear of clinicians’ wrath after the bathroom incident, because he “didn′t want to get any of the staff in trouble or have anybody imply that they weren′t giving the care that they should be giving”.
Our findings here suggest that patients and caregivers feel so connected to their clinicians that they desire to protect them, and are at times willing to sacrifice their own information needs to do so. Moreover, patients’ and caregivers’ desire to protect the clinicians they work with opposes their desire to report undesirable events, meaning that problems observed by patients can go unaddressed, ultimately impacting the quality of care in the hospital.
Aspects of the Clinician-Patient Relationship that Encourage Engagement
By contrast, some aspects of the clinician-patient relationship encouraged participants to engage with their safety. Participants were motivated to engage with their safety by two factors: desiring to ease clinicians’ burden, and feeling a personal connection to clinicians.
Easing clinicians’ burden
Some participants engaged with their care and safety because they wanted to ease the burden on clinicians. As mentioned above, T-A12-C decided to help his wife go to the bathroom without clinician assistance because he felt they were busy and wanted to help them out by taking on a part of their duties. T-A13 likewise made a point of taking care of her own ileostomy bag, saying, “I don′t like … causing grief for anybody, and I know that they go ahead and work hard, so if there′s things that I can … do to make their job easier, you know, I will … do my best to do that.” Hearing a patient across the hall voicing his discontent, she took it upon herself to be an especially easy patient: “… I … listen to the gentleman across the hall, so I figure you′ve got to have somebody that′s not quite that challenging.”
A couple of participants wished they could ease the burden on their clinicians by doing more research on their own but felt they did not have the resources. Responding to a feature card that would give them access to care-related information digitally in their room, both L-Y13 and L-A05 discussed how being able to look up information on their own would let them take up less of clinicians’ time. As L-A05 put it, “… I don’t like bugging people all the time. I’d like a separate resource that I can look at that sort of reinforces what the staff is saying.”
Our findings illustrate how patients’ and caregivers’ desire to help clinicians can motivate information-seeking about their hospital care and nudge patients towards greater self-management, both of which could improve patients’ safety and health outcomes.
Feeling a personal connection
Feeling a personal connection to their clinicians enabled some participants to engage with their care. T-Y13 said they were more comfortable asking their nurses questions “since I have known them for a few years.” T-Y02’s sense of personal connection came from “when the nurses care, like ask me questions about my life, like my siblings and stuff like that. It makes me feel more comfortable and actually want to ask them questions” Another participant, L-A07, described how important it was to him to understand why his clinicians had decided to work in healthcare in the first place: “to know that you have people who are just not here 8 to 5, but they′re here because … they feel good about helping. … once you realize they are our family in a sense, these are my community, that … would make me feel more comfortable.”
This sense of personal connection did not stem from a single source: amongst our participants it seemed to come from a sense of feeling cared for (T-Y02), a sense of clinicians as people (L-A07), or simply familiarity over time (T-Y13). Despite the elusive nature of this personal connection, our findings demonstrate its importance in encouraging patients to engage actively with their care.
Discussion
Our findings demonstrate that aspects of the clinician-patient relationship can either encourage or inhibit patient and caregiver engagement in safety. The clinician-patient relationship exists independently of technology, in the face-to-face encounters that lie at the core of medical practice. However, as information technology becomes increasingly central to the practice and consumption of medicine, designers of these technologies have the opportunity to advance the clinician-patient relationship to promote patient engagement, and to mitigate the influences that inhibit engagement. Below we discuss two ways patient-facing technologies could address these inhibiting factors and encourage patients to engage in safety behaviors by both supporting non-confrontational communication with clinicians, and framing safety behaviors as collaborative acts that reduce clinicians’ burden.
Supporting non-confrontational communication
We describe two ways to support patients in non-confrontational communication with clinicians: provision of health-and care-related information up front, and provision of alternate channels for reporting concerns and expressing needs.
Provision of health- and care-related information up front
Participants in our studies expressed worry about both real and potential conflict with clinicians. At times, this worry dissuaded them from seeking information about their care, even though having such information provides an important strategy in patient safety interventions. Our findings suggest that patients would be more willing to learn information about their care if they felt that it was normal or that clinicians expected for them to know it. One way to set up that expectation would be for the healthcare organization to provide that information, rather than requiring patients to seek it elsewhere. For example, T-Y08-C, who was worried about conflict with his son’s clinicians if he knew too much about the plan of care, might have been less worried if the hospital had provided him with information about clinical pathways directly, and thus implicitly endorsed his engagement efforts. In addition, our findings suggest that information should be provided in a way that does not appear to impose new burdens on clinicians. Just as L-A04’s concern about clinicians being forced into a scheduled visit time was resolved by the “marauders’ map”, patients might be more accepting of new informational features if they do not feel that clinicians are being forced into anything. For example, when patients are granted access to traditionally inaccessible information, such as progress notes and other content from the EHR, patients could benefit from knowing when clinicians chose to share that information with them. If the system has an opt-out for clinicians so that they do not have to share information, like OpenNotes installations,52 patients could be informed that clinicians have the ability to keep information private when they choose to do so, so that they know that their clinicians were not obliged or forced to reveal anything they did not feel comfortable sharing.
Provision of alternate channels for reporting concerns and expressing needs
Our findings about participants’ desire to keep the peace and their reluctance to report concerns point to the need for non-punitive communication channels. Patients should have ways to report concerns and communicate their needs where they feel confident that neither they nor the clinicians they rely on will suffer negative consequences.
This finding suggests a need for helping patients report undesirable events in a way that highlights their potential for helping clinicians improve their practice, rather than the potential for retribution. In other words, patient-facing reporting systems should stress the value of reporting to provide clinicians constructive feedback and improvement rather than punishing clinicians. One approach, adopted by Couture et al. in MySafeCare, is to allow patients to report concerns anonymously, coupled with the option to submit positive feedback.16 Another possibility is to enable patients to give private, electronic feedback, anonymous or otherwise, to the clinicians responsible for the concern. Thus, patients could give constructive feedback to clinicians without worrying about harming the clinicians professionally, and in a technology-mediated, non-confrontational way. Researchers should explore ways to support this feature while ensuring confidentiality, for instance by allowing patients to set a timer on the report, so that patients can describe the details in the moment but not submit the report until sufficient time has elapsed that they are not easily identifiable.
Patients and caregivers are sometimes concerned that voicing their needs will bring negative repercussions from the clinicians who care for them, as in the example of T-A13. To help patients and caregivers in this position, researchers should investigate whether helping patients switch providers within the hospital setting would empower them to communicate their needs without fear. Designers of patient-facing systems could set the expectation that it is ok for patients to request care from different clinicians, for instance to request a different clinician, or even to request a chance to speak with a different clinician, so that patients do not feel stuck with a clinician with whom they have a negative relationship. However, this strategy could also make patients feel as though they are going behind a clinician’s back, or make them worry about harm to the clinician’s professional reputation. Such strategies also impact the hospital’s ability to provide efficient care. Thus, this strategy requires further investigation.
Framing safety behaviors as collaborative acts
We found that patients refrained from performing safety behaviors out of a desire to shield clinicians from emotional or professional injury, but that they were motivated to perform safety behaviors by a desire to collaborate with clinicians and share the load. These findings suggest that reframing safety behaviors as cooperative acts could promote patient engagement. One method we suggest exploring is to provide a shared checklist of safety-related behaviors with tasks assigned to both clinicians and patients. For example, patients could be tasked with confirming that their medication is correct or reading a brief passage about their care. Transparently assigning tasks to both parties could help cultivate a sense of teamwork between patients and clinicians, especially if participation is framed as helping clinicians and contributing to the team, rather than simply ensuring personal safety, and could facilitate conversations about safety between clinicians and patients. If self-management related tasks are included on the shared checklist, then this feature also has the potential to help clinicians monitor patients’ progress towards building the self-management skills they will need when they are discharged, and to help patients build their self-efficacy for self-management. Building self-efficacy is an important part of preparing patients for discharge.18
Another challenge that arises from our findings is how to motivate patients to engage in their safety without damaging the trust in clinicians that discourages them from doing so. We suggest that researchers explore the potential of commitment statements to encourage patient engagement. Building on recommendations that clinicians invite patient participation and comment,48,53 we suggest framing patient engagement in care as a commitment that patients make to their care team, to engage with their safety to the extent they are able. Patients could be encouraged to commit to performing specific actions of their own choosing: for example, patients could pledge to speak up about their concerns or even commit to double-checking that they are receiving the correct medications. Researchers can use patient-facing systems both to ask patients to make these commitments and to remind them of their commitments throughout their stay. For example, patient-facing systems could send just-in-time reminders to patients of their commitments to double check that they are receiving the right medication just before medication administration time. Asking patients to commit to engaging in their safety may mitigate the discouraging influence of excessive trust in clinicians described in our findings without eroding that trust itself.
Limitations and Future Work
Because the clinician-patient relationship influences patient engagement in complex ways, we caution that technologies built to support the motivating aspects of the clinician-patient relationship must be evaluated to ensure they do not cause new problems for people who are already engaged with their safety. In addition, we emphasize that that technologies should be used to supplement face-to-face communication, rather than completely replacing that communication.
In addition, although we describe how aspects of the clinician-patient relationship affect engagement, we do not offer a comprehensive model of the clinician-patient relationship. Future work should assess how other aspects of this relationship affect patient engagement in safety. A comprehensive model of how different aspects of clinician-patient relation affect safety behaviors in different healthcare contexts (e.g. both inpatient and outpatient settings) could be used to develop interventions to help patients participate more actively in their care. In addition, future work should evaluate the intervention techniques suggested in this paper.
Conclusion
Patients’ willingness to perform safety-related behaviors is influenced by their relationship with their clinicians. Our findings shed light on how different aspects of the clinician-patient relationship motivate or discourage patients from engaging with their safety. We discuss how patient-facing technologies could support the motivational aspects of this relationship while mitigating the inhibiting influence of other aspects of the clinician-patient relationship. We suggest that designing patient-facing technology to facilitate non-confrontational communication with clinicians could frame safety behaviors as collaborative acts that would encourage safety engagement. These approaches have the potential to help patients to engage with their safety and prevent unnecessary harm in the hospital.
Acknowledgments
We thank our funding sources: the Agency for Healthcare Research and Quality (grant #1R01HS022894) and the NIH National Library of Medicine Biomedical and Health Informatics Training Grant at the University of Washington (grant #T15LM007442). We also thank our participants, our two research sites (Seattle Children’s Hospital and Virginia Mason Hospital), and past and present members of the Patients as Safeguards research team, including Dr. Barry Aaronson, Calvin Apodaca, Erin Beneteau, Rashmi G. Elera, and Jordan Eschler.
References
- 1.Institute of Medicine. To err is human: building a safe health system. Washington, DC: The National Academies Press; 2000. [PubMed] [Google Scholar]
- 2.Institute of Medicine, Committee on the Quality of Healthcare in America Crossing the quality chasm. Washington, DC: Natonal Academies Press; 2001. [Google Scholar]
- 3.Schwappach DLB. Engaging patients as vigilant partners in safety: a systematic review. Med Care Res Rev. 2010;67(2):119–48. doi: 10.1177/1077558709342254. [DOI] [PubMed] [Google Scholar]
- 4.Unruh KT, Pratt W. Patients as actors: the patient’s role in detecting, preventing, and recovering from medical errors. Int J Med Inform. 2007;76(SUPPL. 1):236–44. doi: 10.1016/j.ijmedinf.2006.05.021. [DOI] [PubMed] [Google Scholar]
- 5.Weingart SN, Zhu J, Chiappetta L, Stuver SO, Schneider EC, Epstein AM. Hospitalized patients’ participation and its impact on quality of care and patient safety. Int J Qual Health Care [Internet] 2011;23(3):269–77. doi: 10.1093/intqhc/mzr002. Available from: http://intqhc.oxfordjournals.org/content/early/2011/02/09/intqhc.mzr002.full?°/o3E. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Longtin Y, Sax H, Leape LL, Sheridan SE, Donaldson L, Pittet D. Patient participation: current knowledge and applicability to patient safety. Mayo Clin Proc. 2010;85(1):53–62. doi: 10.4065/mcp.2009.0248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Charmel PA, Frampton SB. Building the business case for patient-centered care. Healthc Financ Manag [Internet] 2008;62(3):80–5. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19097611. [PubMed] [Google Scholar]
- 8.Mosen DM, Schmittdiel J, Hibbard J, Sobel D, Remmers C, Bellows J. Is patient activation associated with outcomes of care for adults with chronic conditions? J Ambul Care Manag. 2007;30(1):21–9. doi: 10.1097/00004479-200701000-00005. [DOI] [PubMed] [Google Scholar]
- 9.Makary MA, Daniel M. Medical error-the third leading cause of death in the US. BMJ. 2016 (May)353:1–5. doi: 10.1136/bmj.i2139. [DOI] [PubMed] [Google Scholar]
- 10.The Joint Commission. Speak Up Initiatives. The Joint Commission; 2018. [Google Scholar]
- 11.AHRQ. 20 tips to help prevent medical errors: patient fact sheet [Internet] Rockville, MD: Agency for Healthcare Research and Quality; 2017. p. 2. Available from: http://archive.ahrq.gov/patients-consumers/care-planning/errors/20tips/20tips.pdf. [Google Scholar]
- 12.Duckworth M, Leung E, Fuller T, Espares J, Couture B, Chang F, et al. Nurse, patient, and care partner perceptions of a personalized safety plan screensaver. 2017;43(4):15–22. doi: 10.3928/00989134-20170313-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schwappach DLB, Frank O, Davis RE. A vignette study to examine health care professionals’ attitudes towards patient involvement in error prevention. J Eval Clin Pract. 2013;19(5):840–8. doi: 10.1111/j.1365-2753.2012.01861.x. [DOI] [PubMed] [Google Scholar]
- 14.Landers T, Abusalem S, Coty MB, Bingham J. Patient-centered hand hygiene: the next step in infection prevention. Am J Infect Control [Internet]. Elsevier. 2012;40(4 SUPPL):S11–7. doi: 10.1016/j.ajic.2012.02.006. Available from: [DOI] [PubMed] [Google Scholar]
- 15.DiGiovanni CW, Kang L, Manuel J. Patient compliance in avoiding wrong-site surgery. J Bone Jt Surg - Ser A. 2003;85(5):815–9. doi: 10.2106/00004623-200305000-00007. [DOI] [PubMed] [Google Scholar]
- 16.Couture B, Cleveland J, Ergai A, Katsulis Z, Ichihara N, Goodwin A, et al. User-centered design of the MySafeCare patient facing application. CIN Comput Informatics, Nurs [Internet] 2015;33(6):225–6. Available from: http://content.wkhealth.com/linkback/openurl?sid=WKPTLP:landingpage&an=00024665-201506000-00001. [Google Scholar]
- 17.Sutton E, Eborall H, Martin G. Patient involvement in patient safety. Public Manag Rev. 2015;17(1):72–89. [Google Scholar]
- 18.Pollack AH, Backonja U, Miller AD, Mishra SR, Khelifi M, Kendall L, et al. Closing the gap: supporting patients’ transition to self-management after hospitalization. Proceedings of CHI ‘16 [Internet] 2016. p. 53245336. Available from: http://doi.acm.org/10.1145/2858036.2858240%5Cnhttp://dl.acm.org/ft_gateway.cfm?id=2858240&type=pdf. [DOI] [PMC free article] [PubMed]
- 19.Miller AD, Pollack AH, Pratt W. 2016. Bursting the information bubble: identifying opportunities for pediatric patient-centered technology. AMIA Annual Symposium Proceedings; pp. 894–903. [PMC free article] [PubMed] [Google Scholar]
- 20.Benham-Hutchins M, Staggers N, Mackert M, Johnson AH, DeBronkart D. “I want to know everything”: a qualitative study of perspectives from patients with chronic diseases on sharing health information during hospitalization. BMC Heal Serv Reseasrch. BMC Health Services Research. 2017;17:529–38. doi: 10.1186/s12913-017-2487-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Park SY, Chen Y. Patient strategies as active adaptation: understanding patient behaviors during an emergency visit. Proceedings of the 2017 CHI Conference on Human Factors in Computing Systems (CHI ‘17) [Internet]; New York, NY, USA: ACM; 2017. pp. 880–892. Available from: http://doi.acm.org/10.1145/3025453.3025978%5Cnhttp://dl.acm.org.libproxy1.nus.edu.sg/ft_gateway.cfm?id=3025978&type=pdf. [Google Scholar]
- 22.Wilcox L, Morris D, Tan D, Gatewood J. Designing patient-centric information displays for hospitals. Proceedings of the SIGCHI Conference on Human Factors in Computing Systems (CHI ‘ 10) [Internet]; New York, NY, USA: ACM; 2010. pp. 2123–32. Available from: http://portal.acm.org/citation.cfm?doid=1753326.1753650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vardoulakis LP, Karlson A, Morris D, Smith G, Gatewood J, Tan D. Using mobile phones to present medical information to hospital patients. Proceedings of the SIGCHI Conference on Human Factors in Computing Systems (CHI ‘12) [Internet]; New York, NY, USA: ACM; 2012. p. 1411. Available from: http://www.bibsonomy.org/bibtex/208d4dca5f0af11730416729e57c5259b/dblp%5Cnhttp://dl.acm.org/citation.cfm?id=2207676.2208601%5Cnhttp://arnetminer.org/publication/using-mobile-phones-to-present-medical-information-to-hospital-patients-3439820.html;jsessioni. [Google Scholar]
- 24.Woollen J, Prey J, Wilcox L, Sackeim A, Restaino S, Raza ST, et al. Patient experiences using an inpatient personal health record. Appl Clin Inform. 2016;7:446–60. doi: 10.4338/ACI-2015-10-RA-0130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wilcox L, Woollen J, Prey J, Restaino S, Bakken S, Feiner S, et al. Interactive tools for inpatient medication tracking: a multi-phase study with cardiothoracic surgery patients. J Am Med Informatics Assoc. 2016;23:144–58. doi: 10.1093/jamia/ocv160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.O’Leary KJ, Lohman ME, Culver E, Killarney A, Smith GR, Liebovitz DM. The effect of tablet computers with a mobile patient portal application on hospitalized patients’ knowledge and activation. J Am Med Informatics Assoc. 2016;23(1):159–65. doi: 10.1093/jamia/ocv058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Vawdrey DK, Wilcox LG, Collins S a, Bakken S, Feiner S, Boyer A, et al. A tablet computer application for patients to participate in their hospital care. AMIA Annual Symposium proceedings [Internet] 2011. p. 142835. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3243172&tool=pmcentrez&rendertype=abstract. [PMC free article] [PubMed]
- 28.Kelly MM, Dean SM, Carayon P, Wetterneck TB, Hoonakker PLT. Healthcare team perceptions of a port- al for parents of hospitalized children before and after implementation. Appl Clin Inform. 2017:265–78. doi: 10.4338/ACI-2016-11-RA-0194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dykes PC, Rozenblum R, Dalal A, Massaro A, Chang F, Clements M, et al. Prospective evaluation of a multifaceted intervention to improve outcomes in intensive care. Crit Care Med [Internet] 2017;45(8):e806–13. doi: 10.1097/CCM.0000000000002449. Available from: http://insights.ovid.com/crossref?an=00003246-201708000-00036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dykes PC, Carroll DL, Hurley AC, Benoit A, Chang F, Pozzar R, et al. Building and testing a patient-centric electronic bedside communication center. J Gerontol Nurs. 2012;39(1):15–9. doi: 10.3928/00989134-20121204-03. [DOI] [PubMed] [Google Scholar]
- 31.Dalal AK, Bates DW, Collins S. Opportunities and challenges for improving the patient experience in the acute and postacute care setting using patient portals: the patient’s perspective. J Hosp Med [Internet] 2017. Available from: http://www.journalofhospitalmedicine.com/jhospmed/article/149080/hospital-medicine/opportunities-and-challenges-improving-patient-experience. [DOI] [PubMed]
- 32.Grossman L V, Choi SW, Collins S, Dykes PC, O’Leary KJ, Rizer M, et al. Implementation of acute care patient portals: recommendations on utility and use from six early adopters. J Am Med Informatics Assoc [Internet] 2017. (February) pp. 1–10. Available from: http://academic.oup.com/jamia/article/doi/10.1093/jamia/ocx074/4103502/Implementation-of-acute-care-patient-portals. [DOI] [PMC free article] [PubMed]
- 33.Bickmore TW, Pfeifer LM, Jack BW. Taking the time to care: empowering low health literacy hospital patients with virtual nurse agents. Proc 27th Int Conf Hum factors Comput Syst - CHI 09 [Internet]; 2009. pp. 1265–74. Available from: http://dl.acm.org/citation.cfm?id=1518701.1518891. [Google Scholar]
- 34.Collins S, Dykes P, Bates DW, Couture B, Rozenblum R, Prey J, et al. An informatics research agenda to support patient and family empowerment and engagement in care and recovery during and after hospitalization. J Am Med Informatics Assoc [Internet] 2017. (June 2017) pp. 206–9. Available from: https://academic.oup.com/jamia/article-lookup/doi/10.1093/jamia/ocx054. [DOI] [PMC free article] [PubMed]
- 35.Weingart SN, Toth M, Eneman J, Aronson MD, Sands DZ, Ship AN, et al. Lessons from a patient partnership intervention to prevent adverse drug events. Int J Qual Heal Care. 2004;16(6):499–507. doi: 10.1093/intqhc/mzh083. [DOI] [PubMed] [Google Scholar]
- 36.Collins S, Couture B, Lilley L, Smith A, Chang F, Gershanik E. 2016. Increased understanding of safety concerns experienced by hospitalized patients and their families through real-time reporting in MySafeCare app. AMIA Annu Symp Proc; pp. 41–2. [Google Scholar]
- 37.Dykes PC, Carroll DL, Hurley A, Benoit A, Chang F, Meltzer S, et al. Fall prevention in acute care hospitals: a randomized trial. J Am Med Assoc. 2010;304(17):1912–8. doi: 10.1001/jama.2010.1567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Greysen SR, Khanna RR, Jacolbia R, Lee HM, Auerbach AD. Tablet computers for hospitalized patients: a pilot study to improve inpatient engagement. J Hosp Med. 2014;9(6):396–9. doi: 10.1002/jhm.2169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Yin L, Ring L, Bickmore T. Using an interactive visual novel to promote patient empowerment through engagement. Proc Int Conf Found Digit Games - FDG ‘ 12 [Internet] 2012. p. 41. Available from: http://dl.acm.org/citation.cfm?id=2282338.2282351.
- 40.Miller AD, Mishra SR, Kendall L, Haldar S, Pollack AH, Pratt W. Partners in care: design considerations for caregivers and patients during a hospital stay. Proceedings of the 19th ACM Conference on Computer-Supported Cooperative Work & Social Computing (CSCW ‘16); New York: ACM; 2016. pp. 756–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Haldar S, Mishra SR, Khelifi M, Pollack AH, Pratt W. Opportunities and design considerations for peer support in a hospital setting. Proceedings of the 2017 CHI Conference on Human Factors in Computing Systems (CHI ‘17) [Internet]; New York, NY, USA: ACM; 2017. pp. 867–79. Available from: http://dl.acm.org/citation.cfm?doid=3025453.3026040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hibbard JH, Peters E, Slovic P, Tusler M. Can patients be part of the solution? Views on their role in preventing medical errors. Med Care Res Rev. 2005;62(1):601–16. doi: 10.1177/1077558705279313. [DOI] [PubMed] [Google Scholar]
- 43.Doherty C, Stavropoulou C. Patients’ willingness and ability to participate actively in the reduction of clinical errors: a systematic literature review. Soc Sci Med [Internet]. Elsevier Ltd. 2012;75(2):257–63. doi: 10.1016/j.socscimed.2012.02.056. Available from: [DOI] [PubMed] [Google Scholar]
- 44.Schwappach DLB, Wernli M. Barriers and facilitators to chemotherapy patients’ engagement in medical error prevention. Ann Oncol. 2011;22(2):424–30. doi: 10.1093/annonc/mdq346. [DOI] [PubMed] [Google Scholar]
- 45.Mishra SR, Haldar S, Pollack AH, Kendall L, Miller AD, Khelifi M, et al. “Not just a receiver”: understanding patient behavior in the hospital environment. Proceedings of the 2016 CHI Conference on Human Factors in Computing Systems (CHI ‘16) [Internet]; New York, NY, USA: ACM; 2016. pp. 3103–3114. Available from: http://doi.acm.org/10.1145/2858036.2858167%5Cnhttp://dl.acm.org/ft_gateway.cfm?id=2858167&type=pdf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.David L.B, Schwappach Olga Frank JK, Mϋller B, Wasserfallen J-B. Patients ‘ and healthcare workers ‘ perceptions of a patient safety advisory. Int J Qual Heal Care [Internet] 2011;23(6):713–20. doi: 10.1093/intqhc/mzr062. Available from: http://intqhc.oxfordjournals.org/content/intqhc/23/6/713.full.pdf. [DOI] [PubMed] [Google Scholar]
- 47.Rainey H, Ehrich K, Mackintosh N, Sandall J. The role of patients and their relatives in “speaking up” about their own safety - a qualitative study of acute illness. Heal Expect. 2015;18(3):392–405. doi: 10.1111/hex.12044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Entwistle VA, McCaughan D, Watt IS, Birks Y, Hall J, Peat M, et al. Speaking up about safety concerns: multi-setting qualitative study of patients’ views and experiences. BMJ Qual Saf [Internet] 2010;19(6):e33–e33. doi: 10.1136/qshc.2009.039743. Available from: http://qualitysafety.bmj.com/lookup/doi/10.1136/qshc.2009.039743. [DOI] [PubMed] [Google Scholar]
- 49.Waterman AD, Gallagher TH, Garbutt J, Waterman BM, Fraser V, Burroughs TE. Brief report: hospitalized patients’ attitudes about and participation in error prevention. J Gen Intern Med. 2006;21:367–70. doi: 10.1111/j.1525-1497.2005.00385.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Scott J, Dawson P, Jones D. Do older patients’ perceptions of safety highlight barriers that could make their care safer during organisational care transfers? BMJ Qual Saf. 2012;21(2):112–7. doi: 10.1136/bmjqs-2011-000300. [DOI] [PubMed] [Google Scholar]
- 51.Eveleigh RM, Muskens E, Van Ravesteijn H, Van Dijk I, Van Rijswijk E, Lucassen P. An overview of 19 instruments assessing the doctor-patient relationship: different models or concepts are used. J Clin Epidemiol [Internet]. Elsevier Inc. 2012;65(1):10–5. doi: 10.1016/j.jclinepi.2011.05.011. Available from: [DOI] [PubMed] [Google Scholar]
- 52.Feldman HJ, Walker J, Li J, Delbanco T. OpenNotes: hospitalists’ challenge and opportunity. J Hosp Med. 2013;8(7):414–7. doi: 10.1002/jhm.2052. [DOI] [PubMed] [Google Scholar]
- 53.Waterman AD, Gallagher TH, Garbutt J, Waterman BM, Fraser V, Burroughs TE. Brief report: hospitalized patients’ attitudes about and participation in error prevention. J Gen Intern Med. 2006;21(4):367–70. doi: 10.1111/j.1525-1497.2005.00385.x. [DOI] [PMC free article] [PubMed] [Google Scholar]