Abstract
Patient adherence to medications is crucial for reducing cardiovascular risk after an acute coronary syndrome (ACS). Although causes for low adherence are diverse, forgetfulness and lack of awareness about treatment importance are accountable for many cases. As a result, medication reminder apps have attempted to tackle this problem. In our work, we present the development of an app with gamification mechanisms to foster adherence and to support the behavior change processes of the Health Access Process Approach (HAPA) theoretical framework. To design our intervention, we relied on a user-centric approach. We listed the main factors related to high and low adherence from the Medication Adherence Reasons Scale (MAR-Scale) and identified functionalities that could address it. We focused in particular on forgetfulness, knowledge and beliefs about medication as the main barriers for adherence. We implemented a quiz and storytelling as gamification strategies to help motivate patients complete their medication journal and to maintain adherence on the long-term.
Introduction
In Switzerland, cardiovascular diseases are the first cause of mortality with close to half of the deaths linked to coronary artery disease [1]. Although preventive measures are well known, their integration into patients’ daily lives remains challenging. After a heart attack and the subsequent acute medical care, secondary preventive measures are recommended to prevent a relapse. As it is a chronic condition, patients will need to start taking daily medication on the long run [2]. Additionally, they often need other medications if they have comorbidities. The patient is therefore confronted to a new or modified daily medication intake, which can impact their lifestyle habits [3].
Implementing health behavior changes such as a new medication routine is a difficult process. Insufficient support or guidance is common, especially as the majority of self-management in chronic diseases occurs away from the healthcare providers [17]. After implementing a new behavior, patients face the additional challenge of maintaining this new behavior over time. A multi-centric study reported increasing medication discontinuation over time, with subsequent higher mortality: nearly a third of the patients stopped therapy only one month after a myocardial infarction [18].
Medication non-adherence has been consistently associated with worse clinical outcomes, higher downstream re-hospitalization rates and a higher use of resources. Despite the care-providers’ efforts to convey the importance of the medications they prescribe, patients have many intentional and/or unintentional reasons for deviating from the treatment plan. The most common factors associated with non-adherence include forgetfulness (50%), having other medications to take (20%), and being symptom-free (20%) [4]. The risk of deviation is further increased with the medication regimen complexity (MRC), a term used to describe the cumulative patient effort required to take medication correctly. MRC increases each time a patient is required to make a decision about taking medication. Following an acute coronary syndrome (ACS), a patient needs an average of five daily medications according to current management guidelines [5].
The cause of medication non-adherence varies among patients and can be broadly categorized as unintentional or intentional [6]. Unintentional non-adherence concerns the intention to take a medication as instructed but failing to do so for some reason (e.g., forgetfulness, carelessness). Unintentional non-adherence is influenced by patient characteristics, treatment factors, and patient–provider issues [7–9]. In contrast, intentional non-adherence involves making a conscious decision not to take a medication as instructed, based on perceptions, feelings, or beliefs [10]. Intentional non-adherence reflects a rational decision-making process by the patient, where the benefits of treatment are compared with the perceptions of adverse effects of the treatment. Characterizing non-adherence may oversimplify the complexities involved with non-adherence, but it helps to illustrates that alleviating non-adherence requires multiple interventions [11–13].
Ubiquitous and easy to use mobile technologies, such as smart-phone/tablet applications are especially promising for tackling medication non-adherence in patients with chronic diseases. Mobile technologies have been utilized and shown to be effective in increasing medication adherence in patients with various chronic medical conditions such as acquired immunodeficiency syndrome, diabetes, and chronic pulmonary obstructive disease. One of the challenges however is to maintain the behaviour changes on the long-term. Gamification has shown promise in engaging users in the long-term, but has not been explored for medication adherence. In our current work, we aimed to develop an app with gamification mechanisms based on the HAPA framework, using a user-centric design, to fostering long-term treatment adherence.
Related work
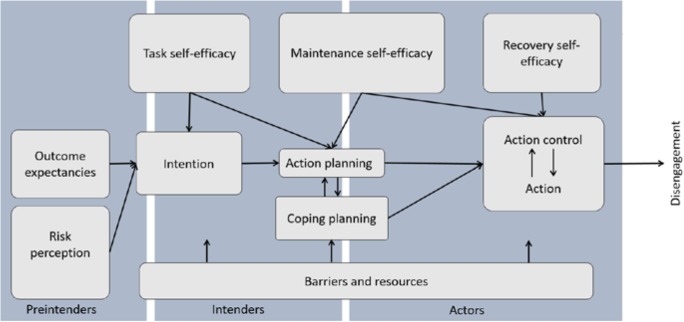
Although many frameworks exist to describe factors related to medication adherence, we decided to focus on the patient-related factors to guide our app development, based on the items of the Medication Adherence Reasons Scale (MAR-Scale, Figure 1) [14,15]. The MAR-Scale is based on the ten most frequently reported reasons for non-adherence identified by Vik et al. [16], retrieved from a literature review of medication adherence. The scale contains five domains ranging from management issues to forgetfulness.
Figure 1.
Medication Adherence Reasons Scale (MAR-Scale)
Behavior change
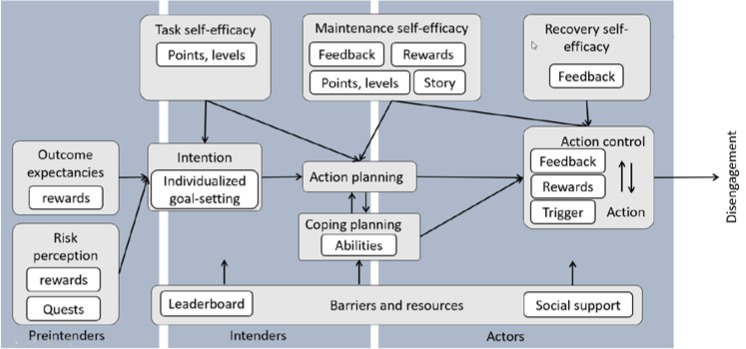
Over 30 different psychological theories have been elaborated for behavior change [19]. When designing an intervention, it is therefore important to choose an appropriate model. The Health Access Process Approach (HAPA) behavior change model contains several interesting concepts (Figure 2) [20]. In particular, it has been applied to a population similar to the one we are targeting, where it was used to study physical exercise adherence after cardiac rehabilitation, in a population similar to the one we are targeting.
Figure 2.
HAPA behavior change model
The HAPA model suggests that behavior is formed through two phases: a motivational phase and a volitional phase. In the motivational phase (characterized by pre-intenders and intenders), individuals form an Intention to perform a behavior, determined by how confident they are in being able to enact the behavior (Self-efficacy), what outcomes might result from engaging in the behavior (Outcome Expectancies) and/or Risk Perceptions about performing (or not performing) the behavior. The volitional phase (represented by actors) describes how these Intentions are translated into behavior. This phase consists of Action Planning (to specify when, where and how to perform the behavior), Coping Planning (how to circumvent anticipated barriers to ensure the behavior is performed), and Action Control (being aware of standards, self-monitoring progress and putting in effort) [21]. Self-efficacy plays a role in both phases, as do barrier resource and social support. The HAPA model can help us understand which modifiable factors determine the Intention to adhere to medication, as well as which post-intentional factors help to ensure that motivation is translated into medication adherence.
Previous HAPA-based studies have found that persons are more likely to adhere to exercises during phase II cardiac rehabilitation (CR) participation [22] and to maintain exercise after completion of phase II CR [23], when they have high maintenance self-efficacy for these behaviors.
Gamification and narratives
Gamification builds on the core idea that people have a natural drive to seek achievement, status, and competition [28]. Video games are fun to play because they give a sense of achievement when one successfully completes a level, usually while being entertained by either the story or the game mechanics itself. Gamification seeks to replicate this sensation by integrating gaming elements in a non-gaming setting. For example, the user may receive a virtual reward after completing a task. To keep people engaged with the intervention, video games use other gaming strategies, such as increasing the level of difficulty over time, or adding a compelling narrative with part of a story that unfolds at each level. Although gamification has been applied to many industries successfully, such as in marketing and in advertising, these strategies have not yet been fully applied in health care settings [29,30].
One of the effective gamification techniques is storytelling. Narratives have already been used successfully in healthcare to motivate behavior change [31,32]. Some elements were identified for success: for example, immersion in a story that users perceive as realistic, and story characters that the users can identify with, increase the probability of a narrative-driven belief change. Narratives, testimonials, and use of personal cases have received considerable attention as effective means of persuasion, and as tools to convey information to promote health behaviors. Narrative persuasion theory suggests that the experience of being absorbed in a story is a key mechanism that can influence real-world beliefs and behaviors [33].
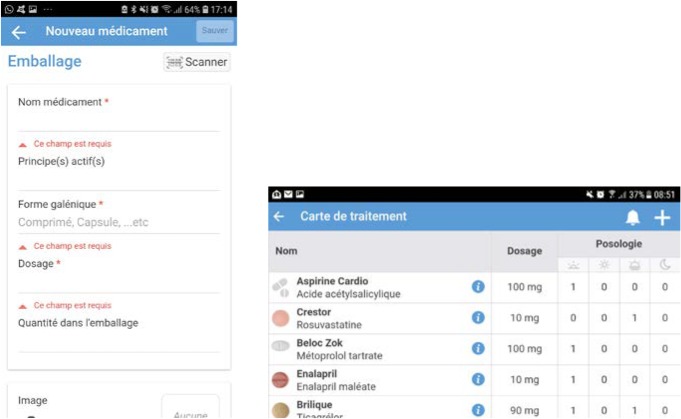
In a prior qualitative study with ACS patients, we proposed a modified HAPA framework, which integrates different gamification elements (Figure 2) [34]. This previous study explored gamification for the four targeted behavior changes for cardiovascular risk factors: smoking cessation, increased physical activity, healthier diet and better medication adherence.
Figure 2.
Gamified HAPA behavior change model
Use of technology
With the increasing popularity of smartphones, people now have access to thousands of health-related apps with many tools to support behavior change. One common aim of medication adherence apps is to help users remember to take their medications. Reminders sent via text messages have been shown to improve adherence in chronic diseases [25]. The recent growth in smartphone users has induced an increase in the number of health-related mobile phone apps available in the app stores, including those dedicated to improving medication-taking behaviors. These medication adherence apps have the potential to address known barriers to adherence with functionalities such as reminders that may help patients take their medications correctly and avoid medication errors [26,27]. This is especially true for patients with high pill burden and complex regimens, such as patients with cardiovascular diseases.
Unfortunately many of these apps are still pretty ineffective. A study by Stawarz [24] demonstrated that most of the available medication reminder apps on the market only have basic reminder functionalities and do not offer an efficient solution to motivate the user toward a better adherence to their medication plan.
There is still a great potential to improve the efficiency of app for medication adherence especially with the use of gamification. In our work, we take a user-centered approach to explore the integration of gamification mechanisms into a mobile app aiming to foster medication adherence. Filling this gap in our understanding of how gamification mechanisms can be integrated will help to ground the design of supportive technologies that can further help patients play an active role in their self-management.
Method
To design our intervention, we looked for app functionalities that could support the adherence and non-adherence factors from the MAR-Scale. In order to maximize adherence, these functionalities were extended to support the constructs from our gamified HAPA theoretical framework. Guided by these frameworks, the application was developed following a user-centric design involving specialists and end-users at each stage of the process. In iterative cycles of requirement and prototyping, we conducted a sequence of focus groups with patients enrolled in a cardiac rehabilitation program. Five patients (4 men, 1 woman) were recruited for this project. Their participation in the different focus groups depended on their availability. The focus groups were used to understand the users’ needs and to provide an adapted solution. More particularly, one focus group was organized to test the usability of the medication summary and another about the use of gamification to support the HAPA model. We also collected informal feedback from a larger patient population (up to 15 patients) on various topics to optimize generalizability. We considered this additional feedback especially important for the health literacy issues, such as the simplified educational texts for medication side effects and usefulness, the content of the quiz and the attractiveness of the story.
Results
Functionalities of medication reminder
During the focus group, we identified the functionalities that help the users address the difficulties associated with the five domains of the MAR-Scale.
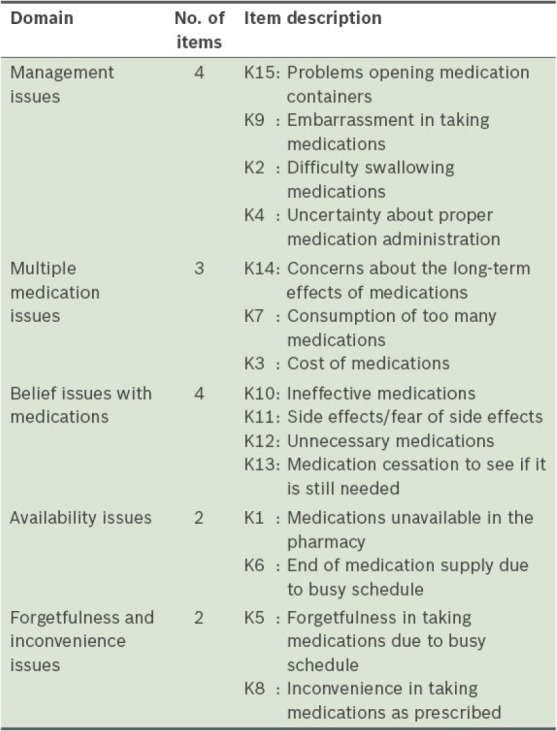
The core functionality of the app supports the users’ medication management issues with an overview of their current medication plan. The user can add a medication to the list by scanning the barcode on the medication box, or by manual entry. A link to a national medication database allows the auto-completion of drug name(s), active ingredient(s) and image(s) of the pills. Scanning the barcode on the medication box allows the user to retrieve all the information linked to the medication in the database, which can then be individualized (dosage, schedule, etc.). This provides a quick, efficient and secure method to create the medication summary. In the case of manual entry, the auto-completion provides existing options and combinations of drug name, dose and image for the user to choose from. Each medication has an associated image (from the database or taken by the user) to help ensure that the proper identification of the medication, particularly when multiple medications are administered at the same schedule.
Once the medication is entered in the summary, the user can set individual notifications for each medication to remind the user to take the medication at the right time. The application also computes the expected end of the medication box and thus sends a reminder to the user to get a refill.
To address the issues related to beliefs and comprehension about medications, we created educational materials for all the coronary heart disease-related medications, as well as for commonly used medications (ex: ibuprofen). These materials were adapted to the users’ health literacy level, and tested with the users. We wanted to help patients acquire a better understanding of their medication, and to help them assess the implications of both adherence and non-adherence to their treatment.. We particularly focused on the known side effects and the reasons for the treatment.
Gamified HAPA model
Although the app functionalities presented above are necessary to support medication adherence, they do not tackle the toughest challenge for adherence: fostering long-term habits. As mentioned above, gamification strategies can help engage the user in the long term, thus helping to maintain the healthy behavior over time, hopefully long enough for the behavior to become a new habit. By applying the gamified HAPA model, there are links between appropriate gamification techniques and each construct of the HAPA model, which help users to progress with their behavior change process. In order to identify how these gamification mechanisms can be translated into concrete functionalities for each construct of the HAPA, we conducted several focus groups with our group of end-users and specialists.
One of the most salient gamification mechanisms in the app is the use of storytelling. As soon as the user starts to use the app she is invited to discover a story about a journey in the mountains. Every day she reports her medication intake, a new section of the story is revealed. Bonus episodes can be unlocked with points, which can be won by responding correctly to a quiz question. The themes of these questions cover not only awareness about medications, but also more general cardiovascular risk and coronary artery disease facts. A team of specialists, including cardiology and pharmacy experts, created the content of the quiz. The questions challenge the user regarding assertions about their treatment or verify their comprehension of the usefulness of specific drugs.
Generation of the storyline
The story in the app is the central piece to engage the user in their behavior change. The story is based on several storytelling techniques aiming at increasing engagement and reinforcing the construct of the HAPA model. The story relies on narrative identification and aims to push the reader to adopt the character’s goals and plans, and to simulate or imagine the events that happen to the character. The user can thus experience empathy or emotions which are in consonance with the success or failure of these plans [35,36].
The story is inspired by an annual outing for ACS patients at the cardiac rehabilitation center of the University Hospitals of Geneva. Patients can take part in a program to prepare for this annual group outing, which is a journey of the ascent of a nearby mountain. The story focuses on the main character who decides to take on the challenge of climbing a summit. It leads us through stages of doubt and excitement, as we observe him as he adopts a new way of life. Initial evaluation of the app by a group of patients showed good acceptance and projection of the reader into the story.
Future works
This app is currently being finalized, and also includes a basic patient education module on coronary heart disease and its management, which have been studied and reported elsewhere. In the near future, we plan to conduct an initial proof of concept study with the app in a population of ACS patients, assessing medication intake, app use, quiz results, as well as pre-post comparisons of questionnaires on health and medication beliefs and knowledge. The final study with the app will focus on studying the effect of gamification to promote long-term behavior changes in this population.
Conclusion
Medication adherence is a key factor in the health outcome of patients suffering of cardiovascular diseases. We present the development of a novel app combining gamification elements with a validated behavior change framework (HAPA) that address the identified barriers to medication adherence. The app has a medication summary with barcode scanning to facilitate data entry and pill images for better identification. It also provides literacy-adapted information about the medications, in particular for the side effects. Storytelling is used to help motivate patients to complete their medication journal, and can help support self-efficacy, by relating to the characters in the story. All the stages have involved patients and experts in a user centric way. A pre-post study aiming to define if patients using the app improve their literacy about their treatment and improve their adherence will be conducted in the near future.
Figure 3.
Data entry screen for new medication and medication summary
Figure 4.
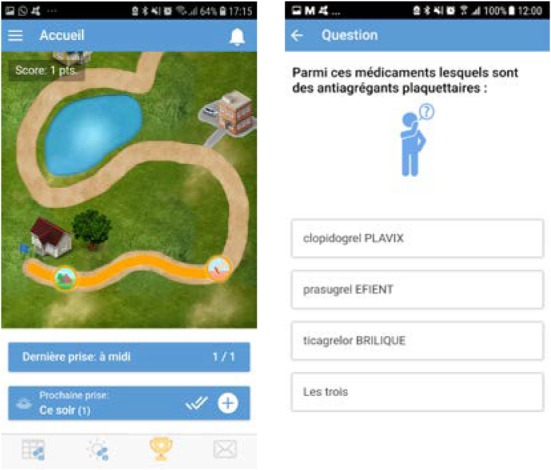
Visualization of the story and quiz to increase medications literacy
Table 1.
Identified functionalities in the app of the IOS and Android app store [15].
| Functionality | Explanation |
|---|---|
| Medication tracking history | Ability to record and track taken and missed doses. |
| Snooze option | Ability to snooze the reminder for a predetermined period of time, for example, 15 minutes. |
| Flexible scheduling | Ability to schedule reminders to occur on a non-daily or monthly basis or every X days, or ability to schedule medications with stop dates. |
| Medication database | Availability of a medication database that allows the user to search and select a medication from the database. |
| Refill reminders | Ability to set reminders to the date when medication needs to be refilled. |
| Reminders with no connectivity | No Internet connection required for the reminders to function. |
| Data exporting and sharing | Ability to export and share the medication information to a third party, for example, family member or healthcare provider. |
| Multiple users support | Ability to generate medication reminders on different medications for more than one user, for example, family members. |
| Notification for other people | Availability of an option to alert other people about when to take their medication or when missed doses are registered. |
| Data security | The app developer ensures data security |
| Data privacy: password protection | Password option to access the app. |
| Multilingual | Availability of languages other than English. |
| Time zone support | Ability to change time zones to ensure medication is taken at the right time when traveling. |
| Adherence rewards | Availability of a feature that rewards the patient when the medication is taken on schedule, for example, awarding points for each medication taken that could be redeemed into vouchers. |
| Adherence statistics and charts | Availability of statistics and charts describing medication usage trends and adherence rates. |
| Customizable alert sounds | Availability of different types of notification sounds. |
| Visual aids | Availability of icons (e.g., tablet, syringe, drops) or ability to add a picture to provide visual clues (e.g., to ensure correct medication is taken) |
Table 2.
Domains of the MAR-Scale and app functionalities identified to support each domain.
| Domain | App functionalities |
|---|---|
| Management issues | Barcode scanning, medication images |
| Multiple medication | Global view on medication plan |
| Belief issue with medication | Quiz, information about medication adapted for patients |
| Availability issues | Reminders, also for refills |
| Forgetfulness and inconvenience issue | Timely notifications as reminders |
Table 3.
Phases of the HAPA model and functionalities identified to support each phase.
| Phase | Construct | App functionalities |
|---|---|---|
| Motivational | Self-efficacy | Badges, progress in the story, visualization |
| Motivational | Outcome Expectancies | Discovery of the story |
| Motivational | Risk Perceptions | Information proposed in the app |
| volitional | Action Planning | Reminders |
| volitional | Coping Planning | Quiz |
| volitional | Action Control | Medication reporting to progress in the story |
| Both | Barriers & Resources | Information proposed in the app, Sharing achievement |
Table 4.
Techniques of storytelling and their interest to support medication adherence
| Technique | Mechanism | Interest |
| Monomyth | Taking the audience on a journey Showing the benefit of taking risks Demonstrating how you learned some newly found wisdom | Outcome Expectancies Risk Perceptions |
| The mountain | Showing how you overcame a series of challenges Slowly building tension Delivering a satisfying conclusion | Self-efficacy |
| Sparklines | Inspiring the audience to action Creating hope and excitement Creating a following | Action Control |
| In medias res | Grabbing attention from the start Keep an audience craving resolution Focusing attention on a pivotal moment in your story | Maintenance |
References
- 1.Berlin C, Panczak R, Hasler R, Zwahlen M. Do acute myocardial infarction and stroke mortality vary by distance to hospitals in Switzerland? Results from the Swiss National Cohort Study. BMJ Open. 2016;6(11) doi: 10.1136/bmjopen-2016-013090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Skinner JS, Cooper A, Feder GS. Secondary prevention for patients following a myocardial infarction: Summary of NICE guidance. Heart. 2007;93(7):862–4. doi: 10.1136/hrt.2007.124321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Steca P, Monzani D, Greco A, Franzelli C, Magrin ME, Miglioretti M, et al. Stability and change of lifestyle profiles in cardiovascular patients after their first acute coronary event. PLoS One. 2017;12(8):1–17. doi: 10.1371/journal.pone.0183905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Aggarwal B, Pender A, Mosca L, Mochari-Greenberger H. Factors associated with medication adherence among heart failure patients and their caregivers. J Nurs Educ Pr. 2015;5(3):22–7. doi: 10.5430/jnep.v5n3p22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pantuzza LL, Ceccato M, das GB, Silveira MR, Junqueira LMR, Reis AMM. Association between medication regimen complexity and pharmacotherapy adherence: a systematic review. Eur J Clin Pharmacol. 2017;73(11):1475–89. doi: 10.1007/s00228-017-2315-2. [DOI] [PubMed] [Google Scholar]
- 6.Hsu C, Lemon JM, Wong ES, Carson-Cheng E, Perkins M, Nordstrom MS, et al. Factors affecting medication adherence: Patient perspectives from five veterans affairs facilities. BMC Health Serv Res. 2014;14(1):1–9. doi: 10.1186/s12913-014-0533-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gadkari AS, McHorney CA. Unintentional non-adherence to chronic prescription medications: How unintentional is it really? BMC Health Serv Res. 2012;12(1) doi: 10.1186/1472-6963-12-98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wroe AL. Intentional and Unintentional Nonadherence: A Study of Decision Making. J Behav Med. 2002;25(4):355–72. doi: 10.1023/a:1015866415552. [DOI] [PubMed] [Google Scholar]
- 9.Lehane E, McCarthy G. Intentional and unintentional medication non-adherence: A comprehensive framework for clinical research and practice? A discussion paper. Int J Nurs Stud. 2007;44(8):1468–77. doi: 10.1016/j.ijnurstu.2006.07.010. [DOI] [PubMed] [Google Scholar]
- 10.Daleboudt GMN, Broadbent E, McQueen F, Kaptein AA. Intentional and unintentional treatment nonadherence in patients with systemic lupus erythematosus. Arthritis Care Res. 2011;63(3):342–50. doi: 10.1002/acr.20411. [DOI] [PubMed] [Google Scholar]
- 11.Foot H, Caze A, Gujral G, Cottrell N. The necessity-concerns framework predicts adherence to medication in multiple illness conditions: A meta-analysis. Patient Educ Couns. 2016;99(5):706–17. doi: 10.1016/j.pec.2015.11.004. [DOI] [PubMed] [Google Scholar]
- 12.Stawarz K, Cox AL, Blandford A, Horne R, Beale R. 2017. Towards Better Medication Adherence Apps: Preventing Forgetfulness By Facilitating The Formation Of Routine-Based Remembering Strategies. Doctoral thesis. [Google Scholar]
- 13.Dayer L, Heldenbrand S, Anderson P, Gubbins PO, Martin BC. Smartphone Medication Adherence Apps: Potential Benefits To Patients And Providers. J Am Pharm Assoc. 2013;53(2):172–81. doi: 10.1331/JAPhA.2013.12202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Unni EJ, Olson JL, Farris KB. Revision and validation of Medication Adherence Reasons Scale (MAR-Scale). Curr Med Res Opin. 2014;30(2):211–21. doi: 10.1185/03007995.2013.851075. [DOI] [PubMed] [Google Scholar]
- 15.Dayer LE, Shilling R, Valkenburg M Van, Hons BS, Bradley C. Assessing the Medication Adherence App Marketplace From the Health Professional and Consumer Vantage Points Corresponding Author. 2017;5(4) doi: 10.2196/mhealth.6582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vik SA, Maxwell CJ, Hogan DB. Measurement, Correlates, and Health Outcomes of Medication Adherence among Seniors. Ann Pharmacother. 2004;38(2):303–12. doi: 10.1345/aph.1D252. [DOI] [PubMed] [Google Scholar]
- 17.Grady PA, Gough LL. Self-management: A comprehensive approach to management of chronic conditions. Am J Public Health. 2014;104(8):25–31. doi: 10.2105/AJPH.2014.302041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ho PM, Spertus JA, Reid FAMKJ, Peterson ED, Magid DJ, Krumholz HM. Impact of Medication Therapy Discontinuation on Mortality After Myocardial Infarction. Arch Intern Med. 2006;166:1842–7. doi: 10.1001/archinte.166.17.1842. [DOI] [PubMed] [Google Scholar]
- 19.Munro S, Lewin S, Swart T, Volmink J. A review of health behaviour theories: How useful are these for developing interventions to promote long-term medication adherence for TB and HIV/AIDS? BMC Public Health. 2007;7:1–16. doi: 10.1186/1471-2458-7-104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Greer AE, Milner K, Marcello R, Mazin K. Health Action Process Approach: Application to Medication Adherence in Cardiac Rehabilitation (CR) Patients. Educ Gerontol. 2015;41(10):685–94. [Google Scholar]
- 21.Presseau J, Schwalm JD, Grimshaw JM, Witteman HO, Natarajan MK, Linklater S, et al. Identifying determinants of medication adherence following myocardial infarction using the Theoretical Domains Framework and the Health Action Process Approach. Psychol Health. 2016;446:1–19. doi: 10.1080/08870446.2016.1260724. [DOI] [PubMed] [Google Scholar]
- 22.Scholz U, Sniehotta2 FF, Schwarzer R. Predicting Physical Exercise in Cardiac Rehabilitation: The Role of Phase-Specific Self-Efficacy Beliefs. J Sport Exerc Psychol. 2005;27:135–51. [Google Scholar]
- 23.Luszczynska A, Sutton S. Physical activity after cardiac rehabilitation: Evidence that different types of self-efficacy are important in maintainers and relapsers. Rehabil Psychol. 2006;51(4):314–21. [Google Scholar]
- 24.Stawarz K, Cox AL, Blandford A. New York, New York, USA: ACM Press; 2014. Don’t forget your pill! In: Proceedings of the 32nd annual ACM conference on Human factors in computing systems - CHI ‘14; pp. 2269–78. [Google Scholar]
- 25.Thakkar J, Kurup R, Laba T-L, Santo K, Thiagalingam A, Rodgers A, et al. Mobile Telephone Text Messaging for Medication Adherence in Chronic Disease. JAMA Intern Med. 2016;176(3):340. doi: 10.1001/jamainternmed.2015.7667. [DOI] [PubMed] [Google Scholar]
- 26.Osterberg L, Blaschke T. Adherence to Medication. N Engl J Med. 2005 Aug;353(5):487–97. doi: 10.1056/NEJMra050100. [DOI] [PubMed] [Google Scholar]
- 27.Santo K, Richtering SS, Chalmers J, Thiagalingam A. Mobile Phone Apps to Improve Medication Adherence : A Systematic Stepwise Process to Identify High-Quality Apps Corresponding Author. 4(4) doi: 10.2196/mhealth.6742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Abdul Rahim MI, Thomas RH. Gamification of Medication Adherence in Epilepsy. Seizure. 2017;52:11–4. doi: 10.1016/j.seizure.2017.09.008. [DOI] [PubMed] [Google Scholar]
- 29.King D, Greaves F, Exeter C, Darzi A. “Gamification”: Influencing health behaviours with games. J R Soc Med. 2013;106(3):76–8. doi: 10.1177/0141076813480996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Edwards EA, Lumsden J, Rivas C, Steed L, Edwards LA, Thiyagarajan A, et al. Gamification for health promotion: systematic review of behaviour change techniques in smartphone apps. BMJ Open. 2016;6(10):e012447. doi: 10.1136/bmjopen-2016-012447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Green MC. Narratives and cancer communication. J Commun. 2006;56(SUPPL.):163–83. [Google Scholar]
- 32.Kreuter MW, Green MC, Cappella JN, Slater MD, Wise ME, Storey D, et al. Narrative communication in cancer prevention and control: A framework to guide research and application. Ann Behav Med. 2007;33(3):221–35. doi: 10.1007/BF02879904. [DOI] [PubMed] [Google Scholar]
- 33.Moyer-Guse E. Toward a theory of entertainment persuasion: Explaining the persuasive effects of entertainment-education messages. Commun Theory. 2008;18(3):407–25. [Google Scholar]
- 34.Blondon K, Meyer P, Lovis C, Ehrler F. Gamification and mHealth: a model to bolster cardiovascular disease self-management. Swiss Med Informatics. 2017;33(0):1–6. [Google Scholar]
- 35.Zillmann D. Exemplification effects in the promotion of safety and health. J Commun. 2006;56(SUPPL):221–37. [Google Scholar]
- 36.Jarva V. Emotion and narrative fiction: Interactive influences before, during, and after reading Raymond. J Futur Stud. 2014;18(3):5–26. [Google Scholar]