Abstract
Determining networks of healthcare providers quantitatively can identify impactful care processes that improve health outcomes for a high-risk populations such as elderly people with multiple chronic conditions. By applying social network analysis to health claim data of a large university in the Midwest, we measured healthcare provider networks of patients with diabetes for two consecutive years. Networks were built based on the assumption that having common patients may indicate potential working relationships between providers. Measures of the social network analysis including degree and betweenness centrality were utilized to identify healthcare providers with an important role in the care process. Both degree and betweenness centrality measures identified a supply center and three laboratories as the central providers of the network for both years. This study can positively impact informed decision-making of policymakers and insurance companies to better design their insurance coverage plans based on the collaboration patterns of the healthcare providers.
Introduction
Approximately 117 million people in the U.S. have at least one chronic condition as reported by the National Health Interview Surveys(1). In a recent report from the Center for Disease Control and Prevention (CDC), population in the U.S. living with diabetes or prediabetes has been estimated to be 100 million(2). Needs and processes for the management of diabetes are often complex and highly varied. Patients with chronic conditions can develop or have already developed multiple comorbidities; collaboration among healthcare providers is key to improving the health outcomes of these patients(3).
Focusing on diabetes, the care team involved are complex and with a wide variety of roles and responsibilities. The care team for patients with diabetes can consist of physicians, nurse practitioners, physician’ assistants, nurses, dietitians, exercise specialists, pharmacists, dentists and mental health professionals(4). Despite large networks and variation in specialties, collaborative approaches among providers have been shown to improve health outcomes of patients with diabetes(5),(6). Researchers have suggested that these collaborations among healthcare providers promote shared problem-solving and decision-making which increase team awareness and facilitate continuous improvement(7). Although benefits of collaboration have been discussed, it remains a challenge to determine quantitatively the care collaboration that are actually occurring in practice and how providers work together, e.g., providers with large influence or central to care (8).
Social network analysis (SNA) is a quantitative approach for the assessment of collaboration among healthcare providers(9). Previous studies have shown that SNA can be applied to survey and interview data collected from providers to identify channels of communication, advise network formation, and change in the workflow(10),(11),(12). Data collected through survey and interview are limited and may not cover all the possible relationships among the healthcare providers(13). Application of SNA to administrative data to identify connections between providers based on their common patients have also been recommended to get a more detailed understanding of the hidden and informal relationship that may exist between the healthcare providers(8).
Social network analysis measures relationships, either formal or informal, to understand how the knowledge and information are shared between the actors of the network(14). In the healthcare domain, SNA has been used to study collaboration between the providers. These relationships have been explored in three domains: hospital social networks, physicians social networks, and referral networks(15). Barnett et al. (2012) used Medicare data to construct networks of 68,288 office-based physicians affiliated with 528 hospitals over a one-year period, and linear regression models were used to evaluate relationships between the hospital network structure including degree and betweenness and hospital spending and care density. The findings showed that hospitals with physicians who had higher number of connections had higher costs and more intensive care(16). Landon et al. (2013) showed that applying SNA to administrative data and using the patient-sharing approach could identify naturally occurring networks of physicians that could form an Accountable Care Organization. Physicians who already had established relationships, had higher chances of delivering coordinated and integrated care(17). Mandl et al. (2014), performed a retrospective analysis of a three-year period data of a single insurer and looked at the recurrence of provider constellations and network cohesion by assessing measures including network density, collaborative pair, triad, provider personal network and constellation. They showed that the prevalence of healthcare providers’ teams that consistently worked together and provided care to one specific patient was rare (18). Thus, SNA techniques have the potential to quantitatively measure care networks; however, current studies primarily characterize the collaborative networks for physicians that provide direct care to patients. Considering the complications of diabetes and different types of the providers that should be included in the process(19), limiting the network to only physicians that offer direct care may fail to include other providers including nurses, nutritionists and pharmacists.
In this study, we used the patient sharing approach and SNA to study network of healthcare providers for patient with diabetes. We assessed healthcare provider types within the network and their relationships by developing the networks based on the patient sharing. Characteristics of the networks (degree, centrality, patient sharing, and density) over a two-year period were used to identify providers with key roles in the care process.
Methodology
Data Source
This study was approved by the university Institutional Review Board. The data source included health claim data of the employees (faculty and staff) of a large university in the Midwest and their dependents (spouse, partners, and children). Dataset was managed by the Regenstrief Center for Healthcare Engineering. The dataset followed individuals who were eligible for the insurance plans from this population for two consecutive years (2012, 2013). This study excluded student population as they had different insurance coverages and plans.
Study Design and Analysis
This is a retrospective analysis of the health insurance claim data. The claim data included eligibility and medical information of the employees (faculty and staff) and their dependents (spouse and child). The eligibility file included demographic data including age, gender, type of compensation (hourly and salary), type of plan, and date of eligibility. The medical file included information such as primary, secondary and tertiary diagnosis, date of service, cost of service, and healthcare provider information. Every eligible individual and every healthcare provider had a unique identifier. Individuals with diabetes and their healthcare providers were identified in 2012 (Year1), and 2013 (Year2) using their unique IDs. To determine population with diabetes, we checked primary, secondary and tertiary diagnoses for the International Classification of Diseases 9th edition code (ICD9) starting by 250. All health services utilization and healthcare providers for the patients with diabetes were extracted from the medical file.
Measuring Healthcare Providers Network
To develop the networks of healthcare providers, we defined a relationship (link, edge, and tie) between two healthcare providers if they had one or more common patients. In the network, the nodes represent the healthcare providers and the edges between them represent the patient shared. The weights of the edges represent the number of patients shared among the healthcare providers.
Measures of the social network analysis described characteristics of the healthcare providers’ networks. The Degree was defined as the number of ties the provider had in the network. The providers that were counted toward the degree number could be any provider that the patient had visited during a one-year period. Another measure was betweenness centrality. Betweenness centrality measured the degree of which a node was ‘between’ pair of other nodes in the network. A node that had higher betweenness centrality had better access to other nodes and more influence on other actors of the network(16). Components of healthcare providers-subgroups of providers all connected to each other- and graph clustering coefficient were measured(20). Density of the network represented proportion of edges in a graph to the maximum possible number of edges(20). All analysis was completed using SAS (v 9.4, SAS Inc., Cary, NC) and RStudio (version 0.99.903) with igraph package (version 1.1.2).
Result
The study cohort of patients included individuals diagnosed with diabetes (N=911). The cohort consisted of 50% women with average age of 53 ± 10 years (age in Year1) and 50% men with average age of 54 ± 11 years (age in Year1). For the study cohort, 57% of the population were 65 years or older. From the study population, 66% were employees (N=599) while 34% were dependents (spouse and children, N=312). In Year1, the study population received services from 2,351 healthcare providers, and in Year2 from 2,273 providers. For both Year1 and Year2 females had higher utilizations compared to males (1,640 vs. 1,322 and 1,499 vs. 1,367). In Year1, the range of providers visited by patients was from 1 to 90 providers and in Year2 from 1 to 50. In both years, the provider type with the highest utilization was an acute care hospital with 541, and 525 patients respectively.
Network Characteristics
The provider network in Year1 is depicted in Figure 1. The circles represent the providers as the nodes; the thicker lines between the nodes represent stronger ties between the providers. The network consisted of 2,348 nodes and 51,955 edges with a density of 0.0188. Eighty-five percent of the edges in the network (44,329) represented observations where only one patient was shared. Eight percent of the edges represented 2 patients shared, 3% represented 3 patients shared, and 4% represented 4 patients or more.
Figure 1.
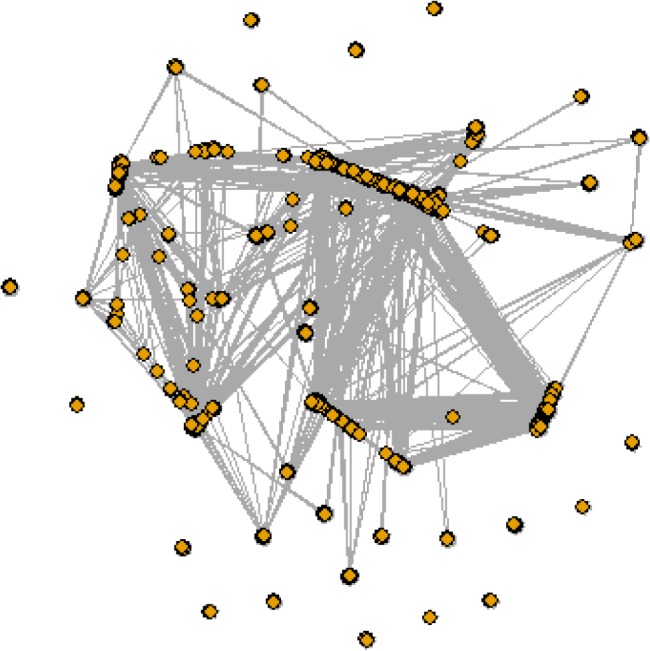
Network of healthcare providers for patients with diabetes in Year1. Node represent the healthcare providers and edges between them represent the patients shared among the healthcare providers. Thicker edges show stronger relationships in other words larger number of patient shared.
We identified the top four providers with highest degree centrality and betweenness. The provider with the highest betweenness centrality (655,960) and degree (1,089) was a supply center providing home care to 164 unique patients. The three other providers were laboratories (Table 1).
Table 1.
Providers with the highest degree centrality and betweenness in Year1
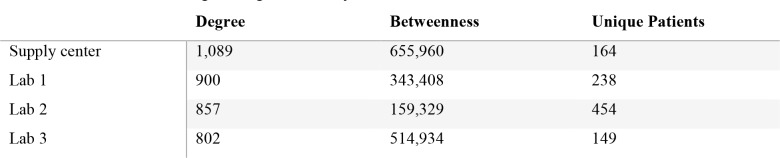 |
The network composed of 15 components; the biggest component with all nodes directly or indirectly connected (20) composed of 2,268 providers with 51,641 edges. The global transitivity of the network was 0.312.
In Year2, the network composed of 2,270 nodes and 44,315 edges with a density of 0.0172 (Figure 2). In Year2 network, 83% of the edges were shaped based on 1 patient shared, 9% based on 2 patients shared, 3% based on 3 patient shared and 5% based on 4 patients shared or more. Similar to Year1, nodes with highest degree centrality and betweenness were further described in Table 2. The node with the highest betweenness centrality (487,403) and degree (893) was the same provider as Year1 with 155 unique patients; 128 of these patient also received services from this provider in Year1. The other three providers with highest degree and betweenness were also the same providers from Year1.
Figure 2.
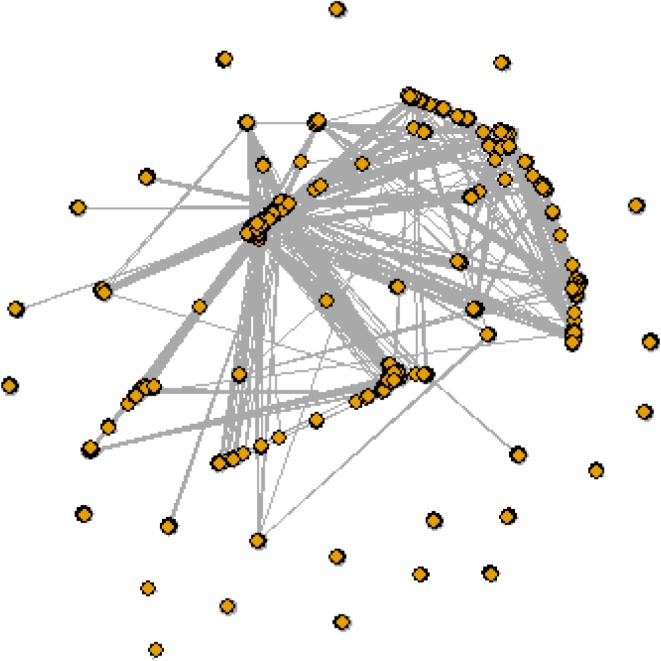
Network of healthcare providers for patients with diabetes in Year2. The nodes represent the healthcare providers and the edges represent the patients shared between them. The thicker edges represent larger number of patients shared among the providers.
Table 2.
Providers with the highest degree centrality and betweenness in Year2
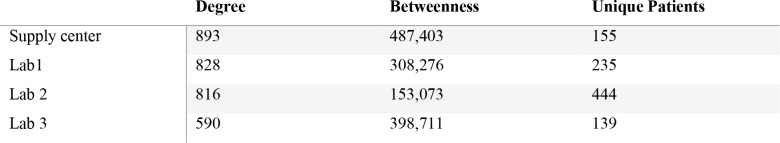 |
The network had 19 components; the biggest component of the network composed of 2,109 nodes and 43,321 edges. The global transitivity of the network was 0.292.
Discussion
This study applied social network analysis to health administrative data for assessing the healthcare providers included in the care process of patients with diabetes. Social network analysis has been used in the healthcare context to assess collaboration of healthcare professionals(9). In recent years, a new approach has been started by researchers to apply SNA to large-scale health data sets and identify relations between providers based on the patient sharing patterns(21). For patients with chronic conditions, there is a need to rethink the service delivery models using perspective from novel approaches to address patients’ increasing health services needs and healthcare costs. Identifying the working relationship and network of healthcare providers informs the policymakers and insurance companies for making informed decision to influence healthcare providers’ behavior and better healthcare delivery management(22), (16).
In the study cohort, women had a higher number of healthcare providers compared to the men in both years of the study. Diabetes might have more significant impact on women as it affects both the mother and their unborn. Women who suffer from diabetes or develop diabetes during pregnancy may face more difficulties during the pregnancy including miscarriages or offspring with complications and impairments(23). Compared to men, women with diabetes are at higher risk for blindness and depression(24). There might be a chance that women associated with this institution include an over-representation of people having sufficient healthcare insurance coverage and receiving improved healthcare. Having gestational diabetes in earlier years and socioeconomic challenges as children have higher impact on developing diabetes for women vs. men(25). Nevertheless, considering the key role of women in performing health-related activities for the family(26), further study regarding healthcare process and path for women with chronic condition is needed to explore ways for improving their health outcomes.
Based on the network of Year1 and Year2, the provider with the highest degree and betweenness was a supply center that provided home care to patients and facilitated the home-based care by variety of services especially after an episode of care and hospitalization. Organizations that offer home health can have a significant role in the care of patients with diabetes as they provide mental and physical stress relief for the patients(27). High betweenness centrality of a provider shows its great influence on the network while the degree shows the number of connections of the provider to other healthcare providers (22). These measures of SNA help to identify key players in the care process for patients with chronic conditions, therefore facilitate informed decision-making of policy makers in defining evidence-based guidelines, policies and plans.
In both years, the providers with highest degree and betweenness (after the supply center) were laboratories. The clinical laboratory has a key role in the diagnosis and monitoring of the disease for patients with diabetes(28). Besides the diagnostic services, clinical laboratories have started to help physicians in the therapeutic decision making. Integrating the laboratory insight with the physicians’ preferences will lead to improved care for the patients(29). Facilitating communication between physicians and laboratory and involving patients in the process will help to move toward a more efficient and transparent healthcare system.
This study has some limitations. The data is limited to one employer only. Based on the employer type and coverage plans, patterns of service utilization may differ for the employee population. Studies that include populations from various types of employers might be helpful to explore impact of employer type and insurance plans on care for patients with diabetes. Identifying meaningful relationships between providers was another challenge. Care of diabetic patients is complicated and requires teams of healthcare providers with various expertise. Therefore, we took a different approach from previous studies and included all providers in the dataset not only the ones from which patients had received direct care. A more complex network algorithm is needed to better identify relationships between healthcare providers from the administrative data. Moreover, despite the patient-sharing approach validation(21) as a method to identify collaborative networks of healthcare providers, relationships identified through this approach may not necessarily mean that those providers who share patients also have constant communication. Another limitation was that we did not have access to the medication file of the study population which included their pharmacy usage. A more comprehensive data set that includes all providers including the pharmacists will be used for the future research. Lastly, health administrative data does not include patient health outcomes, therefore limiting the ability to compare health outcomes of the patients that are treated in different types of provider networks. Datasets with unique patient IDs in medical health records and health administrative data will enable the researchers to compare the outcome of care for patients with diabetes when treated in different types of networks.
Applying social network analysis to large-scale health data is a rising approach that facilitates assessment of healthcare providers collaboration(30),(31),(16),(18). In this study, we looked into network of providers for patients with diabetes based on claim data of a large university in the Midwest. By characterizing network of healthcare providers, the long-term goal of this research is to provide decision support tools for policy makers and healthcare providers and facilitate informed decision-making when designing insurance plans and coverages.
Conclusion
This study applied a new methodology based on the work of Barnett et al. (21) to identify providers included in the process of care for patients with diabetes. Increasing prevalence of chronic conditions and the associated costs and service utilization calls for novel methods to detect provider collaboration teams that minimize the costs and improve health outcomes of the patients. By applying social network analysis to claim data, the approach introduced here helps to expand the impact of data analytics to continuously monitor changes in the network of providers for patients with chronic conditions and the impact on the outcome and costs.
Acknowledgment
Authors would like to acknowledge Regenstrief Center for Healthcare Engineering at Purdue University for providing the data of this study. Authors would also like to thank Bruce Landon and his team from Harvard Medical School-Nancy Keating, James O’Malley, Jukka-Pekka Onnela- for their collaboration and specially Laurie Meneades for sharing her network detection algorithm.
References
- 1.Ward BW, Schiller JS, Goodman RA. Multiple chronic conditions among US adults: A 2012 Update. Prev Chronic Dis. 2014;11 doi: 10.5888/pcd11.130389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.National Diabetes Statistics Report 2017. Estimates of diabetes and its burden in the United States. Center for Disease Control and Prevention. 2017.
- 3.Howard-Thompson A, Farland MZ, Byrd DC, Airee A, Thomas J, Campbell J, et al. Pharmacist-physician collaboration for diabetes care: cardiovascular outcomes. Ann Pharmacother. 2013;47(11):1471–7. doi: 10.1177/1060028013504738. [DOI] [PubMed] [Google Scholar]
- 4.American Diabetes Association. Standards of medical care in diabetes—2017. Diabetes Care. 2017;40(1) [Google Scholar]
- 5.Burke SD, Sherr D, Lipman RD. Partnering with diabetes educators to improve patients outcomes. Diabetes Metab Syndr Obes Targets Ther. 2014;7:45–53. doi: 10.2147/DMSO.S40036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hellquist K, Bradley R, Grambart S, Kapustin J, Loch J. Collaborative practice benefits patients: An examination of interprofessional approaches to diabetes care. Health and Interprofessional Practice. Health Interprofessional Pract. 2012;1(2) [Google Scholar]
- 7.O’Daniel M, Rosenstein AH. Rockville (MD):: Agency for Healthcare Research and Quality;; 2008.. Professional communication and team collaboration. In: Patient Safety and Quality: An Evidence-Based Handbook for Nurses [Internet]. Available from https://www.ncbi.nlm.nih.gov/books/NBK2637/ [PubMed] [Google Scholar]
- 8.Barnett ML, Landon BE, O’Malley AJ, Keating NL, Christakis N. Mapping physician network with self-reported and administrative data. Health Serv Res. 2011;46(5):1592–609. doi: 10.1111/j.1475-6773.2011.01262.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bae S-H, Nikolaev A, Seo JY, Castner J. Health care provider social network analysis: A systematic review. Nurs Outlook. 2015;63(5):566–84. doi: 10.1016/j.outlook.2015.05.006. [DOI] [PubMed] [Google Scholar]
- 10.Keating NL, Ayanian JZ, Cleary PD, Marsden PV. Factors affecting influential discussion among physicians: A social network analysis of a primary care practice. J Gen Intern Med. 2007;22(6):794–8. doi: 10.1007/s11606-007-0190-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Creswick N, Westbrook JI, Braithwaite J. Understanding communication networks in the emergency department. BMC Health Serv Res. 2009;9(247) doi: 10.1186/1472-6963-9-247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mascia D, Cicchetti A, Fantini MP, Damiani G, Ricciardi W. Physicians’ propensity to collaborate and their attitude towards EBM: A cross-sectional study. BMC Health Serv Res. 2011;11(172) doi: 10.1186/1472-6963-11-172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kennedy J, Vargus B. Challenges in survey research and their implications for philanthropic studies research. Nonprofit Volunt Sect Qtly. 2001;30:483–94. [Google Scholar]
- 14.Serrat O. Singapore:: Springer Singapore; 2017. Social network analysis. In: Knowledge Solutions: Tools, Methods, and Approaches to Drive Organizational Performance [Internet]. pp. 39–43. Available from . [DOI] [Google Scholar]
- 15.H Guo, F Wei, S Cheng, F Jiang. 2015. Find referral social networks. In: 2015 International Symposium on Security and Privacy in Social Networks and Big Data (SocialSec) pp. 58–63. [Google Scholar]
- 16.Barnett ML, Christakis N, O’Malley AJ, Onnela J-P, Keating NL, Landon BE. Physician patient-sharing networks and the cost and intensity of care in US hospitals. Med Care. 2012;50(2):152–60. doi: 10.1097/MLR.0b013e31822dcef7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Landon BE, Onnela J-P, Keating NL, Barnett M, Paul S, O’Malley AJ, et al. Using administrative data to identify naturally occurring networks of physicians. Med Care. 2013;51(8):715–21. doi: 10.1097/MLR.0b013e3182977991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mandl KD, Olson KL, Mines D, Liu C, Tian F. Provider collaboration: cohesion, constellations, and shared patients. J Gen Intern Med. 2014;29(11):1499–505. doi: 10.1007/s11606-014-2964-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Diabetes - Symptoms and causes [Internet]. Mayo Clinic. 2014. [cited 2018 Mar 3]. Available from http://www.mayoclinic.org/diseases-conditions/diabetes/symptoms-causes/syc-20371444.
- 20.Luke D. Switzerland: Springer Cham; 2015. A User’s guide to network analysis in R. [Google Scholar]
- 21.Barnett ML, Landon BE, O’Malley AJ, Keating NL, Christakis N. Mapping physician networks with self-reported and administrative data. Health Serv Res. 2011;46(5):1592–609. doi: 10.1111/j.1475-6773.2011.01262.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Landon BE, Keating NL, Barnett ML, Onnela J-P, Paul S, O’Malley AJ, et al. Variation in patient-sharing networks of physicians across the United States. JAMA. 2012;308(3):265–73. doi: 10.1001/jama.2012.7615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Women [Internet]. American Diabetes Association. 2018. [cited 2018 Mar 5]. Available from http://www.diabetes.org/living-with-diabetes/treatment-and-care/women/
- 24.Diabetes [Internet]. womenshealth.gov. 2017. [cited 2018 Mar 5]. Available from https://www.womenshealth.gov/a-z-topics/diabetes.
- 25.Maty S, Lunch J, Raghunathan T, Kaplan GA. Childhood socioeconomic position gender, adult body mass index and incidence of type 2 diabetes mellitus over 34 years in the Alameda County study. Am J Public Health. 2008;98(8) doi: 10.2105/AJPH.2007.123653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Carpenter E. Children’s health care and the changing role of women. Med Care. 1980;18(12):1208–18. doi: 10.1097/00005650-198012000-00006. [DOI] [PubMed] [Google Scholar]
- 27.Linekin P. Home health care and diabetes assessment care, and education. Diabetes Spectr. 2003;16(4):217–22. [Google Scholar]
- 28.Miedema K. Laboratory tests in diagnosis and management of diabetes mellitus. Practical Considerations. Clin Chem Lab Med. 2003;41(9):1259–65. doi: 10.1515/CCLM.2003.193. [DOI] [PubMed] [Google Scholar]
- 29.Panteghini M. The Future of laboratory medicine: understanding the new pressures. Clin Biochem Rev. 2004;25(4):207–15. [PMC free article] [PubMed] [Google Scholar]
- 30.Pollack C, Weissman G, Lemke K, Hussey PS, Weiner J. Patient sharing among physicians and costs of care: A network analytic approach to care coordination using claims data. J Gen Intern Med. 2012;28(3):459–65. doi: 10.1007/s11606-012-2104-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Landon BE, Keating NL, Onnela J-P, Zaslavsky AM, Christakis N, O’Malley AJ. Patient-sharing networks of physicians and health care utilization and spending among Medicare beneficiaries. JAMA Intern Med. 2017;178(1) doi: 10.1001/jamainternmed.2017.5034. [DOI] [PMC free article] [PubMed] [Google Scholar]


