Abstract
In our preceding paper (Part 1), we identified three 1,5-bis-diaryl-1,2,4-triazole-based compounds that merited evaluation as potential positron emission tomography (PET) radioligands for selectively imaging cyclooxygenase-1 (COX-1) in monkey and human brain, namely, 1,5-bis(4-methoxyphenyl)-3-(alkoxy)-1H-1,2,4-triazoles bearing a 3-methoxy (PS1), a 3-(2,2,2-trifluoroethoxy) (PS13), or a 3-fluoromethoxy substituent (PS2). PS1 and PS13 were labeled from phenol precursors by O-11C-methylation with [11C]-iodomethane and PS2 by O-18F-fluoroalkylation with [2H2, 18F]fluorobromomethane. Here, we evaluated these PET radioligands in monkey. All three radioligands gave moderately high uptake in brain, although [2H 2,18F]PS2 also showed undesirable radioactivity uptake in skull. [11C]PS13 was selected for further evaluation, mainly based on more favorable brain kinetics than [11C]PS1. Pharmacological preblock experiments showed that about 55% of the radioactivity uptake in brain was specifically bound to COX-1. An index of enzyme density, VT, was well identified from serial brain scans and from the concentrations of parent radioligand in arterial plasma. In addition, VT values were stable within 80 min, suggesting that brain uptake was not contaminated by radiometabolites. [11C]PS13 successfully images and quantifies COX-1 in monkey brain, and merits further investigation for imaging COX-1 in monkey models of neuroinflammation and in healthy human subjects.
Keywords: COX-1, PET, Radioligand, Brain, carbon-11, fluorine-18
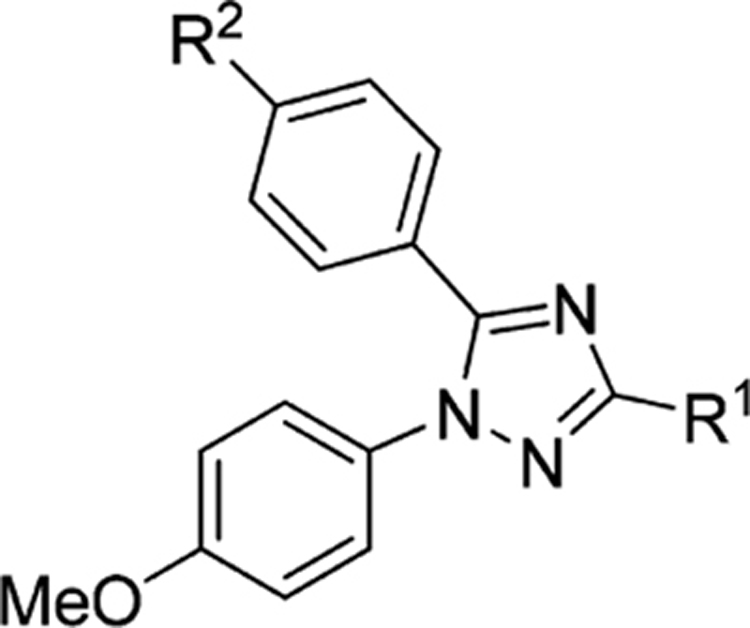
Graphical Abstract
INTRODUCTION
As mentioned in Part 1,1 there has been no positron emission tomography (PET) radioligand suitable for imaging and quantifying cyclooxygenase-1 (COX-1) in primate brain. Such an imaging tool could prove valuable for the investigation of neuroinflammation in neuropsychiatric disorders and could also aid anti-inflammatory drug development.2 The only radiotracer that has been evaluated in human for PET imaging of COX-1 is racemic [11C]ketoprofen methyl ester ((R,S)-[11C]2-(3-benzoylphenyl)propionic acid; [11C]KTP-Me). [11C]-Ketoprofen ([11C]KTP) itself is poorly brain-penetrant, whereas its methyl ester readily traverses the blood-brain barrier.3 However, [11C]KTP-Me rapidly hydrolyzes within brain to [11C]KTP, which is largely retained because of its extensive ionization and hence inability to cross the blood-brain barrier. Despite encouraging results in rodent models of Alzheimer’s disease (AD),4 racemic [11C]KTP-Me was unsuccessful for imaging COX-1 in the brains of human subjects that have AD or mild cognitive impairment.5 A possible explanation is that KTP has only moderately high potency for inhibiting human COX-1 (IC50 = 20 nM1 or 47 nM6). Furthermore, the R-enantiomer of KTP has negligible potency for inhibiting COX-1 and its presence in the administered racemate would only have served to increase nonspecific binding relative to any COX-1 specific binding arising from the eutomer.3 The single more potent S-enantiomer may be obtained with use of chiral HPLC at the end of radiosynthesis.4 Notwithstanding, it is questionable whether a “pro-drug” type radiotracer, such as [11C]KTP-Me, could ever be successful for quantification of COX-1 because of the need to distinguish parent radiotracer ([11C]KTP-Me) from its radiometabolite, ([11C]KTP). Therefore, a readily prepared, high-affinity, and direct-acting radioligand for COX-1 is needed.
In the first stage of our investigation of 1,2,4-triazole-based compounds as potential PET radioligands for imaging cyclooxygenase-1 (COX-1) in monkey and human brain, we identified three COX-1 selective inhibitors, now dubbed PS1, PS2, and PS13 (Table 1), that merited labeling with carbon-11 (t1/2 = 20.4 min) or fluorine-18 (t1/2 = 109.8 min),1 mainly based on their high potencies for inhibiting both monkey and human COX-1, very low potencies for inhibiting the COX-2 isoform, moderate computed lipophilicities, and amenability to labeling (Table 1). We presented methods for their labeling and production for intravenous injection. Here, we report an evaluation of the three PET radioligands in rhesus monkey to test whether any of these three radioligands might be useful for imaging and quantifying COX-1 in human brain. We found that [11C]PS13 ([11C]1,5-bis(4-methoxyphenyl)-3-(2,2,2-trifluoroethoxy)-1H-1,2,4-triazole) shows a moderately high uptake in healthy monkey brain, and that a majority of this uptake represents specific binding to COX-1. Therefore, [11C]PS13 is an excellent candidate to take forward for further evaluation in neuroinflammation models in monkeys, and in healthy human subjects.
Table 1.
Structures and in Vitro Pharmacology Data for the Radioligands Selected for Screening and Evaluation with PETa
RESULTS AND DISCUSSION
Radioligand Production.
Table 2 summarizes the mean radiochemical yields (RCY) and molar activities (Am)7 of the three radioligands produced for this study. The radiochemical purities of all three radioligands exceeded 99%, as measured with analytical HPLC.1 Yields and molar activities were adequate for PET experiments in monkey.
Table 2.
Radioligand Production Parameters
| radioligand | RCY (%) | Am (GBq/μmol)a |
|---|---|---|
| [11C]PS1 | 20 ± 3b | 125 ± 62 (n = 12) |
| [2H2,18F]PS2 | 14 ± 4c | 53 ± 17 (n = 8) |
| [11C]PS13 | 13 ± 3b | 244 ± 130 (n = 19) |
At the end of synthesis, determined by analytical radio-HPLC with UV absorbance detection.1
From cyclotron-produced [11C]carbon dioxide.
From cyclotron-produced [18F]fluoride ion.
Lipophilicities and Plasma Free Fractions.
Lipophilicity influences many characteristics of PET radioligand performance, such as plasma protein binding, brain penetrance nonspecific binding in brain, and metabolism. 8 Generally, moderate lipophilicity, represented by log D in the range 2–3.5, is desirable. The computed lipophilicities (clog D values) of ligands PS1, PS2, and PS13 quite well predicted the measured values (log D’s), which were found to be lower than the computed values for PS1 and PS2 by up to 0.58, and higher for the most lipophilic compound PS13 by 0.67. Computations of log D typically have errors of such magnitude.9 The free fractions (f P) of [11C]PS1, [2H2,18F]PS2, and [11C]PS13 in pooled monkey, and human plasma were found to be low, in accord with their generally moderate to high measured lipophilicities9 (Table 3).
Table 3.
cLog D, log D, and Monkey and Human Plasma Free Fractions of COX-1-Selective Radioligands
| radioligand | clog D | log D (n = 6) | monkey fP (n = 3) | human fP (n = 3) |
|---|---|---|---|---|
| [11C]PS1 | 3.72 | 3.29 ± 0.00 | 0.042 ± 0.001 | 0.036 ± 0.001 |
| [2H2,18F]PS2 | 3.84 | 3.26 ± 0.01 | 0.039 ± 0.001 | 0.021 ± 0.000 |
| [11C]PS13 | 3.59 | 4.26 ± 0.04 | 0.011 ± 0.001 | 0.002 ± 0.000 |
PET Experiments in Monkeys.
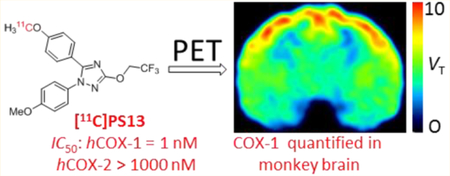
After intravenous injection of [2H2,18F]PS2 into monkey, radioactivity concentration in whole brain peaked at 4.11 SUV (standardized uptake value units) at 7 min and then declined by 74% to 1.05 SUV at 85 min (Figure 1). Three radiometabolites emerged quickly in plasma. By about 25 min, only 50% of the radioactivity in plasma was parent radioligand. These radiometabolites appeared to be less lipophilic than parent radioligand based on shorter retention times in the reversed phase HPLC analysis. Two deuterium atoms had been included in the [18F]fluoromethoxy group as a strategy to minimize possible radiodefluorination in vivo.8,10–12 Nonetheless, the brain image of [2H2,18F]PS2 showed uptake of radioactivity in skull, which is evidence of some radiodefluorination (see the Supporting Information (SI), Figure S1). Because skull radioactivity can be problematic for quantification of radioactivity in brain, this radioligand was not investigated further.
Figure 1.
PET time–activity curves from rhesus monkey whole brain (gray matter) following intravenous injection of [11C]PS1 (n = 1), [2H2,18F]PS2 (n = 1), and [11C]PS13 (mean ± SD, n = 3). The inset expands the data presentation over the early stage of scanning.
After injecting monkey with [11C]PS1, radioactivity concentration in whole brain peaked at 4.26 SUV at 1.75 min and then declined by 85% to 0.62 SUV at 85 min (Figure 1). [11C]PS13 gave similarly high radioactivity concentration in brain after intravenous injection, on average peaking at 4.29 SUV at 9 min and then declining by 54% to 1.99 SUV at 85 min (Figure 1). Brain radioactivity from [11C]PS13 washed out of brain more slowly than that from [11C]PS1 or [2H2,18F]PS2, even though [11C]PS13 cleared more quickly from plasma than [11C]PS1 or [2H2,18F]PS2 (see the SI, Figure S2). This indicated that [11C]PS13 gave potentially the highest COX-1 specific binding in brain (Figure 1), as might have been expected from PS13 having the somewhat higher COX-1 inhibitory potency (Table 1). PS13 has a 3-(2,2,2-trifluoroethoxy) group which might be amenable to labeling13 to provide a potentially useful longer-lived 18F-labeled version of this radioligand. This is not an option for PS1. After full consideration, [11C]PS13 was advanced for further evaluation.
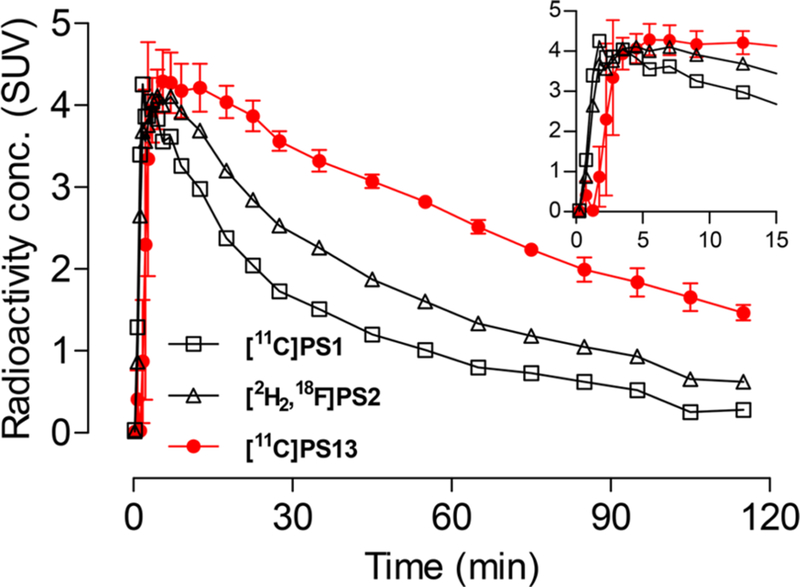
To test for the possible presence of COX-1 specific binding, each baseline PET experiment in monkey was followed at 3 h later with a blocking scan where PS13, KTP-Me as a prodrug for KTP, or MC1 was administered intravenously at about 5 min before the radioligand. KTP has high inhibitory potency for monkey COX-1 ( IC50 = 1 nM) and low inhibitory potency for COX-2 (IC50 = 400 nM).1 MC1 has high potency for inhibiting COX-2 (IC50 = 1 nM) and >1000-fold lower potency for inhibiting COX-1 in both human1,14 and monkey.1 MC1, like KTP-Me, also readily traverses the monkey blood-brain barrier.15 Potency and solubility considerations were taken into account when selecting the doses to be administered intravenously, which were 1, 3, and 0.3 mg/kg for PS13, KTP (as KTP-Me), and MC1, respectively.
In the paired experiments using PS13, radioactivity in whole brain peaked at 2.92 SUV at baseline, and at 3.60 SUV after administration of PS13. At 45 min after radioligand injection these values declined by 36% to 1.88 SUV and 69% to 1.11 SUV, respectively (Figure 2, panel A). In the paired experiment using KTP-Me, radioactivity in whole brain peaked at 2.90 SUV at baseline and at 4.14 SUV after administration of KTP-Me (Figure 2, panel B). At 45 min after radioligand administration, these values were reduced by 43% to 1.65 SUV and by 74% to 1.09 SUV, respectively (Figure 2, panel B). Factors, such as displacement of radioligand from peripheral COX-1, or differences in blood flow, may account for the higher peak radioactivity levels in brain after administration with either of the COX-1 selective agents, PS13 or KTP-Me. Preadministration of these agents also caused much faster washout of radioactivity from brain than at baseline. Accordingly, the areas under the brain time-activity curves in the 60 to 120 min scan interval were higher in the baseline experiments than in the preblock experiments. At baseline in this scanning interval, radioactivity concentration in neocortex was notably higher than in other brain regions.
Figure 2.
PET time–activity curves for whole brain from three rhesus monkeys following injection of [11C]PS13; at baseline and after administration of PS13 (1 mg/kg, i.v.) 3 min before [11C]PS13 (panel A); at baseline and after administration of KTP-Me (3 mg/kg, i.v.) at 5 to 10 min before [11C]PS13 (panel B); at baseline and after administration of MC1 (0.3 mg/kg, i.v.) at 5–10 min before [11C]PS13 (panel C).
In the paired experiment with the COX-2 selective inhibitor, MC1, the peak uptake of radioactivity in brain at baseline (3.73 SUV at 3.5 min) was lower than that after administration of MC1 (4.86 SUV at 3.5 min) (Figure 2, panel C). Subsequently, brain time–activity curves became overlapping, such that there was little difference in the areas under the curves for the 60- to 120 min scan interval. Therefore, no specific binding of [11C]PS13 to COX-2 was evident, in accord with the extremely low potency of MC1 for inhibition of monkey COX-1 in vitro.
Stabilities of Radioligands in Monkey Whole Blood and Plasma in Vitro.
[11C]PS1, [2H2,18F]PS2, and [11C]PS13 were found to be >99% radiochemically stable when stored in monkey whole blood or plasma for 30 min at room temperature. Therefore, blood samples taken from monkey in PET experiments were radiochemically stable during the ex vivo analyses of plasma radiometabolites.
Emergence of Radiometabolites of [11C]PS13 in Plasma.
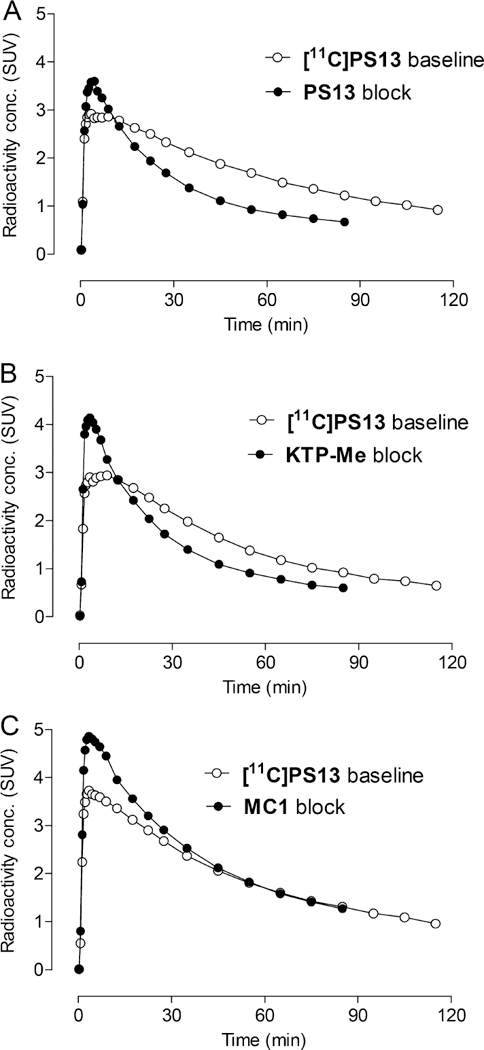
After intravenous injection of [11C]PS13 in baseline and self-block experiments, total radioactivity in plasma declined rapidly. The radioactivity in plasma represented by unchanged [11C]PS13 declined to about 50% at 90 min in baseline and self-block experiments (Figure 3).
Figure 3.
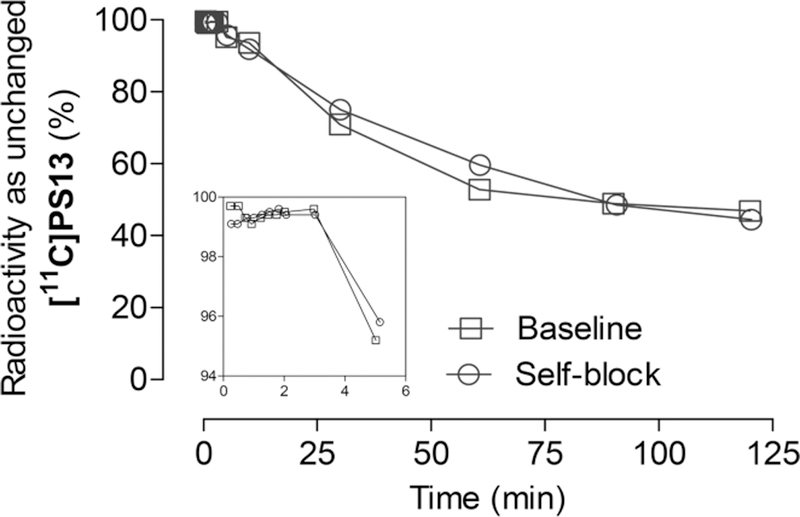
Radioactivity in monkey plasma represented by unchanged [11C]PS13 (%) under baseline and self-block conditions. The inset expands data presentation over the early scanning period.
[11C]PS13 produced four radiometabolites ([11C]A–D) in plasma that eluted before and one radiometabolite ([11C]E) that eluted after [11C]PS13 on reversed phase HPLC. The radiometabolites [11C]A–D were not well resolved from each other, but they were well resolved from [11C]PS13 (Figure 4); their shorter retention times indicate they are appreciably less lipophilic than [11C]PS13, and therefore perhaps less likely to enter brain. The more lipophilic radiometabolite [11C]E was barely perceptible. At 90 min after radioligand injection, the radioactivity in plasma represented by each radiometabolite was: [11C]A = 14.4%; [11C]B = 18.1%; [11C]C = 6.5%; [11C]D = 11.8%; [11C]PS13 = 48.9%; [11C]E = 0.2% (Figure 4).
Figure 4.
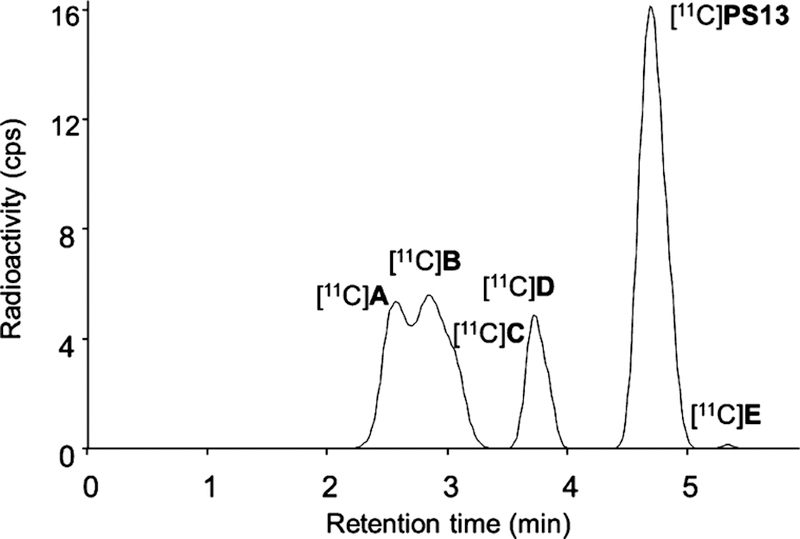
Reversed phase radio-HPLC analysis of monkey plasma at 90 min after the intravenous injection of [11C]PS13.
Kinetic Modeling of PET Data.
For [11C]PS13, the density of the target enzyme, COX-1, was quantified as total volume of distribution (VT), using the Logan graphical analysis noncompartmental model and serial concentrations of parent radioligand in arterial plasma. VT was well identified in all examined brain regions, with identifiability (SE) of 0.1–1.8%. VT for whole brain in baseline experiments quickly stabilized with the length of scanning after radioligand injection that was used for its calculation (Figure 5 ). Thus, VT calculated from the first 80 min of scan data fell well within 10% of the value calculated from the full 120 min of scan data. This strongly indicates the measurement of VT is not influenced by any appreciable influx of any radiometabolites from plasma into brain.
Figure 5.
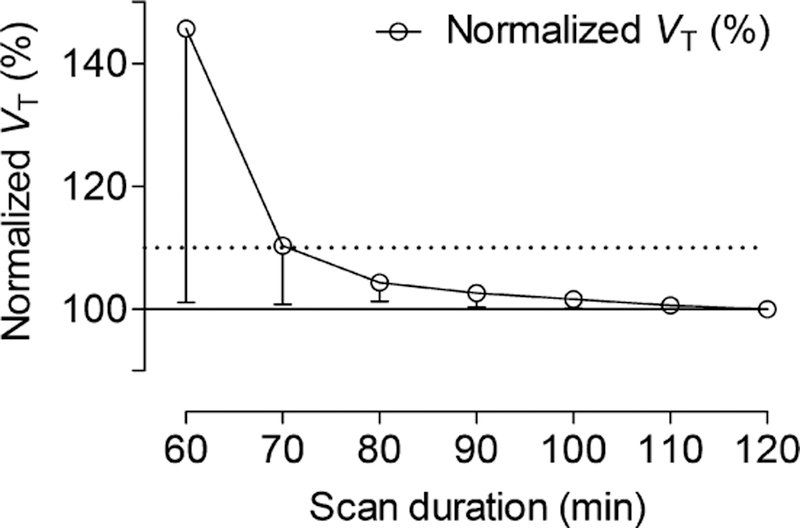
Stability of whole brain VT with duration of scan after [11C]PS13 administration to rhesus monkey at baseline. Error bars are SD for n = 3 (and within symbol size if not shown). Data are normalized to VT at 120 min; 90 min scan duration was sufficient to reliably determine VT.
VT parametric images of [11C]PS13 in monkey brain at baseline showed high uptake in neocortex, with temporal cortex, striatum, thalamus, midbrain and hippocampus, following in descending order (Figure 6, top row). COX-1 is known to be widely expressed in human brain, primarily in frontal, temporal and cerebellar cortices, hippocampus, and caudate.16 There are however no previous reports of the distribution of COX-1 in healthy monkey brain with which to make a direct comparison. Preadministration of PS13 at a dose of 1 mg/kg reduced VT values in all regions by about 55% (Figure 6, bottom row and SI Figure S3). A similar result was obtained when KTP-Me was administered at a dose of 3 mg/kg before [11C]PS13 (Figure 7 and SI Figure S3). Preadministration of the COX-2 selective ligand MC1 at a dose of 0.3 mg/kg had no effect on brain regional VT values, thereby showing that [11C]PS13 has high selectivity for inhibiting COX-1 over COX-2 in vivo as in vitro (Figure 7 and SI Figure S3).
Figure 6.
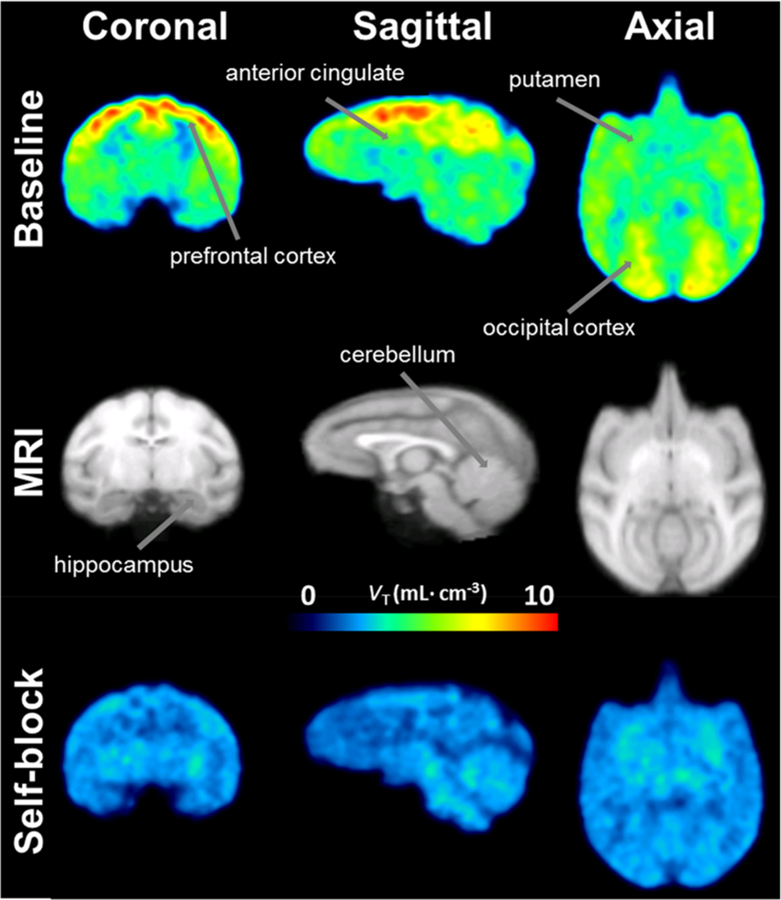
Parametric images of VT for [11C]PS13 in brain of a normal rhesus monkey at baseline (top row) and after blocking with PS13 (1 mg/kg, i.v.; bottom row). Kinetic analysis was performed at the voxel level using a Logan plot, so that the resulting VT values are shown as PET images. The middle row shows template MRI scans.
Figure 7.
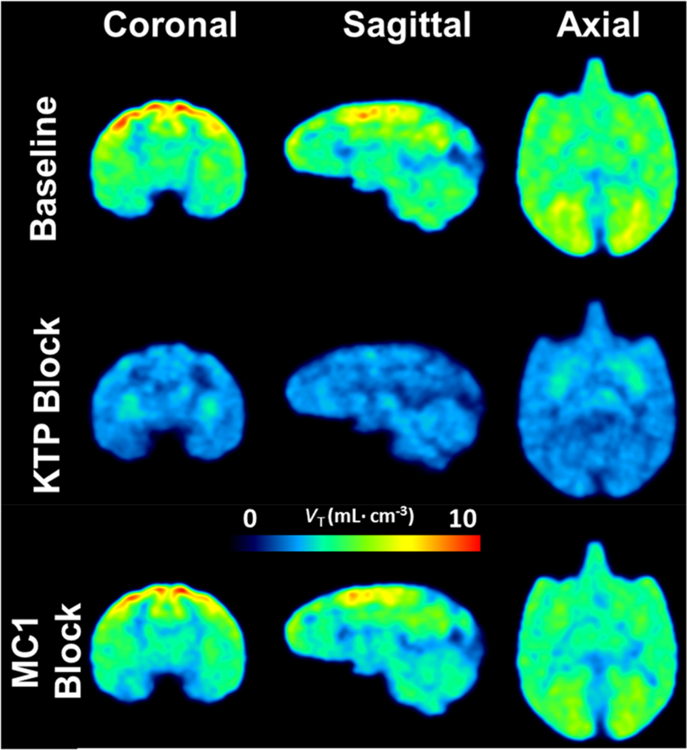
[11C]PS13 binds selectively to COX-1. Parametric images of VT in the brain of a normal rhesus monkey at baseline (top row) and after administration of either KTP-Me (3 mg/kg, i.v.; as prodrug of COX-1 specific KTP; middle row) or MC1 (0.3 mg/kg, i.v.; COX-2 specific; bottom row). Only KTP-Me reduced whole-brain uptake of [11C]PS13.
In the PS13 and KTP-Me preblock experiments the VT values still varied to some extent across brain regions (see the SI, Figure S3). These variations indicate that the preblocks of brain COX −1 by PS13 and KTP (from KTP-Me) were incomplete. However, blocker solubility limitations precluded experiments with higher doses to try to achieve higher blocking effects.
Generally, it is considered that only free radioligand in plasma is available for transit across the blood-brain barrier. Correction of VT by plasma free fraction ( f P) gave similar results as VT (see SI Figure S3). The f P of [11C]PS13 was 0.011 ± 0.001 in monkey plasma and 0.002 ± 0.000 in standard human plasma. These values are low due to high radioligand lipophilicity (logD). For this reason, the VT values for [11C]PS13 are considered more reliable than the VT/f P values. A lower lipophilicity (logD) would be desirable in follow-up radioligands because lower lipophilicity would likely increase f P to an accurately measurable level and reduce nonspecific binding in brain. Ideally, such radioligands would also have higher COX-1 inhibitory potency (as a surrogate for binding affinity) to provide higher COX-1 specific signal. To increase the reliability and reproducibility of our f P measurements, they were done in triplicate in monkey plasma. f P was also measured in pooled plasma from human, which allowed for f P normalization.17 The percent error of the γ-counter measurements of the samples with the least counts was low at 1.3 ± 0.04% (n = 6).
The extent to which COX-1 is occupied by a blocking agent may be estimated graphically using a Lassen plot for several brain regions where the x-axis is VT at baseline and the y-axis is the decrease in VT from baseline to block condition (Figure 8). Major assumptions underlying the Lassen plot are that the radioligand and blocking agent bind selectively to the target, in this case COX-1, and that target occupancy and nonspecific binding are uniform across brain. We found a COX-1 occupancy of 87 ± 4% with 1 mg/kg of PS13, and 72 ± 4% with 3 mg/kg of KTP-Me, based on the slopes of the respective Lassen plots. Using the assumptions of the Lassen plot, VND (the x-axis intercept) was estimated as 2.5 mL/cm3 from the PS13 experiment and 1.8 mL/cm3 from the KTP-Me experiment. The strong correlation coefficients for these plots (Figure 8) indicate that the major assumptions of the Lassen plots were well satisfied.
Figure 8.
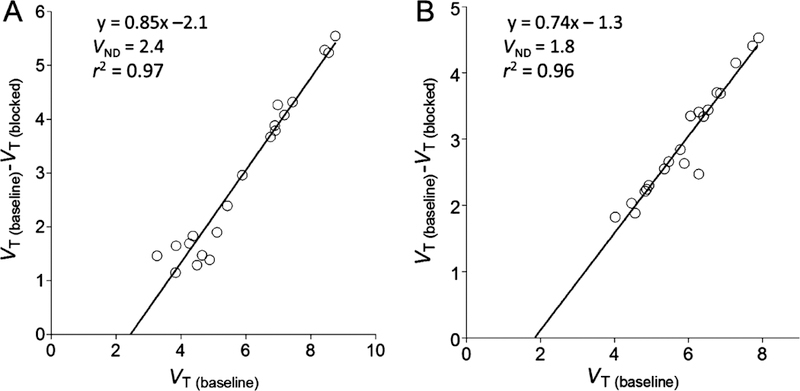
Lassen plots for [11C]PS13 in monkey brain, in which (A) PS13 (1 mg/kg) and (B) KTP-Me (3 mg/kg) were administered intravenously at 5–10 min before radioligand injection. The lines were fitted by linear regression.
CONCLUSIONS
Among the three evaluated 1,2,4-triazole-based radioligands, [11C]PS13 showed the most favorable characteristics for imaging and quantifying brain COX-1, such as moderately high brain uptake, appreciable COX-1 specific binding, identifiable washout, and robust VT values. [11C]PS13 merits further evaluation in monkey neuroinflammation models and in human subjects.
METHODS
Materials and Methods.
KTP-Me ((S)-ketoprofen methyl ester) was prepared18 from KTP ((S)-ketoprofen), purchased from Sigma-Aldrich (St. Louis, MO). The COX-2 ligand, MC1 (6-methoxy-2-(4-(methylsulfonyl)phenyl)-N-(thiophen-2-ylmethyl)pyrimidin-4-amine), was prepared as previously described.1
γ-Radioactivity from carbon-11 and fluorine-18 was measured with a calibrated dose calibrator (Atomlab 300, Biodex Medical Systems, Shirley, NY) or an automatic γ-counter (Wizard 3″, 1480 instrument; PerkinElmer; Waltham, MA). Radioactivity measurements were corrected for physical decay.
cLog D values were computed with Pallas for Windows software version 3.8 in default option (CompuDrug International; Bal Harbor, FL).
Results of statistical analyses are presented as mean ± SD, unless otherwise stated as SE (standard error).
Radioligand Syntheses.
Radioligands were prepared for intravenous injection in sterile saline-ethanol (90:10 v/v) for [11C]PS1 and [2H2,18F]PS2, or saline-ethanol (90:10 v/v) containing Tween 80 (1.2 mg/mL; J.T. Baker, Phillipsburg, NJ) for [11C]PS13, as described in Part 1.1
Radioligand Lipophilicity (Log D) Determinations.
The log D’s of [11C]PS1, [2H2,18F]PS2, and [11C]PS13 were measured with a method based on partition of formulated radioligand between n-octanol and sodium phosphate buffer (0.15 M; pH 7.4), as described previously.8 The amounts of radioactivity in the n-octanol and buffer phases were determined with a γ-counter. Radioactivity concentrations in the buffer phases were corrected for parent fraction with reversed phase radio-HPLC on a Novapak C18 column (100 × 8 mm, 4 μm; Waters Corp.; Milford, MA) fitted with a radial compression module (RCM-100) and eluted at 2.5 mL/min with MeOH–10 mM H3PO4 (60:40 v/v) for [11C]PS1 (tR = 2.48 min), MeOH–H2O–Et3N (85:15:0.1 by volume) for [2H2,18F]PS2 (tR = 3.65 min) and MeOH–H2O–Et3N (80–20–0.1 by volume) for [11C]PS13 (tR = 4.10 min).8
Stabilities of Radioligands in Monkey Whole Blood and Plasma in Vitro.
Samples of formulated [11C]PS1, [2H2,18F]PS2, and [11C]PS13 (2–12 μL) were incubated with monkey whole blood and plasma (200 μL) in vitro at room temperature for at least 30 min. Radioactive whole blood samples were then mixed with distilled water (300 μL) for 30 s to lyse blood cells. Samples (450 μL) of the lysed cells and the incubated radioactive plasma samples were each added to acetonitrile (720 μL) for deproteinization and then centrifuged (10 000g). The resultant clear supernatant liquids were analyzed with reversed phase radio-HPLC (as described above under log D determination). The precipitates were measured for radioactivity in a γ-counter to allow calculation of the extraction efficiencies. The extraction effi ciencies of all samples were 97 ± 3% (n = 65). The percentage of unchanged radioligand in the analyte, as determined by radio-HPLC, was divided by the radiochemical purity of the radioligand to give the stabilities of the radioligands in whole blood and plasma.
Plasma Free Fraction Determinations.
Plasma free fractions ( f p) were measured in triplicate for [11C]PS1, [ 2H2,18F]PS2, and [11C]PS13 in venous plasma for each monkey and in pooled human arterial plasma (stored at −80 °C). The latter served as the standard for normalization across studies. Measurements were performed by ultrafiltration through membrane filters (Centrifree, Millipore; Burlington, MA), as previously described.19
Monkey PET Experiments.
PET imaging experiments in male rhesus monkeys (Macaca mulatta, 7.5–12.8 kg) were performed in accordance with the Guide for Care and Use of Laboratory Animals20 and were approved by the Animal Care and Use Committee of the National Institute of Mental Health.
PET Scans.
Typically, the monkey subject was anesthetized with ketamine (10 mg/kg, i.m.) and then maintained in anesthesia with 1.6% isoflurane and 98.4% O2, for a single PET scanning session or for two sessions separated by at least 3 h. The position of the head was fixed using a stereotaxic frame. Electrocardiogram, body temperature, heart, and respiration rates were monitored throughout the scanning sessions. A microPET Focus 220 scanner (Siemens Medical Solution; Knoxville, TN) was used to acquire PET images of the brain.
PET experiments were performed with [11C]PS1 in one monkey, [2H2,18F]PS2 in one monkey, and [11C]PS13 in three different monkeys. At the start of each PET experiment, the radioligand (212 ± 37 MBq; 114 ± 74 GBq/μmol) was injected intravenously as a bolus (∼10 mL) over a period of 1 min. In the three PET scanning sessions with [11C]PS13, the baseline experiment was followed at more than 3 h later with a blocking PET experiment in which a COX-1 selective inhibitor (PS13 or KTP derived from KTP-Me) or a COX-2 selective inhibitor (MC1) (0.3 mg/kg), was administered intravenously at 5 to 10 min before the radioligand (246 ± 44 MBq; 105 ± 63 GBq/μmol). Each blocking agent was administered as a bolus in 20 mL of vehicle, composed of ethanol–propylene glycol–PEG-400–water (10:10:30:50 by volume) for PS13, ethanol-saline (10:90 v/v) for KTP-Me, and sodium citrate buffer (0.1 M citric acid–0.1 M trisodium citrate, 68.5:31.5 v/v)–ethanol–PEG-400 (65:10:25 by volume) for MC1.
PET data were acquired for 120 min in each baseline session to capture the full kinetic data and to enable the estimation of VT at late time points. Blocking experiments were performed for 90 min, which was found to be sufficient for reliable VT determination. Scan frame durations ranged from 30 s at the start to 10 min at the end of scanning.
Image Analysis.
PET images were reconstructed using Fourier rebinning plus two-dimensional filtered back-projection. Images were coregistered to a standardized monkey MRI template using SPM8 (The Wellcome Trust Centre for Neuroimaging, UCL, London, UK). A set of 33 predefined brain regions of interest from the template were then applied to the coregistered PET image to obtain regional decay-corrected time–activity curves. Reported whole brain data are from gray matter. Neocortex represented a weighted combination of frontal, cingulate, temporal, parietal, and occipital cortices. All PET images were corrected for attenuation and scatter. Radioactivity concen-trations were expressed as standardized uptake value (SUV), which normalizes for subject weight and injected radioactivity.
Analysis of [11C]PS13 Radiometabolites in Monkey Plasma.
To determine a radiometabolite-corrected arterial input function for brain PET scans, blood samples (0.5–1 mL each) were drawn from the femoral artery at 15 s intervals until 120 s, followed by 0.5–4 mL samples at 3, 5, 10, 30, 60, 90, and 120 min. The concentration of parent radioligand was measured with reversed phase HPLC on an X-terra column (7.8 × 300 mm, 10 μm; Waters Corp.) eluted at 5.0 mL/ min with methanol–water–triethylamine (85:15:0.1, by volume), after separating plasma from whole blood, as previously described.21
PET Data Analysis.
Total distribution volume (VT), a sum of a specific binding component known as the specific volume of distribution (VS) and a nondisplaceable volume of distribution (VND), may serve as an index of receptor density that equals the ratio at equilibrium of the concentration of radioligand in tissue to that in plasma.22 VT values, uncorrected for radioactivity in blood (5% of brain volume), were estimated for different brain regions with Logan graphical analysis23 by using the PET brain time–activity curves and the measured radiometabolite-corrected arterial input functions. Kinetic analyses were performed at the voxel level, so that the resulting VT values for [11C]PS13 could be shown as parametric PET images. The temporal stabilities of VT in whole brain in the baseline experiments (n = 3) were assessed by estimating VT from progressively time-truncated data sets. Standard Error (i.e., % SE or identifiability) was expressed as a percentage. A smaller percentage indicates better identifiability.24
Additionally, regional brain VT data were used to generate a Lassen plot25,26 to estimate COX-1 occupancy in the preblock condition and to estimate VND. The PET image analysis, including kinetic modeling, was performed with PMOD 3.704 (PMOD Technologies; Zurich, Switzerland).
Supplementary Material
ACKNOWLEDGMENTS
We thank the NIH Clinical PET Center (Director: Dr. P. Herscovitch) for radioisotope production.
Funding
This study was supported by the Intramural Research Program of the National Institute of Health (NIH) (Projects ZIAMH002852 and ZIA-MH002793).
ABBREVIATIONS
- COX-1
cyclooxygenase-1
- SUV
standardized uptake value
- VT
volume of distribution
- fp
plasma free fraction
Footnotes
Notes
The authors declare no competing financial interest.
Supporting Information
The Supporting Information is available free of charge on the ACS Publications website at DOI: 10.1021/acschemneuro.8b00103.
Additional PET results (PDF)
REFERENCES
- (1).Singh P, Shrestha S, Cortes-Salva MY, Jenko KJ, Zoghbi SS, Morse CL, Innis RB, and Pike VW (2018) 3-Substituted 1,5diaryl-1H-1,2,4-triazoles as prospective PET radioligands for imaging brain COX-1 in monkey. Part 1: synthesis and pharmacology. ACS Chem. Neurosci, 10.1021/acschemneuro.8b00102. [DOI] [PMC free article] [PubMed]
- (2).Aïd S, and Bosetti F (2011) Targeting cyclooxygenases-1 and -2 in neuroinflammation: Therapeutic implications. Biochimie 93, 46–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (3).Takashima-Hirano M, Shukuri M, Takashima T, Goto M, Wada Y, Watanabe Y, Doi H, and Suzuki M (2010) General method for the 11C-labeling of 2-arylpropionic acids and their esters, construction of a PET tracer library for a study of biological events involved in COXs expression. Chem. A - Eur. J 16, 4250–4258. [DOI] [PubMed] [Google Scholar]
- (4).Shukuri M, Mawatari A, Ohno M, Suzuki M, Doi M, Watanabe Y, and Onoe H (2016) Detection of cyclooxygenase-1 in activated microglia during amyloid plaque progression: PET studies in Alzheimer’s disease mouse model. J. Nucl. Med 57, 291–296. [DOI] [PubMed] [Google Scholar]
- (5).Ohnishi A, Senda M, Yamane T, Mikami T, Nishida H, Nishio T, Akamatsu G, Ikari Y, Kimoto S, Aita K, Sasaki M, Shinkawa H, Yamamoto Y, Shukuri M, Mawatari A, Doi H, Watanabe Y, and Onoe H (2016) Exploratory human PET study of the effectiveness of 11C-ketoprofen methyl ester, a potential biomarker of neuroinflammatory processes in Alzheimer’s disease. Nucl. Med. Biol 43, 438–444. [DOI] [PubMed] [Google Scholar]
- (6).Warner TD, Giuliano F, Vojnovic I, Bukasa A, Mitchell JA, and Vane JR (1999) Nonsteroid drug selectivities for cyclooxygenase-1 rather than cyclooxygenase-2 are associated with human gastrointestinal toxicity: a full in vitro analysis. Proc. Natl. Acad. Sci. U. S. A 96, 7563–7568; (1999) Erratum. Proc. Natl. Acad. Sci. U. S. A. 96, 9666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (7).Coenen HH, Gee AD, Adam M, Antoni G, Cutler CS, Fujibayashi Y, Jeong J-M, Mach RH, Mindt TL, Pike VW, and Windhorst AD (2017) Consensus nomenclature rules for radiopharmaceutical chemistry — setting the record straight. Nucl. Med. Biol 55,v–xi. [DOI] [PubMed] [Google Scholar]
- (8).Pike VW (2016) Considerations in the development of reversibly binding PET radioligands for brain imaging. Curr. Med. Chem 23, 1818–1869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (9).Zoghbi SS, Anderson KB, Jenko KJ, Luckenbaugh DA, Innis RB, and Pike VW (2012) On quantitative relationships between drug-like compound lipophilicity and plasma free fraction in monkey and human. J. Pharm. Sci 101, 1028–1039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (10).Schou M, Halldin C, Sovago J, Pike VW, Hall H, Gulyás B, Mozley PD, Dobson D, Shchukin E, Innis RB, and Farde L (2004) PET evaluation of novel radiofluorinated reboxetine analogs as norepinephrine transporter probes in the monkey brain. Synapse 53, 57–67. [DOI] [PubMed] [Google Scholar]
- (11).Terry GE, Hirvonen J, Liow J-S, Zoghbi SS, Gladding R, Tauscher JT, Schaus JM, Phebus L, Felder CC, Morse CL, Donohue SR, Pike VW, Halldin C, and Innis RB (2010) Imaging and quantitation of cannabinoid CB1 receptors in human and monkey brains using 18F-labeled inverse agonist radioligands. J. Nucl. Med 51, 112–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (12).Kuchar M, and Mamat C (2015) Methods to increase the metabolic stability of 18F-radiotracers. Molecules 20, 16186–16220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (13).Riss PJ, and Aigbirhio FI (2011) A simple, rapid procedure for nucleophilic radiosynthesis of aliphatic [18F]trifluoromethyl groups. Chem. Commun 47, 11873–11875. [DOI] [PubMed] [Google Scholar]
- (14).Orjales A, Mosquera R, Lopez B, Olivera R, Labeaga L, and Nuñez MT (2008) Novel 2-(4-methylsulfonylphenyl)pyrimidine derivatives as highly potent and specific COX-2 inhibitors. Bioorg. Med. Chem 16, 2183–2199. [DOI] [PubMed] [Google Scholar]
- (15).Cortes M, Singh P, Morse C, Shrestha S, Jenko K, Kowalski A, Zoghbi S, Fujita M, Innis R, and Pike V (2015) Synthesis of PET radioligands as potential probes for imaging COX-2 in neuroinflammation. J. Nucl. Med 56 (Suppl. 3), 1092. [Google Scholar]
- (16).Yermakova AV, Rollins J, Callahan LM, Rogers J, and O’Banion MK (1999) Cyclooxygenase-1 in human Alzheimer and control brain: quantitative analysis of expression by microglia and CA3 hippocampal neurons. J. Neuropathol. Exp. Neurol 58, 1135–1146. [DOI] [PubMed] [Google Scholar]
- (17).Abi-Dargham A, Gandelman M, Zoghbi SS, Laruelle M, Baldwin RM, Randall P, Zea-Ponce Y, Charney DS, Hoffer PB, and Innis RB (1995) Reproducibility of SPECT measurement of benzodiazepine receptors in human brain with iodine-123-iomazenil. J. Nucl. Med 36, 167–175. [PubMed] [Google Scholar]
- (18).Zheng G-W, Yu H-L, Zhang J-D, and Xu J-H (2009) Enzymatic production of l-menthol by a high substrate concentration tolerable esterase from newly isolated Bacillus subtilis ECU0554. Adv. Synth. Catal 351, 405–414. [Google Scholar]
- (19).Gandelman MS, Baldwin RM, Zoghbi SS, Zea-Ponce Y, and Innis R (1994) Evaluation of ultrafiltration for the free-fraction detection of single photon emission computed tomography (SPECT) radiotracers: β-CIT, IBF, and iomazenil. J. Pharm. Sci 83, 1014–1019. [DOI] [PubMed] [Google Scholar]
- (20).National Research Council. (2011) Guide for the Care and Use of Laboratory Animals, eighth ed., The National Academies Press, Washington, DC, 10.17226/5140. [DOI] [Google Scholar]
- (21).Zoghbi SS, Shetty UH, Ichise M, Fujita M, Imaizumi M, Liow J-S, Shah J, Musachio JL, Pike VW, and Innis RB (2006) PET Imaging of the dopamine transporter with 18F-FECNT: a polar radiometabolite confounds brain radioligand measurements. J. Nucl. Med 47, 520–527. [PubMed] [Google Scholar]
- (22).Innis RB, Cunningham VJ, Delforge J, Fujita M, Gjedde A, Gunn RN, Holden J, Houle S, Huang SC, Ichise M, Iida H, Ito H, Kimura Y, Koeppe RA, Knudsen GM, Knuuti J, Lammertsma AA, Laruelle M, Logan J, Maguire RP, Mintun MA, Morris ED, Parsey R, Price JC, Slifstein M, Sossi V, Suhara T, Votaw JR, Wong DF, and Carson RE (2007) Consensus nomenclature for in vivo imaging of reversibly binding radioligands. J. Cereb. Blood Flow Metab 27, 1533–1539. [DOI] [PubMed] [Google Scholar]
- (23).Logan J, Fowler JS, Volkow ND, Wolf AP, Dewey SL, Schlyer DJ, MacGregor RR, Hitzemann R, Bendriem B, Gatley SJ, and Christman DR (1990) Graphical analysis of reversible radioligand binding from time-activity measurements applied to [N-11C-methyl]-(-)-cocaine PET studies in human subjects. J. Cereb. Blood Flow Metab 10, 740–747. [DOI] [PubMed] [Google Scholar]
- (24).Carson RE (1986) Parameter estimation in positron emission tomography. In Positron Emission Tomography and Autoradiography: Principles and Applications for the Brain and Heart (Phelps ME, Mazziotta JC, and Schelbert HR, Eds.), Raven Press, New York, pp 347–390, Ch. 8. [Google Scholar]
- (25).Lassen NA, Bartenstein PA, Lammertsma AA, Prevett MC, Turton DR, Luthra SK, Osman S, Bloomfield PM, Jones T, Patsalos PN, O’Connell MT, Duncan JS, and Andersen JV (1995) Benzodiazepine receptor quantification in vivo in humans using [11C]flumazenil and PET: application of the steady-state principle. J. Cereb. Blood Flow Metab 15, 152–165. [DOI] [PubMed] [Google Scholar]
- (26).Cunningham VJ, Rabiner EA, Slifstein M, Laruelle M, and Gunn RN (2010) Measuring drug occupancy in the absence of a reference region: the Lassen plot re-visited. J. Cereb. Blood Flow Metab 30, 46–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.