Abstract
Objective
To provide family physicians with the information needed to recognize, diagnose, and discuss available treatment options for steatocystoma multiplex (SM).
Sources of information
A comprehensive PubMed search using steatocystoma multiplex as either a text word or a MeSH term was conducted, and articles reporting on treatment outcomes were included.
Main message
Steatocystoma multiplex is a benign disorder often characterized by numerous asymptomatic dermal cysts on the trunk, arms, axillae, face, thighs, and scalp. Psychological distress due to these undesirable lesions is not uncommon for this condition. A literature review identified the following SM treatments, all of which were associated with limitations: carbon dioxide laser, modified surgical techniques, cryotherapy, and medical management. Steatocystoma multiplex is challenging to treat and, at this time, effective management is most often achieved through patient education.
Conclusion
Family physicians play a critical role in the early diagnosis and management of SM. Education about treatment options and managing patient expectations might greatly alleviate the psychosocial implications of this disease.
Steatocystoma multiplex (SM) is a benign disorder of the pilosebaceous unit, manifesting as multiple asymptomatic dermal cysts. Although sporadic presentation is most often reported, it is believed to have an autosomal dominant pattern of inheritance involving a keratin 17 mutation.1 The following described case and review of treatment options can be used as a learning tool for how to recognize, diagnose, and manage SM. Early disease recognition and patient education might play a critical role in alleviating psychological implications associated with this disease.
Case description
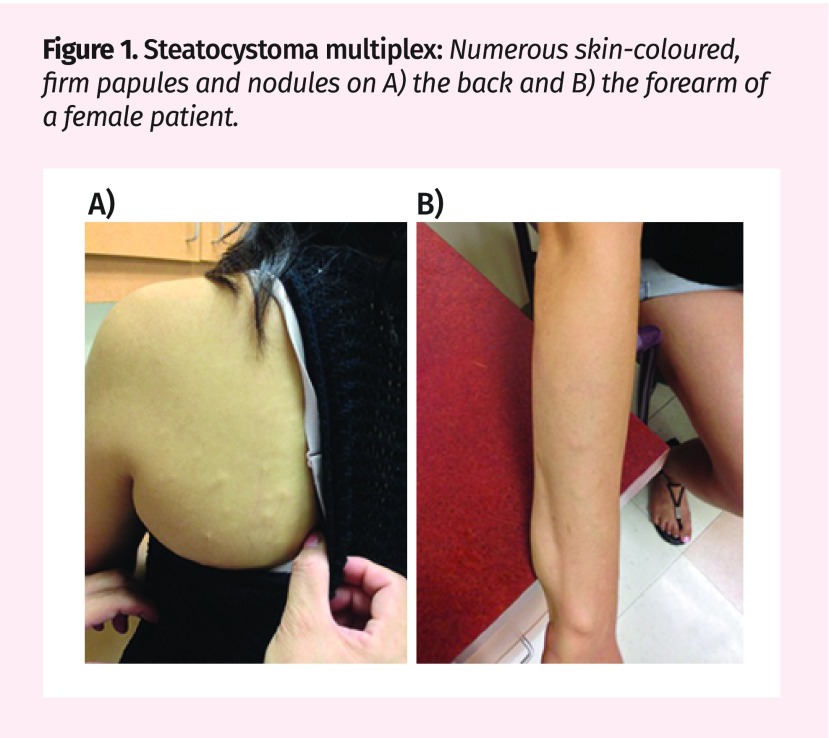
A 22-year-old woman presented to an academic dermatology clinic concerned about numerous bumps on her arms, thighs, and trunk. She was referred by her family doctor to confirm the diagnosis of SM and discuss treatment options for these cosmetically bothersome lesions. Physical examination revealed numerous yellow- to skin-coloured, firm, freely mobile papules and nodules on her arms, thighs, and trunk that had slowly enlarged and increased in number over 5 years (Figures 1A and 1B). Her family history was not relevant for similar lesions and no other cutaneous findings were identified at the time of presentation.
While her history and physical examination findings strongly suggested the diagnosis of SM, the patient requested a biopsy to obtain a definitive answer. Two punch biopsies were taken of subcutaneous nodules using a 4-mm full-thickness punch at 2 separate sites. Histopathology revealed encapsulated cysts lined by several layers of epithelial cells folded in an irregular manner. The cystic lumen was lined with a thick eosinophilic band. These findings confirmed the diagnosis of SM. The contents of the cyst could not be elucidated by the pathologist; however, vellus hairs and hair follicles are commonly observed under microscopy.2
Figure 1.
Steatocystoma multiplex: Numerous skin-coloured, firm papules and nodules on A) the back and B) the forearm of a female patient.
Sources of information
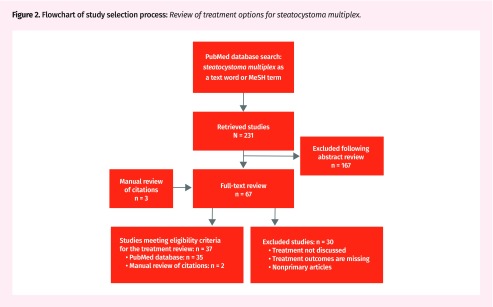
A review of the PubMed database was conducted and relevant studies were retrieved using steatocystoma multiplex as either a text word or a MeSH term on March 20, 2017. The initial search yielded 231 articles for screening (Figure 2). After abstract and full-text review, primary articles (ie, case reports or case series) reporting treatment outcomes for SM were identified for inclusion in this review of treatment options. In addition, manual reviews of citation lists for relevant articles were performed.
Figure 2.
Flowchart of study selection process: Review of treatment options for steatocystoma multiplex.
Main message
Common presentation.
Steatocystoma multiplex papules or nodules commonly present on areas with densely concentrated pilosebaceous units including the trunk, arms, axillae, face, thighs, scalp, and less commonly the genitals and breasts.3–6 It most frequently presents in adolescence or early adulthood, with a mean age of 26 years at the time of diagnosis, and has no predilection for sex.7 Although the lesions are asymptomatic, with no malignant potential, patients often seek treatment options owing to the psychological distress caused by the cosmetically undesirable lesions. The case described here represents the classic presentation of SM and highlights the important role family physicians can play in early disease recognition.
Diagnosis.
Although SM shares similar characteristics with other diseases, its diagnosis is often made through history and physical examination alone.8 Pathologic analysis of sebaceous cysts, such as those seen in SM, provides little value when there is a low index of concern for malignancy. For this reason, a diagnosis of SM based on clinical findings is often warranted unless clinical suspicion suggests otherwise.8 If a biopsy is required, multiple samples should be taken because variations in the classic histopathologic features of SM have been described.2 A 4-mm full-thickness punch biopsy is recommended.
Evaluation and differential diagnosis.
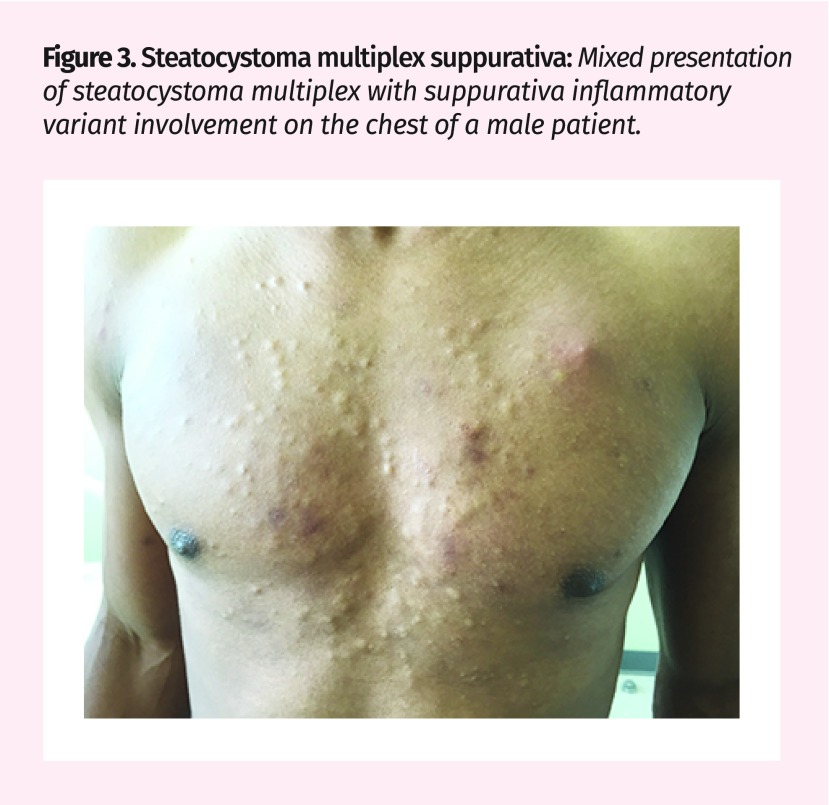
Despite the benign and often asymptomatic nature of this disease, an inflammatory variant known as steatocystoma multiplex suppurativa (SMS) can present.2 This is seen in a male patient who presented to the clinic with numerous SM lesions on his chest, some of which were inflamed (Figure 3). The inflamed lesions of SMS pose a great risk of infection, purulent discharge, and scarring.9 A mixed presentation of asymptomatic and inflamed lesions is common. Additionally, SM might mimic other common skin disorders, sometimes leading to misdiagnosis and unnecessary treatment. The clinical appearance of SM can resemble acne vulgaris, vellus cyst, epidermoid or dermoid cyst, hidradenitis suppurativa, milia, follicular infundibular tumours, and lipomas.10
Figure 3.
Steatocystoma multiplex suppurativa: Mixed presentation of steatocystoma multiplex with suppurativa inflammatory variant involvement on the chest of a male patient.
Treatment options.
Although SM is difficult to treat, having a strong understanding of all available treatment options, with a focus on recurrence and cosmetic outcomes, is crucial for patient education and disease perception. A total of 37 relevant publications describing treatment outcomes of SM patients were identified and are summarized in Table 1.3–5,9,11–43 Goals of SM treatment include substantial reduction of cyst size, prevention of recurrence, good cosmetic outcome, and patient satisfaction. At this time, no treatment can prevent the formation of new lesions. Positive outcomes are often challenging to achieve, as the described treatment methods are associated with limitations. Effective management is most often achieved through patient education. However, recent advanced techniques include the following.
Table 1.
Summary of available publications describing treatment outcomes for SM, by treatment
| REFERENCE | NO. OF PARTICIPANTS | SM OR SMS | LOCATION OF CYSTS | TREATMENT DESCRIPTION | BENEFITS | LIMITATIONS |
|---|---|---|---|---|---|---|
| Laser | ||||||
| Kassira et al, 201611 | 1 | SM | Face | Fractionated ablative CO2 laser |
|
|
| Bakkour and Madan, 201412 | 8 | SM | Chest, back, and axilla | CO2 laser incision and cyst removal with Volkmann spoon |
|
|
| Moody et al, 201213 | 1 | SM | Abdomen and lower chest | Targeted laser treatment of the sebaceous glands and dermal cysts |
|
|
| Varshney et al, 201114 | 1 | SM | Head and neck | CO2 laser ablation |
|
|
| Mumcuoğlu et al, 201015 | 1 | SM | Chest, forehead, axillae, and knees | Er:YAG laser and drainage |
|
|
| Madan and August, 200916 | 1 | SM | Back, chest, and abdomen | CO2 laser incision and cyst removal with Volkmann spoon |
|
|
| Riedel et al,* 200817 | 1 | SM | Forehead and cheeks | Laser and surgical: incision, cyst removal with sharp spoon, followed by CO2 vaporization of remaining content |
|
|
| Rossi et al, 200318 | 1 | SM | Forehead, eyelids, and neck | CO2 laser and cyst removal with forceps |
|
|
| Krähenbühl et al, 199119 | 1 | SM | Trunk | Focused CO2 laser incision followed by defocused laser therapy of cyst wall |
|
|
| Surgical | ||||||
| Kumar et al, 201420 | 1 | SM | Malar region | Wide local surgical excision |
|
|
| Gordon Spratt et al,* 201321 | 1 | SMS | Thigh, buttocks, groin, arms, and legs | Surgical and antimicrobial therapy: incision and drainage followed by topical clindamycin solution and benzoyl peroxide wash |
|
|
| Choudhary et al, 20104 | 2 | SM | Scrotum | Incision using a radiofrequency instrument, drainage, and cyst extraction with forceps |
|
|
| Lee et al, 200722 | 5 | SM | Not reported | Incision and vein hook cyst removal |
|
|
| Ichikawa et al, 200623 | 1 | SM | Face | Forehead flap and cyst extraction |
|
|
| Düzova and Șentürk, 200424 | 2 | SM | Face | 22-gauge needle aspiration |
|
|
| Kaya et al, 200125 | 1 | SM | Chest, neck, axilla, inguinal folds, and inguinal regions | Puncture with sharp-tipped cautery point, drainage, and cyst removal with forceps |
|
|
| Schmook et al, 200126 | 5 | SM | Not reported | Incision, drainage, and cyst wall removal with curette followed by forceps |
|
|
| Adams et al, 199927 | 1 | SM | Chest and neck | Incision and cyst removal with small artery forceps |
|
|
| Oertel and Scott, 19985 | 3 | SM | Arm, forearm, chest, neck, axilla, and breast | 22-gauge needle aspiration |
|
|
| Pamoukian and Westreich, 199728 | 7 | SM | Head and neck | Incision and cyst removal with mosquito hemostat |
|
|
| Kanekura et al, 199529 | 1 | SM | Scalp, forehead, and chest | 3-mm biopsy punch, drainage, and cyst removal with forceps |
|
|
| Sato et al, 199330 | 1 | SM | Head, neck, trunk, and upper extremities | Aspiration and scraping with a syringe connected to an 18-gauge needle |
|
|
| Keefe et al, 199231 | 1 | SM | Neck, forearms, behind the ears, over the scapula, chest | Surgical blade puncture, drainage, and cyst removal with forceps |
|
|
| Feinstein et al, 198332 | 1 | SM | Scalp and forehead | Excision and skin graft |
|
|
| Holmes and Black, 198033 | 1 | SM | Face, trunk, and axillae | Hairline flap and cyst extraction |
|
|
| Egbert et al, 197934 | 1 | SMS and SM | Entire body surface | Incision, drainage, and electrocautery |
|
|
| Medical management | ||||||
| Lima Santana et al, 201635 | 1 | SMS | Axillary regions, inguinal region, trunk, lower limbs, antecubital fossae, face, and scalp | Isotretinoin |
|
|
| Adams and Shwayder, 200836 | 1 | SMS | Face, scalp, trunk, and extremities | Tetracycline |
|
|
| Moritz and Silverman, 198837 | 1 | NA | Not reported | Isotretinoin |
|
|
| Friedman, 198738 | 1 | SM | Not reported | Isotretinoin |
|
|
| Rosen and Brodkin, 198639 | 1 | SMS | Not reported | Isotretinoin |
|
|
| Statham and Cunliffe, 198440 | 3 | SMS and SM | Trunk and limbs | Isotretinoin |
|
|
| Schwartz and Goldsmith, 198441 | 1 | SMS | Not reported | Isotretinoin |
|
|
| Other | ||||||
| Kamra et al,*20133 | 1 | SM | Chest, breast, axilla, inguinal region, and extremities | Radiofrequency probe and isotretinoin |
|
|
| Fekete and Fekete,* 201042 | 1 | SMS and SM | Entire body surface | Cryotherapy and isotretinoin |
|
|
| Apaydin et al,* 20009 | 1 | SMS and SM | Entire body surface | Cryotherapy and isotretinoin |
|
|
| Notowicz, 198043 | NA | SM | Not reported | Cryotherapy: necrotic tissue and cyst content removed with pressure 3–4 d later |
|
|
CO2—carbon dioxide, Er:YAG—erbium:yttrium-aluminum-garnet, NA—not available, SM—steatocystoma multiplex, SMS–steatocystoma multiplex suppurativa.
Combination therapy.
Carbon dioxide laser: Carbon dioxide laser has recently been shown to successfully treat multiple lesions in a single session with good cosmetic outcomes. However, this procedure might not be suited for larger cysts and is not easily accessible to all patients.11,12 This laser method is comparable to excising the lesion, as the wavelength of the laser ablates skin tissue.
Modified needle aspiration: Needle aspiration with gentle extirpation of cystic contents has proven successful, with excellent cosmetic outcomes.5,13,14 Despite good results, this treatment requires a skilled operator and does not work well on very large (> 15 mm in diameter) or small (< 3 mm in diameter) cysts. Recurrence rates are extremely high for this treatment method.
Modified surgical techniques: Surgical techniques, including fine incision followed by cyst wall extraction with forceps, vein hooks, or curette, show excellent cosmetic results but are time-consuming and invasive.4,15–17
Cryotherapy: Cryotherapy allows for the treatment of multiple lesions in a single session; however, it is greatly limited owing to the cosmetic disfigurement it causes and its extremely low efficacy.9,18
Medical management: Medical management with oral isotretinoin is the preferred treatment for SMS and it provides great reduction in inflammation.9,19,20 However, results are often not seen for months and recurrence following discontinuation has been reported.21,22 Mixed variants of both SM and SMS might require combination therapy.9,18 Isotretinoin has no effect on noninflamed lesions.20 A short course (2 to 4 weeks) of oral tetracycline, topical clindamycin, or benzoyl peroxide wash (ie, antibiotics with anti-inflammatory properties) might be considered for management of noninfectious inflammatory lesions.21,36
Case resolution
Two weeks after the biopsies were taken, the patient was seen in the clinic for consultation regarding her confirmed diagnosis of SM. After educational guidance, she was aware that this condition posed no medical risk and that treatment was not required or recommended. Owing to the extensive number of lesions and evidence showing that effective treatment often leads to scarring, the patient elected to forgo therapy at this time. She was instructed to return for follow-up should any changes occur, including extensive growth, discoloration, or severe inflammation suggesting infection.
Conclusion
Owing to limited evidence for effective treatment methods, SM is a therapeutically challenging diagnosis. The ability to identify multiple asymptomatic dermal cysts and recognize the characteristic pattern of multiplication and progressive growth seen in SM can allow for early education about the benign nature of this disease. Furthermore, a concrete understanding of treatment options, including risks and benefits, can play a critical role in managing the psychosocial implications of SM. Patients should be informed that effective treatment options are time-consuming and often result in scarring, and recurrence is common. Unrealistic expectations and risks of unnecessary treatment should be discussed in depth with this patient population, as these individuals might desire unattainable outcomes.
Editor’s key points
▸ Steatocystoma multiplex is a benign disorder that presents as papules or nodules on areas with densely concentrated pilosebaceous units including the trunk, arms, axillae, face, thighs, scalp, and less commonly the genitals and breasts. Although the lesions are asymptomatic, with no malignant potential, patients often seek treatment options owing to the psychological distress caused by the cosmetically undesirable lesions.
▸ Despite the benign and often asymptomatic nature of this disease, an inflammatory variant known as steatocystoma multiplex suppurativa can present. The inflamed lesions of steatocystoma multiplex suppurativa pose a great risk of infection, purulent discharge, and scarring.
▸ Patients should be informed that effective treatment options are time-consuming and can result in scarring, and recurrence is common. Unrealistic expectations and risks of unnecessary treatment should be discussed in depth with this patient population.
Footnotes
Contributors
All authors contributed to the literature review and interpretation, and to preparing the manuscript for submission.
Competing interests
None declared
This article is eligible for Mainpro+ certified Self-Learning credits. To earn credits, go to www.cfp.ca and click on the Mainpro+ link.
This article has been peer reviewed.
La traduction en français de cet article se trouve à www.cfp.ca dans la table des matières du numéro de décembre 2018 à la page e517.
References
- 1.Covello SP, Smith FJ, Sillevis Smitt JH, Paller AS, Munro CS, Jonkman MF, et al. Keratin 17 mutations cause either steatocystoma multiplex or pachyonychia congenita type 2. Br J Dermatol. 1998;139(3):475–80. doi: 10.1046/j.1365-2133.1998.02413.x. [DOI] [PubMed] [Google Scholar]
- 2.Plewig G, Wolff HH, Braun-Falco O. Steatocystoma multiplex: anatomic reevaluation, electron microscopy, and autoradiography. Arch Dermatol Res. 1982;272(3–4):363–80. doi: 10.1007/BF00509068. [DOI] [PubMed] [Google Scholar]
- 3.Kamra HT, Gadgil PA, Ovhal AG, Narkhede RR. Steatocystoma multiplex—a rare genetic disorder: a case report and review of the literature. J Clin Diagn Res. 2013;7(1):166–8. doi: 10.7860/JCDR/2012/4691.2698. Epub 2013 Jan 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Choudhary S, Koley S, Salodkar A. A modified surgical technique for steatocystoma multiplex. J Cutan Aesthet Surg. 2010;3(1):25–8. doi: 10.4103/0974-2077.63284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Oertel YC, Scott DM. Cytologic-pathologic correlations: fine needle aspiration of three cases of steatocystoma multiplex. Ann Diagn Pathol. 1998;2(5):318–20. doi: 10.1016/s1092-9134(98)80025-7. [DOI] [PubMed] [Google Scholar]
- 6.Senel E. Steatocystoma multiplex [Dermacase] Can Fam Physician. 2010;56:667, 672. [PMC free article] [PubMed] [Google Scholar]
- 7.Cho S, Chang SE, Choi JH, Sung KJ, Moon KC, Koh JK. Clinical and histologic features of 64 cases of steatocystoma multiplex. J Dermatol. 2002;29(3):152–6. doi: 10.1111/j.1346-8138.2002.tb00238.x. [DOI] [PubMed] [Google Scholar]
- 8.Gargya V, Lucas HD, Wendel Spiczka AJ, Mahabir RC. Is routine pathologic evaluation of sebaceous cysts necessary?: a 15-year retrospective review of a single institution. Ann Plast Surg. 2017;78(2):e1–3. doi: 10.1097/SAP.0000000000000826. [DOI] [PubMed] [Google Scholar]
- 9.Apaydin R, Bilen N, Bayramgürler D, Başdaş F, Harova G, Dökmeci C. Steatocystoma multiplex suppurativum: oral isotretinoin treatment combined with cryotherapy. Australas J Dermatol. 2000;41(2):98–100. doi: 10.1046/j.1440-0960.2000.00403.x. [DOI] [PubMed] [Google Scholar]
- 10.Vivas A, Keri J. Steatocystoma multiplex. In: Zeichner JA, editor. Acneiform eruptions in dermatology. A differential diagnosis. New York, NY: Springer; 2014. pp. 343–8. [Google Scholar]
- 11.Kassira S, Korta DZ, de Feraudy S, Zachary CB. Fractionated ablative carbon dioxide laser treatment of steatocystoma multiplex. J Cosmet Laser Ther. 2016;18(7):364–6. doi: 10.1080/14764172.2016.1188212. Epub 2016 Jul 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bakkour W, Madan V. Carbon dioxide laser perforation and extirpation of steatocystoma multiplex. Dermatol Surg. 2014;40(6):658–62. doi: 10.1111/dsu.0000000000000013. [DOI] [PubMed] [Google Scholar]
- 13.Moody MN, Landau JM, Goldberg LH, Friedman PM. 1450-nm diode laser in combination with the 1550-nm fractionated erbium-doped fiber laser for the treatment of steatocystoma multiplex: a case report. Dermatol Surg. 2012;38(7 Pt 1):1104–6. doi: 10.1111/j.1524-4725.2012.02391.x. Epub 2012 Apr 9. [DOI] [PubMed] [Google Scholar]
- 14.Varshney M, Aziz M, Maheshwari V, Alam K, Jain A, Arif SH, et al. Steatocystoma multiplex. BMJ Case Rep. 2011;2011 doi: 10.1136/bcr.04.2011.4165. bcr0420114165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mumcuoğlu CT, Gurel MS, Kiremitci U, Erdemir AVT, Karakoca Y, Huten O. Er:YAG laser therapy for steatocystoma multiplex. Indian J Dermatol. 2010;55(3):300–1. doi: 10.4103/0019-5154.70690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Madan V, August PJ. Perforation and extirpation of steatocystoma multiplex. Int J Dermatol. 2009;48(3):329–30. doi: 10.1111/j.1365-4632.2009.03904.x. [DOI] [PubMed] [Google Scholar]
- 17.Riedel C, Brinkmeier T, Kutzne H, Plewig G, Frosch PJ. Late onset of a facial variant of steatocystoma multiplex—calretinin as a specific marker of the follicular companion cell layer. J Dtsch Dermatol Ges. 2008;6(6):480–2. doi: 10.1111/j.1610-0387.2007.06603.x. [DOI] [PubMed] [Google Scholar]
- 18.Rossi R, Cappugi P, Battini M, Mavilia L, Campolmi P. CO laser therapy in a case of steatocystoma multiplex with prominent nodules on the face and neck. Int J Dermatol. 2003;42(4):302–4. doi: 10.1046/j.1365-4362.2003.01309.x. [DOI] [PubMed] [Google Scholar]
- 19.Krähenbühl A, Eichmann A, Pfaltz M. CO2 laser therapy for steatocystoma multiplex. Dermatologica. 1991;183(4):294–6. doi: 10.1159/000247704. [DOI] [PubMed] [Google Scholar]
- 20.Kumar S, Kurien NM, Menon V. Steatocystoma multiplex of face: a case report. Int J Case Rep Imag. 2014;5(3):207–10. [Google Scholar]
- 21.Gordon Spratt EA, Kaplan J, Patel RR, Kamino H, Ramachandran SM. Steatocystoma. Dermatol Online J. 2013;19(12):20721. [PubMed] [Google Scholar]
- 22.Lee SJ, Choe YS, Park BC, Lee WJ, Kim DW. The vein hook successfully used for eradication of steatocystoma multiplex. Dermatol Surg. 2007;33(1):82–4. doi: 10.1111/j.1524-4725.2007.33013.x. [DOI] [PubMed] [Google Scholar]
- 23.Ichikawa K, Akamatsu T, Tanino R, Miyasaka M. Surgical treatment of facial steatocystoma multiplex. Eur J Plast Surg. 2006;29(2):81–4. [Google Scholar]
- 24.Düzova AN, Șentürk GB. Suggestion for the treatment of steatocystoma multiplex located exclusively on the face. Int J Dermatol. 2004;43(1):60–2. doi: 10.1111/j.1365-4632.2004.02068.x. [DOI] [PubMed] [Google Scholar]
- 25.Kaya TI, Ikizoglu G, Kokturk A, Tursen U. A simple surgical technique for the treatment of steatocystoma multiplex. Int J Dermatol. 2001;40(12):785–8. doi: 10.1046/j.1365-4362.2001.01325.x. [DOI] [PubMed] [Google Scholar]
- 26.Schmook T, Burg G, Hafner J. Surgical pearl: mini-incisions for the extraction of steatocystoma multiplex. J Am Acad Dermatol. 2001;44(6):1041–2. doi: 10.1067/mjd.2001.112351. [DOI] [PubMed] [Google Scholar]
- 27.Adams BB, Mutasim DF, Nordlund JJ. Steatocystoma multiplex: a quick removal technique. Cutis. 1999;64(2):127–30. [PubMed] [Google Scholar]
- 28.Pamoukian VN, Westreich M. Five generations with steatocystoma multiplex congenita: a treatment regimen. Plast Reconstr Surg. 1997;99(4):1142–6. doi: 10.1097/00006534-199704000-00036. [DOI] [PubMed] [Google Scholar]
- 29.Kanekura T, Kawamura K, Nishi M, Kanzaki T. A case of steatocystoma multiplex with prominent cysts on the scalp treated successfully using a simple surgical technique. J Dermatol. 1995;22(6):438–40. doi: 10.1111/j.1346-8138.1995.tb03420.x. [DOI] [PubMed] [Google Scholar]
- 30.Sato K, Shibuya K, Taguchi H, Kitano Y, Yoshikawa K. Aspiration therapy in steatocystoma multiplex. Arch Dermatol. 1993;129(1):35–7. [PubMed] [Google Scholar]
- 31.Keefe M, Leppard BJ, Royle G. Successful treatment of steatocystoma multiplex by simple surgery. Br J Dermatol. 1992;127(1):41–4. doi: 10.1111/j.1365-2133.1992.tb14825.x. [DOI] [PubMed] [Google Scholar]
- 32.Feinstein A, Trau H, Movshovitz M, Schewach-Millet M. Steatocystoma multiplex. Cutis. 1983;31(4):425–7. [PubMed] [Google Scholar]
- 33.Holmes R, Black MM. Steatocystoma multiplex with unusually prominent cysts on the face. Br J Dermatol. 1980;102(6):711–3. doi: 10.1111/j.1365-2133.1980.tb06573.x. [DOI] [PubMed] [Google Scholar]
- 34.Egbert BM, Price NM, Segal RJ. Steatocystoma multiplex. Report of a florid case and a review. Arch Dermatol. 1979;115(3):334–5. doi: 10.1001/archderm.115.3.334. [DOI] [PubMed] [Google Scholar]
- 35.Lima Santana CNL, do Nascimento Pereira D, Paixão Lisboa A, Martins Leal J, Lago Obadia D, Souto da Silva R. Steatocystoma multiplex suppurativa: case report of a rare condition. An Bras Dermatol. 2016;91(5 Suppl 1):51–3. doi: 10.1590/abd1806-4841.20164539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Adams B, Shwayder T. Steatocystoma multiplex suppurativum. Int J Dermatol. 2008;47(11):1155–6. doi: 10.1111/j.1365-4632.2008.03698.x. [DOI] [PubMed] [Google Scholar]
- 37.Moritz DL, Silverman RA. Steatocystoma multiplex treated with isotretinoin: a delayed response. Cutis. 1988;42(5):437–9. [PubMed] [Google Scholar]
- 38.Friedman SJ. Treatment of steatocystoma multiplex and pseudofolliculitis barbae with isotretinoin. Cutis. 1987;39(6):506–7. [PubMed] [Google Scholar]
- 39.Rosen BL, Brodkin RH. Isotretinoin in the treatment of steatocystoma multiplex: a possible adverse reaction. Cutis. 1986;37(2):115, 120. [PubMed] [Google Scholar]
- 40.Statham BN, Cunliffe WJ. The treatment of steatocystoma multiplex suppurativum with isotretinoin. Br J Dermatol. 1984;111(2):246. doi: 10.1111/j.1365-2133.1984.tb04054.x. [DOI] [PubMed] [Google Scholar]
- 41.Schwartz JL, Goldsmith LA. Steatocystoma multiplex suppurativum: treatment with isotretinoin. Cutis. 1984;34(2):149–50. 153. [PubMed] [Google Scholar]
- 42.Fekete GL, Fekete JE. Steatocystoma multiplex generalisata partially suppurativa—case report. Acta Dermatovenerol Croat. 2010;18(2):114–9. [PubMed] [Google Scholar]
- 43.Notowicz A. Treatment of lesions of steatocystoma multiplex and other epidermal cysts by cryosurgery. J Dermatol Surg Oncol. 1980;6(2):98–9. doi: 10.1111/j.1524-4725.1980.tb00820.x. [DOI] [PubMed] [Google Scholar]